Incidence, Risk, and Visual Outcomes after Repositioning of Acute Non-Traumatic Flap Dislocations Following Femtosecond-Assisted LASIK
Abstract
1. Introduction
2. Patients and Methods
2.1. LASIK Technique
2.2. Flap Repositioning Technique
2.3. Data Collection
3. Results
3.1. Incidence of Flap Repositioning Secondary to Acute Flap Dislocation and Striae
3.2. Preoperative and Intraoperative Characteristics of Patients Requiring Flap Repositioning
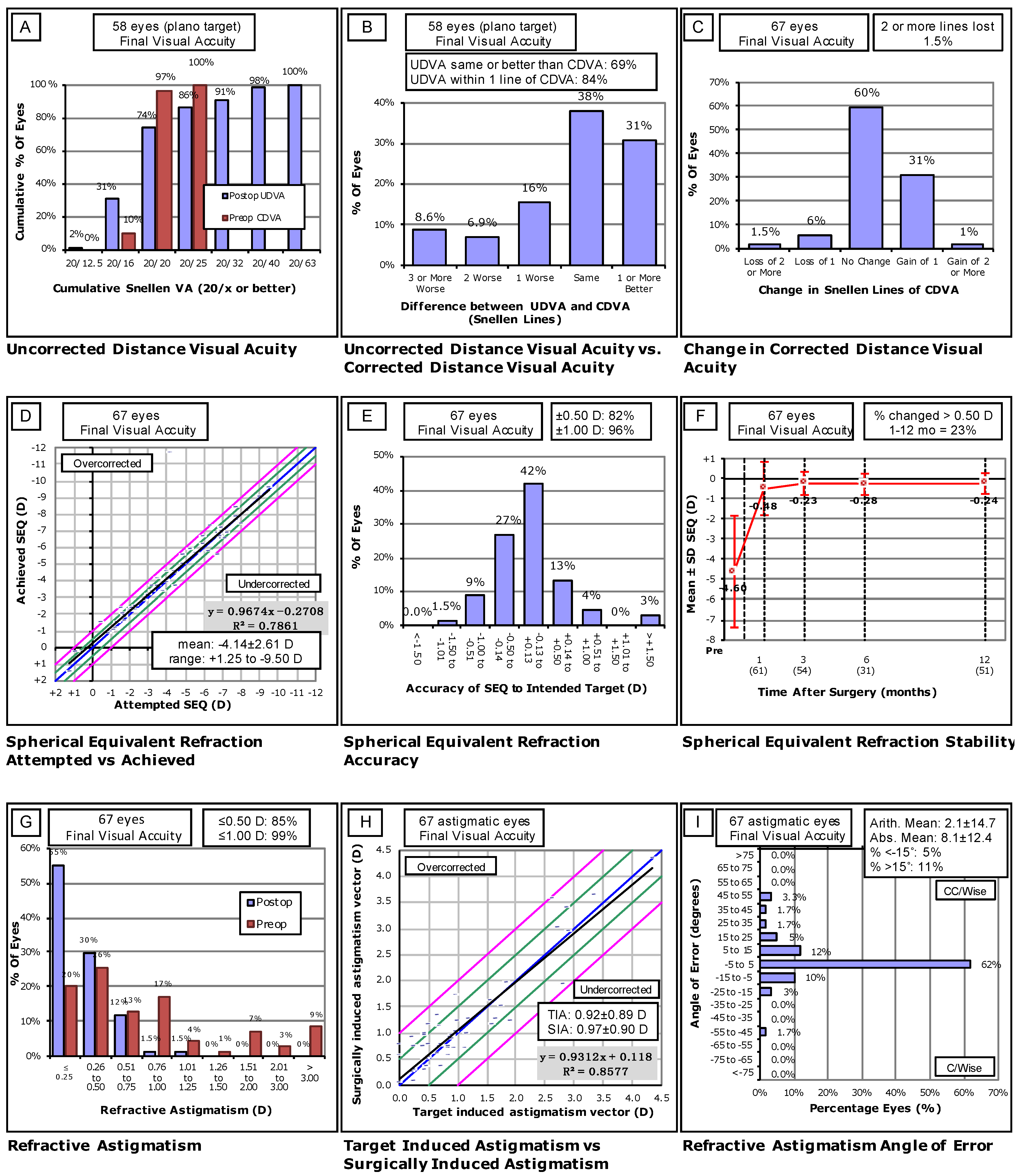
3.3. Visual Outcomes of Flap Repositioning Patients
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Segev, F.; Mimouni, M.; Sela, T.; Munzer, G.; Kaiserman, I. Risk factors for sporadic diffuse lamellar keratitis after microkeratome laser-assisted in situ keratomileusis: A retrospective large database analysis. Cornea 2018, 37, 1124–1129. [Google Scholar] [CrossRef]
- Wallerstein, A.; Gauvin, M.; Adiguzel, E.; Singh, H.; Gupta, V.; Harissi-Dagher, M.; Cohen, M. Clinically significant laser in situ keratomileusis flap striae. J. Cataract Refract. Surg. 2017, 43, 1523–1533. [Google Scholar] [CrossRef]
- Farjo, A.A.; Sugar, A.; Schallhorn, S.C.; Majmudar, P.A.; Tanzer, D.J.; Trattler, W.B.; Cason, J.B.; Donaldson, K.E.; Kymionis, G.D. Femtosecond lasers for LASIK flap creation: A report by the American academy of ophthalmology. Ophthalmology 2013, 120, e5–e20. [Google Scholar] [CrossRef]
- Moshirfar, M.; Gardiner, J.P.; Schliesser, J.A.; Espandar, L.; Feiz, V.; Mifflin, M.D.; Chang, J.C. Laser in situ keratomileusis flap complications using mechanical microkeratome versus femtosecond laser: Retrospective comparison. J. Cataract Refract. Surg. 2010, 36, 1925–1933. [Google Scholar] [CrossRef]
- Clare, G.; Moore, T.C.B.; Grills, C.; Leccisotti, A.; Moore, J.E.; Schallhorn, S. Early flap displacement after LASIK. Ophthalmology 2011, 118, 1760–1765. [Google Scholar] [CrossRef]
- Galvis, V.; Tello, A.; Guerra, A.R.; Rey, J.J.; Camacho, P.A. Risk factors and visual results in cases of LASIK flap repositioning due to folds or dislocation: Case series and literature review. Int. Ophthalmol. 2014, 34, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Mimouni, M.; Vainer, I.; Assad, N.; Nemet, A.; Sela, T.; Munzer, G.; Kaiserman, I. Incidence, indications, and outcomes of eyes needing early flap lifting after LASIK. Cornea 2018, 37, 1118–1123. [Google Scholar] [CrossRef]
- Chang, J.S.M. Complications of sub-Bowman’s keratomileusis with a femtosecond laser in 3009 eyes. J. Refract. Surg. 2008, 24, S97–S101. [Google Scholar] [CrossRef]
- Kamburoǧlu, G.; Ertan, A. Epithelial ingrowth after femtosecond laser-assisted in situ keratomileusis. Cornea 2008, 27, 1122–1125. [Google Scholar] [CrossRef]
- Kezirian, G.M.; Moore, C.R.; Stonecipher, K.G.; Brint, S.I.; Abell, T.; Arrowsmith, P.; Binder, P.; Bond, W.; Chotiner, B.; Dulaney, D.D.; et al. Four-year postoperative results of the US ALLEGRETTO WAVE clinical trial for the treatment of hyperopia. J. Refract. Surg. 2008, 24, S431–S438. [Google Scholar] [CrossRef]
- Letko, E.; Price, M.O.; Price, F.W. Influence of original flap creation method on incidence of epithelial ingrowth after LASIK retreatment. J. Refract. Surg. 2009, 25, 1039–1041. [Google Scholar] [CrossRef] [PubMed]
- Sutton, G.; Hodge, C. Accuracy and precision of LASIK flap thickness using the intralase femtosecond laser in 1000 consecutive cases. J. Refract. Surg. 2008, 24, 802–806. [Google Scholar] [CrossRef] [PubMed]
- Reinstein, D.Z.; Carp, G.I.; Archer, T.J.; Buick, T.; Gobbe, M.; Rowe, E.L.; Jukic, M.; Brandon, E.; Moore, J.; Moore, T. LASIK for the correction of high hyperopic astigmatism with epithelial thickness monitoring. J. Refract. Surg. 2017, 33, 314–321. [Google Scholar] [CrossRef]
- Friehmann, A.; Mimouni, M.; Nemet, A.Y.; Sela, T.; Munzer, G.; Kaiserman, I. Risk Factors for Epithelial Ingrowth Following Microkeratome-Assisted LASIK. J. Refract. Surg. 2018, 34, 100–105. [Google Scholar] [CrossRef]
- Luger, M.H.A.; Ewering, T.; Arba-Mosquera, S. Influence of patient age on high myopic correction in corneal laser refractive surgery. J. Cataract Refract. Surg. 2013, 39, 204–210. [Google Scholar] [CrossRef] [PubMed]
- Mimouni, M.; Flores, V.; Sela, T.; Kaiserman, I. Risk Factors for Re-treatment Following Hyperopic LASIK. J. Refract Surg. 2018, 5, 316–320. [Google Scholar] [CrossRef] [PubMed]
- Ghanem, R.C.; de la Cruz, J.; Tobaigy, F.M.; Ang, L.P.K.; Azar, D.T. LASIK in the Presbyopic Age Group. Safety, Efficacy, and Predictability in 40- to 69-Year-Old Patients. Ophthalmology 2007, 114, 1303–1310. [Google Scholar] [CrossRef]
- Taurone, S.; Miglietta, S.; Spoletini, M.; Feher, J.; Artico, M.; Papa, V.; Matassa, R.; Familiari, G.; Gobbi, P.; Micera, A. Age related changes seen in human cornea in formalin fixed sections and on biomicroscopy in living subjects: A comparison. Clin. Anat. 2020, 33, 245–256. [Google Scholar] [CrossRef]
- Gambato, C.; Longhin, E.; Catania, A.G.; Lazzarini, D.; Parrozzani, R.; Midena, E. Aging and corneal layers: An in vivo corneal confocal microscopy study. Graefe’s Arch. Clin. Exp. Ophthalmol. 2015, 253, 267–275. [Google Scholar] [CrossRef]
- Zheng, T.; Le, Q.; Hong, J.; Xu, J. Comparison of human corneal cell density by age and corneal location: An in vivo confocal microscopy study. BMC Ophthalmol. 2016, 16. [Google Scholar] [CrossRef]
- Cartwright, N.E.K.; Tyrer, J.R.; Marshall, J. Age-related differences in the elasticity of the human cornea. Investig. Ophthalmol. Vis. Sci. 2011, 52, 4324–4329. [Google Scholar] [CrossRef]
- Elsheikh, A.; Wang, D.; Brown, M.; Rama, P.; Campanelli, M.; Pye, D. Assessment of corneal biomechanical properties and their variation with age. Curr. Eye Res. 2007, 32, 11–19. [Google Scholar] [CrossRef]
- Leung, T.; Zhou, Y.; French, H.M.; Lin, M.C. Increased corneal epithelial permeability after overnight sleep. Investig. Ophthalmol. Vis. Sci. 2014, 55, 5718–5722. [Google Scholar] [CrossRef][Green Version]
- Hernandez-Zimbron, L.F.; Gulias-Cañizo, R.; Golzarri, M.F.; Martínez-Baéz, B.E.; Quiroz-Mercado, H.; Gonzalez-Salinas, R. Molecular Age-Related Changes in the Anterior Segment of the Eye. J. Ophthalmol. 2017, 2017, 1295132. [Google Scholar] [CrossRef] [PubMed]
- Chang, S.W.; Hu, F.R. Changes in corneal autofluorescence and corneal epithelial barrier function with aging. Cornea 1993, 12, 493–499. [Google Scholar] [CrossRef] [PubMed]
- Whitcomb, E.A.; Shang, F.; Taylor, A. Common cell biologic and biochemical changes in aging and age-related diseases of the eye: Toward new therapeutic approaches to age-related ocular diseases. Investig. Ophthalmol. Vis. Sci. 2013, 54. [Google Scholar] [CrossRef]
- Arita, R.; Itoh, K.; Inoue, K.; Amano, S. Noncontact Infrared Meibography to Document Age-Related Changes of the Meibomian Glands in a Normal Population. Ophthalmology 2008, 115, 911–915. [Google Scholar] [CrossRef] [PubMed]
- Qiu, X.; Gong, L.; Sun, X.; Jin, H. Age-related variations of human tear meniscus and diagnosis of dry eye with fourier-domain anterior segment optical coherence tomography. Cornea 2011, 30, 543–549. [Google Scholar] [CrossRef] [PubMed]
- Shehadeh-Mashor, R.; Mimouni, M.; Shapira, Y.; Sela, T.; Munzer, G.; Kaiserman, I. Risk Factors for Dry Eye after Refractive Surgery. Cornea 2019, 38, 1495–1499. [Google Scholar] [CrossRef] [PubMed]
- Stapleton, F.; Alves, M.; Bunya, V.Y.; Jalbert, I.; Lekhanont, K.; Malet, F.; Na, K.S.; Schaumberg, D.; Uchino, M.; Vehof, J.; et al. TFOS DEWS II Epidemiology Report. Ocul. Surf. 2017, 15, 334–365. [Google Scholar] [CrossRef]
- Salomão, M.Q.; Ambrósio, R.; Wilson, S.E. Dry eye associated with laser in situ keratomileusis: Mechanical microkeratome versus femtosecond laser. J. Cataract Refract. Surg. 2009, 35, 1756–1760. [Google Scholar] [CrossRef]
- Morgan, S.R.; Dooley, E.P.; Kamma-Lorger, C.; Funderburgh, J.L.; Funderburgh, M.L.; Meek, K.M. Early wound healing of laser in situ keratomileusis-like flaps after treatment with human corneal stromal stem cells. J. Cataract Refract. Surg. 2016, 42, 302–309. [Google Scholar] [CrossRef][Green Version]
- Netto, M.V.; Mohan, R.R.; Ambrósio, R.; Hutcheon, A.E.K.; Zieske, J.D.; Wilson, S.E. Wound healing in the cornea: A review of refractive surgery complications and new prospects for therapy. Cornea 2005, 24, 509–522. [Google Scholar] [CrossRef]
- Salomao, M.Q.; Wilson, S.E. Corneal molecular and cellular biology update for the refractive surgeon. J. Refract. Surg. 2009, 25, 459–466. [Google Scholar] [CrossRef]
- Wilson, S.E. Biology of keratorefractive surgery-PRK, PTK, LASIK, SMILE, inlays and other refractive procedures. Exp. Eye Res. 2020, 198. [Google Scholar] [CrossRef]
- Solomon, R.; Donnenfeld, E.D.; Perry, H.D.; Nirankari, V.S. Post-LASIK corneal flap displacement following penetrating keratoplasty for bullous keratopathy. Cornea 2005, 24, 874–878. [Google Scholar] [CrossRef]
- Laurent, J.M.; Schallhorn, S.C.; Spigelmire, J.R.; Tanzer, D.J. Stability of the laser in situ keratomileusis corneal flap in rabbit eyes. J. Cataract Refract. Surg. 2006, 32, 1046–1051. [Google Scholar] [CrossRef]
- Perez, E.P.; Viramontes, B.; Schor, P.; Miller, D. Factors affecting corneal strip stroma-to-stroma adhesion. J. Refract. Surg. 1998, 14, 460–462. [Google Scholar] [CrossRef] [PubMed]
- Nowroozzadeh, M.H. Early flap dislocation with perioperative brimonidine use in laser in situ keratomileusis. J. Cataract Refract. Surg. 2010, 36, 368. [Google Scholar] [CrossRef]
- Muñoz, G.; Albarrán-Diego, C.; Sakla, H.F.; Javaloy, J. Increased risk for flap dislocation with perioperative brimonidine use in femtosecond laser in situ keratomileusis. J. Cataract Refract. Surg. 2009, 35, 1338–1342. [Google Scholar] [CrossRef]
- Bolívar, G.; Teus, M.A.; Hernández-Verdejo, J.L. Short-term effect of topical brimonidine tartrate on intrastromal corneal pressure in rabbits. J. Refract. Surg. 2010, 26, 533–535. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Chen, J.; Fu, Y.; Fan, X. The signaling pathway involved in the proliferation of corneal endothelial cells. J. Recept. Signal Transduct. 2015, 35, 585–591. [Google Scholar] [CrossRef]
| Demographic/Risk Factor | Median (IQR) | Range |
|---|---|---|
| Age (Years) | 35 (14) | 20–61 |
| n (eyes) | % | |
| Requiring Repositioning Following First LASIK | 68 | 97.10% |
| Requiring Repositioning Following Enhancement | 2 | 2.90% |
| Gender (Male/Female) | 31/39 | 44.3%/55.7% |
| Affected Eye | ||
| OD Only | 28 | 40% |
| OS Only | 38 | 54.30% |
| OU | 4 | 5.70% |
| Refractive Error | ||
| Simple Myopia | 8 | 11.40% |
| Simple Hyperopia | 0 | 0.00% |
| Compound Myopic Astigmatism | 60 | 85.70% |
| Compound Hyperopic Astigmatism | 2 | 2.80% |
| Indications for Repositioning | ||
| Flap Dislocation | 25 | 35.70% |
| Striae | 45 | 64.30% |
| Postoperative Days to Repositioning | ||
| 1 Day | 64 | 91.40% |
| 2–7 Days | 1 | 1.40% |
| 8–14 Days | 5 | 7.10% |
| Repositioning Group (n = 70) | Control Cohort (n = 14,418) | ||||
|---|---|---|---|---|---|
| Variable | Mean ± SD | Range | Mean ± SD | Range | p-Value |
| Age | 35 ± 8.50 | 20, 61 | 32 ± 9.93 | 17, 85 | 0.001 |
| Keratometry | |||||
| Kf | 43.35 ± 1.58 | 37.6, 47.5 | 43.281 ± 1.51 | 31.2, 46.9 | 0.6926 |
| Ks | 44.54 ± 1.70 | 38.7, 48.1 | 44.5 ± 1.61 | 31.9, 49.0 | 0.8147 |
| Km | 43.94 ± 1.56 | 38.1, 47.7 | 43.89 ± 1.50 | 31.55, 47.8 | 0.8045 |
| Manifest Refraction | |||||
| Sphere (D) | −4.11 ± 2.68 | −10.0, +3.00 | −3.03 ± 2.21 | −12.0, +6.25 | <0.001 |
| Cylinder (D) | −1.00 ± 1.02 | −4.50, 0 | −0.93 ± 0.96 | −7.50, +2.25 | 0.4822 |
| Spherical Equivalent (D) | −4.62 ± 2.72 | −12.1, +0.88 | −3.49 ± 2.15 | −13.2, +4.38 | <0.001 |
| n | Percent | n | Percent | p-value | |
| Gender | 31/39 | 44.3%/55.7% | 7440/6978 | 51.6%/48.4% | 0.27 |
| Refractive Error | 0.696 | ||||
| Simple Myopia | 8 | 11.40% | 2081 | [14.5%] | |
| Simple Hyperopia | 0 | 0.00% | 47 | [0.3%] | |
| Compound Myopic | 60 | 85.70% | 11,594 | [80.6%] | |
| Astigmatism | |||||
| Compound Hyperopic | 2 | 2.80% | 659 | [4.6%] | |
| Astigmatism | |||||
| Laser | 0.615 | ||||
| AMO iFS | 59 | [84.3%] | 12,014 | [83.5%] | |
| WL FS200 | 5 | [7.1%] | 843 | [5.9%] | |
| Zeiss VisuMax | 6 | [8.6%] | 1524 | [10.6%] | |
| Surgeon | 0.728 | ||||
| A | 59 | [84.3%] | 11,716 | [81.5%] | |
| B | 6 | [8.6%] | 1221 | [8.5%] | |
| C | 4 | [5.7%] | 794 | [5.5%] | |
| D | 1 | [1.4%] | 650 | [4.5%] | |
| Sphere (D) | Eyes (n) | % Requiring | Flap | Odds Ratio | 95% CI | p-Value | |
|---|---|---|---|---|---|---|---|
| Reposition | Reposition (n) | ||||||
| Age | |||||||
| ≤29 * | 4657 | 0.43% | 20 | - | - | - | |
| 30–39 | 6147 | 0.41% | 24 | 0.9 | 0.49–1.64 | 0.717 | |
| 40–49 | 2297 | 0.61% | 14 | 1.4 | 0.69–2.76 | 0.336 | |
| ≥50 | 638 | 1.41% | 9 | 3.69 | 1.57–7.93 | 0.001 | |
| Myopia Severity | |||||||
| Mild * | −0.50 to −1.50 | 3026 | 0.465 | 14 | - | - | - |
| Moderate | −1.5 to −6.00 | 8828 | 0.34% | 30 | 0.74 | 0.39–1.45 | 0.365 |
| Severe | ≥−6.00 | 1677 | 1.37% | 23 | 3.04 | 1.56–6.14 | 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moshirfar, M.; West, D.G.; Miller, C.M.; West, W.B., Jr.; McCabe, S.E.; Shmunes, K.M.; Baker, P.A.; Ronquillo, Y.C.; Hoopes, P.C. Incidence, Risk, and Visual Outcomes after Repositioning of Acute Non-Traumatic Flap Dislocations Following Femtosecond-Assisted LASIK. J. Clin. Med. 2021, 10, 2478. https://doi.org/10.3390/jcm10112478
Moshirfar M, West DG, Miller CM, West WB Jr., McCabe SE, Shmunes KM, Baker PA, Ronquillo YC, Hoopes PC. Incidence, Risk, and Visual Outcomes after Repositioning of Acute Non-Traumatic Flap Dislocations Following Femtosecond-Assisted LASIK. Journal of Clinical Medicine. 2021; 10(11):2478. https://doi.org/10.3390/jcm10112478
Chicago/Turabian StyleMoshirfar, Majid, David G. West, Chase M Miller, William B. West, Jr., Shannon E. McCabe, Kathryn M. Shmunes, Preston A. Baker, Yasmyne C. Ronquillo, and Phillip C. Hoopes. 2021. "Incidence, Risk, and Visual Outcomes after Repositioning of Acute Non-Traumatic Flap Dislocations Following Femtosecond-Assisted LASIK" Journal of Clinical Medicine 10, no. 11: 2478. https://doi.org/10.3390/jcm10112478
APA StyleMoshirfar, M., West, D. G., Miller, C. M., West, W. B., Jr., McCabe, S. E., Shmunes, K. M., Baker, P. A., Ronquillo, Y. C., & Hoopes, P. C. (2021). Incidence, Risk, and Visual Outcomes after Repositioning of Acute Non-Traumatic Flap Dislocations Following Femtosecond-Assisted LASIK. Journal of Clinical Medicine, 10(11), 2478. https://doi.org/10.3390/jcm10112478







