Circulating Trimethylamine N-Oxide Is Associated with Increased Risk of Cardiovascular Mortality in Type-2 Diabetes: Results from a Dutch Diabetes Cohort (ZODIAC-59)
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population and Data Collection
2.2. Clinical Endpoint
2.3. Laboratory Measurements
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Cross-Sectional Analyses
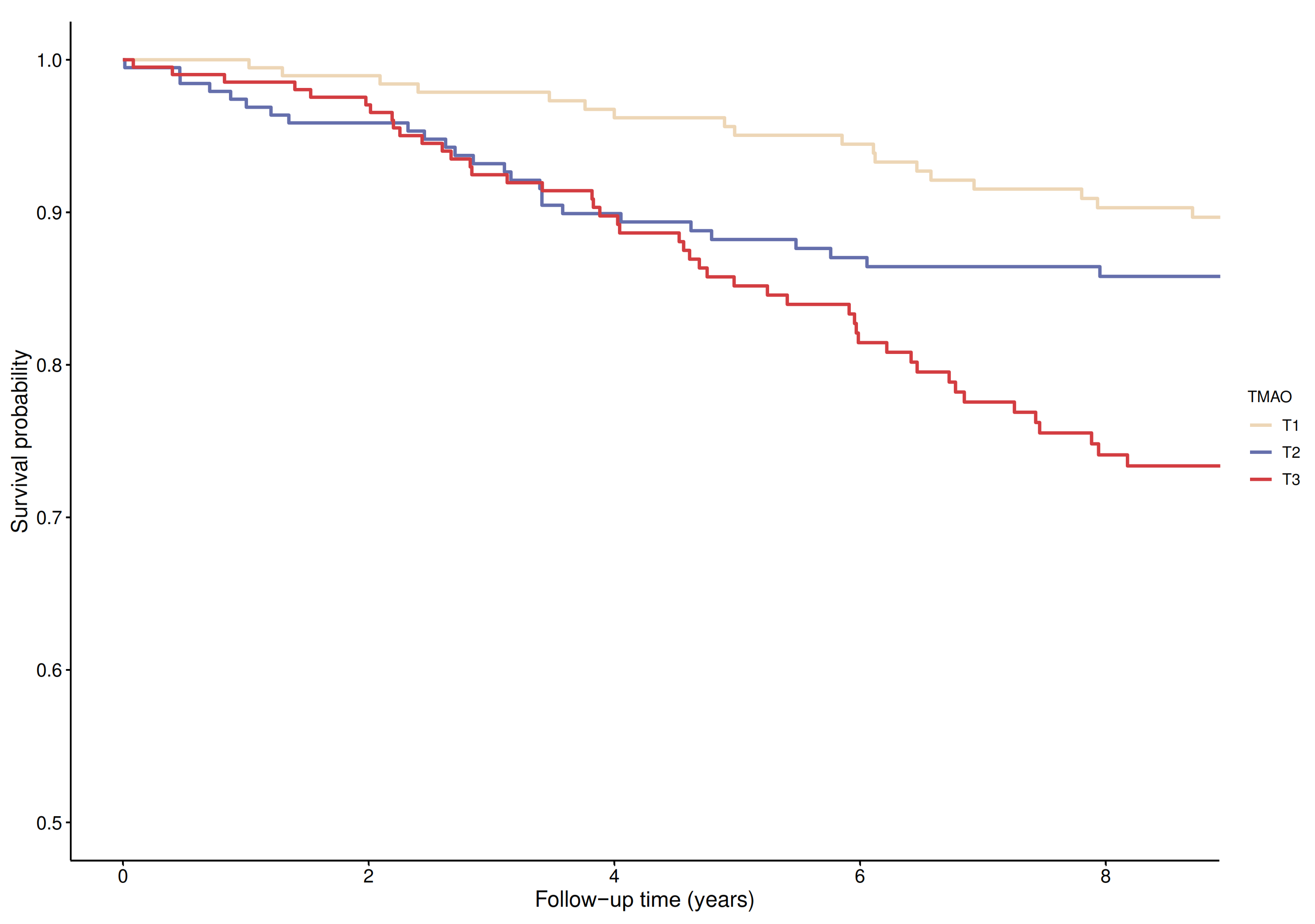
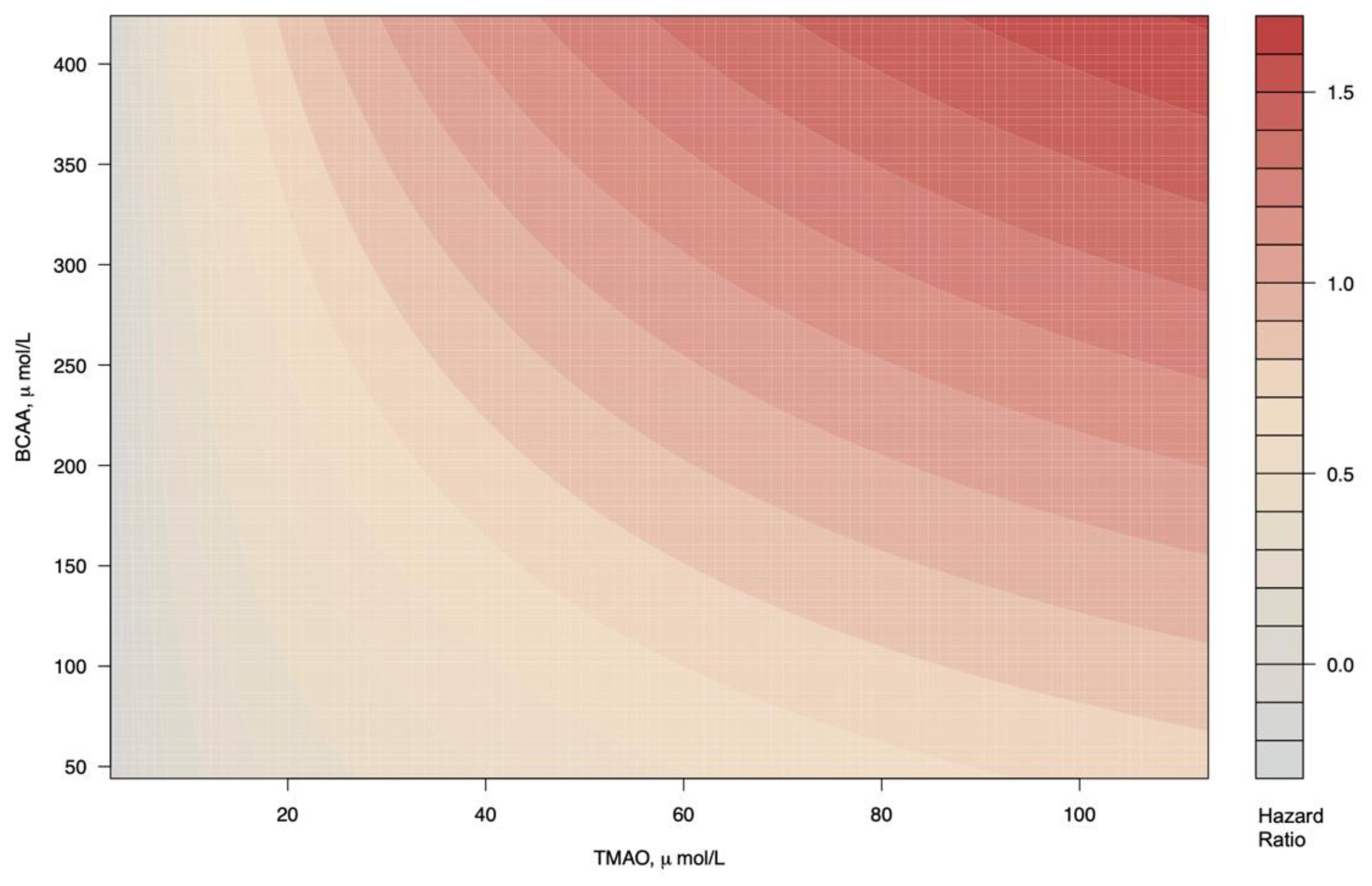
3.3. Longitudinal Analyses on TMAO and CV Mortality
3.4. Longitudinal Analysis on BCAA and CV Mortality
4. Discussion
Strengths and Limitations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wang, Z.; Klipfell, E.; Bennett, B.J.; Koeth, R.; Levison, B.S.; Dugar, B.; Feldstein, A.E.; Britt, E.B.; Fu, X.; Chung, Y.-M.; et al. Gut flora metabolism of phosphatidylcholine promotes cardiovascular disease. Nature 2011, 472, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Koeth, R.A.; Wang, Z.; Levison, B.S.; Buffa, J.A.; Org, E.; Sheehy, B.T.; Britt, E.B.; Fu, X.; Wu, Y.; Li, L.; et al. Intestinal microbiota metabolism of l-carnitine, a nutrient in red meat, promotes atherosclerosis. Nat. Med. 2013, 19, 576–585. [Google Scholar] [CrossRef] [PubMed]
- Yu, D.; Shu, X.; Rivera, E.; Zhang, X.; Cai, Q.; Calcutt, M.W.; Xiang, Y.; Li, H.; Gao, Y.; Wang, T.J.; et al. Urinary Levels of Trimethylamine-N-Oxide and Incident Coronary Heart Disease: A Prospective Investigation Among Urban Chinese Adults. J. Am. Heart Assoc. 2019, 8, e010606. [Google Scholar] [CrossRef]
- Gencer, B.; Li, X.S.; Gurmu, Y.; Bonaca, M.P.; Morrow, D.A.; Cohen, M.; Bhatt, D.L.; Steg, P.G.; Storey, R.F.; Johanson, P.; et al. Gut Microbiota-Dependent Trimethylamine N-oxide and Cardiovascular Outcomes in Patients With Prior Myocardial Infarction: A Nested Case Control Study From the PEGASUS-TIMI 54 Trial. J. Am. Heart Assoc. 2020, 9, e015331. [Google Scholar] [CrossRef] [PubMed]
- Kaysen, G.A.; Johansen, K.L.; Chertow, G.M.; Dalrymple, L.S.; Kornak, J.; Grimes, B.; Dwyer, T.; Chassy, A.W.; Fiehn, O. Associations of Trimethylamine N-Oxide With Nutritional and Inflammatory Biomarkers and Cardiovascular Outcomes in Patients New to Dialysis. J. Ren. Nutr. 2015, 25, 351–356. [Google Scholar] [CrossRef] [PubMed]
- Shafi, T.; Powe, N.R.; Meyer, T.W.; Hwang, S.; Hai, X.; Melamed, M.L.; Banerjee, T.; Coresh, J.; Hostetter, T.H. Trimethylamine N-Oxide and Cardiovascular Events in Hemodialysis Patients. J. Am. Soc. Nephrol. 2016, 28, 321–331. [Google Scholar] [CrossRef]
- Tang, W.W.; Wang, Z.; Kennedy, D.J.; Wu, Y.; Buffa, J.A.; Agatisa-Boyle, B.; Li, X.S.; Levison, B.S.; Hazen, S.L. Gut Microbiota-Dependent TrimethylamineN-Oxide (TMAO) Pathway Contributes to Both Development of Renal Insufficiency and Mortality Risk in Chronic Kidney Disease. Circ. Res. 2015, 116, 448–455. [Google Scholar] [CrossRef]
- Croyal, M.; Saulnier, P.-J.; Aguesse, A.; Gand, E.; Ragot, S.; Roussel, R.; Halimi, J.-M.; Ducrocq, G.; Cariou, B.; Montaigne, D.; et al. Plasma Trimethylamine N-Oxide and Risk of Cardiovascular Events in Patients with Type 2 Diabetes. J. Clin. Endocrinol. Metab. 2020, 105, 2371–2380. [Google Scholar] [CrossRef]
- Cardona, A.; O’Brien, A.; Bernier, M.C.; Somogyi, A.; Wysocki, V.H.; Smart, S.; He, X.; Ambrosio, G.; Hsueh, W.A.; Raman, S.V. Trimethylamine N-oxide and incident atherosclerotic events in high-risk individuals with diabetes: An ACCORD trial post hoc analysis. BMJ Open Diabetes Res. Care 2019, 7, e000718. [Google Scholar] [CrossRef]
- Gruppen, E.G.; Garcia, E.; Connelly, M.A.; Jeyarajah, E.J.; Otvos, J.D.; Bakker, S.J.L.; Dullaart, R.P.F. TMAO is Associated with Mortality: Impact of Modestly Impaired Renal Function. Sci. Rep 2017, 7, 1–9. [Google Scholar] [CrossRef]
- Poll, B.G.; Cheema, M.U.; Pluznick, J.L. Gut Microbial Metabolites and Blood Pressure Regulation: Focus on SCFAs and TMAO. Physiology 2020, 35, 275–284. [Google Scholar] [CrossRef]
- Tang, W.H.W.; Wang, Z.; Li, X.S.; Fan, Y.; Li, D.S.; Wu, Y.; Hazen, S.L. Increased Trimethylamine N-Oxide Portends High Mortality Risk Independent of Glycemic Control in Patients with Type 2 Diabetes Mellitus. Clin. Chem. 2017, 63, 297–306. [Google Scholar] [CrossRef]
- Vera, I.M.; Tapia, M.S.; Noriega-López, L.; Granados-Portillo, O.; Guevara-Cruz, M.; Flores-López, A.; Avila-Nava, A.; Fernández, M.L.; Tovar, A.R.; Torres, N. A dietary intervention with functional foods reduces metabolic endotoxaemia and attenuates biochemical abnormalities by modifying faecal microbiota in people with type 2 diabetes. Diabetes Metab. 2019, 45, 122–131. [Google Scholar] [CrossRef]
- Pedersen, H.K.; Gudmundsdottir, V.; Nielsen, H.B.; Hyotylainen, T.; Nielsen, T.; Jensen, B.A.H.; Forslund, K.; Hildebrand, F.; Prifti, E.; Falony, G.; et al. Human gut microbes impact host serum metabolome and insulin sensitivity. Nature 2016, 535, 376–381. [Google Scholar] [CrossRef] [PubMed]
- Ubink-Veltmaat, L.J.; Bilo, H.J.G.; Groenier, K.H.; Rischen, R.O.; Jong, B.M.-D. Shared care with task delegation to nurses for type 2 diabetes: Prospective observational study. Neth. J. Med. 2005, 63, 103–110. [Google Scholar]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA J. Am. Med. Assoc. 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Landman, G.W.; Van Dijk, P.R.; Drion, I.; Van Hateren, K.J.; Struck, J.; Groenier, K.H.; Gans, R.O.; Bilo, H.J.; Bakker, S.J.; Kleefstra, N. Midregional Fragment of Proadrenomedullin, New-Onset Albuminuria, and Cardiovascular and All-Cause Mortality in Patients With Type 2 Diabetes (ZODIAC-30). Diabetes Care 2013, 37, 839–845. [Google Scholar] [CrossRef][Green Version]
- Riphagen, I.J.; Boertien, W.E.; Alkhalaf, A.; Kleefstra, N.; Gansevoort, R.T.; Groenier, K.H.; Van Hateren, K.J.; Struck, J.; Navis, G.; Bilo, H.J.; et al. Copeptin, a Surrogate Marker for Arginine Vasopressin, Is Associated With Cardiovascular and All-Cause Mortality in Patients With Type 2 Diabetes (ZODIAC-31). Diabetes Care 2013, 36, 3201–3207. [Google Scholar] [CrossRef]
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.L.; Castro, A.F., 3rd; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T.; et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 2009, 150, 604–612. [Google Scholar] [CrossRef]
- Levey, A.S.; Coresh, J.; Greene, T.; Marsh, J.; Stevens, L.A.; Kusek, J.W.; Van Lente, F. Expressing the Modification of Diet in Renal Disease Study Equation for Estimating Glomerular Filtration Rate with Standardized Serum Creatinine Values. Clin. Chem. 2007, 53, 766–772. [Google Scholar] [CrossRef]
- Dullaart, R.P.F.; Garcia, E.; Jeyarajah, E.; Gruppen, E.G.; Connelly, M.A. Plasma phospholipid transfer protein activity is inversely associated with betaine in diabetic and non-diabetic subjects. Lipids Health Dis. 2016, 15, 143. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Garcia, E.; Osté, M.C.J.; Bennett, D.W.; Jeyarajah, E.J.; Shalaurova, I.; Gruppen, E.G.; Hazen, S.L.; Otvos, J.D.; Bakker, S.J.L.; Dullaart, R.P.; et al. High Betaine, a Trimethylamine N-Oxide Related Metabolite, Is Prospectively Associated with Low Future Risk of Type 2 Diabetes Mellitus in the PREVEND Study. J. Clin. Med. 2019, 8, 1813. [Google Scholar] [CrossRef] [PubMed]
- Connelly, M.A.; Wolak-Dinsmore, J.; Dullaart, R.P.F. Branched Chain Amino Acids Are Associated with Insulin Resistance Independent of Leptin and Adiponectin in Subjects with Varying Degrees of Glucose Tolerance. Metab. Syndr. Relat. Dis. 2017, 15, 183–186. [Google Scholar] [CrossRef] [PubMed]
- Wolak-Dinsmore, J.; Gruppen, E.G.; Shalaurova, I.; Matyus, S.P.; Grant, R.P.; Gegen, R.; Bakker, S.J.; Otvos, J.D.; Connelly, M.A.; Dullaart, R.P. A novel NMR-based assay to measure circulating concentrations of branched-chain amino acids: Elevation in subjects with type 2 diabetes mellitus and association with carotid intima media thickness. Clin. Biochem. 2018, 54, 92–99. [Google Scholar] [CrossRef]
- Therneau, T.M.; Grambsch, P.M. Modeling Survival Data: Extending the Cox Model; Statistics for Biology and Health; Springer: New York, NY, USA, 2000; ISBN 978-1-4419-3161-0. [Google Scholar]
- Alqifari, H.N.; Coolen, F.P.A. Robustness of Nonparametric Predictive Inference for Future Order Statistics. J. Stat. Theory Pract. 2019, 13, 12. [Google Scholar] [CrossRef]
- Pencina, M.J.; D’Agostino, R.B.D.; Vasan, R.S. Evaluating the added predictive ability of a new marker: From area under the ROC curve to reclassification and beyond. Stat. Med. 2008, 27, 157–172. [Google Scholar] [CrossRef]
- Agarwal, S.; Cox, A.J.; Herrington, D.M.; Jorgensen, N.W.; Xu, J.; Freedman, B.I.; Carr, J.J.; Bowden, D.W. Coronary Calcium Score Predicts Cardiovascular Mortality in Diabetes: Diabetes Heart Study. Diabetes Care 2012, 36, 972–977. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2019. [Google Scholar]
- Chobanian, A.V.; Bakris, G.L.; Black, H.R.; Cushman, W.C.; Green, L.A.; Izzo, J.J.L.; Jones, D.W.; Materson, B.J.; Oparil, S.; Wright, J.J.T.; et al. Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003, 42, 1206–1252. [Google Scholar] [CrossRef]
- Brunt, V.E.; Gioscia-Ryan, R.A.; Casso, A.G.; Vandongen, N.S.; Ziemba, B.P.; Sapinsley, Z.J.; Richey, J.J.; Zigler, M.C.; Neilson, A.P.; Davy, K.P.; et al. Trimethylamine-N-Oxide Promotes Age-Related Vascular Oxidative Stress and Endothelial Dysfunction in Mice and Healthy Humans. Hypertension 2020, 76, 101–112. [Google Scholar] [CrossRef]
- Zhu, W.; Gregory, J.C.; Org, E.; Buffa, J.A.; Gupta, N.; Wang, Z.; Li, L.; Fu, X.; Wu, Y.; Mehrabian, M.; et al. Gut Microbial Metabolite TMAO Enhances Platelet Hyperreactivity and Thrombosis Risk. Cell 2016, 165, 111–124. [Google Scholar] [CrossRef]
- Heianza, Y.; Ma, W.; Manson, J.E.; Rexrode, K.M.; Qi, L. Gut Microbiota Metabolites and Risk of Major Adverse Cardiovascular Disease Events and Death: A Systematic Review and Meta-Analysis of Prospective Studies. J. Am. Heart Assoc. 2017, 6, 7. [Google Scholar] [CrossRef]
- Herrema, H.; Niess, J.H. Intestinal microbial metabolites in human metabolism and type 2 diabetes. Diabetologia 2020, 63, 2533–2547. [Google Scholar] [CrossRef]
- Bennette, C.; Vickers, A. Against quantiles: Categorization of continuous variables in epidemiologic research, and its discontents. BMC Med. Res. Methodol. 2012, 12, 21. [Google Scholar] [CrossRef]
- Koppe, L.; Fouque, D.; Soulage, C.O. Metabolic Abnormalities in Diabetes and Kidney Disease: Role of Uremic Toxins. Curr. Diabetes Rep. 2018, 18, 97. [Google Scholar] [CrossRef]
| Characteristic | All (n = 594) | Tertile 1 (n = 194) | Tertile 2 (n = 193) | Tertile 3 (n = 207) | p Value * |
|---|---|---|---|---|---|
| Men, n (%) | 250 (42.1%) | 94 (48.5%) | 74 (38.3%) | 82 (39.6%) | 0.08 |
| Age, years | 69.45 (11.19) | 66.93 (11.30) | 68.64 (11.60) | 72.55 (9.93) | <0.001 |
| BMI, kg/m2 | 28.84 (4.53) | 28.73 (4.29) | 29.12 (4.51) | 28.69 (4.77) | 0.58 |
| SBP, mmHg | 154.40 (24.02) | 151.06 (24.68) | 156.39 (22.48) | 155.68 (24.57) | 0.05 |
| DBP, mmHg | 83.38 (10.88) | 83.55 (11.24) | 85.17 (10.32) | 81.54 (10.82) | 0.004 |
| Never smoked, n (%) | 123 (20.7%) | 37 (19.1%) | 47 (24.4%) | 39 (18.8%) | 0.31 |
| Diabetes duration, years | 4.62 (2.00, 9.11) | 4.00 (2.0, 8.0) | 5.00 (2.0, 10.0) | 5.00 (2.0, 11.0) | 0.58 |
| Macrovascular comp., n (%) | 220 (37.0%) | 69 (35.6%) | 60 (31.1%) | 91 (44.0%) | 0.02 |
| Microvascular comp., n (%) | 136 (48.4%) | 44 (45.8%) | 44 (44.9%) | 48 (55.2%) | 0.31 |
| Glucose, mg/dL | 155.62 (63.15) | 157.99 (60.02) | 157.96 (64.88) | 151.22 (64.44) | 0.24 |
| HbA1c, % | 7.32 (1.26) | 7.28 (1.35) | 7.35 (1.26) | 7.33 (1.19) | 0.88 |
| TMAO, μmol/L | 3.90 (2.40, 6.50) | 1.90 (1.30, 2.40) | 3.90 (3.30, 4.50) | 8.20 (6.30, 11.75) | <0.001 |
| TC, mmol/L | 5.58 (1.12) | 5.53 (1.13) | 5.59 (0.98) | 5.61 (1.23) | 0.76 |
| HDL-C, mmol/L | 1.11 (0.93, 1.36) | 1.10 (0.92, 1.37) | 1.11 (0.93, 1.37) | 1.14 (0.95, 1.35) | 0.69 |
| Triglycerides, mmol/L | 2.55 (1.50) | 2.58 (1.58) | 2.64 (1.59) | 2.44 (1.34) | 0.38 |
| BCAA, μmol/L | 512.94 (126.69) | 510.97 (120.61) | 508.90 (125.24) | 518.55 (133.80) | 0.72 |
| Valine, μmol/L | 273.47 (54.40) | 274.56 (52.37) | 273.26 (53.50) | 272.65 (57.28) | 0.93 |
| Leucine, μmol/L | 171.21 (53.46) | 169.80 (49.66) | 166.44 (51.17) | 176.98 (58.47) | 0.13 |
| Isoleucine, μmol/L | 68.27 (30.03) | 66.63 (28.17) | 69.22 (30.34) | 68.93 (31.48) | 0.64 |
| Serum creatinine, mmol/L | 94.16 (18.94) | 90.09 (15.09) | 92.18 (16.33) | 99.81 (22.79) | <0.001 |
| eGFR, mL/1.73 m2/min) 2 | 68.44 (18.80) | 72.37 (17.66) | 71.22 (18.29) | 62.16 (18.76) | <0.001 |
| Albuminuria, n (%) | 194 (33.9%) | 49 (25.9%) | 70 (37.6%) | 75 (37.9%) | 0.02 |
| Variable | Std β (95% CI) | p Value |
|---|---|---|
| Men, (yes) | −0.17 (−0.36; 0.01) | 0.06 |
| Age, years | −0.04 (−0.13; 0.06) | 0.45 |
| BMI, kg/m2 | 0.00 (−0.08; 0.08) | 0.98 |
| SBP, mmHg | 0.27 (0.17; 0.38) | <0.001 |
| DBP, mmHg | −0.19 (−0.29; −0.09) | <0.001 |
| Never smoked, (yes) | −0.07 (−0.28; 0.13) | 0.47 |
| Diabetes duration, years | −0.05 (−0.13; 0.03) | 0.24 |
| Macrovascular comp., (yes) | 0.11 (−0.06; 0.28) | 0.22 |
| Microvascular comp., (yes) | 0.23 (0.06; 0.41) | 0.009 |
| Glucose, mg/dL | −0.04 (−0.13; 0.05) | 0.35 |
| HbA1c, % | −0.01 (−0.11; 0.08) | 0.75 |
| TC, mmol/L | 0.12 (0.02; 0.22) | 0.02 |
| HDL-C, mmol/L | −0.02 (−0.11; 0.07) | 0.69 |
| Triglycerides, mmol/L | −0.10 (−0.19; 0.00) | 0.05 |
| BCAA, μmol/L | 0.18 (0.09; 0.27) | <0.001 |
| Serum creatinine, mmol/L | 0.17 (0.09; 0.26) | <0.001 |
| Albuminuria, (yes) | −0.10 (−0.28; 0.08) | 0.28 |
| TMAO per 1 Ln SD Increment | T1 | T2 | T3 | ||||
|---|---|---|---|---|---|---|---|
| Participants, n | 595 | 194 | 193 | 208 | |||
| Events, n | 113 | 22 | 32 | 59 | |||
| HR (95% CI) | p value | HR (95% CI) | p value * | HR (95% CI) | p value ** | ||
| Crude Model | 1.58 (1.33; 1.87) | <0.001 | (ref) | 1.61 (0.94; 2.77) | 0.08 | 3.26 (1.99; 5.34) | <0.001 |
| Model 1 | 1.39 (1.16; 1.67) | <0.001 | (ref) | 1.49 (0.86; 2.56) | 0.15 | 2.18 (1.33; 3.58) | 0.002 |
| Model 2 | 1.29 (1.07; 1.56) | 0.007 | (ref) | 1.58 (0.91; 2.72) | 0.10 | 2.06 (1.25; 3.41) | 0.004 |
| Model 3 | 1.26 (1.04; 1.54) | 0.02 | (ref) | 1.42 (0.82; 2.46) | 0.21 | 1.87 (1.12; 3.12) | 0.02 |
| Model 4 | 1.27 (1.03; 1.56) | 0.02 | (ref) | 1.39 (0.78; 2.48) | 0.26 | 1.92 (1.12; 3.30) | 0.02 |
| Model 5 | 1.32 (1.07; 1.63) | 0.01 | (ref) | 1.30 (0.73; 2.32) | 0.38 | 1.93 (1.12; 3.35) | 0.02 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Flores-Guerrero, J.L.; van Dijk, P.R.; Connelly, M.A.; Garcia, E.; Bilo, H.J.G.; Navis, G.; Bakker, S.J.L.; Dullaart, R.P.F. Circulating Trimethylamine N-Oxide Is Associated with Increased Risk of Cardiovascular Mortality in Type-2 Diabetes: Results from a Dutch Diabetes Cohort (ZODIAC-59). J. Clin. Med. 2021, 10, 2269. https://doi.org/10.3390/jcm10112269
Flores-Guerrero JL, van Dijk PR, Connelly MA, Garcia E, Bilo HJG, Navis G, Bakker SJL, Dullaart RPF. Circulating Trimethylamine N-Oxide Is Associated with Increased Risk of Cardiovascular Mortality in Type-2 Diabetes: Results from a Dutch Diabetes Cohort (ZODIAC-59). Journal of Clinical Medicine. 2021; 10(11):2269. https://doi.org/10.3390/jcm10112269
Chicago/Turabian StyleFlores-Guerrero, Jose L., Peter R. van Dijk, Margery A. Connelly, Erwin Garcia, Henk J. G. Bilo, Gerjan Navis, Stephan J. L. Bakker, and Robin P. F. Dullaart. 2021. "Circulating Trimethylamine N-Oxide Is Associated with Increased Risk of Cardiovascular Mortality in Type-2 Diabetes: Results from a Dutch Diabetes Cohort (ZODIAC-59)" Journal of Clinical Medicine 10, no. 11: 2269. https://doi.org/10.3390/jcm10112269
APA StyleFlores-Guerrero, J. L., van Dijk, P. R., Connelly, M. A., Garcia, E., Bilo, H. J. G., Navis, G., Bakker, S. J. L., & Dullaart, R. P. F. (2021). Circulating Trimethylamine N-Oxide Is Associated with Increased Risk of Cardiovascular Mortality in Type-2 Diabetes: Results from a Dutch Diabetes Cohort (ZODIAC-59). Journal of Clinical Medicine, 10(11), 2269. https://doi.org/10.3390/jcm10112269








