Evaluation of Streptococcus uberis Surface Proteins as Vaccine Antigens to Control S. uberis Mastitis in Dairy Cows
Abstract
1. Introduction
2. Materials and Methods
2.1. Extraction of SUSP
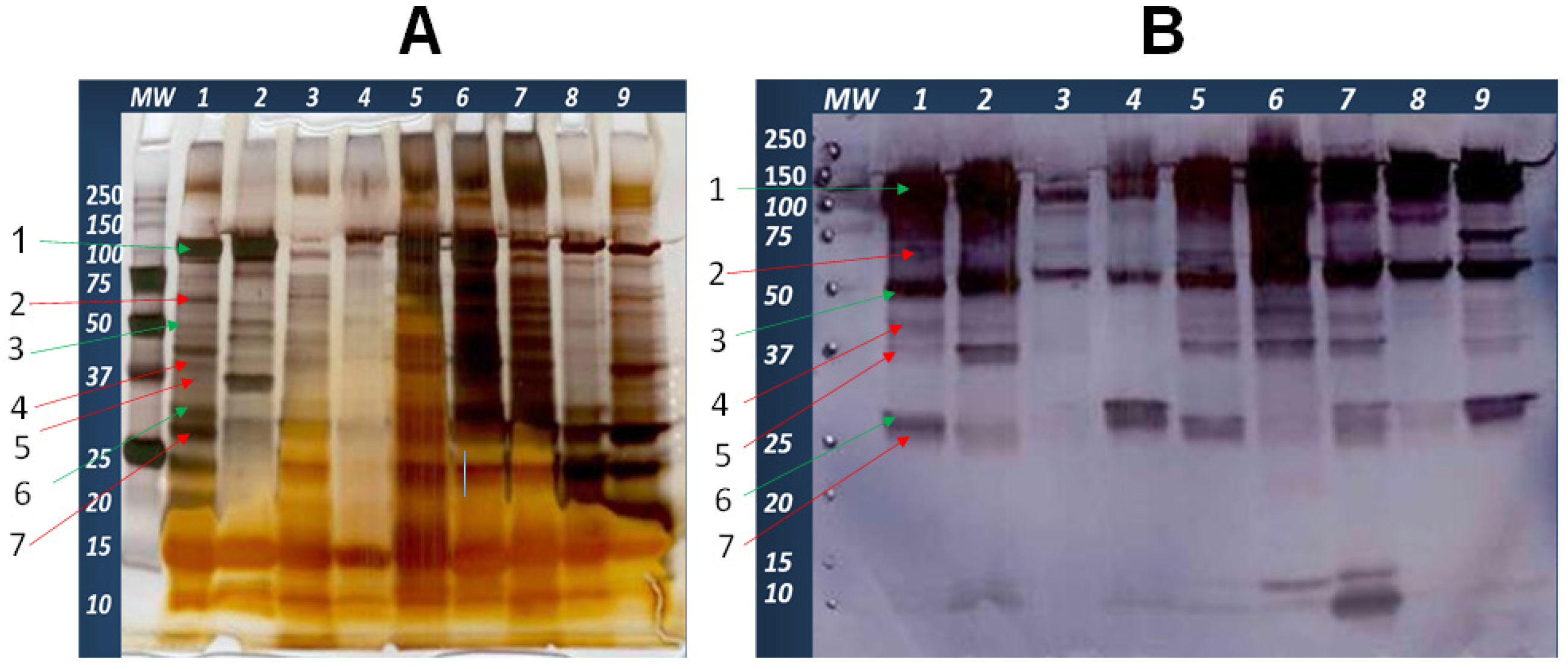
2.2. Evaluation of SUSP by Sodium Dodecyl Sulfate-Polyacrylamide Gel Electrophoresis (SDS-PAGE)
2.3. Evaluation of SUSP by Western Blot
2.4. Identification of Immunoreactive Proteins in the SUSP from S. uberis UT888 by Sequencing from Gel Band
2.5. Evaluation of Immune Responses Induced by SUSP Vaccine
2.5.1. Experimental Animals and Vaccination Protocol
2.5.2. Clinical Assessment of Animals Following Vaccination
2.5.3. Sample Collection
2.5.4. Evaluation of Anti-SUSP IgG Antibody in Milk and Blood
2.6. Experimental Infection and Assessment of Efficacy
2.6.1. Challenge Inoculum Preparation and Challenge
2.6.2. Clinical Examination of Cows after Challenge
2.6.3. Sample Collection
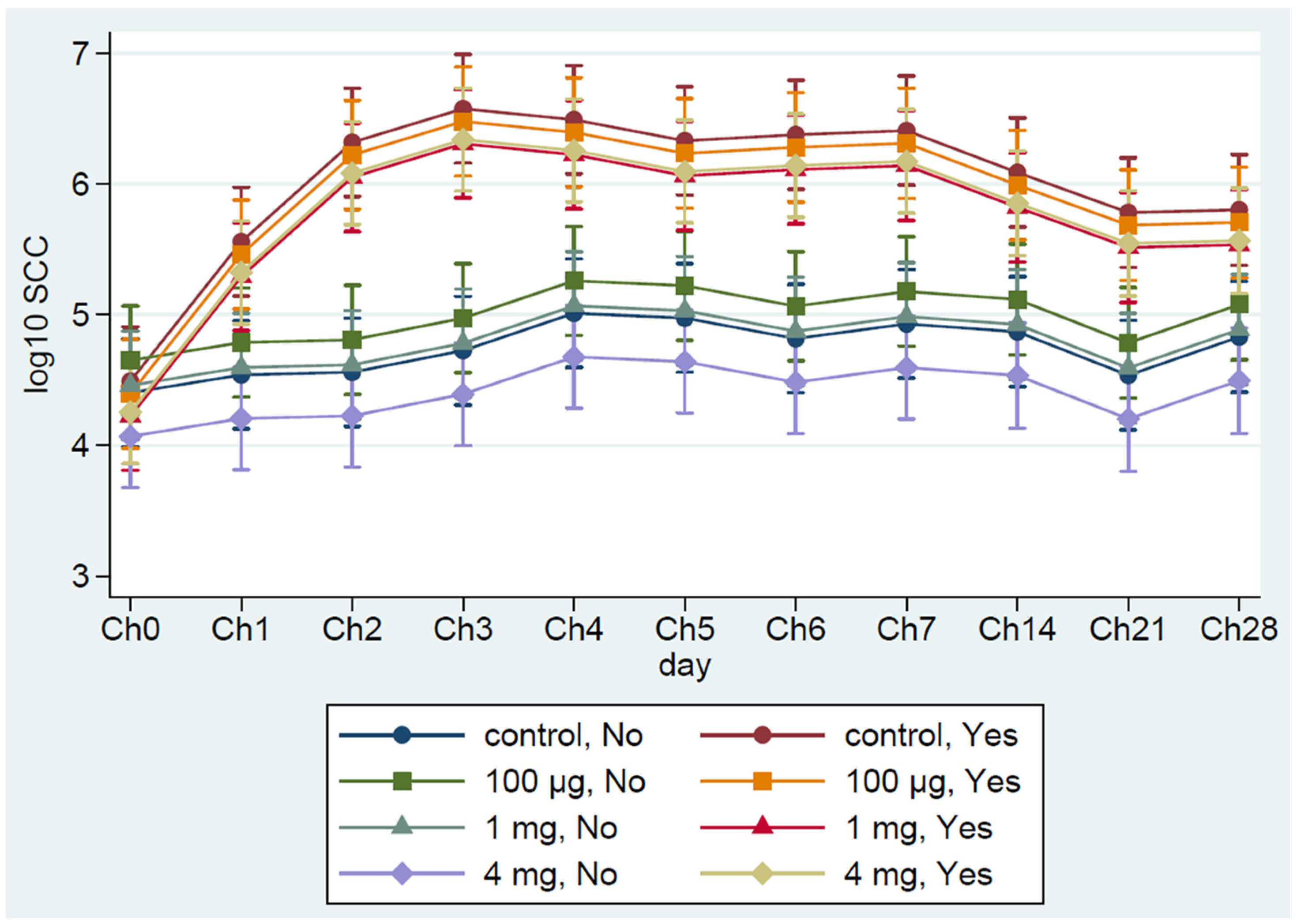
2.6.4. Somatic Cell Count (SCC)
2.6.5. Milk Bacterial Count
2.6.6. Streptococcus Uberis Identification
2.6.7. Treatment of Cows That Developed Clinical Mastitis
2.7. Statistical Analysis
3. Results
3.1. Extraction of SUSP and Evaluation of Their Immunoreactivity under In Vitro Condition
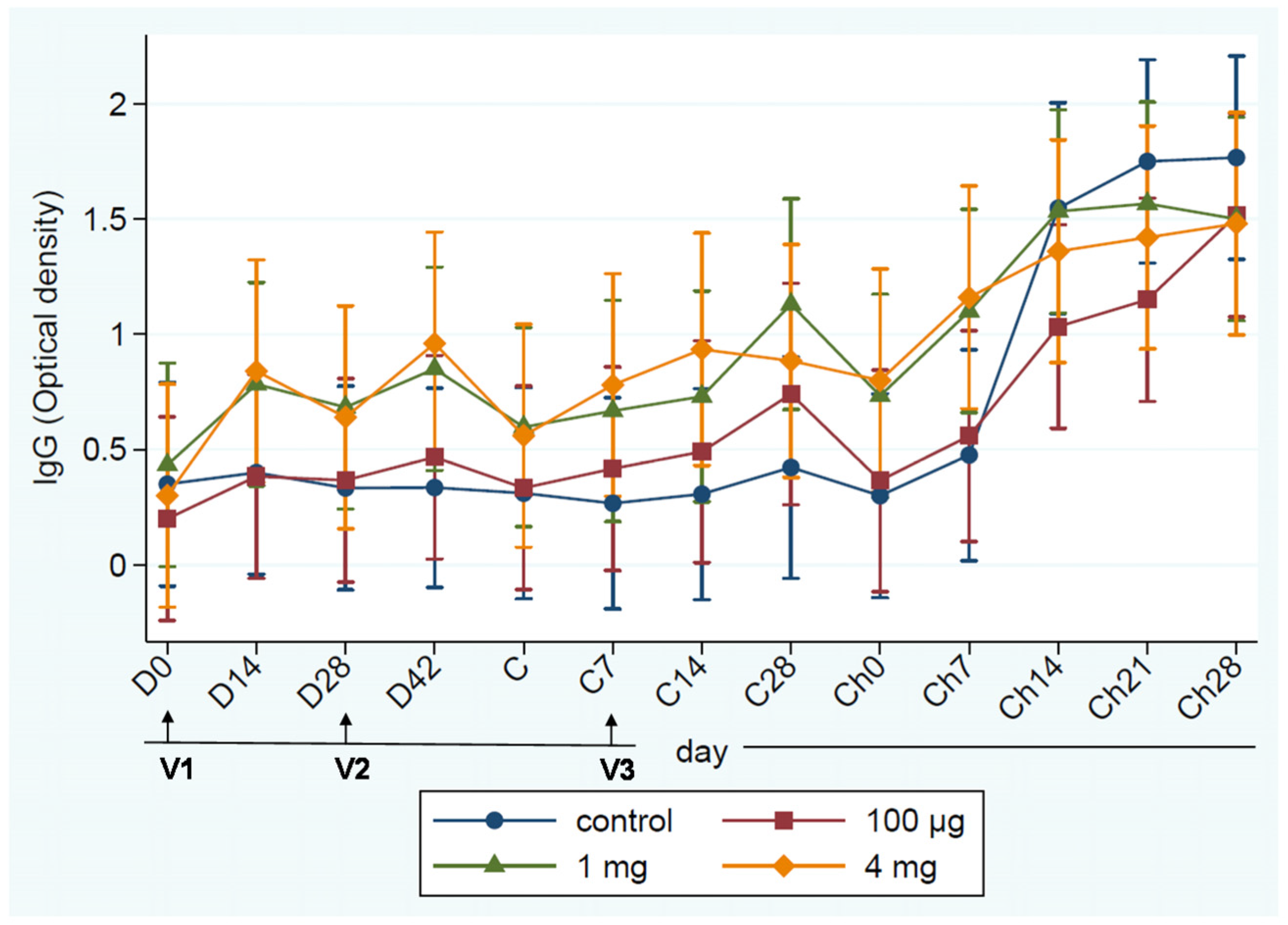
3.2. Evaluation of the Immunogenicity of SUSP in Dairy Cows
3.2.1. Safety of SUSP Vaccine
3.2.2. Immunogenicity of SUSP Vaccine and Its Efficacy
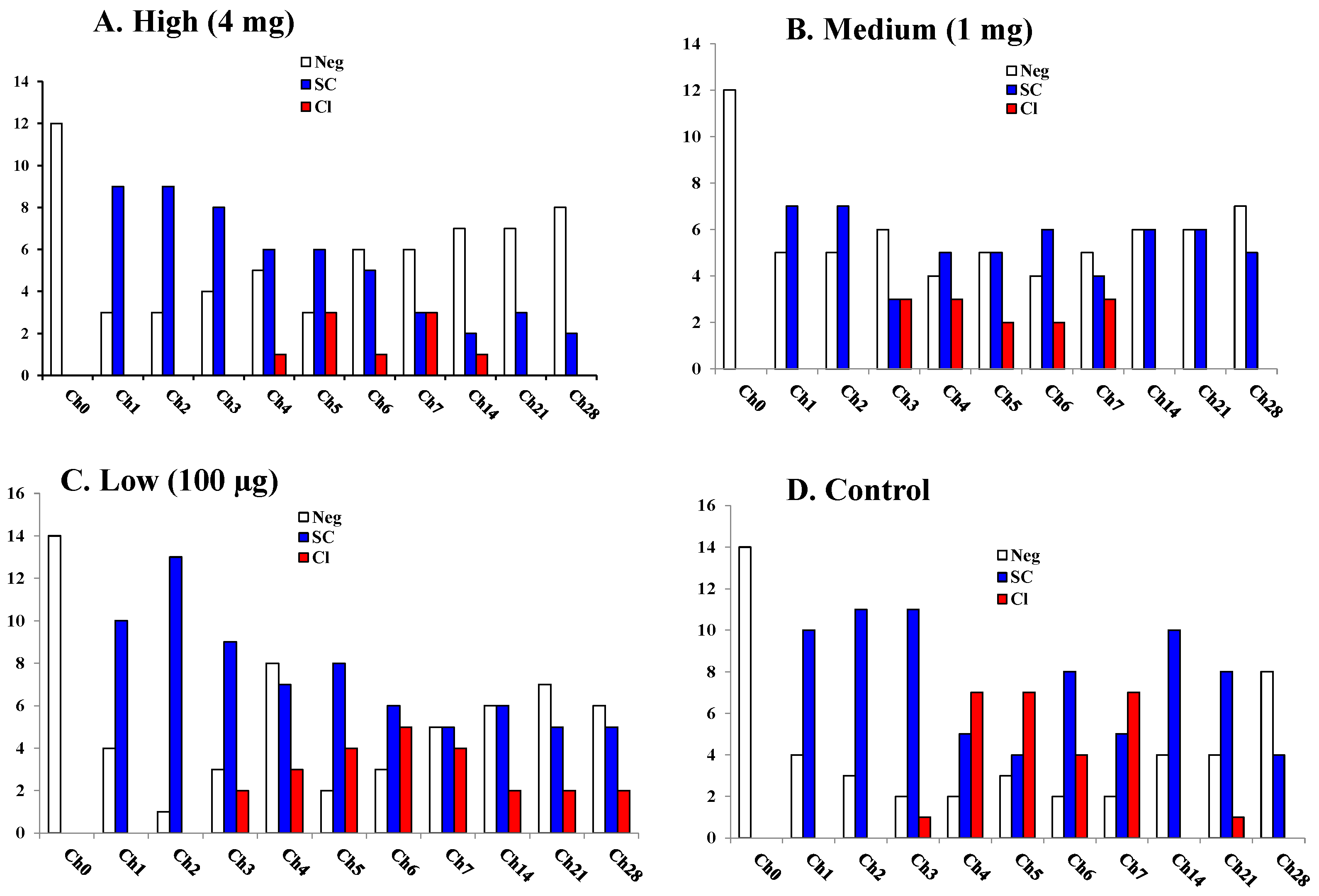
3.2.3. Milk Bacterial Counts
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tassi, R.; McNeilly, T.N.; Fitzpatrick, J.L.; Fontaine, M.C.; Reddick, D.; Ramage, C.; Lutton, M.; Schukken, Y.H.; Zadoks, R.N. Strain-specific pathogenicity of putative host-adapted and nonadapted strains of Streptococcus uberis in dairy cattle. J. Dairy Sci. 2013, 96, 5129–5145. [Google Scholar] [CrossRef]
- Zadoks, R.N.; Gillespie, B.E.; Barkema, H.W.; Sampimon, O.C.; Oliver, S.P.; Schukken, Y.H. Clinical, epidemiological and molecular characteristics of Streptococcus uberis infections in dairy herds. Epidemiol. Infect. 2003, 130, 335–349. [Google Scholar] [CrossRef]
- Collado, R.; Montbrau, C.; Sitja, M.; Prenafeta, A. Study of the efficacy of a Streptococcus uberis mastitis vaccine against an experimental intramammary infection with a heterologous strain in dairy cows. J. Dairy Sci. 2018, 101, 10290–10302. [Google Scholar] [CrossRef]
- Finch, J.M.; Hill, A.W.; Field, T.R.; Leigh, J.A. Local vaccination with killed Streptococcus uberis protects the bovine mammary gland against experimental intramammary challenge with the homologous strain. Infect. Immun. 1994, 62, 3599–3603. [Google Scholar] [CrossRef] [PubMed]
- Finch, J.M.; Winter, A.; Walton, A.W.; Leigh, J.A. Further studies on the efficacy of a live vaccine against mastitis caused by Streptococcus uberis. Vaccine 1997, 15, 1138–1143. [Google Scholar] [CrossRef]
- Fontaine, M.C.; Perez-Casal, J.; Song, X.M.; Shelford, J.; Willson, P.J.; Potter, A.A. Immunisation of dairy cattle with recombinant Streptococcus uberis GapC or a chimeric CAMP antigen confers protection against heterologous bacterial challenge. Vaccine 2002, 20, 2278–2286. [Google Scholar] [CrossRef]
- Leigh, J.A. Letter to the editor, Immunisation of dairy cattle with recombinant Streptococcus uberis GapC or a chimeric CAMP antigen confers protection against heterologous bacterial challenge. M.C. Fontaine et al. [Vaccine 20 (2002) 2278-2286]. Vaccine 2002, 20, 3047–3048. [Google Scholar] [CrossRef]
- Lincoln, R.A.; Leigh, J.A. Characterization of a novel plasminogen activator from Streptococcus uberis. Adv. Exp. Med. Biol. 1997, 418, 643–645. [Google Scholar] [CrossRef]
- Leigh, J.A.; Lincoln, R.A. Streptococcus uberis acquires plasmin activity following growth in the presence of bovine plasminogen through the action of its specific plasminogen activator. FEMS Microbiol. Lett. 1997, 154, 23–29. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Leigh, J.A.; Finch, J.M.; Field, T.R.; Real, N.C.; Winter, A.; Walton, A.W.; Hodgkinson, S.M. Vaccination with the plasminogen activator from Streptococcus uberis induces an inhibitory response and protects against experimental infection in the dairy cow. Vaccine 1999, 17, 851–857. [Google Scholar] [CrossRef]
- Ward, P.N.; Field, T.R.; Rapier, C.D.; Leigh, J.A. The activation of bovine plasminogen by PauA is not required for virulence of Streptococcus uberis. Infect. Immun. 2003, 71, 7193–7196. [Google Scholar] [CrossRef]
- Almeida, R.A.; Luther, D.A.; Park, H.M.; Oliver, S.P. Identification, isolation, and partial characterization of a novel Streptococcus uberis adhesion molecule (SUAM). Vet. Microbiol. 2006, 115, 183–191. [Google Scholar] [CrossRef]
- Almeida, R.A.; Oliver, S.P. Role of collagen in adherence of Streptococcus uberis to bovine mammary epithelial cells. J. Vet. Med. B Infect. Dis. Vet. Public Health 2001, 48, 759–763. [Google Scholar] [CrossRef] [PubMed]
- Almeida, R.A.; Luther, D.A.; Kumar, S.J.; Calvinho, L.F.; Bronze, M.S.; Oliver, S.P. Adherence of Streptococcus uberis to bovine mammary epithelial cells and to extracellular matrix proteins. J. Vet. Med. Ser. B 1996, 43, 385–392. [Google Scholar] [CrossRef]
- Almeida, R.A.; Oliver, S.P. Trafficking of Streptococcus uberis in bovine mammary epithelial cells. Microb. Pathog. 2006, 41, 80–89. [Google Scholar] [CrossRef] [PubMed]
- Almeida, R.A.; Dego, O.K.; Headrick, S.I.; Lewis, M.J.; Oliver, S.P. Role of Streptococcus uberis adhesion molecule in the pathogenesis of Streptococcus uberis mastitis. Vet. Microbiol. 2015, 179, 332–335. [Google Scholar] [CrossRef] [PubMed]
- Almeida, R.A.; Dunlap, J.R.; Oliver, S.P. Binding of Host Factors Influences Internalization and Intracellular Trafficking of Streptococcus uberis in Bovine Mammary Epithelial Cells. Vet. Med. Int. 2010, 2010, 319192. [Google Scholar] [CrossRef]
- Almeida, R.A.; Fang, W.; Oliver, S.P. Adherence and internalization of Streptococcus uberis to bovine mammary epithelial cells are mediated by host cell proteoglycans. FEMS Microbiol. Lett. 1999, 177, 313–317. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Patel, D.; Almeida, R.A.; Dunlap, J.R.; Oliver, S.P. Bovine lactoferrin serves as a molecular bridge for internalization of Streptococcus uberis into bovine mammary epithelial cells. Vet. Microbiol. 2009, 137, 297–301. [Google Scholar] [CrossRef] [PubMed]
- Prado, M.E.; Almeida, R.A.; Ozen, C.; Luther, D.A.; Lewis, M.J.; Headrick, S.J.; Oliver, S.P. Vaccination of dairy cows with recombinant Streptococcus uberis adhesion molecule induces antibodies that reduce adherence to and internalization of S. uberis into bovine mammary epithelial cells. Vet. Immunol. Immunopathol. 2011, 141, 201–208. [Google Scholar] [CrossRef]
- Almeida, R.A.; Kerro-Dego, O.; Prado, M.E.; Headrick, S.I.; Lewis, M.J.; Siebert, L.J.; Pighetti, G.M.; Oliver, S.P. Protective effect of anti-SUAM antibodies on Streptococcus uberis mastitis. Vet. Res. 2015, 46, 133. [Google Scholar] [CrossRef]
- Chen, X.; Dego, O.K.; Almeida, R.A.; Fuller, T.E.; Luther, D.A.; Oliver, S.P. Deletion of sua gene reduces the ability of Streptococcus uberis to adhere to and internalize into bovine mammary epithelial cells. Vet. Microbiol. 2011, 147, 426–434. [Google Scholar] [CrossRef] [PubMed]
- Ward, P.N.; Field, T.R.; Ditcham, W.G.; Maguin, E.; Leigh, J.A. Identification and disruption of two discrete loci encoding hyaluronic acid capsule biosynthesis genes hasA, hasB, and hasC in Streptococcus uberis. Infect. Immun. 2001, 69, 392–399. [Google Scholar] [CrossRef]
- Varhimo, E.; Varmanen, P.; Fallarero, A.; Skogman, M.; Pyorala, S.; Iivanainen, A.; Sukura, A.; Vuorela, P.; Savijoki, K. Alpha- and beta-casein components of host milk induce biofilm formation in the mastitis bacterium Streptococcus uberis. Vet. Microbiol. 2011, 149, 381–389. [Google Scholar] [CrossRef]
- Kaczorek, E.; Malaczewska, J.; Wojcik, R.; Siwicki, A.K. Biofilm production and other virulence factors in Streptococcus spp. isolated from clinical cases of bovine mastitis in Poland. BMC Vet. Res. 2017, 13, 398. [Google Scholar] [CrossRef] [PubMed]
- Matthews, K.; Almeida, R.; Oliver, S. Bovine mammary epithelial cell invasion by Streptococcus uberis. Infect. Immun. 1994, 62, 5641–5646. [Google Scholar] [CrossRef] [PubMed]
- Matthews, K.R.; Oliver, S.P. Encapsulation of streptococci isolated from bovine milk. J. Vet. Med. Ser. B 1993, 40, 597–602. [Google Scholar] [CrossRef] [PubMed]
- Crowley, R.C.; Leigh, J.A.; Ward, P.N.; Lappin-Scott, H.M.; Bowler, L.D. Differential protein expression in Streptococcus uberis under planktonic and biofilm growth conditions. Appl. Environ. Microbiol. 2011, 77, 382–384. [Google Scholar] [CrossRef][Green Version]
- Kerro Dego, O.; Almeida, R.A.; Saxton, A.M.; Abdi, R.D.; Ensermu, D.B.; Oliver, S.P. Bovine intramammary infection associated immunogenic surface proteins of Streptococcus uberis. Microb. Pathog. 2018, 115, 304–311. [Google Scholar] [CrossRef] [PubMed]
- Gunther, J.; Czabanska, A.; Bauer, I.; Leigh, J.A.; Holst, O.; Seyfert, H.M. Streptococcus uberis strains isolated from the bovine mammary gland evade immune recognition by mammary epithelial cells, but not of macrophages. Vet. Res. 2016, 47, 13. [Google Scholar] [CrossRef]
- Egan, S.A.; Ward, P.N.; Watson, M.; Field, T.R.; Leigh, J.A. Vru (Sub0144) controls expression of proven and putative virulence determinants and alters the ability of Streptococcus uberis to cause disease in dairy cattle. Microbiology 2012, 158, 1581–1592. [Google Scholar] [CrossRef]
- Ward, P.N.; Holden, M.T.; Leigh, J.A.; Lennard, N.; Bignell, A.; Barron, A.; Clark, L.; Quail, M.A.; Woodward, J.; Barrell, B.G.; et al. Evidence for niche adaptation in the genome of the bovine pathogen Streptococcus uberis. BMC Genom. 2009, 10, 54. [Google Scholar] [CrossRef]
- Abdi, R.D.; Dunlap, J.R.; Gillespie, B.E.; Ensermu, D.B.; Almeida, R.A.; Kerro Dego, O. Comparison of Staphylococcus aureus surface protein extraction methods and immunogenicity. Heliyon 2019, 5, e02528. [Google Scholar] [CrossRef]
- Laemmli, U.K. Cleavage of structural proteins during the assembly of the head of bacteriophage T4. Nature 1970, 227, 680–685. [Google Scholar] [CrossRef]
- Schagger, H.; von Jagow, G. Tricine-sodium dodecyl sulfate-polyacrylamide gel electrophoresis for the separation of proteins in the range from 1 to 100 kDa. Anal. Biochem. 1987, 166, 368–379. [Google Scholar] [CrossRef]
- Merrill, C.; Ensermu, D.B.; Abdi, R.D.; Gillespie, B.E.; Vaughn, J.; Headrick, S.I.; Hash, K.; Walker, T.B.; Stone, E.; Kerro Dego, O. Immunological responses and evaluation of the protection in dairy cows vaccinated with staphylococcal surface proteins. Vet. Immunol. Immunopathol. 2019, 214, 109890. [Google Scholar] [CrossRef]
- Oliver, S.; Gonzalez, R.; Hogan, J.; Jayarao, B.; Owens, W. Microbiological Procedures for the Diagnosis of Bovine Udder Infection and Determination of Milk Quality; National Mastitis Council: Verona, WI, USA, 2004. [Google Scholar]
- Jayarao, B.M.; Gillespie, B.E.; Oliver, S.P. Application of Randomly Amplified Polymorphic DNA Fingerprinting for Species Identification of Bacteria Isolated from Bovine Milk. J. Food. Prot. 1996, 59, 615–620. [Google Scholar] [CrossRef]
- CLSI. Performance Standards for Antimicrobial Susceptibility Testing, 28th ed.; CLSI supplement M100; CLSI, Clinical Laboratory Standard Institute: Wayne, PA, USA, 2018; p. 296. [Google Scholar]
- Amblee, V.; Jeffery, C.J. Physical Features of Intracellular Proteins that Moonlight on the Cell Surface. PLoS ONE 2015, 10, e0130575. [Google Scholar] [CrossRef] [PubMed]
- Jin, H.; Song, Y.P.; Boel, G.; Kochar, J.; Pancholi, V. Group A Streptococcal Surface GAPDH, SDH, Recognizes uPAR/CD87 as its Receptor on the Human Pharyngeal Cell and Mediates Bacterial Adherence to Host Cells. J. Mol. Biol. 2005, 350, 27–41. [Google Scholar] [CrossRef] [PubMed]
- Boel, G.; Jin, H.; Pancholi, V. Inhibition of cell surface export of group A streptococcal anchorless surface dehydrogenase affects bacterial adherence and antiphagocytic properties. Infect. Immun. 2005, 73, 6237–6248. [Google Scholar] [CrossRef] [PubMed]
- Madureira, P.; Baptista, M.; Vieira, M.; Magalhaes, V.; Camelo, A.; Oliveira, L.; Ribeiro, A.; Tavares, D.; Trieu-Cuot, P.; Vilanova, M.; et al. Streptococcus agalactiae GAPDH is a virulence-associated immunomodulatory protein. J. Immunol. 2007, 178, 1379–1387. [Google Scholar] [CrossRef]
- Wang, K.; Lu, C. Adhesion activity of glyceraldehyde-3-phosphate dehydrogenase in a Chinese Streptococcus suis type 2 strain. Berl. Munch. Tierarztl. Wochenschr. 2007, 120, 207–209. [Google Scholar] [PubMed]
- Maeda, K.; Nagata, H.; Kuboniwa, M.; Kataoka, K.; Nishida, N.; Tanaka, M.; Shizukuishi, S. Characterization of binding of Streptococcus oralis glyceraldehyde-3-phosphate dehydrogenase to Porphyromonas gingivalis major fimbriae. Infect. Immun. 2004, 72, 5475–5477. [Google Scholar] [CrossRef] [PubMed]
- Kinoshita, H.; Uchida, H.; Kawai, Y.; Kawasaki, T.; Wakahara, N.; Matsuo, H.; Watanabe, M.; Kitazawa, H.; Ohnuma, S.; Miura, K.; et al. Cell surface Lactobacillus plantarum LA 318 glyceraldehyde-3-phosphate dehydrogenase (GAPDH) adheres to human colonic mucin. J. Appl. Microbiol. 2008, 104, 1667–1674. [Google Scholar] [CrossRef] [PubMed]
- Perez-Casal, J.; Potter, A.A. Glyceradehyde-3-phosphate dehydrogenase as a suitable vaccine candidate for protection against bacterial and parasitic diseases. Vaccine 2016, 34, 1012–1017. [Google Scholar] [CrossRef]
- Tallima, H.; Dvorak, J.; Kareem, S.; Abou El Dahab, M.; Abdel Aziz, N.; Dalton, J.P.; El Ridi, R. Protective immune responses against Schistosoma mansoni infection by immunization with functionally active gut-derived cysteine peptidases alone and in combination with glyceraldehyde 3-phosphate dehydrogenase. PLoS Negl. Trop. Dis. 2017, 11, e0005443. [Google Scholar] [CrossRef] [PubMed]
- El Ridi, R.; Shoemaker, C.B.; Farouk, F.; El Sherif, N.H.; Afifi, A. Human T- and B-cell responses to Schistosoma mansoni recombinant glyceraldehyde 3-phosphate dehydrogenase correlate with resistance to reinfection with S. mansoni or Schistosoma haematobium after chemotherapy. Infect. Immun. 2001, 69, 237–244. [Google Scholar] [CrossRef]
- El Ridi, R.; Ragab, S.; Lewis, S.; Afifi, A. Role of IgE in primary murine Schistosomiasis mansoni. Scand. J. Immunol. 2001, 53, 24–31. [Google Scholar] [CrossRef]
- El Ridi, R.; Mahrous, A.; Afifi, A.; Montash, M.; Velek, J.; Jezek, J. Human and murine humoral immune recognition of multiple peptides from Schistosoma mansoni glyceraldehyde 3-P dehydrogenase is associated with resistance to Schistosomiasis. Scand. J. Immunol. 2001, 54, 477–485. [Google Scholar] [CrossRef]
- Rosinha, G.M.S.; Myioshi, A.; Azevedo, V.; Splitter, G.A.; Oliveira, S.C. Molecular and immunological characterisation of recombinant Brucella abortus glyceraldehyde-3-phosphate-dehydrogenase, a T- and B-cell reactive protein that induces partial protection when co-administered with an interleukin-12-expressing plasmid in a DNA vaccine formulation. J. Med. Microbiol. 2002, 51, 661–671. [Google Scholar] [CrossRef]
- Gozalbo, D.; Gil-Navarro, I.; Azorin, I.; Renau-Piqueras, J.; Martinez, J.P.; Gil, M.L. The cell wall-associated glyceraldehyde-3-phosphate dehydrogenase of Candida albicans is also a fibronectin and laminin binding protein. Infect. Immun. 1998, 66, 2052–2059. [Google Scholar] [CrossRef] [PubMed]
- Gillespie, B.E.; Lewis, M.J.; Boonyayatra, S.; Maxwell, M.L.; Saxton, A.; Oliver, S.P.; Almeida, R.A. Short communication: Evaluation of bulk tank milk microbiological quality of nine dairy farms in Tennessee. J. Dairy Sci. 2012, 95, 4275–4279. [Google Scholar] [CrossRef]
- Barbano, D.M.; Lynch, J.M. Major advances in testing of dairy products: Milk component and dairy product attribute testing. J. Dairy Sci. 2006, 89, 1189–1194. [Google Scholar] [CrossRef]
- Barbano, D.M.; Ma, Y.; Santos, M.V. Influence of raw milk quality on fluid milk shelf life. J. Dairy Sci. 2006, 89 (Suppl. 1), E15–E19. [Google Scholar] [CrossRef]
- Parrodi, P.W. Milk fat in human nutrition. Aust. J. Dairy Technol. 2004, 59, 3–59. [Google Scholar]
- Jayarao, B.M.; Pillai, S.R.; Sawant, A.A.; Wolfgang, D.R.; Hegde, N.V. Guidelines for monitoring bulk tank milk somatic cell and bacterial counts. J. Dairy Sci. 2004, 87, 3561–3573. [Google Scholar] [CrossRef]

| Gr | # of Animals | Vaccine (SUSP) Dose | Dose/Volume | Route/Frequency |
|---|---|---|---|---|
| 1 | 6 | High: 4 mg in 2.5 mL of PBS | 4 mg/5 mL | SC/3 times at D0, D28, C7 for all groups |
| 2 | 6 | Mediu: 1 mg in 2.5 mL of PBS | 1 mg/5 mL | |
| 3 | 7 | Low: 100 μg in 2.5 mL | 0.1 mg/5 mL | |
| 4 | 7 | 2.5 mL PBS | 5 mL |
| Band # | Uniprot Protein ID | Mass | Log10E | Intensity | Peptide | Identification | Spectra | Coverage | Parsimony |
|---|---|---|---|---|---|---|---|---|---|
| 1: SUAM | Q2VEB5 | 97.79 | −32,153 | 2.23 | 195 | 2880 | 2880 | 90.3 | differentiable |
| 2: Lbp | Q6U7J0 | 62.864 | −22.6 | 0.48 | 3 | 4 | 4 | 12.3 | differentiable |
| 3: GlnA | B9DVR7 | 50.49 | −39.9 | 0.48 | 3 | 3 | 3 | 27.1 | equivalent |
| 4: EF-Tu | B9DRL9 | 43.91 | −353 | 1.49 | 23 | 53 | 53 | 87.7 | differentiable |
| 5: GapC | Q8kVU6 | 35.9 | −341.8 | 1.45 | 22 | 42 | 42 | 84.8 | differentiable |
| 6: PauA | Q7B2W7 | 33.42 | −1314 | 1.61 | 36 | 100 | 100 | 82.5 | set |
| 7: FbA | B9DTK0 | 31 | −296.8 | 1.41 | 22 | 41 | 41 | 76 | differentiable |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kerro Dego, O.; Almeida, R.; Ivey, S.; Agga, G.E. Evaluation of Streptococcus uberis Surface Proteins as Vaccine Antigens to Control S. uberis Mastitis in Dairy Cows. Vaccines 2021, 9, 868. https://doi.org/10.3390/vaccines9080868
Kerro Dego O, Almeida R, Ivey S, Agga GE. Evaluation of Streptococcus uberis Surface Proteins as Vaccine Antigens to Control S. uberis Mastitis in Dairy Cows. Vaccines. 2021; 9(8):868. https://doi.org/10.3390/vaccines9080868
Chicago/Turabian StyleKerro Dego, Oudessa, Raul Almeida, Susan Ivey, and Getahun E. Agga. 2021. "Evaluation of Streptococcus uberis Surface Proteins as Vaccine Antigens to Control S. uberis Mastitis in Dairy Cows" Vaccines 9, no. 8: 868. https://doi.org/10.3390/vaccines9080868
APA StyleKerro Dego, O., Almeida, R., Ivey, S., & Agga, G. E. (2021). Evaluation of Streptococcus uberis Surface Proteins as Vaccine Antigens to Control S. uberis Mastitis in Dairy Cows. Vaccines, 9(8), 868. https://doi.org/10.3390/vaccines9080868






