Red Blood Cell Transfusion in the Emergency Department: An Observational Cross-Sectional Multicenter Study
Abstract
1. Introduction
2. Methods
2.1. Objectives
2.2. Study Design, Settings, and Participants
2.3. Analysis
2.4. Ethical Aproval
3. Results
3.1. General Characteristics, Reasons for ED Referral, and Physical Examination
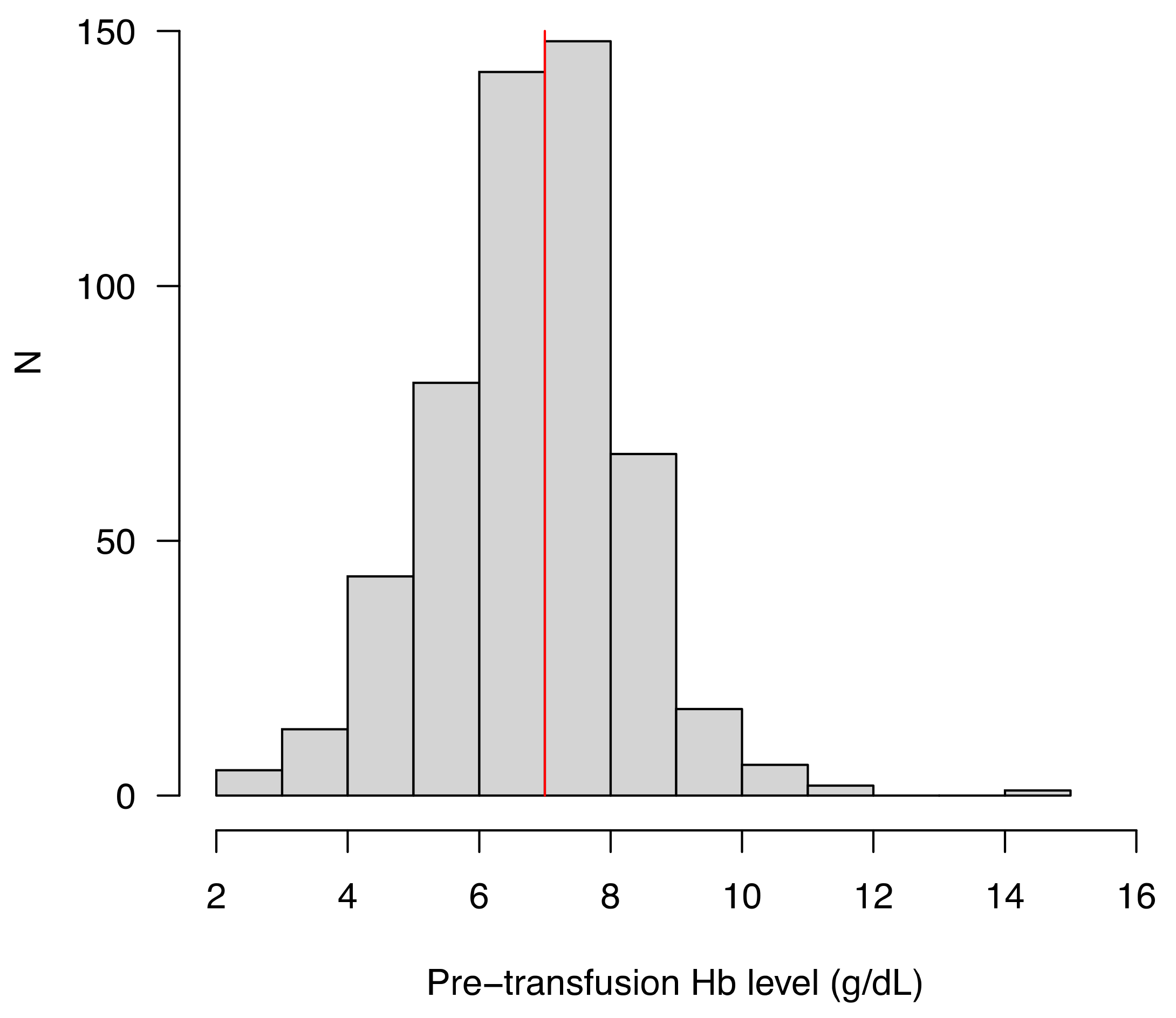
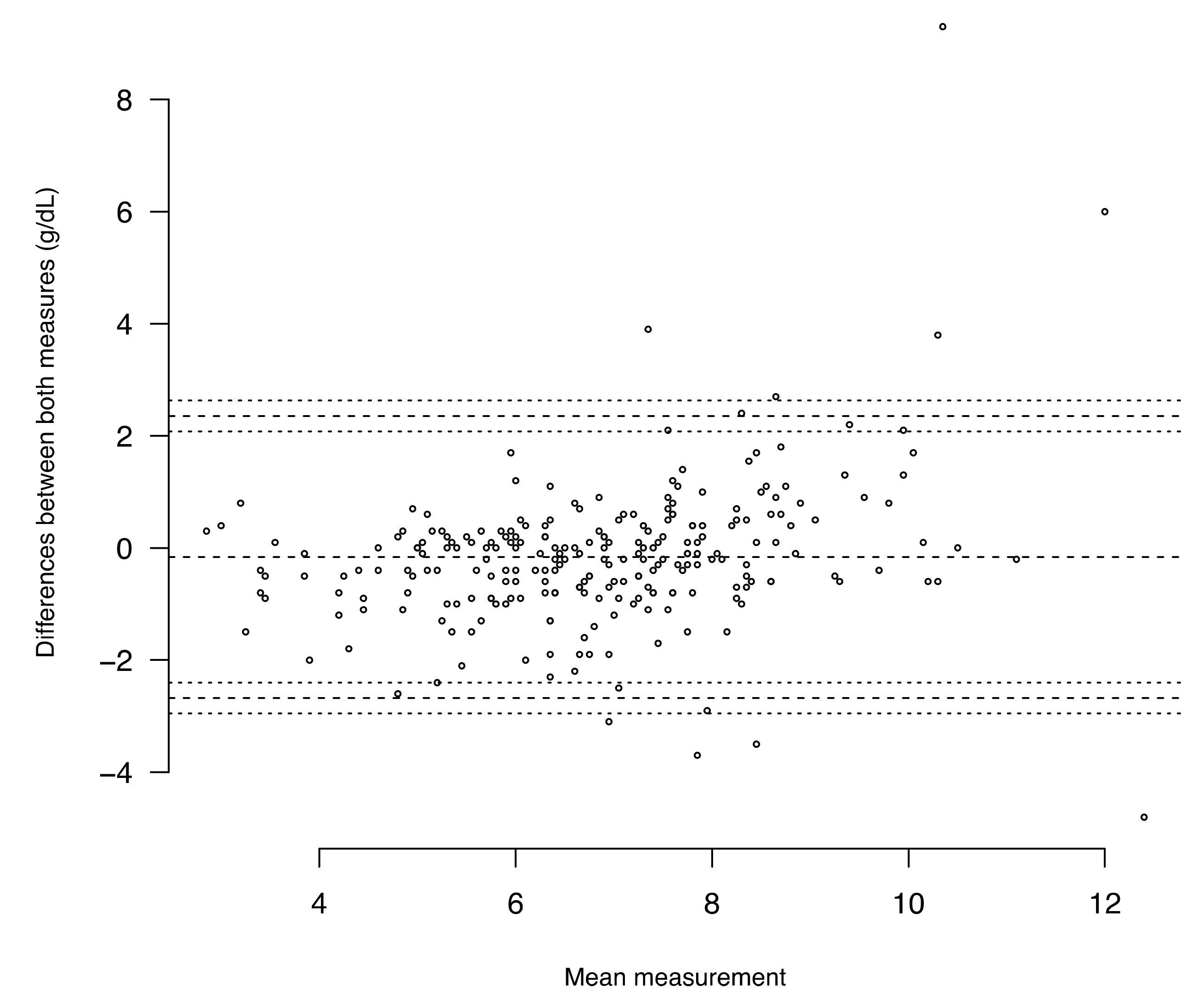
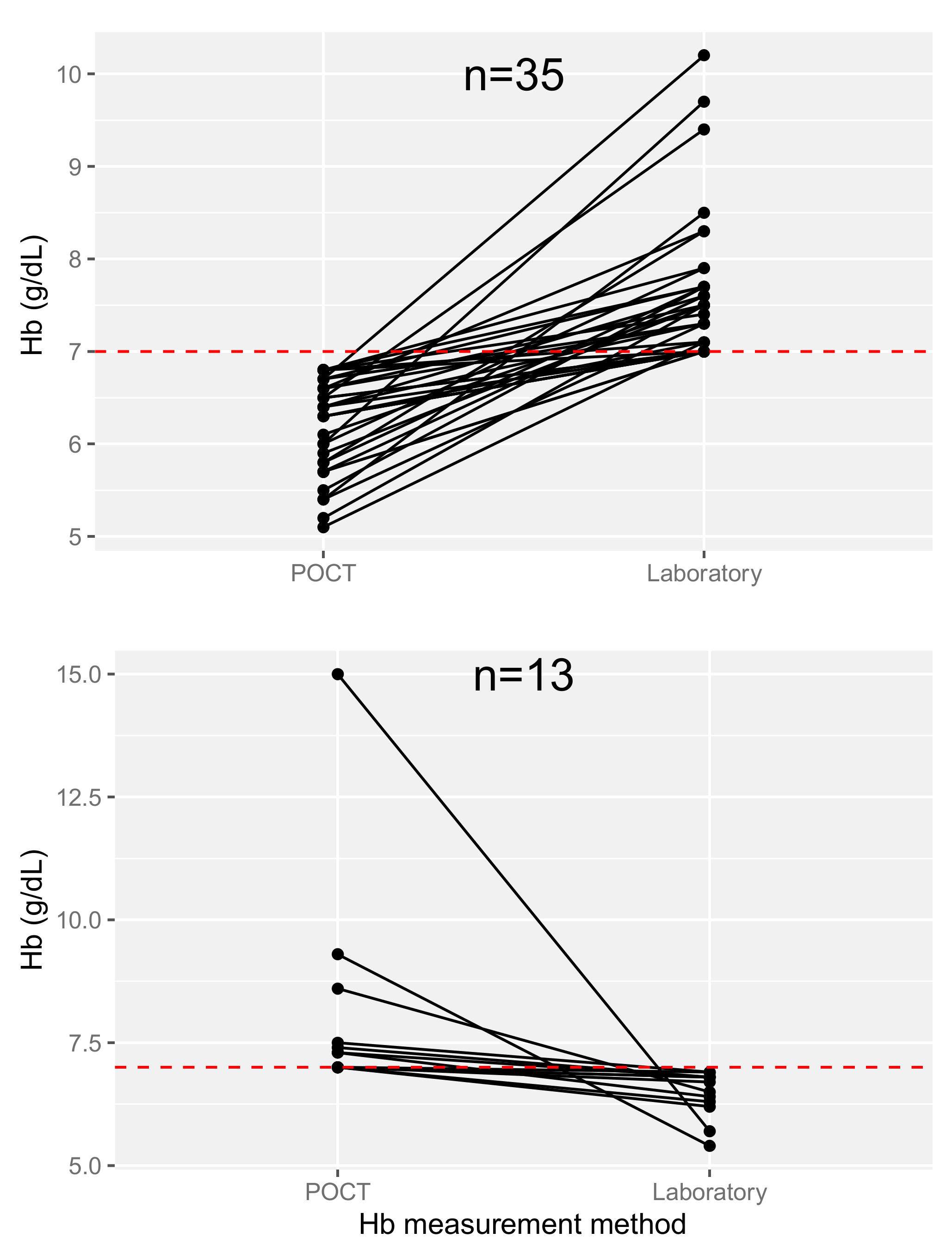
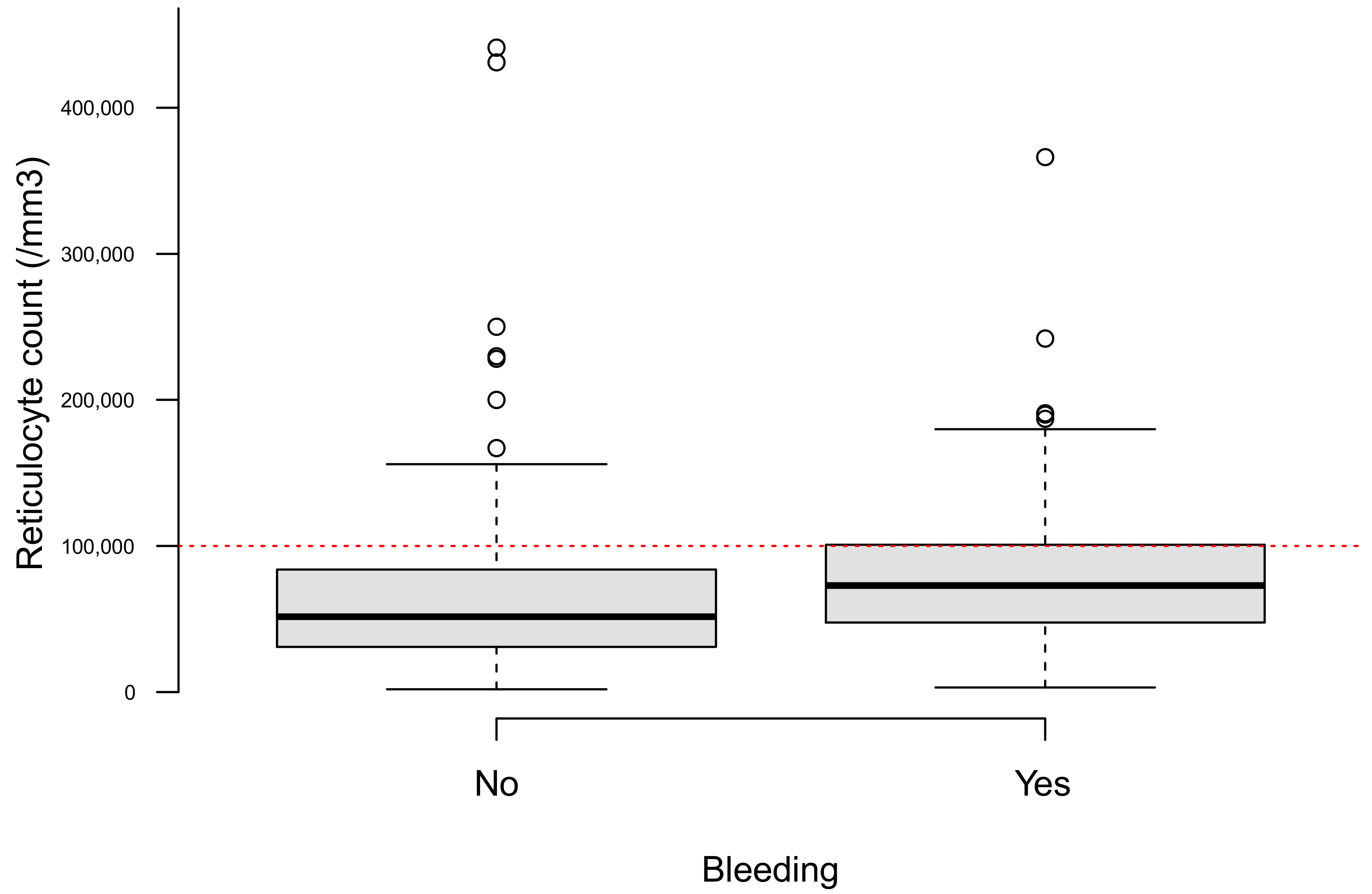
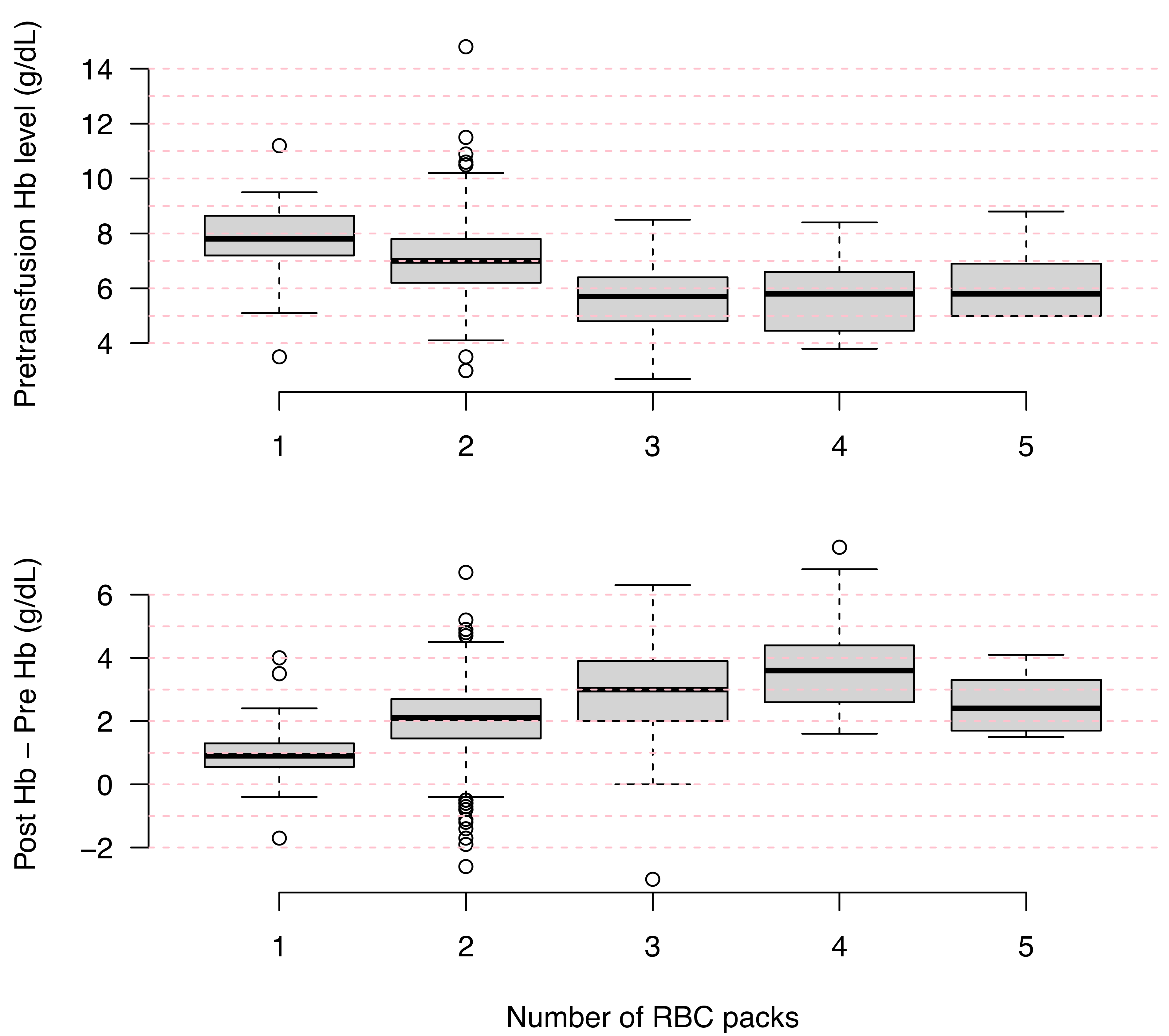
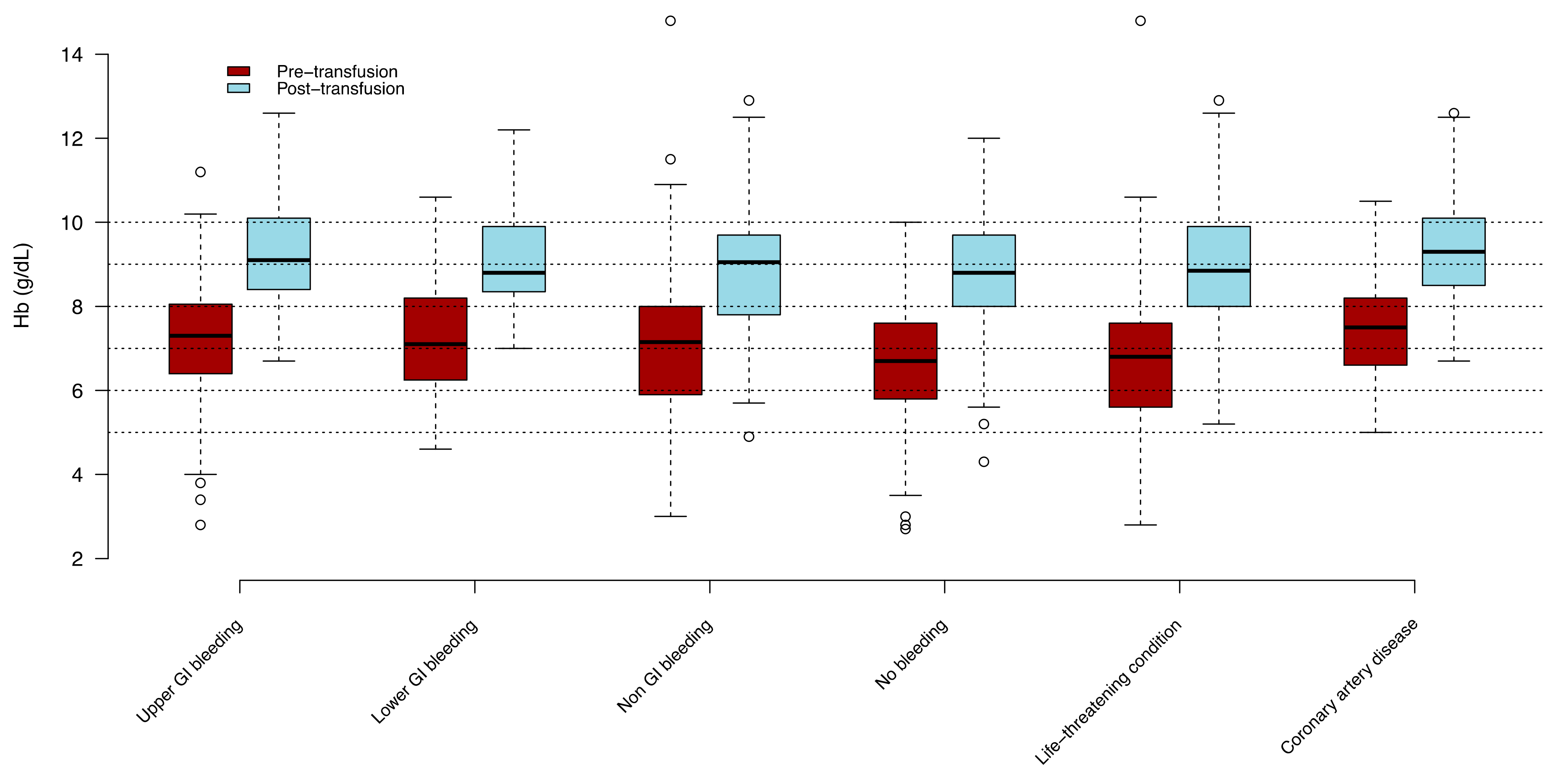
3.2. Transfusion
3.3. Adverse Events
3.4. Outcomes
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hillenkamp, J.Z.; Wolfson, A.B. Liberal vs Restrictive Hemoglobin Levels as Thresholds for Blood Transfusions. Acad. Emerg. Med. 2021, 28, 593–594. [Google Scholar] [CrossRef] [PubMed]
- Haute Autorité de Santé. Transfusion de Globules Rouges Homologues: Produits, Indications Alternatives. Rapport d’activité de l’hémovigilance 2018. 2014. Available online: https://ansm.sante.fr/var/ansm_site/storage/original/application/94eaed87fcb1d3c9d2187f4945256875.pdf (accessed on 1 November 2020).
- Mueller, M.M.; Van Remoortel, H.; Meybohm, P.; Aranko, K.; Aubron, C.; Burger, R.; Carson, J.L.; Cichutek, K.; De Buck, E.; Devine, D.; et al. Patient Blood Management: Recommendations From the 2018 Frankfurt Consensus Conference. JAMA 2019, 321, 983–997. [Google Scholar] [CrossRef] [PubMed]
- Thiebaud, P.C.; Yordanov, Y.; Galimard, J.E.; Raynal, P.A.; Beaune, S.; Jacquin, L.; Ageron, F.X.; Pateron, D.; Initiatives de Recherche aux Urgences Group. Management of upper gastrointestinal bleeding in emergency departments, from bleeding symptoms to diagnosis: A prospective, multicenter, observational study. Scand J. Trauma Resusc. Emerg. Med. 2017, 25, 78. [Google Scholar] [CrossRef] [PubMed]
- Thiebaud, P.C.; Yordanov, Y.; Galimard, J.E.; Naouri, D.; Brigant, F.; Truchot, J.; Moustafa, F.; Pateron, D.; aux Urgences, T.I. Suspected lower gastrointestinal bleeding in emergency departments, from bleeding symptoms to diagnosis. Am. J. Emerg. Med. 2019, 37, 772–774. [Google Scholar] [CrossRef]
- Vincent, J.L.; Baron, J.F.; Reinhart, K.; Gattinoni, L.; Thijs, L.; Webb, A.; Meier-Hellmann, A.; Nollet, G.; Peres-Bota, D.; ABC (Anemia and Blood Transfusion in Critical Care) Investigators. Anemia and blood transfusion in critically ill patients. JAMA 2002, 288, 1499–1507. [Google Scholar] [CrossRef]
- Cable, C.A.; Razavi, S.A.; Roback, J.D.; Murphy, D.J. RBC Transfusion Strategies in the ICU: A Concise Review. Crit. Care Med. 2019, 47, 1637–1644. [Google Scholar] [CrossRef] [PubMed]
- Villanueva, C.; Colomo, A.; Bosch, A.; Concepción, M.; Hernandez-Gea, V.; Aracil, C.; Graupera, I.; Poca, M.; Alvarez-Urturi, C.; Gordillo, J.; et al. Transfusion strategies for acute upper gastrointestinal bleeding. N. Engl. J. Med. 2013, 368, 11–21. [Google Scholar] [CrossRef]
- Jairath, V.; Kahan, B.C.; Gray, A.; Doré, C.J.; Mora, A.; James, M.W.; Stanley, A.J.; Everett, S.M.; Bailey, A.A.; Dallal, H.; et al. Restrictive versus liberal blood transfusion for acute upper gastrointestinal bleeding (TRIGGER): A pragmatic, open-label, cluster randomised feasibility trial. Lancet 2015, 386, 137–144. [Google Scholar] [CrossRef]
- Maher, P.J.; Khan, S.; Karim, R.; Richardson, L.D. Determinants of empiric transfusion in gastrointestinal bleeding in the emergency department. Am. J. Emerg. Med. 2020, 38, 962–965. [Google Scholar] [CrossRef]
- Ley, E.J.; Liou, D.Z.; Singer, M.B.; Mirocha, J.; Melo, N.; Chung, R.; Bukur, M.; Salim, A. Emergency department blood transfusion: The first two units are free. J. Surg. Res. 2013, 184, 546–550. [Google Scholar] [CrossRef]
- Langlais, M.L.; Dargère, M.; Le Niger, C.; Goetghebeur, D. Pertinence des prescriptions de concentrés de globules rouges par le médecin urgentiste avant et après la mise en place d’un protocole [Appropriate use of red blood cell transfusion in the emergency department before and after a specific protocol]. Transfus. Clin. Biol. 2019, 26, 38–47. [Google Scholar] [CrossRef]
- Beckwith, H.; Manson, L.; McFarlane, C.; Reed, M.J. A review of blood product usage in a large emergency department over a one-year period. Emerg. Med. J. 2010, 27, 439–442. [Google Scholar] [CrossRef] [PubMed]
- Díaz, M.Q.; Borobia, A.M.; Erce, J.A.; Maroun-Eid, C.; Fabra, S.; Carcas, A.; Frías, J.; Muñoz, M. USEES-URG Research Group. Appropriate use of red blood cell transfusion in emergency departments: A study in five emergency departments. Blood Transfus. 2017, 15, 199–206. [Google Scholar]
- Beyer, A.; Rees, R.; Palmer, C.; Wessman, B.T.; Fuller, B.M. Blood product transfusion in emergency department patients: A case-control study of practice patterns and impact on outcome. Int. J. Emerg. Med. 2017, 10, 5. [Google Scholar] [CrossRef] [PubMed]
- Reed, M.J.; Kelly, S.L.; Beckwith, H.; Innes, C.J.; Manson, L. Successful implementation of strategies to transform Emergency Department transfusion practice. BMJ Qual. Improv. Rep. 2013, 2, u201055.w690. [Google Scholar] [CrossRef]
- Quintana-Díaz, M.; Andrés-Esteban, E.M.; Sánchez-Serrano, J.; Martínez-Virto, A.; Juárez-Vela, R.; García-Erce, J.A. Transfusions in the Emergency department: More than a blood transfusion. Rev. Clin. Esp. 2020, 220, 393–399. [Google Scholar] [CrossRef]
- Barr, P.J.; Donnelly, M.; Cardwell, C.R.; Parker, M.; Morris, K.; Bailie, K.E. The appropriateness of red blood cell use and the extent of overtransfusion: Right decision? Right amount? Transfusion 2011, 51, 1684–1694. [Google Scholar] [CrossRef]
- Alavi-Moghaddam, M.; Bardeh, M.; Alimohammadi, H.; Emami, H.; Hosseini-Zijoud, S.M. Blood Transfusion Practice before and after Implementation of Type and Screen Protocol in Emergency Department of a University Affiliated Hospital in Iran. Emerg. Med. Int. 2014, 2014, 316463. [Google Scholar] [CrossRef] [PubMed]
- Peyrony, O.; Fontaine, J.P.; Beaune, S.; Khoury, A.; Truchot, J.; Balen, F.; Vally, R.; Schmitt, J.; Ben Hammouda, K.; Roussel, M.; et al. EPICANCER-Cancer Patients Presenting to the Emergency Departments in France: A Prospective Nationwide Study. J. Clin. Med. 2020, 9, 1505. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Kim, D.H.; Kim, K.; Rhee, J.E.; Kim, T.Y.; Jo, Y.H.; Lee, J.H.; Suh, G.J.; Hwang, S.S.; Lee, C.C.; et al. Predicting change of hemoglobin after transfusion in hemodynamically stable anemic patients in emergency department. J. Trauma. 2010, 68, 337–341. [Google Scholar] [CrossRef]
- Moretti, K.; Marqués, C.G.; Garbern, S.; Mbanjumucyo, G.; Uwamahoro, C.; Beaudoin, F.L.; Amanullah, S.; Gjelsvik, A.; Aluisio, A.R. Transfusion, mortality and hemoglobin level: Associations among emergency department patients in Kigali, Rwanda. Afr. J. Emerg. Med. 2020, 10, 68–73. [Google Scholar] [CrossRef] [PubMed]
- Long, B.; Koyfman, A. Red Blood Cell Transfusion in the Emergency Department. J. Emerg. Med. 2016, 51, 120–130. [Google Scholar] [CrossRef] [PubMed]
- Osborn, Z.T.; Villalba, N.; Derickson, P.R.; Sewatsky, T.P.; Wager, A.P.; Freeman, K. Accuracy of Point-of-Care Testing for Anemia in the Emergency Department. Respir. Care 2019, 64, 1343–1350. [Google Scholar] [CrossRef] [PubMed]
- Van de Louw, A.; Lasserre, N.; Drouhin, F.; Thierry, S.; Lecuyer, L.; Caen, D.; Tenaillon, A. Reliability of HemoCue in patients with gastrointestinal bleeding. Intensive Care Med. 2007, 33, 355–358. [Google Scholar] [CrossRef]
- Dolscheid-Pommerich, R.C.; Dolscheid, S.; Grigutsch, D.; Stoffel-Wagner, B.; Graeff, I. Comparability of Point-of-Care versus Central Laboratory Hemoglobin Determination in Emergency Patients at a Supra-Maximal Care Hospital. PLoS ONE 2016, 11, e0166521. [Google Scholar] [CrossRef]
- Critchley, L.A.; Critchley, J.A. A meta-analysis of studies using bias and precision statistics to compare cardiac output measurement techniques. J. Clin. Monit. Comput. 1999, 15, 85–91. [Google Scholar] [CrossRef]
| Variable | Missing Data | ||
|---|---|---|---|
| N | 529 | ||
| Female gender, n (%) | 277 | (52.4) | 0 |
| Age (years), median (IQR) | 74 | (59–85) | 0 |
| Night shift (6 p.m.–8 a.m.), n (%) | 185 | (35.4) | 6 |
| Medical history, n (%) | |||
| None | 72 | (13.7) | 4 |
| Hypertension | 235 | (44.8) | 4 |
| Coronary artery disease | 144 | (27.5) | 4 |
| Chronic heart failure | 74 | (14.1) | 3 |
| Chronic pulmonary disease | 55 | (10.4) | 2 |
| Renal insufficiency | 18 | (3.4) | 4 |
| Iron or vitamin deficiency | 97 | (18.3) | 0 |
| Solid malignancy | 109 | (20.7) | 3 |
| Hematological malignancy | 69 | (13.4) | 4 |
| Non-malignant hematological disease | 15 | (2.9) | 4 |
| Chemotherapy < 1 month, n (%) | 62 | (12.0) | 12 |
| Iterative transfusions n (%) | 73 | (14.1) | 13 |
| Bleeding risk, n (%) | |||
| Medication | 238 | (45.6) | 7 |
| Antiplatelet therapy | 135 | (25.9) | |
| Vitamin K antagonist | 48 | (9.2) | |
| Direct oral anticoagulant | 38 | (7.3) | |
| Heparin | 36 | (6.9) | |
| Non-steroidal anti-inflammatory drug | 8 | (1.5) | |
| Thrombopenia | 63 | (12.9) | 40 |
| Other * | 83 | (15.8) | 3 |
| Patient referred by, n (%) | 289 | (56.0) | 13 |
| General practitioner | 97 | (18.8) | |
| Laboratory | 72 | (14.0) | |
| Nursing home care institution | 50 | (9.7) | |
| Pre-hospital emergency service | 26 | (5.0) | |
| Specialist | 17 | (3.3) | |
| Other | 14 | (2.7) |
| Variables | Missing Data | ||
|---|---|---|---|
| N | 529 | ||
| Reasons for ED referral, n (%) | 0 | ||
| Anemia | 191 | (36.1) | 0 |
| Bleeding | 187 | (35.3) | 0 |
| Fatigue | 156 | (29.5) | 0 |
| Dizziness | 39 | (7.4) | 0 |
| Thoracic pain | 37 | (7.0) | 0 |
| Trauma | 32 | (6.0) | 0 |
| Neurological disorders | 18 | (3.4) | 0 |
| Physical examination, n (%) | |||
| Tachycardia (≥100/bpm) | 169 | (32.6) | 10 |
| Dyspnea | 101 | (19.3) | 6 |
| Shock | 57 | (10.9) | 4 |
| Altered mental status | 32 | (6.1) | 5 |
| Any bleeding observed in the ED, n (%) | 242 | (46.0) | 3 |
| Gastro-intestinal | 145 | (27.6) | 3 |
| Cutaneous | 29 | (5.5) | 3 |
| Mucosal * | 22 | (4.2) | 3 |
| Genitourinary | 21 | (4.0) | 3 |
| Urinary | 17 | (3.2) | 3 |
| Peritoneal | 3 | (0.6) | 3 |
| Hemoptysis * | 3 | (0.6) | 3 |
| Variable | Missing Data | ||
|---|---|---|---|
| N | 103 | ||
| Female gender, n (%) | 63 | (61.2) | 0 |
| Age (years), median (IQR) | 80 | (66–88) | 0 |
| Coronary artery disease, n (%) | 40 | (39.2) | 1 |
| Hypertension, n (%) | 52 | (51.0) | 1 |
| Chronic heart failure, n (%) | 22 | (21.6) | 1 |
| Chronic anemia, n (%) | 34 | (40.5) | 19 |
| Malignancy, n (%) | 36 | (35.6) | 2 |
| Hb POCT, median (IQR) | 7.5 | (6.5–9.0) | 46 |
| Tachycardia (≥100/bpm), n (%) | 32 | (32.0) | 3 |
| Life-threatening condition, n (%) | 8 | (31.1) | 0 |
| Any bleeding observed in the ED, n (%) | 8 | (50.5) | 0 |
| Pre-transfusion Hb level, median (IQR) | 7.8 | (6.9–8.6) | 1 |
| Number of RBC pack, n (%) | 3 | ||
| 1 | 10 | (10.0) | |
| 2 | 68 | (68.0) | |
| 3 | 9 | (9.0) | |
| 4 | 12 | (12.0) | |
| 5 | 1 | (1.0) | |
| Adverse event, n (%) | 1 | (1.0) | 0 |
| ICU during hospital stay, n (%) | 9 | (10.2) | 15 |
| Length of hospital stay, median (IQR) | 2 | (1–8) | 29 |
| Hospital death, n (%) | 1 | (1.1) | 15 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Peyrony, O.; Gamelon, D.; Brune, R.; Chauvin, A.; Ghazali, D.A.; Yordanov, Y.; Arsicaud, A.; Gilleron, P.; Curac, S.; Richard, M.-C.; et al. Red Blood Cell Transfusion in the Emergency Department: An Observational Cross-Sectional Multicenter Study. J. Clin. Med. 2021, 10, 2475. https://doi.org/10.3390/jcm10112475
Peyrony O, Gamelon D, Brune R, Chauvin A, Ghazali DA, Yordanov Y, Arsicaud A, Gilleron P, Curac S, Richard M-C, et al. Red Blood Cell Transfusion in the Emergency Department: An Observational Cross-Sectional Multicenter Study. Journal of Clinical Medicine. 2021; 10(11):2475. https://doi.org/10.3390/jcm10112475
Chicago/Turabian StylePeyrony, Olivier, Danaé Gamelon, Romain Brune, Anthony Chauvin, Daniel Aiham Ghazali, Youri Yordanov, Aude Arsicaud, Pauline Gilleron, Sonja Curac, Marie-Caroline Richard, and et al. 2021. "Red Blood Cell Transfusion in the Emergency Department: An Observational Cross-Sectional Multicenter Study" Journal of Clinical Medicine 10, no. 11: 2475. https://doi.org/10.3390/jcm10112475
APA StylePeyrony, O., Gamelon, D., Brune, R., Chauvin, A., Ghazali, D. A., Yordanov, Y., Arsicaud, A., Gilleron, P., Curac, S., Richard, M.-C., Feral-Pierssens, A.-L., Villoing, B., Beaune, S., Goulet, H., Fontaine, J.-P., François, A., & Pirenne, F. (2021). Red Blood Cell Transfusion in the Emergency Department: An Observational Cross-Sectional Multicenter Study. Journal of Clinical Medicine, 10(11), 2475. https://doi.org/10.3390/jcm10112475






