Can a Difference in Gestational Age According to Biparietal Diameter and Abdominal Circumference Predict Intrapartum Placental Abruption?
Abstract
1. Introduction
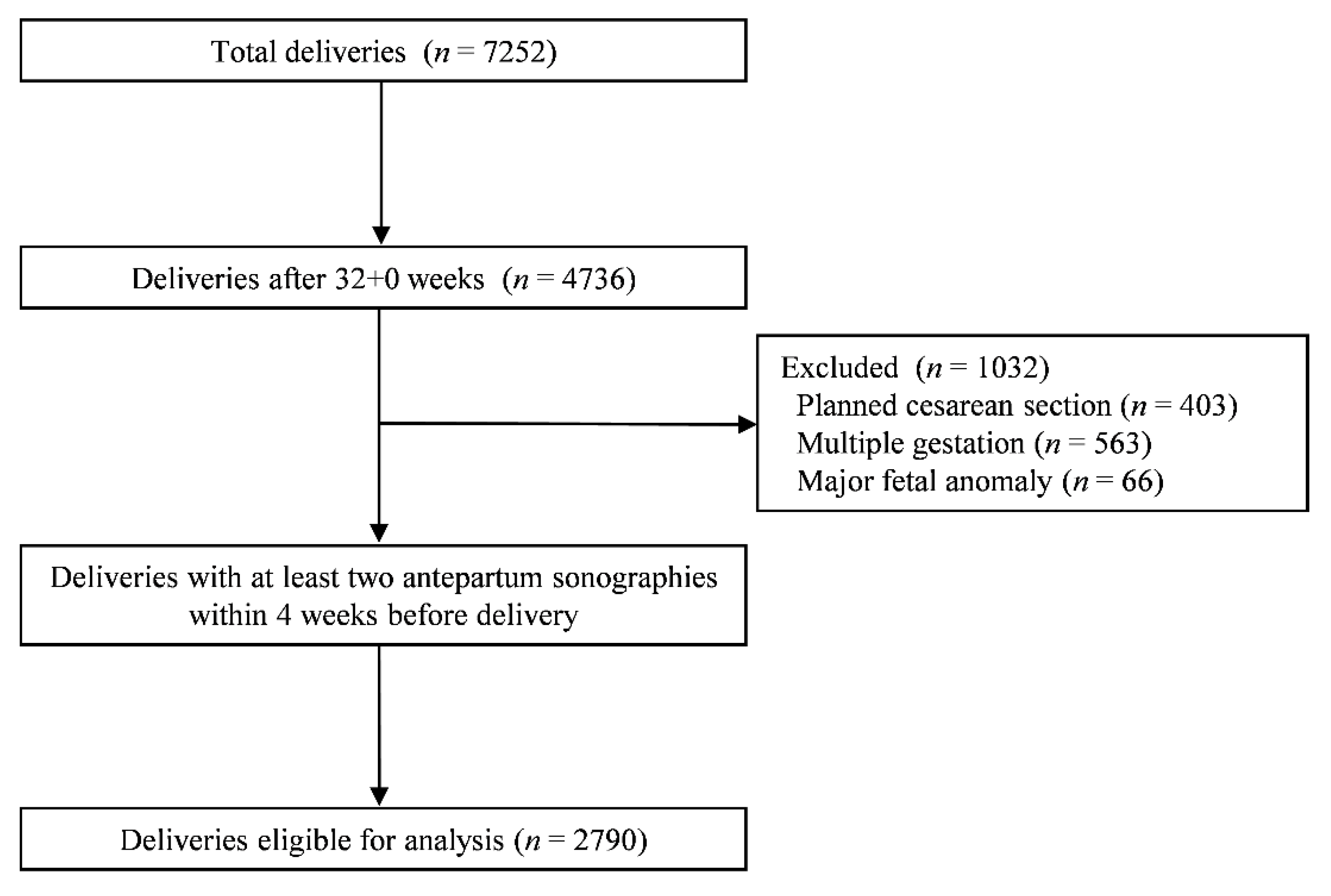
2. Materials and Methods
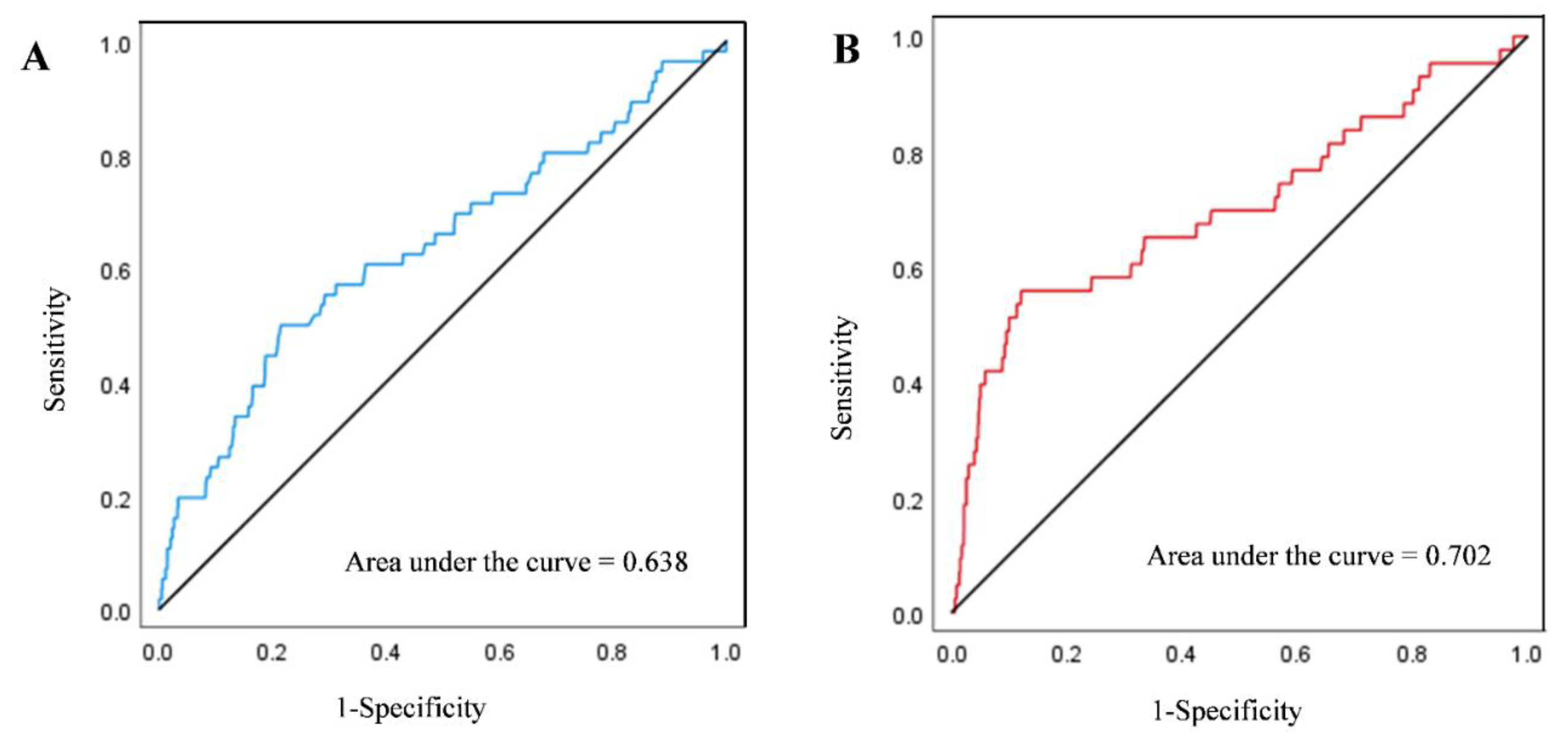
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ananth, C.V.; Wilcox, A.J. Placental abruption and perinatal mortality in the United States. Am. J. Epidemiol. 2001, 153, 332–337. [Google Scholar] [CrossRef]
- Tikkanen, M.; Nuutila, M.; Hiilesmaa, V.; Paavonen, J.; Ylikorkala, O. Clinical presentation and risk factors of placental abruption. Acta Obstet. Gynecol. Scand. 2006, 85, 700–705. [Google Scholar] [CrossRef]
- Oyelese, Y.; Ananth, C.V. Placental abruption. Obstet. Gynecol. 2006, 108, 1005–1016. [Google Scholar] [CrossRef] [PubMed]
- Ananth, C.V.; Berkowitz, G.S.; Savitz, D.A.; Lapinski, R.H. Placental abruption and adverse perinatal outcomes. JAMA 1999, 282, 1646–1651. [Google Scholar] [CrossRef] [PubMed]
- Downes, K.L.; Shenassa, E.D.; Grantz, K.L. Neonatal Outcomes Associated with Placental Abruption. Am. J. Epidemiol. 2017, 186, 1319–1328. [Google Scholar] [CrossRef]
- Cleary-Goldman, J.; Malone, F.D.; Vidaver, J.; Ball, R.H.; Nyberg, D.A.; Comstock, C.H.; Saade, G.R.; Eddleman, K.A.; Klugman, S.; Dugoff, L.; et al. Impact of maternal age on obstetric outcome. Obstet. Gynecol. 2005, 105, 983–990. [Google Scholar] [CrossRef]
- Sheiner, E.; Shoham-Vardi, I.; Hallak, M.; Hadar, A.; Gortzak-Uzan, L.; Katz, M.; Mazor, M. Placental abruption in term pregnancies: Clinical significance and obstetric risk factors. J. Matern. Fetal Neonatal Med. 2003, 13, 45–49. [Google Scholar] [CrossRef]
- Lim, J.W. The changing trends in live birth statistics in Korea, 1970 to 2010. Korean J. Pediatr. 2011, 54, 429–435. [Google Scholar] [CrossRef]
- Lean, S.C.; Derricott, H.; Jones, R.L.; Heazell, A.E.P. Advanced maternal age and adverse pregnancy outcomes: A systematic review and meta-analysis. PLoS ONE 2017, 12, e0186287. [Google Scholar] [CrossRef] [PubMed]
- Ananth, C.V.; Savitz, D.A.; Williams, M.A. Placental abruption and its association with hypertension and prolonged rupture of membranes: A methodologic review and meta-analysis. Obstet. Gynecol. 1996, 88, 309–318. [Google Scholar] [CrossRef]
- Major, C.A.; de Veciana, M.; Lewis, D.F.; Morgan, M.A. Preterm premature rupture of membranes and abruptio placentae: Is there an association between these pregnancy complications? Am. J. Obstet. Gynecol. 1995, 172, 672–676. [Google Scholar] [CrossRef]
- Lindqvist, P.G.; Happach, C. Risk and risk estimation of placental abruption. Eur. J. Obstet. Gynecol. Reprod. Biol. 2006, 126, 160–164. [Google Scholar] [CrossRef] [PubMed]
- Ghaheh, H.S.; Feizi, A.; Mousavi, M.; Sohrabi, D.; Mesghari, L.; Hosseini, Z. Risk factors of placental abruption. J. Res. Med. Sci. 2013, 18, 422–426. [Google Scholar]
- Jenabi, E.; Khazaei, S.; Fereidooni, B. The effect of placenta abruption on the risk of intrauterine growth restriction: A meta-analysis. Adv. Hum. Biol. 2019, 9, 8–11. [Google Scholar]
- Abu-Heija, A.; Al-Chalabi, H.; El-Iloubani, N. Abruptio placentae: Risk factors and perinatal outcome. J. Obstet. Gynaecol. Res. 1998, 24, 141–144. [Google Scholar] [CrossRef]
- McCowan, L.M.; Figueras, F.; Anderson, N.H. Evidence-based national guidelines for the management of suspected fetal growth restriction: Comparison, consensus, and controversy. Am. J. Obstet. Gynecol. 2018, 218, S855–S868. [Google Scholar] [CrossRef] [PubMed]
- Obstetricians, A.C.; Gynecologists, A. ACOG Practice bulletin no. 134: Fetal growth restriction. Obstet. Gynecol. 2013, 121, 1122–1133. [Google Scholar]
- Vayssiere, C.; Sentilhes, L.; Ego, A.; Bernard, C.; Cambourieu, D.; Flamant, C.; Gascoin, G.; Gaudineau, A.; Grange, G.; Houfflin-Debarge, V.; et al. Fetal growth restriction and intra-uterine growth restriction: Guidelines for clinical practice from the French College of Gynaecologists and Obstetricians. Eur. J. Obstet. Gynecol. Reprod. Biol. 2015, 193, 10–18. [Google Scholar] [CrossRef]
- Rad, S.; Beauchamp, S.; Morales, C.; Mirocha, J.; Esakoff, T.F. Defining fetal growth restriction: Abdominal circumference as an alternative criterion. J. Matern. Fetal Neonatal Med. 2018, 31, 3089–3094. [Google Scholar] [CrossRef]
- Turitz, A.L.; Quant, H.; Schwartz, N.; Elovitz, M.; Bastek, J.A. Isolated abdominal circumference <5% or estimated fetal weight 10 to 19% as predictors of small for gestational age infants. Am. J. Perinatol. 2014, 31, 469–476. [Google Scholar]
- Chauhan, S.P.; Cole, J.; Sanderson, M.; Magann, E.F.; Scardo, J.A. Suspicion of intrauterine growth restriction: Use of abdominal circumference alone or estimated fetal weight below 10%. J. Matern. Fetal Neonatal Med. 2006, 19, 557–562. [Google Scholar] [CrossRef]
- Hadlock, F.P.; Harrist, R.B.; Sharman, R.S.; Deter, R.L.; Park, S.K. Estimation of fetal weight with the use of head, body, and femur measurements—A prospective study. Am. J. Obstet. Gynecol. 1985, 151, 333–337. [Google Scholar] [CrossRef]
- Louis, G.B.; Grewal, J.; Albert, P.; Sciscione, A.; Nageotte, M.; Grobman, W.; Newman, R.; Wapner, R.; D’Alton, M.; Skupski, D.; et al. Racial/Ethnic differences in fetal growth, the NICHD fetal growth studies. Am. J. Obstet. Gynecol. 2015, 212, 36. [Google Scholar] [CrossRef]
- Gordijn, S.J.; Beune, I.M.; Thilaganathan, B.; Papageorghiou, A.; Baschat, A.A.; Baker, P.N.; Silver, R.M.; Wynia, K.; Ganzevoort, W. Consensus definition of fetal growth restriction: A Delphi procedure. Ultrasound Obstet. Gynecol. 2016, 48, 333–339. [Google Scholar] [CrossRef]
- Unterscheider, J.; Daly, S.; Geary, M.P.; Kennelly, M.M.; McAuliffe, F.M.; O’Donoghue, K.; Hunter, A.; Morrison, J.J.; Burke, G.; Dicker, P.; et al. Optimizing the definition of intrauterine growth restriction: The multicenter prospective PORTO Study. Am. J. Obstet. Gynecol. 2013, 208, 290.e1–290.e6. [Google Scholar] [CrossRef]
- Sheth, T.; Glantz, J.C. Third-Trimester Fetal Biometry and Neonatal Outcomes in Term and Preterm Deliveries. J. Ultrasound Med. 2016, 35, 103–110. [Google Scholar] [CrossRef]
- Hawkins, L.K.; Schnettler, W.T.; Modest, A.M.; Hacker, M.R.; Rodriguez, D. Association of third-trimester abdominal circumference with provider-initiated preterm delivery. J. Matern. Fetal Neonatal Med. 2014, 27, 1228–1231. [Google Scholar] [CrossRef]
- Kramer, M.S.; Usher, R.H.; Pollack, R.; Boyd, M.; Usher, S. Etiologic determinants of abruptio placentae. Obstet. Gynecol. 1997, 89, 221–226. [Google Scholar] [CrossRef]
- Downes, K.L.; Grantz, K.L.; Shenassa, E.D. Maternal, Labor, Delivery, and Perinatal Outcomes Associated with Placental Abruption: A Systematic Review. Am. J. Perinatol. 2017, 34, 935–957. [Google Scholar]
- Spinillo, A.; Gardella, B.; Bariselli, S.; Alfei, A.; Silini, E.M.; Bello, B.D. Cerebroplacental Doppler ratio and placental histopathological features in pregnancies complicated by fetal growth restriction. J. Perinat. Med. 2014, 42, 321–328. [Google Scholar] [CrossRef]
- Dubiel, M.; Breborowicz, G.H.; Marsal, K.; Gudmundsson, S. Fetal adrenal and middle cerebral artery Doppler velocimetry in high-risk pregnancy. Ultrasound Obstet. Gynecol. 2000, 16, 414–418. [Google Scholar] [CrossRef]
- Lackman, F.; Capewell, V.; Gagnon, R.; Richardson, B. Fetal umbilical cord oxygen values and birth to placental weight ratio in relation to size at birth. Am. J. Obstet. Gynecol. 2001, 185, 674–682. [Google Scholar] [CrossRef]
- Parra-Saavedra, M.; Crovetto, F.; Triunfo, S.; Savchev, S.; Peguero, A.; Nadal, A.; Parra, G.; Gratacos, E.; Figueras, F. Placental findings in late-onset SGA births without Doppler signs of placental insufficiency. Placenta 2013, 34, 1136–1141. [Google Scholar] [CrossRef]
- Morris, R.K.; Say, R.; Robson, S.C.; Kleijnen, J.; Khan, K.S. Systematic review and meta-analysis of middle cerebral artery Doppler to predict perinatal wellbeing. Eur. J. Obstet. Gynecol. Reprod. Biol. 2012, 165, 141–155. [Google Scholar] [CrossRef]
- Dilmen, G.; Toppare, M.F.; Turhan, N.O.; Ozturk, M.; Isik, S. Transverse cerebellar diameter and transverse cerebellar diameter/abdominal circumference index for assessing fetal growth. Fetal Diagn. Ther. 1996, 11, 50–56. [Google Scholar] [CrossRef]
- Tongsong, T.; Wanapirak, C.; Thongpadungroj, T. Sonographic diagnosis of intrauterine growth restriction (IUGR) by fetal transverse cerebellar diameter (TCD)/abdominal circumference (AC) ratio. Int. J. Gynaecol. Obstet. 1999, 66, 1–5. [Google Scholar] [CrossRef]
- Shinohara, S.; Okuda, Y.; Hirata, S.; Suzuki, K. Predictive possibility of the transverse cerebellar diameter to abdominal circumference ratio for small-for-gestational-age fetus suspected as a cause of maternal placental syndromes: A retrospective cohort study. Hypertens. Pregnancy 2020, 39, 145–151. [Google Scholar] [CrossRef] [PubMed]
- Roberts, J.M. Pathophysiology of ischemic placental disease. Semin. Perinatol. 2014, 38, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Burton, G.J.; Woods, A.W.; Jauniaux, E.; Kingdom, J.C. Rheological and physiological consequences of conversion of the maternal spiral arteries for uteroplacental blood flow during human pregnancy. Placenta 2009, 30, 473–482. [Google Scholar] [CrossRef]
- Roberts, J.M.; Escudero, C. The placenta in preeclampsia. Int. J. Womans Cardiovasc. Health 2012, 2, 72–83. [Google Scholar] [CrossRef]
- Arias, F.; Rodriquez, L.; Rayne, S.C.; Kraus, F.T. Maternal placental vasculopathy and infection: Two distinct subgroups among patients with preterm labor and preterm ruptured membranes. Am. J. Obstet. Gynecol. 1993, 168, 585–591. [Google Scholar] [CrossRef]
- Aardema, M.W.; Oosterhof, H.; Timmer, A.; van Rooy, I.; Aarnoudse, J.G. Uterine artery Doppler flow and uteroplacental vascular pathology in normal pregnancies and pregnancies complicated by pre-eclampsia and small for gestational age fetuses. Placenta 2001, 22, 405–411. [Google Scholar] [CrossRef]
- Roberts, D.J.; Post, M.D. The placenta in pre-eclampsia and intrauterine growth restriction. J. Clin. Pathol. 2008, 61, 1254–1260. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, C.; Agrawal, K.K.; Gandhi, S. Assessment of fetal growth using the ratio of the transverse cerebellar diameter to abdominal circumference. Int. J. Gynaecol. Obstet. 2016, 135, 33–37. [Google Scholar] [CrossRef]
- Cohen, E.; Baerts, W.; van Bel, F. Brain-Sparing in Intrauterine Growth Restriction: Considerations for the Neonatologist. Neonatology 2015, 108, 269–276. [Google Scholar] [CrossRef] [PubMed]
- Caradeux, J.; Martinez-Portilla, R.J.; Peguero, A.; Sotiriadis, A.; Figueras, F. Diagnostic performance of third-trimester ultrasound for the prediction of late-onset fetal growth restriction: A systematic review and meta-analysis. Am. J. Obstet. Gynecol. 2019, 220, 449–459. [Google Scholar] [CrossRef]
- Roberts, A.B.; Mitchell, J.M.; McCowan, L.M.; Barker, S. Ultrasonographic measurement of liver length in the small-for-gestational-age fetus. Am. J. Obstet. Gynecol. 1999, 180, 634–638. [Google Scholar] [CrossRef]
| Abruption (+) (n = 56) | Abruption (−) (n = 2734) | p-Value | |
|---|---|---|---|
| Baseline characteristics | |||
| Maternal age, years (mean ± SD) | 34.6 ± 3.6 | 33.3 ± 3.7 | 0.007 |
| Nulliparity, n (%) | 31 (55.4) | 1764 (64.5) | 0.156 |
| Smoker, n (%) | 0 (0.0) | 22 (0.8) | 1.000 |
| BMI (kg/m2) at delivery | 26.4 ± 3.8 | 26.2 ± 3.5 | 0.826 |
| Assisted reproduction techniques, n (%) | 3 (5.4) | 154 (5.6) | 1.000 |
| Past obstetric history | |||
| Previous stillbirth at >20 weeks, n (%) | 2 (3.6) | 24 (0.9) | 0.095 |
| Previous preterm delivery, n (%) | 3 (5.4) | 78 (2.9) | 0.221 |
| Past medical history | |||
| Previous HTN, preeclampsia, n (%) | 2 (3.6) | 28 (1.0) | 0.121 |
| Previous DM, n (%) | 1 (1.8) | 29 (1.1) | 0.457 |
| Current pregnancy complications | |||
| Gestational diabetes mellitus, n (%) | 6 (10.7) | 245 (9.0) | 0.65 |
| Preeclampsia, n (%) | 7 (12.5) | 112 (4.1) | 0.002 |
| Sonographic features | |||
| Oligohydramnios, n (%) | 0 (0.0) | 50 (1.9) | 0.625 |
| EFW | |||
| SGA (<10th centile), n (%) | 18 (32.1) | 212 (7.8) | <0.001 |
| SGA (<5th centile), n (%) | 14 (25.0) | 112 (4.1) | <0.001 |
| SGA (<3rd centile), n (%) | 13 (23.2) | 86 (3.1) | <0.001 |
| AGA, n (%) | 35 (62.5) | 2320 (84.9) | <0.001 |
| LGA, n (%) | 2 (3.6) | 34 (1.2) | 0.162 |
| Difference in BPD and AC gestational age, n (%) | |||
| >2 weeks | 12 (21.4) | 205 (7.5) | <0.001 |
| >3 weeks | 7 (12.5) | 56 (2.0) | <0.001 |
| Delivery outcomes | |||
| Gestational age at delivery, weeks | 37.4 ± 2.4 | 39.3 ± 1.4 | <0.001 |
| Preterm, 32–36 weeks, n (%) | 20 (35.7) | 156 (5.7) | <0.001 |
| Induction or augmentation, n (%) | 34 (60.7) | 1464 (53.5) | 0.287 |
| Mode of delivery | <0.001 | ||
| Normal vaginal devliery, n (%) | 33 (58.9) | 2155 (78.8) | |
| Cesarean delivery, n (%) | 23 (41.1) | 579 (21.2) | |
| Induction failure | 1 (1.8) | 187 (6.8) | 0.178 |
| Fetal distress | 17 (30.4) | 70 (2.6) | <0.001 |
| Failure to progress | 1 (1.8) | 209 (7.6) | 0.123 |
| Other | 4 (7.1) | 113 (4.1) | 0.295 |
| Placental and umbilical cord abnormality, n (%) | 3 (5.4) | 51 (1.9) | 0.093 |
| Abruption (+) (n = 56) | Abruption (−) (n = 2734) | p-Value | |
|---|---|---|---|
| Birth weight, kg (mean ± SD) | 2.7 ± 0.7 | 3.2 ± 0.5 | <0.001 |
| Low Apgar score, 1 min (<4) | 9 (16.1) | 16 (0.6) | <0.001 |
| Low Apgar score, 5 min (<7) | 4 (7.1) | 10 (0.4) | <0.001 |
| Cord pH < 7.1 | 5 (17.9) | 25 (1.3) | <0.001 |
| Base excess of cord blood (mmol/ℓ) | −6.6 ± 5.4 | −4.4 ± 2.7 | 0.042 |
| Base excess of cord blood <−12 (mmol/ℓ) | 4 (14.3) | 22 (1.2) | <0.001 |
| NICU admission, n (%) | 27 (48.2) | 324 (11.9) | <0.001 |
| Duration of NICU stay, days (mean ± SD) | 12.9 ± 44.0 | 1.3 ± 9.6 | 0.054 |
| Neonatal death, n (%) | 2 (3.6) | 3 (0.1) | 0.004 |
| Adjusted Odds Ratio | 95% CI | p-Value | Adjusted Odds Ratio | 95% CI | p-Value | ||
|---|---|---|---|---|---|---|---|
| Maternal age | 1.116 | 1.038–1.199 | 0.003 | Maternal age | 1.114 | 1.036–1.197 | 0.004 |
| SGA (<10th centile) | 4.819 | 2.606–8.909 | <0.001 | SGA (<10th centile) | 4.669 | 2.505–8.702 | <0.001 |
| Preeclampsia | 2.183 | 0.936–5.088 | 0.071 | Preeclampsia | 2.258 | 0.962–5.302 | 0.061 |
| Difference of >2 weeks between BPD and AC gestational age | 2.289 | 1.140–4.600 | 0.020 | Difference of >3 weeks between BPD and AC gestational age | 3.918 | 1.517–9.771 | 0.003 |
| Maternal age | 1.121 | 1.042–1.206 | 0.002 | Maternal age | 1.117 | 1.039–1.202 | 0.003 |
| SGA (<5th centile) | 6.516 | 3.228–13.154 | <0.001 | SGA (<5th centile) | 6.192 | 3.012–12.729 | <0.001 |
| Preeclampsia | 2.098 | 0.891–4.942 | 0.071 | Preeclampsia | 2.178 | 0.919–5.162 | 0.077 |
| Difference of >2 weeks between BPD and AC gestational age | 2.067 | 1.003–4.258 | 0.049 | Difference of >3 weeks between BPD and AC gestational age | 3.186 | 1.218–8.336 | 0.018 |
| Maternal age | 1.118 | 1.039–1.204 | 0.003 | Maternal age | 1.117 | 1.037–1.202 | 0.003 |
| SGA (<3rd centile) | 7.513 | 3.616–15.608 | <0.001 | SGA (<3rd centile) | 7.164 | 3.395–15.119 | <0.001 |
| Preeclampsia | 2.068 | 0.871–4.906 | 0.099 | Preeclampsia | 2.129 | 0.891–5.089 | 0.089 |
| Difference of >2 weeks between BPD and AC gestational age | 2.039 | 0.983–4.227 | 0.056 | Difference of >3 weeks between BPD and AC gestational age | 3.209 | 1.218–8.453 | 0.018 |
| Difference of >2 Weeks between BPD and AC Gestational Age | Difference of >3 Weeks between BPD and AC Gestational Age | |
|---|---|---|
| Positive predictive value | 5.5% | 11.1% |
| Negative predictive value | 98.3% | 98.2% |
| Sensitivity | 21.4% | 12.5% |
| Specificity | 92.5% | 98.0% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hong, J.-Y.; Kim, J.-H.; Kim, S.-y.; Sung, J.-H.; Choi, S.-J.; Oh, S.-y.; Roh, C.-R. Can a Difference in Gestational Age According to Biparietal Diameter and Abdominal Circumference Predict Intrapartum Placental Abruption? J. Clin. Med. 2021, 10, 2413. https://doi.org/10.3390/jcm10112413
Hong J-Y, Kim J-H, Kim S-y, Sung J-H, Choi S-J, Oh S-y, Roh C-R. Can a Difference in Gestational Age According to Biparietal Diameter and Abdominal Circumference Predict Intrapartum Placental Abruption? Journal of Clinical Medicine. 2021; 10(11):2413. https://doi.org/10.3390/jcm10112413
Chicago/Turabian StyleHong, Jee-Youn, Jin-Ha Kim, Seo-yeon Kim, Ji-Hee Sung, Suk-Joo Choi, Soo-young Oh, and Cheong-Rae Roh. 2021. "Can a Difference in Gestational Age According to Biparietal Diameter and Abdominal Circumference Predict Intrapartum Placental Abruption?" Journal of Clinical Medicine 10, no. 11: 2413. https://doi.org/10.3390/jcm10112413
APA StyleHong, J.-Y., Kim, J.-H., Kim, S.-y., Sung, J.-H., Choi, S.-J., Oh, S.-y., & Roh, C.-R. (2021). Can a Difference in Gestational Age According to Biparietal Diameter and Abdominal Circumference Predict Intrapartum Placental Abruption? Journal of Clinical Medicine, 10(11), 2413. https://doi.org/10.3390/jcm10112413






