Differential Demographic and Clinical Characteristics between MMR Vaccinated and Unvaccinated Children in South Korea: A Nationwide Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
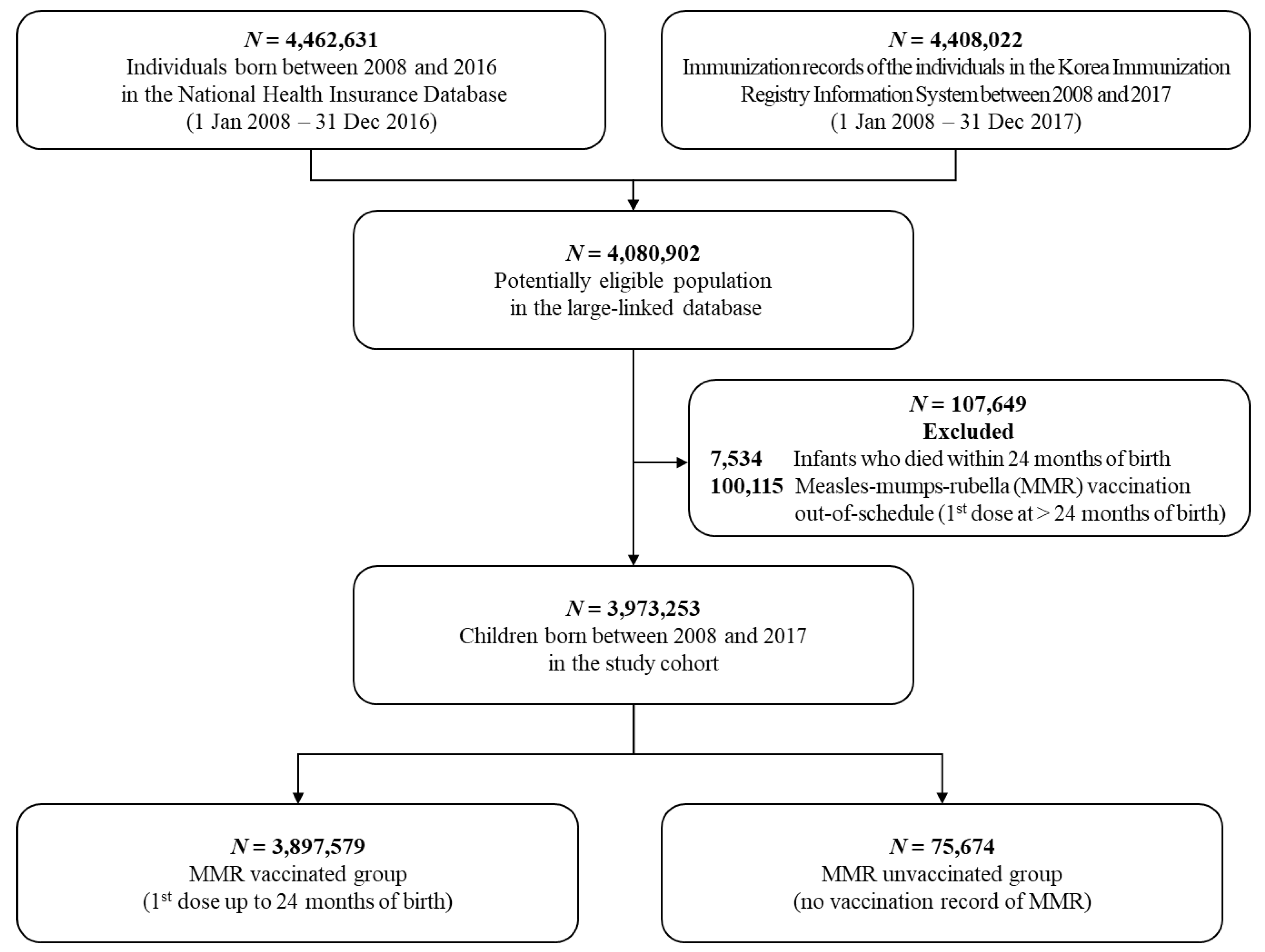
2.2. Study Population
2.3. Ascertainment of MMR Vaccination Status
2.4. Factors Associated with MMR Unvaccination
2.5. Statistical Analyses
2.6. Ethical Approval and Patient Involvement
3. Results
3.1. Population in Study Cohort
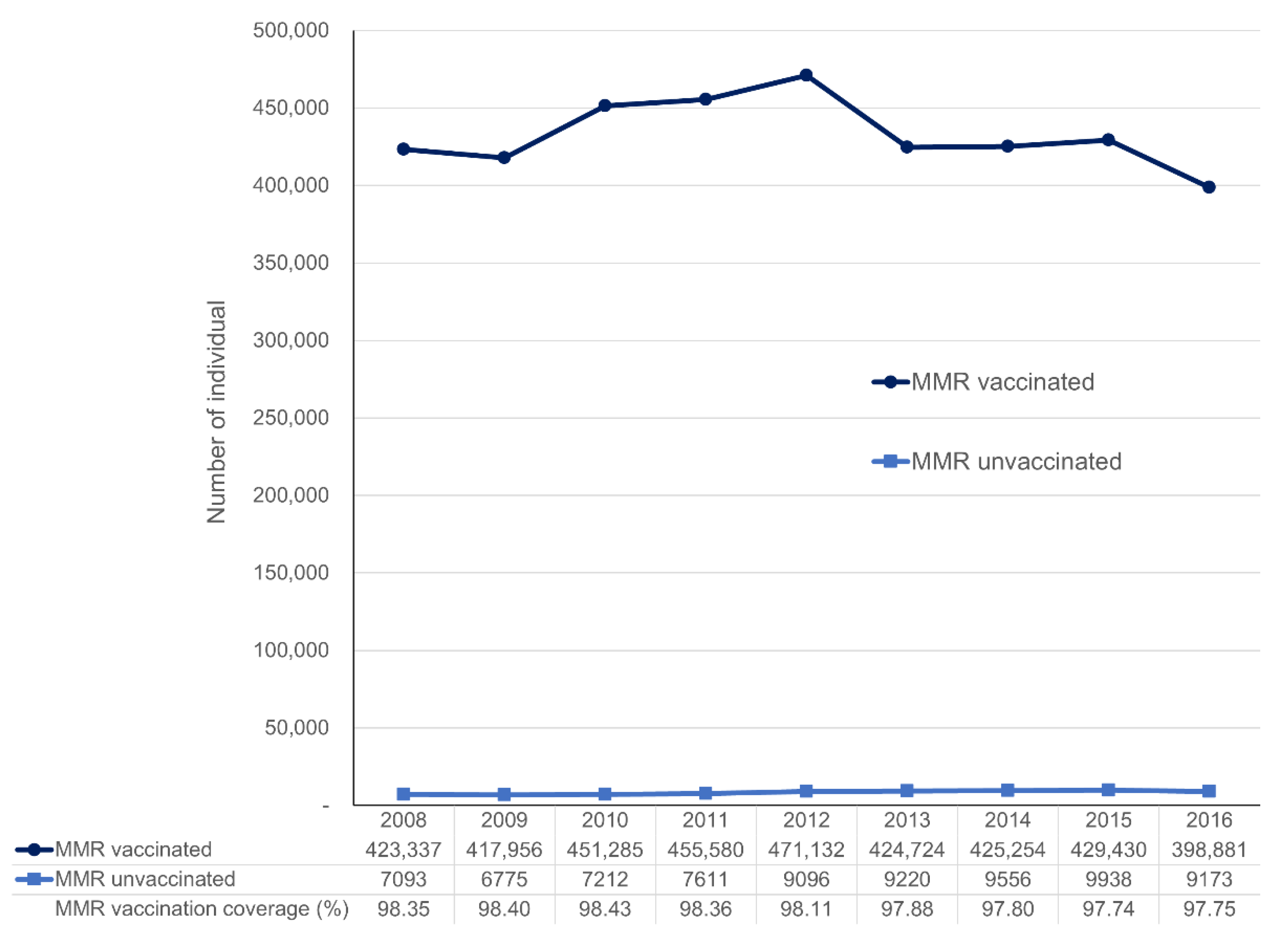
3.2. Annual Trends of Vaccine Coverage
3.3. Factors Associated with MMR Unvaccination
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Measles. Available online: https://www.who.int/news-room/fact-sheets/detail/measles (accessed on 17 March 2021).
- Global Measles Outbreaks. Available online: https://www.cdc.gov/globalhealth/measles/data/global-measles-outbreaks.html (accessed on 17 March 2021).
- Siwon Choi, E.H.C.; Na-Ri, S. Analysis of the occurrence of measles in Korea, 2019. Public Health Wkly. Rep. 2019, 13, 2445–2458. [Google Scholar]
- Lee, J.; Jeong, H.; Kim, S.; Yu, J.; Kim, G. National childhood vaccination coverage among children aged 1–3 and 6 years in Korea, 2018. Public Health Wkly. Rep. 2019, 12, 1548–1558. [Google Scholar]
- Choe, Y.J.; Park, Y.J.; Kim, J.W.; Eom, H.E.; Park, O.; Oh, M.D.; Lee, J.K. An Outbreak of Measles in a University in Korea, 2014. J. Korean Med. Sci. 2017, 32, 1876–1878. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.H.; Ki, H.; Choi, B.Y.; Kim, C.H.; Lee, D.H.; Ko, U.Y.; Ki, M. Evaluation of Mumps Vaccine Effectiveness by outbreak investigation in one kindergarten in Ulsan city, 2006. Epidemiol. Health 2008, 30, 110–118. [Google Scholar] [CrossRef]
- Pearce, A.; Law, C.; Elliman, D.; Cole, T.J.; Bedford, H. Factors associated with uptake of measles, mumps, and rubella vaccine (MMR) and use of single antigen vaccines in a contemporary UK cohort: Prospective cohort study. BMJ 2008, 336, 754–757. [Google Scholar] [CrossRef]
- Restivo, V.; Napoli, G.; Marsala, M.G.; Bonanno, V.; Sciuto, V.; Amodio, E.; Calamusa, G.; Vitale, F.; Firenze, A. Factors associated with poor adherence to MMR vaccination in parents who follow vaccination schedule. Hum. Vaccin. Immunother. 2015, 11, 140–145. [Google Scholar] [CrossRef]
- Park, B.; Choi, E.J.; Park, B.; Han, H.; Cho, S.J.; Choi, H.J.; Lee, S.; Park, H. Factors influencing vaccination in Korea: Findings from focus group interviews. J. Prev. Med. Public Health 2018, 51, 173–180. [Google Scholar] [CrossRef]
- Ntenda, P.A.M. Factors associated with non- and under-vaccination among children aged 12-23 months in Malawi. A multinomial analysis of the population-based sample. Pediatr. Neonatol. 2019, 60, 623–633. [Google Scholar] [CrossRef]
- Ashkenazi, S.; Livni, G.; Klein, A.; Kremer, N.; Havlin, A.; Berkowitz, O. The relationship between parental source of information and knowledge about measles/measles vaccine and vaccine hesitancy. Vaccine 2020, 38, 7292–7298. [Google Scholar] [CrossRef] [PubMed]
- Cheol Seong, S.; Kim, Y.Y.; Khang, Y.H.; Heon Park, J.; Kang, H.J.; Lee, H.; Do, C.H.; Song, J.S.; Hyon Bang, J.; Ha, S.; et al. Data Resource Profile: The national health information database of the national health insurance service in South Korea. Int. J. Epidemiol. 2017, 46, 799–800. [Google Scholar] [CrossRef] [PubMed]
- Park, E.; Jang, S.; Jeon, S.; Lee, S.; Lee, J.; Choi, D. Report of the Evaluation for Validity of Discharged Diagnoses in Korean Health Insurance Database; Health Insurance Review and Assessment Service: Wonju, Korea, 2017.
- Salmon, D.A.; Dudley, M.Z.; Glanz, J.M.; Omer, S.B. Vaccine hesitancy: Causes, consequences, and a call to action. Vaccine 2015, 33, D66–D71. [Google Scholar] [CrossRef] [PubMed]
- Taylor, J.A.; Darden, P.M.; Brooks, D.A.; Hendricks, J.W.; Wasserman, R.C.; Bocian, A.B. Association between parents’ preferences and perceptions of barriers to vaccination and the immunization status of their children: A study from Pediatric Research in office settings and the National Medical Association. Pediatrics 2002, 110, 1110–1116. [Google Scholar] [CrossRef]
- Gust, D.A.; Darling, N.; Kennedy, A.; Schwartz, B. Parents with doubts about vaccines: Which vaccines and reasons why. Pediatrics 2008, 122, 718–725. [Google Scholar] [CrossRef]
- Lam, C.G.; Howard, S.C.; Bouffet, E.; Pritchard-Jones, K. Science and health for all children with cancer. Science 2019, 363, 1182–1186. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.R.; Ortín, M.; Cohen, B.J.; Borrow, R.; Irving, D.; Sheldon, J.; Heath, P.T. Revaccination of children after completion of standard chemotherapy for acute leukemia. Clin. Infect. Dis. 2007, 44, 635–642. [Google Scholar] [CrossRef] [PubMed]
- Saari, T.N. Immunization of preterm and low birth weight infants. American Academy of Pediatrics Committee on Infectious Diseases. Pediatrics 2003, 112, 193–198. [Google Scholar] [CrossRef]
- Siddiqui, M.; Salmon, D.A.; Omer, S.B. Epidemiology of vaccine hesitancy in the United States. Hum. Vaccin. Immunother. 2013, 9, 2643–2648. [Google Scholar] [CrossRef]
- Bugvi, A.S.; Rahat, R.; Zakar, R.; Zakar, M.Z.; Fischer, F.; Nasrullah, M.; Manawar, R. Factors associated with non-utilization of child immunization in Pakistan: Evidence from the Demographic and Health Survey 2006-07. BMC Public Health 2014, 14, 232. [Google Scholar] [CrossRef]
- Dummer, T.J.B.; Cui, Y.; Strang, R.; Parker, L. Immunization completeness of children under two years of age in Nova Scotia, Canada. Can. J. Public Health 2012, 103, e363–e367. [Google Scholar] [CrossRef]
- Barata, R.B.; Sampaio de Almeida Ribeiro, M.C.; de Moraes, J.C.; Flannery, B. Socioeconomic inequalities and vaccination coverage: Results of an immunisation coverage survey in 27 Brazilian capitals, 2007–2008. J. Epidemiol. Community Health 2012, 66, 934–941. [Google Scholar] [CrossRef]
- Cui, F.-Q.; Gofin, R. Immunization coverage and its determinants in children aged 12–23 months in Gansu, China. Vaccine 2007, 25, 664–671. [Google Scholar] [CrossRef] [PubMed]
- Wei, F.; Mullooly, J.P.; Goodman, M.; McCarty, M.C.; Hanson, A.M.; Crane, B.; Nordin, J.D. Identification and characteristics of vaccine refusers. BMC Pediatr. 2009, 9, 18. [Google Scholar] [CrossRef] [PubMed]
- Chang, K.; Lee, S.Y. Why do some Korean parents hesitate to vaccinate their children? Epidemiol. Health 2019, 41, e2019031. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | MMR Vaccinated (n = 3,897,579) | MMR Unvaccinated (n = 75,674) | ||
|---|---|---|---|---|
| N | (%) | N | (%) | |
| Sex | ||||
| Boys | 2,001,404 | (51.3) | 37,633 | (49.7) |
| Girls | 1,896,175 | (48.7) | 38,041 | (50.3) |
| Parental socioeconomic status | ||||
| Residence type † | ||||
| Metropolitan | 1,738,321 | (44.6) | 37,923 | (50.1) |
| Provincial | 2,159,258 | (55.4) | 37,751 | (49.9) |
| Type of health insurance | ||||
| Employer-sponsored | 2,652,840 | (68.1) | 21,097 | (27.9) |
| Self-employed | 783,171 | (20.1) | 43,728 | (57.8) |
| Medical aid beneficiary | 32,872 | (0.8) | 377 | (0.5) |
| Unknown | 428,696 | (11.0) | 10,472 | (13.8) |
| Household income level | ||||
| Low | 286,376 | (7.3) | 15,979 | (21.1) |
| Lower-Middle | 561,145 | (14.4) | 11,903 | (15.7) |
| Upper-Middle | 1,249,361 | (32.1) | 14,145 | (18.7) |
| High | 1,295,646 | (33.2) | 22,474 | (29.7) |
| Unknown | 505,051 | (13.0) | 11,173 | (14.8) |
| Comorbidity | ||||
| Birth injury | 45,031 | (1.16) | 292 | (0.39) |
| Congenital anomaly | 14,395 | (0.37) | 370 | (0.49) |
| Infections in perinatal period | 535,422 | (13.7) | 3311 | (4.38) |
| Low birth weight | 161,489 | (4.14) | 1139 | (1.51) |
| Small for gestational age | 13,111 | (0.34) | 104 | (0.14) |
| Asplenia | 1903 | (0.05) | 26 | (0.03) |
| History of anaphylaxis | 1317 | (0.03) | 16 | (0.02) |
| Prior MMR infection | 6927 | (0.18) | 94 | (0.12) |
| Cancer | 1863 | (0.05) | 107 | (0.14) |
| Healthcare utilization | ||||
| Outpatient visit (mean ± SD) | 25.8 ± 17.06 | 5.73 ± 12.1 | ||
| Hospitalization days (mean ± SD) | 2.32 ± 6.90 | 1.69 ± 14.5 | ||
| ICU visit (mean ± SD) | 0.06 ± 0.33 | 0.04 ± 0.42 | ||
| Yes | 177,865 | (4.56) | 1468 | (1.94) |
| No | 3,719,714 | (95.4) | 74,206 | (98.06) |
| ER visit (mean ± SD) | 0.46 ± 0.90 | 0.15 ± 0.71 | ||
| Yes | 1,049,688 | (26.9) | 6532 | (8.63) |
| No | 2,847,891 | (73.1) | 69,142 | (91.4) |
| Korean traditional medicine clinic visit (mean ± SD) | 0.33 ± 2.37 | 0.34 ± 3.88 | ||
| Yes | 298,356 | (7.6) | 5028 | (6.6) |
| No | 3,599,223 | (92.4) | 70,646 | (93.4) |
| Characteristic | aOR * | 95% CI |
|---|---|---|
| Sex | ||
| Boys | Ref | |
| Girls * | 1.02 | (1.00 to 1.03) |
| Parental socioeconomic status | ||
| Residence type † | ||
| Metropolitan * | 1.44 | (1.41 to 1.46) |
| Provincial | Ref | |
| Type of health insurance | ||
| Employer-sponsored | Ref | |
| Self-employed * | 7.34 | (7.21 to 7.46) |
| Medical aid beneficiary * | 0.43 | (0.39 to 0.48) |
| Household income level | ||
| Low * | 3.66 | (3.58 to 3.74) |
| Lower-Middle | 0.98 | (0.96 to 1.01) |
| Upper-Middle * | 0.62 | (0.61 to 0.64) |
| High | Ref | |
| Comorbidity | ||
| Birth injury * | 0.38 | (0.34 to 0.43) |
| Congenital anomaly * | 2.12 | (1.90 to 2.36) |
| Infections in perinatal period * | 0.32 | (0.31 to 0.33) |
| Low birth weight * | 0.42 | (0.39 to 0.44) |
| Small for gestational age * | 0.63 | (0.51 to 0.76) |
| Asplenia | 0.88 | (0.59 to 1.30) |
| History of anaphylaxis | 1.43 | (0.87 to 2.36) |
| Prior MMR infection | 1.07 | (0.87 to 1.32) |
| Cancer * | 4.89 | (3.97 to 6.01) |
| Healthcare utilization | ||
| ICU visit | ||
| Yes | Ref | |
| No * | 1.88 | (1.78 to 1.98) |
| ER visit | ||
| Yes | Ref | |
| No * | 3.57 | (3.53 to 3.72) |
| Korean traditional medicine clinic visit | ||
| Yes | Ref | |
| No | 0.99 | (0.96 to 1.02) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yoon, D.; Kim, J.; Shin, J. Differential Demographic and Clinical Characteristics between MMR Vaccinated and Unvaccinated Children in South Korea: A Nationwide Study. Vaccines 2021, 9, 653. https://doi.org/10.3390/vaccines9060653
Yoon D, Kim J, Shin J. Differential Demographic and Clinical Characteristics between MMR Vaccinated and Unvaccinated Children in South Korea: A Nationwide Study. Vaccines. 2021; 9(6):653. https://doi.org/10.3390/vaccines9060653
Chicago/Turabian StyleYoon, Dongwon, Juhwan Kim, and Juyoung Shin. 2021. "Differential Demographic and Clinical Characteristics between MMR Vaccinated and Unvaccinated Children in South Korea: A Nationwide Study" Vaccines 9, no. 6: 653. https://doi.org/10.3390/vaccines9060653
APA StyleYoon, D., Kim, J., & Shin, J. (2021). Differential Demographic and Clinical Characteristics between MMR Vaccinated and Unvaccinated Children in South Korea: A Nationwide Study. Vaccines, 9(6), 653. https://doi.org/10.3390/vaccines9060653






