Cationic Polymers for the Delivery of the Ebola DNA Vaccine Encoding Artificial T-Cell Immunogen
Abstract
1. Introduction
2. Materials and Methods
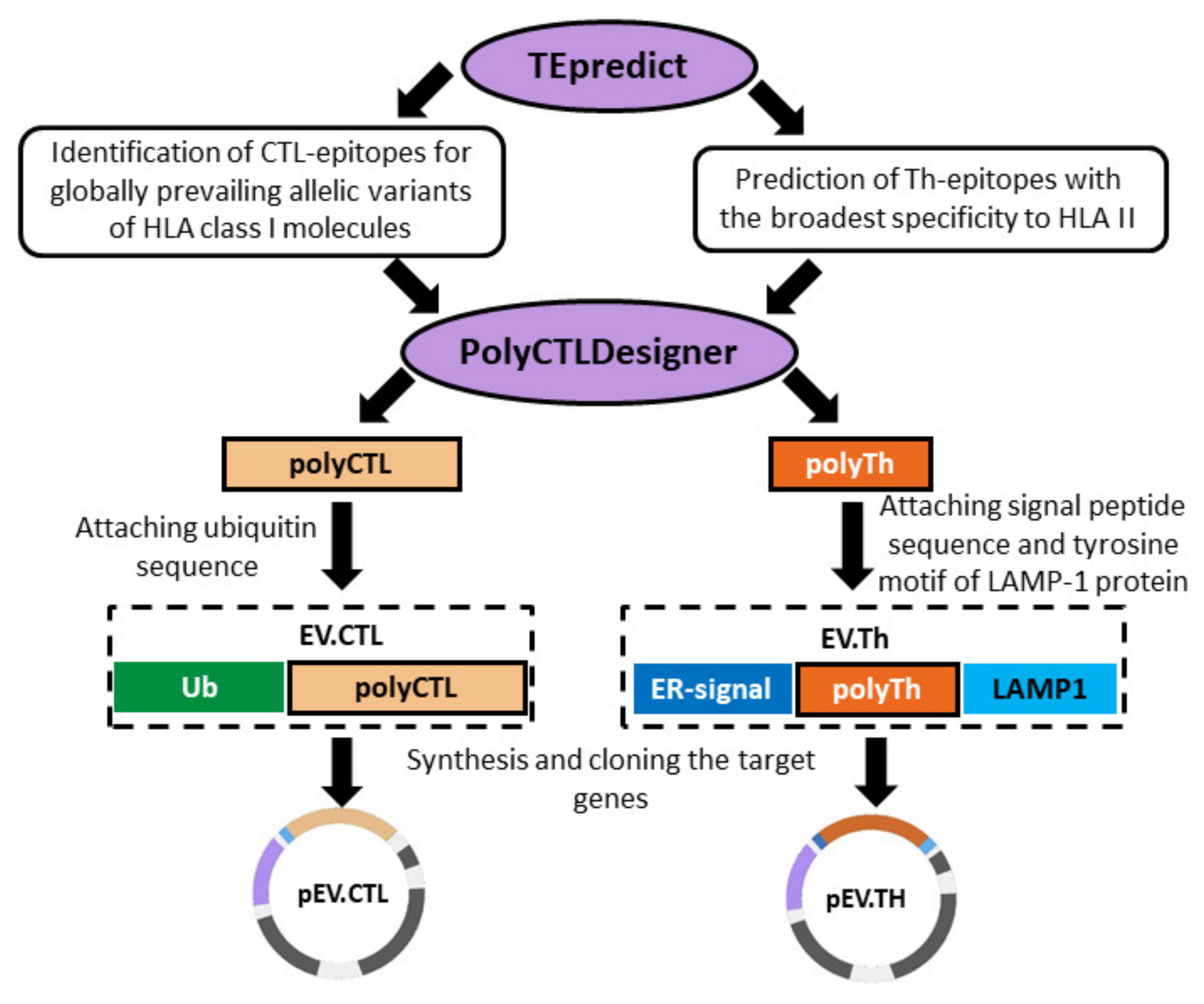
2.1. DNA Vaccine Constructions
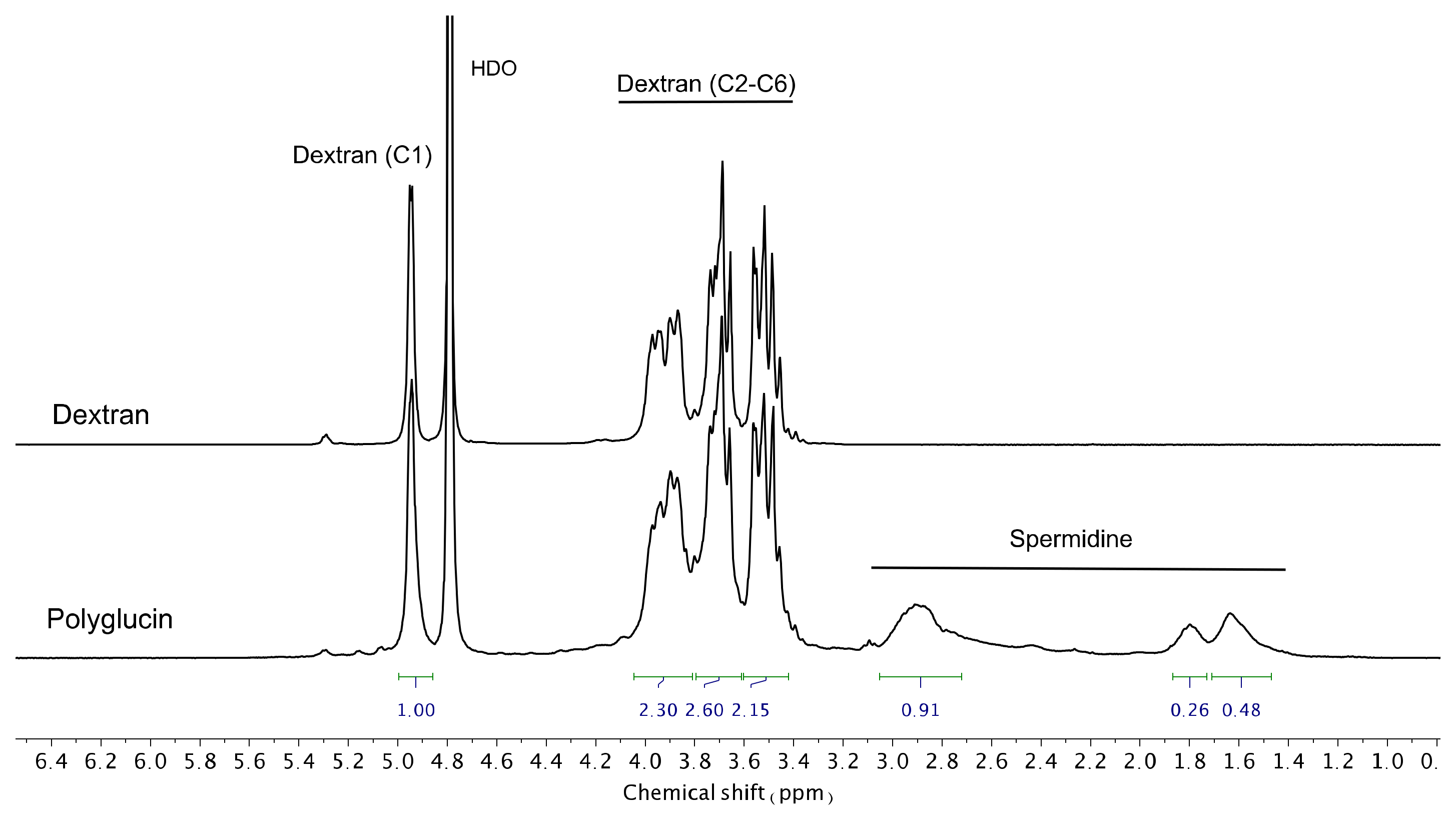
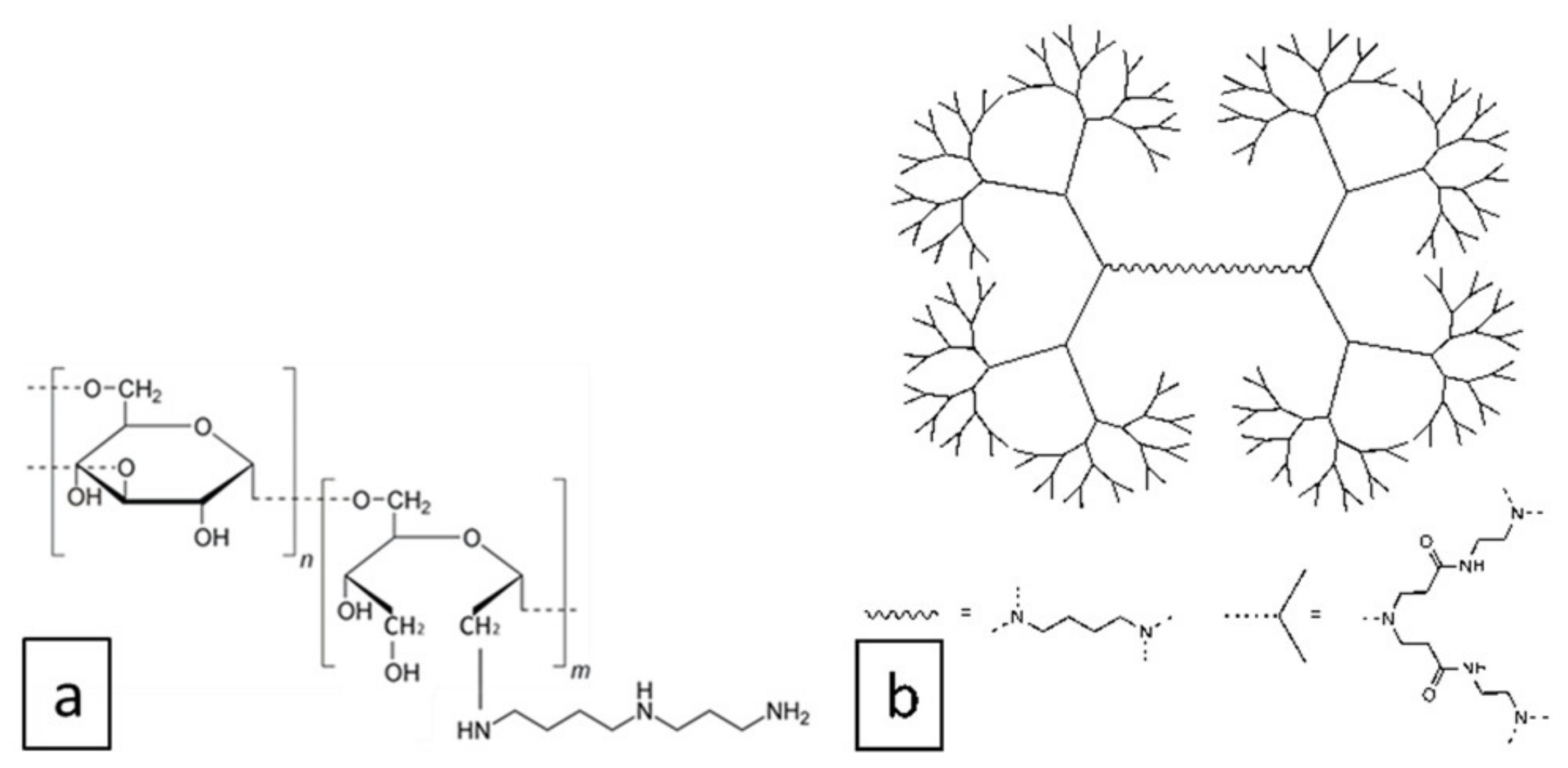
2.2. Cationic Polymers
2.3. Physicochemical Analysis of DNA-Polymer Complexes
2.4. Verification of Complex Formation before Immunization
2.5. Immunization
- ∑DNA group—mice immunized with a mixture of DNA plasmids pEV.CTL and pEV.Th encoding CTL and Th epitopes of the Ebola virus, respectively;
- Group ∑DNA+PG—mice immunized with a mixture of complexes formed from the conjugate polyglucin:spermidine with DNA plasmids pEV.CTL and pEV.Th;
- Group ∑DNA+PAMAM—mice immunized with a mixture of complexes formed from the generation 4 polyamidoamine dendrimer with DNA plasmids pEV.CTL and pEV.Th;
- Group pcDNA3.1—mice immunized with the vector plasmid (a negative control).
2.6. ELISpot and ICS
2.7. Statistical Analysis
3. Results
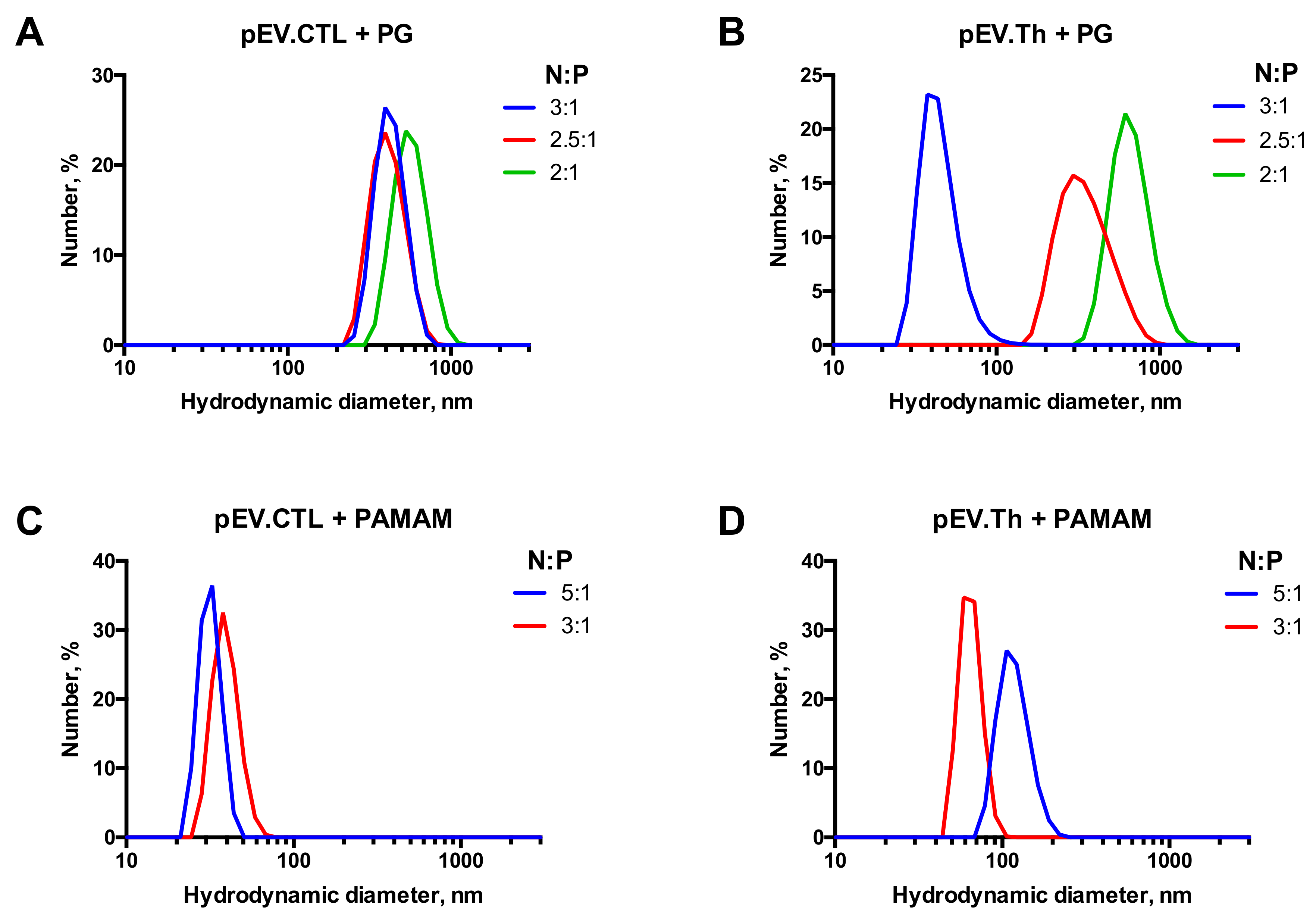
3.1. DNA Complexation with Polycationic Adjuvants
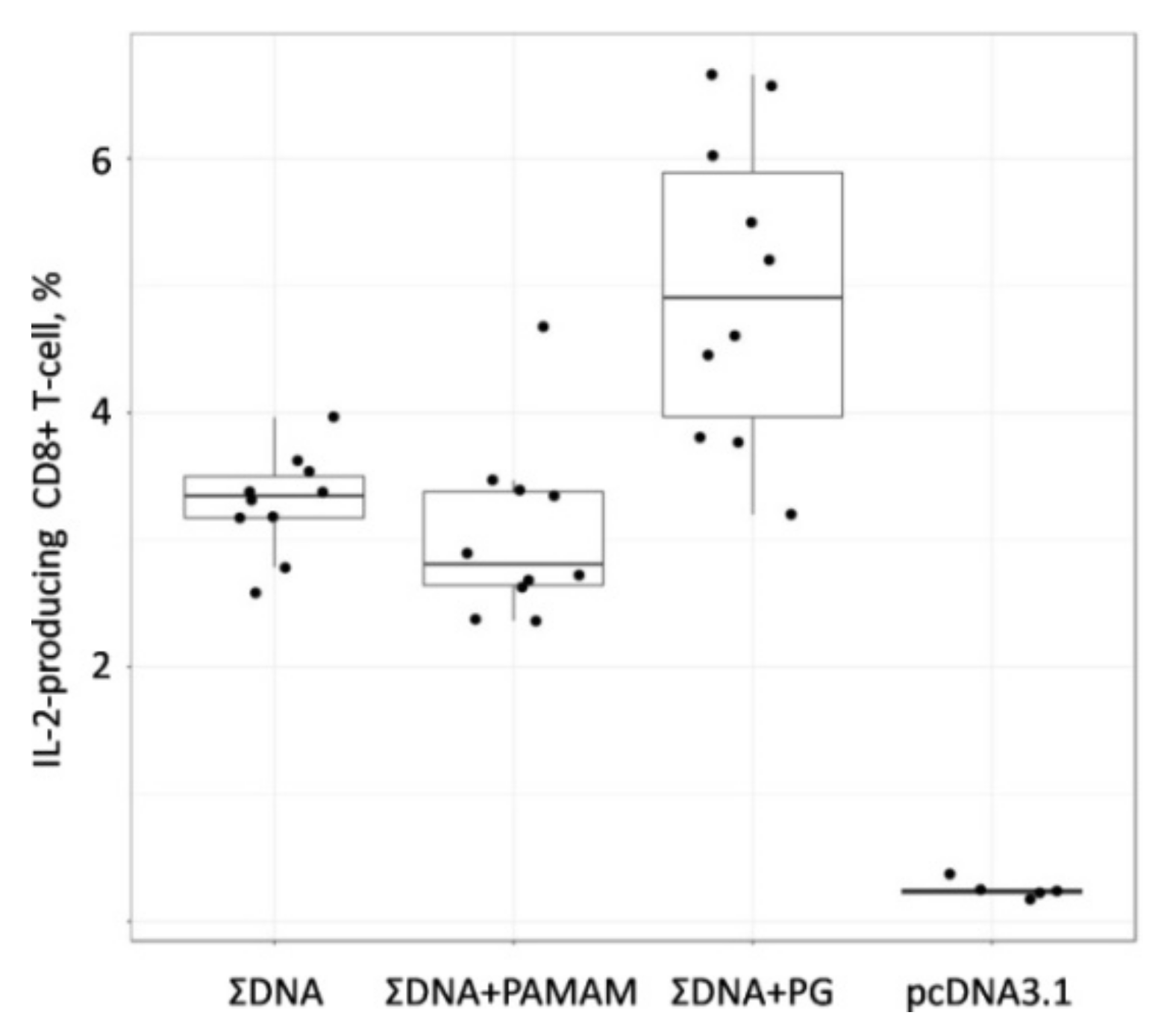
3.2. Immunogenicity of Cationic Polymer Complexes with DNA Vaccine Constructs
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Pavot, V. Ebola virus vaccines: Where do we stand? Clin. Immunol. 2016, 173, 44–49. [Google Scholar] [CrossRef] [PubMed]
- Pyankov, O.V.; Setoh, Y.X.; Bodnev, S.A.; Edmonds, J.H.; Pyankova, O.G.; Pyankov, S.A.; Pali, G.; Belford, S.; Lu, L.; La, M.; et al. Successful post-exposure prophylaxis of Ebola infected non-human primates using Ebola glycoprotein-specific equine IgG. Sci. Rep. 2017, 7. [Google Scholar] [CrossRef] [PubMed]
- Reynard, O.; Nguyen, X.N.; Alazard-Dany, N.; Barateau, V.; Cimarelli, A.; Volchkov, V.E. Identification of a new ribonucleoside inhibitor of ebola virus replication. Viruses 2015, 7, 6233–6240. [Google Scholar] [CrossRef] [PubMed]
- Marzi, A.; Feldmann, H. Ebola virus vaccines: An overview of current approaches. Expert Rev. Vaccines 2014, 13, 521–531. [Google Scholar] [CrossRef] [PubMed]
- Henao-Restrepo, A.M.; Camacho, A.; Longini, I.M.; Watson, C.H.; Edmunds, W.J.; Egger, M.; Carroll, M.W.; Dean, N.E.; Diatta, I.; Doumbia, M.; et al. Efficacy and effectiveness of an rVSV-vectored vaccine in preventing Ebola virus disease: Final results from the Guinea ring vaccination, open-label, cluster-randomised trial (Ebola Ça Suffit!). Lancet 2017, 389, 505–518. [Google Scholar] [CrossRef]
- Marzi, A.; Robertson, S.J.; Haddock, E.; Feldmann, F.; Hanley, P.W.; Scott, D.P.; Strong, J.E.; Kobinger, G.; Best, S.M.; Feldmann, H. VSV-EBOV rapidly protects macaques against infection with the 2014/15 Ebola virus outbreak strain. Science 2015, 349, 739–742. [Google Scholar] [CrossRef] [PubMed]
- Meyer, M.; Huang, E.; Yuzhakov, O.; Ramanathan, P.; Ciaramella, G.; Bukreyev, A. Modified mRNA-Based Vaccines Elicit Robust Immune Responses and Protect Guinea Pigs from Ebola Virus Disease. J. Infect. Dis. 2018, 217, 451–455. [Google Scholar] [CrossRef]
- Chahal, J.S.; Khan, O.F.; Cooper, C.L.; McPartlan, J.S.; Tsosie, J.K.; Tilley, L.D.; Sidik, S.M.; Lourido, S.; Langer, R.; Bavari, S.; et al. Dendrimer-RNA nanoparticles generate protective immunity against lethal ebola, H1N1 influenza and Toxoplasma gondii challenges with a single dose. Proc. Natl. Acad. Sci. USA 2016, 113, E4133–E4142. [Google Scholar] [CrossRef]
- Dolzhikova, I.V.; Zubkova, O.V.; Tukhvatulin, A.I.; Dzharullaeva, A.S.; Tukhvatulina, N.M.; Shcheblyakov, D.V.; Shmarov, M.M.; Tokarskaya, E.A.; Simakova, Y.V.; Egorova, D.A.; et al. Safety and immunogenicity of GamEvac-Combi, a heterologous VSV- and Ad5-vectored Ebola vaccine: An open phase I/II trial in healthy adults in Russia. Hum. Vaccines Immunother. 2017, 13, 613–620. [Google Scholar] [CrossRef]
- Sullivan, N.J.; Hensley, L.; Asiedu, C.; Geisbert, T.W.; Stanley, D.; Johnson, J.; Honko, A.; Olinger, G.; Bailey, M.; Geisbert, J.B.; et al. CD8 + cellular immunity mediates rAd5 vaccine protection against Ebola virus infection of nonhuman primates. Nat. Med. 2011, 17, 1128–1131. [Google Scholar] [CrossRef]
- Marzi, A.; Engelmann, F.; Feldmann, F.; Haberthur, K.; Shupert, W.L.; Brining, D.; Scott, D.P.; Geisbert, T.W.; Kawaoka, Y.; Katze, M.G.; et al. Antibodies are necessary for rVSV/ZEBOV-GP-mediated protection against lethal Ebola virus challenge in nonhuman primates. Proc. Natl. Acad. Sci. USA 2013, 110, 1893–1898. [Google Scholar] [CrossRef] [PubMed]
- Rahim, M.N.; Wee, E.G.; He, S.; Audet, J.; Tierney, K.; Moyo, N.; Hannoun, Z.; Crook, A.; Baines, A.; Korber, B.; et al. Complete protection of the BALB/c and C57BL/6J mice against Ebola and Marburg virus lethal challenges by pan-filovirus T-cell epigraph vaccine. PLoS Pathog. 2019, 15. [Google Scholar] [CrossRef] [PubMed]
- Sakabe, S.; Sullivan, B.M.; Hartnett, J.N.; Robles-Sikisaka, R.; Gangavarapu, K.; Cubitt, B.; Ware, B.C.; Kotliar, D.; Branco, L.M.; Goba, A.; et al. Analysis of CD8+ T cell response during the 2013–2016 Ebola epidemic in West Africa. Proc. Natl. Acad. Sci. USA 2018, 115, E7578–E7586. [Google Scholar] [CrossRef] [PubMed]
- Bazhan, S.I.; Antonets, D.V.; Karpenko, L.I.; Oreshkova, S.F.; Kaplina, O.N.; Starostina, E.V.; Dudko, S.G.; Fedotova, S.A.; Ilyichev, A.A. In silico Designed Ebola Virus T-Cell Multi-Epitope DNA Vaccine Constructions Are Immunogenic in Mice. Vaccines 2019, 7, 34. [Google Scholar] [CrossRef] [PubMed]
- Grant-Klein, R.J.; Van Deusen, N.M.; Badger, C.V.; Hannaman, D.; Dupuy, L.C.; Schmaljohn, C.S. A multiagent filovirus DNA vaccine delivered by intramuscular electroporation completely protects mice from ebola and Marburg virus challenge. Hum. Vaccines Immunother. 2012, 8, 1703–1706. [Google Scholar] [CrossRef] [PubMed]
- Sardesai, N.Y.; Weiner, D.B. Electroporation delivery of DNA vaccines: Prospects for success. Curr. Opin. Immunol. 2011, 23, 421–429. [Google Scholar] [CrossRef] [PubMed]
- Tzeng, S.Y.; Green, J.J. Polymeric nucleic acid delivery for immunoengineering. Curr. Opin. Biomed. Eng. 2018, 7, 42–50. [Google Scholar] [CrossRef]
- Vita, R.; Overton, J.A.; Greenbaum, J.A.; Ponomarenko, J.; Clark, J.D.; Cantrell, J.R.; Wheeler, D.K.; Gabbard, J.L.; Hix, D.; Sette, A.; et al. The immune epitope database (IEDB) 3.0. Nucleic Acids Res. 2015, 43, D405–D412. [Google Scholar] [CrossRef]
- Antonets, D.V.; Bazhan, S.I. PolyCTLDesigner: A computational tool for constructing polyepitope T-cell antigens. BMC Res. Notes 2013, 6. [Google Scholar] [CrossRef]
- Antonets, D.V.; Maksyutov, A.Z. TEpredict: Software for T-Cell epitope prediction. Mol. Biol. 2010, 44, 119–127. [Google Scholar] [CrossRef]
- Villalobos, A.; Welch, M.; Minshull, J. In silico design of functional DNA constructs. In Methods in Molecular Biology; Humana Press: Totowa, NJ, USA, 2012; Volume 852, pp. 197–213. [Google Scholar]
- Robin Harris, J.; Horne, R.W. Negative staining: A brief assessment of current technical benefits, limitations and future possibilities. Micron 1994, 25, 5–13. [Google Scholar] [CrossRef]
- Lebedev, L.R.; Karpenko, L.I.; Poryvaeva, V.A.; Azaev, M.S.; Riabchikova, E.I.; Gileva, I.P.; Il’ichev, A.A. Design of virus-like particles, exposing HIV-1 epitopes. Mol. Biol. 2000, 34, 480–485. [Google Scholar] [PubMed]
- Karpenko, L.I.; Lebedev, L.R.; Ignatyev, G.M.; Agafonov, A.P.; Poryvaeva, V.A.; Pronyaeva, T.R.; Ryabchikova, E.I.; Pokrovsky, A.G.; Ilyichev, A.A. Construction of artificial virus-like particles exposing HIV epitopes and the study of their immunogenic properties. Vaccine 2003, 21, 386–392. [Google Scholar] [CrossRef]
- Bazhan, S.I.; Karpenko, L.I.; Lebedev, L.R.; Uzhachenko, R.V.; Belavin, P.A.; Eroshkin, A.M.; Ilyichev, A.A. A synergistic effect of a combined bivalent DNA-protein anti-HIV-1 vaccine containing multiple T- and B-cell epitopes of HIV-1 proteins. Mol. Immunol. 2008, 45, 661–669. [Google Scholar] [CrossRef] [PubMed]
- Esina, T.I.; Volosnikova, E.A.; Lebedev, L.R.; Kochneva, G.V.; Grazhdantseva, A.A. Study on the Methods for Synthesis of GM-CSF Conjugates with Alendronic Acid. Russ. J. Bioorg. Chem. 2020, 46, 342–348. [Google Scholar] [CrossRef]
- Karpenko, L.I.; Ilyichev, A.A.; Eroshkin, A.M.; Lebedev, L.R.; Uzhachenko, R.V.; Nekrasova, N.A.; Plyasunova, O.A.; Belavin, P.A.; Seregin, S.V.; Danilyuk, N.K.; et al. Combined virus-like particle-based polyepitope DNA/protein HIV-1 vaccine—Design, immunogenicity and toxicity studies. Vaccine 2007, 25, 4312–4323. [Google Scholar] [CrossRef]
- Karpenko, L.I.; Bazhan, S.I.; Bogryantseva, M.P.; Ryndyuk, N.N.; Ginko, Z.I.; Kuzubov, V.I.; Lebedev, L.R.; Kaplina, O.N.; Reguzova, A.Y.; Ryzhikov, A.B.; et al. Results of phase I clinical trials of a combined vaccine against HIV-1 based on synthetic polyepitope immunogens. Russ. J. Bioorg. Chem. 2016, 42, 170–182. [Google Scholar] [CrossRef]
- De Araújo, R.V.; da Silva Santos, S.; Ferreira, E.I.; Giarolla, J. New advances in general biomedical applications of PAMAM dendrimers. Molecules 2018, 23, 2849. [Google Scholar] [CrossRef]
- Abedi-Gaballu, F.; Dehghan, G.; Ghaffari, M.; Yekta, R.; Abbaspour-Ravasjani, S.; Baradaran, B.; Ezzati Nazhad Dolatabadi, J.; Hamblin, M.R. PAMAM dendrimers as efficient drug and gene delivery nanosystems for cancer therapy. Appl. Mater. Today 2018, 12, 177–190. [Google Scholar] [CrossRef]
- Dzmitruk, V.; Apartsin, E.; Ihnatsyeu-Kachan, A.; Abashkin, V.; Shcharbin, D.; Bryszewska, M. Dendrimers show promise for siRNA and microrna therapeutics. Pharmaceutics 2018, 10, 126. [Google Scholar] [CrossRef]
- Knauer, N.; Pashkina, E.; Apartsin, E. Topological aspects of the design of nanocarriers for therapeutic peptides and proteins. Pharmaceutics 2019, 11. [Google Scholar] [CrossRef] [PubMed]
- Sampathkumar, S.-G.; Yarema, K.J. Dendrimers in Cancer Treatment and Diagnosis. In Nanotechnologies for the Life Sciences; Wiley-VCH Verlag GmbH & Co. KGaA: Weinheim, Germany, 2007. [Google Scholar] [CrossRef]
- Wang, X.; Dai, Y.; Zhao, S.; Tang, J.; Li, H.; Xing, Y.; Qu, G.; Li, X.; Dai, J.; Zhu, Y.; et al. PAMAM-Lys, a novel vaccine delivery vector, enhances the protective effects of the SjC23 DNA vaccine against schistosoma japonicum infection. PLoS ONE 2014, 9. [Google Scholar] [CrossRef] [PubMed]
- Daftarian, P.; Kaifer, A.E.; Li, W.; Blomberg, B.B.; Frasca, D.; Roth, F.; Chowdhury, R.; Berg, E.A.; Fishman, J.B.; Al Sayegh, H.A.; et al. Peptide-conjugated PAMAM dendrimer as a universal DNA vaccine platform to target antigen-presenting cells. Cancer Res. 2011, 71, 7452–7462. [Google Scholar] [CrossRef] [PubMed]
- Chauhan, A.S.; Jain, N.K.; Diwan, P.V. Pre-clinical and behavioural toxicity profile of PAMAM dendrimers in mice. Proc. R. Soc. A Math. Phys. Eng. Sci. 2010, 466, 1535–1550. [Google Scholar] [CrossRef]
- Albertazzi, L.; Gherardini, L.; Brondi, M.; Sulis Sato, S.; Bifone, A.; Pizzorusso, T.; Ratto, G.M.; Bardi, G. In vivo distribution and toxicity of PAMAM dendrimers in the central nervous system depend on their surface chemistry. Mol. Pharm. 2013, 10, 249–260. [Google Scholar] [CrossRef]
- Patel, A.; Reuschel, E.L.; Kraynyak, K.A.; Racine, T.; Park, D.H.; Scott, V.L.; Audet, J.; Amante, D.; Wise, M.C.; Keaton, A.A.; et al. Protective Efficacy and Long-Term Immunogenicity in Cynomolgus Macaques by Ebola Virus Glycoprotein Synthetic DNA Vaccines. J. Infect. Dis. 2019, 219, 544–555. [Google Scholar] [CrossRef]
- Martin, J.E.; Sullivan, N.J.; Enama, M.E.; Gordon, I.J.; Roederer, M.; Koup, R.A.; Bailer, R.T.; Chakrabarti, B.K.; Bailey, M.A.; Gomez, P.L.; et al. A DNA vaccine for Ebola virus is safe and immunogenic in a phase I clinical trial. Clin. Vaccine Immunol. 2006, 13, 1267–1277. [Google Scholar] [CrossRef]
- Wang, S.; Lu, S. DNA immunization. Curr. Protoc. Microbiol. 2013. [Google Scholar] [CrossRef]
- Zukancic, D.; Suys, E.J.A.; Pilkington, E.H.; Algarni, A.; Al-Wassiti, H.; Truong, N.P. The importance of poly(Ethylene glycol) and lipid structure in targeted gene delivery to lymph nodes by lipid nanoparticles. Pharmaceutics 2020, 12, 1068. [Google Scholar] [CrossRef]
- Eichman, J.D.; Bielinska, A.U.; Kukowska-Latallo, J.F.; Baker, J.R., Jr. The use of PAMAM dendrimers in the efficient transfer of genetic material into cells. Pharm. Sci. Technol. Today 2000, 3, 232–245. [Google Scholar] [CrossRef]
- Farris, E.; Brown, D.M.; Ramer-Tait, A.E.; Pannier, A.K. Micro- and nanoparticulates for DNA vaccine delivery. Exp. Biol. Med. 2016, 241, 919–929. [Google Scholar] [CrossRef] [PubMed]
- Glass, J.J.; Kent, S.J.; De Rose, R. Enhancing dendritic cell activation and HIV vaccine effectiveness through nanoparticle vaccination. Expert Rev. Vaccines 2016, 15, 719–729. [Google Scholar] [CrossRef] [PubMed]
- Yan, S.; Gu, W.; Xu, Z.P. Re-considering how particle size and other properties of antigen-adjuvant complexes impact on the immune responses. J. Colloid Interface Sci. 2013, 395, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Joshi, V.B.; Geary, S.M.; Salem, A.K. Biodegradable particles as vaccine delivery systems: Size matters. AAPS J. 2013, 15, 85–94. [Google Scholar] [CrossRef] [PubMed]
- Kesharwani, P.; Banerjee, S.; Gupta, U.; Mohd Amin, M.C.I.; Padhye, S.; Sarkar, F.H.; Iyer, A.K. PAMAM dendrimers as promising nanocarriers for RNAi therapeutics. Mater. Today 2015, 18, 565–572. [Google Scholar] [CrossRef]
- Fox, L.J.; Richardson, R.M.; Briscoe, W.H. PAMAM dendrimer—Cell membrane interactions. Adv. Colloid Interface Sci. 2018, 257, 1–18. [Google Scholar] [CrossRef]
- Liu, X.; Wu, J.; Yammine, M.; Zhou, J.; Posocco, P.; Viel, S.; Liu, C.; Ziarelli, F.; Fermeglia, M.; Pricl, S.; et al. Structurally flexible triethanolamine core pamam dendrimers are effective nanovectors for DNA transfection in vitro and in vivo to the mouse thymus. Bioconjugate Chem. 2011, 22, 2461–2473. [Google Scholar] [CrossRef]


| CTL Peptides | Th Peptides |
|---|---|
| KFINKLDALH | FKRTSFFLWVIILFQRTFSIPLGVIHNSTLQVSDVDKL |
| NYNGLLSSI | TNTNHFNMRTQRVKEQLSLKMLSLIRSNILKFINKLDA |
| PGPAKFSLL | LTLDNFLYYLTTQIHNLPHRSLRILKPTFKHASVMSRL |
| YFTFDLTALK | TQTYHFIRTAKGRITKLVNDYLKFFLIVQALKHNGTWQAE |
| LFLRATTEL | WDRQSLIMFITAFLNIALQLPCESSAVVVSGLRTLVPQSD |
| EYLFEVDNL | ESADSFLLMLCLHHAYQGDYKLFLESGAVKYLE |
| LYDRLASTV |
| Sample | Charge Ratio (N:P) | Zeta Potential, mV |
|---|---|---|
| pEV.CTL + PG | 2.5:1 | −5.0 ± 11.5 |
| pEV.Th + PG | 2.5:1 | −3.3 ± 20.9 |
| pEV.CTL + PAMAM | 3:1 | −27.3 ± 6.9 |
| pEV.Th + PAMAM | 3:1 | −9.6 ± 6.7 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Karpenko, L.I.; Apartsin, E.K.; Dudko, S.G.; Starostina, E.V.; Kaplina, O.N.; Antonets, D.V.; Volosnikova, E.A.; Zaitsev, B.N.; Bakulina, A.Y.; Venyaminova, A.G.; et al. Cationic Polymers for the Delivery of the Ebola DNA Vaccine Encoding Artificial T-Cell Immunogen. Vaccines 2020, 8, 718. https://doi.org/10.3390/vaccines8040718
Karpenko LI, Apartsin EK, Dudko SG, Starostina EV, Kaplina ON, Antonets DV, Volosnikova EA, Zaitsev BN, Bakulina AY, Venyaminova AG, et al. Cationic Polymers for the Delivery of the Ebola DNA Vaccine Encoding Artificial T-Cell Immunogen. Vaccines. 2020; 8(4):718. https://doi.org/10.3390/vaccines8040718
Chicago/Turabian StyleKarpenko, Larisa I., Evgeny K. Apartsin, Sergei G. Dudko, Ekaterina V. Starostina, Olga N. Kaplina, Denis V. Antonets, Ekaterina A. Volosnikova, Boris N. Zaitsev, Anastasiya Yu. Bakulina, Aliya G. Venyaminova, and et al. 2020. "Cationic Polymers for the Delivery of the Ebola DNA Vaccine Encoding Artificial T-Cell Immunogen" Vaccines 8, no. 4: 718. https://doi.org/10.3390/vaccines8040718
APA StyleKarpenko, L. I., Apartsin, E. K., Dudko, S. G., Starostina, E. V., Kaplina, O. N., Antonets, D. V., Volosnikova, E. A., Zaitsev, B. N., Bakulina, A. Y., Venyaminova, A. G., Ilyichev, A. A., & Bazhan, S. I. (2020). Cationic Polymers for the Delivery of the Ebola DNA Vaccine Encoding Artificial T-Cell Immunogen. Vaccines, 8(4), 718. https://doi.org/10.3390/vaccines8040718






