Abstract
We aimed to estimate the prevalence and factors associated with parents’ non-intention to vaccinate their children and adolescents against COVID-19 in Latin America and the Caribbean (LAC). We performed a secondary analysis using a database generated by the University of Maryland and Facebook (Facebook, Inc., Menlo Park, CA, USA). We included adult (18 and over) Facebook users residing in LAC who responded to the survey between 20 May 2021 and 14 July 2021. We included sociodemographic characteristics, comorbidities, mental health, economic and food insecurity, compliance with mitigation strategies against COVID-19, and practices related to vaccination against this disease. We estimated the crude (cPR) and adjusted (aPR) prevalence ratios with their respective 95%CI. We analyzed a sample of 227,740 adults from 20 LAC countries. The prevalence of parents’ non-intention to vaccinate their children and adolescents against COVID-19 was 7.8% (n = 15,196). An age above 35 years old, educational level above college, compliance with physical distancing, use of masks, having economic insecurity, having had COVID-19, anxiety symptoms, depressive symptoms, having a chronic condition or two or more comorbidities, and being vaccinated were associated with a lower prevalence of non-intention to vaccinate children and adolescents against COVID-19. Living in a town, a village, or a rural area was associated with a higher prevalence of non-intention to vaccinate children and adolescents against COVID-19. Approximately nine out of ten parents in LAC intended to vaccinate their children and adolescents against COVID-19. Our results allow for understanding parents’ intentions to vaccinate children and adolescents and help promote and develop education strategies for national vaccination plans against COVID-19.
Keywords:
COVID-19; SARS-CoV-2; COVID-19 vaccines; vaccination refusal; vaccination; child; adolescent; parents; Latin America 1. Introduction
As of 1 November 2021, more than 246 million confirmed cases of COVID-19 had been reported worldwide with more than 5 million deaths [1]. As for many other infectious diseases, immunization is the most effective public health strategy against the SARS-COV-2 pandemic. It is necessary to reach at least 70% of the population to control this disease [2]. To date, more than 7 billion doses have been administered globally [1].
Given the reticence of vaccination among adults [3,4,5] and other access barriers, it will be necessary to expand vaccination coverage by adding other populations such as children and adolescents, who may constitute a reservoir of the virus and maintain transmission [6]. Although COVID-19 affects children to a lesser extent and severity than adults [2,7], it is known that when community transmission increases, additional deaths occur in children and adolescents [8]. In this regard, clinical trials are currently testing the safety and efficacy of COVID-19 vaccines in adolescents [9]. With the endorsement of some ongoing trials for children [10], some regulatory agencies such as the European Medicines Agency (EMA) and the Food and Drug Administration (FDA) have approved emergency use in adolescents between 12 and 15 years of age, as well other national agencies [11,12]. In this sense, some countries have already started vaccination against COVID-19 in adolescents and considered including children in their schedules [2,13].
Among the multiple barriers to achieve access to vaccination, vaccine reluctance is one of the most complex phenomena and is considered by the WHO as a threat to global health [14]. As in the case of vaccination in adults, parents fear adverse events and have doubts regarding the need to vaccinate their children and adolescents against COVID-19. Nevertheless, previous studies report an intention to vaccinate against COVID-19 in children of between 60% and 70% [15,16,17,18,19]. Various factors related to acceptance of the vaccine in children and adolescents have been described, such as the age of the children, having chronic diseases, having complied with the other vaccines of the immunization schedule, recent vaccination against influenza and if the parents showed concern that their child had COVID-19 and confidence in the vaccine and health institutions, among other factors [15,16,17,18,19,20,21,22].
Latin America is one of the regions most affected by the pandemic. Studies show that LAC countries, although implementing strict control measures against COVID-19 and gradually increasing the capacity of their health systems, experienced many cases and deaths, which in some cases were much higher than the official figures reported [23,24]. This was because pre-pandemic conditions in their health systems and social determinants [21,22] undermined the effectiveness of their responses. Likewise, there was no comprehensive strategy for testing, monitoring and tracking the cases, which contributed to the fact that the spread of the virus was not adequately contained [23,24]. Similarly, economic support measures were implemented late for most countries [23,24].
Likewise, there are problems in the availability of vaccines, which means that in July 2021, some countries only had vaccines available for 3% of their populations [25]. Despite being a global phenomenon, the factors associated with vaccine reticence vary according to the context and characteristics of the population group evaluated [26,27]. Therefore, regional studies involving different populations are necessary to generate specific campaigns [20]. Taking this into account, and given the need to better understand the phenomena related to the acceptance of the vaccine in various population groups in our context, the objective of this study was to estimate the prevalence and factors associated with parents’ non-intention to vaccinate their children and adolescents against COVID-19 in Latin America and the Caribbean (LAC).
2. Materials and Methods
2.1. Study Design
We performed a secondary analysis using a database generated by the University of Maryland and Facebook (Facebook, Inc., Menlo Park, CA, USA). Both institutions designed a survey to assess sociodemographic characteristics, comorbidities, mental health, economic and food insecurity, compliance with mitigation strategies against COVID-19 and practices related to vaccination against this disease. The survey has been carried out daily since 23 April 2020 in more than 200 countries and in the primary language of the territory. The proportion of Facebook users who are ineligible to participate in the survey due to language and geographic restrictions is less than 5% globally (people for whom it is not possible to ensure that the entire communication from invitation to the study survey is in the user’s language). The surveys are daily repeated cross-sections, including participants that are Facebook users with similar characteristics across each day. The sampling frame for the random selection of participants included the total of Facebook users over 18 years of age from a particular region and country daily. Stratified random sampling using the administrative boundaries within countries or territories is conducted to provide geographic coverage. The selection of the surveyed participants was random based on the sampling frame, which was recalculated daily. If a Facebook user refused to participate, another was randomly invited within the sampling frame. The participants could only answer the survey once within an 8-week time frame. This survey has been used to develop previous studies [22], and the survey methodology has been previously described in greater detail [28]. We have attached in Supplementary Materials the questionnaire used.
2.2. Population and Sample
We included adult (18 and over) Facebook users residing in LAC who responded to the survey between 20 May 2021 and 14 July 2021. We excluded participants who did not have the variables of interest, did not have children, were of non-binary gender and were over 54 years of age. We excluded participants over 54 years of age to reduce the probability of not exclusively including parents of children under 18. Thus, we analyzed 227,740 adults from LAC (Figure 1).
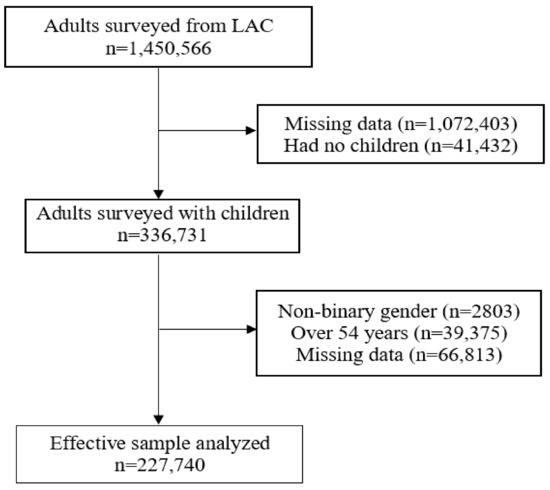
Figure 1.
Flowchart of the selection of the study sample.
2.3. Variables and Measures
2.3.1. Outcome Variable: Parents’ Non-Intention to Vaccinate Their Children and Adolescents against COVID-19
We evaluated the parents’ intention to vaccinate their children and adolescents against COVID-19 using the following survey question: Will you choose to get a COVID-19 vaccine for your child or children when they are eligible? This question had four possible alternatives: yes, definitely; yes, probably; no, probably not; and no, definitely not. Subsequently, we dichotomized the variable considering the first two alternatives for the parents’ intention to vaccinate their children and adolescents, while the last two were considered non-intention.
2.3.2. Independent Variables
Sociodemographic Variables: We included the following sociodemographic variables (in parenthesis is the described the survey question related to the study variables and the categories considered for these variables in the study): gender (What is your gender: male or female?); age (What is your age: 18–24, 25–34, 35–44 or 45–54 years?); educational level (What is the highest level of education that you have completed: university post-graduate degree completed, university completed, college or pre-university; secondary school or high school (or equivalent) completed; primary school completed, less than primary school or no formal schooling?); and area of residence (Which of these best describes the area where you are currently staying: city, town, village or rural area?). We defined a town as a populated area with fixed boundaries and a local self-government, a city as an important or large town and a village as a group of houses and other buildings—usually in the countryside—that is smaller than a town.
Comorbidities, Personal, and COVID-19 History: The participants self-reported the following comorbidities (survey question: Have you ever been told by a doctor, nurse or other health professional that you have any of the following medical conditions?): asthma, chronic obstructive pulmonary disease (COPD) or chronic bronchitis or emphysema, cancer, diabetes, high blood pressure, kidney disease, a compromised or weakened immune system, heart attack or another heart disease and obesity. We generated a variable that grouped the comorbidities as 0, 1, 2, or more. We also included self-reporting of being a smoker (yes or no), having had COVID-19 (yes or no) and having been vaccinated against COVID-19 (yes or no).
Compliance with Community Mitigation Strategies: The community mitigation strategies included were physical distancing and a mask during the last 7 days. We defined physical distancing as a participant reported having intentionally avoided contact with other people at some point in the last 7 days (survey question: In the past 7 days, how often did you intentionally avoid contact with other people?). In addition, the use of masks was defined as whether a participant reported wearing a mask in public at some point during the last 7 days (survey question: In the past 7 days, how often did you wear a mask when in public?).
Food and Economic Insecurity: We assessed food insecurity with the following survey question: How worried are you about having enough to eat in the next week? This question had 4 possible answers: very worried, somewhat worried, not too worried and not worried at all. We considered the first three responses as food insecurity.
We defined economic insecurity using the following survey question: How worried are you about your household’s finances in the next month? It had 4 possible responses: very worried, somewhat worried, not too worried and not worried at all. We defined economic insecurity using the first three responses.
Anxiety and Depressive Symptoms: We evaluated anxiety symptoms using the survey question: During the last 7 days, how often did you feel so nervous that nothing could calm you down? This question is part of the Kessler Psychological Distress Scale (K10), and the survey had 5 possible responses: all the time, most of the time, some of the time, a little of the time and none of the time. Therefore, we dichotomized the variable by considering the first 3 alternatives as the presence of anxiety symptoms.
We evaluated depressive symptoms using the following survey question: How often did you feel so depressed that nothing could cheer you up in the past 7 days? This question is part of the Kessler Psychological Distress Scale (K10), and they survey had 5 possible responses: all the time, most of the time, some of the time, a little of the time and none of the time. Therefore, we dichotomized the variable by considering the first 4 alternatives as the presence of depressive symptoms.
2.4. Statistical Analysis
We downloaded the databases in Microsoft Excel 2016® format and imported them into the statistical package Stata/SE ® version 17.0 (StataCorp, College Station, TX, USA). Then, we performed the statistical analysis while considering the complex sampling of the survey and the svy command.
We utilized weighted proportions with their respective 95% confidence intervals (95%CI) and absolute frequencies to present the qualitative variables. We used the Chi-square test with Rao-Scott correction to perform the bivariate analysis between the independent variables and the parents’ non-intention to vaccinate their children and adolescents against COVID-19. We used two generalized linear models (crude and adjusted) of the Poisson family with a logarithmic link function to estimate the factors associated with the parents’ non-intention to vaccinate their children and adolescents against COVID-19. We estimated the crude (cPR) and adjusted (aPR) prevalence ratios with a 95%CI. We elaborated a crude model and an adjusted statistical model (we included the variables with a p value < 0.05 in the crude model). We evaluated the possible collinearity of the associated factors included in the final adjusted model.
2.5. Ethical Considerations
The participants who responded to the survey provided informed consent. This study analyzed a secondary database that collected data without identifiers and did not violate the integrity of the participants. Access to the database was given with permission from the University of Maryland.
3. Results
3.1. Characteristics of the Study Sample
We analyzed a sample of 227,740 adults from 20 LAC countries between 20 May and 14 July 2021. We found that 55.0% (n = 140,355) were female, 33.8% (n = 86,869) were between 35 and 44 years, 47.3% (n = 99,228) had completed primary education or less, and 75.3% (n = 182,980) lived in a city. In addition, 90.6% (n = 208,183) and 93.4% (n = 214,204) had complied with physical distancing and the use of a mask, respectively. We found that 71.1% (n = 154,833) reported food insecurity, while 86.7% (n = 195,130) reported economic insecurity. In addition, 41.4% (n = 98,562) and 45.9% (n = 108,557) reported having anxious and depressive symptoms, respectively. Furthermore, 60.9% (n = 134,454) of the participants did not report comorbidities, and 66.8% (n = 141,615) were not yet vaccinated against COVID-19, while 31.3% (n = 70,494) had had COVID-19 at some point, and 7.8% (n = 15,196) reported that they had no intention to vaccinate their children and adolescents against COVID-19 (Table 1). In addition, we reported the parents’ answers about intention to vaccinate their children against COVID-19 (Figure 2).

Table 1.
Descriptive analysis of the study sample (n = 227,740; N = 3,378,612).
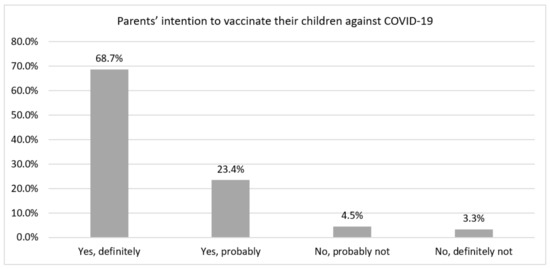
Figure 2.
Frequency of parents’ answers about intention to vaccinate their children against COVID-19 in Latin America and the Caribbean countries.
3.2. Bivariate Analysis According to Parents’ Non-Intention to Vaccinate Their Children and Adolescents against COVID-19
We found statistically significant differences in the bivariate analysis between the independent variables and the parents’ non-intention to vaccinate their children and adolescents against COVID-19, except for smoking (p = 0.481) and food insecurity (p = 0.070). The analysis is detailed in Table 2.

Table 2.
Characteristics according to parents’ intention to vaccinate their children against COVID-19 (n = 227,740; N = 3,378,612).
3.3. Prevalence of Parents’ Non-Intention to Vaccinate Their Children and Adolescents against COVID-19 According to Each LAC Country
We found that the countries with the highest prevalence of parents’ non-intention to vaccinate their children and adolescents against COVID-19 were Haiti (n = 142; 50.0%), Bolivia (n = 565; 13.8%), Panama (n = 157; 13.7%), Uruguay (n = 397; 12.9%) and Nicaragua (n = 217; 12.9%). On the other hand, the countries with the lowest prevalence of parents’ non-intention to vaccinate their children and adolescents against COVID-19 were Mexico (n = 2200; 5.4%), Honduras (n = 113; 5.9%), Brazil (n = 4409; 6.1%), El Salvador (n = 180; 6.8%), and Peru (n = 531; 7.3%) (Figure 3 and Supplementary Materials).

Figure 3.
Prevalence of parents’ non-intention to vaccinate their children against COVID-19 in Latin America and the Caribbean countries.
3.4. Factors Associated with Parents’ Non-Intention to Vaccinate Their Children and Adolescents against COVID-19
The adjusted statistical regression model showed a lower prevalence of non-intention to vaccinate children and adolescents against COVID-19 among parents between 35 and 44 years old (aPR = 0.86; 95%CI: 0.78–0.94; p = 0.001) and 45 to 54 years (aPR = 0.88; 95%CI: 0.80–0.97; p = 0.011) compared to those between 18 and 24. We found a higher prevalence of non-intention to vaccinate children and adolescents in parents with college, university, and post-graduate studies (aPR = 1.20; 95%CI: 1.10–1.31; p < 0.001), compared to the group without formal schooling, complete or incomplete elementary school. Physical distancing was the practice that was most strongly associated with the outcome (aPR = 0.46; 95%CI: 0.42–0.50; p < 0.001). Likewise, use of masks (aPR = 0.66; 95%CI: 0.61–0.70; p < 0.001), having economic insecurity (aPR = 0.80; 95%CI: 0.75–0.85; p < 0.001), anxiety symptoms (aPR = 0.87; 95%CI: 0.82–0.92; p < 0.001), depressive symptoms (aPR = 0.93; 95%CI: 0.87–0.99; p = 0.030) and having had COVID-19 (aPR = 0.93; 95%CI: 0.87–0.99; p = 0.045) were associated with a lower prevalence of parents’ non-intention to vaccinate their children and adolescents against COVID-19. Additionally, compared to not having comorbidities, having a chronic condition (aPR = 0.82; 95%CI: 0.77–0.87; p < 0.001) or two or more comorbidities (aPR = 0.87; 95%CI: 0.81–0.95; p = 0.001) was associated with a lower prevalence of parents’ non-intention to vaccinate their children and adolescents against COVID-19. Being vaccinated (aPR = 0.26; 95%CI: 0.23–0.28; p < 0.001) was also strongly associated with a lower prevalence of parents’ non-intention to vaccinate their children and adolescents against COVID-19. Conversely, compared to living in a city, living in a town (aPR = 1.29; 95%CI: 1.12–1.48; p < 0.001), a village or rural area (aPR = 1.34; 95%CI: 1.22–1.47; p < 0.001) was associated with a higher prevalence of parents’ non-intention to vaccinate their children and adolescents against COVID-19 (Table 3).

Table 3.
Factors associated with parents’ non-intention to vaccinate their children against COVID-19.
4. Discussion
We found that 9 out of 10 parents in Latin America intended to vaccinate their children or adolescents against COVID-19. This prevalence was higher than that reported in previous studies on this topic. For example, in Canada, a study carried out on parents of children between 9 and 12 years old reported an intention to vaccinate of 60.4% [18]. In Turkey, the intention to vaccinate was as high as 56.8%, with a preference for a locally developed over foreign vaccine [17]. In Switzerland, 59.2% of respondents indicated their intention to vaccinate their children once the vaccine was available [19]. In China, vaccine acceptability for children was 72.6% [16]. A multinational study in the United States, Canada, Israel, Spain, and Switzerland reported that 65% of parents intended to vaccinate their children against COVID-19 [20]. Another multinational study that included Latin American countries, such as Peru, Brazil, Mexico, Argentina, Colombia and Chile, found that 69.2% intended to vaccinate their children [15]. However, these results were not comparable with ours for various reasons, such as the time the study was carried out and the representativeness of the chosen sample. Indeed, the Canadian [18], Chinese and both multinational studies [15,20] were carried out in 2020 before vaccination in children and adolescents was a real possibility. One of the multinational studies only included mothers, whether pregnant or not [15]. The other included only parents who attended emergency departments of hospitals in the countries studied [20]. The Chinese study only included factory workers [16], and the Swiss study only included parents from two regions of the country [19].
Concerning parents between 35 and 54 years old having a greater intention to vaccinate their children, some studies have shown that the older persons are, the more likely they are to accept the COVID-19 vaccine [5]. This finding could be related to the fact that this age group is more likely to have children or adolescents than those over 54 years of age, while those under 35 are more likely to have young children and not consider it necessary or relevant to vaccinate them against COVID -19. Likewise, it was found that parents with comorbidities or health problems such as depression or anxiety had a greater intention to vaccinate their children. In this regard, given the known association between comorbidities and worse clinical outcomes in patients with COVID-19 [29], it is expected that a parent with these clinical conditions may have a higher assessment of the usefulness of vaccines, as they are a group vulnerable to this sickness.
Adherence to maintaining physical distance or wearing a mask and being vaccinated against COVID-19 were associated with a greater intention to vaccinate children against COVID-19. These findings suggest that people adhering to measures based on nationally and globally recommended evidence would follow vaccination recommendations for their children in the same way, indicating family vaccination intention. This correlates with what was found in the multinational study in 16 countries in pregnant women and mothers, which described that the use of face masks was one of the predictors for greater acceptance of the COVID-19 vaccine [15]. In adults, other studies have also shown that the use of masks and social distancing and anxiety were also strongly associated with getting vaccinated [30,31]. Compliance with these community mitigation measures and acceptance of the vaccine for their children may be related to concern about the disease in general and parents’ fear of the consequences of infection for their children [20].
Regarding the parents’ residence, living in a village, town or rural area was associated with a higher probability of non-intention to vaccinate children than parents living in a city. Unfortunately, no study has evaluated the differences regarding the parents’ place of residence. However, a lower intention and vaccination coverage against COVID-19 has been described in adults and pregnant women residing in rural areas [32,33]. Likewise, a previous study described lower vaccination coverage against the human papillomavirus in adolescents in rural areas of the United States [34], suggesting the presence of greater reluctance toward the vaccine against COVID-19 in these areas [35]. In addition, keeping children up to date in the vaccination schedule and having a caregiver vaccinated against influenza has been associated with a greater intention to vaccinate children against COVID-19 [20]. Therefore, vaccination coverage against COVID-19 in adolescents could be improved by increasing vaccination intention in parents residing in rural areas. We found that the parents’ having high educational levels was associated with a greater probability of non-intention to vaccinate their children and adolescents from LAC. This finding is consistent with a previous study carried out in China, which found that parents with college educations or below had a higher acceptance of COVID-19 vaccines, compared with parents with master’s diploma or above [36]. However, this does not agree with a study that evaluated the HPV vaccine hesitancy among parents in Italy, which found no difference between knowing that the HPV vaccine was a preventive measure for this disease and educational level [37]. This could be explained by an infodemic that occurred in LAC countries during 2020 [38,39] and could equally affect people of different educational levels.
It was found that financially insecure parents were more likely to vaccinate their children than those who were not. This result was contrary to various studies showing that parents with low education and income were less likely to intend to vaccinate their children [18]. The higher the income, the greater the probability of accepting vaccination against COVID -19 [40,41]. However, this might be explained by persons with economic insecurity having been more vulnerable to COVID-19 in the region [42]. Those who live with a job and social insecurity are at greater risk of presenting other infections during the pandemic [43]. In this sense, it has been described that people living in areas highly affected by the pandemic have a greater intention to be vaccinated [44], which could support our findings.
Regarding the differences in the non-intention to vaccinate among the countries, differences in the epidemiological situation, the wave or time of the pandemic in which they were found, and the proportion of people affected by COVID-19 in these countries must be taken into account. Likewise, the circulation of variants of the SARS-CoV-2 virus of the most significance, such as the alpha, beta, gamma, and delta variants [45], and especially the latter, could influence the decision to get vaccinated. As of 4 August 2021, this variant is present in 24 countries in the Americas region, and due to its greater transmissibility, mortality from this disease could increase, and health systems could collapse [46].
We must emphasize that the associated factors have different magnitudes, and their interpretation is relevant to prioritize the interventions to be carried out to increase the intention of vaccination in children and adolescents. Then, we highlight the im-portance of some factors that could improve vaccination intention in children, such as compliance with physical distancing and the use of masks, as well as vaccination by parents. On the other hand, they should encourage vaccination in children living in rural areas, as well as in the highest educational levels.
5. Limitations
This study has limitations. The respondents were users of a network (Facebook), which implies that the data obtained are from people with internet access and social networks and do not represent a population without these characteristics. Additionally, we did not have the non-response rate, which is relevant within the context of an online survey. Likewise, the variables included in this analysis were those that were available in the survey database, as there may have been other associated factors that were not measured by the survey and should be included in future studies. There is the possibility of hidden bias due to unmeasured confusion (i.e., there may have been some other associated factors that were not measured by the survey and should be included in future studies). Additionally, the data were obtained by self-reporting, and therefore, there may have been an underreporting of information. In addition, due to the study’s design, our results should be interpreted only in the context of associations; causality among the variables evaluated could not be established. Nonetheless, this study presents the strength of analyzing a database with a large representative sample of social network users widely used in LAC countries.
6. Conclusions
In conclusion, 9 out of 10 parents in LAC intended to vaccinate their children and adolescents against COVID-19. The intention to vaccinate their children was more remarkable in parents residing in a city and those presenting good adherence to health recommendations or chronic health conditions. In LAC countries, the population of children and adolescents represents a considerable proportion of the population, and despite not being a priority for being among the groups most at risk of severe disease due to COVID-19, they do play an essential role from the point of view of transmission and a source of new infections. It has been estimated that 70% vaccination coverage is necessary to achieve group or herd immunity and to be able to control the pandemic, and this fundamentally depends on vaccination rather than seroprevalence [47]. In this sense, the vaccination of children can play an important role in achieving this coverage [48]. For this reason, favoring vaccination in these groups and understanding the intention of parents to vaccinate is of great importance in developing possible promotion and education strategies for national vaccination plans against COVID-19.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/vaccines9111303/s1, Table S1: Proportion of parents with intention to vaccinate their children against COVID-19 in Latin America and the Caribbean region, File S1: Questionnaire.
Author Contributions
Conceptualization, D.U.-P., P.H.-A., A.U.-C., G.B.-Q., C.J.T.-H., A.J.R.-M., A.V.H. and V.A.B.-Z.; data curation, D.U.-P.; formal analysis, D.U.-P. and V.A.B.-Z.; methodology, D.U.-P. and V.A.B.-Z.; writing—original draft, D.U.-P., P.H.-A., A.U.-C., G.B.-Q., C.J.T.-H., A.J.R.-M., A.V.H. and V.A.B.-Z.; writing—review and editing, D.U.-P., P.H.-A., A.U.-C., G.B.-Q., C.J.T.-H., A.J.R.-M., A.V.H. and V.A.B.-Z. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. The APC was covered by the Universidad Científica del Sur and the Universidad Privada Norbert Wiener.
Institutional Review Board Statement
This study analyzed a secondary database that collected data without identifiers and did not violate the integrity of the participants. Access to the database was given with permission from the University of Maryland.
Informed Consent Statement
The participants who responded to the survey provided informed consent.
Data Availability Statement
Restrictions apply to the availability of these data. The authors obtained the data after signing a contract with the University of Maryland and have no permission to share the database.
Acknowledgments
We want to thank the Universidad Científica del Sur and the Universidad Privada Norbert Wiener for the financial support in the payment of the article processing charge.
Conflicts of Interest
Rodriguez-Morales, report being medical advisor of Abbott Diagnostics, Amgen, and Roche for Latin America, outside the submitted work. The rest of the authors declare no conflict of interest.
References
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 15 August 2021).
- Shah, S. Children and the American Rescue Plan: Countering COVID-19 vaccine hesitancy during a global pandemic. Pediatr. Res. 2021, 90, 237–239. [Google Scholar] [CrossRef]
- Wang, Q.; Yang, L.; Jin, H.; Lin, L. Vaccination against COVID-19: A systematic review and meta-analysis of acceptability and its predictors. Prev. Med. 2021, 150, 106694. [Google Scholar] [CrossRef] [PubMed]
- Sallam, M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines 2021, 9, 160. [Google Scholar] [CrossRef] [PubMed]
- Al-Amer, R.; Maneze, D.; Everett, B.; Montayre, J.; Villarosa, A.R.; Dwekat, E.; Salamonson, Y. COVID-19 vaccination intention in the first year of the pandemic: A systematic review. J. Clin. Nurs. 2021. [Google Scholar] [CrossRef] [PubMed]
- Plotkin, S.A.; Levy, O. Considering Mandatory Vaccination of Children for COVID-19. Pediatrics 2021, 147, 147. [Google Scholar] [CrossRef] [PubMed]
- Leeb, R.T.; Price, S.; Sliwa, S.; Kimball, A.; Szucs, L.; Caruso, E.; Godfred-Cato, S.; Lozier, M. COVID-19 trends among school-aged children—United States, 1 March–19 September 2020. Morb. Mortal. Wkly. Rep. 2020, 69, 1410. [Google Scholar] [CrossRef] [PubMed]
- Bhopal, S.S.; Bagaria, J.; Olabi, B.; Bhopal, R. Children and young people remain at low risk of COVID-19 mortality. Lancet Child Adolesc. Health 2021, 5, e12–e13. [Google Scholar] [CrossRef]
- Han, B.; Song, Y.; Li, C.; Yang, W.; Ma, Q.; Jiang, Z.; Li, M.; Lian, X.; Jiao, W.; Wang, L. Safety, tolerability, and immunogenicity of an inactivated SARS-CoV-2 vaccine (CoronaVac) in healthy children and adolescents: A double-blind, randomised, controlled, phase 1/2 clinical trial. Lancet Infect. Dis. 2021, 21, 803–812. [Google Scholar] [CrossRef]
- ModernaTX, Inc. A Study to Evaluate Safety and Effectiveness of mRNA-1273 COVID-19 Vaccine in Healthy Children between 6 Months of Age and Less Than 12 Years of Age. Available online: https://clinicaltrials.gov/ct2/show/NCT04796896 (accessed on 10 August 2021).
- U.S. Food & Drug Administration. Coronavirus (COVID-19) Update: FDA Authorizes Pfizer-BioNTech COVID-19 Vaccine for Emergency Use in Adolescents in Another Important Action in Fight Against Pandemic. Available online: https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-authorizes-pfizer-biontech-covid-19-vaccine-emergency-use (accessed on 10 August 2021).
- European Medicines Agency. First COVID-19 Vaccine Approved for Children Aged 12 to 15 in EU. Available online: https://www.ema.europa.eu/en/news/first-covid-19-vaccine-approved-children-aged-12-15-eu (accessed on 10 August 2021).
- Zimet, G.D.; Silverman, R.D.; Fortenberry, J.D. Coronavirus Disease 2019 and Vaccination of Children and Adolescents: Prospects and Challenges. J. Pediatr. 2021, 231, 254–258. [Google Scholar] [CrossRef]
- World Health Organization. Ten Threats to Global Health in 2019. 2019. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 10 September 2021).
- Skjefte, M.; Ngirbabul, M.; Akeju, O.; Escudero, D.; Hernandez-Diaz, S.; Wyszynski, D.F.; Wu, J.W. COVID-19 vaccine acceptance among pregnant women and mothers of young children: Results of a survey in 16 countries. Eur. J. Epidemiol. 2021, 36, 197–211. [Google Scholar] [CrossRef]
- Zhang, K.C.; Fang, Y.; Cao, H.; Chen, H.; Hu, T.; Chen, Y.Q.; Zhou, X.; Wang, Z. Parental Acceptability of COVID-19 Vaccination for Children Under the Age of 18 Years: Cross-Sectional Online Survey. JMIR Pediatr. Parent. 2020, 3, e24827. [Google Scholar] [CrossRef] [PubMed]
- Yigit, M.; Ozkaya-Parlakay, A.; Senel, E. Evaluation of COVID-19 Vaccine Refusal in Parents. Pediatr. Infect. Dis. J. 2021, 40, e134–e136. [Google Scholar] [CrossRef]
- Hetherington, E.; Edwards, S.A.; MacDonald, S.E.; Racine, N.; Madigan, S.; McDonald, S.; Tough, S. SARS-CoV-2 vaccination intentions among mothers of children aged 9 to 12 years: A survey of the All Our Families cohort. CMAJ Open 2021, 9, E548. [Google Scholar] [CrossRef]
- Seiler, M.; Goldman, R.D.; Staubli, G.; Hoeffe, J.; Gualco, G.; Manzano, S.; Part of the International COVID-19 Parental Attitude Study (COVIPAS) Group. Parents’ intent to vaccinate against influenza during the COVID-19 pandemic in two regions in Switzerland. Swiss Med. Wkly. 2021, 151, w20508. [Google Scholar] [CrossRef]
- Goldman, R.D.; Yan, T.D.; Seiler, M.; Cotanda, C.P.; Brown, J.C.; Klein, E.J.; Hoeffe, J.; Gelernter, R.; Hall, J.E.; Davis, A.L.; et al. Caregiver willingness to vaccinate their children against COVID-19: Cross sectional survey. Vaccine 2020, 38, 7668–7673. [Google Scholar] [CrossRef] [PubMed]
- Guzman-Holst, A.; DeAntonio, R.; Prado-Cohrs, D.; Juliao, P. Barriers to vaccination in Latin America: A systematic literature review. Vaccine 2020, 38, 470–481. [Google Scholar] [CrossRef]
- Urrunaga-Pastor, D.; Bendezu-Quispe, G.; Herrera-Añazco, P.; Uyen-Cateriano, A.; Toro-Huamanchumo, C.J.; Rodriguez-Morales, A.J.; Hernandez, A.V.; Benites-Zapata, V.A. Cross-sectional analysis of COVID-19 vaccine intention, perceptions and hesitancy across Latin America and the Caribbean. Travel Med. Infect. Dis. 2021, 41, 102059. [Google Scholar] [CrossRef]
- Benítez, M.A.; Velasco, C.; Sequeira, A.R.; Henríquez, J.; Menezes, F.M.; Paolucci, F. Responses to COVID-19 in five Latin American countries. Health Policy Technol. 2020, 9, 525–559. [Google Scholar] [CrossRef]
- Martinez-Valle, A. Public health matters: Why is Latin America struggling in addressing the pandemic? J. Public Health Policy 2021, 42, 27–40. [Google Scholar] [CrossRef] [PubMed]
- PAHO. PAHO Director Calls for Fair and Broad Access to COVID-19 Vaccines for Latin America and the Caribbean. Available online: https://www.paho.org/en/news/7-7-2021-paho-director-calls-fair-and-broad-access-covid-19-vaccines-latin-america-and (accessed on 10 August 2021).
- Larson, H.J.; Jarrett, C.; Eckersberger, E.; Smith, D.M.D.; Paterson, P. Understanding Vaccine Hesitancy around Vaccines and Vaccination from a Global Perspective: A Systematic Review of Published Literature, 2007–2012. Vaccine 2014, 32, 2150–2159. [Google Scholar] [CrossRef] [PubMed]
- Di Giuseppe, G.; Pelullo, C.P.; Della Polla, G.; Pavia, M.; Angelillo, I.F. Exploring the willingness to accept SARS-CoV-2 vaccine in a University population in Southern Italy, September to November 2020. Vaccines 2021, 9, 275. [Google Scholar] [CrossRef]
- Barkay, N.; Cobb, C.; Eilat, R.; Galili, T.; Haimovich, D.; LaRocca, S.; Morris, K.; Sarig, T. Weights and methodology brief for the COVID-19 symptom survey by University of Maryland and Carnegie Mellon University, in partnership with Facebook. arXiv 2020, arXiv:2009.14675. [Google Scholar]
- Fang, X.; Li, S.; Yu, H.; Wang, P.; Zhang, Y.; Chen, Z.; Li, Y.; Cheng, L.; Li, W.; Jia, H.; et al. Epidemiological, comorbidity factors with severity and prognosis of COVID-19: A systematic review and meta-analysis. Aging 2020, 12, 12493–12503. [Google Scholar] [CrossRef] [PubMed]
- Latkin, C.A.; Dayton, L.; Yi, G.; Colon, B.; Kong, X. Mask usage, social distancing, racial, and gender correlates of COVID-19 vaccine intentions among adults in the US. PLoS ONE 2021, 16, e0246970. [Google Scholar] [CrossRef] [PubMed]
- Bendau, A.; Plag, J.; Petzold, M.B.; Ströhle, A. COVID-19 vaccine hesitancy and related fears and anxiety. Int. Immunopharmacol. 2021, 97, 107724. [Google Scholar] [CrossRef]
- Kaur, R.; Callaghan, T.; Regan, A.K. Disparities in maternal influenza immunization among women in rural and urban areas of the United States. Prev. Med. 2021, 147, 106531. [Google Scholar] [CrossRef]
- Murthy, B.P.; Sterrett, N.; Weller, D.; Zell, E.; Reynolds, L.; Toblin, R.L.; Murthy, N.; Kriss, J.; Rose, C.; Cadwell, B.; et al. Disparities in COVID-19 Vaccination Coverage Between Urban and Rural Counties—United States, 14 December 2020–10 April 2021. MMWR. Morb. Mortal. Wkly. Rep. 2021, 70, 759–764. [Google Scholar] [CrossRef]
- Zhai, Y.; Santibanez, T.A.; Kahn, K.E.; Srivastav, A.; Walker, T.Y.; Singleton, J.A. Rural, urban, and suburban differences in influenza vaccination coverage among children. Vaccine 2020, 38, 7596–7602. [Google Scholar] [CrossRef] [PubMed]
- Vanderpool, R.C.; Stradtman, L.R.; Brandt, H.M. Policy opportunities to increase HPV vaccination in rural communities. Hum. Vaccines Immunother. 2019, 15, 1527–1532. [Google Scholar] [CrossRef]
- Wang, Q.; Xiu, S.; Zhao, S.; Wang, J.; Han, Y.; Dong, S.; Huang, J.; Cui, T.; Yang, L.; Shi, N.; et al. Vaccine Hesitancy: COVID-19 and Influenza Vaccine Willingness among Parents in Wuxi, China—A Cross-Sectional Study. Vaccines 2021, 9, 342. [Google Scholar] [CrossRef]
- Della Polla, G.; Pelullo, C.P.; Napolitano, F.; Angelillo, I.F. HPV vaccine hesitancy among parents in Italy: A cross-sectional study. Hum. Vaccines Immunother. 2020, 16, 2744–2751. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ceron, W.; Sanseverino, G.G.; De-Lima-Santos, M.-F.; Quiles, M.G. COVID-19 fake news diffusion across Latin America. Soc. Netw. Anal. Min. 2021, 11, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Alvarez-Risco, A.; Mejia, C.R.; Delgado-Zegarra, J.; Del-Aguila-Arcentales, S.; Arce-Esquivel, A.A.; Valladares-Garrido, M.J.; Del Portal, M.R.; Villegas, L.F.; Curioso, W.H.; Sekar, M.C.; et al. The Peru Approach against the COVID-19 Infodemic: Insights and Strategies. Am. J. Trop. Med. Hyg. 2020, 103, 583–586. [Google Scholar] [CrossRef]
- Boyle, J.; Berman, L.; Nowak, G.J.; Iachan, R.; Middleton, D.; Deng, Y. An assessment of parents’ childhood immunization beliefs, intentions, and behaviors using a smartphone panel. Vaccine 2020, 38, 2416–2423. [Google Scholar] [CrossRef]
- He, K.; Mack, W.J.; Neely, M.; Lewis, L.; Anand, V. Parental Perspectives on Immunizations: Impact of the COVID-19 Pandemic on Childhood Vaccine Hesitancy. J. Community Health 2021, 23, 1–14. [Google Scholar] [CrossRef]
- Del Brutto, O.H.; Mera, R.M.; Recalde, B.Y.; Costa, A.F. Social determinants of health and risk of SARS-CoV-2 infection in community-dwelling older adults living in a rural Latin American setting. J. Community Health 2021, 46, 292–297. [Google Scholar] [CrossRef] [PubMed]
- Duarte, R.; Aguiar, A.; Pinto, M.; Furtado, I.; Tiberi, S.; Lönnroth, K.; Migliori, G. Different disease, same challenges: Social determinants of tuberculosis and COVID-19. Pulmonology 2021, 27, 338–344. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.; Hu, Z.; Zhao, Q.; Alias, H.; Danaee, M.; Wong, L.P. Understanding COVID-19 vaccine demand and hesitancy: A nationwide online survey in China. PLoS Negl. Trop. Dis. 2020, 14, e0008961. [Google Scholar] [CrossRef]
- de Puig, H.; Lee, R.A.; Najjar, D.; Tan, X.; Soekensen, L.R.; Angenent-Mari, N.M.; Donghia, N.M.; Weckman, N.E.; Ory, A.; Ng, C.F. Minimally instrumented SHERLOCK (miSHERLOCK) for CRISPR-based point-of-care diagnosis of SARS-CoV-2 and emerging variants. Sci. Adv. 2021, 7, eabh2944. [Google Scholar] [CrossRef]
- Sheikh, A.; McMenamin, J.; Taylor, B.; Robertson, C. SARS-CoV-2 Delta VOC in Scotland: Demographics, risk of hospital admission, and vaccine effectiveness. Lancet 2021, 397, 2461–2462. [Google Scholar] [CrossRef]
- Núñez-Zapata, S.F.; Benites-Peralta, B.; Mayta-Tristan, P.; Rodríguez-Morales, A.J. High seroprevalence for SARS-CoV-2 infection in South America, but still not enough for heard immunity! Int. J. Infect. Dis. 2021, 109, 244–246. [Google Scholar] [CrossRef] [PubMed]
- Anderson, R.M.; Vegvari, C.; Truscott, J.; Collyer, B.S. Challenges in creating herd immunity to SARS-CoV-2 infection by mass vaccination. Lancet 2020, 396, 1614–1616. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).