Abstract
To control the spread of the novel coronavirus disease 2019 (COVID-19), COVID-19 vaccination has been quickly developed. However, the COVID-19 pandemic will not be controlled if the COVID-19 vaccination uptake willingness is low. Therefore, the study aim was to explore the COVID-19 vaccination uptake willingness among the outpatient population and healthcare workers in Taiwan during the worldwide pandemic period without community outbreaks. A cross-sectional survey was conducted among healthcare workers (HCWs; n = 500; mean age = 32.96 years) of National Cheng Kung University Hospital (NCKUH) and outpatients (n = 238; mean age = 34.43 years) arriving at NCKUH. We used an online survey conducted between September 24 and 21 November 2020, for healthcare workers, and between 27 October and 31 December 2020, for the outpatient sample. Information regarding willingness to receive vaccination, willingness to rapid test, fear of COVID-19, risk perception, and preventive behaviors was collected in both samples; information regarding willingness to care for patients was collected in healthcare workers. Willingness to receive vaccination was the main variable in the present study; willingness to rapid test, willingness to care for patients, fear of COVID-19, risk perception, and preventive behaviors were the secondary variables in the study. The factors associated with vaccination willingness were identified through logistic regression analysis. The participants’ willingness to receive vaccination was low for both healthcare workers (23.4%) and the outpatient sample (30.7%). Similarly, their willingness to take rapid tests was low (23.6% for healthcare workers and 28.6% for outpatient sample). Risk perception (crude odds ratio (COR) = 1.29; 95% confidence interval (CI) = 1.03, 1.63), willingness to take rapid test (COR = 9.24; 95% CI = 5.76, 14.83), and preventive COVID-19 infection behaviors (COR = 2.32; 95% CI = 1.52, 3.56) were significant factors explaining the healthcare workers’ willingness to receive vaccination. Willingness to take a rapid test (COR = 8.91; 95% CI = 4.71, 16.87) and preventive COVID-19 infection behaviors (COR = 1.69; 95% CI = 1.09, 2.60) were significant factors explaining the outpatient sample’s willingness to receive vaccination. Willingness to vaccinate against COVID-19 among HCWs and outpatients is low due to the relatively safe status of COVID-19 infection in Taiwan. These findings can help policymakers advocate for the effectiveness of and provide transparent information on COVID-19 vaccination uptake in a country/region with a relatively safe COVID-19 outbreak status.
1. Introduction
The novel coronavirus disease 2019 (COVID-19) was discovered in late 2019 and resulted the worldwide pandemic [1]. The threat of COVID-19 transmission is ongoing, given several variants that have been identified [2]. The impacts of COVID-19 have far exceeded its high mortality rate [3]: psychological and social health have been largely impacted worldwide due to the direct and indirect effects of COVID-19 [4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20]. The direct impacts include psychological distress and mental health problems, given the fear of COVID-19 [4,5,6,7,8,9]. The indirect impacts may be attributed to the changes in human lifestyles, which have occurred due to some policies implemented to control the spread of COVID-19 infection [10,20,21]. These changed lifestyles (e.g., lack of outdoor activities due to lockdown) may also impair individuals’ mental health [10,11,13,14,15,16,19,22]. Therefore, the entire world is awaiting COVID-19 vaccination to effectively and efficiently control the transmission of COVID-19 infections.
However, prior evidence showed that individuals may be reluctant to receive vaccination due to several reasons, including the 3 Cs model: little confidence in vaccination, high complacency due to perceived low risk of infection, and low convenience of getting vaccinated [23], in addition to economic issues [24,25,26]. Although prior evidence has indicated the benefits of vaccination, especially from the perspective of social protection and the effectiveness in preventing deaths (preventing 2 to 3 million deaths per year) [26], some studies have still reported low levels of willingness to receive COVID-19 vaccination [24,27,28], posing a global challenge for healthcare providers and policy makers to increase and promote COVID-19 vaccination coverage. Without a certain level of COVID-19 vaccination coverage, controlling COVID-19 infections will be difficult. Moreover, as the development of COVID-19 vaccination was accelerated (i.e., over 160 candidate vaccines have been tested with around 20 being under clinical evaluation worldwide) [29,30,31], healthcare providers and policy makers may need to advocate and promote COVID-19 vaccination to achieve a high level of vaccination coverage. Thus, the social protection can be maximized, and the threat of COVID-19 can be minimized.
The issue of COVID-19 vaccination has thus been widely discussed in the current literature in different countries and regions [24,25,26,27,28,30,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50]. From a literature review, we found that most published studies focused on the COVID-19 vaccination willingness in general populations. More specifically, a relatively high rate of COVID-19 vaccination uptake willingness (49.7% to 91.3%) has been observed in the general populations in some Asian countries, including mainland China [35], Malaysia [37], and Indonesia [32]; some Europe countries, including Turkey, France, Italy, the UK, Ireland, Denmark, Germany, Portugal, and the Netherlands [33]; and the U.S. [34,41,50]. Low levels of willingness toward COVID-19 vaccination (27.0% to 29.4%) have been documented in general populations in Nigeria [28] and Arab countries, including Jordan, Kuwait, and Saudi Arabia [27]. Aside from general populations, willingness toward COVID-19 vaccination has been investigated in other populations, including healthcare workers in the Republic of Congo (27.7% were willing to receive vaccination) [24], Hong Kong (40.0% to 63.0% were willing to receive vaccination) [25,46], and the Republic of Malta (61.8% were willing to receive vaccination) [42]. Of medical students in the U.S., 53.0% were willing to receive vaccination [40]. Of parents or guardians in the U.K., 90.1% were willing to receive vaccination [36], and 72.6% in mainland China [49]. Of caregivers in the U.S., Israel, Japan, Spain, and Switzerland, overall, 65.0% were willing to receive vaccination [43].
To the best of our knowledge, no studies have explored COVID-19 vaccination uptake willingness among outpatient populations, and only few studies have investigated the COVID-19 vaccination uptake among healthcare workers [24,25,42,46]. In addition, most of the evidence has been derived from countries/regions with serious COVID-19 outbreaks or those with serious COVID-19 community transmission [25,32,47,50]. To fill this literature gap, we investigated the COVID-19 vaccination willingness in two Taiwanese populations, healthcare workers and outpatients, during the pandemic period but without community transmission in the country. More specifically, the COVID-19 cases were well-controlled by the Taiwan government, with most of the confirmed cases being imported, and COVID-19-related deaths limited to under 10 people [51]. In addition, we explored potential factors that could explain the COVID-19 vaccination uptake willingness in the two samples, separately.
2. Materials and Methods
2.1. Participants and Recruitment Procedure
We adopted a cross-sectional design with convenience sampling. There were two target samples in this study: the National Cheng Kung University Hospital (NCKUH) healthcare workers and the NCKUH outpatients. The NCKUH, with more than 5000 employees and more than 1500 beds, is the largest medical center in Southern Taiwan. We used a cross-sectional design to recruit 500 healthcare workers and 238 NCKUH outpatients who were willing to participate in this study. All the participants were approached using an online survey. Specifically, we sent out the survey link to the NCKUH healthcare workers and outpatients who had provided their email information in the NCKUH IT system. In the link, the study purpose and information (including the right to withdrawal) were clearly mentioned in the first page of the online survey. Only when the participant clicked on the button to agree to participate could they continue the online survey. The inclusion criteria for healthcare workers were (1) a healthcare worker in the NCKUH; (2) aged over 20 years; and (3) willing to participate in the study. The inclusion criteria for outpatients were (1) being a NCKUH outpatient; (2) aged over 20 years; and (3) willing to participate in the study. The survey period for healthcare workers was between 24 September and 21 November 2020; the survey period for the outpatient sample was between 27 October and 31 December 2020. We obtained Institute Review Board (IRB) approval (IRB number A-ER-109-149) from the NCKUH for this study prior to commencement.
The needed sample size for the present study was calculated as follows: For healthcare workers, we referenced a similar study (i.e., a healthcare worker population from Hong Kong [46]) to assume a prevalence rate of 40%, with 5% precision and a population size of 5200 (i.e., about the size of the NCKUH healthcare staff). We calculated an estimated sample size of 345. For outpatients, we referenced a similar study (i.e., a general population from mainland China [35]) to assume a prevalence rate at 83.3%, with 5% precision and a population size of 40,000 (i.e., about the number of NCKUH outpatients in two months). We estimated the sample size as 213. Therefore, we obtained sufficient responses from both healthcare workers (i.e., 500) and outpatients (i.e., 238) to investigate their COVID-19 vaccination uptake willingness.
2.2. Measures
2.2.1. Background Information Sheet
Participants’ characteristics, including age (fill in a number with the unit of year), sex (male or female), and educational level (elementary school or below, junior high, senior high, bachelor’s degree, master’s degree, or Ph.D. degree) were self-reported by the participants.
2.2.2. Willingness to Receive Vaccination
The item, “To what extent you would like to receive vaccination if not considering the price?” with a five-point Likert scale (1 = very unlikely, 2 = unlikely, 3 = neutral, 4 = likely, and 5 = very likely), was used to examine the willingness to receive vaccination. We then converted the item into a dichotomous scale, where original scores 1 to 3 were recoded as low willingness to receive vaccination and original scores 4 and 5 as high willingness.
2.2.3. Willingness to Take Rapid Test
The item, “To what extent you would like to take a rapid COVID-19 infection test if not considering price?” with a five-point Likert scale (1 = very unlikely, 2 = unlikely, 3 = neutral, 4 = likely, and 5 = very likely), was used to examine the willingness to take a rapid test. We then converted the item into a dichotomous scale, where original scores 1 to 3 were recoded as low willingness and original scores 4 and 5 as high willingness to take a rapid test.
2.2.4. Risk Perception
The item, “What is the likelihood that you may be infected by COVID-19?” with a five-point Likert scale (1 = very unlikely, 2 = unlikely, 3 = neutral, 4 = likely, and 5 = very likely), was used to examine the risk perception of the participants.
2.2.5. Fear of COVID-19
The Fear of COVID-19 Scale (FCV-19S) was used to assess fear of COVID-19. The FCV-19S consists of 7 items with a five-point Likert scale (1 = strongly disagree, 2 = disagree, 3 = neither disagree nor agree, 4 = agree, and 5 = strongly agree). The average score of the 7 items was then computed to obtain the level of fear for a participant. A higher score indicates greater fear, and the psychometric properties of the FCV-19S were found to be satisfactory [8].
2.2.6. Preventive COVID-19 Infection Behaviors
Sixteen behaviors related to prevention of being infected by COVID-19 were used to examine the participants’ preventive COVID-19 infection behaviors. The 16 behaviors included those recommended by the World Health Organization (e.g., clean hands thoroughly, use elbow and handkerchief to cover mouth and nose when sneezing) and those listed in the validated Preventive COVID-19 Infection Behaviors Scale [8].
2.2.7. Willingness to Care for Patients
The item, “To what extent you would like to provide healthcare services to patients?” with a 0–10 visual analogue scale, was assessed for healthcare workers, only, and not for the outpatient sample. All the other measures were assessed for both healthcare workers and the outpatient sample.
2.3. Statistical Analysis
Descriptive statistics were first used to examine the participants’ characteristics, including their demographic information and measure scores. Then, univariate logistic regression models were used to examine the crude odds ratios (CORs) regarding how different variables (age, sex, fear of COVID-19, risk perception, willingness to take rapid test, preventive COVID-19 infection behaviors, and willingness to care for patients) explained the participants’ willingness to receive vaccination. Afterward, multivariate logistic regression models were used to examine the adjusted odds ratios (AORs) when the variables were simultaneously entered in the logistic regression models. All the CORs and AORs are presented with a 95% confidence interval (CI). Data retrieved from healthcare workers and the outpatient sample were separated in all the analyses. Willingness to care for patients was only analyzed for healthcare workers. All the statistical analyses were performed using the IBM SPSS 21.0 (IBM Corp., Armonk, NY, USA).
3. Results
The two samples were relatively young. For the sample of healthcare workers, the mean (SD) age was 32.96 (7.99) years; in comparison, the mean age of healthcare workers in the population was 34.8 years. The mean (SD) age was 34.43 (10.02) years for the outpatient sample; in comparison, the mean age of the outpatients in the population was 41.50 years. The proportion of male healthcare workers in the sample was small (40, 8.0%). For comparison, the ratio of men in healthcare workers in the population was 18.0%. For the outpatient sample, there were 79 male respondents (33.2%); in the population, this proportion is 48.8%. The educational level of the present samples was high: more than 80% of the participants had completed higher education. The participants’ willingness to receive vaccination was low (n = 117, 23.4%, for healthcare workers; n = 73, 30.7%, for the outpatient sample); similarly, their willingness to take a rapid test was low (n = 118, 23.6% for healthcare workers; n = 68, 28.6%, for outpatients). Table 1 lists participants’ scores on the survey measures

Table 1.
Participant characteristics.
The logistic regression models showed that risk perception (COR = 1.29; 95% CI = 1.03, 1.63), willingness to take a rapid test (COR = 9.24; 95% CI = 5.76, 14.83), and preventive COVID-19 infection behaviors (COR = 2.32; 95% CI = 1.52, 3.56) were the significant factors explaining the healthcare workers’ willingness to receive vaccination. However, only willingness to take a rapid test (AOR = 9.06; 95% CI = 5.49, 14.94) and preventive COVID-19 infection behaviors (AOR = 1.89; 95% CI = 1.15, 3.10) remained significant in the multivariate logistic model (Table 2). Willingness to take a rapid test (COR = 8.91; 95% CI = 4.71, 16.87) and preventive COVID-19 infection behaviors (COR = 1.69; 95% CI = 1.09, 2.60) were significant factors explaining the outpatient sample’s willingness to receive vaccination. However, only willingness to take a rapid test (AOR = 8.24; 95% CI = 4.24, 16.02) remained significant in the multivariate logistic model (Table 2).

Table 2.
Logistic model examining the predictors on willingness to receive vaccination.
4. Discussion
Through an online survey, with a cross-sectional design, we investigated the willingness toward COVID-19 vaccination uptake in two populations (healthcare workers and outpatients), which has been rarely discussed in the contemporary literature. Both samples reported a low level of willingness to receive COVID-19 vaccination, which may be due to the relatively safe status of COVID-19 infections in Taiwan. More specifically, during the survey period (24 September to 31 December 2020), the COVID-19 cases were controlled to under 800 with most (~88%) of the confirmed cases being imported [51]. Therefore, we postulate that individuals residing in Taiwan may not appreciate the importance of vaccination uptake. This postulation is partially based on the 3 Cs model (confidence, complacency, and convenience) [23]; that is, Taiwan residents might be aware of the low risk of being infected with COVID-19 and, thus, had high levels of complacency. However, we did not collect information regarding whether the COVID-19 infection status was the underlying reason for the low levels of willingness to receive COVID-19 vaccination. Therefore, we summarized the published evidence of the COVID-19 vaccination uptake willingness. Illustrated in Figure 1, high levels of willingness of COVID-19 vaccination uptake can be observed in most countries/regions. Low levels of willingness toward COVID-19 vaccination uptake were observed among healthcare workers in the Republic of the Congo (27.7%), general population in Nigeria (29.0%) [28], and the Arab countries (29.4%) [27], to which we can add our healthcare worker (23.4%) and outpatient (30.7%) samples.
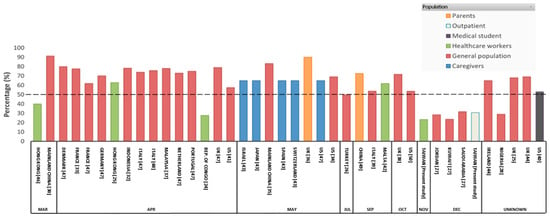
Figure 1.
Willingness to receive COVID-19 vaccination as a percentage. The dashed line indicates 50% willingness to receive vaccination.
A review of the confirmed COVID-19 cases and deaths in the studies [24,25,26,27,28,30,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50] that published information on COVID-19 vaccination uptake willingness somewhat supports our aforementioned postulation. The Republic of the Congo, which had low levels of willingness to receive COVID-19 vaccination in the general population (27.7%) [24], had relatively few confirmed COVID-19 cases (n = 220) and deaths (n = 9). All the other countries/regions with high numbers of COVID-19 cases and deaths reported high levels of COVID-19 vaccination uptake willingness (Table 3), except for the Arab countries [27]. The low levels of COVID-19 vaccination uptake willingness among Arab countries, where the burden of COVID-19 was severe, may be due to the low trust in the government and low levels of education [27]. Additionally, an increased level of willingness has been observed among Hong Kong healthcare workers, ranging from 40.0% to 63.0%, when an outbreak occurred [1,25,46]. This finding also indirectly supports the postulation mentioned above (i.e., the low levels of willingness found in the present study were due to the relatively low status in Taiwan).

Table 3.
Study review showing percentage of COVID-19 vaccination willingness and total cases, deaths, and population during the survey period.
For both samples, the willingness to take a rapid test was the only factor that significantly explained the COVID-19 vaccination uptake willingness in the multivariate logistic regression models. Individuals with higher levels of willingness to take a rapid test may have higher levels of intent to avoid being infected by COVID-19. This finding echoes prior evidence in the relationship between willingness to get influenza vaccinated and diagnostic testing [52]. Therefore, willingness to take a rapid test is a good predictor of COVID-19 vaccination uptake willingness. Preventive COVID-19 infection behaviors were found to be significant factors in both samples in the univariate logistic regression models. This explains that the samples with higher compliance with preventive COVID-19 infection behaviors were likely to accept COVID-19 vaccination if not considering their willingness to take a rapid test. The significant association between preventive COVID-19 infection behaviors and COVID-19 vaccination uptake willingness was lower in outpatients and remained significant in healthcare workers when accounting for willingness to take a rapid test. This implies that the willingness to take rapid test and preventive COVID-19 infection behaviors may share the same underlying reasons explaining COVID-19 vaccination uptake willingness, that is, higher levels of intention to avoid being infected by COVID-19.
There are some limitations to the present study. First, the study samples were recruited using convenience sampling, and the participants were affiliated with the NCKUH (either the hospital staff or hospital outpatients). Therefore, the representativeness of the samples is relatively low, and the generalizability of our findings is somewhat restricted. Following this limitation, the readers should be cautious with the high educational levels and young age of the study’s respondents. Future studies recruiting individuals with low educational levels and older age are thus needed. Second, we adopted a cross-sectional design; thus, causal relationships cannot be drawn. Therefore, future studies using longitudinal designs are warranted to further corroborate the significant association between the rapid test willingness and COVID-19 vaccination uptake willingness found in the present study. Third, some of the variables (e.g., rapid test willingness and COVID-19 vaccination uptake willingness) were not assessed using standardized instruments. Therefore, it is unclear whether there are any measurement biases in assessing these variables.
5. Conclusions
Our findings demonstrated a low level of willingness to receive vaccination among Taiwanese individuals (23.4% of healthcare workers and 30.7% of outpatients). The low willingness may be due to the relatively safe status of COVID-19 in Taiwan, as evidenced by the high levels of willingness to receive vaccination among individuals residing in regions with a high risk of COVID-19 infection. Although several potential factors were found to significantly explain the COVID-19 vaccination uptake willingness, willingness to take a rapid COVID-19 test was the only significant factor in both samples in the controlled logistic regression models. According to the present findings, policy makers may want to advocate for the effectiveness of and provide transparent information on COVID-19 vaccination uptake in countries and regions that are relatively safe from COVID-19 outbreaks. COVID-19 vaccination uptake may start from those who have taken a rapid COVID-19 infection test to achieve initial vaccination coverage.
Author Contributions
Conceptualization, S.K., M.-Y.L., Y.-H.L., C.S., C.-Y.L., N.-Y.K., P.-L.C., and W.-C.K.; methodology, S.K. and C.-Y.L.; software, C.-Y.L.; validation, C.S., N.-Y.K., P.-L.C., and W.-C.K.; formal analysis, C.-Y.L.; investigation, C.S., C.-Y.L., N.-Y.K., P.-L.C., and W.-C.K.; resources, C.S., C.-Y.L., N.-Y.K., P.-L.C., and W.-C.K.; data curation, M.-Y.L. and Y.-H.L.; writing—original draft preparation, S.K. and C.-Y.L.; writing—review and editing, M.-Y.L., Y.-H.L., C.S., C.-Y.L., N.-Y.K., P.-L.C., and W.-C.K.; visualization, S.K.; supervision, N.-Y.K., P.-L.C., and W.-C.K.; project administration, C.S., C.-Y.L., N.-Y.K., P.-L.C., and W.-C.K.; funding acquisition, C.S., C.-Y.L., N.-Y.K., P.-L.C., and W.-C.K. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported in part by a research grant from the Ministry of Science and Technology, Taiwan (MOST109-2327-B-006-005) and in part by a research grant from the Taipei Municipal Wanfang Hospital Cross-Institutions Fund (110-swf-01).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board of National Cheng Kung University Hospital (IRB number A-ER-109-149; date of approval 12 August 2020).
Informed Consent Statement
Online informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data will be available upon reasonable request to the corresponding authors.
Acknowledgments
We thank all the participants.
Conflicts of Interest
The authors declare no conflict of interest.
References
- World Health Organization (WHO). World Health Organization Coronavirus Disease (COVID-19). 2020. Available online: https://covid19.who.int (accessed on 4 March 2021).
- Madabhavi, I.; Sarkar, M.; Kadakol, N. COVID-19: A review. Monaldi Arch. Chest Dis. 2020, 90. [Google Scholar] [CrossRef]
- Weiss, P.; Murdoch, D.R. Clinical course and mortality risk of severe COVID-19. Lancet 2020, 395, 1014–1015. [Google Scholar] [CrossRef]
- Pramukti, I.; Strong, C.; Sitthimongkol, Y.; Setiawan, A.; Pandin, M.G.R.; Yen, C.-F.; Lin, C.-Y.; Griffiths, M.D.; Ko, N.-Y. Anxiety and Suicidal Thoughts During the COVID-19 Pandemic: Cross-Country Comparative Study Among Indonesian, Taiwanese, and Thai University Students. J. Med. Internet Res. 2020, 22, e24487. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.-Y.; Chen, I.-H.; O’Brien, K.S.; Latner, J.D.; Lin, C.-Y. Psychological distress and internet-related behaviors between schoolchildren with and without overweight during the COVID-19 outbreak. Int. J. Obes. 2021, 45, 677–686. [Google Scholar] [CrossRef]
- Fazeli, S.; Zeidi, I.M.; Lin, C.-Y.; Namdar, P.; Griffiths, M.D.; Ahorsu, D.K.; Pakpour, A.H. Depression, anxiety, and stress mediate the associations between internet gaming disorder, insomnia, and quality of life during the COVID-19 outbreak. Addict. Behav. Rep. 2020, 12, 100307. [Google Scholar] [CrossRef]
- Nathiya, D.; Singh, P.; Suman, S.; Raj, P.; Tomar, B.S. Mental health problems and impact on youth minds during the COVID-19 outbreak: Cross-sectional (RED-COVID) survey. Soc. Health Behav. 2020, 3, 83–88. [Google Scholar]
- Chang, K.-C.; Hou, W.-L.; Pakpour, A.H.; Lin, C.-Y.; Griffiths, M.D. Psychometric testing of three COVID-19-related scales among people with mental illness. Int. J. Ment. Health Addict. 2020, 1–13. [Google Scholar] [CrossRef]
- Ahorsu, D.K.; Lin, C.-Y.; Imani, V.; Saffari, M.; Griffiths, M.D.; Pakpour, A.H. The fear of COVID-19 scale: Development and initial validation. Int. J. Ment. Health Addict. 2020, 1–9. [Google Scholar] [CrossRef]
- Chen, I.-H.; Chen, C.-Y.; Pakpour, A.H.; Griffiths, M.D.; Lin, C.-Y. Internet-related behaviors and psychological distress among schoolchildren during COVID-19 school suspension. J. Am. Acad. Child Adolesc. Psychiatry 2020, 59, 1099–1102. [Google Scholar] [CrossRef] [PubMed]
- Shrivastava, S.R.; Shrivastava, P.S. Roping-In religious leaders and faith experts in the effective containment of the coronavirus disease-2019 pandemic. Soc. Health Behav. 2020, 3, 130–131. [Google Scholar] [CrossRef]
- Ahorsu, D.K.; Lin, C.-Y.; Pakpour, A.H. The Association Between Health Status and Insomnia, Mental Health, and Preventive Behaviors: The Mediating Role of Fear of COVID-19. Gerontol. Geriatr. Med. 2020, 6, 2333721420966081. [Google Scholar] [CrossRef] [PubMed]
- Chang, K.-C.; Strong, C.; Pakpour, A.H.; Griffiths, M.D.; Lin, C.-Y. Factors related to preventive COVID-19 infection behaviors among people with mental illness. J. Formos. Med. Assoc. 2020, 119, 1772–1780. [Google Scholar] [CrossRef] [PubMed]
- Lin, M.W.; Cheng, Y. Policy actions to alleviate psychosocial impacts of COVID-19 pandemic: Experiences from Taiwan. Soc. Health Behav. 2020, 3, 72–73. [Google Scholar] [CrossRef]
- Winter, T.; Riordan, B.; Pakpour, A.; Griffiths, M.; Mason, A.; Poulgrain, J.; Damian, S. Evaluation of the English version of the Fear of COVID-19 Scale and its relationship with behavior change and political beliefs. Int. J. Ment. Health Addict. 2020, 1–11. [Google Scholar] [CrossRef]
- Ahorsu, D.K.; Imani, V.; Lin, C.-Y.; Timpka, T.; Broström, A.; Updegraff, J.A.; Årestedt, K.; Griffiths, M.D.; Pakpour, A.H. Associations between fear of COVID-19, mental health, and preventive behaviours across pregnant women and husbands: An actor-partner interdependence modelling. Int. J. Ment. Health Addict. 2020, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Mamun, M.A.; Sakib, N.; Gozal, D.; Bhuiyan, A.I.; Hossain, S.; Bodrud-Doza, M.; Al Mamun, F.; Hosen, I.; Safiq, M.B.; Abdullah, A.H. The COVID-19 pandemic and serious psychological consequences in Bangladesh: A population-based nationwide study. J. Affect. Disord. 2020, 279, 462–472. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.Y.; Imani, V.; Majd, N.R.; Ghasemi, Z.; Griffiths, M.D.; Hamilton, K.; Hagger, M.S.; Pakpour, A.H. Using an integrated social cognition model to predict COVID-19 preventive behaviours. Br. J. Health Psychol. 2020, 25, 981–1005. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.-Y.; Chen, I.-H.; Pakpour, A.H.; Lin, C.-Y.; Griffiths, M.D. Internet-related behaviors and psychological distress among schoolchildren during the COVID-19 school hiatus. Cyberpsychol. Behav. Soc. Netw. 2021. [Google Scholar] [CrossRef]
- Chen, I.-H.; Chen, C.-Y.; Pakpour, A.H.; Griffiths, M.D.; Lin, C.-Y.; Li, X.-D.; Tsang, H.W.H. Problematic internet-related behaviors mediate the associations between levels of internet engagement and distress among schoolchildren during COVID-19 lockdown: A longitudinal structural equation modeling study. J. Behav. Addict. 2021, 1–14. [Google Scholar] [CrossRef]
- European Society for Child and Adolescent Psychiatry. Concerns for the Mental Health of Children and Adolescents during the Coronavirus Pandemic. 2020. Available online: https://www.escap.eu/index/coronavirus-and-mental-health/ (accessed on 4 March 2021).
- Mamun, M.A.; Ullah, I. COVID-19 suicides in Pakistan, dying off not COVID-19 fear but poverty? The forthcoming economic challenges for a developing country. Brain Behav. Immunity 2020, 87, 163–166. [Google Scholar] [CrossRef]
- MacDonald, N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef] [PubMed]
- Kabamba Nzaji, M.; Kabamba Ngombe, L.; Ngoie Mwamba, G.; Banza Ndala, D.B.; Mbidi Miema, J.; Luhata Lungoyo, C.; Lora Mwimba, B.; Cikomola Mwana Bene, A.; Mukamba Musenga, E. Acceptability of Vaccination Against COVID-19 among Healthcare Workers in the Democratic Republic of the Congo. Pragmatic Obs. Res. 2020, 11, 103. [Google Scholar] [CrossRef]
- Kwok, K.O.; Li, K.-K.; Wei, W.I.; Tang, A.; Wong, S.Y.S.; Lee, S.S. Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: A survey. Int. J. Nurs. Stud. 2021, 114, 103854. [Google Scholar] [CrossRef] [PubMed]
- Akarsu, B.; Canbay Özdemir, D.; Ayhan Baser, D.; Aksoy, H.; Fidancı, İ.; Cankurtaran, M. While studies on COVID-19 vaccine is ongoing, the public’s thoughts and attitudes to the future COVID-19 vaccine. Int. J. Clin. Pract. 2020, e13891. [Google Scholar] [CrossRef]
- Sallam, M.; Dababseh, D.; Eid, H.; Al-Mahzoum, K.; Al-Haidar, A.; Taim, D.; Yaseen, A.; Ababneh, N.A.; Bakri, F.G.; Mahafzah, A. High Rates of COVID-19 Vaccine Hesitancy and Its Association with Conspiracy Beliefs: A Study in Jordan and Kuwait among Other Arab Countries. Vaccines 2021, 9, 42. [Google Scholar] [CrossRef] [PubMed]
- Reuben, R.C.; Danladi, M.M.; Saleh, D.A.; Ejembi, P.E. Knowledge, attitudes and practices towards COVID-19: An epidemiological survey in North-Central Nigeria. J. Community Health 2020, 1–14. [Google Scholar] [CrossRef]
- Lurie, N.; Saville, M.; Hatchett, R.; Halton, J. Developing Covid-19 vaccines at pandemic speed. N. Engl. J. Med. 2020, 382, 1969–1973. [Google Scholar] [CrossRef]
- Wang, J.; Jing, R.; Lai, X.; Zhang, H.; Lyu, Y.; Knoll, M.D.; Fang, H. Acceptance of COVID-19 Vaccination during the COVID-19 Pandemic in China. Vaccines 2020, 8, 482. [Google Scholar] [CrossRef]
- World Health Organization (WHO). World Health Organization DRAFT Landscape of COVID-19 Candidate Vaccines—14 July 2020. Available online: https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines (accessed on 14 July 2020).
- Harapan, H.; Wagner, A.L.; Yufika, A.; Winardi, W.; Anwar, S.; Gan, A.K.; Setiawan, A.M.; Rajamoorthy, Y.; Sofyan, H.; Vo, T.Q. Willingness-to-pay for a COVID-19 vaccine and its associated determinants in Indonesia. Hum. Vaccines Immunother. 2020, 16, 3074–3080. [Google Scholar] [CrossRef]
- Detoc, M.; Bruel, S.; Frappe, P.; Tardy, B.; Botelho-Nevers, E.; Gagneux-Brunon, A. Intention to participate in a COVID-19 vaccine clinical trial and to receive vaccination against COVID-19 in France during the pandemic. Vaccine 2020, 38, 7002–7006. [Google Scholar] [CrossRef]
- Reiter, P.L.; Pennell, M.L.; Katz, M.L. Acceptability of a COVID-19 vaccine among adults in the United States: How many people would receive vaccination? Vaccine 2020, 38, 6500–6507. [Google Scholar] [CrossRef]
- Lin, Y.; Hu, Z.; Zhao, Q.; Alias, H.; Danaee, M.; Wong, L.P. Understanding COVID-19 vaccine demand and hesitancy: A nationwide online survey in China. PLoS Negl. Trop. Dis. 2020, 14, e0008961. [Google Scholar] [CrossRef]
- Bell, S.; Clarke, R.; Mounier-Jack, S.; Walker, J.L.; Paterson, P. Parents’ and guardians’ views on the acceptability of a future COVID-19 vaccine: A multi-methods study in England. Vaccine 2020, 38, 7789–7798. [Google Scholar] [CrossRef]
- Wong, L.P.; Alias, H.; Wong, P.-F.; Lee, H.Y.; AbuBakar, S. The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Hum. Vaccines Immunother. 2020, 16, 2204–2214. [Google Scholar] [CrossRef] [PubMed]
- Freeman, D.; Loe, B.S.; Chadwick, A.; Vaccari, C.; Waite, F.; Rosebrock, L.; Jenner, L.; Petit, A.; Lewandowsky, S.; Vanderslott, S. COVID-19 vaccine hesitancy in the UK: The Oxford coronavirus explanations, attitudes, and narratives survey (Oceans) II. Psychol. Med. 2020, 1–15. [Google Scholar] [CrossRef]
- La Vecchia, C.; Negri, E.; Alicandro, G.; Scarpino, V. Attitudes towards influenza vaccine and a potential COVID-19 vaccine in Italy and differences across occupational groups. La Med. Del. Lav. 2020, 111, 445–448. [Google Scholar] [CrossRef]
- Lucia, V.C.; Kelekar, A.; Afonso, N.M. COVID-19 vaccine hesitancy among medical students. J. Public Health 2020. [Google Scholar] [CrossRef] [PubMed]
- Fisher, K.A.; Bloomstone, S.J.; Walder, J.; Crawford, S.; Fouayzi, H.; Mazor, K.M. Attitudes toward a potential SARS-CoV-2 vaccine: A survey of US adults. Ann. Intern. Med. 2020, 173, 964–973. [Google Scholar] [CrossRef] [PubMed]
- Grech, V.; Bonnici, J.; Zammit, D. Vaccine hesitancy in Maltese family physicians and their trainees vis-a-vis influenza and novel COVID-19 vaccination. Early Hum. Dev. 2020, 105259. [Google Scholar] [CrossRef]
- Goldman, R.D.; Yan, T.D.; Seiler, M.; Cotanda, C.P.; Brown, J.C.; Klein, E.J.; Hoeffe, J.; Gelernter, R.; Hall, J.E.; Davis, A.L. Caregiver willingness to vaccinate their children against COVID-19: Cross sectional survey. Vaccine 2020, 38, 7668–7673. [Google Scholar] [CrossRef] [PubMed]
- Murphy, J.; Vallières, F.; Bentall, R.P.; Shevlin, M.; McBride, O.; Hartman, T.K.; McKay, R.; Bennett, K.; Mason, L.; Gibson-Miller, J. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat. Commun. 2021, 12, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Pogue, K.; Jensen, J.L.; Stancil, C.K.; Ferguson, D.G.; Hughes, S.J.; Mello, E.J.; Burgess, R.; Berges, B.K.; Quaye, A.; Poole, B.D. Influences on attitudes regarding potential COVID-19 vaccination in the United States. Vaccines 2020, 8, 582. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Wong, E.L.Y.; Ho, K.F.; Cheung, A.W.L.; Chan, E.Y.Y.; Yeoh, E.K.; Wong, S.Y.S. Intention of nurses to accept coronavirus disease 2019 vaccination and change of intention to accept seasonal influenza vaccination during the coronavirus disease 2019 pandemic: A cross-sectional survey. Vaccine 2020, 38, 7049–7056. [Google Scholar] [CrossRef] [PubMed]
- Neumann-Böhme, S.; Varghese, N.E.; Sabat, I.; Barros, P.P.; Brouwer, W.; van Exel, J.; Schreyögg, J.; Stargardt, T. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur. J. Health Econ. 2020, 21, 977–982. [Google Scholar] [CrossRef] [PubMed]
- Prati, G. Intention to receive a vaccine against SARS-CoV-2 in Italy and its association with trust, worry and beliefs about the origin of the virus. Health Educ. Res. 2020, 35, 505–511. [Google Scholar] [CrossRef] [PubMed]
- Zhang, K.C.; Fang, Y.; Cao, H.; Chen, H.; Hu, T.; Chen, Y.Q.; Zhou, X.; Wang, Z. Parental Acceptability of COVID-19 Vaccination for Children Under the Age of 18 Years: Cross-Sectional Online Survey. JMIR Pediatr. Parent. 2020, 3, e24827. [Google Scholar] [CrossRef] [PubMed]
- Daly, M.; Robinson, E. Willingness to vaccinate against COVID-19 in the US: Longitudinal evidence from a nationally representative sample of adults from April-October 2020. medRxiv 2020. [Google Scholar] [CrossRef]
- Taiwan Centers for Disease Control. Coronavirus Disease 2019 (COVID-19). 2021. Available online: https://www.cdc.gov.tw/en/Disease/SubIndex/ (accessed on 26 January 2021).
- Tubiana, S.; Launay, O.; Galtier, F.; Tattevin, P.; Postil, D.; Vanhems, P.; Lenzi, N.; Verger, P.; Duval, X. Attitudes, knowledge, and willingness to be vaccinated against seasonal influenza among patients hospitalized with influenza-like-illness: Impact of diagnostic testing. Hum. Vaccines Immunother. 2020, 16, 851–857. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).