Recommendations for Patients with High Return to Sports Expectations after TKA Remain Controversial
Abstract
1. Introduction
2. Experimental Section
3. Results
3.1. Survey Participants
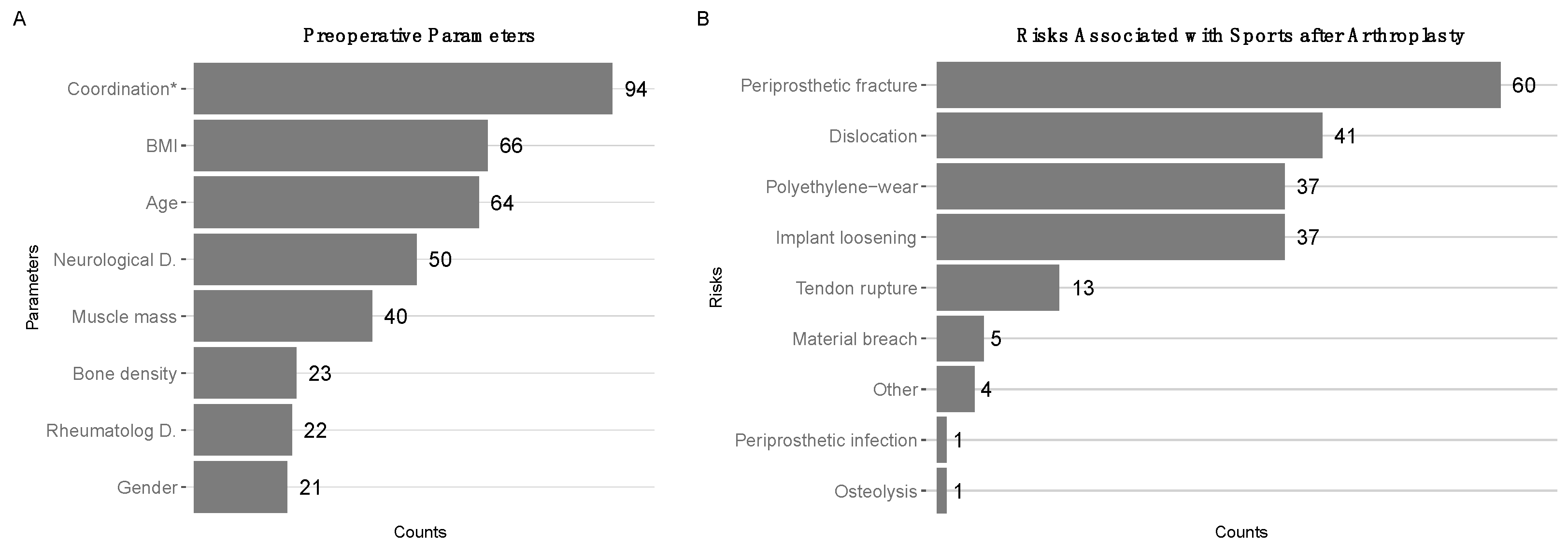
3.2. Perioperative Assessments Regarding Return to Sports after TKA
3.3. Significance of Physical Activity after TKA
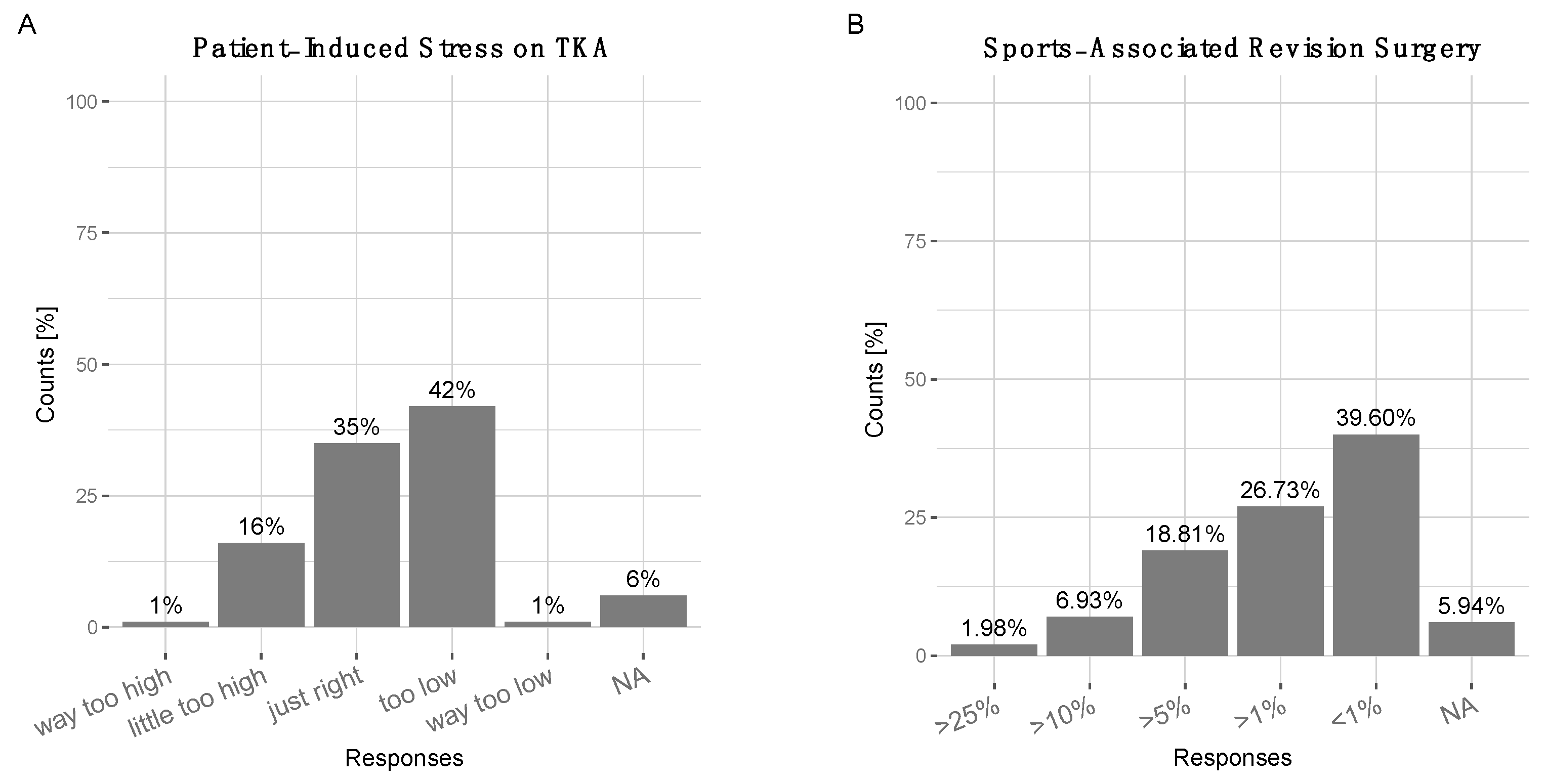
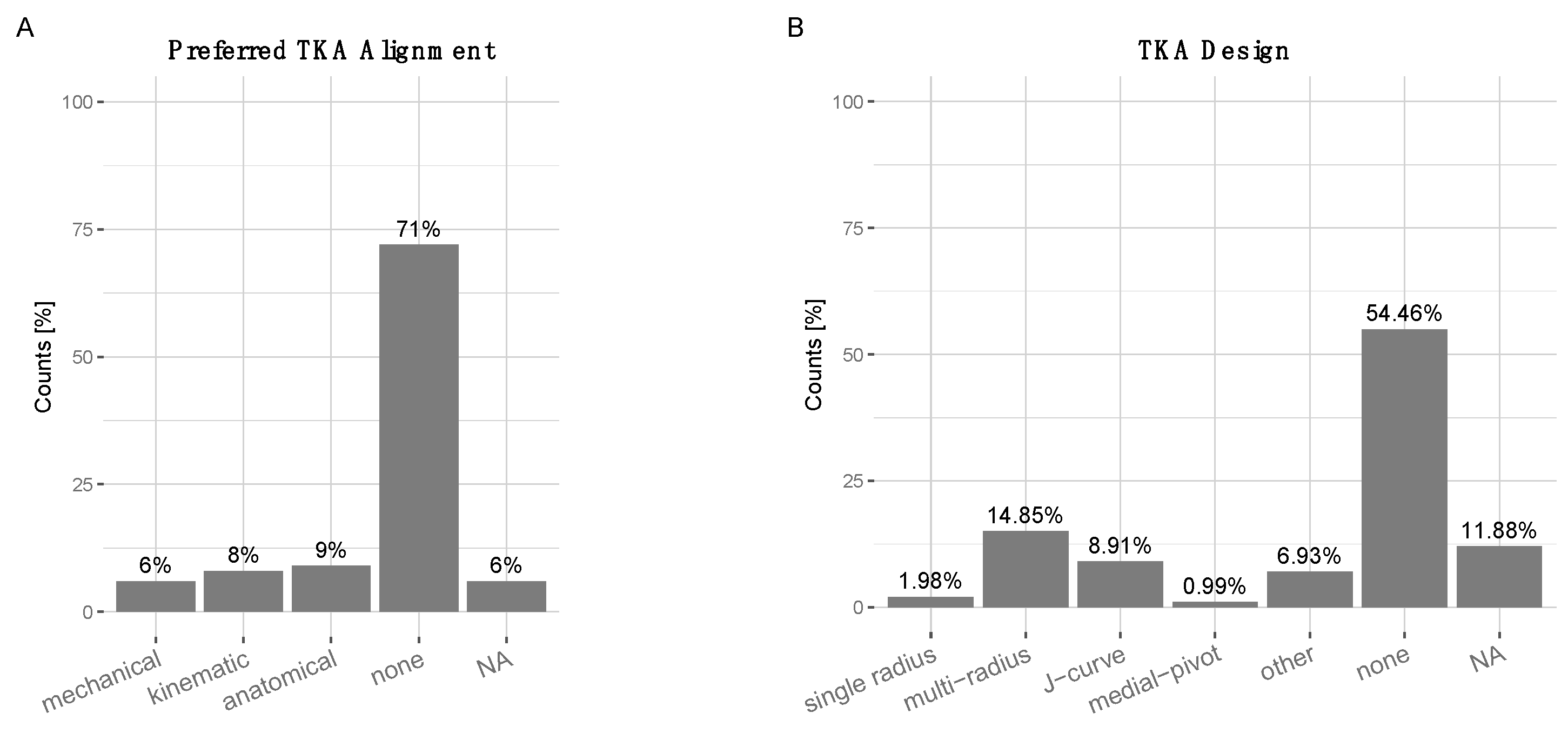
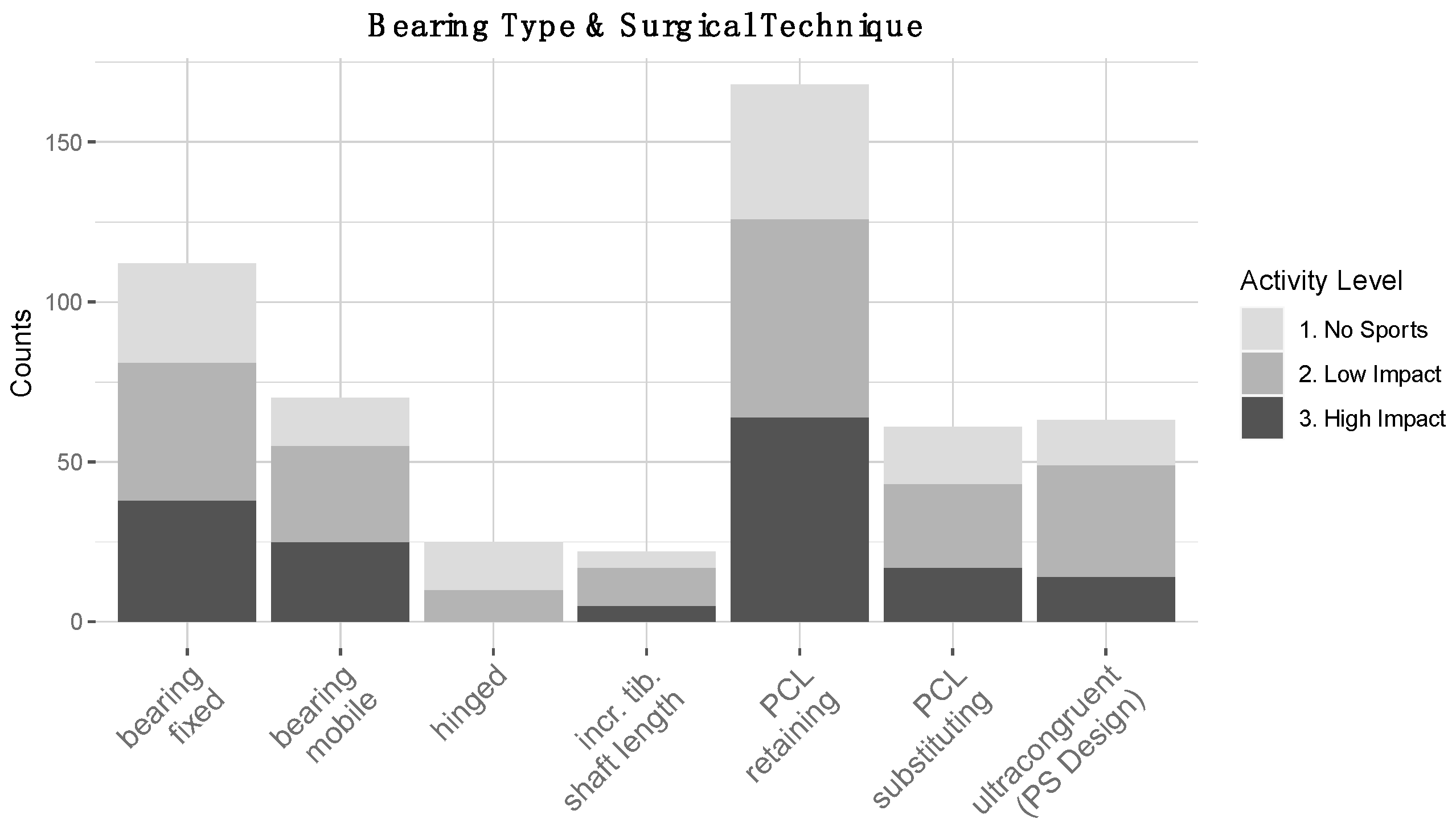
3.4. Surgical Decision-Making in Patients with High RTS Expectations after TKA
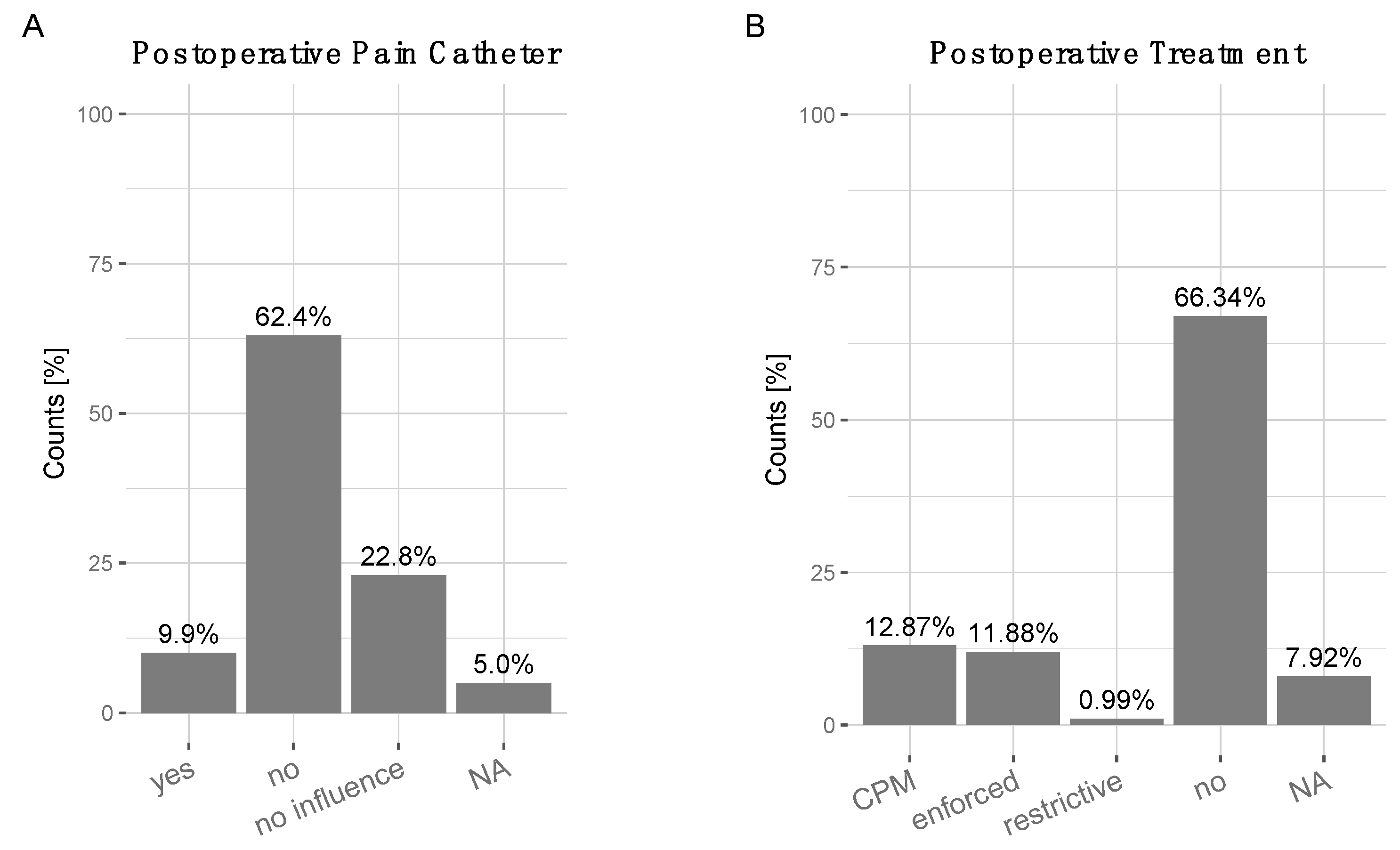
3.5. Postoperative Treatment
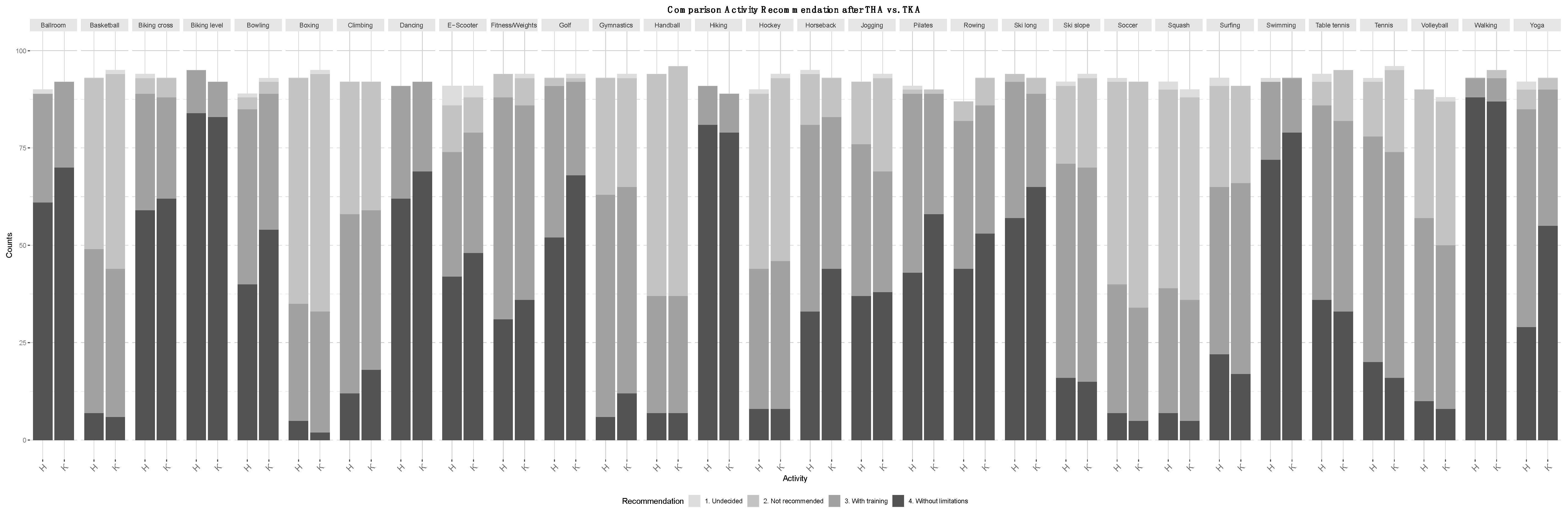
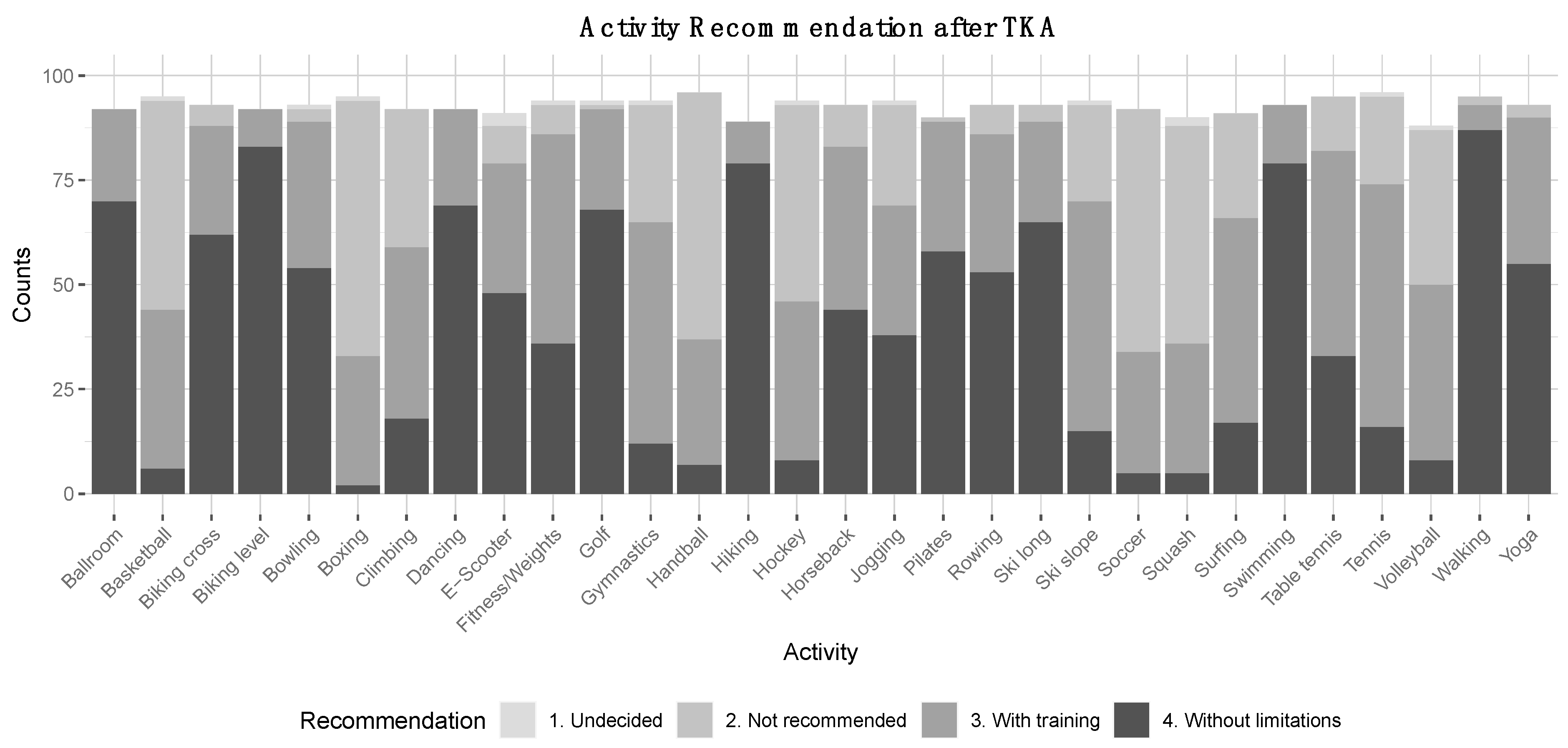
3.6. Recommendations for Patients with High RTS Expectations after TKA
4. Discussion
4.1. Sports after TKA
4.2. Surgical Techniques
4.3. Implant Specifications
4.4. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AA | anatomical alignment |
| CAS | computer-assisted surgery |
| GAS | goal attainment scaling |
| KA | kinematic alignment |
| LIA | local infiltration analgesia |
| MA | mechanical alignment NA |
| NA | not available, no response |
| PCR | posterior-cruciate ligament retaining |
| PCS | posterior-cruciate ligament substituting/sacrificing |
| PS | posterior stabilized (knee arthroplasty) |
| PSI | patient-specific instrumentation |
| RAS | robot-assisted surgery |
| ROM | range of motion |
| THA | total hip arthroplasty |
| TKA | total knee arthroplasty |
| UID | unique identity |
Appendix A
References
- Fawaz, W.S.; Masri, B.A. Allowed Activities After Primary Total Knee Arthroplasty and Total Hip Arthroplasty. Orthop. Clin. N. Am. 2020, 51, 441–452. [Google Scholar] [CrossRef]
- Kohl, H.W., 3rd; Craig, C.L.; Lambert, E.V.; Inoue, S.; Alkandari, J.R.; Leetongin, G.; Kahlmeier, S. The pandemic of physical inactivity: Global action for public health. Lancet 2012, 380, 294–305. [Google Scholar] [CrossRef]
- Almeida, G.J.; Khoja, S.S.; Piva, S.R. Physical activity after total joint arthroplasty: A narrative review. J. Sports Med. 2018, 9, 55–68. [Google Scholar] [CrossRef] [PubMed]
- Murphy, B.P.D.; Dowsey, M.M.; Choong, P.F.M. The Impact of Advanced Age on the Outcomes of Primary Total Hip and Knee Arthroplasty for Osteoarthritis: A Systematic Review. JBJS Rev. 2018, 6, e6. [Google Scholar] [CrossRef] [PubMed]
- Murphy, L.; Helmick, C.G. The impact of osteoarthritis in the United States: A population-health perspective. Am. J. Nurs. 2012, 112, S13–19. [Google Scholar] [CrossRef] [PubMed]
- Sideman, S. Hinged knee prosthesis. Q. Bull. Northwestern Univ. (Evanst. Ill.). Med. Sch. 1961, 35, 338–345. [Google Scholar]
- Inacio, M.C.S.; Paxton, E.W.; Graves, S.E.; Namba, R.S.; Nemes, S. Projected increase in total knee arthroplasty in the United States—An alternative projection model. Osteoarthr. Cartil. 2017, 25, 1797–1803. [Google Scholar] [CrossRef] [PubMed]
- Guerrero-Luduena, R.E.; Comas, M.; Espallargues, M.; Coll, M.; Pons, M.; Sabates, S.; Allepuz, A.; Castells, X. Predicting the Burden of Revision Knee Arthroplasty: Simulation of a 20-Year Horizon. Value Health 2016, 19, 680–687. [Google Scholar] [CrossRef][Green Version]
- Bryan, S.; Goldsmith, L.J.; Davis, J.C.; Hejazi, S.; MacDonald, V.; McAllister, P.; Randall, E.; Suryaprakash, N.; Wu, A.D.; Sawatzky, R. Revisiting patient satisfaction following total knee arthroplasty: A longitudinal observational study. BMC Musculoskelet Disord. 2018, 19, 423. [Google Scholar] [CrossRef]
- Bourne, R.B.; Chesworth, B.M.; Davis, A.M.; Mahomed, N.N.; Charron, K.D. Patient satisfaction after total knee arthroplasty: Who is satisfied and who is not? Clin. Orthop. Relat. Res. 2010, 468, 57–63. [Google Scholar] [CrossRef]
- Culliford, D.; Maskell, J.; Judge, A.; Cooper, C.; Prieto-Alhambra, D.; Arden, N.K.; Group, C.O.S. Future projections of total hip and knee arthroplasty in the UK: Results from the UK Clinical Practice Research Datalink. Osteoarthr. Cartil. 2015, 23, 594–600. [Google Scholar] [CrossRef] [PubMed]
- Witjes, S.; van Geenen, R.C.; Koenraadt, K.L.; van der Hart, C.P.; Blankevoort, L.; Kerkhoffs, G.M.; Kuijer, P.P. Expectations of younger patients concerning activities after knee arthroplasty: Are we asking the right questions? Qual. Life Res. 2017, 26, 403–417. [Google Scholar] [CrossRef] [PubMed]
- Kurtz, S.; Ong, K.; Lau, E.; Mowat, F.; Halpern, M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J. Bone Jt. Surg. Am. 2007, 89, 780–785. [Google Scholar] [CrossRef]
- Kurtz, S.M.; Lau, E.; Ong, K.; Zhao, K.; Kelly, M.; Bozic, K.J. Future young patient demand for primary and revision joint replacement: National projections from 2010 to 2030. Clin. Orthop. Relat. Res. 2009, 467, 2606–2612. [Google Scholar] [CrossRef]
- Gibon, E.; Goodman, M.J.; Goodman, S.B. Patient Satisfaction After Total Knee Arthroplasty: A Realistic or Imaginary Goal? Orthop. Clin. N. Am. 2017, 48, 421–431. [Google Scholar] [CrossRef]
- Dunbar, M.J.; Richardson, G.; Robertsson, O. I can’t get no satisfaction after my total knee replacement RHYMES AND REASONS. Bone Jt. Surg. 2013. [Google Scholar] [CrossRef]
- Khatib, Y.; Madan, A.; Naylor, J.M.; Harris, I.A. Do Psychological Factors Predict Poor Outcome in Patients Undergoing TKA? A Systematic Review. Clin. Orthop. Relat. Res. 2015, 473, 2630–2638. [Google Scholar] [CrossRef]
- Lau, R.L.; Gandhi, R.; Mahomed, S.; Mahomed, N. Patient satisfaction after total knee and hip arthroplasty. Clin. Geriatr. Med. 2012, 28, 349–365. [Google Scholar] [CrossRef]
- Lopez-Olivo, M.A.; Ingleshwar, A.; Landon, G.C.; Siff, S.J.; Barbo, A.; Lin, H.Y.; Suarez-Almazor, M.E. Psychosocial Determinants of Total Knee Arthroplasty Outcomes Two Years After Surgery. ACR Open Rheumatol. 2020, 2, 573–581. [Google Scholar] [CrossRef]
- Abe, H.; Sakai, T.; Nishii, T.; Takao, M.; Nakamura, N.; Sugano, N. Jogging after total hip arthroplasty. Am. J. Sports Med. 2014, 42, 131–137. [Google Scholar] [CrossRef]
- Clifford, P.E.; Mallon, W.J. Sports after total joint replacement. Clin. Sports Med. 2005, 24, 175–186. [Google Scholar] [CrossRef] [PubMed]
- Wickham, H. ggplot2: Elegant Graphics for Data Analysis; Springer: Berlin/Heidelberg, Germany, 2009; p. 35. [Google Scholar]
- OCED. Heatlh at a Glance 2019: OECD Indicators; OCED: Paris, France, 2019. [Google Scholar]
- Mont, M.A.; Rajadhyaksha, A.D.; Marxen, J.L.; Silberstein, C.E.; Hungerford, D.S. Tennis after total knee arthroplasty. Am. J. Sports Med. 2002, 30, 163–166. [Google Scholar] [CrossRef] [PubMed]
- Plassard, J.; Masson, J.B.; Malatray, M.; Swan, J.; Luceri, F.; Roger, J.; Batailler, C.; Servien, E.; Lustig, S. Factors lead to return to sports and recreational activity after total knee replacement—A retrospective study. Sicot J. 2020, 6, 11. [Google Scholar] [CrossRef] [PubMed]
- Valle, C.; Sperr, M.; Lemhofer, C.; Bartel, K.E.; Schmitt-Sody, M. Does Sports Activity Influence Total Knee Arthroplasty Durability? Analysis with a Follow-Up of 12 Years. Sportverletz Sportschaden 2017, 31, 111–115. [Google Scholar] [CrossRef] [PubMed]
- Hanreich, C.; Martelanz, L.; Koller, U.; Windhager, R.; Waldstein, W. Sport and Physical Activity Following Primary Total Knee Arthroplasty: A Systematic Review and Meta-Analysis. J. Arthroplast. 2020, 35, 2274–2285 e2271. [Google Scholar] [CrossRef]
- Hoorntje, A.; Janssen, K.Y.; Bolder, S.B.T.; Koenraadt, K.L.M.; Daams, J.G.; Blankevoort, L.; Kerkhoffs, G.; Kuijer, P. The Effect of Total Hip Arthroplasty on Sports and Work Participation: A Systematic Review and Meta-Analysis. Sports Med. 2018, 48, 1695–1726. [Google Scholar] [CrossRef]
- Hoorntje, A.; Waterval-Witjes, S.; Koenraadt, K.L.M.; Kuijer, P.; Blankevoort, L.; Kerkhoffs, G.; van Geenen, R.C.I. Goal Attainment Scaling Rehabilitation Improves Satisfaction with Work Activities for Younger Working Patients After Knee Arthroplasty: Results from the Randomized Controlled ACTION Trial. J. Bone Jt. Surg Am. 2020, 102, 1445–1453. [Google Scholar] [CrossRef]
- Hoorntje, A.; Witjes, S.; Kuijer, P.; Koenraadt, K.L.M.; van Geenen, R.C.I.; Daams, J.G.; Getgood, A.; Kerkhoffs, G. High Rates of Return to Sports Activities and Work After Osteotomies Around the Knee: A Systematic Review and Meta-Analysis. Sports Med. 2017, 47, 2219–2244. [Google Scholar] [CrossRef]
- Healy, W.L.; Iorio, R.; Lemos, M.J. Athletic Activity after Joint Replacement. Am. J. Sports Med. 2001, 29. [Google Scholar] [CrossRef]
- Healy, W.L.; Sharma, S.; Schwartz, B.; Iorio, R. Athletic activity after total joint arthroplasty. J. Bone Jt. Surg Am. 2008, 90, 2245–2252. [Google Scholar] [CrossRef]
- Schmalzried, T.P.; Shepherd, E.F.; Dorey, F.J.; Jackson, W.O.; dela Rosa, M.; Fa’vae, F.; McKellop, H.A.; McClung, C.D.; Martell, J.; Moreland, J.R.; et al. The John Charnley Award. Wear is a function of use, not time. Clin. Orthop Relat Res. 2000, 36–46. [Google Scholar] [CrossRef] [PubMed]
- Kuster, M.S.; Stachowiak, G.W. Factors affecting polyethylene wear in total knee arthroplasty. Orthopedics 2002, 25, s235–S242. [Google Scholar] [PubMed]
- D’Lima, D.D.; Steklov, N.; Patil, S.; Colwell, C.W., Jr. The Mark Coventry Award: In vivo knee forces during recreation and exercise after knee arthroplasty. Clin. Orthop. Relat. Res. 2008, 466, 2605–2611. [Google Scholar] [CrossRef] [PubMed]
- Widhalm, R.; Höfer, G.; Krugluger, J.; Bartalsky, L. Is there greater danger of sports injury or osteoporosis caused by inactivity in patients with hip prosthesis? Sequelae for long-term stability of prosthesis anchorage. Z. Orthop. Ihre Grenzgeb 1990, 128, 139–143. [Google Scholar] [CrossRef]
- Kuster, M.S. Exercise recommendations after total joint replacement: A review of the current literature and proposal of scientifically based guidelines. Sports Med. 2002, 32, 433–445. [Google Scholar] [CrossRef]
- Girard, J.; Miletic, B.; Deny, A.; Migaud, H.; Fouilleron, N. Can patients return to high-impact physical activities after hip resurfacing? A prospective study. Int. Orthop. 2013, 37, 1019–1024. [Google Scholar] [CrossRef]
- Rochoy, M.; Six, J.; Favre, J.; Lagrange, N.; Lefebvre, J.M.; Rollier, J.C.; Girard, J. Does hip or knee joint replacement decrease chances to complete an ultra-trail race? Study in participants at the Ultra-Trail du Mont Blanc(R). Orthop. Traumatol. Surg. Res. Otsr 2020, 106, 1539–1544. [Google Scholar] [CrossRef]
- Ollivier, M.; Frey, S.; Parratte, S.; Flecher, X.; Argenson, J.N. Does impact sport activity influence total hip arthroplasty durability? Clin. Orthop. Relat. Res. 2012, 470, 3060–3066. [Google Scholar] [CrossRef]
- Mont, M.A.; Marker, D.R.; Seyler, T.M.; Jones, L.C.; Kolisek, F.R.; Hungerford, D.S. High-impact sports after total knee arthroplasty. J. Arthroplast. 2008, 23, 80–84. [Google Scholar] [CrossRef]
- Swanson, E.A.; Schmalzried, T.P.; Dorey, F.J. Activity recommendations after total hip and knee arthroplasty: A survey of the American Association for Hip and Knee Surgeons. J. Arthroplast. 2009, 24, 120–126. [Google Scholar] [CrossRef]
- Huch, K.; Muller, K.A.; Sturmer, T.; Brenner, H.; Puhl, W.; Gunther, K.P. Sports activities 5 years after total knee or hip arthroplasty: The Ulm Osteoarthritis Study. Ann. Rheum. Dis. 2005, 64, 1715–1720. [Google Scholar] [CrossRef] [PubMed]
- Von Langenbeck, B. Zur resection des kniegellenks. Verh. Der Dtsch. Ges. Churg. 1878, 7, 23–30. [Google Scholar]
- Hofmann, A.A.; Plaster, R.L.; Murdock, L.E. Subvastus (Southern) approach for primary total knee arthroplasty. Clin. Orthop. Relat Res. 1991, 70–77. [Google Scholar] [CrossRef]
- Engh, G.A.; Holt, B.T.; Parks, N.L. A midvastus muscle-splitting approach for total knee arthroplasty. J. Arthroplast. 1997, 12, 322–331. [Google Scholar] [CrossRef]
- Khan, R.J.K.; Keogh, A.; Fick, D.P.; Wood, D.J. Surgical approaches in total knee arthroplasty. Cochrane Database Syst. Rev. 2005. [Google Scholar] [CrossRef]
- Gunst, S.; Villa, V.; Magnussen, R.; Servien, E.; Lustig, S.; Neyret, P. Equivalent results of medial and lateral parapatellar approach for total knee arthroplasty in mild valgus deformities. Int. Orthop. 2016, 40, 945–951. [Google Scholar] [CrossRef]
- Bonutti, P.M.; Zywiel, M.G.; Ulrich, S.D.; Stroh, D.A.; Seyler, T.M.; Mont, M.A. A Comparison of Subvastus and Midvastus Approaches in Minimally Invasive Total Knee Arthroplasty. J. Bone Jt. Surg. Am. 2010, 92, 575–582. [Google Scholar] [CrossRef]
- Lotke, P.A.; Ecker, M.L. Influence of positioning of prosthesis in total knee replacement. J. Bone Jt. Surg Am. 1977, 59, 77–79. [Google Scholar] [CrossRef]
- Becker, R.; Tandogan, N.R.; Violante, B. Alignment in total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 2393–2394. [Google Scholar] [CrossRef]
- Fu, H.; Wang, J.; Zhou, S.; Cheng, T.; Zhang, W.; Wang, Q.; Zhang, X. No difference in mechanical alignment and femoral component placement between patient-specific instrumentation and conventional instrumentation in TKA. Knee Surg. Sports Traumatol. Arthrosc. 2015, 23, 3288–3295. [Google Scholar] [CrossRef]
- Riviere, C.; Iranpour, F.; Auvinet, E.; Howell, S.; Vendittoli, P.A.; Cobb, J.; Parratte, S. Alignment options for total knee arthroplasty: A systematic review. Orthop. Traumatol. Surg. Res. Otsr 2017, 103, 1047–1056. [Google Scholar] [CrossRef] [PubMed]
- Dall’Oca, C.; Ricci, M.; Vecchini, E.; Giannini, N.; Lamberti, D.; Tromponi, C.; Magnan, B. Evolution of TKA design. Acta Biomed. 2017, 88, 17–31. [Google Scholar] [CrossRef] [PubMed]
- Ranawat, C.S.; White, P.B.; West, S.; Ranawat, A.S. Clinical and Radiographic Results of Attune and PFC Sigma Knee Designs at 2-Year Follow-Up: A Prospective Matched-Pair Analysis. J. Arthroplast. 2017, 32, 431–436. [Google Scholar] [CrossRef] [PubMed]
- Bateman, D.K.; Preston, J.S.; Mennona, S.; Gui, E.; Kayiaros, S. Comparison Between the Attune and PFC Sigma in Total Knee Arthroplasty: No Difference in Patellar Clunk and Crepitus or Anterior Knee Pain. Orthopedics 2020, 43, e508–e514. [Google Scholar] [CrossRef]
- Bonutti, P.M.; Khlopas, A.; Chughtai, M.; Cole, C.; Gwam, C.U.; Harwin, S.F.; Whited, B.; Omiyi, D.E.; Drumm, J.E. Unusually High Rate of Early Failure of Tibial Component in ATTUNE Total Knee Arthroplasty System at Implant-Cement Interface. J. Knee Surg. 2017, 30, 435–439. [Google Scholar] [CrossRef]
- Carey, B.W.; Harty, J. A comparison of clinical- and patient-reported outcomes of the cemented ATTUNE and PFC sigma fixed bearing cruciate sacrificing knee systems in patients who underwent total knee replacement with both prostheses in opposite knees. J. Orthop. Surg. Res. 2018, 13, 54. [Google Scholar] [CrossRef]
- Molloy, I.B.; Keeney, B.J.; Sparks, M.B.; Paddock, N.G.; Koenig, K.M.; Moschetti, W.E.; Jevsevar, D.S. Short term patient outcomes after total knee arthroplasty: Does the implant matter? Knee 2019, 26, 687–699. [Google Scholar] [CrossRef]
- Song, S.J.; Kang, S.G.; Park, C.H.; Bae, D.K. Comparison of Clinical Results and Risk of Patellar Injury between Attune and PFC Sigma Knee Systems. Knee Surg. Relat. Res. 2018, 30, 334–340. [Google Scholar] [CrossRef]
- Staats, K.; Wannmacher, T.; Weihs, V.; Koller, U.; Kubista, B.; Windhager, R. Modern cemented total knee arthroplasty design shows a higher incidence of radiolucent lines compared to its predecessor. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 1148–1155. [Google Scholar] [CrossRef]
- Parcells, B.W.; Tria, A.J., Jr. The Cruciate Ligaments in Total Knee Arthroplasty. Am. J. Orthop. 2016, 45, E153–160. [Google Scholar]
- Verra, W.C.; van den Boom, L.G.; Jacobs, W.; Clement, D.J.; Wymenga, A.A.; Nelissen, R.G. Retention versus sacrifice of the posterior cruciate ligament in total knee arthroplasty for treating osteoarthritis. Cochrane Database Syst Rev. 2013, CD004803. [Google Scholar] [CrossRef] [PubMed]
- Götz, J.; Beckmann, J.; Sperrer, I.; Baier, C.; Dullien, S.; Grifka, J.; Koeck, F. Retrospective comparative study shows no significant difference in postural stability between cruciate-retaining (CR) and cruciate-substituting (PS) total knee implant systems. Int. Orthop. 2016, 40, 1441–1446. [Google Scholar] [CrossRef] [PubMed]
- Vandekerckhove, P.J.; Parys, R.; Tampere, T.; Linden, P.; Van den Daelen, L.; Verdonk, P.C. Does cruciate retention primary total knee arthroplasty affect proprioception, strength and clinical outcome? Knee Surg. Sports Traumatol. Arthrosc 2015, 23, 1644–1652. [Google Scholar] [CrossRef] [PubMed]
- Cho, K.Y.; Kim, K.I.; Song, S.J.; Bae, D.K. Does Cruciate-Retaining Total Knee Arthroplasty Show Better Quadriceps Recovery than Posterior-Stabilized Total Knee Arthroplasty?—Objective Measurement with a Dynamometer in 102 Knees. Clin. Orthop. Surg. 2016, 8, 379–385. [Google Scholar] [CrossRef]
- van den Boom, L.G.; Halbertsma, J.P.; van Raaij, J.J.; Brouwer, R.W.; Bulstra, S.K.; van den Akker-Scheek, I. No difference in gait between posterior cruciate retention and the posterior stabilized design after total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 3135–3141. [Google Scholar] [CrossRef]
- Sadoghi, P. Controversies in total knee arthroplasty: Cochrane evidence or surgeons’ philosophy? Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 3331–3332. [Google Scholar] [CrossRef]
- Pritchett, J.W. Patient preferences in knee prostheses. J. Bone Jt. Surg. Br. Vol. 2004, 86, 979–982. [Google Scholar] [CrossRef]
- Capella, M.; Dolfin, M.; Saccia, F. Mobile bearing and fixed bearing total knee arthroplasty. Ann. Transl Med. 2016, 4, 127. [Google Scholar] [CrossRef]
- Cao, Z.; Niu, C.; Gong, C.; Sun, Y.; Xie, J.; Song, Y. Comparison of Fixed-Bearing and Mobile-Bearing Unicompartmental Knee Arthroplasty: A Systematic Review and Meta-Analysis. J. Arthroplast. 2019, 34, 3114–3123 e3113. [Google Scholar] [CrossRef]
- Kim, Y.H.; Park, J.W.; Kim, J.S. The Long-Term Results of Simultaneous High-Flexion Mobile-Bearing and Fixed-Bearing Total Knee Arthroplasties Performed in the Same Patients. J. Arthroplast. 2019, 34, 501–507. [Google Scholar] [CrossRef]
- Poirier, N.; Graf, P.; Dubrana, F. Mobile-bearing versus fixed-bearing total knee implants. Results of a series of 100 randomised cases after 9 years follow-up. Orthop. Traumatol. Surg. Res. Otsr. 2015, 101, S187–S192. [Google Scholar] [CrossRef] [PubMed]
- Artz, N.J.; Hassaballa, M.A.; Robinson, J.R.; Newman, J.H.; Porteous, A.J.; Murray, J.R. Patient Reported Kneeling Ability in Fixed and Mobile Bearing Knee Arthroplasty. J. Arthroplast. 2015, 30, 2159–2163. [Google Scholar] [CrossRef] [PubMed]
- Amundson, A.W.; Johnson, R.L.; Abdel, M.P.; Mantilla, C.B.; Panchamia, J.K.; Taunton, M.J.; Kralovec, M.E.; Hebl, J.R.; Schroeder, D.R.; Pagnano, M.W.; et al. A Three-arm Randomized Clinical Trial Comparing Continuous Femoral Plus Single-injection Sciatic Peripheral Nerve Blocks versus Periarticular Injection with Ropivacaine or Liposomal Bupivacaine for Patients Undergoing Total Knee Arthroplasty. Anesthesiology 2017, 126, 1139–1150. [Google Scholar] [CrossRef] [PubMed]
- Berninger, M.T.; Friederichs, J.; Leidinger, W.; Augat, P.; Bühren, V.; Fulghum, C.; Reng, W. Effect of local infiltration analgesia, peripheral nerve blocks, general and spinal anesthesia on early functional recovery and pain control in unicompartmental knee arthroplasty. BMC Musculoskelet Disord. 2018, 19, 249. [Google Scholar] [CrossRef]
- Choi, S.; O’Hare, T.; Gollish, J.; Paul, J.E.; Kreder, H.; Thorpe, K.E.; Katz, J.D.; Mamdani, M.; Moisiuk, P.; McCartney, C.J. Optimizing Pain and Rehabilitation After Knee Arthroplasty: A Two-Center, Randomized Trial. Anesth. Analg. 2016, 123, 1316–1324. [Google Scholar] [CrossRef]
- Fenten, M.G.E.; Bakker, S.M.K.; Scheffer, G.J.; Wymenga, A.B.; Stienstra, R.; Heesterbeek, P.J.C. Femoral nerve catheter vs local infiltration for analgesia in fast track total knee arthroplasty: Short-term and long-term outcomes. Br. J. Anaesth. 2018, 121, 850–858. [Google Scholar] [CrossRef]
- Lan, F.; Shen, Y.; Ma, Y.; Cao, G.; Philips, N.; Zhang, T.; Wang, T. Continuous Adductor Canal Block used for postoperative pain relief after medial Unicondylar Knee Arthroplasty: A randomized, double-blind, placebo-controlled trial. BMC Anesth. 2019, 19, 114. [Google Scholar] [CrossRef]
- Smith, E.B.; Kazarian, G.S.; Maltenfort, M.G.; Lonner, J.H.; Sharkey, P.F.; Good, R.P. Periarticular Liposomal Bupivacaine Injection Versus Intra-Articular Bupivacaine Infusion Catheter for Analgesia After Total Knee Arthroplasty: A Double-Blinded, Randomized Controlled Trial. J. Bone Jt. Surg Am. 2017, 99, 1337–1344. [Google Scholar] [CrossRef]
- Soffin, E.M.; Wu, C.L. Regional and Multimodal Analgesia to Reduce Opioid Use After Total Joint Arthroplasty: A Narrative Review. HSS J. 2019, 15, 57–65. [Google Scholar] [CrossRef]
- Harvey, L.A.; Brosseau, L.; Herbert, R.D. Continuous passive motion following total knee arthroplasty in people with arthritis. Cochrane Database Syst Rev. 2014, CD004260. [Google Scholar] [CrossRef]
- Hoorntje, A.; Witjes, S.; Kuijer, P.; Bussmann, J.B.J.; Horemans, H.L.D.; Kerkhoffs, G.; van Geenen, R.C.I.; Koenraadt, K.L.M. Does Activity-Based Rehabilitation With Goal Attainment Scaling Increase Physical Activity Among Younger Knee Arthroplasty Patients? Results From the Randomized Controlled ACTION Trial. J. Arthroplast. 2020, 35, 706–711. [Google Scholar] [CrossRef] [PubMed]
- Cheng, T.; Pan, X.Y.; Mao, X.; Zhang, G.Y.; Zhang, X.L. Little clinical advantage of computer-assisted navigation over conventional instrumentation in primary total knee arthroplasty at early follow-up. Knee 2012, 19, 237–245. [Google Scholar] [CrossRef] [PubMed]
- Naal, F.D.; Fischer, M.; Preuss, A.; Goldhahn, J.; von Knoch, F.; Preiss, S.; Munzinger, U.; Drobny, T. Return to sports and recreational activity after unicompartmental knee arthroplasty. Am. J. Sports Med. 2007, 35, 1688–1695. [Google Scholar] [CrossRef] [PubMed]
- Bergmann, G.; Bender, A.; Graichen, F.; Dymke, J.; Rohlmann, A.; Trepczynski, A.; Heller, M.O.; Kutzner, I. Standardized loads acting in knee implants. PLoS ONE 2014, 9, e86035. [Google Scholar] [CrossRef] [PubMed]
- Damm, P.; Kutzner, I.; Bergmann, G.; Rohlmann, A.; Schmidt, H. Comparison of in vivo measured loads in knee, hip and spinal implants during level walking. J. Biomech. 2017, 51, 128–132. [Google Scholar] [CrossRef] [PubMed]
- Kutzner, I.; Bender, A.; Dymke, J.; Duda, G.; von Roth, P.; Bergmann, G. Mediolateral force distribution at the knee joint shifts across activities and is driven by tibiofemoral alignment. Bone Jt. J. 2017, 99-B, 779–787. [Google Scholar] [CrossRef] [PubMed]
- Schwachmeyer, V.; Kutzner, I.; Bornschein, J.; Bender, A.; Dymke, J.; Bergmann, G. Medial and lateral foot loading and its effect on knee joint loading. Clin. Biomech. 2015, 30, 860–866. [Google Scholar] [CrossRef]
- Dagneaux, L.; Bourlez, J.; Degeorge, B.; Canovas, F. Return to sport after total or unicompartmental knee arthroplasty: An informative guide for residents to patients. EFORT Open Rev. 2017, 2, 496–501. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vu-Han, T.-L.; Gwinner, C.; Perka, C.; Hardt, S. Recommendations for Patients with High Return to Sports Expectations after TKA Remain Controversial. J. Clin. Med. 2021, 10, 54. https://doi.org/10.3390/jcm10010054
Vu-Han T-L, Gwinner C, Perka C, Hardt S. Recommendations for Patients with High Return to Sports Expectations after TKA Remain Controversial. Journal of Clinical Medicine. 2021; 10(1):54. https://doi.org/10.3390/jcm10010054
Chicago/Turabian StyleVu-Han, Tu-Lan, Clemens Gwinner, Carsten Perka, and Sebastian Hardt. 2021. "Recommendations for Patients with High Return to Sports Expectations after TKA Remain Controversial" Journal of Clinical Medicine 10, no. 1: 54. https://doi.org/10.3390/jcm10010054
APA StyleVu-Han, T.-L., Gwinner, C., Perka, C., & Hardt, S. (2021). Recommendations for Patients with High Return to Sports Expectations after TKA Remain Controversial. Journal of Clinical Medicine, 10(1), 54. https://doi.org/10.3390/jcm10010054




