COVID-19 Vaccine Acceptance among Health Care Workers in the United States
Abstract
1. Introduction
2. Methods
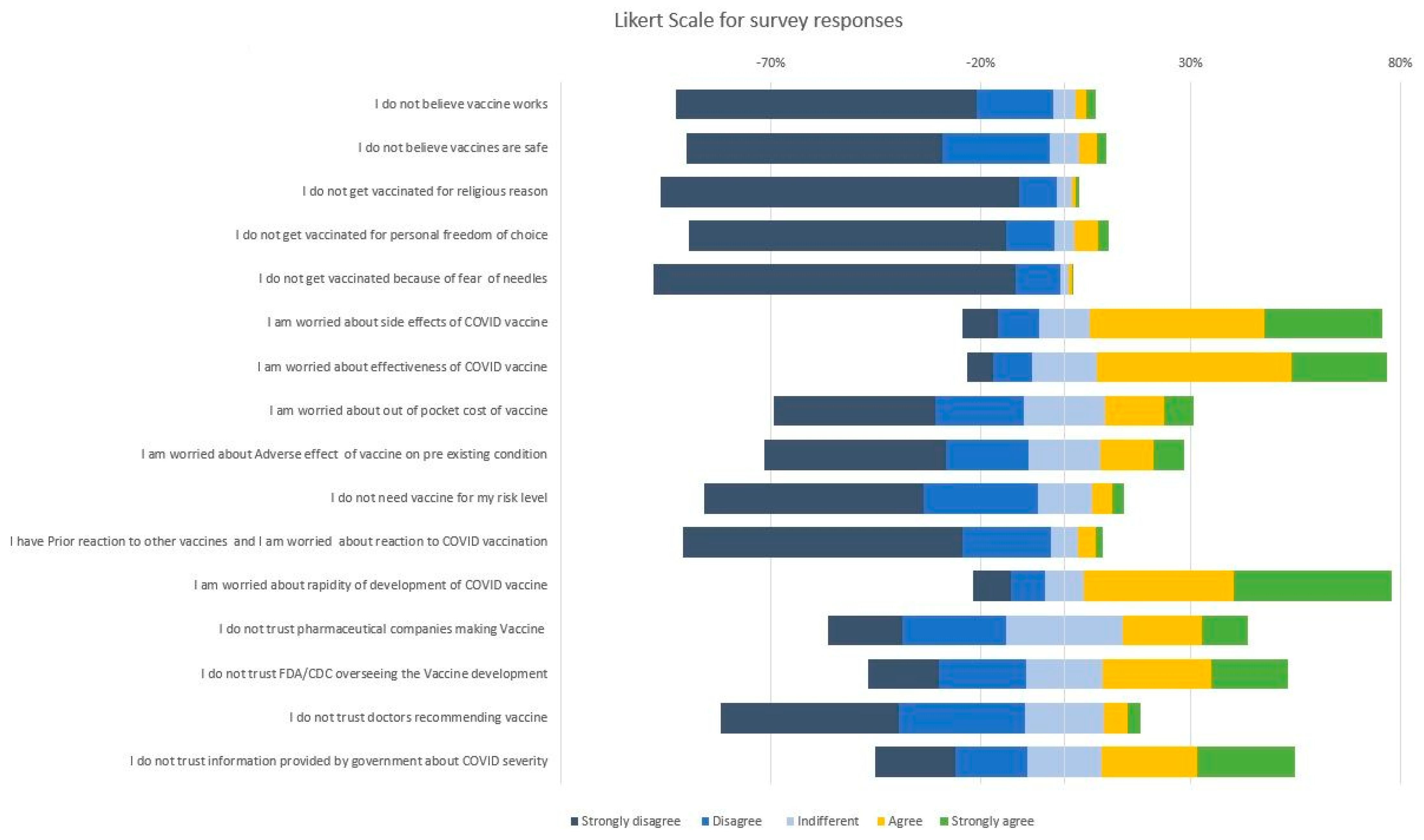
3. Measures
4. Outcome
5. Results
6. Discussion
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Johns Hopkins Coronavirus Resource Center. Global Map. Available online: https://coronavirus.jhu.edu/map.html (accessed on 6 October 2020).
- Adaptive Phase IB-II Randomized Clinical Trial of Preventive Vaccine Consisting of Autologous Dendritic Cells Loaded with Antigens from Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2), with or without GM-CSF, in Subjects Negative for COVID-19 Infection and Anti-SARS-CoV-2 Antibodies. ClinicalTrials.gov identifier (NCT number): NCT04386252. Available online: https://clinicaltrials.gov/ct2/show/NCT04386252 (accessed on 11 December 2020).
- A Randomized, Double-blind, Placebo-controlled Phase 3 Study to Assess the Efficacy and Safety of Ad26.COV2.S for the Prevention of SARS-CoV-2-mediated COVID-19 in Adults Aged 18 Years and Older. ClinicalTrials.gov Identifier: NCT04505722. Available online: https://clinicaltrials.gov/ct2/show/NCT04505722 (accessed on 11 December 2020).
- A Phase 2a, Randomized, Observer-Blind, Placebo Controlled, Dose-Confirmation Study to Evaluate the Safety, Reactogenicity, and Immunogenicity of mRNA-1273 SARS-COV-2 Vaccine in Adults Aged 18 Years and Older. ClinicalTrials.gov Identifier: NCT04405076. Available online: https://clinicaltrials.gov/ct2/show/NCT04405076 (accessed on 11 December 2020).
- A Phase 1/Phase 2, Randomized, Double-Blind, Placebo-Controlled, Dose-Ranging Trial to Evaluate the Safety, Tolerability and Immunogenicity of V591 (COVID-19 Vaccine) in Healthy Younger and Older Participants. ClinicalTrials.gov Identifier: NCT04498247. Available online: https://www.clinicaltrials.gov/ct2/show/NCT04498247 (accessed on 11 December 2020).
- Phadke, V.K.; Bednarczyk, R.A.; Salmon, D.A.; Omer, S.B. Association between Vaccine Refusal and Vaccine-Preventable Diseases in the United States. JAMA 2016, 315, 1149–1158. [Google Scholar] [CrossRef]
- Fisher, K.A.; Bloomstone, S.J.; Walder, J.; Crawford, S.L.; Fouayzi, H.; Mazor, K.M. Attitudes Toward a Potential SARS-CoV-2 Vaccine. Ann. Intern. Med. 2020, 173, 964–973. [Google Scholar] [CrossRef]
- Wheeler, M.; Buttenheim, A.M. Parental vaccine concerns, information source, and choice of alternative immunization schedules. Hum. Vaccines Immunother. 2013, 9, 1782–1789. [Google Scholar] [CrossRef]
- Salmon, D.A.; Moulton, L.H.; Omer, S.B.; Dehart, M.P.; Stokley, S.; Halsey, N.A. Factors Associated with Refusal of Childhood Vaccines among Parents of School-aged Children. Arch. Pediatr. Adolesc. Med. 2005, 159, 470–476. [Google Scholar] [CrossRef]
- Omer, S.B.; Salmon, D.A.; Orenstein, W.A.; Dehart, M.P.; Halsey, N. Vaccine Refusal, Mandatory Immunization, and the Risks of Vaccine-Preventable Diseases. N. Engl. J. Med. 2009, 360, 1981–1988. [Google Scholar] [CrossRef]
- Likert, R. A technique for the measurement of attitudes. Arch. Psychol. 1932, 22, 55. [Google Scholar]
- Malik, A.A.; McFadden, S.M.; Elharake, J.; Omer, S.B. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine 2020, 26, 100495. [Google Scholar] [CrossRef]
- Pogue, K.; Jensen, J.L.; Stancil, C.K.; Ferguson, D.G.; Hughes, S.J.; Mello, E.J.; Burgess, R.; Berges, B.K.; Quaye, A.; Poole, B.D. Influences on Attitudes Regarding Potential COVID-19 Vaccination in the United States. Vaccines 2020, 8, 582. [Google Scholar] [CrossRef]
- Fontanet, A.; Cauchemez, S. COVID-19 herd immunity: Where are we? Nat. Rev. Immunol. 2020, 20, 583–584. [Google Scholar] [CrossRef]
- Lemaitre, M.; Meret, T.; Rothan-Tondeur, M.; Belmin, J.; Lejonc, J.-L.; Luquel, L.; Piette, F.; Salom, M.; Verny, M.; Vetel, J.-M.; et al. Effect of Influenza Vaccination of Nursing Home Staff on Mortality of Residents: A Cluster-Randomized Trial. J. Am. Geriatr. Soc. 2009, 57, 1580–1586. [Google Scholar] [CrossRef]
- Zaffina, S.; Gilardi, F.; Rizzo, C.; Sannino, S.; Brugaletta, R.; Santoro, A.; Gattinara, G.C.; Degli Atti, M.L.C.; Raponi, M.; Vinci, M.R. Seasonal influenza vaccination and absenteeism in health-care workers in two subsequent influenza seasons (2016/17 and 2017/18) in an Italian pediatric hospital. Expert Rev. Vaccines 2019, 18, 411–418. [Google Scholar] [CrossRef] [PubMed]
- Murti, M.; Otterstatter, M.C.; Orth, A.; Balshaw, R.; Halani, K.; Brown, P.D.; Hejazi, S.; Thompson, D.; Allison, S.; Bharmal, A.; et al. Measuring the impact of influenza vaccination on healthcare worker absenteeism in the context of a province-wide mandatory vaccinate-or-mask policy. Vaccine 2019, 37, 4001–4007. [Google Scholar] [CrossRef]
- Imai, C.; Toizumi, M.; Hall, L.; Lambert, S.; Halton, K.; Merollini, K. A systematic review and meta-analysis of the direct epidemiological and economic effects of seasonal influenza vaccination on healthcare workers. PLoS ONE 2018, 13, e0198685. [Google Scholar] [CrossRef]
- Paterson, P.; Meurice, F.; Stanberry, L.R.; Glismann, S.; Rosenthal, S.L.; Larson, H.J. Vaccine hesitancy and healthcare providers. Vaccine 2016, 34, 6700–6706. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; While, A.; Norman, I.J. Nurses’ knowledge and risk perception towards seasonal influenza and vaccination and their vaccination behaviours: A cross-sectional survey. Int. J. Nurs. Stud. 2011, 48, 1281–1289. [Google Scholar] [CrossRef] [PubMed]
- LaVela, S.L.; Smith, B.; Weaver, F.M.; Legro, M.W.; Goldstein, B.; Nichol, K. Attitudes and Practices Regarding Influenza Vaccination among Healthcare Workers Providing Services to Individuals with Spinal Cord Injuries and Disorders. Infect. Control. Hosp. Epidemiol. 2004, 25, 933–940. [Google Scholar] [CrossRef] [PubMed]
- Detoc, M.; Bruel, S.; Frappe, P.; Tardy, B.; Botelho-Nevers, E.; Gagneux-Brunon, A. Intention to participate in a COVID-19 vaccine clinical trial and to get vaccinated against COVID-19 in France during the pandemic. Vaccine 2020, 38, 7002–7006. [Google Scholar] [CrossRef]
- Tse, S.C.; Wyatt, L.C.; Trinh-Shevrin, C.; Kwon, S.C. Racial/Ethnic Differences in Influenza and Pneumococcal Vaccination Rates among Older Adults in New York City and Los Angeles and Orange Counties. Prev. Chronic Dis. 2018, 15. [Google Scholar] [CrossRef]
- Quinn, S.C.; Jamison, A.M.; Freimuth, V.S.; An, J.; Hancock, G.R. Determinants of influenza vaccination among high-risk Black and White adults. Vaccine 2017, 35, 7154–7159. [Google Scholar] [CrossRef]
- Hooper, M.W.; Nápoles, A.M.; Pérez-Stable, E.J. COVID-19 and racial/ethnic disparities. JAMA 2020, 323, 2466–2467. [Google Scholar] [CrossRef]
- Dubé, E.; Leask, J.; Wolff, B.; Hickler, B.; Balaban, V.; Hosein, E.; Habersaat, K.B. The WHO Tailoring Immunization Programmes (TIP) approach: Review of implementation to date. Vaccine 2018, 36, 1509–1515. [Google Scholar] [CrossRef] [PubMed]
- Reiter, P.L.; Pennell, M.L.; Katz, M.L. Acceptability of a COVID-19 vaccine among adults in the United States: How many people would get vaccinated? Vaccine 2020, 38, 6500–6507. [Google Scholar] [CrossRef] [PubMed]
- Romer, D.; Jamieson, K.H. Conspiracy theories as barriers to controlling the spread of COVID-19 in the U.S. Soc. Sci. Med. 2020, 263, 113356. [Google Scholar] [CrossRef]
- Aguilar-Díaz, F.D.C.; Jimenez-Corona, M.-E.; Ponce-De-Leon-Rosales, S. Influenza Vaccine and Healthcare Workers. Arch. Med. Res. 2011, 42, 652–657. [Google Scholar] [CrossRef]
- Kwok, K.O.; Li, K.K.; Wei, W.I.; Tang, A.; Wong, S.Y.S.; Lee, S.S. Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: A survey. Int. J. Nurs. Stud. 2021, 114, 103854. [Google Scholar] [CrossRef]
| Variable | N = 3479 1 |
|---|---|
| Age | |
| 18–30 years | 816 (23%) |
| 31–40 years | 1061 (30%) |
| 41–50 years | 686 (20%) |
| 51–60 years | 571 (16%) |
| 61–70 years | 326 (9.4%) |
| >70 years | 19 (0.5%) |
| Gender | |
| Female | 2598 (75%) |
| Male | 864 (25%) |
| Trans/ Gender non-binary/not specified above | 7 (0.2%) |
| Do not wish to reply | 10 (0.3%) |
| Ethnicity | |
| Hispanic or Latino | 560 (16%) |
| NOT Hispanic or Latino | 2763 (79%) |
| Unknown/Not Reported | 36 (1.0%) |
| Do not wish to answer | 120 (3.4%) |
| Race | |
| White or Caucasian | 2803 (81%) |
| Asian | 218 (6.3%) |
| Black or African American | 74 (2.1%) |
| Native Americans/Alaska Native | 30 (0.9%) |
| Native Hawaiian or Other Pacific Islander | 6 (0.2%) |
| More Than One Race | 126 (3.6%) |
| Unknown/Other | 70 (2.0%) |
| Do not wish to answer | 152 (4.4%) |
| State of Residence | |
| Midwest | 1433 (41%) |
| North East | 81 (2.3%) |
| South | 314 (9.0%) |
| West | 1651 (47%) |
| Occupation | |
| Direct Patient Care Providers (DPCP) | 1573 (45%) |
| Direct Medical Providers (DMP) | 1207 (35%) |
| Administrative staff working in hospital without direct patient contact | 295 (8.5%) |
| Others without direct patient contact | 404 (12%) |
| Primary Area of Work | |
| Primary medical and medical subspecialty | 1882 (54%) |
| Primary surgical and surgical subspecialty | 363 (10%) |
| Diagnostic subspecialty | 246 (7.1%) |
| Others | 988 (28%) |
| Annual Income | |
| <$30,000 | 117 (3.4%) |
| $30,001–$70,000 | 741 (21%) |
| $70,001–$100,00 | 759 (22%) |
| $100,001–$150,000 | 796 (23%) |
| >$150,001 | 1066 (31%) |
| Health Care facility in | |
| Rural area | 293 (8.4%) |
| Suburban area | 957 (28%) |
| Urban area | 2229 (64%) |
| Education | |
| No formal education | 1 (<0.1%) |
| High school graduate, diploma or the equivalent (for example: GED) | 46 (1.3%) |
| Some college credit, no degree | 169 (4.9%) |
| Trade/technical/vocational training | 111 (3.2%) |
| Associate degree | 364 (10%) |
| Bachelor’s degree | 1046 (30%) |
| Master’s degree | 606 (17%) |
| Professional degree | 297 (8.5%) |
| Doctorate degree | 839 (24%) |
| Political Identification | |
| Conservative-Republican | 746 (21%) |
| Democrat-Liberal | 1519 (44%) |
| Unaffiliated | 640 (18%) |
| Do not wish to answer | 574 (16%) |
| Medical comorbidities | |
| No Chronic Condition | 2039 (59%) |
| Diabetes Mellitus Type-1/Type-2 | 136 (3.9%) |
| Heart Disease | 36 (1.0%) |
| Hypertension | 449 (13%) |
| COPD Asthma—Lung Disease | 318 (9.1%) |
| Obesity BMI > 30 | 461 (13%) |
| Cancer | 125 (3.6%) |
| Immuno-compromised/on immunosuppressants | 110 (3.2%) |
| Smoking | 288 (8.3%) |
| Other Medical Conditions | 505 (15%) |
| Have you, your family member or someone you know been diagnosed with COVID-19 (Excluding your patients) | |
| I was Diagnosed with COVID-19 | 90 (2.6%) |
| Family Member was Diagnosed with COVID-19 | 447 (13%) |
| Someone I personally know was Diagnosed with COVID-19 | 1793 (52%) |
| No one I personally know was Diagnosed with COVID-19 | 1400 (40%) |
| Do you think you are at risk of getting COVID-19 in the next 1 year? | |
| I believe I already have the disease and I am immune to it (Not diagnosed by a test) | 138 (4.0%) |
| No, I am confident I won’t get infected | 266 (7.6%) |
| No, I already have recovered and won’t get re-infected (Diagnosed by a test) | 34 (1.0%) |
| Yes, I am concerned that I will get mild symptoms which will probably not require hospitalization | 2294 (66%) |
| Yes, I am concerned that I will get moderate symptoms which will probably need hospitalization | 572 (16%) |
| Yes, I am concerned that I will get severe symptom which will probably require admission to the Intensive care unit | 175 (5.0%) |
| Have you directly or indirectly taken care of the COVID-19 patients? | |
| No | 1263 (36%) |
| Yes, but no direct patient contact | 646 (19%) |
| Yes, I have direct patient contact | 1570 (45%) |
| Would you take the COVID-19 Vaccine | |
| No | 279 (8.0%) |
| Wait for Review | 1953 (56%) |
| Yes | 1247 (36%) |
| Would you advise friends and family to get vaccinated for COVID-19? | |
| No | 519 (15%) |
| Not sure | 1376 (40%) |
| Yes | 1584 (46%) |
| COVID-19 Vaccine for health care workers should be: | |
| Mandated by the employer, like Influenza vaccine | 792 (23%) |
| Mandated by the Federal government for all health care workers | 338 (9.7%) |
| Mandated by the State government for all health care workers | 99 (2.8%) |
| Not sure | 585 (17%) |
| Voluntary | 1665 (48%) |
| Variable | No, n = 279 1 | Wait for Review, n = 1953 1 | Yes, n = 1247 1 | p-Value 2 |
|---|---|---|---|---|
| Age | <0.001 * | |||
| 18–30 years | 72 (8.8%) | 467 (57%) | 277 (34%) | |
| 31–40 years | 83 (7.8%) | 615 (58%) | 363 (34%) | |
| 41–50 years | 70 (10%) | 389 (57%) | 227 (33%) | |
| 51–60 years | 43 (7.5%) | 306 (54%) | 222 (39%) | |
| 61–70 years | 10 (3.1%) | 167 (51%) | 149 (46%) | |
| >70 years | 1 (5.3%) | 9 (47%) | 9 (47%) | |
| Gender | <0.001 * | |||
| Female | 240 (9.2%) | 1540 (59%) | 818 (31%) | |
| Male | 37 (4.3%) | 402 (47%) | 425 (49%) | |
| Trans/Gender non-binary/not specified above | 0 (0%) | 4 (57%) | 3 (43%) | |
| Do not wish to reply | 2 (20%) | 7 (70%) | 1 (10%) | |
| Ethnicity | <0.001 * | |||
| Hispanic or Latino | 55 (9.8%) | 337 (60%) | 168 (30%) | |
| NOT Hispanic or Latino | 191 (6.9%) | 1536 (56%) | 1036 (37%) | |
| Unknown/Not Reported | 8 (22%) | 16 (44%) | 12 (33%) | |
| Do not wish to answer | 25 (21%) | 64 (53%) | 31 (26%) | |
| Race | <0.001 * | |||
| White or Caucasian | 221 (7.9%) | 1545 (55%) | 1037 (37%) | |
| Asian | 1 (0.5%) | 122 (56%) | 95 (44%) | |
| Black or African American | 12 (16%) | 48 (65%) | 14 (19%) | |
| Native Americans/Alaska Native | 3 (10%) | 24 (80%) | 3 (10%) | |
| Native Hawaiian or Other Pacific Islander | 0 (0%) | 6 (100%) | 0 (0%) | |
| More Than One Race | 4 (3.2%) | 82 (65%) | 40 (32%) | |
| Unknown/Other | 9 (13%) | 41 (59%) | 20 (29%) | |
| Do not wish to answer | 29 (19%) | 85 (56%) | 38 (25%) | |
| State of Residence | 0.003 * | |||
| Midwest | 146 (10%) | 776 (54%) | 511 (36%) | |
| North East | 2 (2.5%) | 45 (56%) | 34 (42%) | |
| South | 11 (3.5%) | 151 (48%) | 152 (48%) | |
| West | 120 (7.3%) | 981 (59%) | 550 (33%) | |
| Occupation | <0.001 * | |||
| Direct patient care providers (DPCP) | 187 (12%) | 969 (62%) | 417 (27%) | |
| Direct Medical Provider (DMP) | 30 (2.5%) | 582 (48%) | 595 (49%) | |
| Administrative staff working in hospital without direct patient contact | 25 (8.5%) | 170 (58%) | 100 (34%) | |
| Others without direct patient contact | 37 (9.2%) | 232 (57%) | 135 (33%) | |
| Annual Income | <0.001 * | |||
| <$30,000 | 19 (16%) | 53 (45%) | 45 (38%) | |
| $30,001–$70,000 | 81 (11%) | 420 (57%) | 240 (32%) | |
| $70,001–$100,00 | 80 (11%) | 463 (61%) | 216 (28%) | |
| $100,001–$150,000 | 60 (7.5%) | 472 (59%) | 264 (33%) | |
| >$150,001 | 39 (3.7%) | 545 (51%) | 482 (45%) | |
| Health Care facility in | <0.001 * | |||
| Rural area | 52 (18%) | 164 (56%) | 77 (26%) | |
| Suburban area | 98 (10%) | 523 (55%) | 336 (35%) | |
| Urban area | 129 (5.8%) | 1266 (57%) | 834 (37%) | |
| Education | <0.001 * | |||
| No formal education | 0 (0%) | 1 (100%) | 0 (0%) | |
| High school graduate, diploma, or the equivalent (for example: GED) | 9 (20%) | 26 (57%) | 11 (24%) | |
| Some college credit, no degree | 24 (14%) | 94 (56%) | 51 (30%) | |
| Trade/technical/vocational training | 18 (16%) | 69 (62%) | 24 (22%) | |
| Associate degree | 56 (15%) | 220 (60%) | 88 (24%) | |
| Bachelor’s degree | 109 (10%) | 627 (60%) | 310 (30%) | |
| Master’s degree | 40 (6.6%) | 362 (60%) | 204 (34%) | |
| Professional degree | 6 (2.0%) | 139 (47%) | 152 (51%) | |
| Doctorate degree | 17 (2.0%) | 415 (49%) | 407 (49%) | |
| Political Identification | <0.001 * | |||
| Conservative-Republican | 93 (12%) | 390 (52%) | 263 (35%) | |
| Democrat-Liberal | 42 (2.8%) | 833 (55%) | 644 (42%) | |
| Unaffiliated | 48 (7.5%) | 373 (58%) | 219 (34%) | |
| Do not wish to answer | 96 (17%) | 357 (62%) | 121 (21%) | |
| Did you get the Influenza vaccine Last Year? | <0.001 * | |||
| No | 50 (43%) | 56 (48%) | 10 (8.6%) | |
| Yes | 229 (6.8%) | 1897 (56%) | 1237 (37%) | |
| If you have Children under 18 years old, Have they been vaccinated for other diseases | <0.001 * | |||
| No | 38 (26%) | 67 (46%) | 41 (28%) | |
| Not Applicable | 120 (6.0%) | 1132 (56%) | 754 (38%) | |
| Yes | 121 (9.1%) | 754 (57%) | 452 (34%) | |
| Medical Condition = Chronic Condition | 0.046 | |||
| No | 107 (7.4%) | 819 (57%) | 514 (36%) | |
| Yes | 172 (8.4%) | 1134 (56%) | 733 (36%) | |
| Diabetes Mellitus Type-1/Type-2 | 0.076 | |||
| No | 272 (8.1%) | 1876 (56%) | 1195 (36%) | |
| Yes | 7 (5.1%) | 77 (57%) | 52 (38%) | |
| Heart Disease | 0.067 | |||
| No | 276 (8.0%) | 1935 (56%) | 1232 (36%) | |
| Yes | 3 (8.3%) | 18 (50%) | 15 (42%) | |
| Hypertension | 0.8 | |||
| No | 253 (8.3%) | 1701 (56%) | 1076 (36%) | |
| Yes | 26 (5.8%) | 252 (56%) | 171 (38%) | |
| COPD Asthma—Lung Disease | 0.701 | |||
| No | 258 (8.2%) | 1778 (56%) | 1125 (36%) | |
| Yes | 21 (6.6%) | 175 (55%) | 122 (38%) | |
| Obesity BMI>30 | 0.022 * | |||
| No | 250 (8.3%) | 1671 (55%) | 1097 (36%) | |
| Yes | 29 (6.3%) | 282 (61%) | 150 (33%) | |
| Cancer | 0.399 | |||
| No | 274 (8.2%) | 1882 (56%) | 1198 (36%) | |
| Yes | 5 (4.0%) | 71 (57%) | 49 (39%) | |
| Immuno-compromised/on immunosuppressants | 0.354 | |||
| No | 269 (8.0%) | 1889 (56%) | 1211 (36%) | |
| Yes | 10 (9.1%) | 64 (58%) | 36 (33%) | |
| Smoking | 0.013 * | |||
| No | 262 (8.2%) | 1778 (56%) | 1151 (36%) | |
| Yes | 17 (5.9%) | 175 (61%) | 96 (33%) | |
| Other Medical Conditions | 0.629 | |||
| No | 227 (7.6%) | 1663 (56%) | 1084 (36%) | |
| Yes | 52 (10%) | 290 (57%) | 163 (32%) | |
| I was Diagnosed with COVID-19 | 0.009 * | |||
| No | 272 (8.0%) | 1901 (56%) | 1216 (36%) | |
| Yes | 7 (7.8%) | 52 (58%) | 31 (34%) | |
| Family Member was Diagnosed with COVID-19 | 0.695 | |||
| No | 244 (8.0%) | 1712 (56%) | 1076 (35%) | |
| Yes | 35 (7.8%) | 241 (54%) | 171 (38%) | |
| Someone I personally know was Diagnosed with COVID-19 | 0.003 * | |||
| No | 168 (10.0%) | 924 (55%) | 594 (35%) | |
| Yes | 111 (6.2%) | 1029 (57%) | 653 (36%) | |
| No one I personally know was Diagnosed with COVID-19 | 0.143 | |||
| No | 134 (6.4%) | 1181 (57%) | 764 (37%) | |
| Yes | 145 (10%) | 772 (55%) | 483 (34%) | |
| Do you think you are at risk of getting COVID-19 in next 1 year? | <0.001 * | |||
| I believe I already have the disease and I am immune to it (Not diagnosed by a test) | 30 (22%) | 68 (49%) | 40 (29%) | |
| No, I am confident I won’t get infected | 71 (27%) | 128 (48%) | 67 (25%) | |
| No, I already have recovered and won’t get re-infected (Diagnosed by a test) | 4 (12%) | 18 (53%) | 12 (35%) | |
| Yes, I am concerned that I will get mild symptoms which will probably not require hospitalization | 153 (6.7%) | 1283 (56%) | 858 (37%) | |
| Yes, I am concerned that I will get moderate symptoms which will probably need hospitalization | 15 (2.6%) | 350 (61%) | 207 (36%) | |
| Yes, I am concerned that I will get severe symptom which will probably require admission to the Intensive care unit | 6 (3.4%) | 106 (61%) | 63 (36%) | |
| Have you directly or indirectly taken care of the COVID-19 patients? | <0.001 * | |||
| No | 116 (9.2%) | 714 (57%) | 433 (34%) | |
| Yes, but no direct patient contact | 45 (7.0%) | 358 (55%) | 243 (38%) | |
| Yes, I have direct patient contact | 118 (7.5%) | 881 (56%) | 571 (36%) | |
| I would get the vaccine to prevent COVID-19 in myself | <0.001 * | |||
| No | 277 (20%) | 816 (58%) | 324 (23%) | |
| Yes | 2 (<0.1%) | 1137 (55%) | 923 (45%) | |
| I would get the vaccine to prevent COVID-19 in friends and family members | <0.001 * | |||
| No | 276 (21%) | 723 (56%) | 286 (22%) | |
| Yes | 3 (0.1%) | 1230 (56%) | 961 (44%) | |
| I would get the vaccine to prevent COVID-19 in community | <0.001 * | |||
| No | 277 (26%) | 560 (52%) | 237 (22%) | |
| Yes | 2 (<0.1%) | 1393 (58%) | 1010 (42%) | |
| I would not get the vaccine | <0.001 * | |||
| No | 3 (<0.1%) | 1787 (59%) | 1235 (41%) | |
| Yes | 276 (61%) | 166 (37%) | 12 (2.6%) | |
| Would you advise friends and family to get vaccinated for COVID-19? | <0.001 * | |||
| No | 230 (44%) | 272 (52%) | 17 (3.3%) | |
| Not sure | 49 (3.6%) | 1162 (84%) | 165 (12%) | |
| Yes | 0 (0%) | 519 (33%) | 1065 (67%) | |
| COVID-19 Vaccine for health care workers should be: | <0.001 * | |||
| Mandated by the employer, like Influenza vaccine | 0 (0%) | 245 (31%) | 547 (69%) | |
| Mandated by the Federal government for all health care workers | 0 (0%) | 90 (27%) | 248 (73%) | |
| Mandated by the State government for all health care workers | 0 (0%) | 33 (33%) | 66 (67%) | |
| Not sure | 5 (0.9%) | 457 (78%) | 123 (21%) | |
| Voluntary | 274 (16%) | 1128 (68%) | 263 (16%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shekhar, R.; Sheikh, A.B.; Upadhyay, S.; Singh, M.; Kottewar, S.; Mir, H.; Barrett, E.; Pal, S. COVID-19 Vaccine Acceptance among Health Care Workers in the United States. Vaccines 2021, 9, 119. https://doi.org/10.3390/vaccines9020119
Shekhar R, Sheikh AB, Upadhyay S, Singh M, Kottewar S, Mir H, Barrett E, Pal S. COVID-19 Vaccine Acceptance among Health Care Workers in the United States. Vaccines. 2021; 9(2):119. https://doi.org/10.3390/vaccines9020119
Chicago/Turabian StyleShekhar, Rahul, Abu Baker Sheikh, Shubhra Upadhyay, Mriganka Singh, Saket Kottewar, Hamza Mir, Eileen Barrett, and Suman Pal. 2021. "COVID-19 Vaccine Acceptance among Health Care Workers in the United States" Vaccines 9, no. 2: 119. https://doi.org/10.3390/vaccines9020119
APA StyleShekhar, R., Sheikh, A. B., Upadhyay, S., Singh, M., Kottewar, S., Mir, H., Barrett, E., & Pal, S. (2021). COVID-19 Vaccine Acceptance among Health Care Workers in the United States. Vaccines, 9(2), 119. https://doi.org/10.3390/vaccines9020119








