Prognostic Factors to Predict ICU Mortality in Patients with Severe ARDS Who Received Early and Prolonged Prone Positioning Therapy
Abstract
1. Introduction
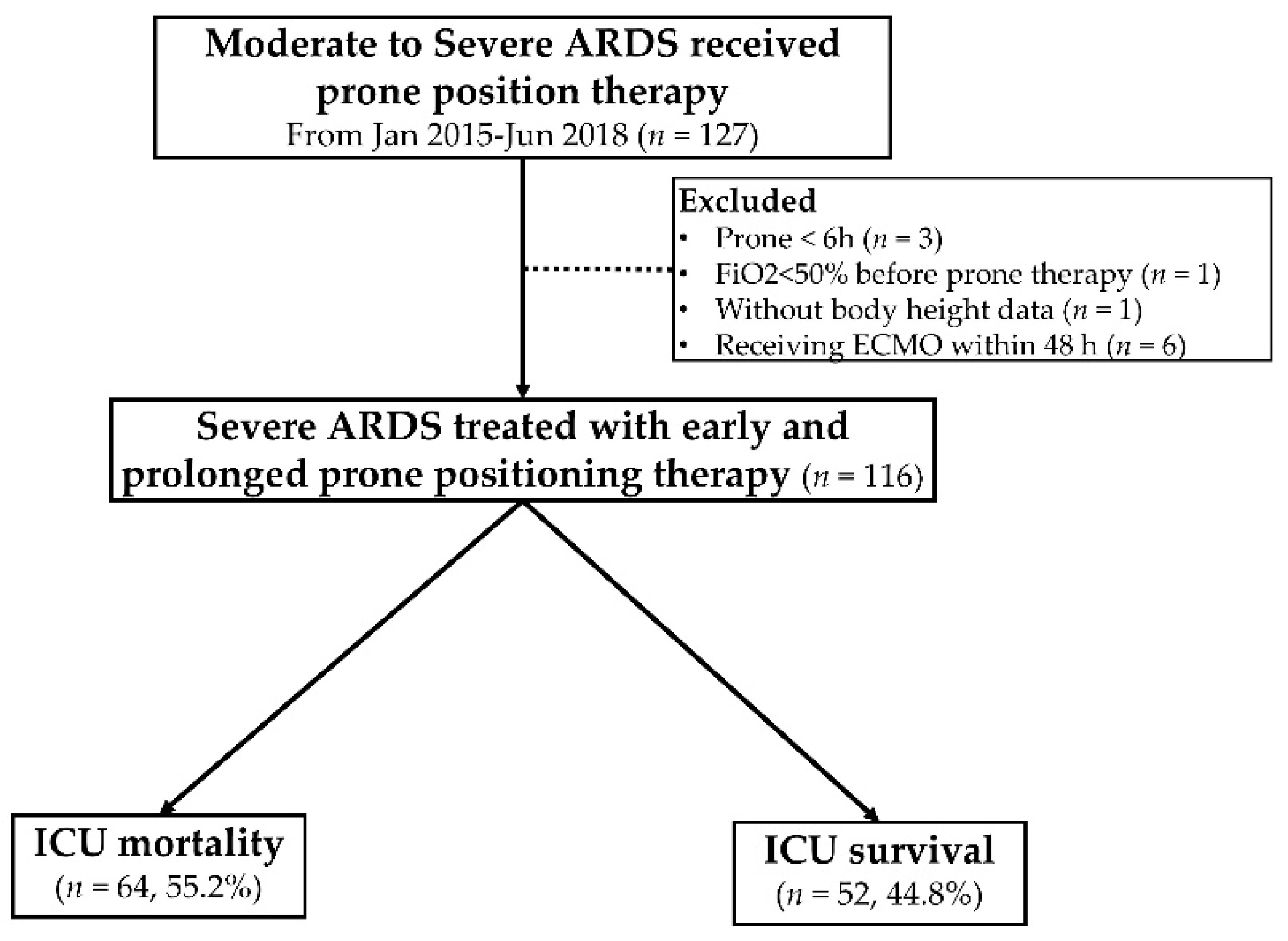
2. Materials and Methods
2.1. Study Design and Patients
2.2. Mechanical Ventilator Setting, Recruitment Maneuver, and Protocol of PP Therapy
2.3. Data Collection, Assessment, and Outcome Measures
2.4. Statistical Analysis
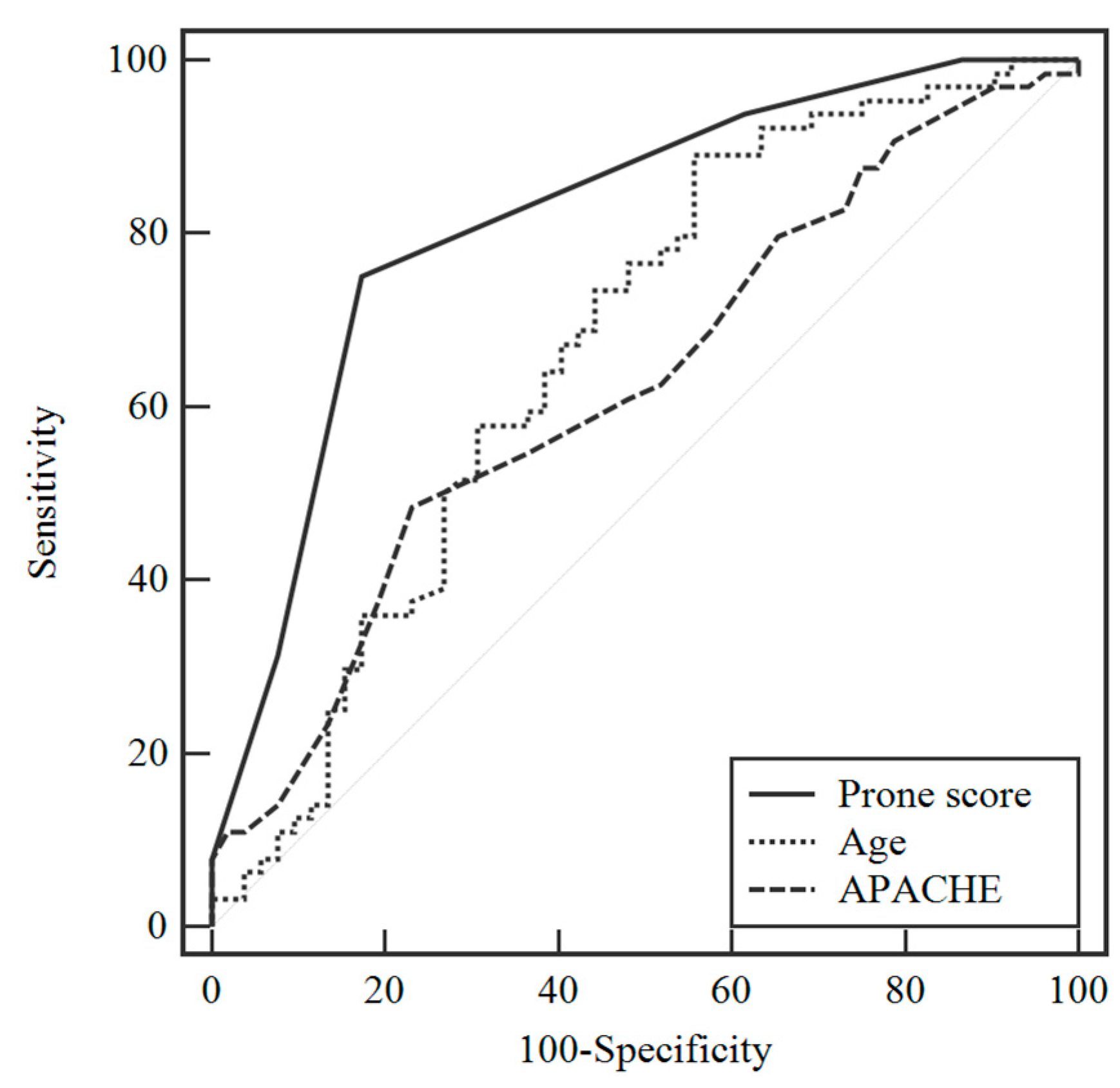
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bellani, G.; Laffey, J.G.; Pham, T.; Fan, E.; Brochard, L.; Esteban, A.; Gattinoni, L.; Van Haren, F.; Larsson, A.; McAuley, D.F.; et al. Epidemiology, Patterns of Care, and Mortality for Patients with Acute Respiratory Distress Syndrome in Intensive Care Units in 50 Countries. JAMA 2016, 315, 788–800. [Google Scholar] [CrossRef] [PubMed]
- Bos, L.D.; Martin-Loeches, I.; Schultz, M.J. ARDS: Challenges in patient care and frontiers in research. Eur. Respir. Rev. 2018, 27, 170107. [Google Scholar] [CrossRef]
- Rilinger, J.; Zotzmann, V.; Bemtgen, X.; Schumacher, C.; Biever, P.M.; Duerschmied, D.; Kaier, K.; Stachon, P.; Mühlen, C.V.Z.; Zehender, M.; et al. Prone positioning in severe ARDS requiring extracorporeal membrane oxygenation. Crit. Care 2020, 24, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Howell, M.D.; Davis, A.M. Management of ARDS in Adults. JAMA 2018, 319, 711–712. [Google Scholar] [CrossRef] [PubMed]
- Scholten, E.L.; Beitler, J.R.; Prisk, G.K.; Malhotra, A. Treatment of ARDS With Prone Positioning. Chest 2017, 151, 215–224. [Google Scholar] [CrossRef]
- Piehl, M.A.; Brown, R.S. Use of extreme position changes in acute respiratory failure. Crit. Care Med. 1976, 4, 13–14. [Google Scholar] [CrossRef] [PubMed]
- Guérin, C.; Reignier, J.; Richard, J.-C.; Beuret, P.; Gacouin, A.; Boulain, T.; Mercier, E.; Badet, M.; Mercat, A.; Baudin, O.; et al. Prone Positioning in Severe Acute Respiratory Distress Syndrome. N. Engl. J. Med. 2013, 368, 2159–2168. [Google Scholar] [CrossRef]
- Demory, D.; Michelet, P.; Arnal, J.-M.; Donati, S.; Forel, J.-M.; Gainnier, M.; Brégeon, F.; Papazian, L. High-frequency oscillatory ventilation following prone positioning prevents a further impairment in oxygenation. Crit. Care Med. 2007, 35, 106–111. [Google Scholar] [CrossRef]
- Mancebo, J.; Fernández, R.; Blanch, L.; Rialp, G.; Gordo, F.; Ferrer, M.; Rodríguez, F.; Garro, P.; Ricart, P.; Vallverdú, I.; et al. A Multicenter Trial of Prolonged Prone Ventilation in Severe Acute Respiratory Distress Syndrome. Am. J. Respir. Crit. Care Med. 2006, 173, 1233–1239. [Google Scholar] [CrossRef] [PubMed]
- Voggenreiter, G.; Aufmkolk, M.; Stiletto, R.J.; Baacke, M.G.; Waydhas, C.; Ose, C.; Bock, E.; Gotzen, L.; Obertacke, U.; Nast-Kolb, D. Prone Positioning Improves Oxygenation in Post-Traumatic Lung Injury—A Prospective Randomized Trial. J. Trauma Inj. Infect. Crit. Care 2005, 59, 333–343. [Google Scholar] [CrossRef] [PubMed]
- Papazian, L.; Gainnier, M.; Marin, V.; Donati, S.; Arnal, J.-M.; Demory, D.; Roch, A.; Forel, J.-M.; Bongrand, P.; Brégeon, F.; et al. Comparison of prone positioning and high-frequency oscillatory ventilation in patients with acute respiratory distress syndrome. Crit. Care Med. 2005, 33, 2162–2171. [Google Scholar] [CrossRef]
- Curley, M.A.Q.; Hibberd, P.L.; Fineman, L.D.; Wypij, D.; Shih, M.-C.; Thompson, J.E.; Grant, M.J.C.; Barr, F.E.; Cvijanovich, N.Z.; Sorce, L.; et al. Effect of Prone Positioning on Clinical Outcomes in Children with Acute Lung Injury. JAMA 2005, 294, 229–237. [Google Scholar] [CrossRef] [PubMed]
- Guerin, C.; Gaillard, S.; Lemasson, S.; Ayzac, L.; Girard, R.; Beuret, P.; Palmier, B.; Le, Q.V.; Sirodot, M.; Rosselli, S.; et al. Effects of Systematic Prone Positioning in Hypoxemic Acute Respiratory Failure. JAMA 2004, 292, 2379–2387. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, I.; Fujihara, H.; Sato, K.; Honda, T.; Ohashi, S.; Endoh, H.; Yamakura, T.; Taga, K.; Shimoji, K. Beneficial effect of a prone position for patients with hypoxemia after transthoracic esophagectomy. Crit. Care Med. 2002, 30, 1799–1802. [Google Scholar] [CrossRef] [PubMed]
- Beuret, P.; Carton, M.-J.; Nourdine, K.; Kaaki, M.; Tramoni, G.; Ducreux, J.-C. Prone position as prevention of lung injury in comatose patients: A prospective, randomized, controlled study. Intensive Care Med. 2002, 28, 564–569. [Google Scholar] [CrossRef] [PubMed]
- Gattinoni, L.; Tognoni, G.; Pesenti, A.; Taccone, P.; Mascheroni, D.; Labarta, V.; Malacrida, R.; Di Giulio, P.; Fumagalli, R.; Pelosi, P.; et al. Effect of Prone Positioning on the Survival of Patients with Acute Respiratory Failure. N. Engl. J. Med. 2001, 345, 568–573. [Google Scholar] [CrossRef]
- Taccone, P.; Pesenti, A.; Latini, R.; Polli, F.; Vagginelli, F.; Mietto, C.; Caspani, L.; Raimondi, F.; Bordone, G.; Iapichino, G.; et al. Prone Positioning in Patients With Moderate and Severe Acute Respiratory Distress Syndrome. JAMA 2009, 302, 1977–1984. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, R.; Trenchs, X.; Klamburg, J.; Castedo, J.; Serrano, J.M.; Besso, G.; Tirapu, J.P.; Santos, A.; Mas, A.; Parraga, M.; et al. Prone positioning in acute respiratory distress syndrome: A multicenter randomized clinical trial. Intensive Care Med. 2008, 34, 1487–1491. [Google Scholar] [CrossRef]
- Munshi, L.; Del Sorbo, L.; Adhikari, N.K.J.; Hodgson, C.L.; Wunsch, H.; Meade, M.O.; Uleryk, E.; Mancebo, J.; Pesenti, A.; Ranieri, V.M.; et al. Prone Position for Acute Respiratory Distress Syndrome. A Systematic Review and Meta-Analysis. Ann. Am. Thorac. Soc. 2017, 14, S280–S288. [Google Scholar] [CrossRef] [PubMed]
- Park, S.Y.; Kim, H.J.; Yoo, K.H.; Park, Y.B.; Kim, S.W.; Lee, S.J.; Kim, E.K.; Kim, J.H.; Kim, Y.H.; Moon, J.-Y.; et al. The efficacy and safety of prone positioning in adults patients with acute respiratory distress syndrome: A meta-analysis of randomized controlled trials. J. Thorac. Dis. 2015, 7, 356–367. [Google Scholar]
- Sud, S.; Friedrich, J.O.; Adhikari, N.K.J.; Taccone, P.; Mancebo, J.; Polli, F.; Latini, R.; Pesenti, A.; Curley, M.A.; Fernandez, R.; et al. Effect of prone positioning during mechanical ventilation on mortality among patients with acute respiratory distress syndrome: A systematic review and meta-analysis. Can. Med. Assoc. J. 2014, 186, E381–E390. [Google Scholar] [CrossRef]
- Lee, J.M.; Bae, W.; Lee, Y.J.; Cho, Y.-J. The Efficacy and Safety of Prone Positional Ventilation in Acute Respiratory Distress Syndrome. Crit. Care Med. 2014, 42, 1252–1262. [Google Scholar] [CrossRef] [PubMed]
- Beitler, J.R.; Shaefi, S.; Montesi, S.B.; Devlin, A.; Loring, S.H.; Talmor, D.; Malhotra, A. Prone positioning reduces mortality from acute respiratory distress syndrome in the low tidal volume era: A meta-analysis. Intensive Care Med. 2014, 40, 332–341. [Google Scholar] [CrossRef] [PubMed]
- Modrykamien, A.M.; Daoud, Y. Factors among patients receiving prone positioning for the acute respiratory distress syndrome found useful for predicting mortality in the intensive care unit. Bayl. Univ. Med. Cent. Proc. 2018, 31, 1–5. [Google Scholar] [CrossRef][Green Version]
- Kao, K.-C.; TSIRC (Taiwan Severe Influenza Research Consortium); Chang, K.-W.; Chan, M.-C.; Liang, S.-J.; Chien, Y.-C.; Hu, H.-C.; Chiu, L.-C.; Chen, W.-C.; Fang, W.-F.; et al. Predictors of survival in patients with influenza pneumonia-related severe acute respiratory distress syndrome treated with prone positioning. Ann. Intensive Care 2018, 8, 94. [Google Scholar] [CrossRef] [PubMed]
- Girard, R.; Proseva Trial Group; Baboi, L.; Ayzac, L.; Richard, J.-C.; Guérin, C. The impact of patient positioning on pressure ulcers in patients with severe ARDS: Results from a multicentre randomised controlled trial on prone positioning. Intensive Care Med. 2013, 40, 397–403. [Google Scholar] [CrossRef] [PubMed]
- Force, A.D.T.; Ranieri, V.M.; Rubenfeld, G.D.; Thompson, B.T.; Ferguson, N.D.; Caldwell, E.; Fan, E.; Camporota, L.; Slutsky, A.S. Acute Respiratory Distress Syndrome. JAMA 2012, 307, 2526–2533. [Google Scholar] [CrossRef]
- Brower, R.G.; Lanken, P.N.; MacIntyre, N.; Matthay, M.A.; Morris, A.; Ancukiewicz, M.; Schoenfeld, D.; Thompson, B.T.; National Heart, Lung, and Blood Institute ARDS Clinical Trials Network. Higher versus Lower Positive End-Expiratory Pressures in Patients with the Acute Respiratory Distress Syndrome. N. Engl. J. Med. 2004, 351, 327–336. [Google Scholar] [CrossRef]
- Network, A.R.D.S.; Brower, R.G.; Matthay, M.A.; Morris, A.; Schoenfeld, D.; Thompson, B.T.; Wheeler, A. Ventilation with Lower Tidal Volumes as Compared with Traditional Tidal Volumes for Acute Lung Injury and the Acute Respiratory Distress Syndrome. N. Engl. J. Med. 2000, 342, 1301–1308. [Google Scholar] [CrossRef]
- Walkey, A.J.; Del Sorbo, L.; Hodgson, C.L.; Adhikari, N.K.J.; Wunsch, H.; Meade, M.O.; Uleryk, E.; Hess, D.; Talmor, D.S.; Thompson, B.T.; et al. Higher PEEP versus Lower PEEP Strategies for Patients with Acute Respiratory Distress Syndrome. A Systematic Review and Meta-Analysis. Ann. Am. Thorac. Soc. 2017, 14, S297–S303. [Google Scholar] [CrossRef]
- Chan, M.-C.; Hsu, J.-Y.; Liu, H.-H.; Lee, Y.-L.; Pong, S.-C.; Chang, L.-Y.; Kuo, B.I.-T.; Wu, C.-L. Effects of Prone Position on Inflammatory Markers in Patients with ARDS Due to Community-acquired Pneumonia. J. Formos. Med. Assoc. 2007, 106, 708–716. [Google Scholar] [CrossRef]
- Oczenski, W.; Hörmann, C.; Keller, C.; Lorenzl, N.; Kepka, A.; Schwarz, S.; Fitzgerald, R.D. Recruitment maneuvers during prone positioning in patients with acute respiratory distress syndrome. Crit. Care Med. 2005, 33, 54–61. [Google Scholar] [CrossRef]
- Grasso, S.; Terragni, P.; Mascia, L.; Fanelli, V.; Quintel, M.; Herrmann, P.; Hedenstierna, G.; Slutsky, A.S.; Ranieri, V.M. Airway pressure-time curve profile (stress index) detects tidal recruitment/hyperinflation in experimental acute lung injury. Crit. Care Med. 2004, 32, 1018–1027. [Google Scholar] [CrossRef] [PubMed]
- Jochmans, S.; Mazerand, S.; Chelly, J.; Pourcine, F.; Sy, O.; Thieulot-Rolin, N.; Ellrodt, O.; Rochettes, E.M.D.; Michaud, G.; Serbource-Goguel, J.; et al. Duration of prone position sessions: A prospective cohort study. Ann. Intensive Care 2020, 10, 1–9. [Google Scholar] [CrossRef]
- Lim, C.-M.; Kim, E.K.; Lee, J.S.; Shim, T.S.; Lee, S.D.; Koh, Y.; Kim, W.S.; Kim, D.S.; Kim, W.D. Comparison of the response to the prone position between pulmonary and extrapulmonary acute respiratory distress syndrome. Intensive Care Med. 2001, 27, 477–485. [Google Scholar] [CrossRef] [PubMed]
- Rhodes, A.A.; Evans, L.E.; Alhazzani, W.; Levy, M.M.; Antonelli, M.; Ferrer, R.; Kumar, A.; Sevransky, J.E.; Sprung, C.L.; Nunnally, M.E.; et al. Surviving Sepsis Campaign. Crit. Care Med. 2017, 45, 486–552. [Google Scholar] [CrossRef]

| Variables | Median | IQR |
|---|---|---|
| Age (year) | 62.9 | 51.8–74.5 |
| Gender-Male (n, %) | 70 | 60.3% |
| Body mass index (kg/m2) | 24.4 | 21.9–27.9 |
| APACHE II score | 31.0 | 27.0–35.0 |
| Cause of ARDS | ||
| Non-influenza pulmonary ARDS (n, %) | 83 | 71.6% |
| Influenza (n, %) | 20 | 17.2% |
| Extrapulmonary ARDS (n, %) | 13 | 11.2% |
| Renal replacement therapy (n, %) | 52 | 44.8 |
| Comorbidities (n, %) | ||
| Congestive heart failure | 6 | 5.2% |
| Coronary artery disease | 8 | 6.9% |
| Interstitial lung disease | 10 | 5.2% |
| Chronic obstructive lung disease | 40 | 34.5% |
| Diabetes mellitus | 44 | 37.9% |
| Chronic kidney disease | 44 | 37.9% |
| Liver cirrhosis | 10 | 8.6% |
| Autoimmune disease | 18 | 15.5% |
| Malignancy | 23 | 19.8% |
| Prone information | ||
| Timing from ARDS to prone (h) | 18.2 | 8.2–34.0 |
| Total prone duration (h) | 66.1 | 44.2–85.3 |
| PaO2/FiO2 (PF ratio) | 90.8 | 70.5–114.0 |
| Ventilator setting | ||
| Tidal volume (mL/kg) | 6.0 | 5.7–6.5 |
| PEEP (cmH2O) | 14.0 | 14–16 |
| PIP (cmH2O) | 32.0 | 29–35 |
| Pplat (cmH2O) | 29.0 | 26.2–31 |
| Driving pressure (cmH2O) | 13.0 | 11.8–16.2 |
| Compliance (mL/cmH2O) | 25.8 | 21.2–32.8 |
| ICU mortality (n, %) | 64 | 55.2% |
| Characteristics | Alive (n = 52; 44.8%) | Death (n = 64; 55.2%) | p Value |
|---|---|---|---|
| Age (years) | 56.7 (46.1–68.3) | 65.7(57.2–76.3) | 0.002 ** |
| Sex-Male, n (%) | 34 (65.4) | 36 (56.3) | 0.418 |
| BMI (kg/m2) | 25.5 (22.0–28.4) | 24.0 (21.7–27.1) | 0.289 |
| APACHE II score | 30.0 (25.3–32.0) | 32.0 (28.0–35.0) | 0.022 * |
| Cause of ARDS | 0.032 * | ||
| Non-influenza pulmonary ARDS | 31 (59.6%) | 52 (81.3%) | |
| Influenza | 12 (23.1%) | 8 (12.5%) | |
| Extra-pulmonary ARDS | 9 (17.3%) | 4 (6.3%) | |
| Renal replacement therapy | 15 (28.8%) | 37 (57.8%) | 0.003 ** |
| Comorbidity | |||
| Congestive heart failure f | 4 (7.7%) | 2 (3.1%) | 0.406 |
| Coronary artery disease f | 4 (7.7%) | 4 (6.3%) | 1.000 |
| Interstitial lung disease f | 3 (5.8%) | 3 (4.7%) | 1.000 |
| Chronic obstructive lung disease f | 6 (11.5%) | 4 (6.3%) | 0.340 |
| Diabetes mellitus | 22 (42.3%) | 18 (28.1%) | 0.161 |
| Chronic kidney disease | 17 (32.7%) | 27 (42.2%) | 0.392 |
| Liver cirrhosis f | 3 (5.8%) | 7 (10.9%) | 0.508 |
| Autoimmune disease | 7 (13.5%) | 11 (17.2%) | 0.769 |
| Malignancy | 3 (5.8%) | 20 (31.3%) | 0.00 ** |
| Prone information | |||
| Timing from ARDS to prone (h) | 15.6 (7.5–30.6) | 21.3 (9.0–47.8) | 0.084 |
| Total prone duration (h) | 69.3 (51.7–85.4) | 66.1 (34.4–85.3) | 0.170 |
| PaO2/FiO2 (PF ratio) | 93.4 (69.1–119.6) | 88.7 (72.0–112.6) | 0.368 |
| Ventilator setting | |||
| Tidal volume (mL/kg) | 5.9 (5.7–6.3) | 6.2 (5.8–6.6) | 0.088 |
| PEEP (cmH2O) | 16.0 (14.0–16.0) | 14.0 (14.0–16.0) | 0.108 |
| PIP (cmH2O) | 32.0 (29.1–35.0) | 32.5 (29.0–35.0) | 0.953 |
| Pplat (cmH2O) | 28.0 (26.4–30.8) | 29.0 (26.0–31.0) | 0.765 |
| Driving pressure (cmH2O) | 13.0 (11.0–16.5) | 14.0 (12.0–16.6) | 0.349 |
| Compliance (mL/cmH2O) | 26.4 (22.6–33.8) | 25.4 (20.0–30.8) | 0.252 |
| Variables | Univariate Analysis OR (95% CI) | Multivariate Analysis OR (95% CI) |
|---|---|---|
| Age (year) | 1.04 (1.01–1.07) ** | 1.02 (0.99–1.05) |
| APACHE II score | 1.07 (1.01–1.14) ** | 1.05 (0.97–1.14) |
| Cause of ARDS | ||
| Extrapulmonary ARDS | Reference | Reference |
| Non-influenza pulmonary ARDS | 3.78 (1.07–13.29) * | 5.17 (1.16–23.16) * |
| Influenza ARDS | 1.50 (0.34–6.58) | 2.00 (0.36–11.12) |
| Renal replacement therapy | 3.38 (1.55–7.36) ** | 8.86 (2.22–35.41) ** |
| Comorbid with malignancy | 7.42 (2.06–26.70) ** | |
| Time from ARDS to prone (h) | 1.01 (1.00–1.03) | |
| Total prone duration (h) | 1.01 (0.99–1.01) | |
| PaO2/FiO2 (PF ratio) | 0.99 (0.98–1.00) | |
| Prone score ≥ 3 | 14.33 (5.74–35.77) ** |
| Variables | Univariate Analysis HR (95% CI) | Multivariate Analysis HR (95% CI) |
|---|---|---|
| Age (year) | 1.02 (1.01–1.03) * | 1.01 (0.99–1.03) |
| APACHE II score | 1.08 (1.03–1.13) ** | 1.06 (1.01–1.11) * |
| Cause of ARDS | ||
| Extrapulmonary ARDS | Reference | |
| Non-influenza pulmonary ARDS | 1.07 (0.38–2.98) | |
| Influenza ARDS | 0.93 (0.28–3.10) | |
| Renal replacement therapy | 1.52 (0.92–2.51) | |
| Comorbid with malignancy | 2.06 (1.20–3.52) ** | |
| Time from ARDS to prone (h) | 1.00 (1.00–1.01) | |
| Total prone duration (h) | 1.00 (0.99–1.00) | |
| PaO2/FiO2 (PF ratio) | 0.99 (0.99–1.00) | |
| Prone score ≥ 3 | 2.84 (1.61–5.01) ** | 2.13 (1.12–4.07) * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, P.-H.; Kuo, C.-T.; Hsu, C.-Y.; Lin, S.-P.; Fu, P.-K. Prognostic Factors to Predict ICU Mortality in Patients with Severe ARDS Who Received Early and Prolonged Prone Positioning Therapy. J. Clin. Med. 2021, 10, 2323. https://doi.org/10.3390/jcm10112323
Lee P-H, Kuo C-T, Hsu C-Y, Lin S-P, Fu P-K. Prognostic Factors to Predict ICU Mortality in Patients with Severe ARDS Who Received Early and Prolonged Prone Positioning Therapy. Journal of Clinical Medicine. 2021; 10(11):2323. https://doi.org/10.3390/jcm10112323
Chicago/Turabian StyleLee, Po-Hsin, Chen-Tsung Kuo, Chiann-Yi Hsu, Shih-Pin Lin, and Pin-Kuei Fu. 2021. "Prognostic Factors to Predict ICU Mortality in Patients with Severe ARDS Who Received Early and Prolonged Prone Positioning Therapy" Journal of Clinical Medicine 10, no. 11: 2323. https://doi.org/10.3390/jcm10112323
APA StyleLee, P.-H., Kuo, C.-T., Hsu, C.-Y., Lin, S.-P., & Fu, P.-K. (2021). Prognostic Factors to Predict ICU Mortality in Patients with Severe ARDS Who Received Early and Prolonged Prone Positioning Therapy. Journal of Clinical Medicine, 10(11), 2323. https://doi.org/10.3390/jcm10112323







