Hesitancy towards COVID-19 Vaccination among Healthcare Workers: A Multi-Centric Survey in France
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Context, Design, and Population
2.2. Self-Questionnaire
2.3. Scenario of Candidate Vaccines
2.4. Outcomes/Statistical Analysis
3. Results
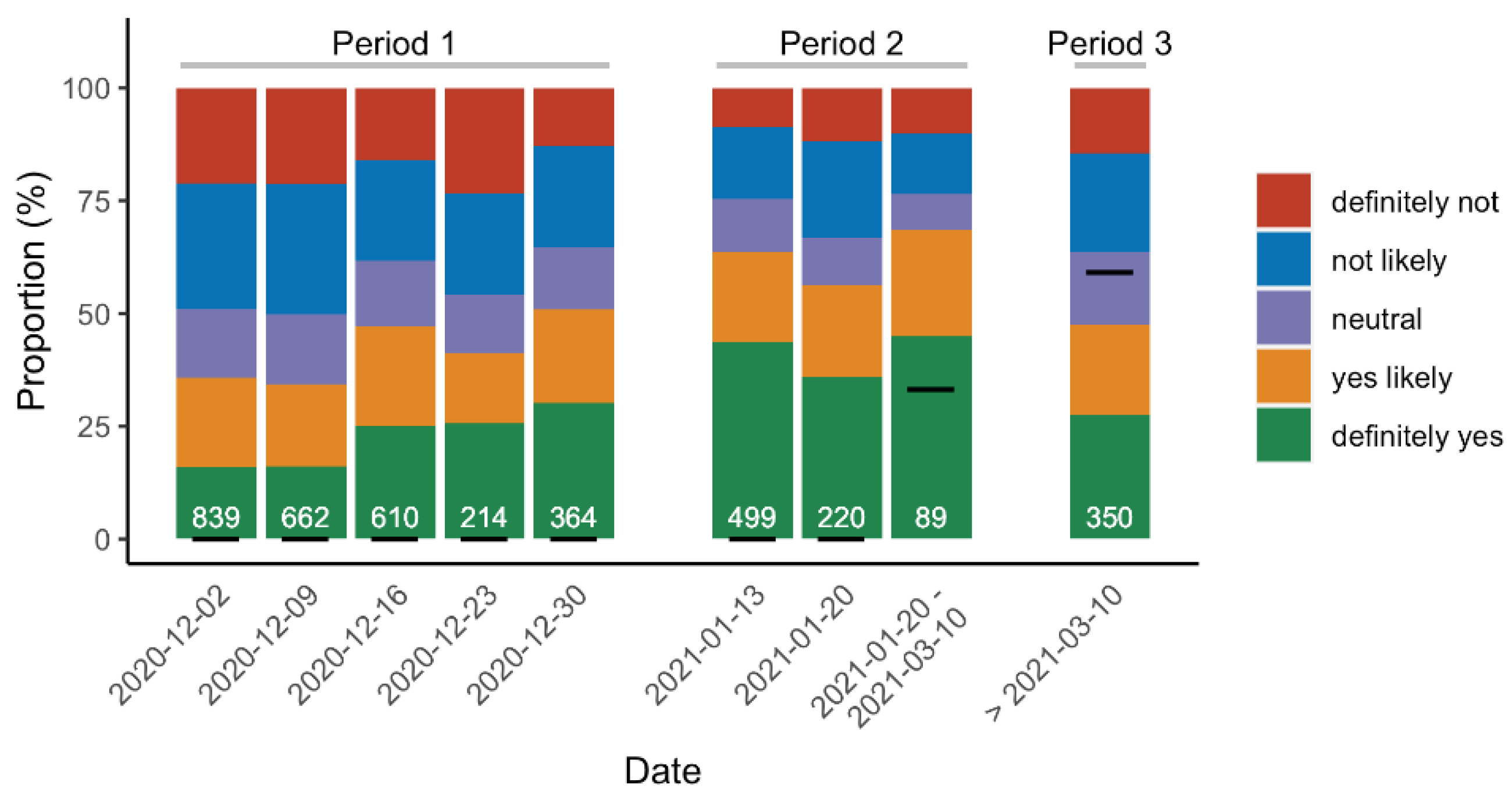
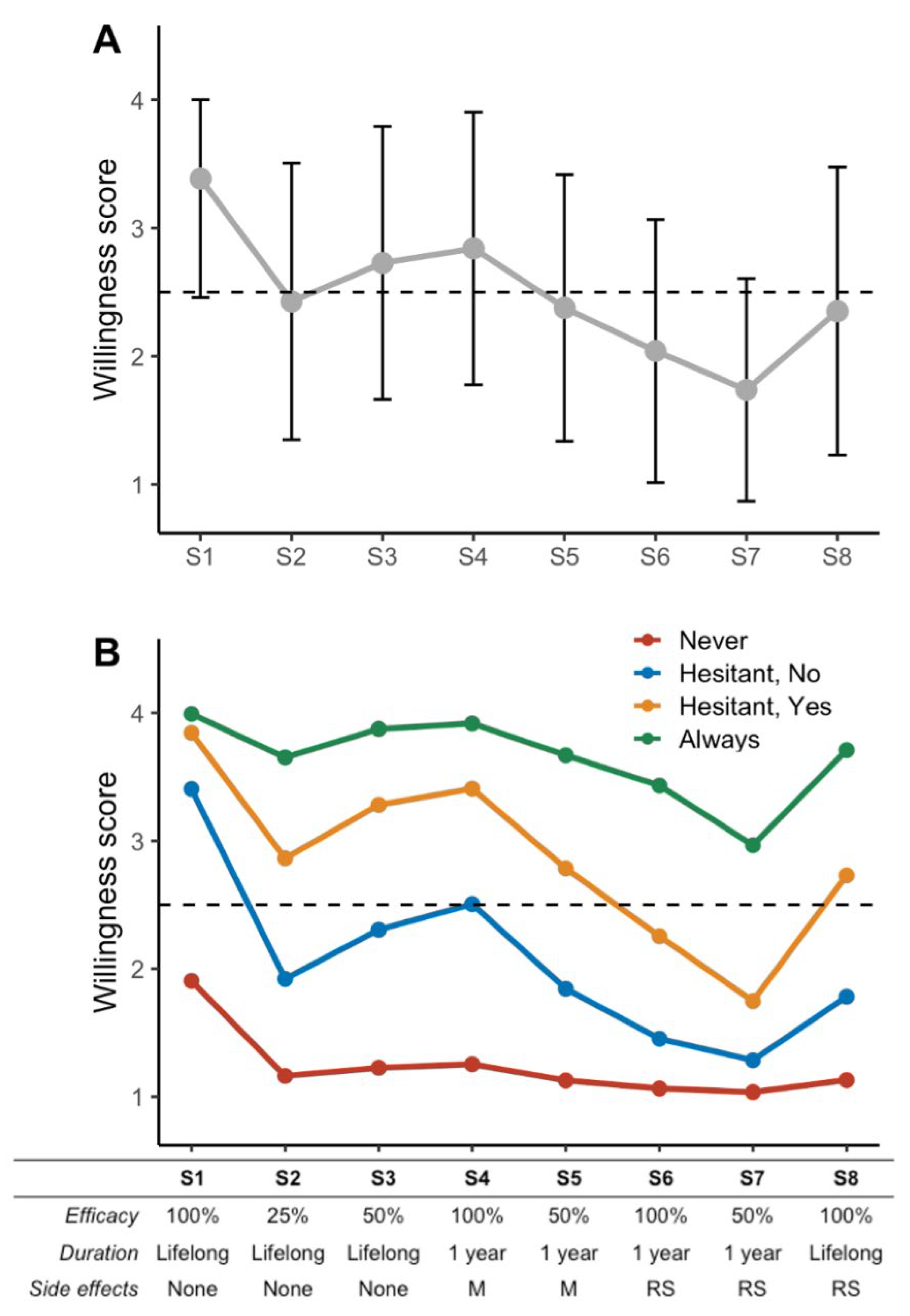
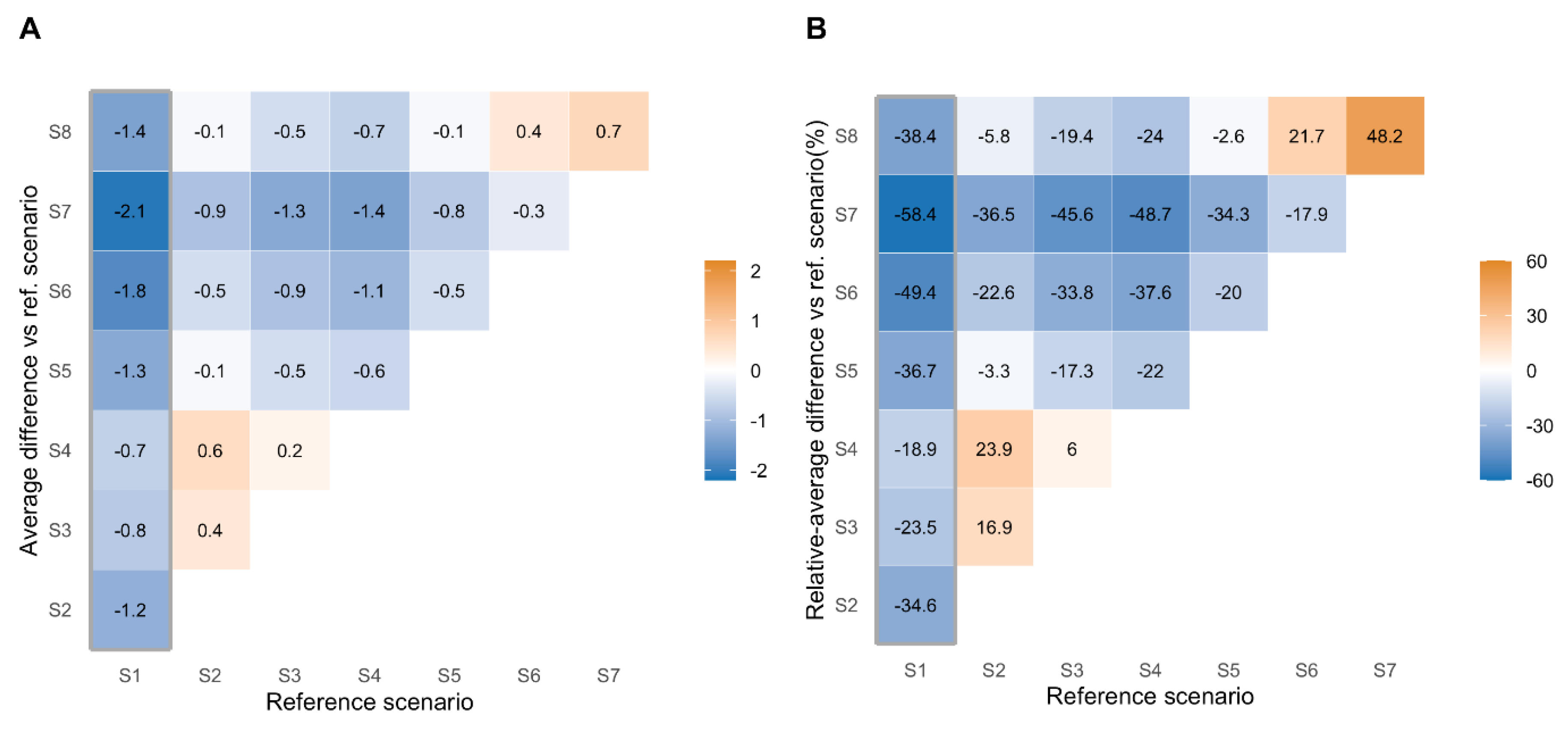
3.1. Scenario and Vaccine Acceptance
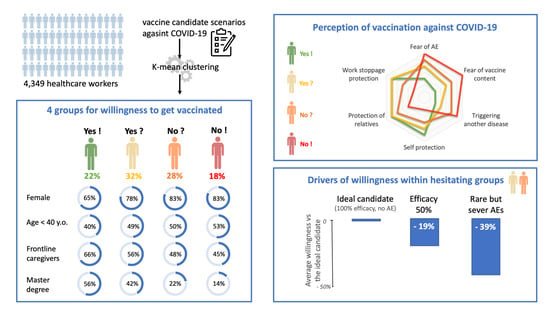
3.2. Cluster Characteristics
3.3. Efficacy, Adverse Events and Length of Immunization Variations on Vaccine Acceptance among Hesitant Healthcare Workers
3.4. Mandatory Vaccination
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Anderson, R.M.; Vegvari, C.; Truscott, J.; Collyer, B.S. Challenges in Creating Herd Immunity to SARS-CoV-2 Infection by Mass Vaccination. Lancet 2020, 396, 1614–1616. [Google Scholar] [CrossRef]
- Shah, A.S.V.; Wood, R.; Gribben, C.; Caldwell, D.; Bishop, J.; Weir, A.; Kennedy, S.; Reid, M.; Smith-Palmer, A.; Goldberg, D.; et al. Risk of Hospital Admission with Coronavirus Disease 2019 in Healthcare Workers and Their Households: Nationwide Linkage Cohort Study. BMJ 2020, 371, m3582. [Google Scholar] [CrossRef] [PubMed]
- Martin, C.; Montesinos, I.; Dauby, N.; Gilles, C.; Dahma, H.; Van Den Wijngaert, S.; De Wit, S.; Delforge, M.; Clumeck, N.; Vandenberg, O. Dynamics of SARS-CoV-2 RT-PCR Positivity and Seroprevalence among High-Risk Healthcare Workers and Hospital Staff. J. Hosp. Infect. 2020, 106, 102–106. [Google Scholar] [CrossRef]
- Haute Autorité de Santé. Stratégie de Vaccination Contre La COVID 19—Anticipation des Scénarios Possibles de Vaccination et Recommandations Préliminaires Sur Les Populations Cibles; Haute Autorité de Santé: Paris, France, 2020. [Google Scholar]
- World Health Organization. WHO SAGE Values Framework for the Allocation and Prioritization of COVID-19 Vaccination|Nitag Resource Center; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Giannattasio, A.; Mariano, M.; Romano, R.; Chiatto, F.; Liguoro, I.; Borgia, G.; Guarino, A.; Lo Vecchio, A. Sustained Low Influenza Vaccination in Health Care Workers after H1N1 Pandemic: A Cross Sectional Study in an Italian Health Care Setting for at-Risk Patients. BMC Infect. Dis. 2015, 15, 329. [Google Scholar] [CrossRef] [PubMed]
- Blasi, F.; Aliberti, S.; Mantero, M.; Centanni, S. Compliance with Anti-H1N1 Vaccine among Healthcare Workers and General Population. Clin. Microbiol Infect. 2012, 18 (Suppl. 5), 37–41. [Google Scholar] [CrossRef]
- Seasonal Influenza Vaccination and Antiviral Use in EU/EEA Member States. Available online: https://www.ecdc.europa.eu/en/publications-data/seasonal-influenza-vaccination-antiviral-use-eu-eea-member-states (accessed on 7 December 2020).
- Sallam, M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines (Basel) 2021, 9, 160. [Google Scholar] [CrossRef]
- Vaux, S.; Fonteneau, L.; Levy-Bruhl, D. Bulletin de Santé Publique Vaccination. Octobre 2019; Santé Publique France: Saint-Maurice, France, 2019; Available online: https://www.santepubliquefrance.fr/determinants-de-sante/vaccination/documents/bulletin-national/bulletin-de-sante-publique-vaccination.-octobre-2019 (accessed on 1 December 2020).
- European Medicines Agency. COVID-19 Vaccine Safety Update, VAXZEVRIA, AstraZeneca AB; European Medicines Agency: Amsterdam, The Netherlands, 2021. [Google Scholar]
- Genolini, C.; Falissard, B. KmL: K-Means for Longitudinal Data. Comput. Stat. 2010, 25, 317–328. [Google Scholar] [CrossRef]
- Verger, P.; Peretti-Watel, P. Understanding the Determinants of Acceptance of COVID-19 Vaccines: A Challenge in a Fast-Moving Situation. Lancet Public Health 2021, 6, e195–e196. [Google Scholar] [CrossRef]
- Hall, V.J.; Foulkes, S.; Saei, A.; Andrews, N.; Oguti, B.; Charlett, A.; Wellington, E.; Stowe, J.; Gillson, N.; Atti, A.; et al. Effectiveness of BNT162b2 MRNA Vaccine Against Infection and COVID-19 Vaccine Coverage in Healthcare Workers in England, Multicentre Prospective Cohort Study (the SIREN Study); Social Science Research Network: Rochester, NY, USA, 2021. [Google Scholar]
- Santé Publique France COVID-19 Vaccination Coverage among Healthcare Worker from France. Available online: https://geodes.santepubliquefrance.fr/#c=indicator&view=map2 (accessed on 26 March 2020).
- Amin, D.P.; Palter, J.S. COVID-19 Vaccination Hesitancy among Healthcare Personnel in the Emergency Department Deserves Continued Attention. Am. J. Emerg. Med. 2021. [Google Scholar] [CrossRef] [PubMed]
- Szmyd, B.; Bartoszek, A.; Karuga, F.F.; Staniecka, K.; Błaszczyk, M.; Radek, M. Medical Students and SARS-CoV-2 Vaccination: Attitude and Behaviors. Vaccines (Basel) 2021, 9, 128. [Google Scholar] [CrossRef]
- Shekhar, R.; Sheikh, A.B.; Upadhyay, S.; Singh, M.; Kottewar, S.; Mir, H.; Barrett, E.; Pal, S. COVID-19 Vaccine Acceptance among Health Care Workers in the United States. Vaccines (Basel) 2021, 9, 119. [Google Scholar] [CrossRef]
- Shaw, J.; Stewart, T.; Anderson, K.B.; Hanley, S.; Thomas, S.J.; Salmon, D.A.; Morley, C. Assessment of U.S. Health Care Personnel (HCP) Attitudes towards COVID-19 Vaccination in a Large University Health Care System. Clin. Infect. Dis. 2021. [Google Scholar] [CrossRef]
- Verger, P.; Scronias, D.; Dauby, N.; Adedzi, K.A.; Gobert, C.; Bergeat, M.; Gagneur, A.; Dubé, E. Attitudes of Healthcare Workers towards COVID-19 Vaccination: A Survey in France and French-Speaking Parts of Belgium and Canada, 2020. Euro. Surveill. 2021, 26. [Google Scholar] [CrossRef]
- Kwok, K.O.; Li, K.-K.; Wei, W.I.; Tang, A.; Wong, S.Y.S.; Lee, S.S. Influenza Vaccine Uptake, COVID-19 Vaccination Intention and Vaccine Hesitancy among Nurses: A Survey. Int. J. Nurs. Stud. 2021, 114, 103854. [Google Scholar] [CrossRef] [PubMed]
- Gagneux-Brunon, A.; Detoc, M.; Bruel, S.; Tardy, B.; Rozaire, O.; Frappe, P.; Botelho-Nevers, E. Intention to Get Vaccinations against COVID-19 in French Healthcare Workers during the First Pandemic Wave: A Cross-Sectional Survey. J. Hosp. Infect. 2021, 108, 168–173. [Google Scholar] [CrossRef]
- Kabamba Nzaji, M.; Kabamba Ngombe, L.; Ngoie Mwamba, G.; Banza Ndala, D.B.; Mbidi Miema, J.; Luhata Lungoyo, C.; Lora Mwimba, B.; Cikomola Mwana Bene, A.; Mukamba Musenga, E. Acceptability of Vaccination Against COVID-19 Among Healthcare Workers in the Democratic Republic of the Congo. Pragmat. Obs. Res. 2020, 11, 103–109. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Wong, E.L.Y.; Ho, K.F.; Cheung, A.W.L.; Chan, E.Y.Y.; Yeoh, E.K.; Wong, S.Y.S. Intention of Nurses to Accept Coronavirus Disease 2019 Vaccination and Change of Intention to Accept Seasonal Influenza Vaccination during the Coronavirus Disease 2019 Pandemic: A Cross-Sectional Survey. Vaccine 2020, 38, 7049–7056. [Google Scholar] [CrossRef] [PubMed]
- Dror, A.A.; Eisenbach, N.; Taiber, S.; Morozov, N.G.; Mizrachi, M.; Zigron, A.; Srouji, S.; Sela, E. Vaccine Hesitancy: The next Challenge in the Fight against COVID-19. Eur. J. Epidemiol. 2020, 35, 775–779. [Google Scholar] [CrossRef]
- Di Gennaro, F.; Murri, R.; Segala, F.V.; Cerruti, L.; Abdulle, A.; Saracino, A.; Bavaro, D.F.; Fantoni, M. Attitudes towards Anti-SARS-CoV2 Vaccination among Healthcare Workers: Results from a National Survey in Italy. Viruses 2021, 13, 371. [Google Scholar] [CrossRef]
- Kuter, B.J.; Browne, S.; Momplaisir, F.M.; Feemster, K.A.; Shen, A.K.; Green-McKenzie, J.; Faig, W.; Offit, P.A. Perspectives on the Receipt of a COVID-19 Vaccine: A Survey of Employees in Two Large Hospitals in Philadelphia. Vaccine 2021, 39, 1693–1700. [Google Scholar] [CrossRef]
- Qattan, A.M.N.; Alshareef, N.; Alsharqi, O.; Al Rahahleh, N.; Chirwa, G.C.; Al-Hanawi, M.K. Acceptability of a COVID-19 Vaccine Among Healthcare Workers in the Kingdom of Saudi Arabia. Front. Med. (Lausanne) 2021, 8. [Google Scholar] [CrossRef]
- Robbins, T.; Berry, L.; Wells, F.; Randeva, H.; Laird, S. Healthcare Staff Perceptions towards Influenza and Potential COVID-19 Vaccination in the 2020 Pandemic Context. J. Hosp. Infect. 2021. [Google Scholar] [CrossRef] [PubMed]
- Goldman, R.D.; Marneni, S.R.; Seiler, M.; Brown, J.C.; Klein, E.J.; Cotanda, C.P.; Gelernter, R.; Yan, T.D.; Hoeffe, J.; Davis, A.L.; et al. Caregivers’ Willingness to Accept Expedited Vaccine Research During the COVID-19 Pandemic: A Cross-Sectional Survey. Clin. Ther. 2020, 42, 2124–2133. [Google Scholar] [CrossRef] [PubMed]
- Papagiannis, D.; Malli, F.; Raptis, D.G.; Papathanasiou, I.V.; Fradelos, E.C.; Daniil, Z.; Rachiotis, G.; Gourgoulianis, K.I. Assessment of Knowledge, Attitudes, and Practices towards New Coronavirus (SARS-CoV-2) of Health Care Professionals in Greece before the Outbreak Period. Int. J. Environ. Res. Public Health 2020, 17, 4925. [Google Scholar] [CrossRef]
- Schrading, W.A.; Trent, S.A.; Paxton, J.H.; Rodriguez, R.M.; Swanson, M.B.; Mohr, N.M.; Talan, D.A. Project COVERED Emergency Department Network Vaccination Rates and Acceptance of SARS-CoV-2 Vaccination among U.S. Emergency Department Health Care Personnel. Acad. Emerg. Med. 2021. [Google Scholar] [CrossRef] [PubMed]
- Qunaibi, E.; Basheti, I.; Soudy, M.; Sultan, I. Hesitancy of Arab Healthcare Workers towards COVID-19 Vaccination: A Large-Scale Multinational Study. Vaccines 2021, 9, 446. [Google Scholar] [CrossRef]
- Nohl, A.; Afflerbach, C.; Lurz, C.; Brune, B.; Ohmann, T.; Weichert, V.; Zeiger, S.; Dudda, M. Acceptance of COVID-19 Vaccination among Front-Line Health Care Workers: A Nationwide Survey of Emergency Medical Services Personnel from Germany. Vaccines (Basel) 2021, 9, 424. [Google Scholar] [CrossRef]
- Kasozi, K.I.; Laudisoit, A.; Osuwat, L.O.; Batiha, G.E.-S.; Al Omairi, N.E.; Aigbogun, E.; Ninsiima, H.I.; Usman, I.M.; DeTora, L.M.; MacLeod, E.T.; et al. A Descriptive-Multivariate Analysis of Community Knowledge, Confidence, and Trust in COVID-19 Clinical Trials among Healthcare Workers in Uganda. Vaccines (Basel) 2021, 9, 253. [Google Scholar] [CrossRef]
- Kukreti, S.; Lu, M.-Y.; Lin, Y.-H.; Strong, C.; Lin, C.-Y.; Ko, N.-Y.; Chen, P.-L.; Ko, W.-C. Willingness of Taiwan’s Healthcare Workers and Outpatients to Vaccinate against COVID-19 during a Period without Community Outbreaks. Vaccines (Basel) 2021, 9, 246. [Google Scholar] [CrossRef]
- Szmyd, B.; Karuga, F.F.; Bartoszek, A.; Staniecka, K.; Siwecka, N.; Bartoszek, A.; Błaszczyk, M.; Radek, M. Attitude and Behaviors towards SARS-CoV-2 Vaccination among Healthcare Workers: A Cross-Sectional Study from Poland. Vaccines (Basel) 2021, 9, 218. [Google Scholar] [CrossRef]
- Papagiannis, D.; Rachiotis, G.; Malli, F.; Papathanasiou, I.V.; Kotsiou, O.; Fradelos, E.C.; Giannakopoulos, K.; Gourgoulianis, K.I. Acceptability of COVID-19 Vaccination among Greek Health Professionals. Vaccines (Basel) 2021, 9, 200. [Google Scholar] [CrossRef]
- Edara, V.V.; Norwood, C.; Floyd, K.; Lai, L.; Davis-Gardner, M.E.; Hudson, W.H.; Mantus, G.; Nyhoff, L.E.; Adelman, M.W.; Fineman, R.; et al. Reduced Binding and Neutralization of Infection- and Vaccine-Induced Antibodies to the B.1.351 (South African) SARS-CoV-2 Variant. bioRxiv 2021. [Google Scholar] [CrossRef]
- Sarah P., O.; Troy, D.; Julien, A.; Caroline, C.; Jonathan, D.; Michael, L.; Samir, M.; Gary, V.D.; Jianhong, W.; Nicolas, H.O. An Evolving Pandemic: The Origins and Potential Future of COVID-19 Variants of Concern. Curr. Biol. Under review.
- Borgey, F.; Henry, L.; Lebeltel, J.; Lescure, P.; Le Coutour, X.; Vabret, A.; Verdon, R.; Thibon, P. Effectiveness of an Intervention Campaign on Influenza Vaccination of Professionals in Nursing Homes: A Cluster-Randomized Controlled Trial. Vaccine 2019, 37, 1260–1265. [Google Scholar] [CrossRef] [PubMed]
- Lanoix, J.-P.; El Samad, Y.; Schmit, J.-L.; Legrain, A.; Joseph, C.; Smail, A.; Douadi, C.; Adjidé, C.; Merlin-Brochart, J.; Couvreur, V. Effect Of Motivational Team On Influenza Vaccination Coverage Among Health Care Workers. Infect. Dis. (Lond.) 2019, 51, 302–304. [Google Scholar] [CrossRef] [PubMed]


| Characteristics | Missing | Never | Hesitating But Not Willing | Hesitating But Willing | Always | Overall | p-Value |
|---|---|---|---|---|---|---|---|
| % | N = 675 | N = 1190 | N = 1050 | N = 817 | N = 4349 | ||
| Age group | 16.7 | <0.001 | |||||
| <25 years | 52 (8.0%) | 69 (6.0%) | 49 (4.8%) | 32 (4.0%) | 202 (5.6%) | ||
| 25–40 years | 338 (52.3%) | 522 (45.4%) | 473 (46.1%) | 342 (42.6%) | 1675 (46.2%) | ||
| 41–50 years | 131 (20.3%) | 317 (27.6%) | 250 (24.4%) | 210 (26.2%) | 908 (25.1%) | ||
| >50 years | 125 (19.3%) | 241 (21.0%) | 254 (24.8%) | 218 (27.2%) | 838 (23.1%) | ||
| Sex, female | 16.7 | 531 (82.2%) | 951 (82.8%) | 800 (78.0%) | 524 (65.3%) | 2806 (77.4%) | <0.001 |
| Educational level | 27.4 | <0.001 | |||||
| High school diploma or less | 67 (13.6%) | 89 (9.2%) | 37 (4.0%) | 16 (2.1%) | 209 (6.6%) | ||
| Bachelor’s degree | 284 (57.6%) | 544 (56.3%) | 407 (43.6%) | 237 (31.0%) | 1472 (46.6%) | ||
| Master or higher | 71 (14.4%) | 216 (22.3%) | 391 (41.9%) | 431 (56.3%) | 1109 (35.1%) | ||
| Other | 71 (14.4%) | 118 (12.2%) | 99 (10.6%) | 81 (10.6%) | 369 (11.7%) | ||
| Professional category † | 16.8 | <0.001 | |||||
| Frontline caregiver | 289 (44.9%) | 551 (48.0%) | 573 (55.8%) | 527 (65.8%) | 1940 (53.6%) | ||
| Other caregiver | 180 (28.0%) | 357 (31.1%) | 301 (29.3%) | 180 (22.5%) | 1018 (28.1%) | ||
| Administrative and non-caregiver staff | 165 (25.7%) | 228 (19.9%) | 145 (14.1%) | 86 (10.7%) | 624 (17.3%) | ||
| Unclassified | 9 (1.4%) | 11 (1.0%) | 7 (0.7%) | 8 (1.0%) | 35 (1.0%) | ||
| Frontline caregivers | |||||||
| Doctors | 16.8 | 9 (1.4%) | 63 (5.5%) | 177 (17.3%) | 273 (34.1%) | 522 (14.4%) | <0.001 |
| Nurses | 16.8 | 127 (19.8%) | 289 (25.2%) | 250 (24.4%) | 155 (19.4%) | 821 (22.7%) | 0.003 |
| Assistant nurse | 16.8 | 130 (20.2%) | 125 (10.9%) | 56 (5.5%) | 18 (2.2%) | 329 (9.1%) | <0.001 |
| Other † | 23 (3.6%) | 74 (6.5%) | 90 (8.8%) | 81 (10.1%) | 268 (7.4%) | <0.001 | |
| Relative income ‡ | 51.1 | 5.9 (SD ± 1.9) | 6.4 (SD ± 1.8) | 6.6 (SD ± 1.8) | 6.8 (SD ± 1.8) | 6.4 (SD ± 1.8) | <0.001 |
| Vaccinated against | |||||||
| Flu | 16.0 | 115 (17.6%) | 491 (42.3%) | 778 (75.3%) | 733 (91.1%) | 2117 (58.0%) | <0.001 |
| Hepatitis B | 16.1 | 531 (81.2%) | 1020 (88.1%) | 955 (92.4%) | 765 (95.1%) | 3271 (89.6%) | <0.001 |
| combined (diphteria/tetanos/polio) | 16.2 | 592 (90.7%) | 1110 (96.1%) | 987 (95.7%) | 758 (94.3%) | 3447 (94.6%) | <0.001 |
| whooping cough | 16.3 | 450 (68.9%) | 881 (76.3%) | 833 (80.9%) | 666 (82.8%) | 2830 (77.7%) | <0.001 |
| COVID-19 exposure | |||||||
| Contact with COVID-19 patients | 6.3 | 531 (78.7%) | 931 (78.2%) | 845 (80.5%) | 675 (82.6%) | 3220 (79.0%) | 0.083 |
| Household member with COVID-19 | 7.2 | 296 (43.9%) | 556 (46.7%) | 479 (45.6%) | 381 (46.6%) | 1849 (45.8%) | 0.643 |
| SARS-CoV-2 infection | 6.7 | 124 (18.4%) | 211 (17.7%) | 198 (18.9%) | 142 (17.4%) | 738 (18.2%) | 0.841 |
| Predisposing conditions to severe COVID-19 Ϫ | 7.3 | 41 (6.1%) | 98 (8.2%) | 107 (10.2%) | 103 (12.6%) | 406 (10.1%) | <0.001 |
| Household member with condition for severe COVID-19 | 8.2 | 145 (21.5%) | 283 (23.8%) | 226 (21.5%) | 167 (20.4%) | 872 (21.8%) | 0.308 |
| Characteristics | Missing | Never | Hesitating But Not Willing | Hesitating But Willing | Always | Overall | p-Value |
|---|---|---|---|---|---|---|---|
| % | N = 675 | N = 1190 | N = 1050 | N = 817 | N = 4349 | ||
| Perceptions and attitude towards vaccination and COVID-19 | |||||||
| Vaccination can induce severe adverse events | 27.3 | 281 (66.1%) | 579 (57.0%) | 363 (37.1%) | 225 (30.3%) | 1448 (45.8%) | <0.001 |
| Vaccine-related adverse events are rare | 31.8 | 135 (20.8%) | 514 (47.2%) | 575 (70.2%) | 327 (80.1%) | 1551 (52.3%) | <0.001 |
| It is not necessary to get vaccinated, as others are vaccinated | 16.2 | 52 (8.1%) | 61 (5.2%) | 17 (1.6%) | 7 (0.9%) | 137 (3.8%) | <0.001 |
| Non-mandatory vaccines are not important | 16.5 | 82 (12.9%) | 122 (10.6%) | 57 (5.5%) | 19 (2.3%) | 280 (7.7%) | <0.001 |
| Pharmaceuticals companies are pushing vaccination in their beneficial interest | 33.2 | 178 (58.7%) | 473 (51.8%) | 360 (39.3%) | 174 (22.5%) | 1185 (40.8%) | <0.001 |
| Pharmaceuticals companies are important in the public health perspective | 40.4 | 220 (48.7%) | 628 (73.5%) | 617 (79.7%) | 417 (81.6%) | 1882 (72.6%) | <0.001 |
| Vaccine are reducing the natural immunity | 17.8 | 174 (30.4%) | 191 (16.6%) | 71 (6.8%) | 13 (1.6%) | 449 (12.6%) | <0.001 |
| Self-vaccination can protect others | 61.0 | 247 (43.6%) | 493 (71.3%) | 273 (79.4%) | 75 (81.5%) | 1088 (64.2%) | <0.001 |
| I am afraid of COVID-19 | 8.3 | 158 (23.4%) | 409 (34.4%) | 383 (36.5%) | 310 (37.9%) | 1325 (33.2%) | <0.001 |
| I am confident in the discovery of effective therapies for COVID-19 | 8.6 | 145 (21.5%) | 479 (40.3%) | 521 (49.6%) | 416 (50.9%) | 1653 (41.6%) | <0.001 |
| Alernative medicine or homeopathy are efficient against COVID-19 | 8.8 | 187 (27.7%) | 165 (13.9%) | 56 (5.3%) | 29 (3.5%) | 474 (11.9%) | <0.001 |
| Mandatory COVID-19 vaccination | |||||||
| COVID-19 vaccination should be mandatory for healthcare workers | 11.5 | 16 (2.4%) | 185 (15.5%) | 416 (39.6%) | 490 (60.0%) | 1138 (29.6%) | <0.001 |
| COVID-19 vaccination should be mandatory for general population | 11.5 | 10 (1.5%) | 138 (11.6%) | 275 (26.2%) | 333 (40.8%) | 787 (20.4%) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Janssen, C.; Maillard, A.; Bodelet, C.; Claudel, A.-L.; Gaillat, J.; Delory, T.; on behalf of the ACV Alpin Study Group. Hesitancy towards COVID-19 Vaccination among Healthcare Workers: A Multi-Centric Survey in France. Vaccines 2021, 9, 547. https://doi.org/10.3390/vaccines9060547
Janssen C, Maillard A, Bodelet C, Claudel A-L, Gaillat J, Delory T, on behalf of the ACV Alpin Study Group. Hesitancy towards COVID-19 Vaccination among Healthcare Workers: A Multi-Centric Survey in France. Vaccines. 2021; 9(6):547. https://doi.org/10.3390/vaccines9060547
Chicago/Turabian StyleJanssen, Cécile, Alexis Maillard, Céline Bodelet, Anne-Laure Claudel, Jacques Gaillat, Tristan Delory, and on behalf of the ACV Alpin Study Group. 2021. "Hesitancy towards COVID-19 Vaccination among Healthcare Workers: A Multi-Centric Survey in France" Vaccines 9, no. 6: 547. https://doi.org/10.3390/vaccines9060547
APA StyleJanssen, C., Maillard, A., Bodelet, C., Claudel, A.-L., Gaillat, J., Delory, T., & on behalf of the ACV Alpin Study Group. (2021). Hesitancy towards COVID-19 Vaccination among Healthcare Workers: A Multi-Centric Survey in France. Vaccines, 9(6), 547. https://doi.org/10.3390/vaccines9060547