Importance of Increased Arterial Resistance in Risk Prediction in Patients with Cardiovascular Risk Factors and Degenerative Aortic Stenosis
Abstract
1. Introduction
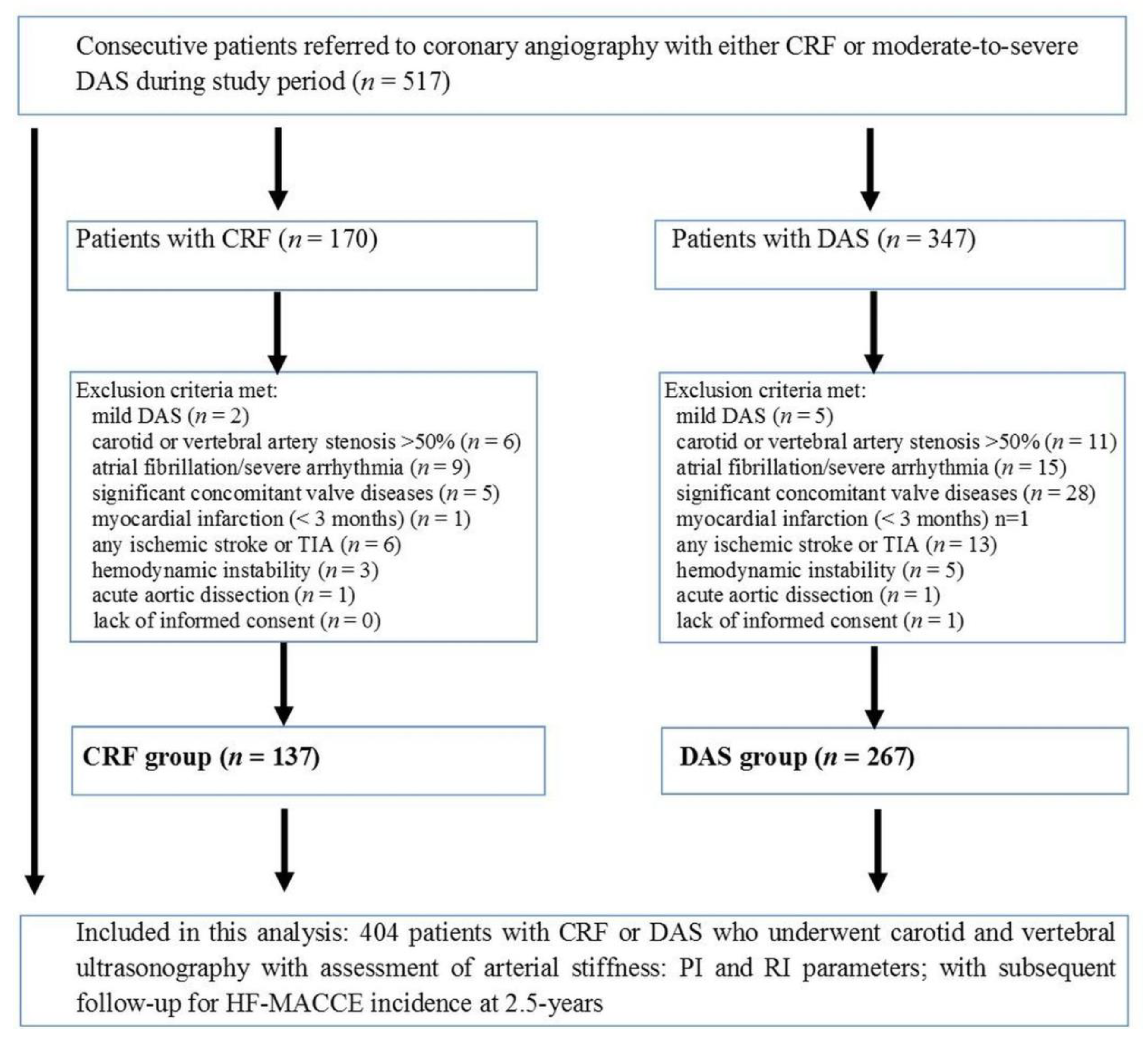
2. Materials and Methods
2.1. Study Population and Cardiovascular Risk Factors
2.2. Echocardiography, Carotid and Vertebral Artery Ultrasonography
2.3. Outcome Data, Follow-Up, and Adverse Cardiovascular Events
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Study Groups and Arterial Stiffness Findings
3.3. Vascular Resistance Properties and the Outcomes
4. Discussion
5. Conclusions
6. Study Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nilsson, P.M.; Boutouyrie, P.; Cunha, P.; Kotsis, V.; Narkiewicz, K.; Parati, G.; Rietzschel, E.; Scuteri, A.; Laurent, S. Early vascular ageing in translation: From laboratory investigations to clinical applications in cardiovascular prevention. J. Hypertens. 2013, 31, 1517–1526. [Google Scholar] [CrossRef]
- Stehouwer, C.D.; Henry, R.M.; Ferreira, I. Arterial stiffness in diabetes and the metabolic syndrome: A pathway to cardiovascular disease. Diabetologia 2008, 51, 527–539. [Google Scholar] [CrossRef]
- Alonso-Fernández, P.; De la Fuente, M. Role of the immune system in aging and longevity. Curr. Aging Sci. 2011, 4, 78–100. [Google Scholar] [CrossRef] [PubMed]
- Scuteri, A.; Orru, M.; Morrell, C.; Taub, D.; Schlessinger, D.; Uda, M.; Lakatta, E.G. Independent and additive effects of cytokine patterns and the metabolic syndrome on arterial aging in the SardiNIA Study. Atherosclerosis 2011, 215, 459–464. [Google Scholar] [CrossRef][Green Version]
- Sutton-Tyrrell, K.; Najjar, S.S.; Boudreau, R.M.; Venkitachalam, L.; Kupelian, V.; Simonsick, E.M.; Havlik, R.; Lakatta, E.G.; Spurgeon, H.; Kritchevsky, S.; et al. Elevated Aortic Pulse Wave Velocity, a Marker of Arterial Stiffness, Predicts Cardiovascular Events in Well-Functioning Older Adults. Circulation 2005, 111, 3384–3390. [Google Scholar] [CrossRef] [PubMed]
- Yan, A.T.; Koh, M.; Chan, K.K.; Guo, H.; Alter, D.A.; Austin, P.C.; Tu, J.V.; Wijeysundera, H.C.; Ko, D.T. Association between Cardiovascular Risk Factors and Aortic Stenosis: The CANHEART Aortic Stenosis Study. J. Am. Coll. Cardiol. 2017, 69, 1523–1532. [Google Scholar] [CrossRef] [PubMed]
- Podolec, J.; Baran, J.; Siedlinski, M.; Urbanczyk, M.; Krupinski, M.; Bartus, K.; Niewiara, L.; Podolec, M.; Guzik, T.; Tomkiewicz-Pajak, L.; et al. Serum rantes, transforming growth factor-β1 and interleukin-6 levels correlate with cardiac muscle fibrosis in patients with aortic valve stenosis. J. Physiol. Pharmacol. 2018, 69, 615–623. [Google Scholar]
- Baran, J.; Podolec, J.; Tomala, M.T.; Nawrotek, B.; Niewiara, Ł.; Gackowski, A.; Przewłocki, T.; Żmudka, K.; Kabłak-Ziembicka, A. Increased risk profile in the treatment of patients with symptomatic degenerative aortic valve stenosis over the last 10 years. Adv. Interv. Cardiol. 2018, 14, 276–284. [Google Scholar] [CrossRef]
- Bardelli, M.; Cavressi, M.; Furlanis, G.; Pinamonti, B.; Leone, M.; Albani, S.; Korcova, R.; Fabris, B.; Sinagra, G. Relationship between aortic valve stenosis and the hemodynamic pattern in the renal circulation, and restoration of the flow wave profile after correction of the valvular defect. J. Int. Med. Res. 2020, 48, 1–14. [Google Scholar] [CrossRef]
- Hamczyk, M.R.; Nevado, R.M.; Barettino, A.; Fuster, V.; Andrés, V. Biological Versus Chronological Aging. J. Am. Coll. Cardiol. 2020, 75, 919–930. [Google Scholar] [CrossRef]
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; Ference, B.A.; et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Eur. Heart J. 2020, 41, 111–188. [Google Scholar] [CrossRef] [PubMed]
- Baumgartner, H.; Hung, J.; Bermejo, J.; Chambers, J.B.; Edvardsen, T.; Goldstein, S.; Lancellotti, P.; LeFevre, M.; Miller, F., Jr.; Otto, C.M. Recommendations on the echocardiographic assessment of aortic valve stenosis: A focused update from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. J. Am. Soc. Echocardiogr. 2017, 30, 372–392. [Google Scholar] [CrossRef] [PubMed]
- Robin, X.A.; Turck, N.; Hainard, A.; Tiberti, N.; Lisacek, F.; Sanchez, J.-C.; Muller, M.J. pROC: An open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinform. 2011, 12, 77. [Google Scholar] [CrossRef] [PubMed]
- Frauchiger, B.; Schmid, H.P.; Roedel, C.; Moosmann, P.; Staub, D. Comparison of carotid arterial resistive indices with intima-media thickness as sonographic markers Atherosclerosis. Stroke 2001, 32, 836–841. [Google Scholar] [CrossRef] [PubMed]
- Kabłak-Ziembicka, A.; Rosławiecka, A.; Badacz, R.; Sokołowski, A.; Rzeźnik, D.; Trystuła, M.; Musiałek, P.; Przewłocki, T. Simple clinical scores to predict blood pressure and renal function response to renal artery stenting for atherosclerotic renal artery stenosis. Pol. Arch. Intern. Med. 2020, 130, 953–959. [Google Scholar] [CrossRef] [PubMed]
- Wielicka, M.; Neubauer-Geryk, J.; Kozera, G.; Bieniaszewski, L. Clinical application of pulsatility index. Med. Res. J. 2020, 5, 201–210. [Google Scholar] [CrossRef]
- Nakano, H.; Shiina, K.; Tomiyama, H. Cardiovascular Outcomes in the Acute Phase of COVID-19. Int. J. Mol. Sci. 2021, 22, 4071. [Google Scholar] [CrossRef]
- Summerhill, V.; Moschetta, D.; Orekhov, A.; Poggio, P.; Myasoedova, V. Sex-Specific Features of Calcific Aortic Valve Disease. Int. J. Mol. Sci. 2020, 21, 5620. [Google Scholar] [CrossRef]
- Thomassen, H.K.; Cioffi, G.; Gerdts, E.; Einarsen, E.; Midtbø, H.B.; Mancusi, C.; Cramariuc, D. Echocardiographic aortic valve calcification and outcomes in women and men with aortic stenosis. Heart 2017, 103, 1619–1624. [Google Scholar] [CrossRef]
- Weisz, S.H.; Magne, J.; Dulgheru, R.; Caso, P.; Piérard, L.A.; Lancellotti, P. Carotid Artery and Aortic Stiffness Evaluation in Aortic Stenosis. J. Am. Soc. Echocardiogr. 2014, 27, 385–392. [Google Scholar] [CrossRef]
- Kablak-Ziembicka, A.; Przewlocki, T.; Tracz, W.; Podolec, P.; Stopa, I.; Kostkiewicz, M.; Sadowski, J.; Mura, A.; Kopeć, G. Prognostic Value of Carotid Intima-Media Thickness in Detection of Coronary Atherosclerosis in Patients with Calcified Aortic Valve Stenosis. J. Ultrasound Med. 2005, 24, 461–467. [Google Scholar] [CrossRef] [PubMed]
- Safar, M.E.; Nilsson, P.M.; Blacher, J.; Mimran, A. Pulse Pressure, Arterial Stiffness, and End-Organ Damage. Curr. Hypertens. Rep. 2012, 14, 339–344. [Google Scholar] [CrossRef] [PubMed]
- Baran, J.; Przewłocki, T.; Podolec, J.; Gryglicka, K.; Badacz, R.; Gackowski, A.; Pieniążek, P.; Legutko, J.; Żmudka, K.; Kabłak-Ziembicka, A. Assessment of the Willis circle flow changes with the severity of degenerative aortic stenosis and cognitive impairment. Kardiol. Pol. 2021, 79, 46–52. [Google Scholar] [PubMed]
- Sequí-Domínguez, I.; Cavero-Redondo, I.; Álvarez-Bueno, C.; Pozuelo-Carrascosa, D.P.; De Arenas-Arroyo, S.N.; Martínez-Vizcaíno, V. Accuracy of Pulse Wave Velocity Predicting Cardiovascular and All-Cause Mortality. A Systematic Review and Meta-Analysis. J. Clin. Med. 2020, 9, 2080. [Google Scholar] [CrossRef]
- Zoungas, S.; Asmar, R.P. Arterial stiffness and cardiovascular outcome. Clin. Exp. Pharmacol. Physiol. 2007, 34, 647–651. [Google Scholar] [CrossRef] [PubMed]
- Saeed, S.; Saeed, N.; Grigoryan, K.; Chowienczyk, P.; Chambers, J.B.; Rajani, R. Determinants and clinical significance of aortic stiffness in patients with moderate or severe aortic stenosis. Int. J. Cardiol. 2020, 315, 99–104. [Google Scholar] [CrossRef]
- Bahlmann, E.; Cramariuc, D.; Saeed, S.; Chambers, J.B.; A Nienaber, C.; Kuck, K.-H.; Lønnebakken, M.T.; Gerdts, E. Low systemic arterial compliance is associated with increased cardiovascular morbidity and mortality in aortic valve stenosis. Heart 2019, 105, 1507–1514. [Google Scholar] [CrossRef]
- Ungvari, Z.; Tarantini, S.; Donato, A.J.; Galvan, V.; Csiszar, A. Mechanisms of Vascular Aging. Circ. Res. 2018, 123, 849–867. [Google Scholar] [CrossRef]
- Humphrey, J.D.; Harrison, D.G.; Figueroa, C.A.; Lacolley, P.; Laurent, S. Central Artery Stiffness in Hypertension and Aging: A Problem with Cause and Consequence. Circ. Res. 2016, 118, 379–381. [Google Scholar] [CrossRef]
- Janić, M.; Lunder, M.; Šabovič, M. Arterial Stiffness and Cardiovascular Therapy. BioMed Res. Int. 2014, 2014, 621437. [Google Scholar] [CrossRef]
- Musa, T.A.; Uddin, A.; Fairbairn, T.A.; Dobson, L.E.; Sourbron, S.P.; Steadman, C.D.; Motwani, M.; Kidambi, A.; Ripley, D.P.; Swoboda, P.P.; et al. Assessment of aortic stiffness by cardiovascular magnetic resonance following the treatment of severe aortic stenosis by TAVI and surgical AVR. J. Cardiovasc. Magn. Reson. 2016, 18, 37. [Google Scholar] [CrossRef] [PubMed]
- Bruschi, G.; Maloberti, A.; Sormani, P.; Colombo, G.; Nava, S.; Vallerio, P.; Casadei, F.; Bruno, J.; Moreo, A.; Merlanti, B. Arterial Stiffness in Aortic Stenosis: Relationship with Severity and Echocardiographic Procedures Response. High Blood Press. Cardiovasc. Prev. 2017, 24, 19–27. [Google Scholar] [CrossRef] [PubMed]

| DAS Group N = 267 | CRF Group N = 137 | p-Value | |
|---|---|---|---|
| Demographic data | |||
| Age (years) ± SD | 74.5 (8.8) | 70.0 (11) | 0.001 |
| Female, n (%) | 172 (64.4) | 87 (63.5) | 0.305 |
| Hypertension, n (%) | 239 (89.5) | 114 (83.2) | 0.157 |
| Diabetes, n (%) | 86 (32.7) | 41 (29.9) | 0.556 |
| Hyperlipidemia (%) | 256 (95.9) | 109 (79.6) | <0.001 |
| Coronary artery disease (%) Previous myocardial infarction, n (%) | 111 (41.6) 54 (20.2) | 54 (39.4) 43 (31.4) | 0.054 0.002 |
| Selected echocardiographic data | |||
| Aortic valve area (cm2) ± SD | 0.82 ± 0.28 | 2.5 ± 0.24 | <0.001 |
| Peak aortic gradient (mmHg) ± SD | 87.8 ± 29 | 9.6 ± 4.5 | <0.001 |
| Mean aortic gradient (mmHg) ± SD | 50.5 ± 18.7 | 4.3 ± 4.2 | <0.001 |
| Left ventricular ejection fraction (%) ± SD | 60.1 ± 6.6 | 60 ± 10 | 0.263 |
| Carotid and vertebral ultrasonography | |||
| Mean Resistive Index ± SD | 0.73 ± 0.06 | 0.64 ± 0.05 | <0.001 |
| Mean Pulsatile Index ± SD | 1.45 ± 0.23 | 1.14 ± 0.16 | <0.001 |
| Left internal carotid artery | |||
| Resistive Index ± SD | 0.75 ± 0.07 | 0.64 ± 0.06 | < 0.001 |
| Pulsatile Index ± SD | 1.52 ± 0.28 | 1.12 ± 0.17 | < 0.001 |
| Right internal carotid artery | |||
| Resistive Index ± SD | 0.75 ± 0.07 | 0.64 ± 0.06 | < 0.001 |
| Pulsatile Index ± SD | 1.52 ± 0.28 | 1.14 ± 0.17 | < 0.001 |
| Left Vertebral artery | |||
| Resistive Index ± SD | 0.72 ± 0.07 | 0.65 ± 0.07 | <0.001 |
| Pulsatile Index ± SD | 1.40 ± 0.25 | 1.16 ± 0.21 | <0.001 |
| Right vertebral artery | |||
| Resistive Index ± SD | 0.72 ± 0.06 | 0.64 ± 0.08 | <0.001 |
| Pulsatile Index ± SD | 1.38 ± 0.23 | 1.12 ± 0.23 | <0.001 |
| Univariate OR (95% CI), p-Value | Multivariate OR (95% CI), p-Value | Multivariate Age-Adjusted OR (95% CI), p-Value | |
|---|---|---|---|
| Predictors of RI ≥ 0.7 Age | 1.22 (1.12–1.33), <0.001 | 1.29 (1.20–1.40), <0.001 | 1.29 (1.20–1.40), <0.001 |
| Female gender | 1.10 (1.01–1.19), 0.025 | 1.07 (0.99–1.16),0.070 | 1.07 (0.99–1.16),0.071 |
| Diabetes | 1.15 (1.04–1.27), 0.004 | 1.10 (1.02–1.18), 0.018 | 1.10 (1.02–1.19), 0.018 |
| Hypertension | 1.17 (1.06–1.29), 0.002 | 1.07 (0.99–1.16), 0.076 | 1.07 (0.99–1.16), 0.076 |
| Hyperlipidemia | 1.27 (1.15–1.39), <0.001 | 1.06 (0.98–1.55), 0.155 | 1.06 (0.98–1.15), 0.155 |
| Coronary artery disease | 1.07 (0.97–1.18), 0.173 | - | |
| Previous myocardial infarction | 1.00 (0.91–1.10), 0.944 | - | |
| Left ventricular ejection fraction | 1.05 (0.95–1.16), 0.319 | - | |
| Aortic valve stenosis | 2.49 (1.64–3.78), <0.001 | 1.65 (1.53–1.79), <0.001 | 1.66 (1.53–1.79), <0.001 |
| Predictors of PI ≥ 1.3 | |||
| Age | 1.44 (1.32–1.58), <0.001 | 1.25 (1.16–1.35), <0.001 | 1.25 (1.16–1.35), <0.001 |
| Female gender | 1.16 (1.05–1.28), 0.002 | 1.12 (1.04–1.20), 0.004 | 1.12 (1.04–1.21), 0.004 |
| Diabetes | 1.17 (1.06–1.29), 0.001 | 1.11 (1.03–1.19), 0.009 | 1.11 (1.03–1.19), 0.009 |
| Hypertension | 1.18 (1.07–1.29), 0.001 | 1.06 (0.98–1.15), 0.117 | 1.06 (0.98–1.15), 0.118 |
| Hyperlipidemia | 1.29 (1.18–1.42), <0.001 | 1.09 (1.01–1.18), 0.027 | 1.09 (1.01–1.18), 0.027 |
| Coronary artery disease | 1.10 (1.00–1.21), 0.059 | - | |
| Previous myocardial infarction | 1.01 (0.92–1.11), 0.934 | - | |
| Left ventricular ejection fraction | 1.04 (0.95–1.15), 0.388 | - | |
| Aortic valve stenosis | 1.79 (1.65–1.94), <0.001 | 1.67 (1.54–1.80), <0.001 | 1.67 (1.54–1.80), <0.001 |
| Parameter | Univariate Analysis | Multivariate Analysis with RI | Multivariate Analysis with PI |
|---|---|---|---|
| OR (95% CI), p-Value | OR (95% CI), p-Value | OR (95% CI), p-Value | |
| Age | 1.23 (1.12–1.35), 0.001 | 1.13 (1.03–1.25), 0.014 | 1.16 (1.04–1.26), 0.008 |
| Female gender | 1.12 (1.02–1.23), 0.019 | 1.07 (0.98–1.18), 0.133 | 1.07 (0.97–1.18), 0.163 |
| Diabetes | 1.11 (1.01–1.23), 0.029 | 1.05 (0.96–1.16), 0.293 | 1.06 (0.96–1.16), 0.269 |
| Hypertension | 1.12 (1.02–1.23), 0.025 | 1.07 (0.97–1.17), 0.169 | 1.07 (0.97–1.18) 0.162 |
| Hyperlipidemia | 1.01 (0.92–1.12), 0.783 | - | - |
| Coronary artery disease | 1.07 (0.97–1.18), 0.172 | - | - |
| Previous myocardial infarction | 1.01 (0.91–1.11), 0.919 | - | - |
| Left ventricle ejection fraction | 1.04 (0.95–1.15), 0.384 | - | - |
| Aortic valve stenosis | 1.10 (1.00–1.21), 0.047 | 1.07 (0.95–1.19), 0.253 | 1.05 (0.94–1.18), 0.407 |
| Peak aortic gradient | 1.10 (0.98–1.24), 0.106 | - | - |
| RI ≥ 0.7 | 1.30 (1.19–1.43),0.001 | 1.25 (1.13–1.37), <0.001 | - |
| PI ≥ 1.3 | 1.28 (1.16–1.40), <0.001 | - | 1.21 (1.10–1.34), <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baran, J.; Kleczyński, P.; Niewiara, Ł.; Podolec, J.; Badacz, R.; Gackowski, A.; Pieniążek, P.; Legutko, J.; Żmudka, K.; Przewłocki, T.; et al. Importance of Increased Arterial Resistance in Risk Prediction in Patients with Cardiovascular Risk Factors and Degenerative Aortic Stenosis. J. Clin. Med. 2021, 10, 2109. https://doi.org/10.3390/jcm10102109
Baran J, Kleczyński P, Niewiara Ł, Podolec J, Badacz R, Gackowski A, Pieniążek P, Legutko J, Żmudka K, Przewłocki T, et al. Importance of Increased Arterial Resistance in Risk Prediction in Patients with Cardiovascular Risk Factors and Degenerative Aortic Stenosis. Journal of Clinical Medicine. 2021; 10(10):2109. https://doi.org/10.3390/jcm10102109
Chicago/Turabian StyleBaran, Jakub, Paweł Kleczyński, Łukasz Niewiara, Jakub Podolec, Rafał Badacz, Andrzej Gackowski, Piotr Pieniążek, Jacek Legutko, Krzysztof Żmudka, Tadeusz Przewłocki, and et al. 2021. "Importance of Increased Arterial Resistance in Risk Prediction in Patients with Cardiovascular Risk Factors and Degenerative Aortic Stenosis" Journal of Clinical Medicine 10, no. 10: 2109. https://doi.org/10.3390/jcm10102109
APA StyleBaran, J., Kleczyński, P., Niewiara, Ł., Podolec, J., Badacz, R., Gackowski, A., Pieniążek, P., Legutko, J., Żmudka, K., Przewłocki, T., & Kabłak-Ziembicka, A. (2021). Importance of Increased Arterial Resistance in Risk Prediction in Patients with Cardiovascular Risk Factors and Degenerative Aortic Stenosis. Journal of Clinical Medicine, 10(10), 2109. https://doi.org/10.3390/jcm10102109






