Quality of Life of Patients after Kinesio Tape Applications Following Impacted Mandibular Third Molar Surgeries
Abstract
1. Introduction
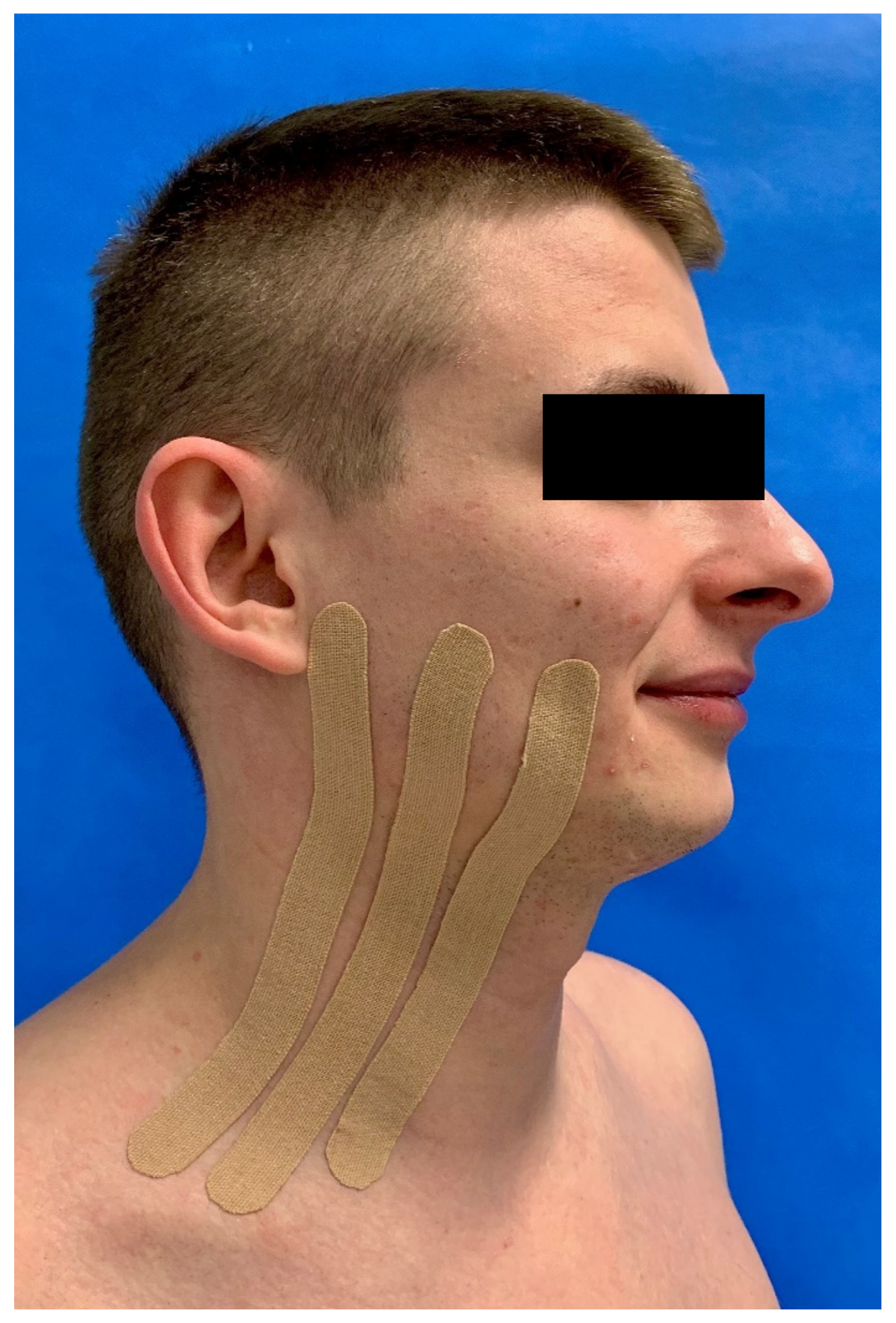
2. Materials and Methods
3. Results
3.1. Group Characteristics
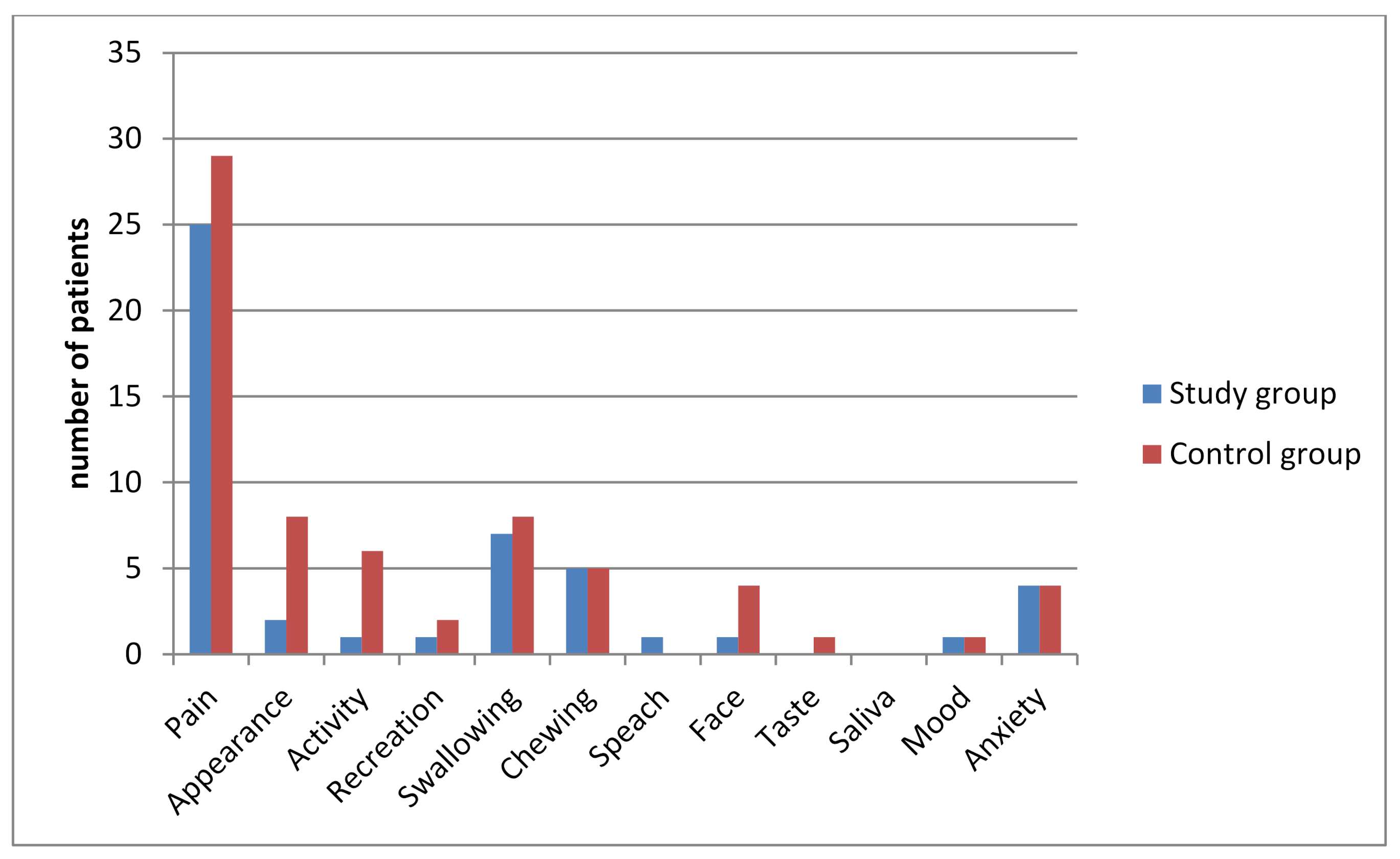
3.2. QOL Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bui, C.H.I.; Seldin, E.; Dodson, T. Types, frequencies, and risk factors for complications after third molar extraction. J. Oral Maxillofac. Surg. 2003, 61, 1379–1389. [Google Scholar] [CrossRef] [PubMed]
- Yuasa, H.; Sugiura, M. Clinical postoperative findings after removal of impacted mandibular third molars: Prediction of postoperative facial swelling and pain based on preoperative variables. J. Oral Maxillofac. Surg. 2004, 42, 209–214. [Google Scholar] [CrossRef]
- Zandi, M.; Amini, P.; Keshavarz, A. Effectiveness of cold therapy in reducing pain, trismus, and edema after impacted mandibular third molar surgery: A randomized, self-controlled, observer-blind, split-mouth clinical trial. Int. J. Oral Maxillofac. Surg. 2016, 45, 118–123. [Google Scholar] [CrossRef]
- Osunde, O.; Saheeb, B.; Bassey, G. Indications and risk factors for complications of lower third molar surgery in a nigerian teaching hospital. Ann. Med. Health Sci. Res. 2014, 4, 938–942. [Google Scholar] [CrossRef] [PubMed]
- Duarte-Rodrigues, L.; Miranda, E.F.P.; Souza, T.O.; de Paiva, H.N.; Falci, S.G.M.; Galvão, E.L. Third molar removal and its impact on quality of life: Systematic review and meta-analysis. Qual. Life Res. 2018, 27, 2477–2489. [Google Scholar] [CrossRef]
- Beech, A.N.; Haworth, S.; Knepil, G.J. Measurement of generic compared with disease-specificquality of life after removal of mandibular third molars: A patient-centered evaluation. Br. J. Oral Maxillofac. Surg. 2017, 55, 274–280. [Google Scholar] [CrossRef][Green Version]
- Deepti, C.; Rehan, H.S.; Mehra, P. Changes in quality of life after surgical removal of impacted mandibular third molar teeth. J. Oral Maxillofac. Surg. 2009, 8, 257–260. [Google Scholar] [CrossRef]
- Colorado-Bonnin, M.; Valmaseda-Castellon, E.; Berini-Aytes, L.; Gay-Escoda, C. Quality of life following lower third molar removal. Int. J. Oral Maxillofac. Surg. 2006, 35, 343–347. [Google Scholar] [CrossRef]
- Beech, A.N.; Haworth, S.; Knepil, G.J. Effect of a domiciliary facial cooling system on generic quality of life after removal of mandibular third molars. Br. J. Oral Maxillofac. Surg. 2018, 56, 315–321. [Google Scholar] [CrossRef]
- Shugars, D.A.; Gentile, M.A.; Ahmad, N.; Stavropoulos, M.F.; Slade, G.D.; Phillips, C.; Conrad, S.M.; Fleuchaus, P.T.; White, R.P., Jr. Assessment of oral health-related quality of life before and after third molar surgery. J. Oral Maxillofac. Surg. 2006, 64, 1721–1730. [Google Scholar] [CrossRef]
- Chugh, A.; Singh, S.; Mittal, Y.; Chugh, V. Submucosal injection of dexamethasone and metyloprednisolone for the control of postoperative sequelae after third molar surgery: Randomized controlled trial. Int. J. Oral Maxillofac. Surg. 2018, 47, 228–233. [Google Scholar] [CrossRef]
- Kocer, G.; Yuce, E.; Tuzuner, O.A.; Dereci, O.; Koskan, O. Effect of the route of administration of methylprednisolone on oedema and trismus in impacted lower third molar surgery. Int. J. Oral Maxillofac. Surg. 2014, 43, 639–643. [Google Scholar] [CrossRef]
- Aras, M.H.; Güngörmüs, M. Placebo-controlled randomized clinical trial of the effect two different low-level laser therapies (LLLT)—intraoral and extraoral—on trismus and facial swelling following surgical extraction of the lower third molar. Lasers Med. Sci. 2010, 25, 641–645. [Google Scholar] [CrossRef]
- Filho, J.R.L.; Silva, E.D.; Camargo, I.B.; Gouveia, F.M.V. The influence of cryotherapy on reduction of swelling, pain and trismus after third molar extraction. J. Am. Dent. Assoc. 2005, 136, 774–778. [Google Scholar] [CrossRef] [PubMed]
- Ristow, O.; Pautke, C.; Kehl, V.; Koerdt, S.; Hahnefeld, L.; Hohlweg-Majert, B. Kinesiologic taping reduces morbidity after oral and maxillofacial surgery: A pooled analysis. Physiother. Theory Pract. 2014, 30, 390–398. [Google Scholar] [CrossRef] [PubMed]
- Jaroń, A.; Jedliński, M.; Grzywacz, E.; Mazur, M.; Trybek, G. Kinesiology Taping as an Innovative Measure against Post-Operative Complications after Third Molar Extraction—Systematic Review. J. Clin. Med. 2020, 9, 3988. [Google Scholar] [CrossRef]
- Jaroń, A.; Preuss, O.; Grzywacz, E.; Trybek, G. The Impact of Using Kinesio Tape on Non-Infectious Complications after Impacted Mandibular Third Molar Surgery. Int. J. Environ. Res. Public Health 2021, 18, 399. [Google Scholar] [CrossRef]
- Kase, K.; Wallis, J.; Kase, T. Clinical Therapeutic Applications of the Kinesio Taping Method, 2nd ed.; Ken Ikai: Tokyo, Japan, 2003. [Google Scholar]
- Gómez-Soriano, J.; Abián-Vicén, J.; Aparicio-García, C.; Ruiz-Lázaro, P.; Simón-Martínez, C.; Bravo-Esteban, E.; Fernández-Rodríguez, J.M. The effects of Kinesio taping on muscle tone in healthy subjects: A double-blind, placebo-controlled crossover trial. Mannual Ther. 2014, 19, 131–136. [Google Scholar] [CrossRef]
- Lowe, D.; Rogers, S.N. Guidance for Scoring and Presentation: University of Washington Quality of Life Questionnaire (UW-QOL v4). 2012. Available online: http://www.hancsupport.com/sites/default/files/assets/pages/UW-QOL-update_2012.pdf (accessed on 12 September 2020).
- Shieh, G.; Jan, S.L.; Randles, R.H. On power and sample size determinations for the Wilcoxon–Mann–Whitney test. J. Nonparametric Stat. 2006, 18, 33–43. [Google Scholar] [CrossRef]
- Adeyemo, W.L.; Taiwo, O.A.; Oderinu, O.H.; Adeyemi, M.F.; Ladeinde, A.L.; Ogunlewe, M.O. Oral health-related quality of life following non-surgical (routine) tooth extraction: A pilot study. Contemp. Clin. Dent. 2012, 3, 427–432. [Google Scholar] [CrossRef]
- Bradshaw, S.; Faulk, J.; Blakey, G.H.; Phillips, C.; Phero, J.A.; White, R.P., Jr. Quality of life outcomes after third molar removal in subjects with minor symptoms of pericoronitis. J. Oral Maxillofac. Surg. 2012, 70, 2494–2500. [Google Scholar] [CrossRef] [PubMed]
- Kieffer, J.M.; van Wijk, A.J.; Ho, J.P.; Lindeboom, J.A. The internal responsiveness of the Oral Health Impact Profile-14 to detect differences in clinical parameters related to surgical third molar removal. Qual. Life Res. 2012, 21, 1241–1247. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kazancioglu, H.O.; Kurklu, E.; Ezirganli, S. Effects of ozone therapy on pain, swelling, and trismus following third molar surgery. Int. J. Oral Maxillofac. Surg. 2014, 43, 644–648. [Google Scholar] [CrossRef] [PubMed]
- Kazancioglu, H.O.; Ezirganli, S.; Demirtas, N. Comparison of the influence of ozone and laser therapies on pain, swelling, and trismus following impacted third-molar surgery. Lasers Med. Sci. 2013, 29, 1313–1319. [Google Scholar] [CrossRef]
- Ibikunle, A.A.; Adeyemo, W.L.; Ladeinde, A.L. Oral health-related quality of life following third molar surgery with either oral administration or submucosal injection of prednisolone. J. Oral Maxillofac. Surg. 2016, 20, 343–352. [Google Scholar] [CrossRef]
- Ibikunle, A.A.; Adeyemo, W.L. Oral health-related quality of life following third molar surgery with or without application of ice pack therapy. J. Oral Maxillofac. Surg. 2016, 20, 239–247. [Google Scholar] [CrossRef]
- Hassan, S.J.; Weymuller, E.A., Jr. Assessment of quality of life in head and neck cancer patients. Head Neck 1993, 15, 485–496. [Google Scholar] [CrossRef]
- Weymuller, E.A., Jr.; Alsarraf, R.; Yueh, B.; Deleyiannis, F.W.; Coltrera, M.D. Analysis of the performance characteristics of the University of Washington Quality of Life instrument and its modification (UW-QOL-R). Arch. Otolaryngol. Head Neck Surg. 2001, 127, 489–493. [Google Scholar] [CrossRef]
- McGrath, C.; Comfort, M.B.; Lo, E.C.; Luo, Y. Changes in life quality following third molar surgery-the immediate postoperative period. Br. Dent. J. 2003, 194, 265–268. [Google Scholar] [CrossRef]
- Grossi, G.B.; Maiorana, C.; Garramone, R.A.; Borgonovo, A.; Creminelli, L.; Santoro, F. Assessing Postoperative Discomfort After Third Molar Surgery: A Prospective Study. J. Oral Maxillofac. Surg. 2007, 65, 901–917. [Google Scholar] [CrossRef]
- Braimah, R.O.; Ndukwe, K.C.; Owotade, F.J.; Aregbesola, S.B. Oral health-related quality of life (OHRQoL) following third molar surgery in Sub-Saharan Africans: An observational study. Afr. Med. J. 2016, 19, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Ristow, O.; Hohlweg-Majert, B.; Kehl, V.; Koerdt, S.; Hahnefeld, L.; Pautke, C. Does elastic therapeutic tape reduce postoperative pain and trismus after open reduction and internal fixation of mandibular fractures. J. Oral Maxillofac. Surg. 2013, 71, 1387–1396. [Google Scholar] [CrossRef]
- Ristow, O.; Hohlweg-Majert, B.; Sturzembaum, S.R.; Kehl, V.; Koerdt, S.; Hahnefeld, L.; Pautke, C. Therapeutic elastic tape reduces morbidity after wisdom teeth removal-a clinical trial. Clin. Oral Investig. 2014, 18, 1205–1212. [Google Scholar] [CrossRef]
- Ristow, O.; Pautke, C.; Kehl, V.; Koerdt, S.; Schwarzler, K.; Hahnefeld, L.; Hohlweg-Majert, B. Influence of kinesiologic tape on postoperative swelling, pain and trismus after zygomatico-orbital fractures. J. Craniomaxillofac. Surg. 2014, 42, 469–476. [Google Scholar] [CrossRef]
- Yurttutan, M.E.; Karaahmetoğlu, Ö.; Üçok, C.; Bağış, N. Comparison of the quality of life of patients with mandibular third molars and mild pericoronitis treated by extraction or by a periodontal approach. Br. J. Oral Maxillofac. Surg. 2020, 58, 179–184. [Google Scholar] [CrossRef]
- Deo, S.P. Single-Dose of Submucosal Injection of Dexamethasone Affects the Post Operative Quality of Life After Third Molar Surgery. J. Oral Maxillofac. Surg. 2016, 15, 367–375. [Google Scholar] [CrossRef]
- Batinjan, G.; Filipović, Z.I.; Rupić, I.; Bag, J.I.; Zore, Z.; Gabrić, P.D. Assessing Health-Related Quality of Life with Antimicrobial Photodynamic Therapy (APDT) and Low Level Laser Therapy (LLLT) after Third Molar Removal. J. Lasers Med. Sci. 2013, 4, 120–126. [Google Scholar]
- Kau, C.H.; Cronin, A.; Durning, P.; Zhurov, A.I.; Sandham, A.; Richmond, S. A new method for the 3D measurement of postoperative swelling following orthognathic surgery. Orthod Craniofac. Res. 2006, 9, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Yip, E.; Smith, A.; Yoshino, M. Volumetric evaluation of facial swelling utilizing a 3-D range camera. Int. J. Oral Maxillofac. Surg. 2004, 33, 179–182. [Google Scholar] [CrossRef]
- Metlerski, M.; Grocholewicz, K.; Jaroń, A.; Lipski, M.; Trybek, G. Comparison of Presurgical Dental Models Manufactured with Two Different Three-Dimensional Printing Techniques. J. Health Eng. 2020, 29, 3338. [Google Scholar] [CrossRef]
- Tatli, U.; Benlidayi, I.C.; Salimov, F.; Guzel, R. Effectiveness of kinesio taping onpostoperative morbidity after impacted mandibular third molar surgery: A prospective, randomized, placebo-controlled clinical study. J. Appl. Oral Sci. 2020, 28, e20200159. [Google Scholar] [CrossRef] [PubMed]
- Younger, J.; McCue, R.; Mackey, S. Pain outcomes: A brief review of instruments and techniques. Curr. Pain Headache Rep. 2009, 13, 39–43. [Google Scholar] [CrossRef] [PubMed]

|
| 13. Which issues have been the most important to you during the past 7 days? Tick up to 3 boxes. | ||
| □ Pain | □ Swallowing | □ Taste |
| □ Appearance | □ Chewing | □ Saliva |
| □ Activity | □ Speech | □ Mood |
| □ Recreation | □ Shoulder | □ Anxiety |
General Questions:
|
| Significant Problem | Scores |
|---|---|
| Pain, appearance, activity, recreation, mood | 0, 25, 50 with important issue (question 13) |
| Swallowing, speech, anxiety | 0, 30 |
| Shoulder, taste, saliva | 0, 30 with important issue (question 13) |
| Chewing | 0 |
| Baseline Characteristic | Age (Years) | Procedure Time (Minutes) | Sex | |||||
|---|---|---|---|---|---|---|---|---|
| Female | Male | |||||||
| Median | Range | Median | Range | n | % | n | % | |
| Study group (n = 50) | 26.5 | 19–59 | 21 | 10–60 | 36 | 72 | 14 | 28 |
| Control group (n = 50) | 25 | 18–38 | 24.5 | 6–60 | 38 | 76 | 12 | 24 |
| Total (n = 100) | 25.5 | 18–59 | 23 | 6–60 | 74 | 74 | 26 | 26 |
| p-value 1 | 0.221 | 0.801 | p-value 2 0.82 | |||||
| Domain | Group | n | Mean | SD | Min | Q1 | Median | Q3 | Max | p * |
|---|---|---|---|---|---|---|---|---|---|---|
| Pain | study | 50 | 53 | 27.03 | 0 | 25 | 50 | 75 | 100 | 0.287 |
| control | 50 | 47.5 | 26.85 | 0 | 25 | 37.5 | 75 | 100 | ||
| Appearance | study | 50 | 68.5 | 25.16 | 25 | 50 | 75 | 100 | 100 | 0.249 |
| control | 50 | 62 | 27.77 | 25 | 31.25 | 75 | 75 | 100 | ||
| Activity | study | 50 | 81.5 | 21.91 | 0 | 75 | 75 | 100 | 100 | 0.017 |
| control | 50 | 68 | 29.47 | 0 | 50 | 75 | 100 | 100 | ||
| Recreation | study | 50 | 78 | 23.5 | 25 | 75 | 75 | 100 | 100 | 0.346 |
| control | 50 | 70 | 31.94 | 0 | 50 | 75 | 100 | 100 | ||
| Swallowing | study | 50 | 83 | 25.01 | 30 | 70 | 100 | 100 | 100 | 0.366 |
| control | 50 | 79.2 | 25.54 | 30 | 70 | 100 | 100 | 100 | ||
| Chewing | study | 50 | 59 | 29.78 | 0 | 50 | 50 | 100 | 100 | 0.351 |
| control | 50 | 54 | 26.42 | 0 | 50 | 50 | 50 | 100 | ||
| Speech | study | 50 | 89.6 | 16.28 | 30 | 70 | 100 | 100 | 100 | 0.734 |
| control | 50 | 89.2 | 14.55 | 70 | 70 | 100 | 100 | 100 | ||
| Face | study | 50 | 73.6 | 27.98 | 0 | 70 | 70 | 100 | 100 | 0.659 |
| control | 50 | 69.8 | 31.53 | 0 | 40 | 70 | 100 | 100 | ||
| Taste | study | 50 | 91.4 | 15.65 | 30 | 77.5 | 100 | 100 | 100 | 0.154 |
| control | 50 | 82.2 | 27.65 | 0 | 70 | 100 | 100 | 100 | ||
| Saliva | study | 50 | 95 | 13.59 | 30 | 100 | 100 | 100 | 100 | 0.625 |
| control | 50 | 94.6 | 11.64 | 70 | 100 | 100 | 100 | 100 | ||
| Mood | study | 50 | 74 | 18.87 | 25 | 75 | 75 | 75 | 100 | 0.048 |
| control | 50 | 65 | 23.15 | 25 | 50 | 75 | 75 | 100 | ||
| Anxiety | study | 50 | 81.2 | 21.06 | 30 | 70 | 70 | 100 | 100 | 0.863 |
| control | 50 | 80.6 | 20.94 | 30 | 70 | 70 | 100 | 100 | ||
| Physical function | study | 50 | 81.08 | 15.39 | 30.83 | 73.33 | 82.92 | 91.67 | 100 | 0.24 |
| control | 50 | 76.87 | 16.84 | 42.5 | 63.75 | 78.33 | 87.5 | 100 | ||
| Social-Emotional Function | study | 50 | 73.46 | 18.24 | 25 | 64 | 79 | 89 | 100 | 0.188 |
| control | 50 | 67.18 | 22.63 | 11 | 49.25 | 70 | 87.75 | 100 | ||
| Health-related QoL compared to time before surgery | study | 50 | 63 | 27.31 | 0 | 50 | 50 | 75 | 100 | 0.509 |
| control | 50 | 67 | 28.32 | 0 | 50 | 62.5 | 100 | 100 | ||
| Health-related QoL during the past 7 days | study | 50 | 56 | 18.52 | 0 | 40 | 60 | 60 | 80 | 0.021 |
| control | 50 | 46.8 | 20.84 | 0 | 40 | 40 | 60 | 80 | ||
| Overall QoL during the past 7 days | study | 50 | 64.4 | 19.5 | 20 | 60 | 60 | 80 | 100 | 0.003 |
| control | 50 | 52.8 | 19.7 | 20 | 40 | 60 | 60 | 100 |
| Domain | Group | n | Mean | SD | Min | Q1 | Median | Q3 | Max | p * |
|---|---|---|---|---|---|---|---|---|---|---|
| Pain | study | 50 | 39.5 | 27.71 | 0 | 25 | 37.5 | 75 | 75 | 0.321 |
| control | 50 | 45 | 27.66 | 0 | 25 | 50 | 75 | 75 | ||
| Appearance | study | 50 | 28 | 25.58 | −25 | 0 | 25 | 50 | 75 | 0.176 |
| control | 50 | 36 | 28.64 | 0 | 0 | 25 | 50 | 75 | ||
| Activity | study | 50 | 13 | 24.35 | −50 | 0 | 0 | 25 | 100 | 0.045 |
| control | 50 | 25 | 29.01 | −25 | 0 | 25 | 50 | 100 | ||
| Recreation | study | 50 | 16.5 | 26.54 | −25 | 0 | 0 | 25 | 75 | 0.544 |
| control | 50 | 22 | 32.2 | −25 | 0 | 0 | 50 | 100 | ||
| Swallowing | study | 50 | 16.4 | 25.05 | 0 | 0 | 0 | 30 | 70 | 0.363 |
| control | 50 | 20.2 | 25.67 | 0 | 0 | 0 | 30 | 70 | ||
| Chewing | study | 50 | 35 | 30.72 | 0 | 0 | 50 | 50 | 100 | 0.112 |
| control | 50 | 44 | 27.92 | 0 | 50 | 50 | 50 | 100 | ||
| Speech | study | 50 | 8.6 | 17.84 | −30 | 0 | 0 | 30 | 70 | 0.611 |
| control | 50 | 9.6 | 16.53 | −30 | 0 | 0 | 30 | 30 | ||
| Face | study | 50 | 24.6 | 26.2 | 0 | 0 | 30 | 30 | 100 | 0.8 |
| control | 50 | 27.8 | 32.41 | −30 | 0 | 30 | 37.5 | 100 | ||
| Taste | study | 50 | 6.2 | 12.6 | 0 | 0 | 0 | 0 | 40 | 0.143 |
| control | 50 | 16 | 28.43 | −30 | 0 | 0 | 30 | 100 | ||
| Saliva | study | 50 | 4.4 | 11.1 | 0 | 0 | 0 | 0 | 40 | 1 |
| control | 50 | 4.2 | 12.14 | −30 | 0 | 0 | 0 | 30 | ||
| Mood | study | 50 | 10 | 19.56 | −25 | 0 | 0 | 25 | 50 | 0.064 |
| control | 50 | 19.5 | 26.39 | −25 | 0 | 25 | 25 | 75 | ||
| Anxiety | study | 50 | 13.4 | 22.73 | −30 | 0 | 0 | 30 | 70 | 0.882 |
| control | 50 | 13.2 | 24.94 | −70 | 0 | 0 | 30 | 70 | ||
| Physical function | study | 50 | 16.43 | 14.09 | −5 | 4.17 | 16.67 | 23.12 | 53.33 | 0.138 |
| control | 50 | 21.67 | 16.44 | −5 | 9.37 | 19.58 | 35 | 57.5 | ||
| Social-Emotional Function | study | 50 | 21.4 | 18.05 | 0 | 7 | 15,5 | 35.5 | 70 | 0.332 |
| control | 50 | 26.6 | 22.51 | −14 | 7 | 26.5 | 43.75 | 81 | ||
| Health-related QoL compared to time before surgery | study | 50 | −2 | 30.66 | −50 | −25 | 0 | 0 | 75 | 0.137 |
| control | 50 | −12 | 37.88 | −100 | −50 | 0 | 0 | 100 | ||
| Health-related QoL during the past 7 days | study | 50 | 15.6 | 22.6 | −20 | 0 | 20 | 20 | 100 | 0.116 |
| control | 50 | 22.4 | 27 | −40 | 5 | 20 | 40 | 80 | ||
| Overall QoL during the past 7 days | study | 50 | 10.8 | 22.57 | −40 | 0 | 10 | 20 | 60 | 0.028 |
| control | 50 | 20.8 | 21.37 | −20 | 0 | 20 | 40 | 60 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jaroń, A.; Preuss, O.; Konkol, B.; Trybek, G. Quality of Life of Patients after Kinesio Tape Applications Following Impacted Mandibular Third Molar Surgeries. J. Clin. Med. 2021, 10, 2197. https://doi.org/10.3390/jcm10102197
Jaroń A, Preuss O, Konkol B, Trybek G. Quality of Life of Patients after Kinesio Tape Applications Following Impacted Mandibular Third Molar Surgeries. Journal of Clinical Medicine. 2021; 10(10):2197. https://doi.org/10.3390/jcm10102197
Chicago/Turabian StyleJaroń, Aleksandra, Olga Preuss, Berenika Konkol, and Grzegorz Trybek. 2021. "Quality of Life of Patients after Kinesio Tape Applications Following Impacted Mandibular Third Molar Surgeries" Journal of Clinical Medicine 10, no. 10: 2197. https://doi.org/10.3390/jcm10102197
APA StyleJaroń, A., Preuss, O., Konkol, B., & Trybek, G. (2021). Quality of Life of Patients after Kinesio Tape Applications Following Impacted Mandibular Third Molar Surgeries. Journal of Clinical Medicine, 10(10), 2197. https://doi.org/10.3390/jcm10102197








