Metabolic Alterations in Sepsis
Abstract
1. Introduction
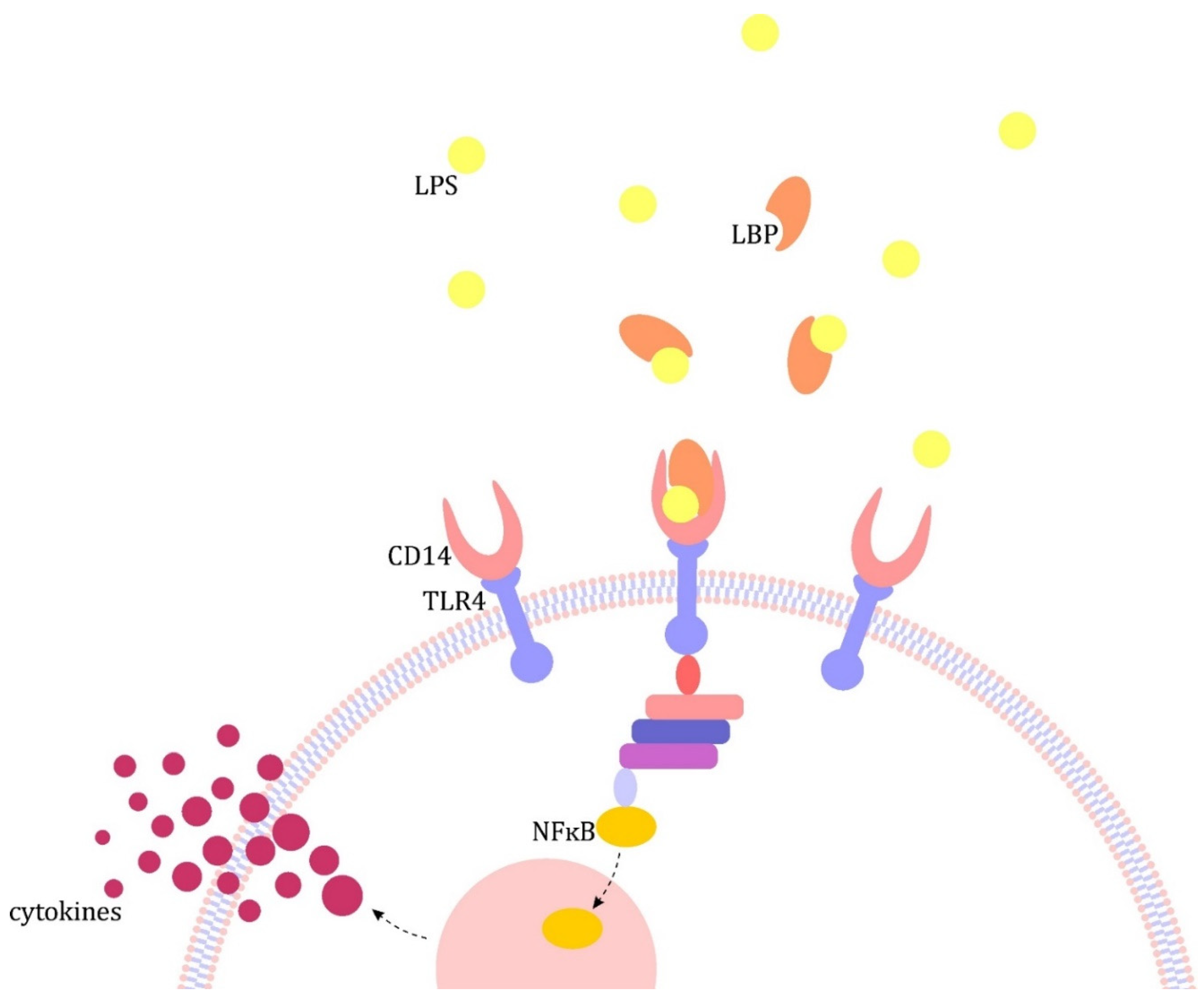
2. Outline of the Pathogenesis of Sepsis
3. Metabolic Disorders in Sepsis
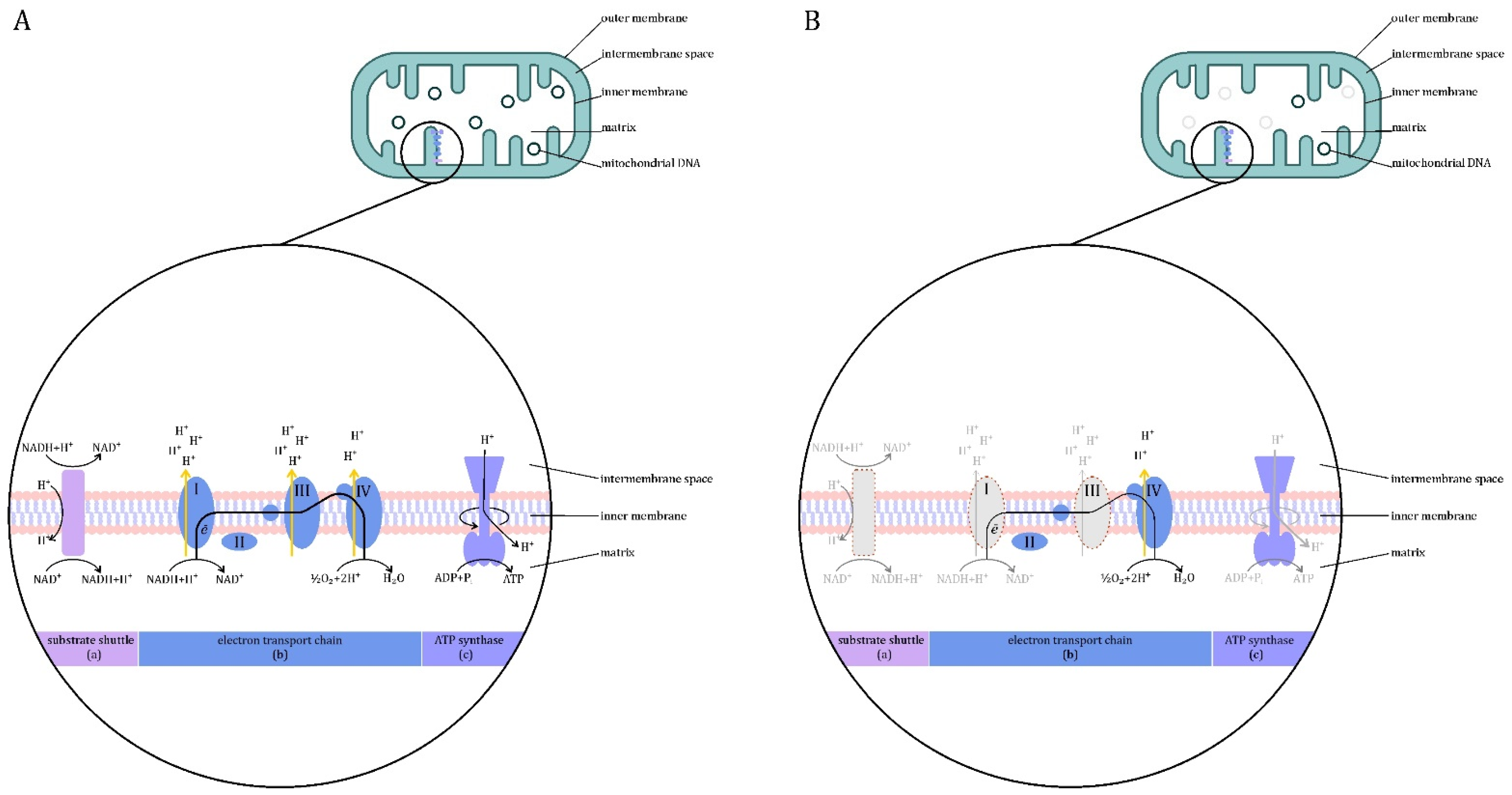
3.1. Mitochondrial Dysfunction
3.2. Carbohydrate Metabolism
3.3. Lipid Metabolism
3.4. Ketone Metabolism
3.5. Amino Acid Metabolism
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.D.; Coopersmith, C.M.; et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef]
- Cohen, J.; Vincent, J.L.; Adhikari, N.K.; Machado, F.R.; Angus, D.C.; Calandra, T.; Jaton, K.; Giulieri, S.; Delaloye, J.; Opal, S.; et al. Sepsis: A roadmap for future research. Lancet Infect. Dis. 2015, 15, 581–614. [Google Scholar] [CrossRef]
- Kenig, A.; Ilan, Y. A Personalized Signature and Chronotherapy-Based Platform for Improving the Efficacy of Sepsis Treatment. Front. Physiol. 2019, 10, 1542. [Google Scholar] [CrossRef]
- Wasyluk, W.; Wasyluk, M.; Zwolak, A. Sepsis as a Pan-Endocrine Illness—Endocrine Disorders in Septic Patients. J. Clin. Med. 2021, 10, 2075. [Google Scholar] [CrossRef]
- Carré, J.; Singer, M.; Moncada, S. Nitric Oxide. In Mechanisms of Sepsis-Induced Organ Dysfunction and Recovery; Abraham, E., Singer, M., Eds.; Springer: Berlin/Heidelberg, Germany; New York, NY, USA, 2007; pp. 77–95. [Google Scholar]
- Singer, M. Dysfunction of the Bioenergetic Pathway. In Mechanisms of Sepsis-Induced Organ Dysfunction and Recovery; Abraham, E., Singer, M., Eds.; Springer: Berlin/Heidelberg, Germany; New York, NY, USA, 2007; pp. 299–310. [Google Scholar]
- Hotchkiss, R.S.; Karl, I.E. The pathophysiology and treatment of sepsis. N. Engl. J. Med. 2003, 348, 138–150. [Google Scholar] [CrossRef]
- Carré, J.E.; Singer, M. Cellular energetic metabolism in sepsis: The need for a systems approach. Biochim. Biophys. Acta 2008, 1777, 763–771. [Google Scholar] [CrossRef]
- Cohen, J. The immunopathogenesis of sepsis. Nature 2002, 420, 885–891. [Google Scholar] [CrossRef] [PubMed]
- Englert, J.A.; Rogers, A.J. Metabolism, Metabolomics, and Nutritional Support of Patients with Sepsis. Clin. Chest Med. 2016, 37, 321–331. [Google Scholar] [CrossRef] [PubMed]
- Pinsky, M.R.; Vincent, J.L.; Deviere, J.; Alegre, M.; Kahn, R.J.; Dupont, E. Serum cytokine levels in human septic shock; Relation to multiple-system organ failure and mortality. Chest 1993, 103, 565–575. [Google Scholar] [CrossRef]
- Remick, D.G. Pathophysiology of sepsis. Am. J. Pathol. 2007, 170, 1435–1444. [Google Scholar] [CrossRef]
- Molloy, R.G.; Mannick, J.A.; Rodrick, M.L. Cytokines, sepsis and immunomodulation. Br. J. Surg. 1993, 80, 289–297. [Google Scholar] [CrossRef]
- Lewis, A.J.; Billiar, T.R.; Rosengart, M.R. Biology and Metabolism of Sepsis: Innate Immunity, Bioenergetics, and Autophagy. Surg. Infect. 2016, 17, 286–293. [Google Scholar] [CrossRef]
- Tharan, K.S.; Abu-Habsa, M. Understanding the metabolic response to sepsis. Br. J. Hosp. Med. 2009, 70 (Suppl. 2), M20–M22. [Google Scholar] [CrossRef]
- Moriyama, S.; Okamoto, K.; Tabira, Y.; Kikuta, K.; Kukita, I.; Hamaguchi, M.; Kitamura, N. Evaluation of oxygen consumption and resting energy expenditure in critically ill patients with systemic inflammatory response syndrome. Crit. Care Med. 1999, 27, 2133–2136. [Google Scholar] [CrossRef]
- Singer, P.M.; de Santis, V.; Vitale, D.; Jeffcoate, W. Multiorgan failure is an adaptive, endocrine-mediated, metabolic response to overwhelming systemic inaflammation. Lancet 2004, 364, 545–548. [Google Scholar] [CrossRef]
- Singer, M. Mitochondrial function in sepsis: Acute phase versus multiple organ failure. Crit. Care Med. 2007, 35, S441–S448. [Google Scholar] [CrossRef] [PubMed]
- Singer, M. The role of mitochondrial dysfunction in sepsis-induced multi-organ failure. Virulence 2014, 5, 66–72. [Google Scholar] [CrossRef] [PubMed]
- Irahara, T.; Sato, N.; Otake, K.; Matsumura, S.; Inoue, K.; Ishihara, K.; Fushiki, T.; Yokota, H. Alterations in energy substrate metabolism in mice with different degrees of sepsis. J. Surg. Res. 2018, 227, 44–51. [Google Scholar] [CrossRef]
- Michie, H.R. Metabolism of sepsis and multiple organ failure. World J. Surg. 1996, 20, 460–464. [Google Scholar] [CrossRef]
- Wolfe, R.R. Sepsis as a modulator of adaptation to low and high carbohydrate and low and high fat intakes. Eur. J. Clin. Nutr. 1999, 53, s136–s142. [Google Scholar] [CrossRef] [PubMed]
- Cerra, F.B.; Siegel, J.H.; Coleman, B.; Border, J.R.; McMenamy, R.R. Septic autocannibalism. A failure of exogenous nutritional support. Ann. Surg. 1980, 192, 570–580. [Google Scholar] [CrossRef]
- Spanaki, A.M.; Tavladaki, T.; Dimitriou, H.; Kozlov, A.V.; Duvigneau, J.C.; Meleti, E.; Weidinger, A.; Papakonstantinou, E.; Briassoulis, G. Longitudinal Profiles of Metabolism and Bioenergetics Associated with Innate Immune Hormonal Inflammatory Responses and Amino-Acid Kinetics in Severe Sepsis and Systemic Inflammatory Response Syndrome in Children. J. Parenter. Enter. Nutr. 2018, 42, 1061–1074. [Google Scholar] [CrossRef]
- Saraste, M. Oxidative phosphorylation at the fin de siècle. Science 1999, 283, 1488–1493. [Google Scholar] [CrossRef]
- McBride, H.M.; Neuspiel, M.; Wasiak, S. Mitochondria: More Than Just a Powerhouse. Curr. Biol. 2006, 16, 551–560. [Google Scholar] [CrossRef]
- Chan, D.C. Mitochondria: Dynamic Organelles in Disease, Aging, and Development. Cell 2006, 125, 1241–1252. [Google Scholar] [CrossRef]
- Galluzzi, L.; Kepp, O.; Kroemer, G. Mitochondria: Master regulators of danger signaling. Nat. Rev. Mol. Cell Biol. 2012, 13, 780–788. [Google Scholar] [CrossRef] [PubMed]
- Osellame, L.D.; Blacker, T.S.; Duchen, M.R. Cellular and molecular mechanisms of mitochondrial function. Best Pract. Res. Clin. Endocrinol. Metab. 2012, 26, 711–723. [Google Scholar] [CrossRef]
- Miller, W.L. Role of mitochondria in steroidogenesis. Pediatr. Adrenal Dis. 2011, 20, 1–19. [Google Scholar] [CrossRef]
- Botham, M.; Mayes, P.A. The Respiratory Chain & Oxidative Phosphorylation. In Harper’s Illustrated Biochemistry, 31e; Rodwell, V.W., Bender, D.A., Botham, K.M., Kennelly, P.J., Weil, P.A., Eds.; McGraw-Hill Education: New York, NY, USA, 2018. [Google Scholar]
- Zhang, H.; Feng, Y.W.; Yao, Y.M. Potential therapy strategy: Targeting mitochondrial dysfunction in sepsis. Mil. Med. Res. 2018, 5, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Corrêa, T.D.; Jakob, S.M.; Takala, J. Mitochondrial Function in Sepsis. Crit. Care Horiz. 2015, 1, 31–41. [Google Scholar]
- Fink, M.P. Bench-to-bedside review: Cytopathic hypoxia. Crit. Care 2002, 6, 491–499. [Google Scholar] [CrossRef] [PubMed]
- Larsen, F.J.; Schiffer, T.A.; Weitzberg, E.; Lundberg, J.O. Regulation of mitochondrial function and energetics by reactive nitrogen oxides. Free Radic. Biol. Med. 2012, 53, 1919–1928. [Google Scholar] [CrossRef]
- Carré, J.E.; Orban, J.C.; Re, L.; Felsmann, K.; Iffert, W.; Bauer, M.; Suliman, H.B.; Piantadosi, C.A.; Mayhew, T.M.; Breen, P.; et al. Survival in critical illness is associated with early activation of mitochondrial biogenesis. Am. J. Respir. Crit. Care Med. 2010, 182, 745–751. [Google Scholar] [CrossRef] [PubMed]
- Lee, I.; Hüttemann, M. Energy crisis: The role of oxidative phosphorylation in acute inflammation and sepsis. Biochim. Biophys. Acta Mol. Basis Dis. 2014, 1842, 1579–1586. [Google Scholar] [CrossRef]
- Callahan, L.A.; Supinski, G.S. Downregulation of diaphragm electron transport chain and glycolytic enzyme gene expression in sepsis. J. Appl. Physiol. 2005, 99, 1120–1126. [Google Scholar] [CrossRef] [PubMed]
- Haden, D.W.; Suliman, H.B.; Carraway, M.S.; Welty-Wolf, K.E.; Ali, A.S.; Shitara, H.; Yonekawa, H.; Piantadosi, C.A. Mitochondrial biogenesis restores oxidative metabolism during Staphylococcus aureus sepsis. Am. J. Respir. Crit. Care Med. 2007, 176, 768–777. [Google Scholar] [CrossRef] [PubMed]
- Wallace, D.C. Mitochondrial diseases in man and mouse. Science 1999, 283, 1482–1488. [Google Scholar] [CrossRef]
- van Wyngene, L.; Vandewalle, J.; Libert, C. Reprogramming of basic metabolic pathways in microbial sepsis: Therapeutic targets at last? EMBO Mol. Med. 2018, 10, e8712. [Google Scholar] [CrossRef]
- Chuang, Y.-C.; Tsai, J.-L.; Chang, A.Y.W.; Chan, J.Y.H.; Liou, C.-W.; Chan, S.H.H. Dysfunction of the Mitochondrial Respiratory Chain in the Rostral Ventrolateral Medulla during Experimental Endotoxemia in the Rat. J. Biomed. Sci. 2003, 9, 542–548. [Google Scholar] [CrossRef]
- Levy, R.J. Mitochondrial dysfunction, bioenergetic impairment, and metabolic down-regulation in sepsis. Shock 2007, 28, 24–28. [Google Scholar] [CrossRef]
- Chen, H.W.; Hsu, C.; Lu, T.S.; Wang, S.J.; Yang, R.C. Heat shock pretreatment prevents cardiac mitochondrial dysfunction during sepsis. Shock 2003, 20, 274–279. [Google Scholar] [CrossRef]
- Fukumoto, K.; Pierro, A.; Spitz, L.; Eaton, S. Neonatal endotoxemia affects heart but not kidney bioenergetics. J. Pediatr. Surg. 2003, 38, 690–693. [Google Scholar] [CrossRef]
- Kalpage, H.A.; Wan, J.; Morse, P.T.; Zurek, M.P.; Turner, A.A.; Khobeir, A.; Yazdi, N.; Hakim, L.; Liu, J.; Vaishnav, A.; et al. Cytochrome c phosphorylation: Control of mitochondrial electron transport chain flux and apoptosis. Int. J. Biochem. Cell Biol. 2020, 121, 105704. [Google Scholar] [CrossRef]
- Arulkumaran, N.; Deutschman, C.S.; Pinsky, M.R.; Zuckerbraun, B.; Schumacker, P.T.; Gomez, H.; Gomez, A.; Murray, P.; Kellum, J.A. Mitochondrial function in sepsis. Shock 2016, 45, 271–281. [Google Scholar] [CrossRef]
- Leverve, X.M. Mitochondrial function and substrate availability. Crit. Care Med. 2007, 35, S454–S460. [Google Scholar] [CrossRef]
- Brealey, D.; Singer, M. Mitochondrial dysfunction in sepsis. Curr. Infect. Dis. Rep. 2003, 5, 365–371. [Google Scholar] [CrossRef] [PubMed]
- Boekstegers, P.; Weidenhöfer, S.; Pilz, G.; Werdan, K. Peripheral oxygen availability within skeletal muscle in sepsis and septic shock: Comparison to limited infection and cardiogenic shock. Infection 1991, 19, 317–323. [Google Scholar] [CrossRef] [PubMed]
- Sair, M.; Etherington, P.J.; Winlove, C.P.; Evans, T.W. Tissue oxygenation and perfusion in patients with systemic sepsis. Crit. Care Med. 2001, 29, 1343–1349. [Google Scholar] [CrossRef]
- VanderMeer, T.J.; Wang, H.; Fink, M.P. Endotoxemia causes ileal mucosal acidosis in the absence of mucosal hypoxia in a normodynamic porcine model of septic shock. Crit. Care Med. 1995, 23, 1217–1226. [Google Scholar] [CrossRef]
- Suetrong, B.; Walley, K.R. Lactic acidosis in sepsis: It’s Not All anaerobic: Implications for diagnosis and management. Chest 2016, 149, 252–261. [Google Scholar] [CrossRef] [PubMed]
- Kreymann, G.; Grosser, S.; Buggisch, P.; Gottschall, C.; Matthaei, S.; Greten, H. Oxygen consumption and resting metabolic rate in sepsis, sepsis syndrome, and septic shock. Crit. Care Med. 1993, 21, 1012–1019. [Google Scholar] [CrossRef]
- Nogueira, V.; Walter, L.; Avéret, N.; Fontaine, E.; Rigoulet, M.; Leverve, X.M. Thyroid status is a key regulator of both flux and efficiency of oxidative phosphorylation in rat hepatocytes. J. Bioenerg. Biomembr. 2002, 34, 55–66. [Google Scholar] [CrossRef]
- Harper, M.-E. Hyperthyroidism stimulates mitochondrial proton leak and ATP turnover in rat hepatocytes but does not change the overall kinetics of substrate oxidation. Can. J. Physiol. Pharm. 1994, 72, 899–908. [Google Scholar] [CrossRef] [PubMed]
- Whelan, S.P.; Carchman, E.H.; Kautza, B.; Nassour, I.; Mollen, K.; Escobar, D.; Gomez, H.; Rosengart, M.A.; Shiva, S.; Zuckerbraun, B.S. Polymicrobial sepsis is associated with decreased hepatic oxidative phosphorylation and an altered metabolic profile. J. Surg. Res. 2014, 186, 297–303. [Google Scholar] [CrossRef]
- Brealey, D.; Brand, M.; Hargreaves, I.; Heales, S.; Land, J.; Smolenski, R.; Davies, N.A.; Cooper, C.E.; Singer, M. Association between mitochondrial dysfunction and severity and outcome of septic shock. Lancet 2002, 360, 219–223. [Google Scholar] [CrossRef]
- Fredriksson, K.; Hammarqvist, F.; Strigård, K.; Hultenby, K.; Ljungqvist, O.; Wernerman, J.; Rooyackers, O. Derangements in mitochondrial metabolism in intercostal and leg muscle of critically ill patients with sepsis-induced multiple organ failure. Am. J. Physiol. Endocrinol. Metab. 2006, 291. [Google Scholar] [CrossRef] [PubMed]
- Mizobata, Y.; Prechek, D.; Rounds, J.D.; Robinson, V.; Wilmore, D.W.; Jacobs, D.O. The duration of infection modifies mitochondrial oxidative capacity in rat skeletal muscle. J. Surg. Res. 1995, 59, 165–173. [Google Scholar] [CrossRef]
- Kantrow, S.P.; Taylor, D.E.; Carraway, M.S.; Piantadosi, C.A. Oxidative Metabolism in Rat Hepatocytes and Mitochondria during Sepsis. Arch. Biochem. Biophys. 1997, 345, 278–288. [Google Scholar] [CrossRef]
- Marik, P.E.; Bellomo, R. Stress hyperglycemia: An essential survival response! Crit. Care 2013, 17, 305. [Google Scholar] [CrossRef]
- Cheng, S.C.; Scicluna, B.P.; Arts, R.J.; Gresnigt, M.S.; Lachmandas, E.; Giamarellos-Bourboulis, E.J.; Kox, M.; Manjeri, G.R.; Wagenaars, J.A.; Cremer, O.L.; et al. Broad defects in the energy metabolism of leukocytes underlie immunoparalysis in sepsis. Nat. Immunol. 2016, 17, 406–413. [Google Scholar] [CrossRef]
- Andersen, S.K.; Gjedsted, J.; Christiansen, C.; Tønnesen, E. The roles of insulin and hyperglycemia in sepsis pathogenesis. J. Leukoc. Biol. 2004, 75, 413–421. [Google Scholar] [CrossRef] [PubMed]
- Bender, D.A.; Mayes, P.A. Gluconeogenesis & the Control of Blood Glucose. In Harper’s Illustrated Biochemistry, 31e; Rodwell, V.W., Bender, D.A., Botham, K.M., Kennelly, P.J., Weil, P.A., Eds.; McGraw-Hill Education: New York, NY, USA, 2018. [Google Scholar]
- Sobotka, L.; Soeters, P.B. Basics in clinical nutrition: Metabolic response to injury and sepsis. e-SPEN 2009, 4, e1–e3. [Google Scholar] [CrossRef][Green Version]
- Szablewski, L. Glucose transporters in healthy heart and in cardiac disease. Int. J. Cardiol. 2017, 230, 70–75. [Google Scholar] [CrossRef] [PubMed]
- Vary, T.C.; Drnevich, D.; Jurasinski, C.; Brennan, W.A., Jr. Mechanisms regulating skeletal muscle glucose metabolism in sepsis. Shock 1995, 3, 403–410. [Google Scholar]
- Lang, C.H.; Dobrescu, C.; Bagby, G.J. Tumor necrosis factor impairs insulin action on peripheral glucose disposal and hepatic glucose output. Endocrinology 1992, 130, 43–52. [Google Scholar] [CrossRef]
- Sakurai, Y.; Zhang, X.J.; Wolfe, A.R. TNF directly stimulates glucose uptake and leucine oxidation and inhibits FFA flux in conscious dogs. Am. J. Physiol. Endocrinol. Metab. 1996, 270, E864–E872. [Google Scholar] [CrossRef] [PubMed]
- Frayn, K.N. Hormonal control of metabolism in trauma and sepsis. Clin. Endocrinol. 1986, 24, 577–599. [Google Scholar] [CrossRef] [PubMed]
- Carlson, G.L. Insulin resistance in human sepsis: Implications for the nutritional and metabolic care of the critically ill surgical patient. Ann. R. Coll. Surg. Engl. 2004, 86, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Carlson, G.L.; Little, R.A. Sympathetic nervous system and metabolism. In Metabolism and Artificial Nutrition in the Critically Ill; Springer: Milan, Italy, 1999; pp. 71–83. [Google Scholar]
- Bender, D.A.; Mayes, P.A. Glycolysis & the Oxidation of Pyruvate. In Harper’s Illustrated Biochemistry, 31e; Rodwell, V.W., Bender, D.A., Botham, K.M., Kennelly, P.J., Weil, P.A., Eds.; McGraw-Hill Education: New York, NY, USA, 2018. [Google Scholar]
- Loftus, R.M.; Finlay, D.K. Immunometabolism: Cellular metabolism turns immune regulator. J. Biol. Chem. 2016, 291, 1–10. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, L.A.J.; Kishton, R.J.; Rathmell, J. A guide to immunometabolism for immunologists. Nat. Rev. Immunol. 2016, 16, 553–565. [Google Scholar] [CrossRef] [PubMed]
- Vary, T.C. Sepsis-induced alterations in pyruvate dehydrogenase complex activity in rat skeletal muscle: Effects on plasma lactate. Shock 1996, 6, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Nuzzo, E.; Berg, K.M.; Andersen, L.W.; Balkema, J.; Montissol, S.; Cocchi, M.N.; Liu, X.; Donnino, M.W. Pyruvate dehydrogenase activity is decreased in the peripheral blood mononuclear cells of patients with sepsis: A prospective observational trial. Ann. Am. Thorac. Soc. 2015, 12, 1662–1666. [Google Scholar] [CrossRef] [PubMed]
- Jeoung, H. Pyruvate dehydrogenase kinases: Therapeutic targets for diabetes and cancers. Diabetes Metab. J. 2015, 39, 188–197. [Google Scholar] [CrossRef] [PubMed]
- Calvano, S.E.; Xiao, W.; Richards, D.R.; Felciano, R.M.; Baker, H.V.; Cho, R.J.; Chen, R.O.; Brownstein, B.H.; Cobb, J.P.; Tschoeke, S.K.; et al. A network-based analysis of systemic inflammation in humans. Nature 2005, 437, 1032–1037. [Google Scholar] [CrossRef] [PubMed]
- Corcoran, S.E.; O’Neill, L.A.J. HIF1α and metabolic reprogramming in inflammation. J. Clin. Investig. 2016, 126, 3699–3707. [Google Scholar] [CrossRef]
- Hamanaka, R.B.; Chandel, N.S. Mitochondrial reactive oxygen species regulate hypoxic signaling. Curr. Opin. Cell. Biol. 2009, 21, 894–899. [Google Scholar] [CrossRef]
- Vanderhaeghen, T.; Vandewalle, J.; Libert, C. Hypoxia-inducible factors in metabolic reprogramming during sepsis. FEBS J. 2020, 287, 1478–1495. [Google Scholar] [CrossRef]
- Peyssonnaux, C.; Datta, V.; Cramer, T.; Doedens, A.; Theodorakis, E.A.; Gallo, R.L.; Hurtado-Ziola, N.; Nizet, V.; Johnson, R.S. HIF-1α expression regulates the bactericidal capacity of phagocytes. J. Clin. Investig. 2005, 115, 1806–1815. [Google Scholar] [CrossRef] [PubMed]
- Nishi, K.; Oda, T.; Takabuchi, S.; Oda, S.; Fukuda, K.; Adachi, T.; Semenza, G.L.; Shingu, K.; Hirota, K. LPS induces hypoxia-inducible factor 1 activation in macrophage-differentiated cells in a reactive oxygen species-dependent manner. Antioxid. Redox Signal. 2008, 10, 983–995. [Google Scholar] [CrossRef]
- Frede, S.; Stockmann, C.; Freitag, P.; Fandrey, J. Bacterial lipopolysaccharide induces HIF-1 activation in human monocytes via p44/42 MAPK and NF-Κb. Biochem. J. 2006, 396, 517–527. [Google Scholar] [CrossRef]
- Regueira, T.; Lepper, P.M.; Brandt, S.; Ochs, M.; Vuda, M.; Takala, J.; Jakob, S.M.; Djafarzadeh, S. Hypoxia inducible factor-1αinduction by tumour necrosis factor-α, but not by toll-like receptor agonists, modulates cellular respiration in cultured human hepatocytes. Liver Int. 2009, 29, 1582–1592. [Google Scholar] [CrossRef]
- Yang, L.; Xie, M.; Yang, M.; Yu, Y.; Zhu, S.; Hou, W.; Kang, R.; Lotze, M.T.; Billiar, T.R.; Wang, H.; et al. PKM2 regulates the Warburg effect and promotes HMGB1 release in sepsis. Nat. Commun. 2014, 5, 4436. [Google Scholar] [CrossRef]
- Warburg, O. The metabolism of carcinoma cells 1. J. Cancer Res. 1925, 9, 148–163. [Google Scholar] [CrossRef]
- Chance, B. Was Warburg right? Or was it that simple? Biol. Ther. 2004, 4, 132–133. [Google Scholar] [CrossRef]
- Bar-Or, D.; Carrick, M.; Tanner, A.; Lieser, M.J.; Rael, L.T.; Brody, E. Overcoming the Warburg Effect: Is it the key to survival in sepsis? J. Crit. Care 2018, 43, 197–201. [Google Scholar] [CrossRef]
- Clemens, M.G.; Chaudry, I.H.; McDermott, P.H.; Baue, A.E. Regulation of glucose production from lactate in experimental sepsis. Am. J. Physiol. Regul. Integr. Comp. Physiol. 1983, 244, R794–R800. [Google Scholar] [CrossRef]
- Jones, G.R. Ionic shuttles in shock. Lancet 1974, 1, 905. [Google Scholar] [CrossRef]
- Leverve, X.M. Derangements in Cellular Oxygen Metabolism; Springer: Berlin/Heidelberg, Germany, 2002; pp. 52–68. [Google Scholar]
- Nichol, A.D.; Egi, M.; Pettila, V.; Bellomo, R.; French, C.; Hartm, G.; Davies, A.; Stachowski, E.; Reade, M.C.; Bailey, M.; et al. Relative hyperlactatemia and hospital mortality in critically ill patients: A retrospective multi-centre study. Crit. Care 2010, 14, R25. [Google Scholar] [CrossRef]
- Rishu, H.; Khan, R.; Al-Dorzi, H.M.; Tamim, H.M.; Al-Qahtani, S.; Al-Ghamdi, G.; Arabi, Y.M. Even Mild Hyperlactatemia Is Associated with Increased Mortality in Critically Ill Patients. Crit. Care 2013, 17, R197. [Google Scholar] [CrossRef]
- Samuvel, D.J.; Sundararaj, K.P.; Nareika, A.; Lopes-Virella, M.F.; Huang, Y. Lactate Boosts TLR4 Signaling and NF-κB Pathway-Mediated Gene Transcription in Macrophages via Monocarboxylate Transporters and MD-2 Up-Regulation. J. Immunol. 2009, 182, 2476–2484. [Google Scholar] [CrossRef]
- Drechsler, S.; Weixelbaumer, K.M.; Weidinger, A.; Raeven, P.; Khadem, A.; Redl, H.; van Griensven, M.; Bahrami, S.; Remick, D.; Kozlov, A.; et al. Why do they die? Comparison of selected aspects of organ injury and dysfunction in mice surviving and dying in acute abdominal sepsis. Intensive Care Med. Exp. 2015, 3, 1–21. [Google Scholar] [CrossRef]
- Miller, S.I.; Wallace, R.J.; Musher, D.M.; Septimus, E.J.; Kohl, S.; Baughn, R.E. Hypoglycemia as a manifestation of sepsis. Am. J. Med. 1980, 68, 649–654. [Google Scholar] [CrossRef]
- Romijn, J.A.; Godfried, M.H.; Wortel, C.; Sauerwein, H.P. Hypoglycemia, hormones and cytokines in fatal meningococcal septicemia. J. Endocrinol. Investig. 1990, 13, 743–747. [Google Scholar] [CrossRef]
- Dendoncker, K.; Libert, C. Glucocorticoid resistance as a major drive in sepsis pathology. Cytokine Growth Factor Rev. 2017, 35, 85–96. [Google Scholar] [CrossRef] [PubMed]
- Weis, S.; Carlos, A.R.; Moita, M.R.; Singh, S.; Blankenhaus, B.; Cardoso, S.; Larsen, R.; Rebelo, S.; Schäuble, S.; Del Barrio, L.; et al. Metabolic Adaptation Establishes Disease Tolerance to Sepsis. Cell 2017, 169, 1263–1275. [Google Scholar] [CrossRef]
- Wang, A.; Huen, S.C.; Luan, H.H.; Yu, S.; Zhang, C.; Gallezot, J.D.; Booth, C.J.; Medzhitov, R. Opposing Effects of Fasting Metabolism on Tissue Tolerance in Bacterial and Viral Inflammation. Cell 2016, 166, 1512–1525.e12. [Google Scholar] [CrossRef] [PubMed]
- Chervonsky, V. Just a Spoonful of Sugar Helps the Tolerance Go Up. Cell 2017, 169, 1170–1172. [Google Scholar] [CrossRef][Green Version]
- Gunst, J.; van den Berghe, G. Blood glucose control in the ICU: Don’t throw out the baby with the bathwater! Intensive Care Med. 2016, 42, 1478–1481. [Google Scholar] [CrossRef]
- Singanayagam, A.; Chalmers, J.D.; Hill, A.T. Admission hypoglycaemia is associated with adverse outcome in community-acquired pneumonia. Eur. Respir. J. 2009, 34, 932–939. [Google Scholar] [CrossRef] [PubMed]
- Krinsley, J.S.; Schultz, M.J.; Spronk, P.E.; Harmsen, R.E.; van Braam Houckgeest, F.; van der Sluijs, J.P.; Mélot, C.; Preiser, J.C. Mild hypoglycemia is independently associated with increased mortality in the critically ill. Crit. Care 2011, 15, R173. [Google Scholar] [CrossRef]
- Kalra, S.; Mukherjee, J.J.; Venkataraman, S.; Bantwal, G.; Shaikh, S.; Saboo, B.; Das, A.K.; Ramachandran, A. Hypoglycemia: The neglected complication. Indian J. Endocrinol. Metab. 2013, 17, 819. [Google Scholar] [CrossRef]
- van den Berghe, G.; Wouters, P.; Weekers, F.; Verwaest, C.; Bruyninckx, F.; Schetz, M.; Vlasselaers, D.; Ferdinande, P.; Lauwers, P.; Bouillon, R. Intensive insulin therapy in critically ill patients. N. Engl. J. Med. 2001, 345, 1359–1367. [Google Scholar] [CrossRef]
- van den Berghe, G.; Wilmer, A.; Hermans, G.; Meersseman, W.; Wouters, P.J.; Milants, I.; Van Wijngaerden, E.; Bobbaers, H.; Bouillon, R. Intensive insulin therapy in the medical ICU. N. Engl. J. Med. 2006, 354, 449–461. [Google Scholar] [CrossRef] [PubMed]
- Vlasselaers, D.; Milants, I.; Desmet, L.; Wouters, P.J.; Vanhorebeek, I.; van den Heuvel, I.; Mesotten, D.; Casaer, M.P.; Meyfroidt, G.; Ingels, C.; et al. Intensive insulin therapy for patients in paediatric intensive care: A prospective, randomised controlled study. Lancet 2009, 373, 547–556. [Google Scholar] [CrossRef]
- Ling, Y.; Li, X.; Gao, X. Intensive versus conventional glucose control in critically ill patients: A meta-analysis of randomized controlled trials. Eur. J. Intern. Med. 2012, 23, 564–574. [Google Scholar] [CrossRef] [PubMed]
- Finfer, S.; Chittock, D.R.; Su, S.Y.; Blair, D.; Foster, D.; Dhingra, V.; Bellomo, R.; Cook, D.; Dodek, P.; Henderson, W.R.; et al. Intensive versus Conventional Glucose Control in Critically Ill Patients. N. Engl. J. Med. 2009, 360, 1283–1297. [Google Scholar] [CrossRef]
- Botham, K.M.; Mayes, P.A. Lipid Transport & Storage. In Harper’s Illustrated Biochemistry, 31e; Rodwell, V.W., Bender, D.A., Botham, K.M., Kennelly, P.J., Weil, P.A., Eds.; McGraw-Hill Education: New York, NY, USA, 2018. [Google Scholar]
- Botham, K.M.; Mayes, P.A. Oxidation of Fatty Acids: Ketogenesis. In Harper’s Illustrated Biochemistry, 31e; Rodwell, V.W., Bender, D.A., Botham, K.M., Kennelly, P.J., Weil, P.A., Eds.; McGraw-Hill Education: New York, NY, USA, 2018. [Google Scholar]
- Ilias, I.; Vassiliadi, D.A.; Theodorakopoulou, M.; Boutati, E.; Maratou, E.; Mitrou, P.; Nikitas, N.; Apollonatou, S.; Dimitriadis, G.; Armaganidis, A.; et al. Adipose tissue lipolysis and circulating lipids in acute and subacute critical illness: Effects of shock and treatment. J. Crit. Care 2014, 29, 1130.e5–1130.e9. [Google Scholar] [CrossRef]
- Rittig, N.; Bach, E.; Thomsen, H.H.; Pedersen, S.B.; Nielsen, T.S.; Jørgensen, J.O.; Jessen, N.; Møller, N. Regulation of lipolysis and adipose tissue signaling during acute endotoxin-induced inflammation: A human randomized crossover trial. PLoS ONE 2016, 11, e0162167. [Google Scholar] [CrossRef] [PubMed]
- Forse, R.A.; Leibel, R.; Askanazi, J.; Hirsch, J.; Kinney, J.M. Adrenergic control of adipocyte lipolysis in trauma and sepsis. Ann. Surg. 1987, 206, 744–751. [Google Scholar] [CrossRef]
- Wellhoener, P.; Vietheer, A.; Sayk, F.; Schaaf, B.; Lehnert, H.; Dodt, C. Metabolic alterations in adipose tissue during the early phase of experimental endotoxemia in humans. Horm. Metab. Res. 2011, 43, 754–759. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.M.; Tucker, D.F.; Gross, D.N.; Easton, R.M.; DiPilato, L.M.; Dean, A.S.; Monks, B.R.; Birnbaum, M.J. Insulin Regulates Adipocyte Lipolysis via an Akt-Independent Signaling Pathway. Mol. Cell. Biol. 2010, 30, 5009–5020. [Google Scholar] [CrossRef] [PubMed]
- Wendel, M.; Paul, R.; Heller, A.R. Lipoproteins in inflammation and sepsis. II. Clinical aspects. Intensive Care Med. 2007, 33, 25–35. [Google Scholar] [CrossRef] [PubMed]
- Rosato, E.F.; Vemulapalli, P.; Lang, C.H.; Lanza-Jacoby, S. Insulin Stimulates Lipoprotein Lipase Activity and Synthesis in Adipocytes from Septic Rats. J. Surg. Res. 1997, 73, 73–79. [Google Scholar] [CrossRef]
- Scholl, A.; Lang, C.H.; Bagby, G.J. Hypertriglyceridemia and its relation to tissue lipoprotein lipase activity in endotoxemic, Escherichia coli bacteremic, and polymicrobial septic rats. J. Surg. Res. 1984, 37, 394–401. [Google Scholar] [CrossRef]
- Lanza-Jacoby, S.; Tabares, A. Triglyceride kinetics, tissue lipoprotein lipase, and liver lipogenesis in septic rats. Am. J. Physiol. Endocrinol. Metab. 1990, 258, E678–E685. [Google Scholar] [CrossRef] [PubMed]
- Nogueira, A.C.; Kawabatam, V.; Biselli, P.; Lins, M.H.; Valeri, C.; Seckler, M.; Hoshino, W.; Júnior, L.G.; Bernik, M.M.; de Andrade Machado, J.B.; et al. Changes in plasma free fatty acid levels in septic patients are associated with cardiac damage and reduction in heart rate variability. Shock 2008, 29, 342–348. [Google Scholar] [CrossRef]
- Feingold, R.; Grunfeld, C. Tumor necrosis factor-alpha stimulates hepatic lipogenesis in the rat in vivo. J. Clin. Investig. 1987, 80, 184–190. [Google Scholar] [CrossRef] [PubMed]
- Nonogaki, K.; Fuller, G.M.; Fuentes, N.L.; Moser, A.H.; Staprans, I.; Grunfeld, C.; Feingold, K.R. Interleukin-6 stimulates hepatic triglyceride secretion in rats. Endocrinology 1995, 136, 2143–2149. [Google Scholar] [CrossRef] [PubMed]
- Askanazi, J.; Carpentier, Y.A.; Elwyn, D.H.; Nordenström, J.; Jeevanandam, M.; Rosenbaum, S.H.; Gump, F.E.; Kinney, J.M. Influence of total parenteral nutrition on fuel utilization in injury and sepsis. Ann. Surg. 1980, 191, 40–46. [Google Scholar] [CrossRef]
- Nordenstrom, J.; Carpentier, Y.A.; Askanazi, J.; Robin, A.P.; Elwyn, D.H.; Hensle, T.W.; Kinney, J.M. Metabolic utilization of intravenous fat emulsion during total parenteral nutrition. Ann. Surg. 1982, 196, 221–231. [Google Scholar] [CrossRef]
- Hiukka, A.; Maranghi, M.; Matikainen, N.; Taskinen, M.R. PPARα: An emerging therapeutic target in diabetic microvascular damage. Nat. Rev. Endocrinol. 2010, 6, 454–463. [Google Scholar] [CrossRef]
- Wong, H.R.; Cvijanovich, N.; Allen, G.L.; Lin, R.; Anas, N.; Meyer, K.; Freishtat, R.J.; Monaco, M.; Odoms, K.; Sakthivel, B.; et al. Genomic expression profiling across the pediatric systemic inflammatory response syndrome, sepsis, and septic shock spectrum. Crit. Care Med. 2009, 37, 1558–1566. [Google Scholar] [CrossRef] [PubMed]
- Drosatos, K.; Drosatos-Tampakaki, Z.; Khan, R.; Homma, S.; Schulze, P.C.; Zannis, V.I.; Goldberg, I.J. Inhibition of c-Jun-N-terminal kinase increases cardiac peroxisome proliferator-activated receptor α expression and fatty acid oxidation and prevents lipopolysaccharide-induced heart dysfunction. J. Biol. Chem. 2011, 286, 36331–36339. [Google Scholar] [CrossRef] [PubMed]
- Randle, P.J.; Garland, P.B.; Hales, C.N.; Newsholme, E.A. The glucose fatty-acid cycle. Its role in insulin sensitivity and the metabolic disturbances of diabetes mellitus. Lancet 1963, 281, 785–789. [Google Scholar] [CrossRef]
- Engin, A.B. What is lipotoxicity? In Advances in Experimental Medicine and Biology; Engin, A.B., Engin, A., Eds.; Springer: New York, NY, USA, 2017; Volume 960, pp. 197–220. [Google Scholar]
- Zager, A.; Johnson, A.C.M.; Hanson, S.Y. Renal tubular triglyercide accumulation following endotoxic, toxic, and ischemic injury. Kidney Int. 2005, 67, 111–121. [Google Scholar] [CrossRef]
- Rossi, A.; Celes, M.R.N.; Prado, C.M.; Saggioro, F.P. Myocardial structural changes in long-term human severe sepsis/septic shock may be responsible for cardiac dysfunction. Shock 2007, 27, 10–18. [Google Scholar] [CrossRef]
- Koskinas, J.; Gomatos, I.P.; Tiniakos, D.G.; Memos, N.; Boutsikou, M.; Garatzioti, A.; Archimandritis, A.; Betrosian, A. Liver histology in ICU patients dying from sepsis: A clinico-pathological study. World J. Gastroenterol. 2008, 14, 1389–1393. [Google Scholar] [CrossRef] [PubMed]
- D’Souza, K.; Nzirorera, C.; Kienesberger, P.C. Lipid metabolism and signaling in cardiac lipotoxicity. Biochim. Biophys. Acta Mol. Cell Biol. Lipids 2016, 1861, 1513–1524. [Google Scholar] [CrossRef] [PubMed]
- Bugger, H.; Abel, E.D. Molecular mechanisms for myocardial mitochondrial dysfunction in the metabolic syndrome. Clin. Sci. 2008, 114, 195–210. [Google Scholar] [CrossRef]
- Yang, R.; Barouch, L.A. Leptin signaling and obesity: Cardiovascular consequences. Circ. Res. 2007, 101, 545–559. [Google Scholar] [CrossRef]
- Unger, R.H.; Orci, L. Lipoapoptosis: Its mechanism and its diseases. Biochim. Biophys. Acta 2002, 1585, 202–212. [Google Scholar] [CrossRef]
- Linkermann, A.; Skouta, R.; Himmerkus, N.; Mulay, S.R.; Dewitz, C.; De Zen, F.; Prokai, A.; Zuchtriegel, G.; Krombach, F.; Welz, P.S.; et al. Synchronized renal tubular cell death involves ferroptosis. Proc. Natl. Acad. Sci. USA 2014, 111, 16836–16841. [Google Scholar] [CrossRef] [PubMed]
- Müller, T.; Dewitz, C.; Schmitz, J.; Schröder, A.S.; Bräsen, J.H.; Stockwell, B.R.; Murphy, J.M.; Kunzendorf, U.; Krautwald, S. Necroptosis and ferroptosis are alternative cell death pathways that operate in acute kidney failure. Cell. Mol. Life Sci. 2017, 74, 3631–3645. [Google Scholar] [CrossRef]
- Wenzel, S.E.; Tyurina, Y.Y.; Zhao, J.; St Croix, C.M.; Dar, H.H.; Mao, G.; Tyurin, V.A.; Anthonymuthu, T.S.; Kapralov, A.A.; Amoscato, A.A.; et al. PEBP1 Wardens Ferroptosis by Enabling Lipoxygenase Generation of Lipid Death Signals. Cell 2017, 171, 628–641. [Google Scholar] [CrossRef]
- Randle, P.J.; Newsholme, E.A.; Garland, P.B. Regulation of glucose uptake by muscle. 8. Effects of fatty acids, ketone bodies and pyruvate, and of alloxan-diabetes and starvation, on the uptake and metabolic fate of glucose in rat heart and diaphragm muscles. Biochem. J. 1964, 93, 652–665. [Google Scholar] [CrossRef]
- Plank, L.D.; Hill, G.L. Sequential metabolic changes following induction of systemic inflammatory response in patients with severe sepsis or major blunt trauma. World J. Surg. 2000, 24, 630–638. [Google Scholar] [CrossRef]
- Vary, C.; Kimball, S.R. Sepsis-induced changes in protein synthesis: Differential effects on fast- and slow-twitch muscles. Am. J. Physiol. Cell Physiol. 1992, 262, C1513–C1519. [Google Scholar] [CrossRef]
- Hummel, R.P., III; Hasselgren, P.O.; James, J.H.; Warner, B.W.; Fischer, J.E. The effect of sepsis in rats on skeletal muscle protein synthesis in vivo and in periphery and central core of incubated muscle preparations in vitro. Metabolism 1988, 37, 1120–1127. [Google Scholar] [CrossRef]
- Hasselgren, P.O.; James, J.H.; Benson, D.W.; Hall-Angerås, M.; Angerås, U.; Hiyama, D.T.; Li, S.; Fischer, J.E. Total and myofibrillar protein breakdown in different types of rat skeletal muscle: Effects of sepsis and regulation by insulin. Metabolism 1989, 38, 634–640. [Google Scholar] [CrossRef]
- Long, L.; Birkhahn, R.H.; Geiger, J.W.; Betts, J.E.; Schiller, W.R.; Blakemore, W.S. Urinary excretion of 3-methylhistidine: An assessment of muscle protein catabolism in adult normal subjects and during malnutrition, sepsis, and skeletal trauma. Metabolism 1981, 30, 765–776. [Google Scholar] [CrossRef]
- Jepson, M.; Bates, P.C.; Broadbent, P.; Pell, J.M.; Millward, D.J. Relationship between glutamine concentration and protein synthesis in rat skeletal muscle. Am. J. Physiol. Endocrinol. Metab. 1988, 255, E166–E172. [Google Scholar] [CrossRef]
- Bruins, M.J.; Deutz, N.E.P.; Soeters, P.B. Aspects of organ protein, amino acid and glucose metabolism in a porcine model of hypermetabolic sepsis. Clin. Sci. 2003, 104, 127–141. [Google Scholar] [CrossRef]
- Druml, W.; Heinzel, G.; Kleinberger, G. Amino acid kinetics in patients with sepsis. Am. J. Clin. Nutr. 2001, 73, 908–913. [Google Scholar] [CrossRef]
- Su, L.; Li, H.; Xie, A.; Liu, D.; Rao, W.; Lan, L.; Li, X.; Li, F.; Xiao, K.; Wang, H.; et al. Dynamic changes in amino acid concentration profiles in patients with sepsis. PLoS ONE 2015, 10, e0121933. [Google Scholar] [CrossRef] [PubMed]
- Hall-Angerås, M.; Angerås, U.; Zamir, O.; Hasselgren, P.O.; Fischer, J.E. Effect of the glucocorticoid receptor antagonist RU 38486 on muscle protein breakdown in sepsis. Surgery 1991, 109, 468–473. [Google Scholar] [PubMed]
- Langouche, L.; Vanhorebeek, I.; van den Berghe, G. The role of insulin therapy in critically ill patients. Treat. Endocrinol. 2005, 4, 353–360. [Google Scholar] [CrossRef] [PubMed]
- Bailey, J.L.; Wang, X.; England, B.K.; Price, S.R.; Ding, X.; Mitch, W.E. The acidosis of chronic renal failure activates muscle proteolysis in rats by augmenting transcription of genes encoding proteins of the ATP-dependent ubiquitin-proteasome pathway. J. Clin. Investig. 1996, 97, 1447–1453. [Google Scholar] [CrossRef]
- Lang, H.; Frost, R.A.; Vary, T.C. Regulation of muscle protein synthesis during sepsis and inflammation. Am. J. Physiol. Endocrinol. Metab. 2007, 292, E1497–E1506. [Google Scholar] [CrossRef]
- Rosenblatt, S.; Clowes, G.H.A.; George, B.C.; Hirsch, E.; Lindberg, B. Exchange of Amino Acids by Muscle and Liver in Sepsis: Comparative Studies In Vivo and In Vitro. Arch. Surg. 1983, 118, 167–175. [Google Scholar] [CrossRef]
- Sax, H.C.; Talamini, M.A.; Hasselgren, P.O.; Rosenblum, L.; Ogle, C.K.; Fischer, J.E. Increased synthesis of secreted hepatic proteins during abdominal sepsis. J. Surg. Res. 1988, 44, 109–116. [Google Scholar] [CrossRef]
- Windmueller, H.G.; Spaeth, A.E. Respiratory fuels and nitrogen metabolism in vivo in small intestine of fed rats. Quantitative importance of glutamine, glutamate, and aspartate. J. Biol. Chem. 1980, 255, 107–112. [Google Scholar] [CrossRef]
- Newsholme, A.; Parry-Billings, M. Properties of Glutamine Release from Muscle and Its Importance for the Immune System. J. Parenter. Enter. Nutr. 1990, 14, 63S–67S. [Google Scholar] [CrossRef] [PubMed]
- Rohde, T.; Ullum, H.; Rasmussen, J.P.; Kristensen, J.H.; Newsholme, E.; Pedersen, B.K. Effects of glutamine on the immune system: Influence of muscular exercise and HIV infection. J. Appl. Physiol. 1995, 79, 146–150. [Google Scholar] [CrossRef] [PubMed]
- Clowes, G.H.A.; George, B.C.; Villee, C.A.; Saravis, C.A. Muscle Proteolysis Induced by a Circulating Peptide in Patients with Sepsis or Trauma. N. Engl. J. Med. 1983, 308, 545–552. [Google Scholar] [CrossRef] [PubMed]
- Nesseler, N.; Launey, Y.; Aninat, C.; Morel, F.; Mallédant, Y.; Seguin, P. Clinical review: The liver in sepsis. Crit. Care 2012, 16, 235. [Google Scholar] [CrossRef]
- Felipo, V.; Butterworth, R.F. Neurobiology of ammonia. Prog. Neurobiol. 2002, 67, 259–279. [Google Scholar] [CrossRef]
- Heidegger, P.; Berger, M.M.; Graf, S.; Zingg, W.; Darmon, P.; Costanza, M.C.; Thibault, R.; Pichard, C. Optimisation of energy provision with supplemental parenteral nutrition in critically ill patients: A randomised controlled clinical trial. Lancet 2013, 381, 385–393. [Google Scholar] [CrossRef]
- Singer, P.; Blaser, A.R.; Berger, M.M.; Alhazzani, W.; Calder, P.C.; Casaer, M.P.; Hiesmayr, M.; Mayer, K.; Montejo, J.C.; Pichard, C.; et al. ESPEN Guideline ESPEN guideline on clinical nutrition in the intensive care unit. Clin. Nutr. 2019, 38, 48–79. [Google Scholar] [CrossRef]
- Reitsema, V.A.; Star, B.S.; de Jager, V.D.; van Meurs, M.; Henning, R.H.; Bouma, H.R. Metabolic Resuscitation Strategies to Prevent Organ Dysfunction in Sepsis. Antioxid. Redox Signal. 2019, 31, 134–152. [Google Scholar] [CrossRef] [PubMed]
- Sanfilippo, F.; Santonocito, C.; Morelli, A.; Foex, P. Beta-blocker use in severe sepsis and septic shock: A systematic review. Curr. Med. Res. Opin. 2015, 31, 1817–1825. [Google Scholar] [CrossRef]
- Wasyluk, W.; Zwolak, A. PARP Inhibitors: An Innovative Approach to the Treatment of Inflammation and Metabolic Disorders in Sepsis. J. Inflamm. Res. 2021, 14, 1827–1844. [Google Scholar] [CrossRef] [PubMed]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wasyluk, W.; Zwolak, A. Metabolic Alterations in Sepsis. J. Clin. Med. 2021, 10, 2412. https://doi.org/10.3390/jcm10112412
Wasyluk W, Zwolak A. Metabolic Alterations in Sepsis. Journal of Clinical Medicine. 2021; 10(11):2412. https://doi.org/10.3390/jcm10112412
Chicago/Turabian StyleWasyluk, Weronika, and Agnieszka Zwolak. 2021. "Metabolic Alterations in Sepsis" Journal of Clinical Medicine 10, no. 11: 2412. https://doi.org/10.3390/jcm10112412
APA StyleWasyluk, W., & Zwolak, A. (2021). Metabolic Alterations in Sepsis. Journal of Clinical Medicine, 10(11), 2412. https://doi.org/10.3390/jcm10112412





