Monitoring of Changes in Masticatory Muscle Stiffness after Gum Chewing Using Shear Wave Elastography
Abstract
1. Introduction
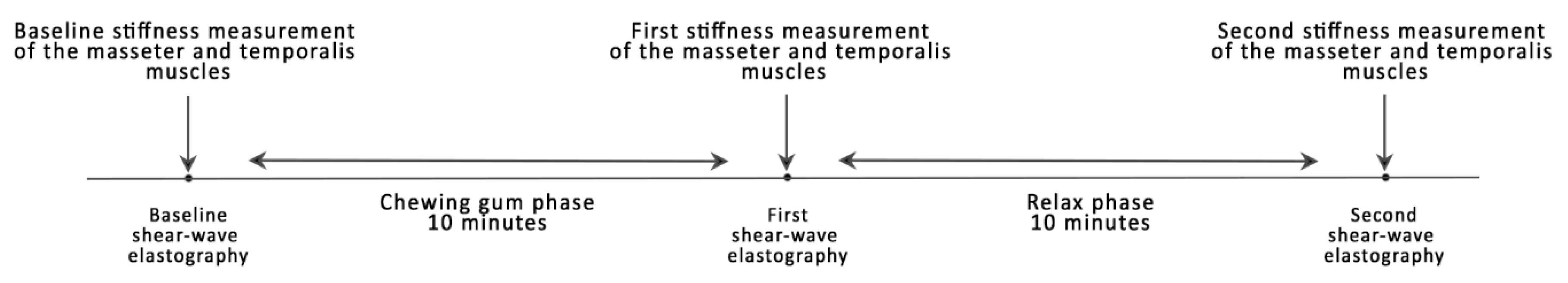
2. Experimental Section
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Basit, H.; Tariq, M.A.; Siccardi, M.A. Anatomy, Head and Neck, Mastication Muscles. Available online: https://www.ncbi.nlm.nih.gov/books/NBK541027/ (accessed on 15 March 2021).
- De Andrade, R.A.; de Cunha, M.D.; da Costa dos Santos Reis, A.M. Morphofunctional analysis of the stomatognathic system in conventional complete dentures users from the Integrated Health Center. Rev. CEFAC 2017, 19, 712–725. [Google Scholar] [CrossRef]
- Alomar, X.; Medrano, J.; Cabratosa, J.; Clavero, J.A.; Lorente, M.; Serra, I.; Monill, J.M.; Salvador, A. Anatomy of the temporomandibular joint. Semin. Ultrasound CT MRI 2007, 28, 170–183. [Google Scholar] [CrossRef] [PubMed]
- Schiffman, E.; Ohrbach, R. Executive summary of the Diagnostic Criteria for Temporomandibular Disorders for clinical and research applications. J. Am. Dent. Assoc. 2016, 147, 438–445. [Google Scholar] [CrossRef] [PubMed]
- Peck, C.C.; Goulet, J.P.; Lobbezoo, F.; Schiffman, E.L.; Alstergren, P.; Anderson, G.C.; de Leeuw, R.; Jensen, R.; Michelotti, A.; Ohrbach, R.; et al. Expanding the taxonomy of the diagnostic criteria for temporomandibular disorders. J. Oral Rehabil. 2014, 41, 2–23. [Google Scholar] [CrossRef]
- Janal, M.N.; Raphael, K.G.; Nayak, S.; Klausner, J. Prevalence of myofascial temporomandibular disorder in US community women. J. Oral Rehabil. 2008, 35, 801–809. [Google Scholar] [CrossRef] [PubMed]
- Al-Jundi, M.A.; John, M.T.; Setz, J.M.; Szentpetery, A.; Kuss, O. Meta-analysis of treatment need for temporomandibular disorders in adult nonpatients. J. Orofac. Pain 2008, 22, 97–107. [Google Scholar] [PubMed]
- Santosh, V.; Hinduja, S.; Manoj, R.; Waghmare, M. Overlaid temporomandibular joint disorders and otology symptoms—A diagnostic approach and management considerations for otolaryngologists and dentists. East. J. Med. Sci. 2020, 5, 25–29. [Google Scholar] [CrossRef]
- Ciancaglini, R.; Testa, M.; Radaelli, G. Association of neck pain with symptoms of temporomandibular dysfunction in the general adult population. Scand. J. Rehabil. Med. 1999, 31, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Cuccia, A.; Caradonna, C. The relationship between the stomatognathic system and body posture. Clinics 2009, 64, 61–66. [Google Scholar] [CrossRef]
- Motta, L.J.; Guedes, C.C.; De Santis, T.O.; Fernandes, K.P.; Mesquita-Ferrari, R.A.; Bussadori, S.K. Association between parafunctional habits and signs and symptoms of temporomandibular dysfunction among adolescents. Oral Health Prev. Dent. 2013, 11, 3–7. [Google Scholar]
- Woźniak, K.; Lipski, M.; Lichota, D.; Szyszka-Sommerfeld, L. Muscle Fatigue in the Temporal and Masseter Muscles in Patients with Temporomandibular Dysfunction. BioMed Res. Int. 2015, 2015, 269734. [Google Scholar] [CrossRef]
- Sarwono, A.P.; Himawan, L.S.; Tant, I. Differences in Pain Threshold Values of Masseter and Temporalis Muscles before and after Mastication. Pesqui. Bras. Odontopediatria Clin. Integr. 2019, 19. [Google Scholar] [CrossRef]
- Lee, Y.-H.; Lee, K.M.; Auh, Q.-S. MRI-Based Assessment of Masticatory Muscle Changes in TMD Patients after Whiplash Injury. J. Clin. Med. 2021, 10, 1404. [Google Scholar] [CrossRef]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.-P.; List, T.; Svensson, P.; Gonzalez, Y.; Lobbezoo, F.; et al. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: Recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J. Oral Facial. Pain Headache 2014, 28, 6–27. [Google Scholar] [CrossRef]
- Komino, M.; Shiga, H. Changes in mandibular movement during chewing of different hardness foods. Odontology 2017, 105, 418–425. [Google Scholar] [CrossRef] [PubMed]
- Cho, G.-H.; Lee, Y. Analysis of Masticatory Muscle Activity Based on Presence of Temporomandibular Joint Disorders. Med. Sci. Monit. 2020, 26, e921337-1–e921337-7. [Google Scholar] [CrossRef] [PubMed]
- Almutairi, A.F.; Albesher, N.; Aljohani, M.; Alsinanni, M.; Turkistani, O.; Salam, M. Association of oral parafunctional habits with anxiety and the Big-Five Personality Traits in the Saudi adult population. Saudi Dent. J. 2021, 33, 90–98. [Google Scholar] [CrossRef]
- Karabicak, G.O.; Hazar Kanik, Z. Temporomandibular disorder prevalence and its association with oral parafunctions, neck pain, and neck function in healthcare students: A cross-sectional study. Cranio 2020, 1–7. [Google Scholar] [CrossRef]
- Owczarek, J.E.; Lion, K.M.; Radwan-Oczko, M. Manifestation of stress and anxiety in the stomatognathic system of undergraduate dentistry students. J. Int. Med. Res. 2020, 48, 300060519889487. [Google Scholar] [CrossRef]
- Ali, K.; Fatima, A.; Ilyas, F.; Khan, M.; Abbassi, Z. Impact of Anxiety and Depression on Temporomandibular Joint Disorders among Sample of Dental Undergraduates of Karachi. J. Pak. Dent. Assoc. 2016, 25, 143–149. [Google Scholar]
- Douglas, C.R.; Avoglio, J.L.V.; de Oliveira, H. Stomatognathic adaptive motor syndrome is the correct diagnosis for temporomandibular disorders. Med. Hypotheses 2010, 74, 710–718. [Google Scholar] [CrossRef]
- Gavish, A.; Winocur, E.; Astandzelov-Nachmias, T.; Gazit, E. Effect of controlled masticatory exercise on pain and muscle performance in myofascial pain patients: A pilot study. Cranio 2006, 24, 184–190. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.-J.; Lee, J.-Y.; Lee, E.-S.; Jung, H.-J.; Ahn, H.-J.; Jung, H.I.; Kim, B.I. Simple oral exercise with chewing gum for improving oral function in older adults. Aging Clin. Exp. Res. 2020. [Google Scholar] [CrossRef] [PubMed]
- Olchowy, A.; Wieckiewicz, M.; Winocur, E.; Dominiak, M.; Dekkers, I.; Łasecki, M.; Olchowy, C. Great potential of ultrasound elastography for the assessment of the masseter muscle in patients with temporomandibular disorders. A systematic review. Dentomaxillofac. Radiol. 2020, 49, 20200024. [Google Scholar] [CrossRef]
- Olchowy, C.; Więckiewicz, M.; Sconfienza, L.M.; Łasecki, M.; Seweryn, P.; Smardz, J.; Hnitecka, S.; Dominiak, M.; Olchowy, A. Potential of Using Shear Wave Elastography in the Clinical Evaluation and Monitoring of Changes in Masseter Muscle Stiffness. Pain Res. Manag. 2020, 2020, 4184268. [Google Scholar] [CrossRef] [PubMed]
- Ariji, Y.; Nakayama, M.; Nishiyama, W.; Ogi, N.; Sakuma, S.; Katsumata, A.; Kurita, K.; Ariji, E. Can sonographic features be efficacy predictors of robotic massage treatment for masseter and temporal muscle in patients with temporomandibular disorder with myofascial pain? Cranio 2016, 34, 13–19. [Google Scholar] [CrossRef] [PubMed]
| Baseline Measurement, Mean (SD), KPa | First Measurement, Mean (SD), KPa | Second Measurement, Mean (SD), KPa | |
|---|---|---|---|
| Left masseter muscle | 10.99 (2.04) | 12.31 (1.38) | 11.29 (2.01) |
| Right masseter muscle | 11.01 (2.21) | 12.32 (1.65) | 11.30 (1.73) |
| Left temporalis muscle | 10.23 (1.23) | 10.92 (1.68) | 10.65 (1.68) |
| Right temporalis muscle | 10.14 (1.32) | 10.73 (1.70) | 10.62 (1.71) |
| Baseline Measurement, Median (IQR), KPa | First Measurement, Median (IQR), KPa | Second Measurement, Median (IQR), KPa | |
|---|---|---|---|
| Masseter muscle | 11.35 (9.7–12.65) | 12.5 (11.1–13.25) | 11.75 (9.95–12.6) |
| Temporalis muscle | 10.1 (9.1–10.95) | 10.3 (10.2–10.52) | 10.2 (9.65–11.9) |
| Difference in medians | 1.25 | 2.2 | 1.55 |
| p-value | 0.0001 | 0.0001 | 0.0033 |
| Median (IQR) | Baseline | 1st Measurement | 2nd Measurement | |||
|---|---|---|---|---|---|---|
| Masseter Muscle (p < 0.0001) | ||||||
| Baseline 11.35 (9.7–12.65) | p < 0.05 | p < 0.05 | ||||
| 1st measurement 12.5 (11.1–13.25) | p < 0.05 | |||||
| 2nd measurement 11.75 (9.95–12.6) | ||||||
| Temporalis Muscle (p < 0.0001) | ||||||
| Baseline 10.1 (9.1–10.95) | p < 0.05 | p < 0.05 | ||||
| 1st measurement 10.3 (9.95–12.2) | p < 0.05 | |||||
| 2nd measurement 10.2 (9.65–11.9) | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Olchowy, C.; Grzech-Leśniak, K.; Hadzik, J.; Olchowy, A.; Łasecki, M. Monitoring of Changes in Masticatory Muscle Stiffness after Gum Chewing Using Shear Wave Elastography. J. Clin. Med. 2021, 10, 2480. https://doi.org/10.3390/jcm10112480
Olchowy C, Grzech-Leśniak K, Hadzik J, Olchowy A, Łasecki M. Monitoring of Changes in Masticatory Muscle Stiffness after Gum Chewing Using Shear Wave Elastography. Journal of Clinical Medicine. 2021; 10(11):2480. https://doi.org/10.3390/jcm10112480
Chicago/Turabian StyleOlchowy, Cyprian, Kinga Grzech-Leśniak, Jakub Hadzik, Anna Olchowy, and Mateusz Łasecki. 2021. "Monitoring of Changes in Masticatory Muscle Stiffness after Gum Chewing Using Shear Wave Elastography" Journal of Clinical Medicine 10, no. 11: 2480. https://doi.org/10.3390/jcm10112480
APA StyleOlchowy, C., Grzech-Leśniak, K., Hadzik, J., Olchowy, A., & Łasecki, M. (2021). Monitoring of Changes in Masticatory Muscle Stiffness after Gum Chewing Using Shear Wave Elastography. Journal of Clinical Medicine, 10(11), 2480. https://doi.org/10.3390/jcm10112480







