HPV Vaccination as Adjuvant to Conization in Women with Cervical Intraepithelial Neoplasia: A Study under Real-Life Conditions
Abstract
1. Introduction
2. Methods
2.1. Selection Criteria
2.2. Criteria for Treatment and Post-Treatment Follow-Up
2.3. Liquid-Based Cytology and HPV Testing
2.4. Histological Diagnosis of Colposcopy-Directed Biopsy
2.5. Cervical Conization and Histological Diagnosis
2.6. HPV Vaccination Policy
2.7. Clinical Outcome Six Months after Conization
2.8. Clinical Outcome at the End of the Follow-Up
3. Data Analysis
4. Results
4.1. General Characteristics of the Women Included in the Study
4.2. Characteristics of Vaccinated and Non-Vaccinated Women
4.3. Vaccination Compliance and Vaccination Scheme
4.4. Results of the First Post-Conization Control
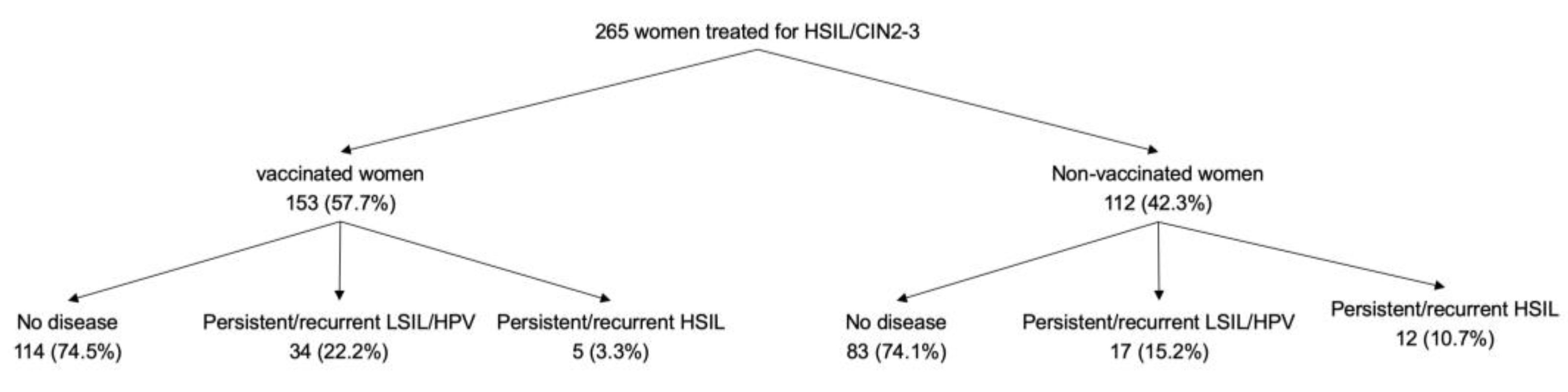
4.5. Clinical Outcome at the End of Follow-Up
5. Discussion
6. Conclusions
7. Ethical Approval
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Martin-Hirsch, P.P.; Paraskevaidis, E.; Bryant, A.; Dickinson, H.O.; Keep, S.L. Surgery for cervical intraepithelial neoplasia. Cochrane Database Syst. Rev. 2010. [Google Scholar] [CrossRef]
- Kocken, M.; Uijterwaal, M.H.; de Vries, A.L.M.; Berkhof, J.; Ket, J.C.F.; Helmerhorst, T.J.M.; Meijer, C.J.L.M. High-risk human papillomavirus testing versus cytology in predicting post-treatment disease in women treated for high-grade cervical disease: A systematic review and meta-analysis. Gynecol. Oncol. 2012, 125, 500–507. [Google Scholar] [CrossRef] [PubMed]
- Uijterwaal, M.H.; Kocken, M.; Berkhof, J.; Bekkers, R.L.M.; Verheijen, R.H.M.; Helmerhorst, T.J.M.; Meijer, C.J.L.M. Posttreatment assessment of women at risk of developing high-grade cervical disease: Proposal for new guidelines based on data from the Netherlands. J. Low. Genit. Tract Dis. 2014, 18, 338–343. [Google Scholar] [CrossRef] [PubMed]
- Kalliala, I.; Anttila, A.; Pukkala, E.; Nieminen, P. Risk of cervical and other cancers after treatment of cervical intraepithelial neoplasia: Retrospective cohort study. Br. Med. J. 2005, 331, 1183–1185. [Google Scholar] [CrossRef]
- Melnikow, J.; McGahan, C.; Sawaya, G.F.; Ehlen, T.; Coldman, A. Cervical intraepithelial neoplasia outcomes after treatment: Long-term follow-up from the british columbia cohort study. J. Natl. Cancer Inst. 2009, 101, 721–728. [Google Scholar] [CrossRef]
- Soutter, W.P.; Sasieni, P.; Panoskaltsis, T. Long-term risk of invasive cervical cancer after treatment of squamous cervical intraepithelial neoplasia. Int. J. Cancer 2006, 118, 2048–2055. [Google Scholar] [CrossRef]
- Strander, B.; Andersson-Ellström, A.; Milsom, I.; Sparén, P. Long term risk of invasive cancer after treatment for cervical intraepithelial neoplasia grade 3: Population based cohort study. Br. Med. J. 2007, 335, 1077–1080. [Google Scholar] [CrossRef]
- Sand, F.L.; Frederiksen, K.; Munk, C.; Jensen, S.M.; Kjær, S.K. Long-term Risk of Cervical Cancer Following Conization of Cervical Intraepithelial Neoplasia Grade 3-A Danish Nationwide Cohort Study. Int. J. Cancer 2018, 142, 1759–1766. [Google Scholar] [CrossRef]
- Cheung, L.C.; Egemen, D.; Chen, X.; Katki, H.A.; Demarco, M.; Wiser, A.L.; Perkins, R.B.; Guido, R.S.; Wentzensen, N.; Schiffman, M. 2019 ASCCP Risk-Based Management Consensus Guidelines: Methods for Risk Estimation, Recommended Management, and Validation. J. Low. Genit. Tract Dis. 2020, 24, 90–101. [Google Scholar] [CrossRef]
- Perkins, R.B.; Guido, R.S.; Castle, P.E.; Chelmow, D.; Einstein, M.H.; Garcia, F.; Huh, W.K.; Kim, J.J.; Moscicki, A.; Nayar, R.; et al. 2019 ASCCP Risk-Based Management Consensus Guidelines for Abnormal Cervical Cancer Screening Tests and Cancer Precursors. J. Low. Genit. Tract Dis. 2020, 24, 102–131. [Google Scholar] [CrossRef]
- Roberts, J.M.; Jin, F.; Poynten, I.M.; Law, C.; Templeton, D.J.; Thurloe, J.K.; Garland, S.M.; Grulich, A.E.; Farnsworth, A.; Hillman, R.J. Histological outcomes of anal high-grade cytopredictions. Cancer Cytopathol. 2018, 126, 136–144. [Google Scholar] [CrossRef] [PubMed]
- Rebolj, M.; Helmerhorst, T.; Habbema, D.; Looman, C.; Boer, R.; van Rosmalen, J.; van Ballegooijen, M. Risk of cervical cancer after completed post-treatment follow-up of cervical intraepithelial neoplasia: Population based cohort study. BMJ 2012, 345, e6855. [Google Scholar] [CrossRef] [PubMed]
- Ebisch, R.M.; Rutten, D.W.; Hout, J.; Melchers, W.J.; Massuger, L.F.; Bulten, J.; Bekkers, R.L.; Siebers, A.G. Long-lasting increased risk of human papillomavirus–related carcinomas and premalignancies after cervical intraepithelial neoplasia grade 3: A population-based cohort study. J. Clin. Oncol. 2017, 35, 2542–2550. [Google Scholar] [CrossRef] [PubMed]
- Joura, E.A.; Garland, S.M.; Paavonen, J.; Ferris, D.G.; Perez, G.; Ault, K.A.; Huh, W.K.; Sings, H.L.; James, M.K.; Haupt, R.M. Effect of the human papillomavirus (HPV) quadrivalent vaccine in a subgroup of women with cervical and vulvar disease: Retrospective pooled analysis of trial data. BMJ 2012, 344, e1401. [Google Scholar] [CrossRef] [PubMed]
- Garland, S.M.; Paavonen, J.; Jaisamrarn, U.; Naud, P.; Salmerón, J.; Chow, S.N.; Apter, D.; Castellsagué, X.; Teixeira, J.C.; Skinner, S.R.; et al. Prior human papillomavirus-16/18 AS04-adjuvanted vaccination prevents recurrent high grade cervical intraepithelial neoplasia after definitive surgical therapy: Post-hoc analysis from a randomized controlled trial. Int. J. Cancer 2016, 139, 2812–2826. [Google Scholar] [CrossRef] [PubMed]
- Ghelardi, A.; Parazzini, F.; Martella, F.; Pieralli, A.; Bay, P.; Tonetti, A.; Svelato, A.; Bertacca, G.; Lombardi, S.; Joura, E.A. SPERANZA project: HPV vaccination after treatment for CIN2+. Gynecol. Oncol. 2018, 151, 229–234. [Google Scholar] [CrossRef]
- Kang, W.D.; Choi, H.S.; Kim, S.M. Is vaccination with quadrivalent HPV vaccine after loop electrosurgical excision procedure effective in preventing recurrence in patients with high-grade cervical intraepithelial neoplasia (CIN2-3)? Gynecol. Oncol. 2013, 130, 264–268. [Google Scholar] [CrossRef]
- Giuliano, A.R.; Joura, E.A.; Garland, S.M.; Huh, W.K.; Iversen, O.E.; Kjaer, S.K.; Ferenczy, A.; Kurman, R.J.; Ronnett, B.M.; Stoler, M.H.; et al. Nine-valent HPV vaccine efficacy against related diseases and definitive therapy: Comparison with historic placebo population. Gynecol. Oncol. 2019. [Google Scholar] [CrossRef]
- Martínez-Gómez, X.; Curran, A.; Campins, M.; Alemany, L.; Rodrigo-Pendás, J.Á.; Borruel, N.; Castellsagué, X.; Díaz-de-Heredia, C.; Moraga-Llop, F.A.; del Pino, M.; et al. Multidisciplinary, evidence-based consensus guidelines for human papillomavirus (HPV) vaccination in highrisk populations, Spain, 2016. Eurosurveillance 2019, 24, 1700857. [Google Scholar] [CrossRef]
- De Catalunya, G. Agència de Salut Pública de Catalunya, Manual de Vacunacions de Catalunya. 2018. Available online: Http://Salutpublica.Gencat.Cat/Web/.Content/Minisite/Aspcat/Promocio_salut/Vacunacions/00manual_de_vacunacions/Manual-de-Vacunacions.Pdf (accessed on 16 October 2019).
- Wright, T.C.; Massad, L.S.; Dunton, C.J.; Spitzer, M.; Wilkinson, E.J.; Solomon, D. 2006 Consensus guidelines for the management of women with cervical intraepithelial neoplasia or adenocarcinoma in situ. J. Low. Genit. Tract Dis. 2007, 223–239. [Google Scholar] [CrossRef]
- Torné, A.; del Pino, M.; Cusidó, M.; Alameda, F.; Andia, D.; Castellsagué, X.; Cortés, J.; Granados, R.; Guarch, R.; Loveras, B.L.; et al. AEPCC-Guía: Prevención del Cáncer de Cuello de Útero 2014, Publicaciones AEPCC. 2015, pp. 1–55. Available online: http://www.aepcc.org/wp-content/uploads/2016/01/AEPCC_revista02.pdf (accessed on 15 November 2019).
- Massad, L.S.; Einstein, M.H.; Huh, W.K.; Katki, H.A.; Kinney, W.K.; Schiffman, M.; Solomon, D.; Wentzensen, N.; Lawson, H.W. 2012 Asccp Consensus Guidelines Conference, 2012 Updated Consensus Guidelines for the Management of Abnormal Cervical Cancer Screening Tests and Cancer Precursors. Obstet. Gynecol. 2013, 121, 829–846. [Google Scholar] [CrossRef] [PubMed]
- Solomon, D.; Davey, D.; Kurman, R.; Moriarty, A.; O’Connor, D.; Prey, M.; Raab, S.; Sherman, M.; Wilbur, D.; Wright, T.; et al. The 2001 Bethesda System: Terminology for reporting results of cervical cytology. J. Am. Med. Assoc. 2002, 287, 2114–2119. [Google Scholar] [CrossRef] [PubMed]
- Bergeron, C.; Ordi, J.; Schmidt, D.; Trunk, M.J.; Keller, T.; Ridder, R. Conjunctive p16INK4a testing significantly increases accuracy in diagnosing high-grade cervical intraepithelial neoplasia. Am. J. Clin. Pathol. 2010, 133, 395–406. [Google Scholar] [CrossRef] [PubMed]
- Darragh, T.M.; Colgan, T.J.; Cox, J.T.; Heller, D.S.; Henry, M.R.; Luff, R.D.; McCalmont, T.; Nayar, R.; Palefsky, J.M.; Stoler, M.H.; et al. The Lower Anogenital Squamous Terminology Standardization Project for HPV-Associated Lesions: Background and Consensus Recommendations from the College of American Pathologists and the American Society for Colposcopy and Cervical Pathology. Arch. Pathol. Lab. Med. 2012, 136, 1266–1297. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Manfredi, A.; Alonso, I.; del Pino, M.; Fusté, P.; Torné, A.; Ordi, J. Predictors of absence of cervical intraepithelial neoplasia in the conization specimen. Gynecol. Oncol. 2013, 128, 271–276. [Google Scholar] [CrossRef]
- EMA. Gardasil, suspensión inyectable. Ficha técnica. Agencia Eur. Medicam. 2012. [Google Scholar] [CrossRef]
- EMA. Cervarix suspensión inyectable. Ficha tecnica o resumen de las caracteristicas del producto 1. Agencia Eur. Med. 2014, 1–33. [Google Scholar] [CrossRef]
- EMA. Gardasil 9 Suspensión Inyectable. Ficha Tecnica o Resumen de las Caracteristicas del Producto 1; EMA/192711/2016; EMA: Amsterdam, The Netherlands, 2016. [Google Scholar]
- Villa, L.L.; Kjaer, S.K.; Muñoz, N.; The FUTURE II Study Group. Quadrivalent Vaccine against Human Papillomavirus to Prevent Hgh-Grade Cervical Lesions. N. Engl. J. Med. 2010, 356, 1991–2002. [Google Scholar] [CrossRef]
- Joura, E.A.; Giuliano, A.R.; Iversen, O.E.; Bouchard, C.; Mao, C.; Mehlsen, J.; Moreira, E.D.; Ngan, Y.; Petersen, L.K.; Lazcano-Ponce, E.; et al. A 9-valent HPV vaccine against infection and intraepithelial Neoplasia in women. Obstet. Gynecol. Surv. 2015, 70, 446–448. [Google Scholar] [CrossRef]
- D’Addario, M.; Redmond, S.; Scott, P.; Egli-Gany, D.; Riveros-Balta, A.X.; Restrepo, A.M.H.; Low, N. Two-dose schedules for human papillomavirus vaccine: Systematic review and meta-analysis. Vaccine 2017, 35, 2892–2901. [Google Scholar] [CrossRef]
- Sankaranarayanan, R.; Joshi, S.; Muwonge, R.; Esmy, P.O.; Basu, P.; Prabhu, P.; Bhatla, N.; Nene, B.M.; Shaw, J.; Poli, U.R.R.; et al. Can a single dose of human papillomavirus (HPV) vaccine prevent cervical cancer? Early findings from an Indian study. Vaccine 2018, 36, 4783–4791. [Google Scholar] [CrossRef] [PubMed]
- Kreimer, A.R.; Herrero, R.; Sampson, J.N.; Porras, C.; Lowy, D.R.; Schiller, J.T.; Schiffman, M.; Rodriguez, A.C.; Chanock, S.; Jimenez, S.; et al. Evidence for single-dose protection by the bivalent HPV vaccine—Review of the Costa Rica HPV vaccine trial and future research studies. Vaccine 2018, 36, 4774–4782. [Google Scholar] [CrossRef] [PubMed]
- Brotherton, J.M.; Budd, A.; Rompotis, C.; Bartlett, N.; Malloy, M.J.; Andersen, R.L.; Coulter, K.A.; Couvee, P.W.; Steel, N.; Ward, G.H.; et al. Is one dose of human papillomavirus vaccine as effective as three?: A national cohort analysis. Papillomavirus Res. 2019, 8, 100177. [Google Scholar] [CrossRef]
- Chen, L.; Liu, L.; Tao, X.; Guo, L.; Zhang, H.; Sui, L. Risk Factor Analysis of Persistent High-Grade Squamous Intraepithelial Lesion after Loop Electrosurgical Excision Procedure Conization. J. Low. Genit. Tract Dis. 2019, 23, 24–27. [Google Scholar] [CrossRef] [PubMed]
| Baseline Clinical Characteristics | Vaccinated Women (n = 153) | Non-Vaccinated Women (n = 112) | p * | ||
|---|---|---|---|---|---|
| Age | 0.115 | ||||
| < 35 years | 68 | (44.4) | 39 | (34.8) | |
| ≥ 35 years | 85 | (55.6) | 73 | (65.2) | |
| Indication of conization | 0.300 | ||||
| Pap test HSIL & biopsy ≤ LSIL/CIN1 | 12 | (7.8) | 13 | (11.6) | |
| Biopsy HSIL/CIN 2–3 | 141 | (92.2) | 99 | (88.4) | |
| HPV genotype (pre-treatment) | 0.063 | ||||
| HPV16 or 18 | 94 | (61.4) | 56 | (50.0) | |
| Other HPV types (non 16 non 18) | 59 | (38.6) | 56 | (50.0) | |
| Year of treatment | <0.001 | ||||
| January 2013 to June 2016 | 47 | (30.7) | 84 | (75.0) | |
| June 2016 to July 2018 | 106 | (69.3) | 28 | (25.0) | |
| Conization specimen diagnosis | 0.436 | ||||
| Negative | 12 | (7.8) | 14 | (12.5) | |
| LSIL/CIN1 | 17 | (11.1) | 13 | (11.6) | |
| HSIL/CIN2-3 | 124 | (81.1) | 85 | (75.9) | |
| Margin status | 0.091 | ||||
| Negative | 94 | (61.4) | 80 | (71.4) | |
| Positive | 59 | (38.6) | 32 | (28.6) | |
| Type of HPV vaccine | |||||
| 2v | 30 | (19.6%) | - | - | - |
| 4v | 7 | (4.6%) | - | - | |
| 9v | 98 | (64.1%) | - | - | |
| unknown | 18 | (11.8%) | - | - | |
| Case Number | Age | Indication of Conization | Pre-Treatment HPV Genotype | Conization Diagnosis | Cone Margins | First Post-Conization Control Result (6 Months) | HPV Genotype at the End of Follow-Up | Vaccine Type | Doses |
|---|---|---|---|---|---|---|---|---|---|
| Vaccinated women who showed persistent/recurrent HSIL (n = 5) | |||||||||
| 1 | 38.2 | HSIL/CIN 2–3 | HPVnon16/non18 | LSIL/CIN1 | Positive | Persistent LSIL/HPV | HPVnon16/non18 | Unknown | 3 |
| 2 | 41.2 | Pap HSIL, biopsy LSIL/CIN1 | HPVnon16/non18 | HSIL/CIN2 | Negative | Persistent LSIL/HPV | HPVnon16/non18 | 2v | 3 |
| 3 | 41.6 | HSIL/CIN 2–3 | HPVnon16/non18 | LSIL/CIN1 | Positive | Persistent LSIL/HPV | HPVnon16/non18 | 9v | 3 |
| 4 | 30.7 | HSIL/CIN 2–3 | HPV16 | HSIL/CIN2 | Positive | Persistent LSIL/HPV | HPV16 | 9v | 3 |
| 5 | 46.5 | Pap HSIL, biopsy LSIL/CIN1 | HPV16 | Negative | Negative | Persistent HSIL/CIN2-3 | HPV16 | 9v | 2 |
| Non-vaccinated women who showed persistent/recurrent HSIL (n = 12) | |||||||||
| 6 | 31.1 | HSIL/CIN 2–3 | HPVnon16/non18 | HSIL/CIN2 | Negative | No disease | HPV16 | - | - |
| 7 | 64.2 | HSIL/CIN 2–3 | HPVnon16/non18 | HSIL/CIN2 | Negative | Persistent LSIL/HPV | HPVnon16/non18 | - | - |
| 8 | 41.6 | Pap HSIL, biopsy LSIL/CIN1 | HPV16 | LSIL/CIN1 | Positive | Persistent LSIL/HPV | HPV16 | - | - |
| 9 | 45.4 | HSIL/CIN 2–3 | HPV16 | HSIL/CIN3 | Negative | No disease | HPVnon16/non18 | - | - |
| 10 | 33.0 | HSIL/CIN 2–3 | HPV18 | HSIL/CIN2 | Negative | No disease | HPVnon16/non18 | - | - |
| 11 | 66.2 | HSIL/CIN 2–3 | HPV16 | HSIL/CIN3 | Negative | Persistent LSIL/HPV | HPVnon16/non18 | - | - |
| 12 | 39.9 | HSIL/CIN 2–3 | HPVnon16/non18 | HSIL/CIN3 | Negative | No disease | HPVnon16/non18 | - | - |
| 13 | 33.2 | HSIL/CIN 2–3 | HPV16 | HSIL/CIN2 | Positive | Persistent LSIL/HPV | HPV16 | - | - |
| 14 | 50.4 | HSIL/CIN 2–3 | HPVnon16/non18 | Negative | Negative | Persistent LSIL/HPV | HPVnon16/non18 | - | - |
| 15 | 61.4 | Pap HSIL, biopsy LSIL/CIN1 | HPVnon16/non18 | LSIL/CIN1 | Negative | Persistent HSIL/CIN2-3 | HPVnon16/non18 | - | - |
| 16 | 54.9 | HSIL/CIN 2–3 | HPV16 | LSIL/CIN1 | Negative | Persistent HSIL/CIN2-3 | HPV16 | - | - |
| 17 | 26.8 | HSIL/CIN 2–3 | HPV16 | HSIL/CIN2 | Positive | Persistent LSIL/HPV | HPV16 | - | - |
| Variable | Persistent/Recurrent HSIL at the End of Follow-Up | |||||
|---|---|---|---|---|---|---|
| Univariate Analysis | Multivariate Analysis | |||||
| OR | (95% CI) | p | AOR | (95% CI) | p | |
| Age | 0.345 | - | ||||
| < 35 years | 1 | - | - | |||
| ≥ 35 years | 1.67 | (0.6–4.9) | - | - | ||
| HPV type | 0.753 | - | ||||
| HPV non 16 non 18 | 1 | - | - | |||
| HPV 16 and/or 18 | 0.85 | (0.3–2.3) | - | - | ||
| Margins of the conization specimen | 0.932 | - | ||||
| Negative | 1 | - | - | |||
| Positive | 1.0 | (0.4–2.9) | - | - | ||
| First post-conization control status | 0.001 | 0.018 | ||||
| No disease | 1 | 1 | ||||
| Persistent LSIL/HPV | 4.1 | (1.2–13.4) | 4.3 | (1.3–14.3) | ||
| Persistent HSIL/CIN2-3 | 14.9 | (2.7–75.3) | 21.0 | (3.6–123.5) | ||
| HPV vaccination | 0.021 | 0.010 | ||||
| No | 1 | 1 | ||||
| Yes | 0.3 | (0.1–0.8) | 0.2 | (0.1–0.7) | ||
| Clinical Outcome at the End of Follow-Up | ||||
|---|---|---|---|---|
| Status at the First Post-Conization Control (6 Months) | No Disease | Persistent/Recurrent LSIL/HPV | Persistent/Recurrent HSIL | p * |
| No disease (n = 153) | 0.032 | |||
| Non-vaccinated | 55 (83.3) | 7 (10.7) | 4 (6.1) | |
| Vaccinated | 78 (89.7) | 9 (10.3) | 0 (0.0) | |
| Persistent LSIL/HPV (n = 101) | 0.173 | |||
| Non-vaccinated | 28 (65.1) | 9 (20.9) | 6 (14.0) | |
| Vaccinated | 33 (56.9) | 21 (36.2) | 4 (6.9) | |
| Persistent HSIL/CIN2-3 (n = 11) | 0.131 | |||
| Non-vaccinated | 0 (0.0) | 1 (33.3) | 2 (66.7) | |
| Vaccinated | 3 (37.5) | 4 (50.0) | 1 (12.5) | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
del Pino, M.; Martí, C.; Torras, I.; Henere, C.; Munmany, M.; Marimon, L.; Saco, A.; Torné, A.; Ordi, J. HPV Vaccination as Adjuvant to Conization in Women with Cervical Intraepithelial Neoplasia: A Study under Real-Life Conditions. Vaccines 2020, 8, 245. https://doi.org/10.3390/vaccines8020245
del Pino M, Martí C, Torras I, Henere C, Munmany M, Marimon L, Saco A, Torné A, Ordi J. HPV Vaccination as Adjuvant to Conization in Women with Cervical Intraepithelial Neoplasia: A Study under Real-Life Conditions. Vaccines. 2020; 8(2):245. https://doi.org/10.3390/vaccines8020245
Chicago/Turabian Styledel Pino, Marta, Cristina Martí, Ines Torras, Carla Henere, Meritxell Munmany, Lorena Marimon, Adela Saco, Aureli Torné, and Jaume Ordi. 2020. "HPV Vaccination as Adjuvant to Conization in Women with Cervical Intraepithelial Neoplasia: A Study under Real-Life Conditions" Vaccines 8, no. 2: 245. https://doi.org/10.3390/vaccines8020245
APA Styledel Pino, M., Martí, C., Torras, I., Henere, C., Munmany, M., Marimon, L., Saco, A., Torné, A., & Ordi, J. (2020). HPV Vaccination as Adjuvant to Conization in Women with Cervical Intraepithelial Neoplasia: A Study under Real-Life Conditions. Vaccines, 8(2), 245. https://doi.org/10.3390/vaccines8020245







