Global Vaccine Hesitancy Segmentation: A Cross-European Approach
Abstract
1. Introduction
2. Materials and Methods
3. Results
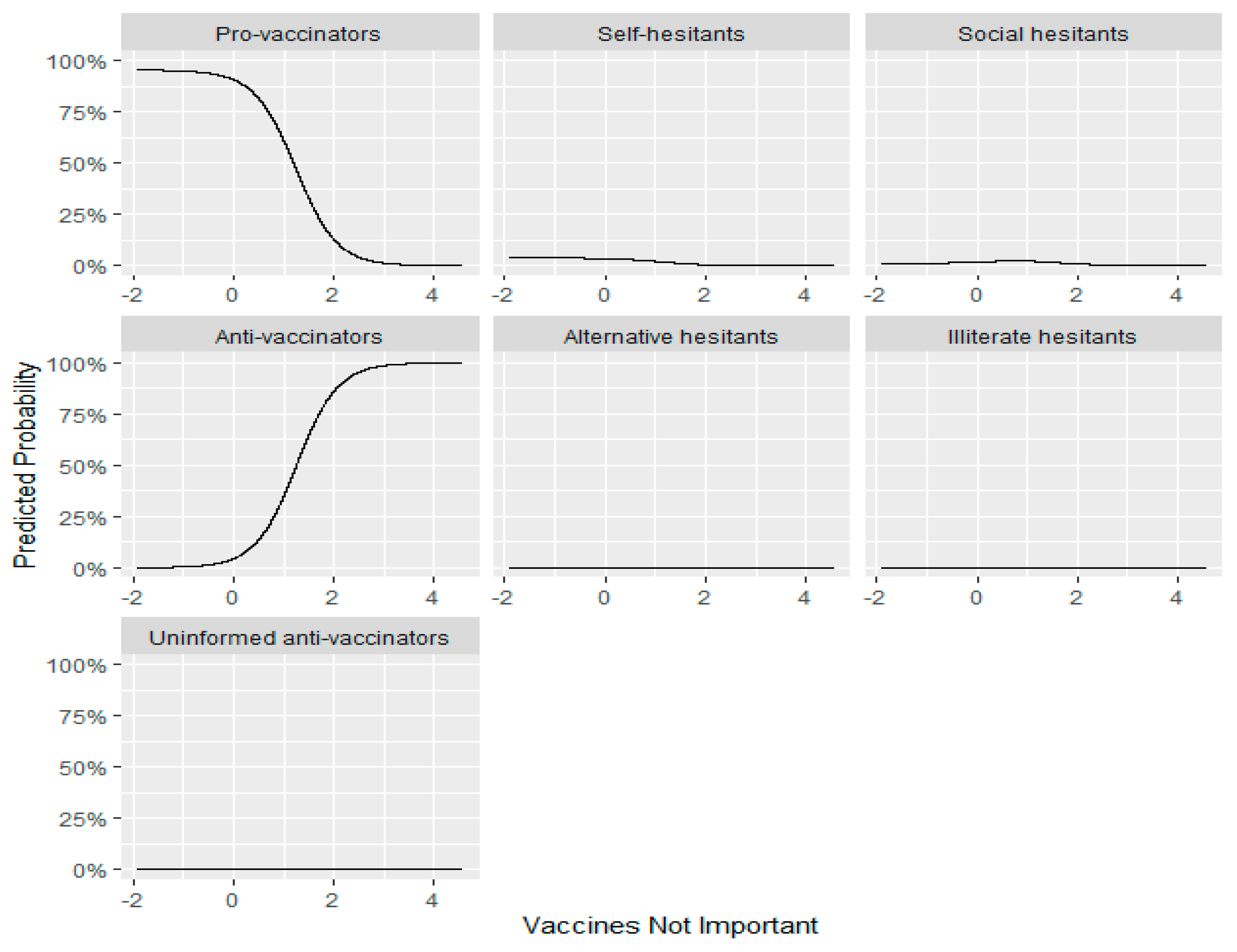
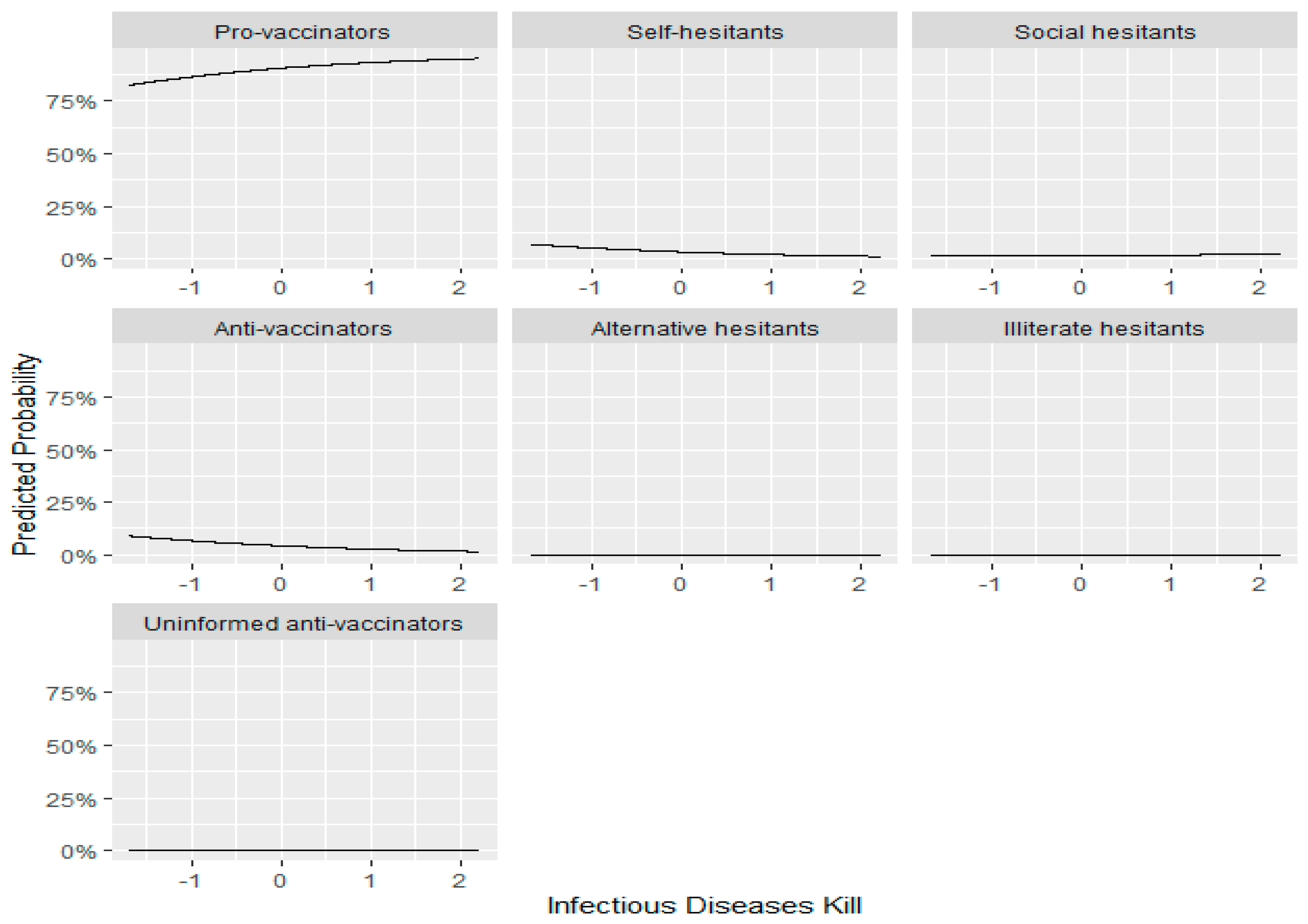
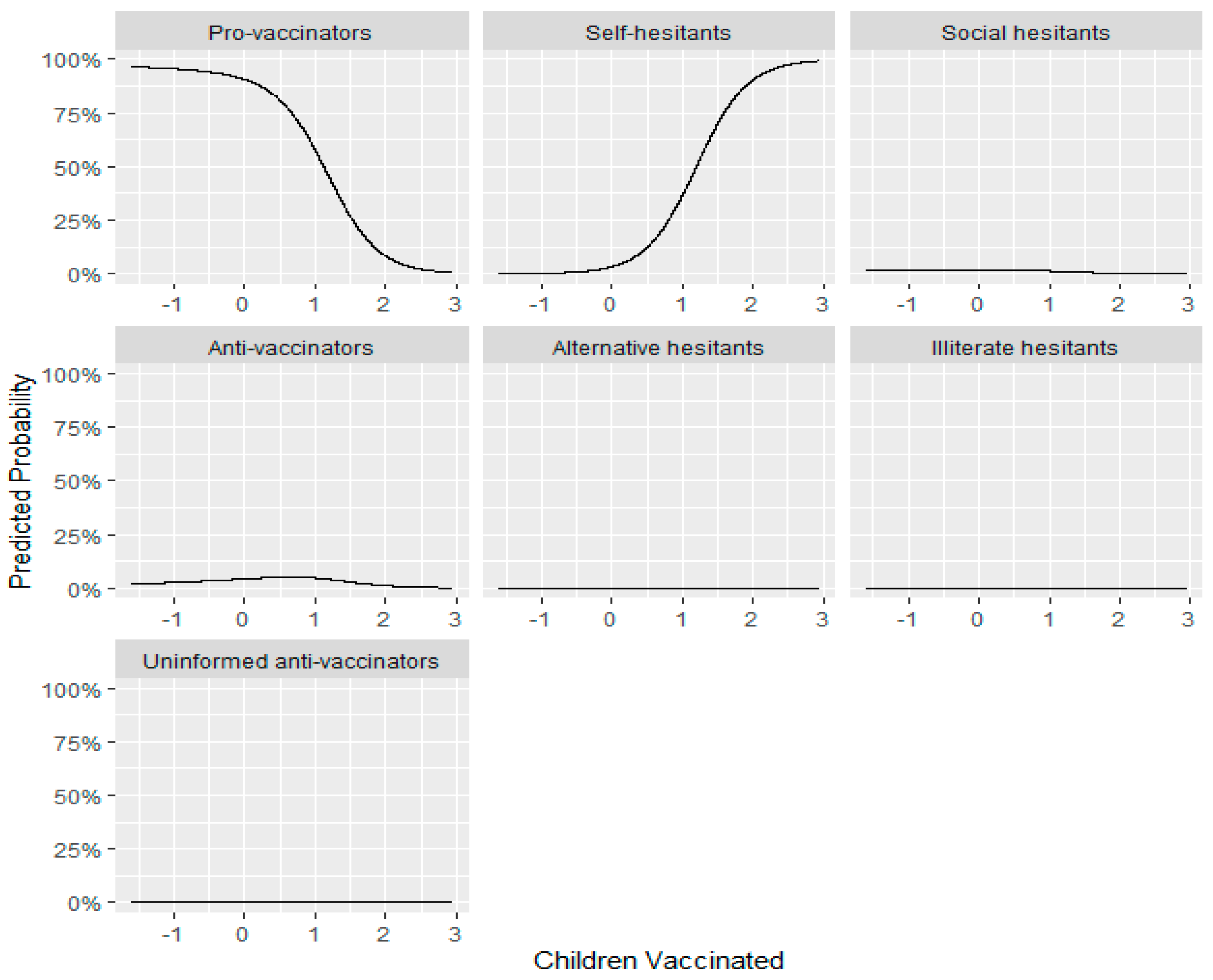
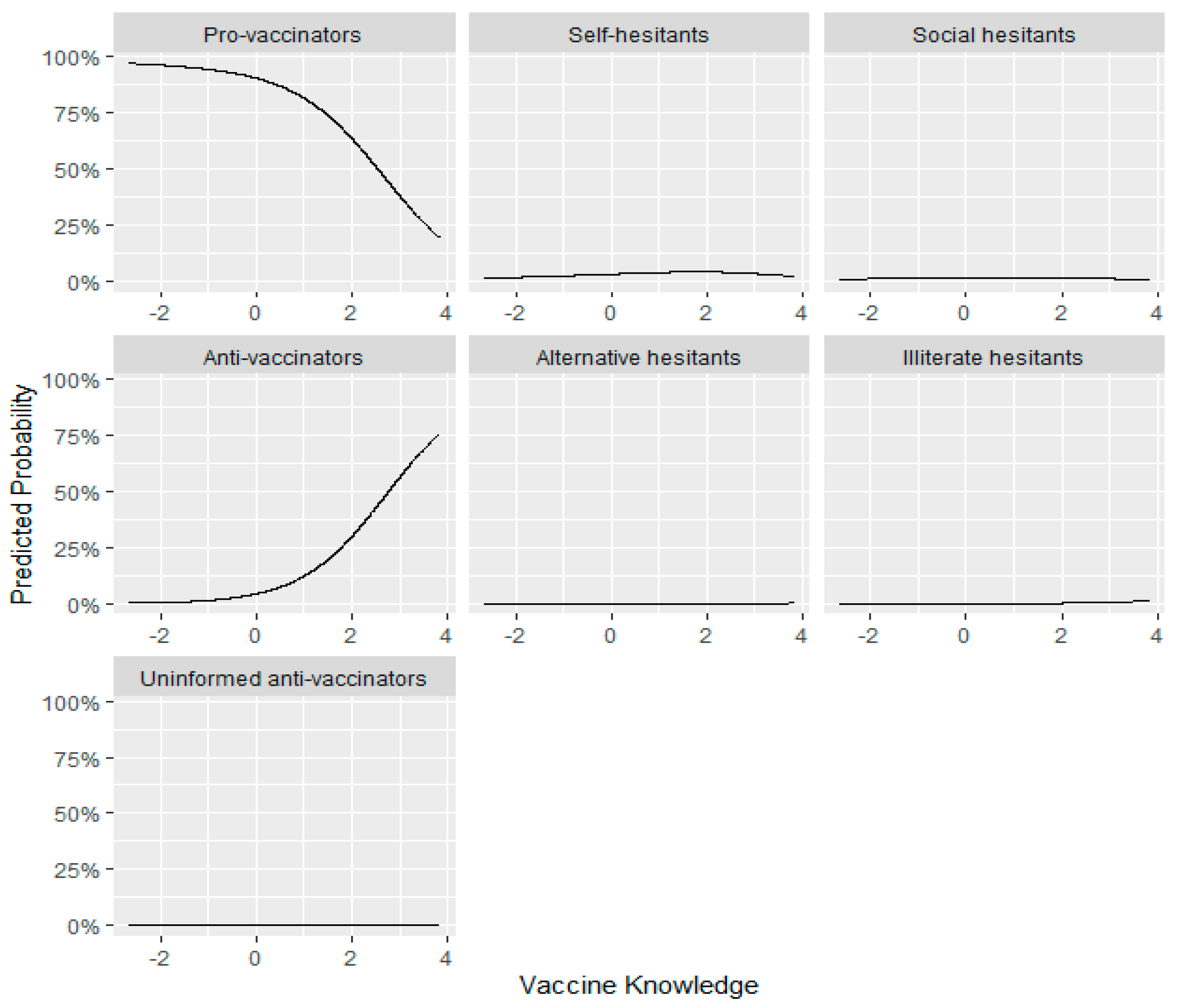
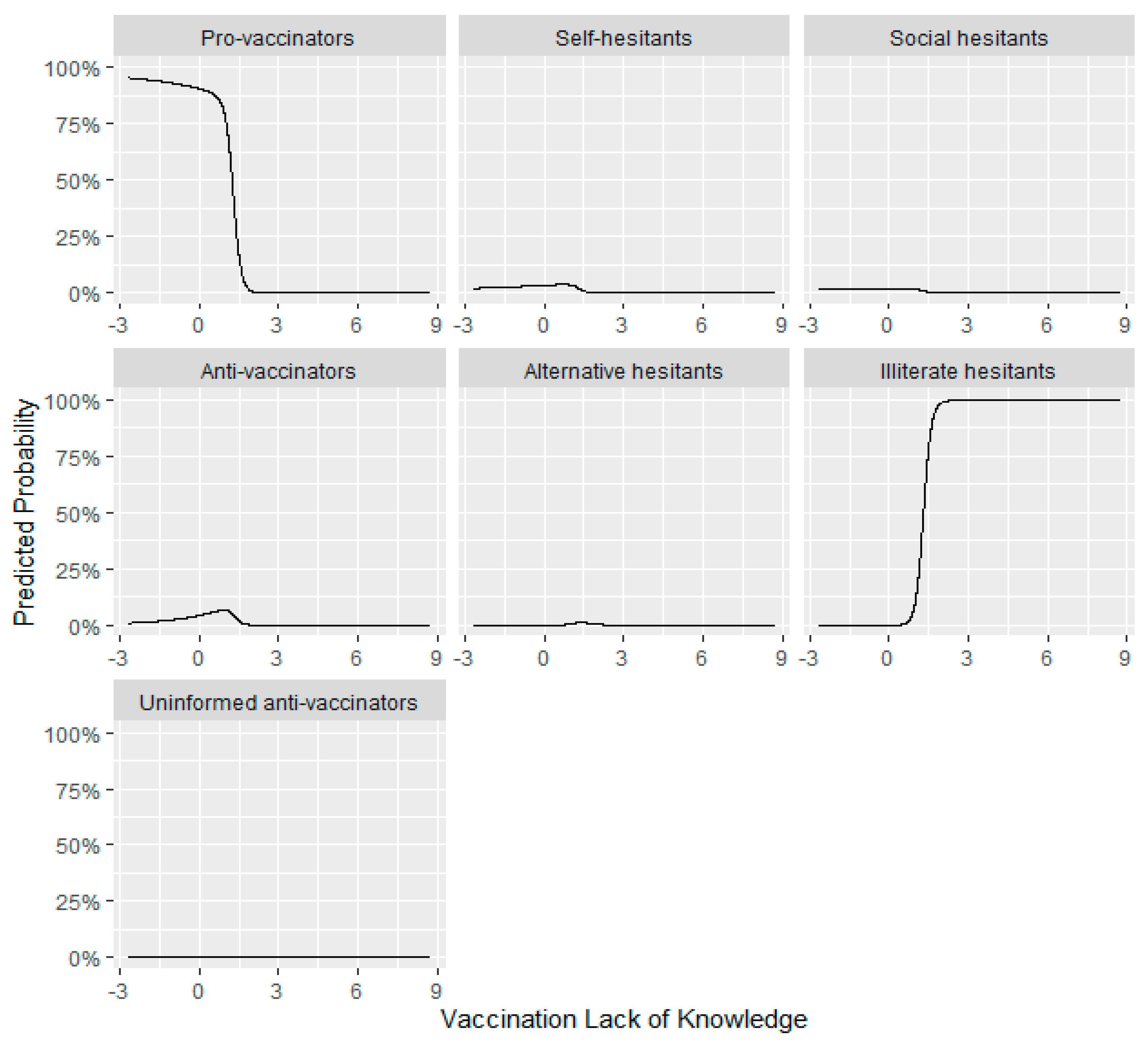
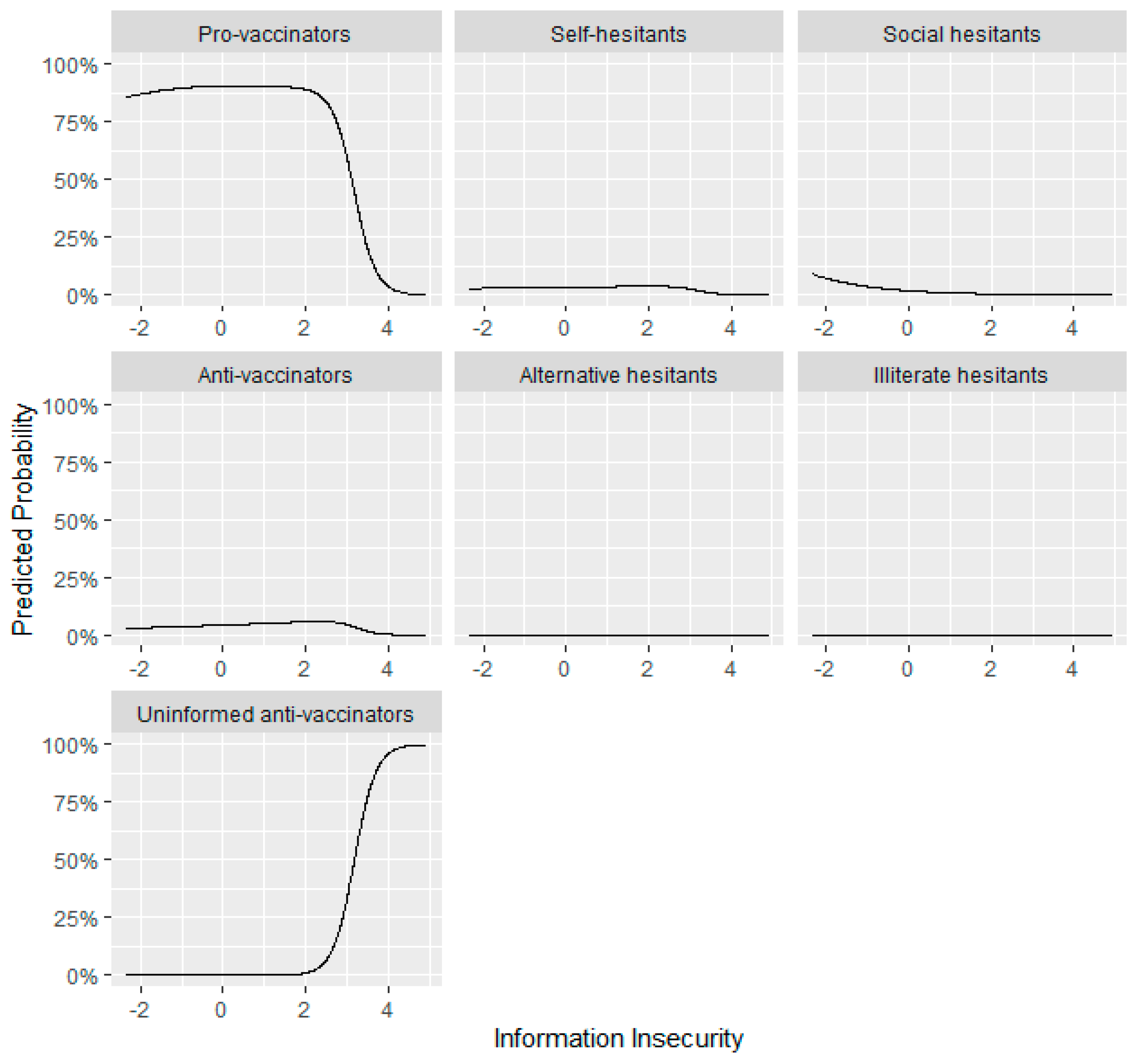
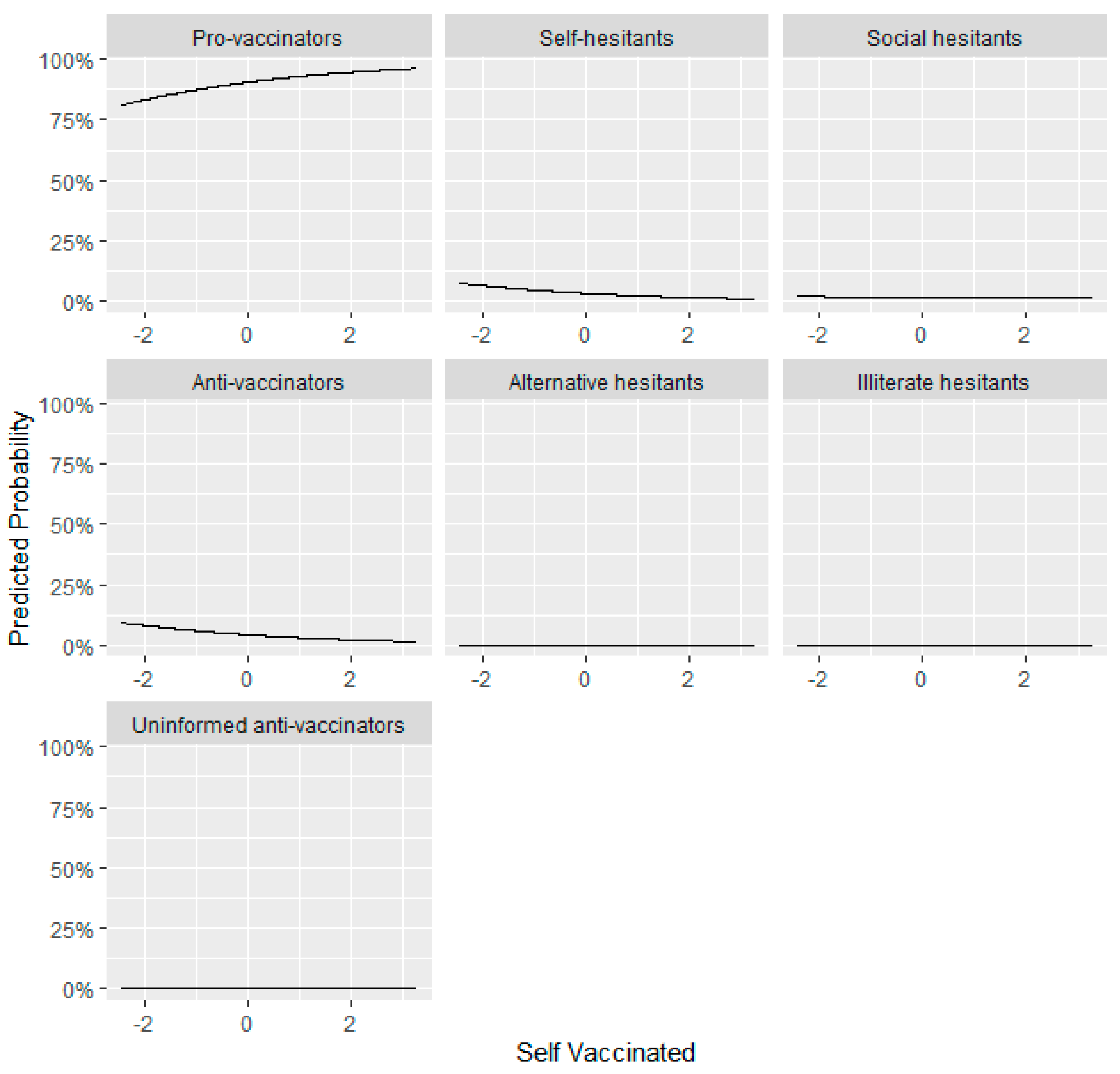
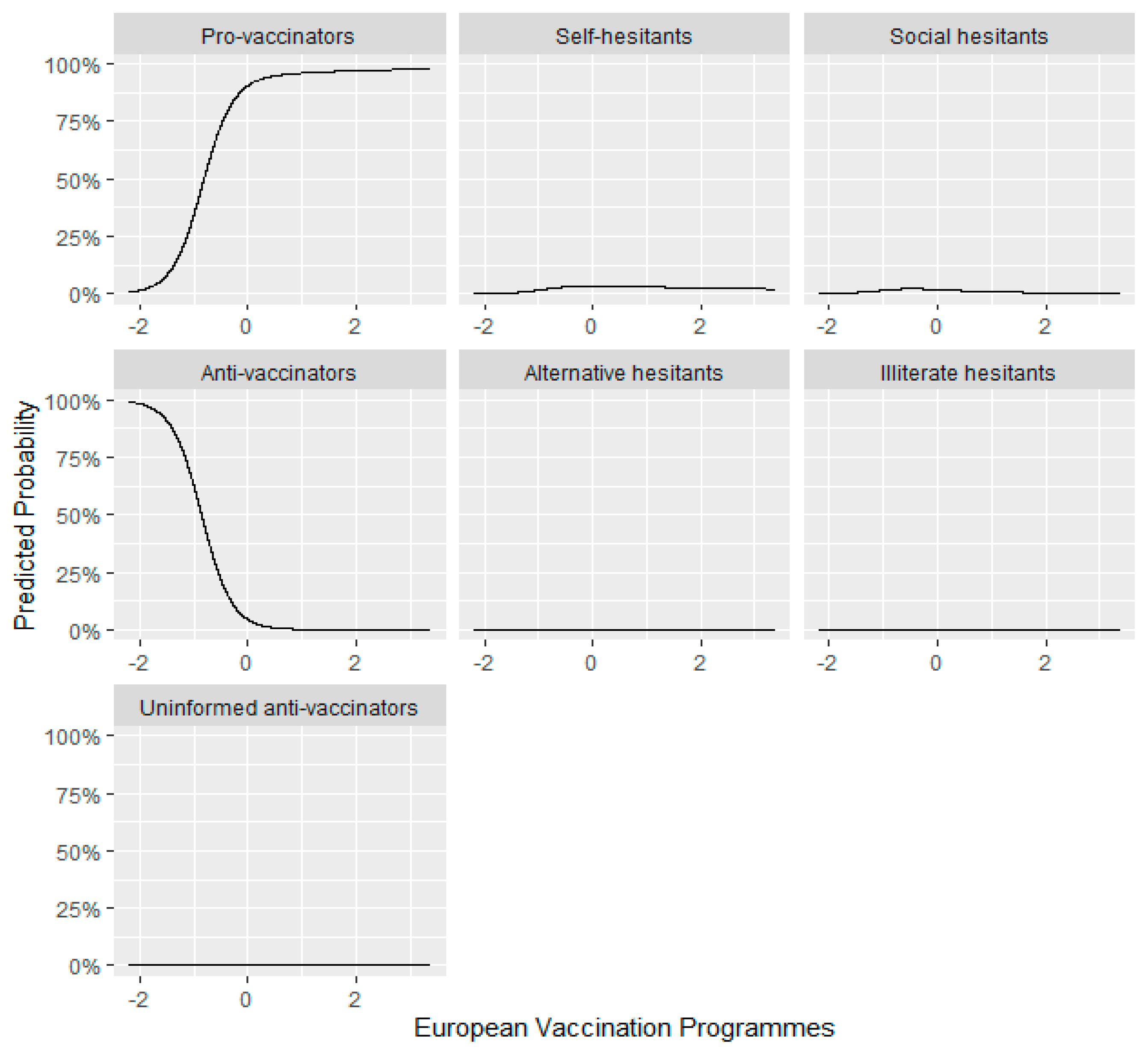
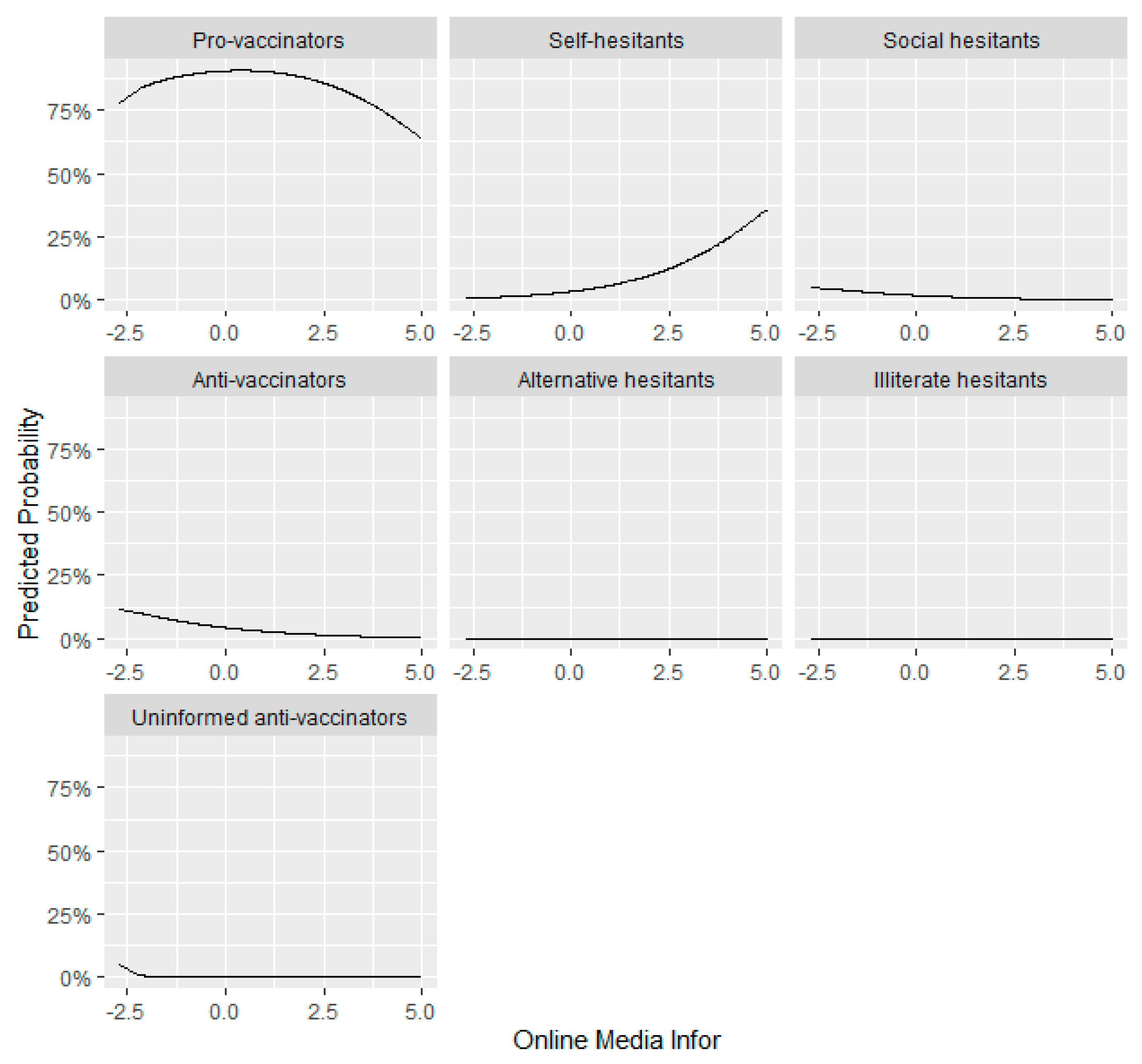
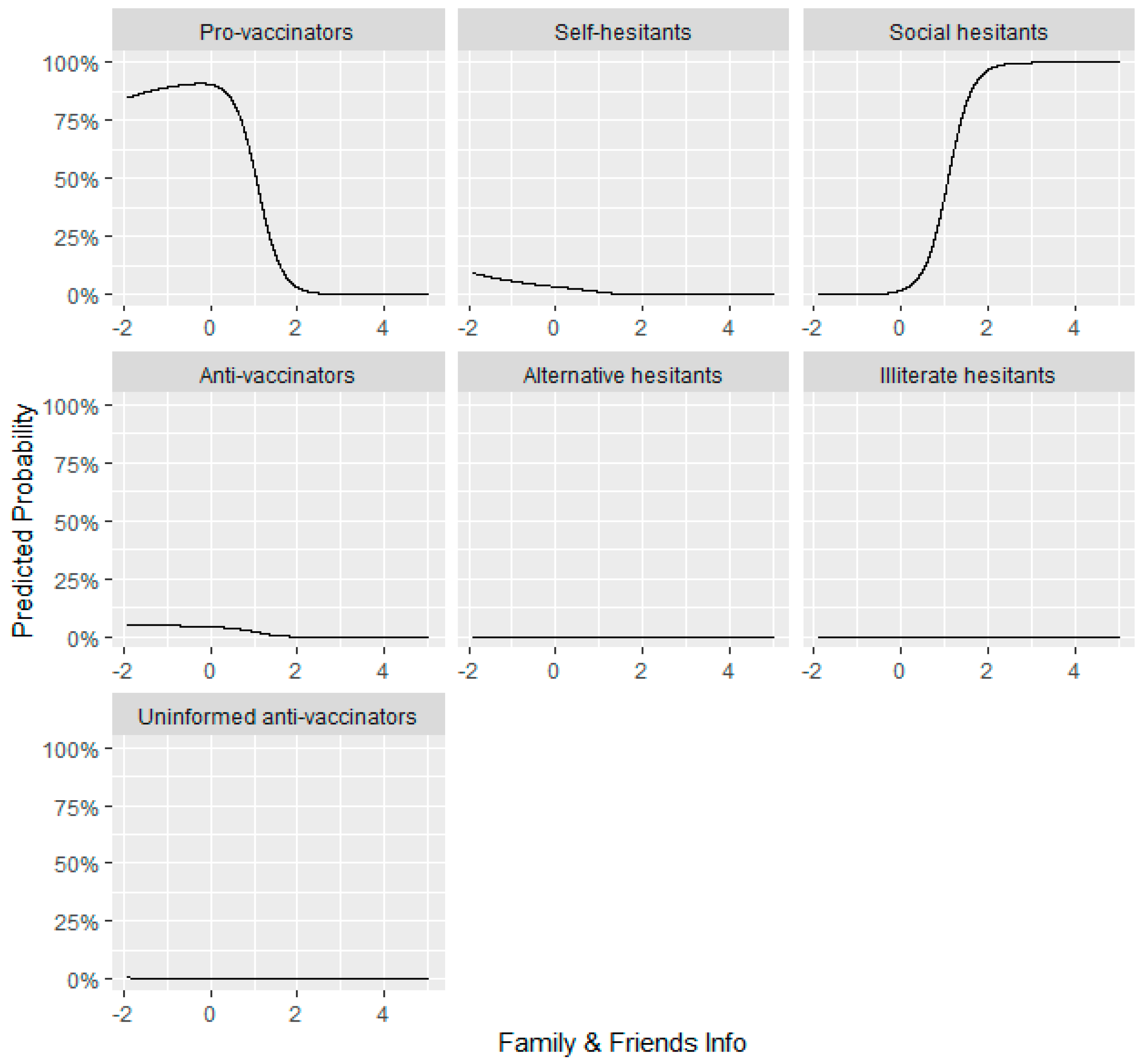
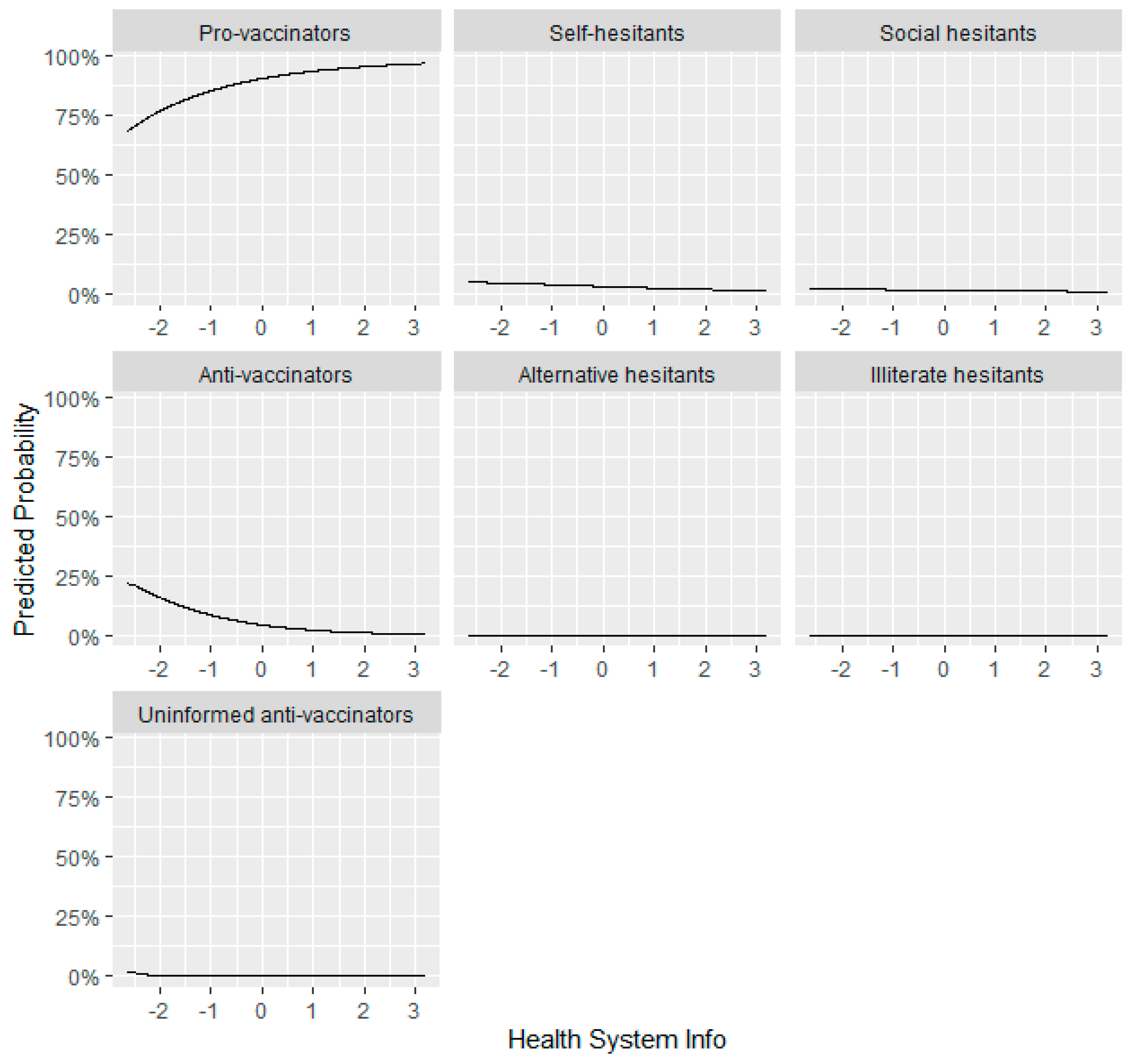
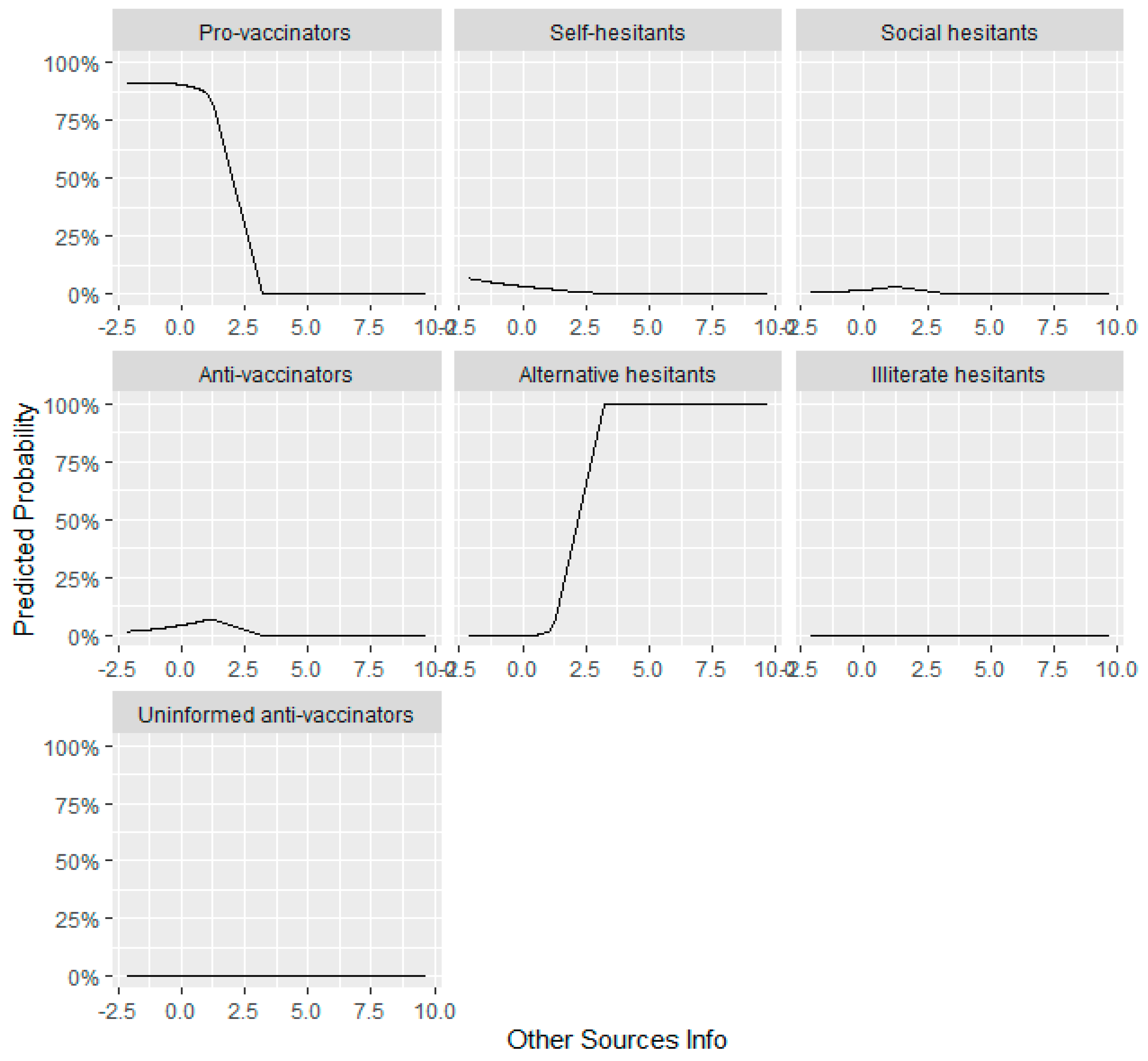
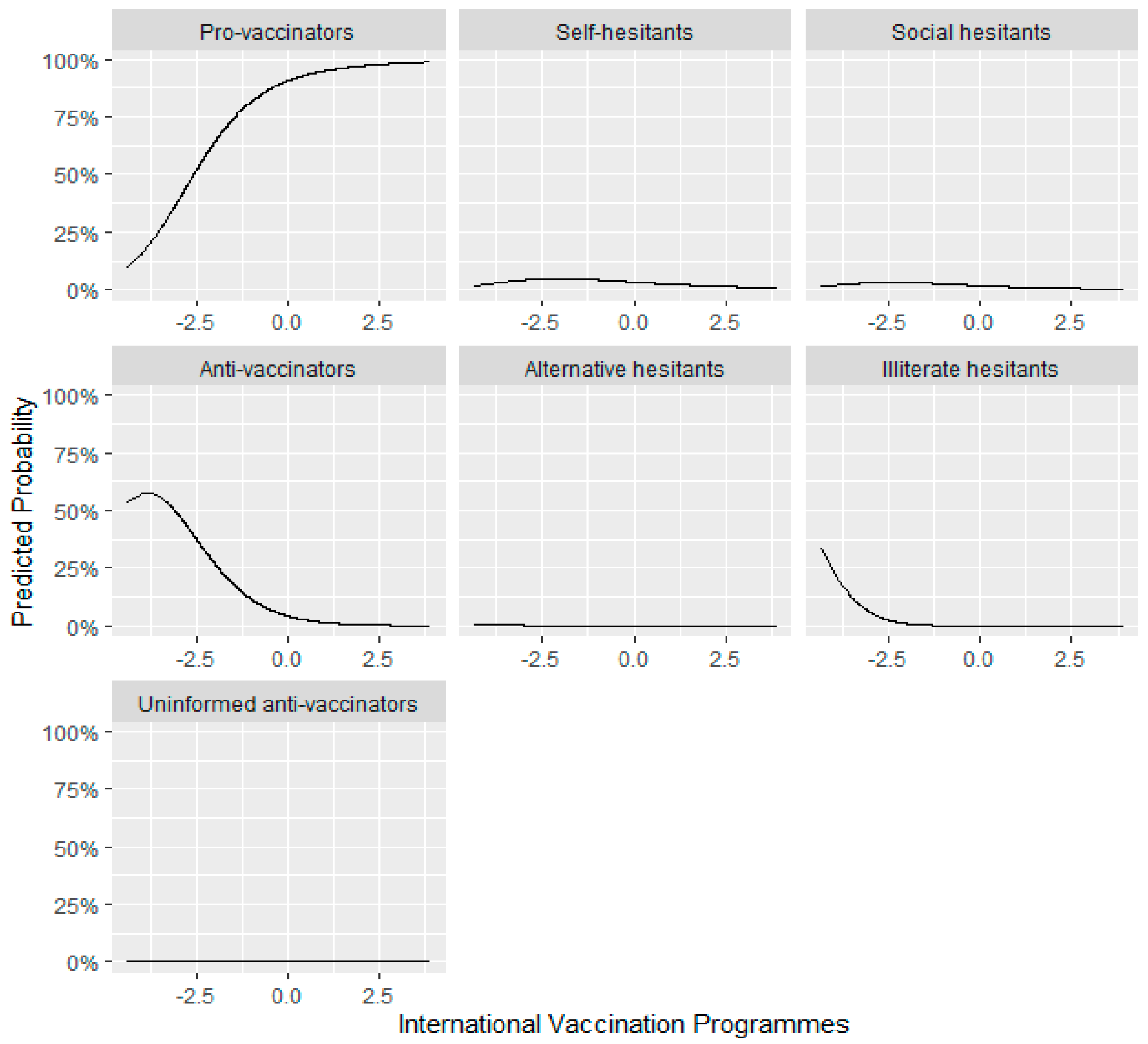
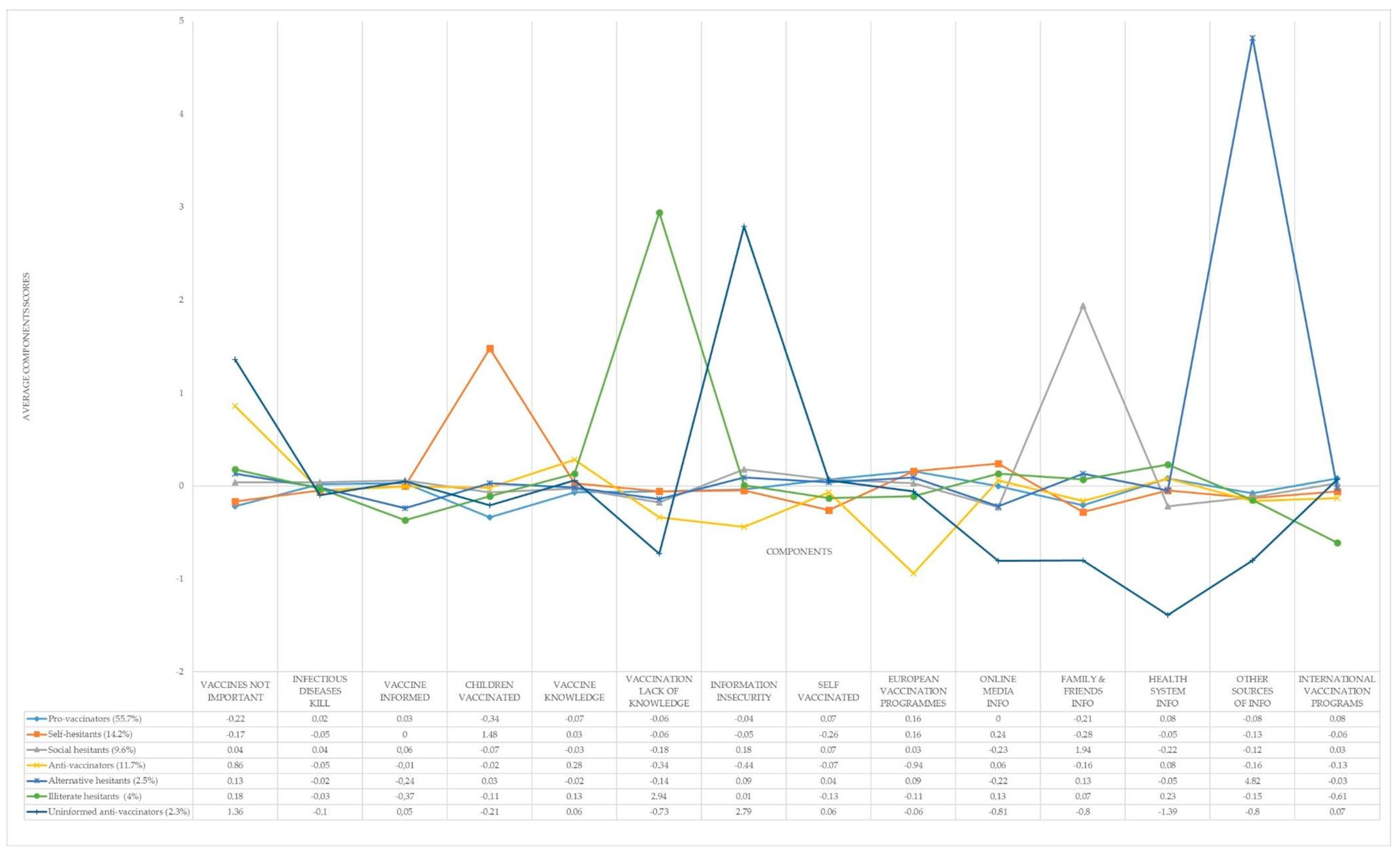
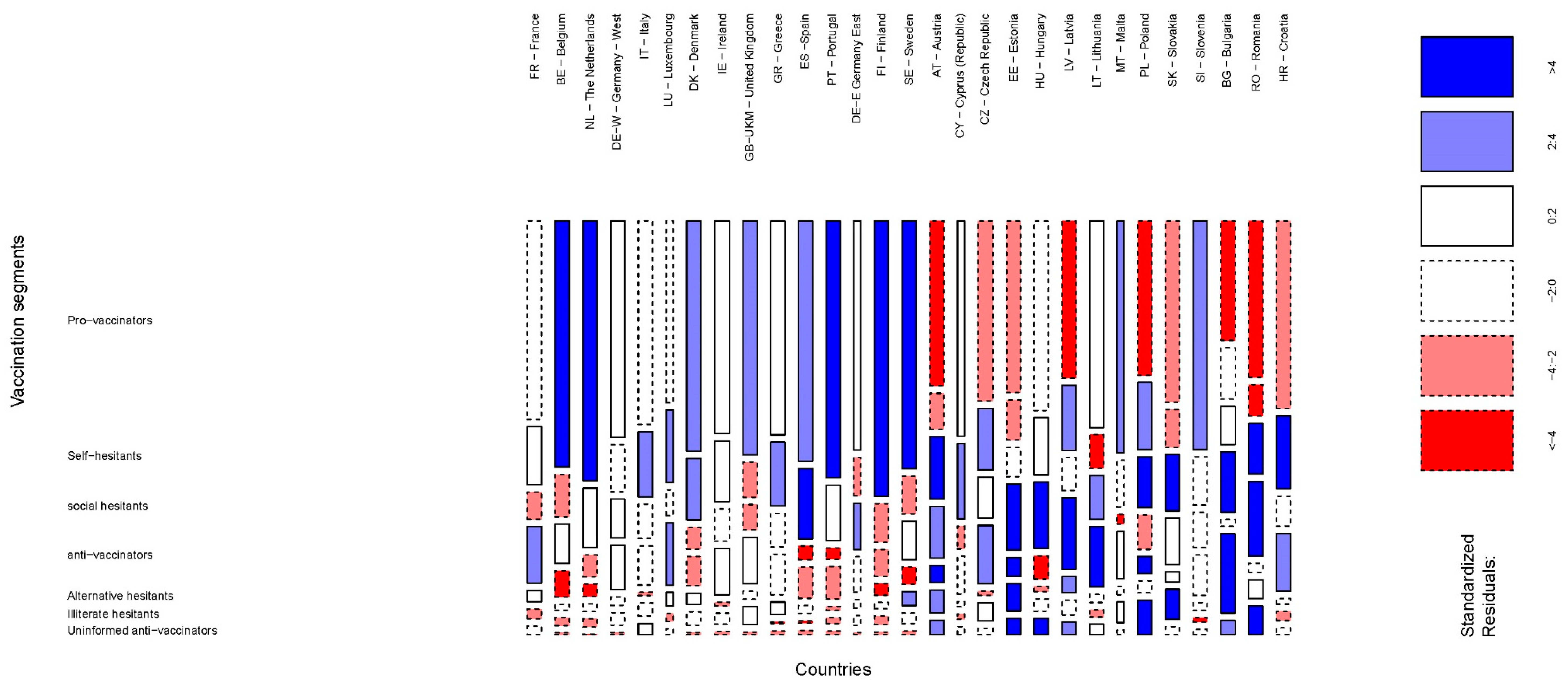
- Pro-Vaccinators (55.7% of the sample). It was the most numerous European segment. Following the segment profile represented in Figure 1, people for whom vaccines were the most important for avoiding the negative effects of infectious diseases formed it (in Table A3, Appendix C, we saw that mean differences with all the other segments were statistically significant). It belonged to the group of segments that answered that they felt better informed about vaccines, but the information received was highly insecure. Attending to how the “Information insecurity” component was composed, we saw that it had three significant loadings—the answers “None (SPONTANEOUS)” and “DK” to the question “If you were looking for information about vaccination, which of the following sources would you consult?”, and the high importance of the option “Family” when responding the question “And which of the following sources do you trust the most for information on vaccination?”—It portrays a component with the family as the most important source of information about vaccination, under the feeling of insecurity about any information source related to this issue. All the fake news that is present in the information environment is affecting the perception of knowledge, even in the pro-vaccinators segment. Insecurity about information affects the perception of knowledge. Therefore, the Europeans that belonged to this segment had the lowest scores on knowledge about vaccines and vaccination. They were vaccinated in the last five years. Their most preferred source of information was the Health System Info. They agreed that either European or international organizations should manage vaccination programs globally.
- Self-hesitants (14.2% of the sample). It was the second segment that made a point on jabs to avoid infectious diseases. They shared a profile with Pro-vaccinators in relation to the information: they had information but not knowledge about vaccines, and were not personally vaccinated due to information insecurity. They had no doubts about their child’s vaccination (see in Figure 1 that they had the highest score of all segments) but they did when they were inoculated. That was why they were labeled as “Self-hesitants”. Their favored source of information was Online Media Info, followed by the Health-System Info.They agreed that vaccination programs should be managed by international organizations, with the European authorities being the most preferred ones.
- Social-hesitants (9.6% of the total sample). This segment displayed a medium-range position on the importance of vaccines in avoiding infectious diseases. The respondents replied having been inoculated in the past five years at the same level as the Pro-vaccinators but their hesitance affected their child’s vaccination. They declared themselves to be informed but with a feeling of lack of knowledge about vaccines and vaccination. This led them to information insecurity. They did not trust Online Media Info nor Health System Info preferring, by far, their relatives as the main information source. That is why we called them Social-hesitants. They slightly preferred that international organizations managed the vaccination programs instead of the European authorities.
- Anti-vaccinators (11.7% of the sample). They showed the lowest confidence in vaccines of all the segments. They declared themselves to be well informed and with top knowledge on vaccines but not on vaccination. They did not feel insecure about the information received. Their unconfident belief caused them not to be open about taking vaccines, but they did not show the same behavior for their children. Their preferred sources of information were Online Media Info and Health System Info. A remarkable characteristic of this segment was that they did not trust international organizations for managing the vaccination programs, mainly favoring the European ones.
- Alternative-hesitants (2.5% of the sample). The hesitancy for this group was mainly based on the lack of confidence in Online Media Info and Health System Info. Otherwise, they felt comfortable with Family and Friends Info and showed an absolute preference for Other Sources of Info. In consequence, the reported information insecurity was also high. They portrayed a lack of knowledge about vaccines and vaccination. They shared with the other hesitant groups the lack of confidence in vaccines but, surprisingly, they and their children were among the top segments that had taken vaccines in the last five years.
- Illiterate-hesitants (4% of the sample). This group share with other hesitants their lack of confidence in vaccines. Their most noteworthy characteristic is that they declared themselves not to be well informed about vaccines. Their vaccination status in the past five years was in the medium range of all groups. The most liked source of information was the Health System Info, closely followed by Online Media Info and Family and Friends. They showed a complete lack of confidence in international organizations when managing the vaccines’ programs. European authorities were also not well considered.
- Uninformed Anti-Vaccinators (2.3% of the sample). The first distinctive attribute is that they had the lowest score in vaccine trust. Accordingly, they showed the lowest score in believing that infectious diseases kill. They declared themselves to be vaccine informed and to have an average knowledge on vaccines. Nonetheless, they had an absolute lack of knowledge about vaccination. The insecurity felt by this group about the information received was also the highest of all the segments found. It was so high that they did not trust any source of information. They rather preferred that the international organization would manage the vaccination programs. All these sentiments produced low vaccination rates among their children.
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Variable # 1 | Variable | Response Categories | n | Sample Share |
|---|---|---|---|---|
| qc1 | Diseases causing deaths in the EU nowadays | Flu | 16,464 | 59.8 |
| Measles | 10,547 | 38.3 | ||
| Polio | 4808 | 17.5 | ||
| Hepatitis | 11,323 | 41.1 | ||
| Meningitis | 14,190 | 51.6 | ||
| Tetanus | 6315 | 22.9 | ||
| None of them | 2348 | 8.5 | ||
| Don’t Know (DK) | 1728 | 6.3 | ||
| qc2 | Vaccines effective | Yes, definitely | 13,972 | 50.8 |
| Yes, probably | 9450 | 34.3 | ||
| No, probably not | 1664 | 6 | ||
| No, not at all | 870 | 3.2 | ||
| It depends on the disease | 1011 | 3.7 | ||
| Don’t Know (DK) | 557 | 2 | ||
| qc3 | Vaccinations in family last five years | Yes, yourself | 11,820 | 42.9 |
| Yes, your children | 7164 | 26 | ||
| Yes, someone else | 5521 | 19.1 | ||
| No | 9683 | 35.2 | ||
| Don’t Know (DK) | 315 | 1.1 | ||
| qc6 | Have vaccination card | Yes, for yourself | 11,754 | 42.7 |
| Yes, for your children | 6813 | 24.8 | ||
| No | 11,978 | 43.5 | ||
| Don’t Know (DK) | 651 | 2.4 | ||
| qc7_1 | Vaccines affect the immune system | TRUE | 8849 | 32.2 |
| FALSE | 14,461 | 52.5 | ||
| Do not Know (DK) | 4214 | 15.3 | ||
| qc7_2 | Vaccines cause diseases | TRUE | 10,669 | 38.8 |
| FALSE | 13,066 | 47.5 | ||
| Don’t Know (DK) | 3789 | 13.8 | ||
| qc7_3 | Vaccines side-effects | TRUE | 13,617 | 49.5 |
| FALSE | 10,735 | 39 | ||
| Don’t Know (DK) | 3172 | 11.5 | ||
| qc7_4 | Vaccines tested | TRUE | 21,884 | 79.5 |
| FALSE | 2736 | 9.9 | ||
| Don’t Know (DK) | 2904 | 10.6 | ||
| qc8_1 | Routine vaccination important | Totally agree | 14,222 | 51.7 |
| Tend to agree | 8776 | 31.9 | ||
| Tend to disagree | 2670 | 9.7 | ||
| Totally disagree | 890 | 3.2 | ||
| Don’t Know (DK) | 966 | 3.5 | ||
| qc8_2 | Vaccines only for children | Totally agree | 3643 | 13.2 |
| Tend to agree | 4551 | 16.5 | ||
| Tend to disagree | 8351 | 30.3 | ||
| Totally disagree | 10,270 | 37.3 | ||
| Don’t Know (DK) | 709 | 2.6 | ||
| qc8_3 | Not vaccinated serious health issues | Totally agree | 13,065 | 47.5 |
| Tend to agree | 9371 | 34 | ||
| Tend to disagree | 3008 | 10.9 | ||
| Totally disagree | 932 | 3.4 | ||
| Don’t Know (DK) | 1148 | 4.2 | ||
| qc8_4 | Vaccines’ importance for self and others | Totally agree | 15,284 | 55.5 |
| Tend to agree | 8956 | 32.5 | ||
| Tend to disagree | 1819 | 6.6 | ||
| Totally disagree | 577 | 2.1 | ||
| Don’t Know (DK) | 888 | 3.2 | ||
| qc8_5 | Vaccines’ importance for non-vaccinated | Totally agree | 14,505 | 52.7 |
| Tend to agree | 9296 | 33.8 | ||
| Tend to disagree | 1786 | 6.5 | ||
| Totally disagree | 598 | 2.2 | ||
| Don’t Know (DK) | 1339 | 4.9 | ||
| qc9 | Vaccine info sources | Family | 2627 | 9.5 |
| Friends | 1351 | 4.9 | ||
| Your general practitioner, a doctor, or a pediatrician | 21,765 | 79.1 | ||
| Other health care workers (nurses, specialist doctors, etc.) | 8647 | 31.4 | ||
| Pharmacists | 5103 | 18.5 | ||
| Online social networks | 1632 | 5.9 | ||
| Other Internet sites | 3539 | 12.9 | ||
| The health authorities | 7570 | 27.5 | ||
| Other (SPONTANEOUS) | 298 | 1.1 | ||
| None (SPONTANEOUS) | 504 | 1.8 | ||
| Don’t Know (DK) | 238 | 0.9 | ||
| qc10 | Most trusted vaccine info source | Family | 845 | 3.1 |
| Friends | 355 | 1.3 | ||
| Your general practitioner, a doctor, or a pediatrician | 17,521 | 63.7 | ||
| Other health care workers (nurses, specialist doctors, etc.) | 2695 | 9.8 | ||
| Pharmacists | 928 | 3.4 | ||
| Online social networks | 285 | 1 | ||
| Other Internet sites | 553 | 2 | ||
| The health authorities | 3323 | 12.1 | ||
| Other (SPONTANEOUS) | 74 | 0.3 | ||
| None (SPONTANEOUS) | 576 | 2.1 | ||
| Don’t Know (DK) | 369 | 1.3 | ||
| qc11 | Vaccine programs’ coordination level | At international level | 8911 | 32.4 |
| At European level | 8399 | 30.5 | ||
| At a national level | 4526 | 42.4 | ||
| At regional or local level | 2512 | 9.1 | ||
| There should be no vaccination programs, it is a personal choice | ||||
| Don’t Know (DK) | 1305 | 4.7 | ||
| qc12 | Media info on vaccine last six months | No | 8052 | 29.3 |
| Yes, on TV | 15,447 | 56.1 | ||
| Yes, on the radio | 4775 | 17.3 | ||
| Yes, in newspapers or magazines | 5771 | 21 | ||
| Yes, on online social networks | 3571 | 13 | ||
| Yes, on other Internet sites | 2835 | 10.3 | ||
| Other (SPONTANEOUS) | 433 | 1.6 | ||
| Don’t Know (DK) | 490 | 1.8 |
Appendix B
| Components | Components (Eigen Values) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| C1 (5.00) | C2 (4.43) | C4 (3.29) | C5 (2.53) | C3 (2.47) | C12 (2.30) | C8 (2.24) | C11 (2.16) | C7 (2.14) | C13 (1.86) | C6 (1.71) | C10 (1.69) | C9 (1.62) | C14 (1.33) | |
| Question | Vaccines are Not Important | Infectious Diseases Kill | Vaccine Informed | Children Vaccinated | Vaccines Are Dangerous | Vaccination Lack of Knowledge | Information Insecurity | Self Vaccinated | European Vaccination Programs | Online Media Info | Family & Friends Info | Health System Info | Other Sources of Information | International Vaccination Programs |
| qc1.1 | 0.7 | |||||||||||||
| qc1.2 | 0.7 | |||||||||||||
| qc1.3 | 0.8 | |||||||||||||
| qc1.4 | 0.7 | |||||||||||||
| qc1.5 | 0.7 | |||||||||||||
| qc1.6 | 0.8 | |||||||||||||
| qc1.7 | ||||||||||||||
| qc1.8 | ||||||||||||||
| qc2 | 0.6 | |||||||||||||
| qc3.1 | 0.7 | |||||||||||||
| qc3.2 | 0.8 | |||||||||||||
| qc3.3 | 0.7 | |||||||||||||
| qc3.4 | ||||||||||||||
| qc3.5 | 0.7 | |||||||||||||
| qc6.1 | 0.5 | 0,5 | ||||||||||||
| qc6.2 | 0.9 | |||||||||||||
| qc6.3 | ||||||||||||||
| qc6.4 | 0.7 | |||||||||||||
| qc7_1 | 0.8 | |||||||||||||
| qc7_2 | 0.8 | |||||||||||||
| qc7_3 | 0.8 | |||||||||||||
| qc7_4 | 0.5 | |||||||||||||
| qc8_1 | 0.8 | |||||||||||||
| qc8_2 | 0.5 | |||||||||||||
| qc8_3 | 0.8 | |||||||||||||
| qc8_4 | 0.9 | |||||||||||||
| qc8_5 | 0.8 | |||||||||||||
| qc9.1 | 0.8 | |||||||||||||
| qc9.2 | 0.8 | |||||||||||||
| qc9.3 | ||||||||||||||
| qc9.4 | 0.7 | |||||||||||||
| qc9.5 | 0.5 | |||||||||||||
| qc9.6 | 0.6 | |||||||||||||
| qc9.7 | 0.8 | |||||||||||||
| qc9.8 | 0.8 | |||||||||||||
| qc9.9 | 0.7 | |||||||||||||
| qc9.10 | 0.5 | 0.5 | ||||||||||||
| qc9.11 | 0.4 | 0.4 | 0.5 | |||||||||||
| qc.10 | 0.9 | |||||||||||||
| qc11.1 | 0,6 | |||||||||||||
| qc11.2 | 0.6 | |||||||||||||
| qc11.3 | 0.8 | |||||||||||||
| qc11.4 | 0.8 | |||||||||||||
| qc11.5 | 0.6 | |||||||||||||
| qc11.6 | 0.4 | |||||||||||||
| qc12.1 | ||||||||||||||
| qc12.2 | 0.8 | |||||||||||||
| qc12.3 | 0.9 | |||||||||||||
| qc12.4 | 0.7 | |||||||||||||
| qc12.5 | 0.6 | 0.5 | ||||||||||||
| qc12.6 | 0.5 | 0.5 | ||||||||||||
| qc12.7 | 0.8 | |||||||||||||
| qc12.8 | 0.5 | |||||||||||||
Appendix C
| Title Vaccine-Hesitancy Segments | Vaccines Are Not Important | Infectious Diseases Kill | Vaccine Informed | Children Vaccinated | Vaccines Are Dangerous | Vaccination Lack of Knowledge | Information Insecurity |
|---|---|---|---|---|---|---|---|
| Self-hesitants/Pro-vaccinators | 0.05 ** | −0.08 *** | −0.03 | 1.82 *** | 0.10 *** | 0 | −0.01 |
| Social hesitants/Pro-vaccinators | 0.27 *** | 0.02 | 0.04 | 0.28 *** | 0.04 | −0.12 *** | 0.22 *** |
| Anti-vaccinators/Pro-vaccinators | 1.08 *** | −0.08 *** | −0.04 | 0.32 *** | 0.35 *** | −0.29 *** | −0.40 *** |
| Alternative hesitants/Pro-vaccinators | 0.35 *** | −0.05 | −0.27 *** | 0.37 *** | 0.05 | −0.08 ** | 0.14 *** |
| Illiterate hesitants/Pro-vaccinators | 0.40 *** | −0.05 | −0.4 *** | 0.24 *** | 0.20 *** | 3.00 *** | 0.05 |
| Uninformed anti-vaccinators/Pro-vaccinators | 1.58 *** | −0.13 ** | 0.02 | 0.13 *** | 0.14 ** | −0.67 *** | 2.84 *** |
| Social hesitants/Self-hesitants | 0.21 *** | 0.09 *** | 0.06* | −1.55 *** | −0.06 | −0.12 *** | 0.23 *** |
| Anti-vaccinators/Self-hesitants | 1.03 *** | 0.00 | −0.01 | −1.5 *** | 0.25 *** | −0.29 *** | −0.39 *** |
| Alternative hesitants/Self-hesitants | 0.30 *** | 0.03 | −0.24 *** | −1.45 *** | −0.05 | −0.08 * | 0.15 *** |
| Illiterate hesitants/Self-hesitants | 0.35 *** | 0.03 | −0.37 *** | −1.59 *** | 0.10 * | 3.00 *** | 0.06 |
| Uninformed anti-vaccinators/Self-hesitants | 1.53 *** | −0.05 | 0.05 | −1.69 *** | 0.04 | −0.67 *** | 2.85 *** |
| Anti-vaccinators/Social hesitants | 0.82 *** | −0.09 *** | −0.08 ** | 0.04 | 0.31 *** | −0.16 *** | −0.62 *** |
| Alternative hesitants/Social hesitants | 0.08 | −0.06 | −0.31 *** | 0.09 | 0.01 | 0.04 | −0.09 |
| Illiterate hesitants-Social hesitants | 0.14 *** | −0.07 | −0.44 *** | −0.04 | 0.16 | 3.13 *** | −0.17 *** |
| Uninformed anti-vaccinators/Social hesitants | 1.32 *** | −0.14 *** | −0.02 | −0.15 *** | 0.1 | −0.55 *** | 2.61 *** |
| Alternative hesitants/Anti-vaccinators | −0.073 *** | 0.03 | −0.23 *** | 0.05 | −0.30 *** | 0.20 *** | 0.53 *** |
| Illiterate hesitants-Anti-vaccinators | −0.68 *** | 0.02 | −0.36 *** | −0.08 * | −0.15 *** | 3.29 *** | 0.45 *** |
| Uninformed anti-vaccinators/Anti-vaccinators | 0.50 *** | −0.05 | 0.06 | −0.19 * | −0.21 *** | −0.38 *** | 3.23 *** |
| Illiterate hesitants/Alternative hesitants | 0.05 | 0.00 | −0.13 * | −0.13 *** | 0.15 * | 3.08 *** | −0.09 |
| Uninformed anti-vaccinators/Alternative hesitants | 1.23 *** | −0.08 | 0.29 *** | −0.24 ** | 0.09 | −0.59 *** | 2.70 *** |
| Uninformed anti-vaccinators/Illiterate hesitants | 1.18 *** | −0.08 | 0.42 *** | −0.11 *** | −0.06 | −3.67 *** | 2.78 *** |
| Self-hesitants/Pro-vaccinators | −0.34 *** | 0.01 | 0.24 *** | −0.07 *** | −0.13 *** | −0.04 *** | −0.14 *** |
| Social hesitants/Pro-vaccinators | 0 | −0.13 *** | −0.23 *** | 2.15 *** | −0.30 *** | −0.04 *** | −0.05 |
| Anti-vaccinators/Pro-vaccinators | −0.14 *** | −1.09 *** | 0.06 * | 0.05 *** | 0 | −0.07 *** | −0.21 *** |
| Alternative hesitants/Pro-vaccinators | −0.04 | −0.07 | −0.22 *** | 0.34 *** | −0.13 ** | 4.90 *** | −0.11 |
| Illiterate hesitants/Pro-vaccinators | −0.20 *** | −0.27 *** | 0.13 *** | 0.28 *** | 0.15 *** | −0.06 *** | −0.69 *** |
| Uninformed anti-vaccinators/Pro-vaccinators | −0.01 | −0.22 *** | −0.81 *** | −0.59 *** | −1.47 *** | −0.72 *** | −0.01 |
| Social hesitants/Self-hesitants | 0.34 *** | −0.14 *** | −0.47 *** | 2.23 *** | −0.16 *** | 0 | 0.10 ** |
| Anti-vaccinators/Self-hesitants | 0.20 *** | −1.10 *** | −0.18 *** | 0.13 *** | 0.13 *** | −0.03 ** | −0.07 * |
| Alternative hesitants/Self-hesitants | 0.30 *** | −0.08 | −0.46 *** | 0.42 *** | 0 | 4.95 *** | 0.03 |
| Illiterate hesitants/Self-hesitants | 0.14 ** | −0.27 *** | −0.11 ** | 0.35 *** | 0.28 *** | −0.02 | −0.54 *** |
| Uninformed anti-vaccinators/Self-hesitants | 0.32 *** | −0.22 *** | −1.05 *** | −0.51 *** | −1.34 *** | −0.67 *** | 0.13 * |
| Anti-vaccinators/Social hesitants | −0.14 *** | −0.96 *** | 0.29 *** | −2.10 *** | 0.30 *** | −0.04 | −0.17 *** |
| Alternative hesitants/Social hesitants | −0.04 | 0.06 | 0.01 | −1.81 *** | 0.16 *** | 4.94 *** | −0.06 |
| Illiterate hesitants-Social hesitants | −0.20 *** | −0.14 *** | 0.35 *** | −1.87 *** | 0.45 *** | −0.03 ** | −0.64 *** |
| Uninformed anti-vaccinators/Social hesitants | −0.01 | −0.09 | −0.59 *** | −2.74 *** | −1.18 *** | −0.68 *** | 0.04 |
| Alternative hesitants/Anti-vaccinators | 0.11 | 1.02 *** | −0.28 *** | 0.29 *** | −0.13 ** | 4.98 *** | 0.10 |
| Illiterate hesitants-Anti-vaccinators | −0.06 | 0.83 *** | 0.07 | 0.23 *** | 0.15 *** | 0.01 | −0.47 *** |
| Uninformed anti-vaccinators/Anti-vaccinators | 0.13 * | 0.88 *** | −0.87 *** | −0.64 *** | −1.47 *** | −0.64 *** | 0.20 *** |
| Illiterate hesitants/Alternative hesitants | −0.17 ** | −0.19 *** | 0.35 *** | −0.06 | 0.28 *** | −4.97 *** | −0.58 *** |
| Uninformed anti-vaccinators/Alternative hesitants | 0.02 | −0.14 * | −0.59 *** | −0.93 *** | −1.34 *** | −5.62 *** | 0.10 |
| Uninformed anti-vaccinators/Illiterate hesitants | 0.19 ** | 0.05 | −0.94 *** | −0.87 *** | −1.63 *** | −0.65 *** | 0.68 *** |
Appendix D

References
- European Parliament. Resolution of 19 April 2018 on Vaccine Hesitancy and Drop in Vaccination Rates in Europe (2017/2951 RSP). Available online: https://www.europarl.europa.eu/doceo/document/TA-8-2018-0188_EN.pdf (accessed on 20 May 2021).
- World Health Organization. Ten Threats to Global Health in 2019. Available online: https://www.who.int/emergencies/ten-threats-to-global-health-in-2019 (accessed on 18 December 2020).
- Williams, G. The Original Antivaxxers. Available online: https://www.economist.com/1843/2019/08/30/the-original-anti-vaxxers (accessed on 30 July 2020).
- Little, L.C. Crimes of the Cowpox Ring; The Liberator Pub. Co.: London, UK, 1907. [Google Scholar]
- Larson, H.; de Figueiredo, A.; Karafillakis, E.; Rawal, M. State of Vaccine Confidence in the EU 2018; European Union: Luxembourg, 2018. [Google Scholar]
- WHO. WHO-UNICEF Coverage Estimates. Available online: https://apps.who.int/immunization_monitoring/globalsummary/timeseries/tswucoveragemcv1.html (accessed on 1 April 2021).
- Funk, S. Critical Immunity Thresholds for Measles Elimination. Available online: https://www.who.int/immunization/sage/meetings/2017/october/2._target_immunity_levels_FUNK.pdf (accessed on 1 April 2021).
- Lazarus, J.V.; Ratzan, S.C.; Palayew, A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Kimball, S.; El-Mohandes, A. A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 2020, 27, 225–228. [Google Scholar] [CrossRef]
- De Figueiredo, A.; Simas, C.; Karafillakis, E.; Paterson, P.; Larson, H.J. Mapping global trends in vaccine confidence and investigating barriers to vaccine uptake: A large-scale retrospective temporal modelling study. Lancet 2020, 396, 898–908. [Google Scholar] [CrossRef]
- The Economist Conspiracy Theories about Covid-19 Vaccines May Prevent Herd Immunity. Econ. 2020. 29 August 2020 Edition. Available online: https://www.economist.com/graphic-detail/2020/08/29/conspiracy-theories-about-covid-19-vaccines-may-prevent-herd-immunity (accessed on 1 March 2021).
- The Council of the European Union Council Recommendation of 7 December 2018 on Strenthened Cooperation against Vaccine-Preventable Diseases 2018/C 466/0. Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:32018H1228(01)&from=ES (accessed on 15 May 2021).
- Dubé, E.; Leask, J.; Wolff, B.; Hickler, B.; Balaban, V.; Hosein, E.; Habersaat, K. The WHO Tailoring Immunization Programmes (TIP) approach: Review of implementation to date. Vaccine 2018, 36, 1509–1515. [Google Scholar] [CrossRef]
- French, J.; Deshpande, S.; Evans, W.; Obregon, R. Key guidelines in developing a pre-emptive COVID-19 vaccination uptake promotion strategy. Int. J. Environ. Res. Public Health 2020, 17, 5893. [Google Scholar] [CrossRef]
- Fournet, N.; Mollema, L.; Ruijs, W.L.; Harmsen, I.A.; Keck, F.; Durand, J.Y.; Cunha, M.P.; Wamsiedel, M.; Reis, R.; French, J.; et al. Under-vaccinated groups in Europe and their beliefs, attitudes and reasons for non-vaccination; Two systematic reviews. BMC Public Health 2018, 18, 196. [Google Scholar] [CrossRef]
- Aurifeille, J.-M.; Quester, P.G.; Lockshin, L.; Spawton, T. Global vs international involvement-based segmentation. A cross-national exploratory study. Int. Mark. Rev. 2002, 19, 369–386. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. Social Marketing Guide for Public Health Programme Managers and Practitioners; ECDC: Stockholm, Sweden, 2014; ISBN 9789291936052. [Google Scholar]
- Zou, S.; Cavusgil, S.T. The GMS: A broad conceptualization of global marketing strategy and its effect on firm performance. J. Mark. 2002, 66, 40–56. [Google Scholar] [CrossRef]
- WHO. Tailoring Immunization Programmes (TIP) An Introductory Overview; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- ECOM Effective Communication in Outbreak Management (ECOM). Available online: http://ecomeu.info/ (accessed on 15 May 2021).
- TeellMe. Transparent Communication in Epidemics: Learning Lessons from Experience, Delivering Effective Messages, Providing Evidence. Available online: https://www.tellmeproject.eu/ (accessed on 15 May 2021).
- UNICEF. Human Centered Design 4 Health. Available online: https://www.hcd4health.org/resources (accessed on 15 May 2021).
- Hallsworth, M.; Snijders, V.; Burd, H.; Prestt, J.; Judah, G.; Huf, S.; Halpern, D. Applying Behavioural Insights WISH Forum 2016; The World Innovation Summit for Health: London, UK, 2016. [Google Scholar]
- Jain, S.C. Standardization of International Marketing Strategy: Some Research Hypotheses. J. Mark. 1989, 53, 70. [Google Scholar] [CrossRef]
- Schilke, O.; Reimann, M.; Thomas, J.S. Standardization Matter to Firm Performance? J. Int. Mark. 2009, 17, 24–46. [Google Scholar] [CrossRef]
- Tan, Q.; Sousa, C.M.P. International Marketing Standardization: A Meta-Analytic Estimation of Its Antecedents and Consequences. Manag. Int. Rev. 2013, 53, 711–739. [Google Scholar] [CrossRef]
- Mikulic, M. Global Pharmaceutical Industry—Statistics & Facts. Available online: https://www.statista.com/topics/1764/global-pharmaceutical-industry/#dossierSummary__chapter5 (accessed on 15 May 2021).
- Kennedy, J. Populist politics and vaccine hesitancy in Western Europe: An analysis of national-level data. Eur. J. Public Health 2019, 29, 512–516. [Google Scholar] [CrossRef]
- Larson, H.J. The biggest pandemic risk? Viral misinformation. Nature 2018, 562, 309. [Google Scholar] [CrossRef] [PubMed]
- Bolton, R.N.; Myers, M.B. Price-Based Global Market Segmentation for Business. J. Mark. 2003, 67, 108–128. [Google Scholar] [CrossRef]
- European Commission. Eurobarometer 91.2, March 2019; Gesis Data Archive: ZA7592, Data file Version 1.0.0; Kantar Public: London, UK, 2019. [Google Scholar]
- European Communities. Eurobarometer 63.4. Basic Bilingual Questionnaire TNS Opinion & Social; European Communities: Luxembourg, 2005. [Google Scholar]
- Fox, J. Polycor: Polychoric and Polyserial Correlations. R Package Version 0.7-10. Available online: https://CRAN.R-project.org/package=polycor (accessed on 5 June 2021).
- Savalei, V. What to do about zero frequency cells when estimating polychoric correlations. Struct. Equ. Model. 2011, 18, 253–273. [Google Scholar] [CrossRef]
- Horn, J. A rationale and test for the number of factors in factor analysis. Psychometrika 1965, 30, 179–185. [Google Scholar] [CrossRef]
- Osborne, J.W. Best Practices in Exploratory Factor Analysis; CreateSpace Independent Publishing: Scotts Valley, CA, USA, 2014; ISBN 978-1500594343. [Google Scholar]
- Tabachnick, B.G.; Fidell, L.S. Using Multivariate Statistics; Pearson: Boston, MA, USA, 2019; ISBN 9780134790541. [Google Scholar]
- Yong, A.G.; Pearce, S. A Beginner’s Guide to Factor Analysis: Focusing on Exploratory Factor Analysis. Tutor. Quant. Methods Psychol. 2013, 9, 79–94. [Google Scholar] [CrossRef]
- Hair, J.F.; Black, W.C.; Babin, B.J.; Anderson, R.E. Multivariate Data Analysis, 7th ed.; Pearson Education Limited: Essex, UK, 2014. [Google Scholar]
- Brock, G.; Pihur, V.; Datta, S.; Datta, S. ClValid: An R package for cluster validation. J. Stat. Softw. 2008, 25, 1–22. [Google Scholar] [CrossRef]
- Stan Development Team Stan Modeling Language Users Guide and Reference Manual, VERSION 2.26. Available online: https://mc-stan.org (accessed on 5 May 2021).
- SAS Computing Marginal Effects for Discrete Dependent Variable Models. Available online: https://support.sas.com/rnd/app/ets/examples/margeff/index.html (accessed on 15 March 2021).
- European Commission. Special Eurobarometer 488 Report Europeans ’ Attitudes towards Vaccination March 2019; European Commission: Brussels, Belgium, 2019. [Google Scholar]
- Meyer, D.; Zeileis, A.; Hornik, K. The strucplot framework: Visualizing multi-way contingency tables with VCD. J. Stat. Softw. 2006, 17, 1–48. [Google Scholar] [CrossRef]
- Friendly, M. Visualizing Categorical Data. Technometrics 2001, 43, 498–499. [Google Scholar]
- Dubé, È.; Ward, J.K.; Verger, P.; Macdonald, N.E. Vaccine Hesitancy, Acceptance, and Anti-Vaccination: Trends and Future Prospects for Public Health. Annu. Rev. Public Health 2021, 42, 175–191. [Google Scholar] [CrossRef]
- World Health Organization Vaccine Market. Available online: https://www.who.int/immunization/programmes_systems/procurement/market/individual_vaccine/en/ (accessed on 4 May 2021).
- Opel, D.J.; Diekema, D.S.; Lee, N.R.; Marcuse, E.K. Social marketing as a strategy to increase immunization rates. Arch. Pediatr. Adolesc. Med. 2009, 163, 432–437. [Google Scholar] [CrossRef]
- Nowak, G.J.; Gellin, B.G.; MacDonald, N.E.; Butler, R.; Eskola, J.; Liang, X.; Chaudhuri, M.; Dube, E.; Gellin, B.; Goldstein, S.; et al. Addressing vaccine hesitancy: The potential value of commercial and social marketing principles and practices. Vaccine 2015, 33, 4204–4211. [Google Scholar] [CrossRef]
- Washington State Department of Health. Social Marketing Recommendations for COVID-19 Vaccine; Washington State Department of Health: Seattle, WA, USA, 2020. [Google Scholar]
- Ahmed, I. Dismantling the anti-vaxx industry. Nat. Med. 2021, 27, 366. [Google Scholar] [CrossRef] [PubMed]
- Killian, M.; Detoc, M.; Berthelot, P.; Charles, R.; Gagneux-Brunon, A.; Lucht, F.; Pulcini, C.; Barbois, S.; Botelho-Nevers, E. Vaccine hesitancy among general practitioners: Evaluation and comparison of their immunisation practice for themselves, their patients and their children. Eur. J. Clin. Microbiol. Infect. Dis. 2016, 35, 1837–1843. [Google Scholar] [CrossRef] [PubMed]
- Wilson, R.J.I.; Vergélys, C.; Ward, J.; Peretti-Watel, P.; Verger, P. Vaccine hesitancy among general practitioners in Southern France and their reluctant trust in the health authorities. Int. J. Qual. Stud. Health Well-Being 2020, 15, 1757336. [Google Scholar] [CrossRef]
- Schmid, P.; Rauber, D.; Betsch, C.; Lidolt, G.; Denker, M.L. Barriers of Influenza Vaccination Intention and Behavior—A Systematic Review of Influenza Vaccine Hesitancy, 2005–2016; World Health Organization: Geneva, Switzerland, 2017; Volume 12. [Google Scholar]
- Paterson, P.; Meurice, F.; Stanberry, L.R.; Glismann, S.; Rosenthal, S.L.; Larson, H.J. Vaccine hesitancy and healthcare providers. Vaccine 2016, 34, 6700–6706. [Google Scholar] [CrossRef]
- Prematunge, C.; Corace, K.; McCarthy, A.; Nair, R.C.; Pugsley, R.; Garber, G. Factors influencing pandemic influenza vaccination of healthcare workers-A systematic review. Vaccine 2012, 30, 4733–4743. [Google Scholar] [CrossRef] [PubMed]
- Bahri, P.; Rägo, L. CIOMS Guide To Vaccine Safety Communication—Executive summary. Vaccine 2019, 37, 401–408. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, S.; MacDonald, N.E.; Guirguis, S.; Eskola, J.; Liang, X.; Chaudhuri, M.; Dube, E.; Gellin, B.; Larson, H.; Manzo, M.L.; et al. Health communication and vaccine hesitancy. Vaccine 2015, 33, 4212–4214. [Google Scholar] [CrossRef]
- Siegrist, M.; Zingg, A. The role of public trust during pandemics: Implications for crisis communication. Eur. Psychol. 2014, 19, 23–32. [Google Scholar] [CrossRef]
- Shore, D.A. Communicating in Times of Uncertainty: The Need for Trust. J. Health Commun. 2003, 8, 13–14. [Google Scholar] [CrossRef] [PubMed]
- European Commission. Communication from the Commission to the European Parliament, the Council, the European Economic and Social Committee and the Committee of the Regions Strengthened Cooperation against Vaccine Preventable Diseases com/2018/245 Final; Office for Official Publications of the European Communities: Luxembourg, 2018. [Google Scholar]
| COUNTRY | Number of Interviews | Population 15+ |
|---|---|---|
| Austria | 1006 | 7,554,711 |
| Belgium | 1041 | 9,693,779 |
| Bulgaria | 1026 | 6,537,535 |
| Croatia | 1010 | 3,796,476 |
| Czech Republic | 1068 | 9,238,431 |
| Denmark | 1017 | 4,838,729 |
| Estonia | 1005 | 1,160,064 |
| Finland | 1000 | 4,747,810 |
| France | 1013 | 54,097,255 |
| Germany | 1507 | 70,160,634 |
| Greece | 1014 | 9,937,810 |
| Hungary | 1030 | 8,781,161 |
| Ireland | 1078 | 3,592,162 |
| Italy | 1021 | 52,334,536 |
| Latvia | 1012 | 1,707,082 |
| Lithuania | 1004 | 2,513,384 |
| Luxemburg | 512 | 457,127 |
| Malta | 497 | 364,171 |
| Netherlands | 1017 | 13,979,215 |
| Poland | 1011 | 33,444,171 |
| Portugal | 1013 | 8,480,126 |
| Republic of Cyprus | 505 | 741,308 |
| Romania | 1025 | 16,852,701 |
| Slovakia | 1020 | 4,586,024 |
| Slovenia | 1016 | 1,760,032 |
| Spain | 1014 | 39,445,245 |
| Sweden | 1021 | 7,998,763 |
| United Kingdom | 1021 | 52,651,777 |
| TOTAL | 27,524 | 431,452,219 |
| Component # 1 | Component Name 1 | Original Variables with Significant Loadings | Percentage of Total Variance |
|---|---|---|---|
| C1 | Vaccines not important | Vaccines important | 9% |
| Vaccines are rigorously tested before being authorized for use | |||
| Everybody needs to have routine vaccinations | |||
| Not getting vaccinated can lead to serious health issues | |||
| Vaccines are important to protect not only yourself but also others | |||
| Vaccination of other people is important to protect those that cannot be vaccinated | |||
| C2 | Infectious diseases kill | Flu is causing deaths in the EU nowadays | 8% |
| Measles is causing deaths in the EU nowadays | |||
| Polio is causing deaths in the EU nowadays | |||
| Hepatitis is causing deaths in the EU nowadays | |||
| Meningitis is causing deaths in the EU nowadays | |||
| Tetanus is causing deaths in the EU nowadays | |||
| C3 | Vaccines are dangerous | Vaccines overload and weaken the immune system | 5% |
| Vaccines can cause the disease against which they protect | |||
| Vaccines can often produce serious side-effects | |||
| Do not know at which level vaccination programs should be coordinated | |||
| C4 | Vaccine informed | Seen vaccine info in the last six months on TV | 6% |
| Seen vaccine info in the last six months on the radio | |||
| Seen vaccine info in the last six months in newspapers or magazines | |||
| Seen vaccine info in the last six months on online social networks | |||
| Seen vaccine info in the last six months on other Internet sites | |||
| C5 | Children vaccinated | Have a vaccination card for children | 5% |
| Children vaccinated in the last five years | |||
| C6 | Family & friends info | If you were looking for information about vaccination, you would consult family | 3% |
| If you were looking for information about vaccination, you would consult friends | |||
| C7 | European vaccination programs | Vaccination programs should be coordinated at European level | 4% |
| Vaccination programs should be coordinated at a national level | |||
| Vaccination programs should be coordinated at a regional or local level | |||
| C8 | Information insecurity | If you were looking for information about vaccination NONE of the following sources you would consult | 4% |
| If you were looking for information about vaccination DO NOT KNOW which of the following sources you would consult | |||
| Family is the source you trust the most for information on vaccination | |||
| C9 | Other sources of info | If you were looking for information about vaccination, you would consult other sources of information | 3% |
| In the past six months, you have seen, read or heard any information on vaccination in other media | |||
| C10 | Health system info | If you were looking for information about vaccination, you would consult other health care workers (nurses, specialist doctors, etc.) | 3% |
| If you were looking for information about vaccination, you would consult pharmacists | |||
| If you were looking for information about vaccination, you would consult the health authorities | |||
| C11 | Self-vaccinated | I got vaccinated in the last five years | 4% |
| I have a vaccination card | |||
| Tend to agree that not getting vaccinated can lead to serious health issues | |||
| C12 | Vaccination lack of knowledge | Do not know if you or someone in your family had any vaccinations in the last five years | 4% |
| Do not know if you have a vaccination card | |||
| Do not know if you were looking for information about vaccination, which of the following sources would you consult | |||
| Do not know if in the past six months you have seen, read or heard any information on vaccination in the media | |||
| C13 | Online media info | If you were looking for information about vaccination you would consult online social networks | 4% |
| If you were looking for information about vaccination you would consult other Internet sites | |||
| In the past six months you have seen, read or heard information on vaccination on online social networks | |||
| In the past six months you have seen, read or heard information on vaccination on another Internet sites | |||
| C14 | International vaccination programs | You think vaccination programs should be coordinated at an international level | 3% |
| You have a vaccination card |
| Posterior Mean 1 | Posterior SD 2 | Rhat 3 | |
|---|---|---|---|
| Population-level effects (reference category: Pro-vaccinators) | |||
| Intercept Self-hesitants | −1.38 | 0.07 | 1.0 |
| Intercept Social-hesitants | −1.85 | 0.11 | 1.0 |
| Intercept Anti-vaccinators | −1.63 | 0.12 | 1.0 |
| Intercept Alternative-hesitants | −3.20 | 0.11 | 1.0 |
| Intercept Illiterate-hesitants | −2.90 | 0.17 | 1.0 |
| Intercept Uninformed Anti-vaccinators | −3.54 | 0.21 | 1.0 |
| Country-level effects (reference category: Pro-vaccinators) | |||
| Intercept Self-hesitants | 0.33 | 0.05 | 1.0 |
| Intercept Social-hesitants | 0.58 | 0.09 | 1.0 |
| Intercept Anti-vaccinators | 0.63 | 0.09 | 1.0 |
| Intercept Alternative-hesitants | 0.55 | 0.09 | 1.0 |
| Intercept Illiterate-hesitants | 0.89 | 0.14 | 1.0 |
| Intercept Uninformed Anti-vaccinators | 1.07 | 0.17 | 1.0 |
| Dependent Variable (Reference Category Pro-Vaccinators): | ||||||
|---|---|---|---|---|---|---|
| Self-Hesitants | Social Hesitants | Anti-Vaccinators | Alternative Hesitants | Illiterate Hesitants | Uninformed Anti-vaccinators | |
| C1 | −0.088 | 0.593 *** | 2.475 *** | 2.037 *** | 1.899 *** | 3.135 *** |
| −0.058 | −0.07 | −0.055 | −0.419 | −0.215 | −0.396 | |
| C2 | −0.498 *** | 0.05 | −0.488 *** | −0.076 | 0.619 *** | 0.454 |
| −0.041 | −0.053 | −0.044 | −0.486 | −0.231 | −0.438 | |
| C3 | 0.308 *** | 0.194 *** | 1.141 *** | 1.257 *** | 1.591 *** | 0.875 *** |
| −0.049 | −0.062 | −0.046 | −0.393 | −0.194 | −0.309 | |
| C4 | −0.262 *** | −0.249 *** | −0.611 *** | −0.691 | −2.597 *** | −1.617 *** |
| −0.039 | −0.056 | −0.05 | −0.555 | −0.273 | −0.554 | |
| C5 | 2.845 *** | 0.157 *** | 0.538 *** | −0.644 | 0.198 | 0.171 |
| −0.043 | −0.051 | −0.043 | −0.663 | −0.23 | −0.464 | |
| C6 | −0.569 *** | 3.694 *** | −0.146 * | 0.912 ** | 0.673 *** | −3.979 *** |
| −0.067 | −0.065 | −0.077 | −0.428 | −0.223 | −1.352 | |
| C7 | −0.180 *** | −0.800 *** | −3.637 *** | −1.922 *** | −1.843 *** | −1.129 ** |
| −0.045 | −0.062 | −0.063 | −0.498 | −0.222 | −0.441 | |
| C8 | 0.06 | −0.720 *** | 0.151 ** | 0.925 | 0.221 | 3.880 *** |
| −0.057 | −0.076 | −0.068 | −0.59 | −0.321 | −0.435 | |
| C9 | −0.337 *** | 0.537 *** | 0.465 *** | 5.333 *** | 0.301 | −0.702 |
| −0.106 | −0.138 | −0.123 | −0.446 | −0.515 | −0.792 | |
| C10 | −0.264 *** | −0.165 ** | −0.729 *** | −1.181 * | −0.014 | −3.343 *** |
| −0.043 | −0.068 | −0.05 | −0.608 | −0.301 | −0.761 | |
| C11 | −0.378 *** | −0.101 ** | −0.359 *** | −0.224 | −0.851 *** | −1.261 ** |
| −0.033 | −0.045 | −0.039 | −0.472 | −0.225 | −0.514 | |
| C12 | 0.214 ** | 0.033 | 0.607 *** | 4.421 *** | 6.999 *** | 0.699 |
| −0.107 | −0.141 | −0.111 | −0.382 | −0.346 | −0.48 | |
| C13 | 0.546 *** | −0.456 *** | −0.425 *** | −0.773 | −0.704 *** | −3.534 *** |
| −0.037 | −0.056 | −0.048 | −0.487 | −0.248 | −1.045 | |
| C14 | −0.366 *** | −0.468 *** | −1.092 *** | −1.366 *** | −2.323 *** | −1.013 ** |
| −0.036 | −0.048 | −0.041 | −0.373 | −0.202 | −0.409 | |
| Constant | −3.303 *** | −3.934 *** | −3.039 *** | −9.268 *** | −8.875 *** | −12.241 *** |
| −0.065 | −0.083 | −0.06 | −0.687 | −0.541 | −1.153 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Recio-Román, A.; Recio-Menéndez, M.; Román-González, M.V. Global Vaccine Hesitancy Segmentation: A Cross-European Approach. Vaccines 2021, 9, 617. https://doi.org/10.3390/vaccines9060617
Recio-Román A, Recio-Menéndez M, Román-González MV. Global Vaccine Hesitancy Segmentation: A Cross-European Approach. Vaccines. 2021; 9(6):617. https://doi.org/10.3390/vaccines9060617
Chicago/Turabian StyleRecio-Román, Almudena, Manuel Recio-Menéndez, and María Victoria Román-González. 2021. "Global Vaccine Hesitancy Segmentation: A Cross-European Approach" Vaccines 9, no. 6: 617. https://doi.org/10.3390/vaccines9060617
APA StyleRecio-Román, A., Recio-Menéndez, M., & Román-González, M. V. (2021). Global Vaccine Hesitancy Segmentation: A Cross-European Approach. Vaccines, 9(6), 617. https://doi.org/10.3390/vaccines9060617






