The Expression of Hemagglutinin by a Recombinant Newcastle Disease Virus Causes Structural Changes and Alters Innate Immune Sensing
Abstract
1. Introduction
2. Materials and Methods
2.1. Chickens
2.2. Vaccines and Viruses
2.3. Cells and Monoclonal Antibodies
2.4. Immunogold Electron Microscopy
2.5. Virus Neutralization
2.6. Evaluation of Hemagglutinating and Neuraminidase Activities
2.7. Immunofluorescence
2.8. Tracheal Organ Cultures (TOCs) Infection
2.9. CEFs Infection
2.10. RNA Extraction and Real-Time Reverse Transcription (RT)-PCR
2.11. Statistical Analyses
3. Results
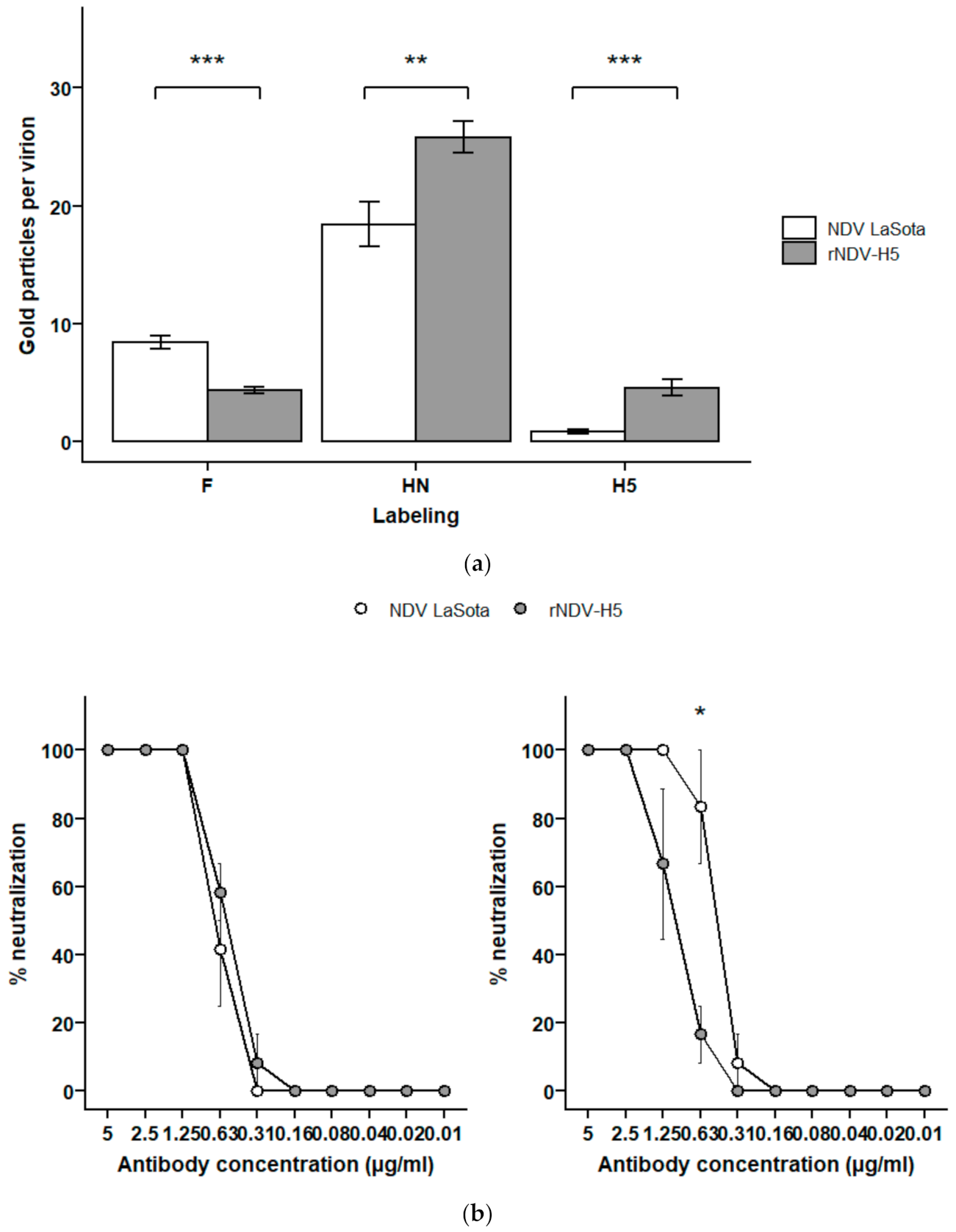
3.1. The Recombinant Virus Expresses Higher Levels of HN Glycoproteins and Lower Levels of F on Its Surface Than the Parental NDV
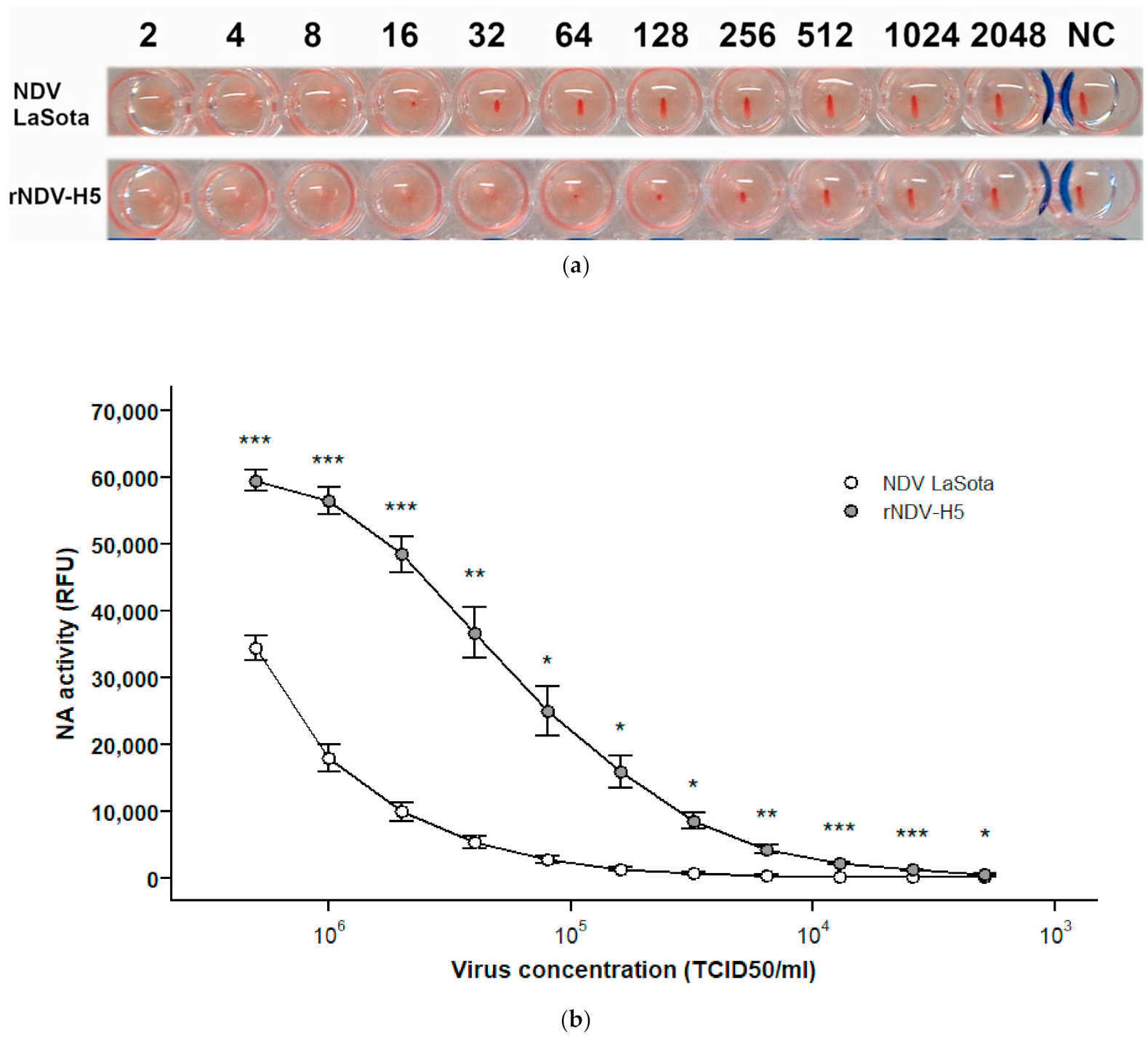
3.2. rNDV-H5 Has Higher Hemagglutinating and Neuraminidase Activities Than Parental NDV LaSota
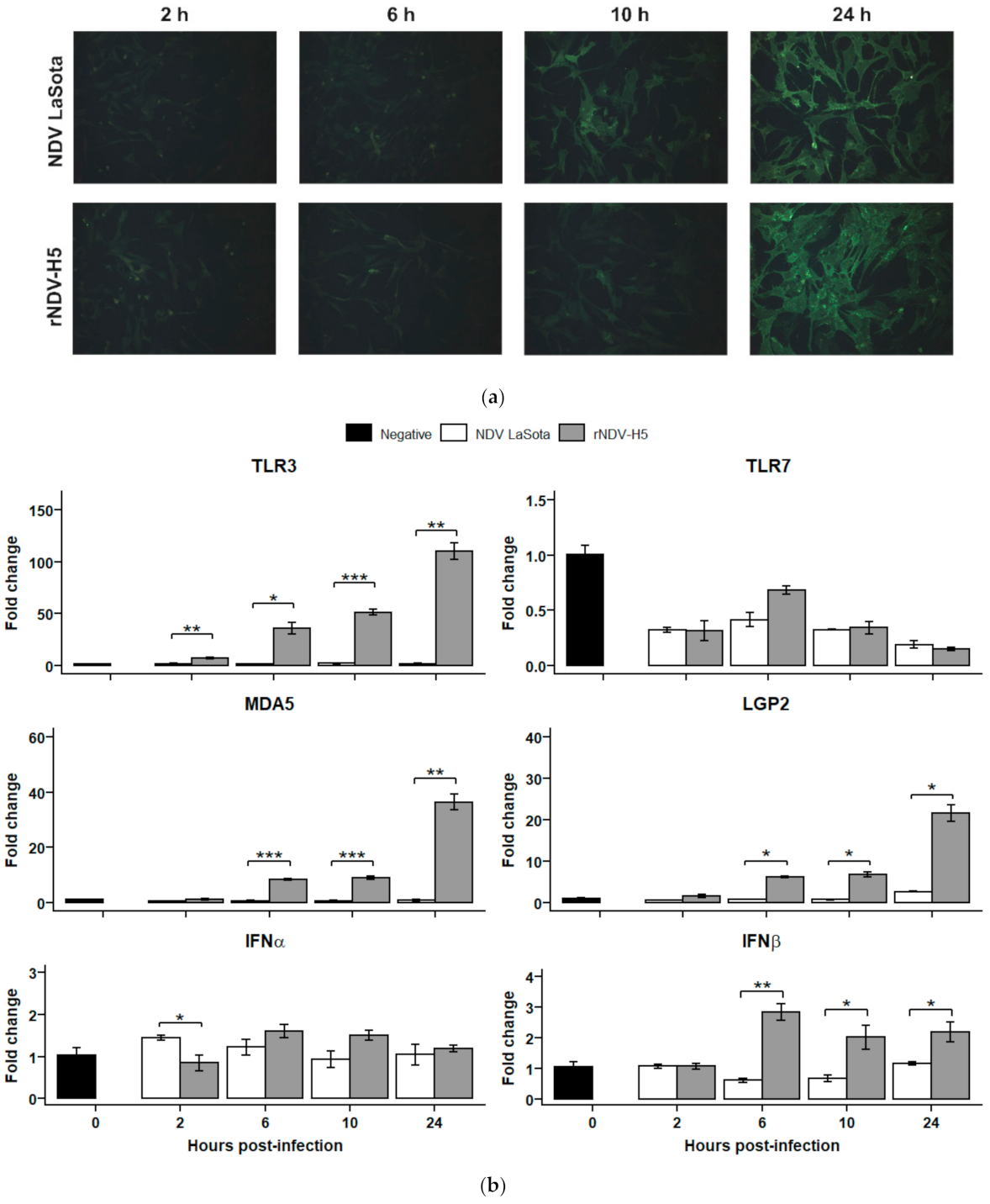
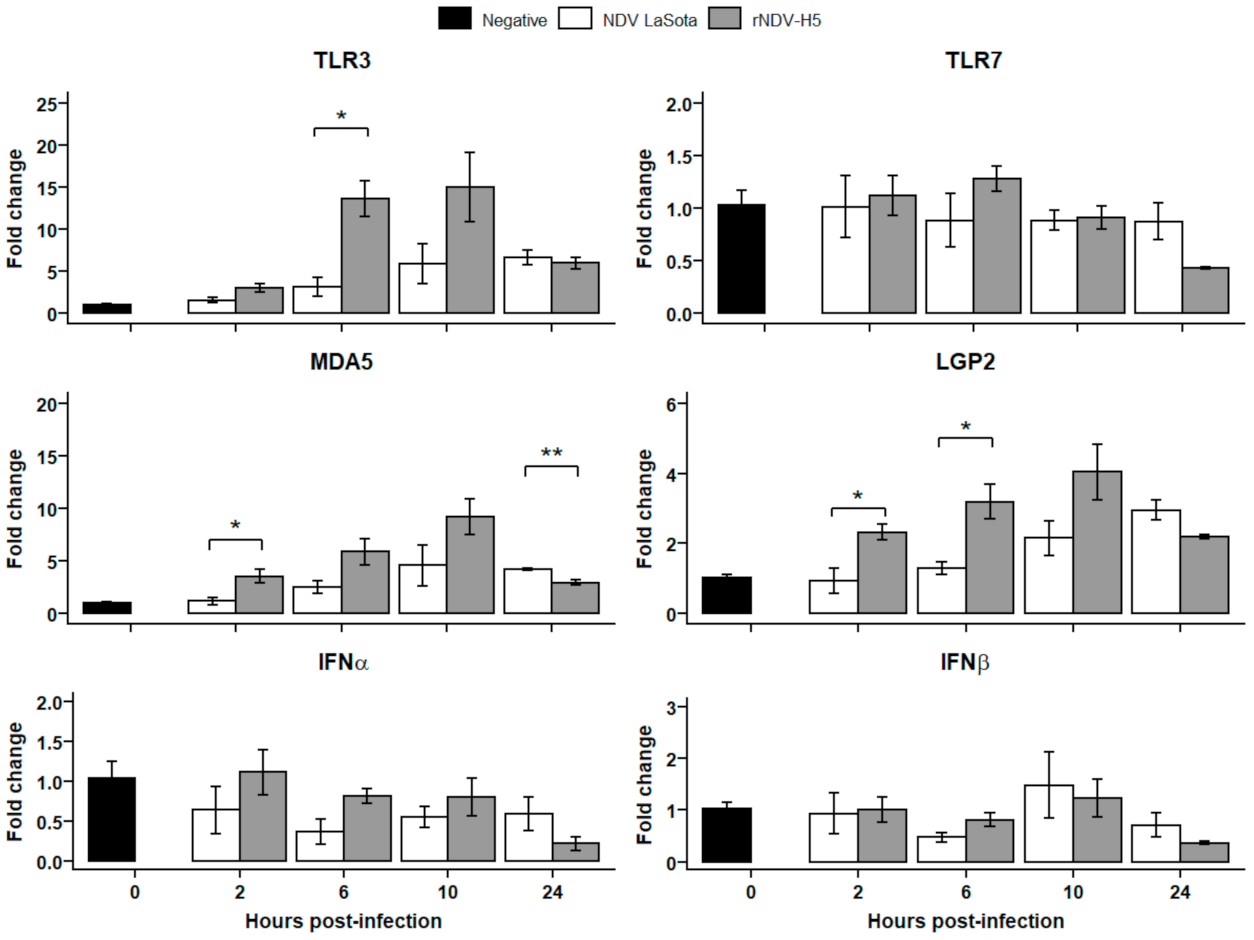
3.3. Innate Sensing of rNDV-H5 Is Mediated by TLR3, MDA5, and LGP2
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dhingra, M.S.; Artois, J.; Dellicour, S.; Lemey, P.; Dauphin, G.; Von Dobschuetz, S.; Van Boeckel, T.P.; Castellan, D.M.; Morzaria, S.; Gilbert, M. Geographical and Historical Patterns in the Emergences of Novel Highly Pathogenic Avian Influenza (HPAI) H5 and H7 Viruses in Poultry. Front. Vet. Sci. 2018, 5, 84. [Google Scholar] [CrossRef]
- Dimitrov, K.M.; Lee, D.-H.; Williams-Coplin, D.; Olivier, T.L.; Miller, P.J.; Afonso, C.L. Newcastle Disease Viruses Causing Recent Outbreaks Worldwide Show Unexpectedly High Genetic Similarity to Historical Virulent Isolates from the 1940’s. J. Clin. Microbiol. 2016, 54, 1228–1235. [Google Scholar] [CrossRef] [PubMed]
- Astill, J.; Dara, R.A.; Fraser, E.D.G.; Sharif, S. Detecting and Predicting Emerging Disease in Poultry With the Implementation of New Technologies and Big Data: A Focus on Avian Influenza Virus. Front. Vet. Sci. 2018, 5. [Google Scholar] [CrossRef]
- Bello, M.B.; Yusoff, K.; Ideris, A.; Hair-Bejo, M.; Peeters, B.P.H.; Omar, A.R. Diagnostic and Vaccination Approaches for Newcastle Disease Virus in Poultry: The Current and Emerging Perspectives. Biomed. Res. Int. 2018, 2018, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Suarez, D.L.; Pantin-Jackwood, M.J. Recombinant Viral-Vectored Vaccines for the Control of Avian Influenza in Poultry. Vet. Microbiol. 2017, 206, 144–151. [Google Scholar] [CrossRef] [PubMed]
- Dimitrov, K.M.; Afonso, C.L.; Yu, Q.; Miller, P.J. Newcastle Disease Vaccines—A Solved Problem or a Continuous Challenge? Vet. Microbiol. 2017, 206, 126–136. [Google Scholar] [CrossRef] [PubMed]
- Spackman, E.; Pantin-Jackwood, M.J. Practical Aspects of Vaccination of Poultry against Avian Influenza Virus. Vet. J. 2014, 202, 408–415. [Google Scholar] [CrossRef] [PubMed]
- Romanutti, C.; Keller, L.; Zanetti, F.A. Current Status of Virus-Vectored Vaccines against Pathogens That Affect Poultry. Vaccine 2020, 38, 6990–7001. [Google Scholar] [CrossRef]
- Kim, S.-H.; Samal, S.K. Newcastle Disease Virus as a Vaccine Vector for Development of Human and Veterinary Vaccines. Viruses 2016, 8, 183. [Google Scholar] [CrossRef]
- Ge, J.; Deng, G.; Wen, Z.; Tian, G.; Wang, Y.; Shi, J.; Wang, X.; Li, Y.; Hu, S.; Jiang, Y.; et al. Newcastle Disease Virus-Based Live Attenuated Vaccine Completely Protects Chickens and Mice from Lethal Challenge of Homologous and Heterologous H5N1 Avian Influenza Viruses. J. Virol. 2007, 81, 150–158. [Google Scholar] [CrossRef]
- Kim, S.-H.; Samal, S.K. Innovation in Newcastle Disease Virus Vectored Avian Influenza Vaccines. Viruses 2019, 11, 300. [Google Scholar] [CrossRef]
- Lardinois, A.; Steensels, M.; Lambrecht, B.; Desloges, N.; Rahaus, M.; Rebeski, D.; van den Berg, T. Potency of a Recombinant NDV-H5 Vaccine Against Various HPAI H5N1 Virus Challenges in SPF Chickens. Avian Dis. 2012, 56, 928–936. [Google Scholar] [CrossRef]
- Nayak, B.; Rout, S.N.; Kumar, S.; Khalil, M.S.; Fouda, M.M.; Ahmed, L.E.; Earhart, K.C.; Perez, D.R.; Collins, P.L.; Samal, S.K. Immunization of Chickens with Newcastle Disease Virus Expressing H5 Hemagglutinin Protects against Highly Pathogenic H5N1 Avian Influenza Viruses. PLoS ONE 2009, 4, e6509. [Google Scholar] [CrossRef]
- Veits, J.; Wiesner, D.; Fuchs, W.; Hoffmann, B.; Granzow, H.; Starick, E.; Mundt, E.; Schirrmeier, H.; Mebatsion, T.; Mettenleiter, T.C.; et al. Newcastle Disease Virus Expressing H5 Hemagglutinin Gene Protects Chickens against Newcastle Disease and Avian Influenza. Proc. Natl. Acad. Sci. USA 2006, 103, 8197–8202. [Google Scholar] [CrossRef]
- Connaris, H.; Takimoto, T.; Russell, R.; Crennell, S.; Moustafa, I.; Portner, A.; Taylor, G. Probing the Sialic Acid Binding Site of the Hemagglutinin-Neuraminidase of Newcastle Disease Virus: Identification of Key Amino Acids Involved in Cell Binding, Catalysis, and Fusion. J. Virol. 2002, 76, 1816–1824. [Google Scholar] [CrossRef]
- Aguilar, H.C.; Henderson, B.A.; Zamora, J.L.; Johnston, G.P. Paramyxovirus Glycoproteins and the Membrane Fusion Process. Curr. Clin. Microbiol. Rep. 2016, 3, 142–154. [Google Scholar] [CrossRef] [PubMed]
- Cantin, C.; Holguera, J.; Ferreira, L.; Villar, E.; Munoz-Barroso, I. Newcastle Disease Virus May Enter Cells by Caveolae-Mediated Endocytosis. J. Gen. Virol. 2007, 88, 559–569. [Google Scholar] [CrossRef] [PubMed]
- Wen, Z.; Zhao, B.; Song, K.; Hu, X.; Chen, W.; Kong, D.; Ge, J.; Bu, Z. Recombinant Lentogenic Newcastle Disease Virus Expressing Ebola Virus GP Infects Cells Independently of Exogenous Trypsin and Uses Macropinocytosis as the Major Pathway for Cell Entry. Virol. J. 2013, 10, 331. [Google Scholar] [CrossRef] [PubMed]
- Edinger, T.O.; Pohl, M.O.; Stertz, S. Entry of Influenza A Virus: Host Factors and Antiviral Targets. J. Gen. Virol. 2014, 95, 263–277. [Google Scholar] [CrossRef] [PubMed]
- Lardinois, A.; Vandersleyen, O.; Steensels, M.; Desloges, N.; Mast, J.; van den Berg, T.; Lambrecht, B. Stronger Interference of Avian Influenza Virus–Specific Than Newcastle Disease Virus–Specific Maternally Derived Antibodies with a Recombinant NDV-H5 Vaccine. Avian Dis. 2016, 60, 191–201. [Google Scholar] [CrossRef]
- Locati, M.; Mantovani, A.; Sica, A. Macrophage Activation and Polarization as an Adaptive Component of Innate Immunity. Adv. Immunol. 2013, 120, 163–184. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, L.A.J.; Bowie, A.G. Sensing and Signaling in Antiviral Innate Immunity. Curr. Biol. 2010, 20, R328–R333. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Cheng, A.; Wang, M. Innate Sensing of Viruses by Pattern Recognition Receptors in Birds. Vet. Res. 2013, 44, 82. [Google Scholar] [CrossRef] [PubMed]
- Denney, L.; Ho, L.-P. The Role of Respiratory Epithelium in Host Defence against Influenza Virus Infection. Biomed. J. 2018, 41, 218–233. [Google Scholar] [CrossRef]
- Santhakumar, D.; Rubbenstroth, D.; Martinez-Sobrido, L.; Munir, M. Avian Interferons and Their Antiviral Effectors. Front. Immunol. 2017, 8. [Google Scholar] [CrossRef] [PubMed]
- Guo, P.; Thomas, J.D.; Bruce, M.P.; Hinton, T.M.; Bean, A.G.D.; Lowenthal, J.W. The Chicken TH1 Response: Potential Therapeutic Applications of ChIFN-γ. Dev. Comp. Immunol. 2013, 41, 389–396. [Google Scholar] [CrossRef] [PubMed]
- St.Paul, M.; Brisbin, J.T.; Abdul-Careem, M.F.; Sharif, S. Immunostimulatory Properties of Toll-like Receptor Ligands in Chickens. Vet. Immunol. Immunopathol. 2013, 152, 191–199. [Google Scholar] [CrossRef]
- Park, M.-S.; Steel, J.; García-Sastre, A.; Swayne, D.; Palese, P. Engineered Viral Vaccine Constructs with Dual Specificity: Avian Influenza and Newcastle Disease. Proc. Natl. Acad. Sci. USA 2006, 103, 8203–8208. [Google Scholar] [CrossRef]
- Zhao, W.; Zhang, Z.; Zsak, L.; Yu, Q. P and M Gene Junction Is the Optimal Insertion Site in Newcastle Disease Virus Vaccine Vector for Foreign Gene Expression. J. Gen. Virol. 2015, 96, 40–45. [Google Scholar] [CrossRef]
- Nagy, A.; Lee, J.; Mena, I.; Henningson, J.; Li, Y.; Ma, J.; Duff, M.; Li, Y.; Lang, Y.; Yang, J.; et al. Recombinant Newcastle Disease Virus Expressing H9 HA Protects Chickens against Heterologous Avian Influenza H9N2 Virus Challenge. Vaccine 2016, 34, 2537–2545. [Google Scholar] [CrossRef]
- Shahsavandi, S.; Ebrahimi, M.M.; Mohammadi, A.; Zarrin Lebas, N. Impact of Chicken-Origin Cells on Adaptation of a Low Pathogenic Influenza Virus. Cytotechnology 2013, 65, 419–424. [Google Scholar] [CrossRef]
- Ren, X.; Xue, C.; Kong, Q.; Zhang, C.; Bi, Y.; Cao, Y. Proteomic Analysis of Purified Newcastle Disease Virus Particles. Proteome Sci. 2012, 10, 32. [Google Scholar] [CrossRef]
- Ferreira, H.L.; Lambrecht, B.; van Borm, S.; Torrieri-Dramard, L.; Klatzmann, D.; Bellier, B.; van den Berg, T. Identification of a Dominant Epitope in the Hemagglutinin of an Asian Highly Pathogenic Avian Influenza H5N1 Clade 1 Virus by Selection of Escape Mutants. Avian Dis. 2010, 54, 565–571. [Google Scholar] [CrossRef]
- Meulemans, G.; Gonze, M.; Carlier, M.C.; Petit, P.; Burny, A.; Long, L. Evaluation of the Use of Monoclonal Antibodies to Hemagglutinin and Fusion Glycoproteins of Newcastle Disease Virus for Virus Identification and Strain Differentiation Purposes. Arch. Virol. 1987, 92, 55–62. [Google Scholar] [CrossRef]
- Kortekaas, J.; Dekker, A.; de Boer, S.M.; Weerdmeester, K.; Vloet, R.P.M.; de Wit, A.A.C.; Peeters, B.P.H.; Moormann, R.J.M. Intramuscular Inoculation of Calves with an Experimental Newcastle Disease Virus-Based Vector Vaccine Elicits Neutralizing Antibodies against Rift Valley Fever Virus. Vaccine 2010, 28, 2271–2276. [Google Scholar] [CrossRef]
- Spackman, E. Animal Influenza Virus, 2nd ed.; Humana Press: New York, NY, USA, 2014; ISBN 978-1-4939-0757-1. [Google Scholar]
- Ingrao, F.; Rauw, F.; van den Berg, T.; Lambrecht, B. Characterization of Two Recombinant HVT-IBD Vaccines by VP2 Insert Detection and Cell-Mediated Immunity after Vaccination of Specific Pathogen-Free Chickens. Avian Pathol. 2017, 46, 289–299. [Google Scholar] [CrossRef]
- Wang, J.; Tang, C.; Wang, Q.; Li, R.; Chen, Z.; Han, X.; Wang, J.; Xu, X. Apoptosis Induction and Release of Inflammatory Cytokines in the Oviduct of Egg-Laying Hens Experimentally Infected with H9N2 Avian Influenza Virus. Vet. Microbiol. 2015, 177, 302–314. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Xie, Z.; Dai, J.; Cao, Y.; Hou, J.; Zheng, Y.; Wei, T.; Mo, M.; Wei, P. Responses of the Toll-like Receptor and Melanoma Differentiation-Associated Protein 5 Signaling Pathways to Avian Infectious Bronchitis Virus Infection in Chicks. Virol. Sin. 2016, 31, 57–68. [Google Scholar] [CrossRef] [PubMed]
- Peters, M.A.; Browning, G.F.; Washington, E.A.; Crabb, B.S.; Kaiser, P. Embryonic Age Influences the Capacity for Cytokine Induction in Chicken Thymocytes. Immunology 2003, 110, 358–367. [Google Scholar] [CrossRef] [PubMed]
- Nang, N.T.; Lee, J.S.; Song, B.M.; Kang, Y.M.; Kim, H.S.; Seo, S.H. Induction of Inflammatory Cytokines and Toll-like Receptors in Chickens Infected with Avian H9N2 Influenza Virus. Vet. Res. 2011, 42, 64. [Google Scholar] [CrossRef] [PubMed]
- Ingrao, F.; Rauw, F.; Steensels, M.; van den Berg, T.; Lambrecht, B. Early Immune Responses and Profiling of Cell-Mediated Immunity-Associated Gene Expression in Response to RHVT-IBD Vaccination. Vaccine 2018, 36, 615–623. [Google Scholar] [CrossRef] [PubMed]
- Staines, K.; Batra, A.; Mwangi, W.; Maier, H.J.; Van Borm, S.; Young, J.R.; Fife, M.; Butter, C. A Versatile Panel of Reference Gene Assays for the Measurement of Chicken MRNA by Quantitative PCR. PLoS ONE 2016, 11, e0160173. [Google Scholar] [CrossRef]
- Livak, K.J.; Schmittgen, T.D. Analysis of Relative Gene Expression Data Using Real-Time Quantitative PCR and the 2−ΔΔCT Method. Methods 2001, 25, 402–408. [Google Scholar] [CrossRef]
- Wickham, H. Ggplot2: Elegant Graphics for Data Analysis, 2nd ed.; Springer International Publishing: Cham, Switzerland, 2016; ISBN 978-3-319-24275-0. [Google Scholar]
- Skiadopoulos, M.H.; Surman, S.R.; Riggs, J.M.; Örvell, C.; Collins, P.L.; Murphy, B.R. Evaluation of the Replication and Immunogenicity of Recombinant Human Parainfluenza Virus Type 3 Vectors Expressing up to Three Foreign Glycoproteins. Virology 2002, 297, 136–152. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Willemsen, A.; Zwart, M.P. On the Stability of Sequences Inserted into Viral Genomes. Virus Evol 2019, 5. [Google Scholar] [CrossRef] [PubMed]
- Jin, J.; Zhao, J.; Ren, Y.; Zhong, Q.; Zhang, G. Contribution of HN Protein Length Diversity to Newcastle Disease Virus Virulence, Replication and Biological Activities. Sci. Rep. 2016, 6, 36890. [Google Scholar] [CrossRef] [PubMed]
- Melanson, V.R.; Iorio, R.M. Amino Acid Substitutions in the F-Specific Domain in the Stalk of the Newcastle Disease Virus HN Protein Modulate Fusion and Interfere with Its Interaction with the F Protein. J. Virol. 2004, 78, 13053–13061. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.C.; Grusovin, J.; Adams, T.E. Electrostatic Interactions between Hendra Virus Matrix Proteins Are Required for Efficient Virus-Like-Particle Assembly. J. Virol. 2018, 92. [Google Scholar] [CrossRef] [PubMed]
- Tappert, M.M.; Porterfield, J.Z.; Mehta-D’Souza, P.; Gulati, S.; Air, G.M. Quantitative Comparison of Human Parainfluenza Virus Hemagglutinin-Neuraminidase Receptor Binding and Receptor Cleavage. J. Virol. 2013, 87, 8962–8970. [Google Scholar] [CrossRef]
- Liu, T.; Song, Y.; Yang, Y.; Bu, Y.; Cheng, J.; Zhang, G.; Xue, J. Hemagglutinin–Neuraminidase and Fusion Genes Are Determinants of NDV Thermostability. Vet. Microbiol. 2019, 228, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Bouvier, N.M.; Palese, P. The Biology of Influenza Viruses. Vaccine 2008, 26, D49–D53. [Google Scholar] [CrossRef] [PubMed]
- Richard, M.; Ferraris, O.; Erny, A.; Barthélémy, M.; Traversier, A.; Sabatier, M.; Hay, A.; Lin, Y.P.; Russell, R.J.; Lina, B. Combinatorial Effect of Two Framework Mutations (E119V and I222L) in the Neuraminidase Active Site of H3N2 Influenza Virus on Resistance to Oseltamivir. Antimicrob. Agents Chemother. 2011, 55, 2942–2952. [Google Scholar] [CrossRef] [PubMed]
- Xu, R.; Zhu, X.; McBride, R.; Nycholat, C.M.; Yu, W.; Paulson, J.C.; Wilson, I.A. Functional Balance of the Hemagglutinin and Neuraminidase Activities Accompanies the Emergence of the 2009 H1N1 Influenza Pandemic. J. Virol. 2012, 86, 9221–9232. [Google Scholar] [CrossRef]
- Du, W.; Wolfert, M.A.; Peeters, B.; van Kuppeveld, F.J.M.; Boons, G.-J.; de Vries, E.; de Haan, C.A.M. Mutation of the Second Sialic Acid-Binding Site of Influenza A Virus Neuraminidase Drives Compensatory Mutations in Hemagglutinin. PLoS Pathog. 2020, 16, e1008816. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.; Sun, Y.; Zhang, X.; Zhang, F.; Zhang, S.; Yu, S.; Qiu, X.; Tan, L.; Song, C.; Gao, S.; et al. Toll-like Receptor 3 Inhibits Newcastle Disease Virus Replication through Activation of pro-Inflammatory Cytokines and the Type-1 Interferon Pathway. Arch. Virol. 2014, 159, 2937–2948. [Google Scholar] [CrossRef] [PubMed]
- Philbin, V.J.; Iqbal, M.; Boyd, Y.; Goodchild, M.J.; Beal, R.K.; Bumstead, N.; Young, J.; Smith, A.L. Identification and Characterization of a Functional, Alternatively Spliced Toll-like Receptor 7 (TLR7) and Genomic Disruption of TLR8 in Chickens. Immunology 2005, 114, 507–521. [Google Scholar] [CrossRef]
- Zhang, P.; Ding, Z.; Liu, X.; Chen, Y.; Li, J.; Tao, Z.; Fei, Y.; Xue, C.; Qian, J.; Wang, X.; et al. Enhanced Replication of Virulent Newcastle Disease Virus in Chicken Macrophages Is Due to Polarized Activation of Cells by Inhibition of TLR7. Front. Immunol. 2018, 9. [Google Scholar] [CrossRef] [PubMed]
- Roman, J.M.; Simon, E.H. Defective Interfering Particles in Monolayer-Propagated Newcastle Disease Virus. Virology 1976, 69, 298–303. [Google Scholar] [CrossRef]
- Vasou, A.; Sultanoglu, N.; Goodbourn, S.; Randall, R.E.; Kostrikis, L.G. Targeting Pattern Recognition Receptors (PRR) for Vaccine Adjuvantation: From Synthetic PRR Agonists to the Potential of Defective Interfering Particles of Viruses. Viruses 2017, 9, 186. [Google Scholar] [CrossRef]
- Vignuzzi, M.; López, C.B. Defective Viral Genomes Are Key Drivers of the Virus–Host Interaction. Nat. Microbiol. 2019, 4, 1075–1087. [Google Scholar] [CrossRef]
- Steward, M.; Vipond, I.B.; Millar, N.S.; Emmerson, P.T. RNA Editing in Newcastle Disease Virus. J. Gen. Virol. 1993, 74, 2539–2547. [Google Scholar] [CrossRef] [PubMed]
- Childs, K.; Stock, N.; Ross, C.; Andrejeva, J.; Hilton, L.; Skinner, M.; Randall, R.; Goodbourn, S. Mda-5, but Not RIG-I, Is a Common Target for Paramyxovirus V Proteins. Virology 2007, 359, 190–200. [Google Scholar] [CrossRef]
- Childs, K.; Randall, R.; Goodbourn, S. Paramyxovirus V Proteins Interact with the RNA Helicase LGP2 To Inhibit RIG-I-Dependent Interferon Induction. J. Virol. 2012, 86, 3411–3421. [Google Scholar] [CrossRef] [PubMed]
- Childs, K.S.; Randall, R.E.; Goodbourn, S. LGP2 Plays a Critical Role in Sensitizing Mda-5 to Activation by Double-Stranded RNA. PLoS ONE 2013, 8. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Dang, R.; Yang, Z. The Interferon Antagonistic Activities of the V Proteins of NDV Correlated with Their Virulence. Virus Genes 2019, 55, 233–237. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ingrao, F.; Duchatel, V.; Rodil, I.F.; Steensels, M.; Verleysen, E.; Mast, J.; Lambrecht, B. The Expression of Hemagglutinin by a Recombinant Newcastle Disease Virus Causes Structural Changes and Alters Innate Immune Sensing. Vaccines 2021, 9, 758. https://doi.org/10.3390/vaccines9070758
Ingrao F, Duchatel V, Rodil IF, Steensels M, Verleysen E, Mast J, Lambrecht B. The Expression of Hemagglutinin by a Recombinant Newcastle Disease Virus Causes Structural Changes and Alters Innate Immune Sensing. Vaccines. 2021; 9(7):758. https://doi.org/10.3390/vaccines9070758
Chicago/Turabian StyleIngrao, Fiona, Victoria Duchatel, Isabel Fernandez Rodil, Mieke Steensels, Eveline Verleysen, Jan Mast, and Bénédicte Lambrecht. 2021. "The Expression of Hemagglutinin by a Recombinant Newcastle Disease Virus Causes Structural Changes and Alters Innate Immune Sensing" Vaccines 9, no. 7: 758. https://doi.org/10.3390/vaccines9070758
APA StyleIngrao, F., Duchatel, V., Rodil, I. F., Steensels, M., Verleysen, E., Mast, J., & Lambrecht, B. (2021). The Expression of Hemagglutinin by a Recombinant Newcastle Disease Virus Causes Structural Changes and Alters Innate Immune Sensing. Vaccines, 9(7), 758. https://doi.org/10.3390/vaccines9070758





