Trends, Coverage and Influencing Determinants of Influenza Vaccination in the Elderly: A Population-Based National Survey in Spain (2006–2017)
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Study Population
2.2. Variables
2.3. Procedure
2.4. Data Analysis
3. Results
3.1. Sociodemographic and Health-Related Variables
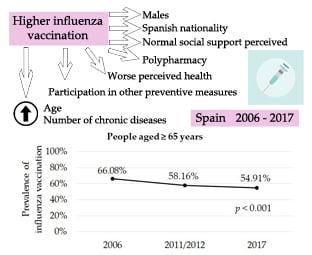
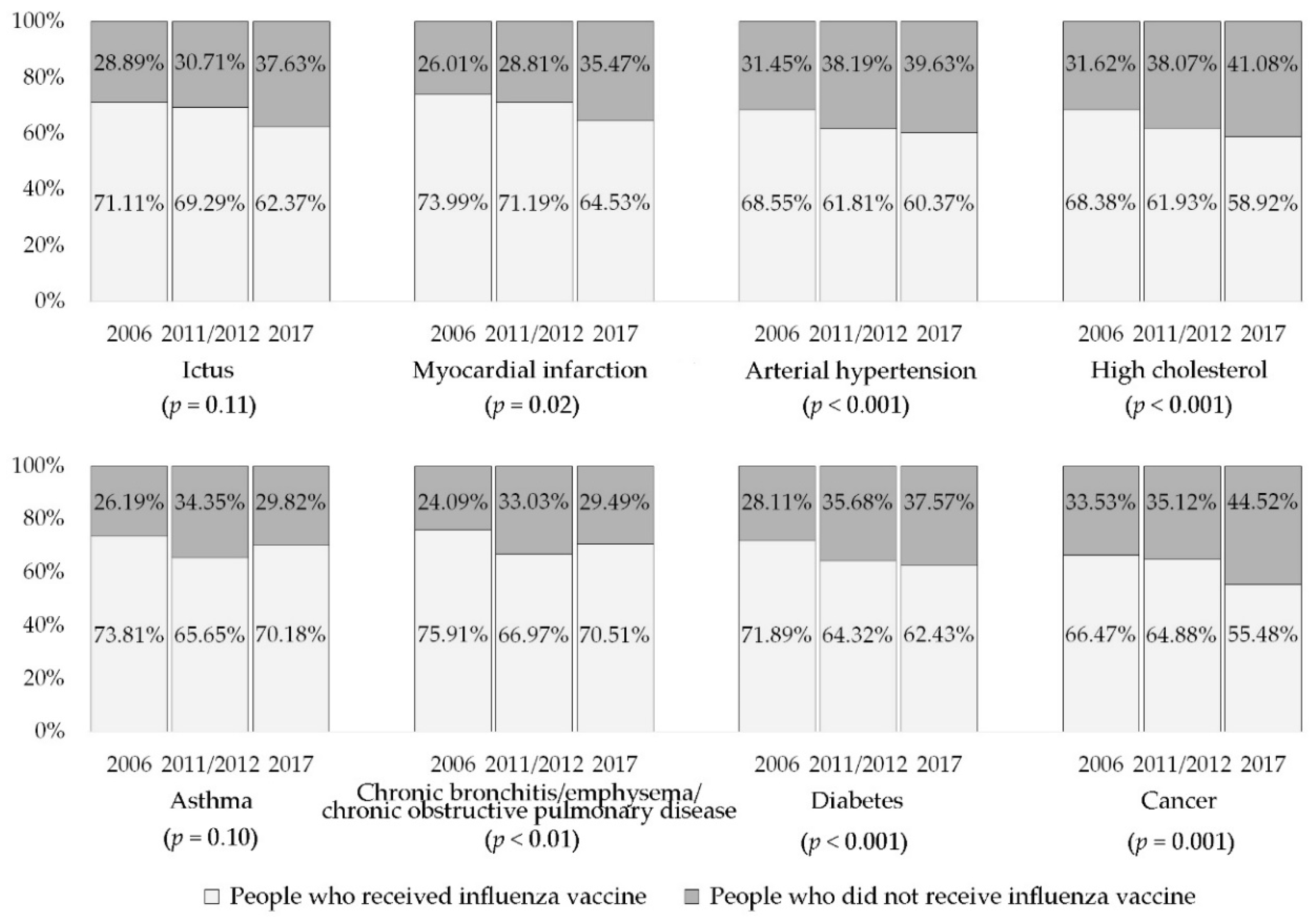
3.2. Influenza Vaccination
3.3. Association between Sociodemographic and Health-Related Variables and Influenza Vaccination
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization (WHO). Influenza—Estimating Burden of Disease 2020. Available online: http://www.euro.who.int/en/health-topics/communicable-diseases/influenza/seasonal-influenza/burden-of-influenza (accessed on 4 April 2020).
- World Health Organization (WHO). Seasonal Influenza Factsheet 2018. Available online: https://www.who.int/news-room/fact-sheets/detail/influenza-(seasonal) (accessed on 4 April 2020).
- Organisation for Economic Cooperation and Development (OECD). Health at Glance 2019: OECD Indicators. Available online: https://www.oecd-ilibrary.org/docserver/4dd50c09-en.pdf?expires=1587226533&id=id&accname=guest&checksum=DFF7AFD63AAFF499673E1EE4F9B17D1D (accessed on 4 April 2020).
- de Francisco Shapovalova, N.; Donadel, M.; Jit, M.; Hutubessy, R. A systematic review of the social and economic burden of influenza in low- and middle-income countries. Vaccine 2015, 33, 6537–6544. [Google Scholar] [CrossRef] [PubMed]
- Federici, C.; Cavazza, M.; Costa, F.; Jommi, C. Health care costs of influenza–related episodes in high income countries: A systematic review. PLoS ONE 2018, 13, e0202787. [Google Scholar] [CrossRef]
- Kassianos, G.; Blank, P.; Falup-Pecurariu, O.; Kuchar, E.; Kyncl, J.; De Lejarazu, R.O.; Nitsch-Osuch, A.; van Essen, G.A. Influenza vaccination: Key facts for general practitioners in Europe—A synthesis by European experts based on national guidelines and best practices in the United Kingdom and the Netherlands. Drugs Context 2016, 5, 212293. [Google Scholar] [CrossRef]
- Garten, R.; Blanton, L.; Abd Elal, A.I.; Alabi, N.; Barnes, J.; Biggerstaff, M.; Brammer, L.; Budd, A.P.; Burns, E.; Cummings, C.N.; et al. Update: Influenza Activity in the United States During the 2017–2018 Season and Composition of the 2018–2019 Influenza Vaccine. MMWR Morb. Mortal. Wkly. Rep. 2018, 67, 634–642. [Google Scholar] [CrossRef] [PubMed]
- Godoy, P.; Romero, A.; Soldevila, N.; Torner, N.; Jané, M.; Martínez, A.; Caylà, J.A.; Rius, C.; Domínguez, A. Influenza vaccine effectiveness in reducing severe outcomes over six influenza seasons, a case-case analysis, Spain, 2010/11 to 2015/16. Eurosurveillance 2018, 23. [Google Scholar] [CrossRef]
- Keshavarz, M.; Mirzaei, H.; Salemi, M.; Momeni, F.; Mousavi, M.J.; Sadeghalvad, M.; Arjeini, Y.; Solaymani-Mohammadi, F.; Sadri Nahand, J. Influenza vaccine: Where are we and where do we go? Rev. Med. Virol. 2019, 29, e2014. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control (ECDC). Seasonal Influenza Vaccination and Antiviral Use in EU/EEA Member States. An Overview of Vaccine Recommendations for 2017–2018 and Vaccination Coverage Rates for 2015–2016 and 2016–2017 Influenza Seasons. Available online: https://www.ecdc.europa.eu/sites/portal/files/documents/Seasonal-influenza-antiviral-use-EU-EEA-Member-States-December-2018_0.pdf (accessed on 26 February 2020).
- Ministry of Health of Spain. Influenza. Available online: https://www.mscbs.gob.es/ciudadanos/enfLesiones/enfTransmisibles/gripe/gripe.htm#prevencion (accessed on 5 April 2020).
- Dios Guerra, C.; Carmona Torres, J.M.; López Soto, P.J.; Morales Cané, I.; Rodríguez Borrego, M.A. Prevalence and factors associated with influenza vaccination of persons over 65 years old in Spain (2009–2014). Vaccine 2017, 35, 7095–7100. [Google Scholar] [CrossRef]
- Mira Iglesias, A.; López Labrador, F.X.; Guglieri López, B.; Tortajada Girbés, M.; Baselga Moreno, V.; Cano, L.; Mollar Maseres, J.; Carballido Fernández, M.; Schwarz Chavarri, G.; Díez Domingo, J.; et al. Influenza vaccine effectiveness in preventing hospitalisation of individuals 60 years of age and over with laboratory-confirmed influenza, Valencia Region, Spain, influenza season 2016/17. Eurosurveillance 2018, 23. [Google Scholar] [CrossRef] [PubMed]
- Interterritorial Board of the Spanish National Health System. Recommendations on Influenza Vaccination: Season 2019–2020. Available online: https://www.mscbs.gob.es/profesionales/saludPublica/prevPromocion/vacunaciones/docs/Recomendaciones_vacunacion_gripe.pdf (accessed on 5 April 2020).
- Eurostat. Elderly People Vaccinated against Influenza. Available online: https://ec.europa.eu/eurostat/web/products-eurostat-news/-/DDN-20191209-2 (accessed on 4 June 2020).
- Organisation for Economic Co-operation and Development. Influenza Vaccination Rates. Available online: https://data.oecd.org/healthcare/influenza-vaccination-rates.htm (accessed on 3 June 2020).
- Sarría Santamera, A.; Rodríguez Cabrera, F.; González Soriano, P.; Pinilla Navas, L.; Corral Canto, T. Determinantes de la vacunación de la gripe en personas de más de 65 años: 20 años no es nada. Rev. Esp. Salud Pública 2019, 93, e1–e9. [Google Scholar]
- Instituto Nacional de Estadística (INE). Indicadores de Estructura de la Población. Proporción de Personas Mayores de Cierta Edad por Provincia. Available online: https://www.ine.es/jaxiT3/Tabla.htm?t=1488&L=0 (accessed on 26 February 2020).
- Instituto Nacional de Estadística (INE). Proyecciones de Población 2018. Available online: https://www.ine.es/prensa/pp_2018_2068.pdf (accessed on 26 February 2020).
- Ministerio de Sanidad, Servicios Sociales e Igualdad, Instituto Nacional de Estadística. Encuesta Europea de Salud en España ENSE 2006; Ministerio de Sanidad, Servicios Sociales e Igualdad: Madrid, Spain, 2007. Available online: https://www.mscbs.gob.es/estadEstudios/estadisticas/encuestaNacional/encuesta2006.htm (accessed on 1 April 2020).
- Ministerio de Sanidad, Servicios Sociales e Igualdad, Instituto Nacional de Estadística. Encuesta Nacional de Salud España ENSE 2011/12; Ministerio de Sanidad, Servicios Sociales e Igualdad: Madrid, Spain, 2013. Available online: https://www.mscbs.gob.es/estadEstudios/estadisticas/encuestaNacional/encuesta2011.htm (accessed on 1 April 2020).
- Ministerio de Sanidad, Servicios Sociales e Igualdad, Instituto Nacional de Estadística. Encuesta Nacional de Salud España ENSE 2017; Ministerio de Sanidad, Servicios Sociales e Igualdad: Madrid, Spain, 2018. Available online: https://www.mscbs.gob.es/estadEstudios/estadisticas/encuestaNacional/encuesta2017.htm (accessed on 1 April 2020).
- Domingo-Salvany, A.; Bacigalupe, A.; Carrasco, J.M.; Espelt, A.; Ferrando, J.; Borrell, C. Proposals for social class classification based on the Spanish National Classification of Occupations 2011 using neo-Weberian and neo-Marxist approaches. Gac. Sanit. 2011, 27, 263–272. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Body Mass Index (BMI). Available online: http://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi (accessed on 1 April 2020).
- Eiras, A.; Teixeira, M.A.; González Montalvo, J.I.; Castell, M.V.; Queipo, R.; Otero, Á. Consumption of drugs in over 65 in Porto (Portugal) and risk of potentially inappropriate medication prescribing. Aten. Primaria 2016, 48, 110–120. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lopes, L.M.; Figueiredo, T.P.; Costa, S.C.; Reis, A.M. Use of potentially inappropriate medications by the elderly at home. Cien. Saude Colet. 2016, 21, 3429–3438. [Google Scholar] [CrossRef] [PubMed]
- Urfer, M.; Elzi, L.; Dell-Kuster, S.; Bassetti, S. Intervention to improve appropriate prescribing and reduce polypharmacy in elderly patients admitted to an Internal Medicine Unit. PLoS ONE 2016, 11, e0166359. [Google Scholar] [CrossRef] [PubMed]
- Masnoon, N.; Shakib, S.; Kalisch-Ellett, L.; Caughey, G.E. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017, 17, 230. [Google Scholar] [CrossRef]
- Broadhead, W.E.; Gehlbach, S.H.; Degruy, F.V.; Kaplan, B.H. The Duke-UNK functional social support questionnaire: Measurement of social support in family medicine patients. Med. Care 1988, 26, 709–723. [Google Scholar] [CrossRef] [PubMed]
- de la Revilla Ahumada, L.; Bailón, E.; de Dios Luna, J.; Delgado, A.; Prados, M.A.; Fleitas, L. Validación de una escala de apoyo social funcional para su uso en la consulta del médico de familia. Aten. Primaria 1991, 8, 688–692. [Google Scholar]
- Bellón Saameño, J.A.; Delgado Sánchez, A.; Luna del Castillo, J.D.; Lardelli Claret, P. Validity and reliability of the Duke-UNC-11 questionnaire of functional social support. Aten. Primaria 1996, 18, 153–156, 158–163. [Google Scholar]
- Ahlmark, N.; Holst Algren, M.; Holmberg, T.; Norredam, M.L.; Smith Nielsen, S.; Blom, A.B.; Bo, A.; Juel, K. Survey nonresponse among ethnic minorities in a national health survey—A mixed-method study of participation, barriers, and potentials. Ethn. Health 2015, 20, 611–632. [Google Scholar] [CrossRef]
- Gotsens, M.; Malmusi, D.; Villarroel, N.; Vives-Cases, C.; García-Subirats, I.; Hernando, C.; Borrel, C. Health inequality between immigrants and natives in Spain: The loss of the healthy immigrant effect in times of economic crisis. Eur. J. Public Health 2015, 25, 923–929. [Google Scholar] [CrossRef]
- González-Rábago, Y.; La Parra, D.; Martín, U.; Malmusi, D. Participation and Representation of the Immigrant Population in the Spanish National Health Survey 2011–2012. Gac. Sanit. 2014, 28, 281–286. [Google Scholar] [CrossRef]
- Eurostat. Vaccination against Influenza of Population Aged 65 and over. Available online: https://appsso.eurostat.ec.europa.eu/nui/show.do?dataset=hlth_ps_immu&lang=en (accessed on 3 June 2020).
- Braeye, T.; Emborg, H.-D.; Llorente-García, A.; Huerta, C.; Martín-Merino, E.; Duarte-Salles, T.; Danieli, G.; Tramontan, L.; Weibel, D.; McGee, C.; et al. Age-specific vaccination coverage estimates for influenza, human papillomavirus and measles containing vaccines from seven population-based healthcare databases from four EU countries–The ADVANCE project. Vaccine 2020, 38, 3243–3254. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Huedo, M.A.; López de Andrés, A.; Mora-Zamorano, E.; Hernández-Barrera, V.; Jiménez-Trujillo, I.; Zamorano-León, J.J.; Jiménez-García, R. Decreasing influenza vaccine coverage among adults with high-risk chronic diseases in Spain from 2014 to 2017. Hum. Vaccin. Immunother. 2020, 16, 95–99. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). European Health Information Gateway. Influenza Vaccination Recommendation, Elderly. Available online: https://gateway.euro.who.int/en/indicators/infl_1-influenza-vaccination-recommendation-elderly/visualizations/#id=31643 (accessed on 20 March 2020).
- Mereckiene, J.; Cotter, S.; Nicoll, A.; Lopalco, P.; Noori, T.; Weber, J.; D’Ancona, F.; Levy-Bruhl, D.; Dematte, L.; Giambi, C.; et al. Seasonal influenza immunisation in Europe. Overview of recommendations and vaccination coverage for three seasons: Pre-pandemic (2008/09), pandemic (2009/10) and post-pandemic (2010/11). Eurosurveillance 2014, 19, 20780. [Google Scholar] [CrossRef] [PubMed]
- Spruijt, I.T.; de Lange, M.M.A.; Dijkstra, F.; Donker, G.A.; van der Hoek, W. Long-Term correlation between influenza vaccination coverage and incidence of influenza-like illnessin 14 European countries. PloS ONE 2016, 11, e0163508. [Google Scholar] [CrossRef]
- Pariani, E.; Amendola, A.; Piatti, A.; Anselmi, G.; Ranghiero, A.; Bubba, L.; Rosa, A.M.; Pellegrinelli, L.; Binda, S.; Coppola, L.; et al. Ten years (2004–2014) of influenza surveillance in Northern Italy. Hum. Vaccin. Immunother. 2015, 11, 198–205. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Droogers, M.; Ciotti, M.; Kreidl, P.; Melidou, A.; Penttinen, P.; Sellwood, C.; Tsolova, S.; Snacken, R. European pandemic influenza preparedness planning: A review of national plans, July 2016. Disaster Med. Public Health Prep. 2019, 13, 582–592. [Google Scholar] [CrossRef]
- Schmid, P.; Rauber, D.; Betsch, C.; Lidolt, G.; Denker, M.L. Barriers of influenza vaccination intention and behavior—A systematic review of influenza vaccine hesitancy, 2005–2016. PLoS ONE 2017, 12, e0170550. [Google Scholar] [CrossRef] [PubMed]
- Jorgensen, P.; Mereckiene, J.; Cotter, S.; Johansen, K.; Tsolova, S.; Brown, C. How close are countries of the WHO European Region to achieving the goal of vaccinating 75% of key risk groups against influenza? Results from national surveys on seasonal influenza vaccination programmes, 2008/2009 to 2014/2015. Vaccine 2018, 36, 442–452. [Google Scholar] [CrossRef]
- Mesch, G.S.; Schwirian, K.P. Social and political determinants of vaccine hesitancy: Lessons learned fromthe H1N1 pandemic of 2009–2010. Am. J. Infect. Control 2015, 43, 1161–1165. [Google Scholar] [CrossRef]
- Bödeker, B.; Remschmidt, C.; Schmich, P.; Wichmann, O. Why are older adults and individuals with underlying chronic diseases in Germany not vaccinated against flu? A population-based study. BMC Public Health 2015, 15, 618. [Google Scholar] [CrossRef]
- Mo, P.K.; Lau, J.T. Influenza vaccination uptake and associated factors among elderly population in Hong Kong: The application of the Health Belief Model. Health Educ. Res. 2015, 30, 706–718. [Google Scholar] [CrossRef] [PubMed]
- Chan, D.P.; Wong, N.S.; Wong, E.L.; Cheung, A.W.; Lee, S.S. Household characteristics and influenza vaccination uptake in the community-dwelling elderly: A cross-sectional study. Prev. Med. Rep. 2015, 2, 803–808. [Google Scholar] [CrossRef] [PubMed]
- Domínguez, À.; Soldevila, N.; Toledo, D.; Godoy, P.; Castilla, J.; Force, L.; Morales, M.; Mayoral, J.M.; Egurrola, M.; Tamames, S.; et al. Factors associated with influenza vaccination of hospitalized elderly patients in Spain. PLoS ONE 2016, 11, e0147931. [Google Scholar] [CrossRef]
- Kwon, D.S.; Kim, K.; Park, S.M. Factors associated with influenza vaccination coverage among the elderly in South Korea: The Fourth Korean National Health and Nutrition Examination Survey (KNHANES IV). BMJ Open 2016, 6, e012618. [Google Scholar] [CrossRef] [PubMed]
- Kan, T.; Zhang, J. Factors influencing seasonal influenza vaccination behaviour among elderly people: A systematic review. Public Health 2018, 156, 67–78. [Google Scholar] [CrossRef] [PubMed]
- Ganczak, M.; Gil, K.; Korzeń, M.; Bażydło, M. Coverage and influencing determinants of influenza vaccination in elderly patients in a country with a poor vaccination implementation. Int. J. Environ. Res. Public Health 2017, 14, 665. [Google Scholar] [CrossRef]
- Astray Mochales, J.; López de Andrés, A.; Hernández Barrera, V.; Rodríguez Rieiro, C.; Carrasco Garrido, P.; Esteban Vasallo, M.D.; Domínguez Berjón, M.F.; Jiménez Trujillo, I.; Jiménez García, R. Influenza vaccination coverages among high risk subjects and health care workers in Spain. Results of two consecutive National Health Surveys (2011–2014). Vaccine 2016, 34, 4898–4904. [Google Scholar] [CrossRef]
- Abbas, K.M.; Kang, G.J.; Chen, D.; Werre, S.R.; Marathe, A. Demographics, perceptions, and socioeconomic factors affecting influenza vaccination among adults in the United States. PeerJ 2018, 6, e5171. [Google Scholar] [CrossRef]
- Crouse Quinn, S.; Jamison, A.M.; Freimuth, V.S.; An, J.; Hancock, G.R. Determinants of influenza vaccination among high-risk black and white adults. Vaccine 2017, 35, 7154–7159. [Google Scholar] [CrossRef]
- de Bekker-Grob, E.W.; Veldwijk, J.; Jonker, M.; Donkers, B.; Huisman, J.; Buis, S.; Swait, J.; Lancsar, E.; Witteman, C.L.M.; Bonsel, G.; et al. The impact of vaccination and patient characteristics on influenza vaccination uptake of elderly people: A discrete choice experiment. Vaccine 2018, 36, 1467–1476. [Google Scholar] [CrossRef]
- Winters, M.; Rechel, B.; de Jong, L.; Pavlova, M. A systematic review on the use of healthcare services by undocumented migrants in Europe. BMC Health Serv. Res. 2018, 18, 30. [Google Scholar] [CrossRef] [PubMed]
- Briggs, L.; Fronek, P.; Quinn, V.; Wilde, T. Perceptions of influenza and pneumococcal vaccine uptake by older persons in Australia. Vaccine 2019, 37, 4454–4459. [Google Scholar] [CrossRef]
- Damiani, G.; Federico, B.; Visca, M.; Agostini, F.; Ricciardi, W. The impact of socioeconomic level on influenza vaccination among Italian adults and elderly: A cross-sectional study. Prev. Med. 2007, 45, 373–379. [Google Scholar] [CrossRef]
- Taheri Tanjani, P.; Babanejad, M.; Najafi, F. Influenza vaccination uptake and its socioeconomic determinants in the older adult Iranian population: A national study. Am. J. Infect. Control 2015, 43, e1–e5. [Google Scholar] [CrossRef]
- Dardalas, I.; Pourzitaki, C.; Manomenidis, G.; Malliou, F.; Galanis, P.; Papazisis, G.; Kouvelas, D.; Bellali, T. Predictors of influenza vaccination among elderly: A cross-sectional survey in Greece. Aging Clin. Exp. Res. 2019. [Google Scholar] [CrossRef] [PubMed]
- Machado, A.; Santos, A.J.; Kislaya, I.; Larrauri, A.; Nunes, B. Understanding influenza vaccination among Portuguese elderly: The social ecological framework. Health Promot. Int. 2020, daaa011. [Google Scholar] [CrossRef] [PubMed]
- López Valcárcel, B.G.; Barber, P. Economic crisis, austerity policies, health and fairness: Lessons learned in Spain. Appl. Health Econ. Health Policy 2017, 15, 13–21. [Google Scholar] [CrossRef]
- Encuentro Foundation. Spain Report 2015. Available online: https://blogs.comillas.edu/informeespana/wp-content/uploads/sites/93/2019/05/IE2015Cap18.pdf (accessed on 9 June 2020).
- Vukovic, V.; Lillini, R.; Asta, F.; Chini, F.; de Waure, C. Analysis of influenza vaccination coverage among the elderly living in Rome, based on a deprivation index, 2009–2013. J. Prev. Med. Hyg. 2019, 59, e31–e37. [Google Scholar] [CrossRef]
- Cano Gutiérrez, C.; Reyes Ortiz, C.; Borda, M.G.; Arciniegas, A. Self-reported vaccination in the elderly: SABE Bogota study, Colombia. Colomb. Med. (Cali) 2016, 47, 25–30. [Google Scholar] [CrossRef]
- Lv, M.; Fang, R.; Wu, J.; Pang, X.; Deng, Y.; Lei, T.; Xie, Z. The free vaccination policy of influenza in Beijing, China: The vaccine coverage and its associated factors. Vaccine 2016, 34, 2135–2140. [Google Scholar] [CrossRef]
- Harris, J.A.; Moniz, M.H.; Lott, B.; Power, R.; Griggs, J.J. Obesity and the receipt of influenza and pneumococcal vaccination: A systematic review and meta-analysis. BMC Obes. 2016, 3, 24. [Google Scholar] [CrossRef]
- Klett, C.J.; Krause, G.; Seefeld, L.; Ott, J.J. Determinants of tetanus, pneumococcal and influenza vaccination in the elderly: A representative cross-sectional study on knowledge, attitude and practice (KAP). BMC Public Health 2016, 16, 121. [Google Scholar] [CrossRef]
- Teloniatis, S.; Tzortzi, A.; Behrakis, P. Seasonal influenza vaccination coverage in Greece in 2009 and 2014. Pneumon 2017, 30, 41–48. [Google Scholar]
- Roy, M.; Sherrard, L.; Dubé, È.; Gilbert, N.L. Determinants of non-vaccination against seasonal influenza. Health Rep. 2018, 29, 12–22. [Google Scholar] [PubMed]
- Sato, A.P.; Antunes, J.L.; Moura, R.F.; de Andrade, F.B.; Duarte, Y.A.; Lebrão, M.L. Factors associated to vaccination against influenza among elderly in a large Brazilian metropolis. PLoS ONE 2015, 10, e0123840. [Google Scholar] [CrossRef] [PubMed]
- Assaf, A.M.; Hammad, E.A.; Haddadin, R.N. Influenza vaccination coverage rates, knowledge, attitudes, and beliefs in Jordan: A comprehensive study. Viral Immunol. 2016, 29, 516–525. [Google Scholar] [CrossRef]
- Nitsch-Osuch, A.; Gołębiak, I.; Wyszkowska, D.; Rosińska, R.; Kargul, L.; Szuba, B.; Tyszko, P.; Brydak, L.B. Influenza vaccination coverage among Polish patients with chronic diseases. Adv. Exp. Med. Biol. 2017, 968, 19–34. [Google Scholar] [CrossRef] [PubMed]
- Restrepo, M.I.; Sibila, O.; Anzueto, A. Pneumonia in patients with chronic obstructive pulmonary disease. Tuberc. Respir. Dis. (Seoul) 2018, 81, 187–197. [Google Scholar] [CrossRef]
- Buchan, S.A.; Kwong, J.C. Trends in influenza vaccine coverage and vaccine hesitancy in Canada, 2006/07 to 2013/14: Results from cross-sectional survey data. CMAJ Open 2016, 4, E455–E462. [Google Scholar] [CrossRef]
- Andrew, M.K.; Shinde, V.; Ye, L.; Hatchette, T.; Haguinet, F.; Dos Santos, G.; McElhaney, J.E.; Ambrose, A.; Boivin, G.; Bowie, W.; et al. The importance of frailty in the assessment of influenza vaccine effectiveness against influenza-related hospitalization in elderly people. J. Infect. Dis. 2017, 216, 405–414. [Google Scholar] [CrossRef]
- Kopsaftis, Z.; Wood-Baker, R.; Poole, P. Influenza vaccine for chronic obstructive pulmonary disease (COPD). Cochrane Database Syst. Rev. 2018, 6, CD002733. [Google Scholar] [CrossRef] [PubMed]
- Bitterman, R.; Eliakim-Raz, N.; Vinograd, I.; Zalmanovici Trestioreanu, A.; Leibovici, L.; Paul, M. Influenza vaccines in immunosuppressed adults with cancer. Cochrane Database Syst. Rev. 2018, 2, CD008983. [Google Scholar] [CrossRef] [PubMed]
- Poeppl, W.; Lagler, H.; Raderer, M.; Sperr, W.R.; Zielinski, C.; Herkner, H.; Burgmann, H. Influenza vaccination perception and coverage among patients with malignant disease. Vaccine 2015, 33, 1682–1687. [Google Scholar] [CrossRef] [PubMed]
- Interterritorial Council of the Spanish National Health Service. Recommendations for Vaccination against Influenza Virus (season 2020–2021). Available online: https://www.mscbs.gob.es/eu/profesionales/saludPublica/prevPromocion/vacunaciones/docs/Recomendaciones_vacunacion_gripe.pdf (accessed on 9 June 2020).
- Dabestani, N.M.; Leidner, A.J.; Seiber, E.E.; Kim, H.; Graitcer, S.B.; Foppa, I.M.; Bridges, C.B. A review of the cost-effectiveness of adult influenza vaccination and other preventive services. Prev. Med. 2019, 126, 105734. [Google Scholar] [CrossRef] [PubMed]
- Dirmesropian, S.; Wood, J.G.; MacIntyre, C.R.; Beutels, P.; Newall, A.T. Economic evaluation of vaccination programmes in older adults and the elderly: Important issues and challenges. Pharmacoeconomics 2016, 34, 723–731. [Google Scholar] [CrossRef] [PubMed]
- Na, L.; Hennessy, S.; Bogner, H.R.; Kurichi, J.E.; Stineman, M.; Streim, J.E.; Kwong, P.L.; Xie, D.; Pezzin, L.E. Disability stage and receipt of recommended care among elderly medicare beneficiaries. Disabil. Health J. 2017, 10, 48–57. [Google Scholar] [CrossRef][Green Version]
- Bock, J.O.; Hajek, A.; König, H.H. Psychological determinants of influenza vaccination. BMC Geriatr. 2017, 17, 194. [Google Scholar] [CrossRef]
- Yeung, M.P.; Lam, F.L.; Coker, R. Factors associated with the uptake of seasonal influenza vaccination in adults: A systematic review. J. Public Health (Oxf.) 2016, 38, 746–753. [Google Scholar] [CrossRef]
- Laranjo, L.; Arguel, A.; Neves, A.L.; Gallagher, A.M.; Kaplan, R.; Mortimer, N.; Mendes, G.A.; Lau, A.Y. The influence of social networking sites on health behavior change: A systematic review and meta-analysis. J. Am. Med. Inform. Assoc. 2015, 22, 243–256. [Google Scholar] [CrossRef]
- Ziegelmann, J.P.; Knoll, N. Future directions in the study of health behavior among older adults. Gerontology 2015, 61, 469–476. [Google Scholar] [CrossRef]
- Rosenstock, I.M. Historical origins of the health belief model. Health Educ. Monogr. 1974, 2, 328–335. [Google Scholar] [CrossRef]
- Doherty, T.M.; Connolly, M.P.; Del Giudice, G.; Flamaing, J.; Goronzy, J.J.; Grubeck-Loebenstein, B.; Lambert, P.H.; Maggi, S.; McElhaney, J.E.; Nagai, H.; et al. Vaccination programs for older adults in an era of demographic change. Eur. Geriatr. Med. 2018, 9, 289–300. [Google Scholar] [CrossRef] [PubMed]
- Bonanni, P.; Picazo, J.J.; Rémy, V. The intangible benefits of vaccination–what is the true economic value of vaccination? J. Mark Access Health Policy 2015, 3, 26964. [Google Scholar] [CrossRef] [PubMed]
- Thomas, R.E.; Lorenzetti, D.L. Interventions to increase influenza vaccination rates of those 60 years and older in the community. Cochrane Database Syst. Rev. 2014, 7, CD005188. [Google Scholar] [CrossRef]
| Variables | 2006 | 2011/2012 | 2017 | p-Value |
|---|---|---|---|---|
| n = 7835 (%) | n = 5896 (%) | n = 7022 (%) | ||
| Gender | <0.001 | |||
| Female | 5022 (64.10) | 3673 (62.30) | 4173 (59.43) | |
| Male | 2813 (35.90) | 2223 (37.70) | 2849 (40.57) | |
| Age group | <0.001 | |||
| 65–74 years | 3931 (50.17) | 2731 (46.32) | 3382 (48.16) | |
| 75–84 years | 3157 (40.30) | 2350 (39.86) | 2543 (36.22) | |
| ≥85 years | 747 (9.53) | 815 (13.82) | 1097 (15.62) | |
| Nationality | <0.001 | |||
| Spanish | 7736 (98.74) | 5826 (98.81) | 7016 (99.91) | |
| Foreigner | 71 (0.91) | 69 (1.17) | 2 (0.03) | |
| Do not know/answer | 28 (0.35) | 1 (0.02) | 4 (0.06) | |
| Level of education | <0.001 | |||
| University | 522 (6.66) | 325 (5.51) | 634 (9.03) | |
| Secondary or PT | 4388 (56.00) | 1882 (31.92) | 1638 (23.33) | |
| Primary | 2428 (30.99) | 1374 (23.30) | 2614 (37.22) | |
| Without studies | 473 (6.04) | 2315 (39.27) | 2136 (30.42) | |
| Do not know/answer | 24 (0.31) | 0 (0.00) | 0 (0.00) | |
| Marital status | <0.001 | |||
| Single | 773 (9.87) | 489 (8.29) | 572 (8.14) | |
| Married | 3886 (49.60) | 2912 (49.39) | 3566 (50.78) | |
| Widowed | 2991 (38.17) | 2310 (39.18) | 2567 (36.56) | |
| Separated/Divorced | 174 (2.22) | 180 (3.05) | 306 (4.36) | |
| Do not know/answer | 11 (0.14) | 5 (0.09) | 11 (0.16) | |
| Social class | <0.001 | |||
| Classes I and II | 938 (11.97) | 726 (12.31) | 924 (13.16) | |
| Classes III and IV | 4247 (54.21) | 1690 (28.66) | 2284 (32.53) | |
| Classes V and VI | 2330 (29.74) | 3097 (52.53) | 3480 (49.56) | |
| Do not know/answer | 320 (4.08) | 383 (6.50) | 334 (4.75) | |
| Size of town of residence | <0.001 | |||
| >100,000 inhabitants | 2810 (35.87) | 2425 (41.13) | 2894 (41.21) | |
| 10,000–100,000 inhabitants | 2379 (30.36) | 1743 (29.56) | 2260 (32.19) | |
| <10,000 inhabitants | 2646 (33.77) | 1728 (29.31) | 1868 (26.60) | |
| Body Mass Index | <0.001 | |||
| Underweight | 64 (0.82) | 47 (0.80) | 72 (1.02) | |
| Normal weight | 1738 (22.18) | 1370 (23.23) | 1978 (28.17) | |
| Overweight | 2784 (35.53) | 2116 (35.89) | 2840 (40.44) | |
| Obese | 1387 (17.70) | 1158 (19.64) | 1487 (21.18) | |
| Do not know/answer | 1862 (23.77) | 1205 (20.44) | 645 (9.19) | |
| Self-perceived health | <0.001 | |||
| Very good | 430 (5.49) | 359 (6.09) | 441 (6.28) | |
| Good | 2581 (32.94) | 2205 (37.40) | 2745 (39.09) | |
| Fair | 3299 (42.11) | 2175 (36.89) | 2592 (36.92) | |
| Poor | 1177 (15.02) | 915 (15.52) | 977 (13.91) | |
| Very poor | 348 (4.44) | 242 (4.10) | 267 (3.80) | |
| Presence of chronic conditions | <0.001 | |||
| None | 394 (5.03) | 360 (6.11) | 347 (4.94) | |
| 1–2 | 1842 (23.51) | 1395 (23.66) | 1500 (21.36) | |
| ≥3 | 5599 (71.46) | 4141 (70.23) | 5175 (73.70) | |
| Blood cholesterol measurement | <0.001 | |||
| No | 379 (4.84) | 317 (5.38) | 49 (0.70) | |
| Yes | 7259 (92.65) | 5555 (94.21) | 6966 (99.20) | |
| Do not know/answer | 197 (2.51) | 24 (0.41) | 7 (0.10) | |
| Blood pressure measurement | <0.001 | |||
| No | 89 (1.14) | 123 (2.09) | 38 (0.54) | |
| Yes | 7632 (97.41) | 5770 (97.86) | 6982 (99.43) | |
| Do not know/answer | 114 (1.45) | 3 (0.05) | 2 (0.03) | |
| Degree of limitation due to a health problem for at least 6 months | <0.001 | |||
| Not at all limited | 4468 (57.03) | 3562 (60.42) | 3530 (50.27) | |
| Limited but not severely | 2565 (32.74) | 1757 (29.80) | 2734 (38.94) | |
| Severely limited | 802 (10.23) | 575 (9.75) | 757 (10.78) | |
| Do not know/answer | 0 (0.00) | 2 (0.03) | 1 (0.01) | |
| Social support | <0.001 | |||
| Low social support | 347 (4.43) | 251 (4.26) | 400 (5.70) | |
| Normal social support | 7040 (89.85) | 5206 (88.30) | 6588 (93.82) | |
| Do not know/answer | 448 (5.72) | 439 (7.44) | 34 (0.48) | |
| Polypharmacy | <0.001 | |||
| Yes | 1570 (20.04) | 1426 (24.19) | 1901 (27.07) | |
| No | 6208 (79.23) | 4432 (75.17) | 5093 (72.53) | |
| Do not know/answer | 57 (0.73) | 38 (0.64) | 28 (0.40) |
| Variables | 2006 | 2011/2012 | 2017 | Total | OR (CI 95%) | p-Value | ORa (CI 95%) | p-Value |
|---|---|---|---|---|---|---|---|---|
| n = 5177 (%) | n = 3429 (%) | n = 3856 (%) | n = 12,462 (%) | |||||
| Gender | ||||||||
| Female | 3263 (63.03) | 2122 (61.88) | 2238 (58.04) | 7623 (61.17) | Reference | Reference | ||
| Male | 1914 (36.97) | 1307 (38.12) | 1618 (41.96) | 4839 (38.83) | 1.09 (1.03–1.16) | <0.01 | 1.32 (1.23–1.41) | <0.001 |
| Age group | ||||||||
| 65–74 years | 2312 (44.66) | 1339 (39.05) | 1520 (39.42) | 5171 (41.49) | Reference | Reference | ||
| 75–84 years | 2307 (44.56) | 1541 (44.94) | 1614 (41.86) | 5462 (43.83) | 1.99 (1.87–2.11) | <0.001 | 1.87 (1.74–2.02) | <0.001 |
| ≥85 years | 558 (10.78) | 549 (16.01) | 722 (18.72) | 1829 (14.68) | 2.08 (1.90–2.27) | <0.001 | 2.08 (1.85–2.34) | <0.001 |
| Nationality | ||||||||
| Spanish | 5128 (99.05) | 3399 (99.13) | 3854 (99.95) | 12,381 (99.35) | Reference | |||
| Foreigner | 30 (0.58) | 30 (0.87) | 0 (0.00) | 60 (0.48) | 0.42 (0.19–0.92) | <0.01 | Reference | |
| Do not know/answer | 19 (0.37) | 0 (0.00) | 2 (0.05) | 21 (0.17) | 0.86 (0.42–0.93) | <0.01 | 0.61 (0.41–0.90) | 0.01 |
| Level of education | ||||||||
| University | 312 (6.03) | 156 (4.55) | 321 (8.33) | 789 (6.33) | Reference | |||
| Secondary or PT | 2872 (55.48) | 1056 (30.80) | 800 (20.75) | 4728 (37.94) | 1.21 (1.14–1.48) | <0.001 | ||
| Primary | 1645 (31.77) | 831 (24.23) | 1440 (37.34) | 3916 (31.42) | 1.11 (1.08–1.62) | <0.001 | ||
| Without studies | 332 (6.41) | 1386 (40.42) | 1295 (33.58) | 3013 (24.18) | 1.13 (1.04–1.51) | <0.001 | ||
| Do not know/answer | 16 (0.31) | 0 (0.00) | 0 (0.00) | 16 (0.13) | 1.27 (1.11–1.92) | <0.001 | ||
| Marital status | ||||||||
| Single | 462 (8.92) | 290 (8.46) | 309 (8.01) | 1061 (8.51) | Reference | |||
| Married | 2609 (50.40) | 1680 (48.99) | 1972 (51.14) | 6261 (50.24) | 1.12 (0.99–1.23) | 0.06 | ||
| Widowed | 2012 (38.86) | 1385 (40.39) | 1433 (37.17) | 4830 (38.76) | 1.16 (1.05–1.28) | 0.01 | ||
| Separated/Divorced | 90 (1.74) | 71 (2.07) | 140 (3.63) | 301 (2.42) | 0.61 (0.51–0.73) | <0.001 | ||
| Do not know/answer | 4 (0.08) | 3 (0.09) | 2 (0.05) | 9 (0.07) | 0.36 (0.16–0.82) | 0.01 | ||
| Social class | ||||||||
| Classes I and II | 617 (11.92) | 379 (11.05) | 470 (12.19) | 1466 (11.76) | Reference | |||
| Classes III and IV | 2830 (54.67) | 994 (28.99) | 1231 (31.92) | 5055 (40.56) | 1.22 (1.12–1.33) | <0.001 | ||
| Classes V and VI | 1532 (29.59) | 1840 (53.66) | 1970 (51.09) | 5342 (42.87) | 1.15 (1.05–1.25) | 0.01 | ||
| Do not know/answer | 198 (3.82) | 216 (6.30) | 185 (4.80) | 599 (4.81) | 1.04 (0.91–1.21) | 0.54 | ||
| Size of town of residence | ||||||||
| >100,000 inhabitants | 1805 (34.87) | 1379 (40.22) | 1522 (39.47) | 4706 (37.76) | Reference | |||
| 10,000–100,000 inhabitants | 1530 (29.55) | 992 (28.93) | 1200 (31.12) | 3722 (29.87) | 1.02 (0.95–1.09) | 0.6 | ||
| <10,000 inhabitants | 1842 (35.58) | 1058 (30.85) | 1134 (29.41) | 4034 (32.37) | 1.33 (1.24–1.42) | <0.001 | ||
| Body Mass Index | ||||||||
| Underweight | 41 (0.79) | 25 (0.73) | 34 (0.88) | 100 (0.80) | Reference | |||
| Normal weight | 1111 (21.46) | 767 (22.37) | 1047 (27.15) | 2925 (23.47) | 0.82 (0.58–1.19) | 0.16 | ||
| Overweight | 1819 (35.14) | 1228 (35.81) | 1580 (40.98) | 4627 (37.13) | 1.11 (1.07–1.21) | 0.01 | ||
| Obese | 924 (17.85) | 689 (20.09) | 834 (21.63) | 2447 (19.64) | 1.13 (1.04–1.25) | 0.01 | ||
| Do not know/answer | 1282 (24.76) | 720 (21.00) | 361 (9.36) | 2363 (18.96) | 1.28 (0.95- 1.73) | 0.1 | ||
| Self-perceived health | ||||||||
| Very good | 227 (4.38) | 153 (4.46) | 169 (4.38) | 549 (4.41) | Reference | Reference | ||
| Good | 1594 (30.79) | 1170 (34.12) | 1364 (35.37) | 4128 (33.12) | 1.51 (1.33–1.70) | <0.001 | 1.31 (1.14–1.52) | <0.001 |
| Fair | 2305 (44.52) | 1371 (39.98) | 1560 (40.46) | 5236 (42.02) | 2.30 (2.03–2.60) | <0.001 | 1.56 (1.35–1.81) | <0.001 |
| Poor | 812 (15.69) | 591 (17.24) | 585 (15.17) | 1988 (15.95) | 2.28 (1.99–2.61) | <0.001 | 1.37 (1.16–1.62) | <0.001 |
| Very poor | 239 (4.62) | 144 (4.20) | 178 (4.62) | 561 (4.50) | 2.35 (1.96–2.82) | <0.001 | 1.43 (1.13–1.80) | <0.01 |
| Presence of chronic diseases | ||||||||
| None | 159 (3.07) | 140 (4.08) | 99 (2.57) | 398 (3.19) | Reference | Reference | ||
| 1–2 | 1058 (20.44) | 672 (19.60) | 661 (17.14) | 2391 (19.19) | 1.80 (1.57–2.06) | <0.001 | 1.57 (1.33–1.84) | <0.001 |
| ≥3 | 3960 (76.49) | 2617 (76.32) | 3096 (80.29) | 9673 (77.62) | 3.24 (2.87–3.70) | <0.001 | 2.31 (1.97–2.71) | <0.001 |
| Blood cholesterol measurement | ||||||||
| No | 186 (3.59) | 126 (3.67) | 17 (0.44) | 329 (2.64) | Reference | |||
| Yes | 4887 (94.40) | 3291 (95.98) | 3839 (99.56) | 12,017 (96.43) | 1.96 (1.69–2.27) | <0.001 | Reference | |
| Do not know/answer | 104 (2.01) | 12 (0.35) | 0 (0.00) | 116 (0.93) | 1.31 (0.97–1.76) | 0.08 | 1.33 (1.10–1.61) | <0.01 |
| Blood pressure measurement | ||||||||
| No | 34 (0.66) | 36 (1.05) | 10 (0.26) | 80 (0.64) | Reference | |||
| Yes | 5093 (98.38) | 3392 (98.92) | 3846 (99.74) | 12,331 (98.95) | 3.25 (2.49–4.25) | <0.001 | Reference | |
| Do not know/answer | 50 (0.96) | 1 (0.03) | 0 (0.00) | 51 (0.41) | 1.59 (1.02–2.50) | 0.04 | 1.70 (1.20–2.40) | <0.01 |
| Degree of limitation due to a health problem for at least 6 months | ||||||||
| Not at all limited | 2816 (54.40) | 1945 (56.72) | 1730 (44.87) | 6491 (52.08) | Reference | |||
| Limited but not severely | 1778 (34.34) | 1117 (32.58) | 1642 (42.58) | 4537 (36.41) | 1.49 (1.32–1.78) | <0.001 | ||
| Severely limited | 583 (11.26) | 366 (10.67) | 484 (12.55) | 1433 (11.50) | 1.44 (1.27–1.62) | <0.001 | ||
| Do not know/answer | 0 (0.00) | 1 (0.03) | 0 (0.00) | 1 (0.01) | 1.50 (0.37–1.21) | 0.1 | ||
| Social support | ||||||||
| Low social support | 212 (4.09) | 125 (3.65) | 204 (5.29) | 541 (4.34) | Reference | |||
| Normal social support | 4670 (90.21) | 3043 (88.74) | 3635 (94.27) | 11,348 (91.06) | 1.28 (1.13–1.46) | <0.001 | Reference | |
| Do not know/answer | 295 (5.70) | 261 (7.61) | 17 (0.44) | 573 (4.60) | 1.39 (1.16–1.67) | <0.001 | 1.41 (1.19–1.67) | <0.001 |
| Polypharmacy | ||||||||
| No | 3959 (76.47) | 2440 (71.16) | 2598 (67.38) | 8997 (72.19) | Reference | |||
| Yes | 1181 (22.81) | 963 (28.08) | 1238 (32.10) | 3382 (27.14) | 1.67 (1.56–1.79) | <0.001 | Reference | |
| Do not know/answer | 37 (0.72) | 26 (0.76) | 20 (0.52) | 83 (0.67) | 1.55 (1.06–2.27) | 0.02 | 1.32 (1.21–1.45) | < 0.001 |
| Country | Year | Influenza Vaccination Coverage Rate in Older People |
|---|---|---|
| Netherlands [35] | 2006 | 76% |
| 2011/2012 | 73.50% | |
| 2013 | 68.80% | |
| 2017 | 64% | |
| Italy [35] | 2006 | 68.35% |
| 2011/2012 | 60.23% | |
| 2014/2015 | 55.45% | |
| 2017 | 52% | |
| Portugal [35] | 2006 | 50.40% |
| 2011/2012 | 43.40% | |
| 2015 | 50.10% | |
| 2017 | 60.80% | |
| Spain [36,37] | 2009/2010 | 58% |
| 2014 | 56.20% | |
| 2017 | 55.70% | |
| Denmark [36] | 2009/2010 | 48.50% |
| United Kingdom [36] | 2011/2012 | 74% |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Portero de la Cruz, S.; Cebrino, J. Trends, Coverage and Influencing Determinants of Influenza Vaccination in the Elderly: A Population-Based National Survey in Spain (2006–2017). Vaccines 2020, 8, 327. https://doi.org/10.3390/vaccines8020327
Portero de la Cruz S, Cebrino J. Trends, Coverage and Influencing Determinants of Influenza Vaccination in the Elderly: A Population-Based National Survey in Spain (2006–2017). Vaccines. 2020; 8(2):327. https://doi.org/10.3390/vaccines8020327
Chicago/Turabian StylePortero de la Cruz, Silvia, and Jesús Cebrino. 2020. "Trends, Coverage and Influencing Determinants of Influenza Vaccination in the Elderly: A Population-Based National Survey in Spain (2006–2017)" Vaccines 8, no. 2: 327. https://doi.org/10.3390/vaccines8020327
APA StylePortero de la Cruz, S., & Cebrino, J. (2020). Trends, Coverage and Influencing Determinants of Influenza Vaccination in the Elderly: A Population-Based National Survey in Spain (2006–2017). Vaccines, 8(2), 327. https://doi.org/10.3390/vaccines8020327