Long Term Outcomes of Anti-COVID-19 Vaccines in Patients with Systemic Lupus Erythematosus: A Multicentre Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Timeframes of Observation
2.2. Short-Term Adverse Events
2.3. Long-Term Complications of Special Interest
2.4. General Features
2.5. Statistical Analysis
3. Results
3.1. General Features
3.2. Short-Term Adverse Events Following Vaccination
3.3. Long-Term Complications
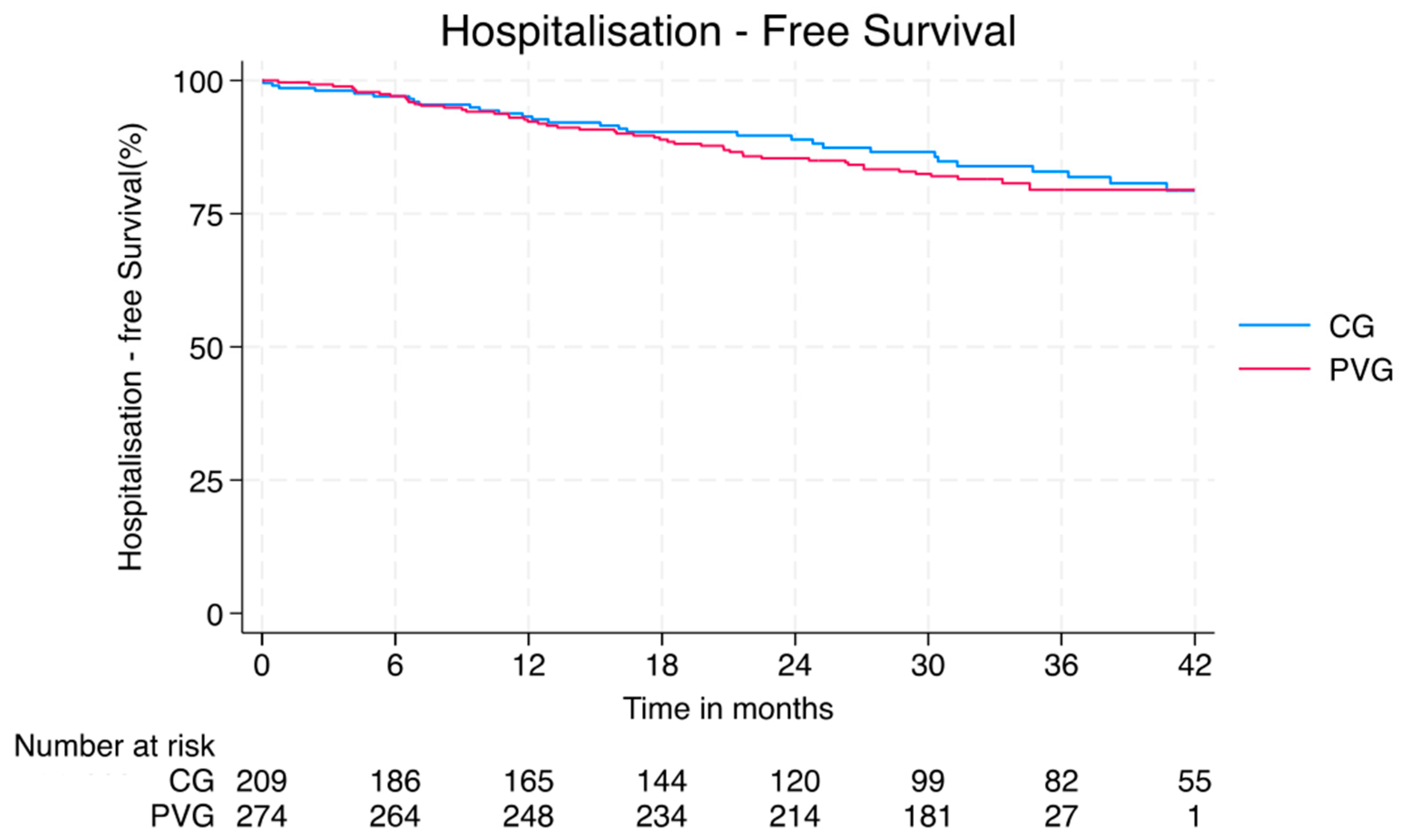
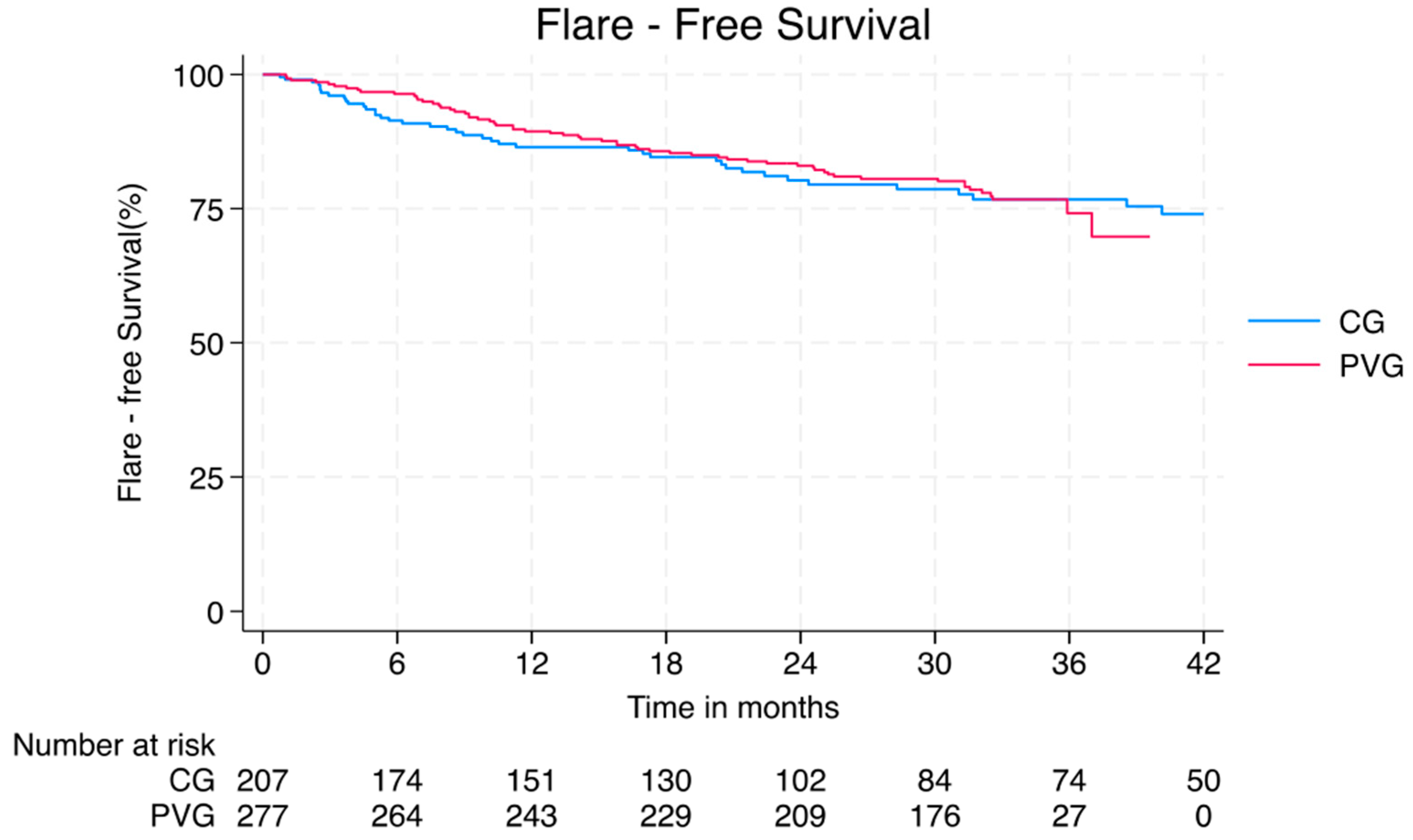
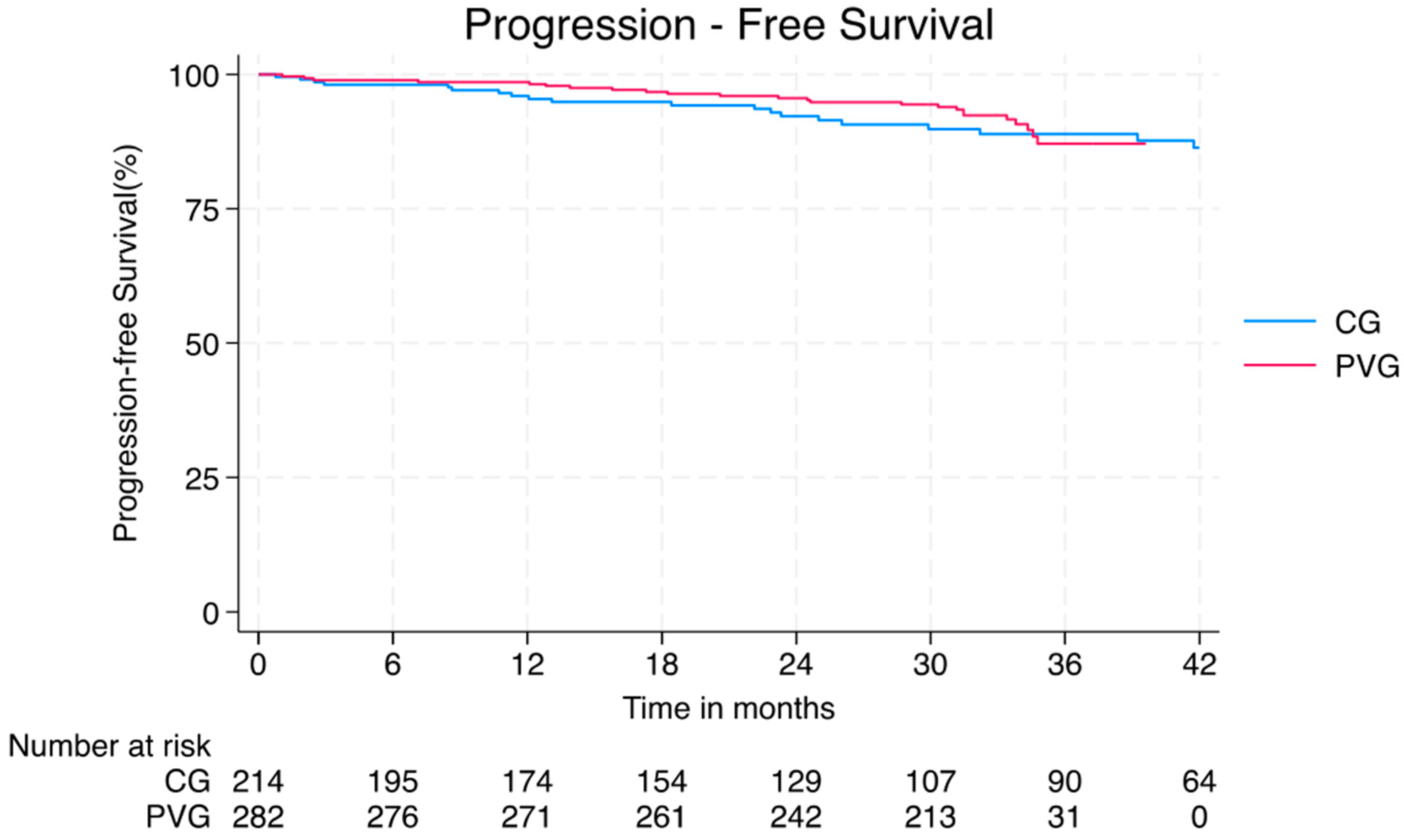
3.3.1. General Outcomes
3.3.2. Infections
3.3.3. SLE Flares and Progression
3.3.4. Chronic Comorbidities
3.3.5. Pregnancies
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mauro, M.; Giancotti, M. Italian responses to the COVID-19 emergency: Overthrowing 30 years of health reforms? Health Policy 2021, 125, 548–552. [Google Scholar] [CrossRef] [PubMed]
- Paudel, D.; Neupane, R.C.; Sigdel, S.; Poudel, P.; Khanal, A.R. COVID-19 Pandemic, Climate Change, and Conflicts on Agriculture: A Trio of Challenges to Global Food Security. Sustainability 2023, 15, 8280. [Google Scholar] [CrossRef]
- De Luca Picione, R.; Martini, E.; Cicchella, S.; Forte, S.; Carranante, M.; Tateo, L.; Rhodes, P. The impact of Covid-19 pandemic: Psycho-social perception of the crisis and sense-making processes. Community Psychol. Glob. Perspect. 2021, 7, 103–128. [Google Scholar]
- Maddock, J.; Parsons, S.; Di Gessa, G.; Green, M.J.; Thompson, E.J.; Stevenson, A.J.; Kwong, A.S.; McElroy, E.; Santorelli, G.; Silverwood, R.J.; et al. Inequalities in healthcare disruptions during the COVID-19 pandemic: Evidence from 12 UK population-based longitudinal studies. BMJ Open 2022, 12, e064981. [Google Scholar] [CrossRef]
- Talarico, R.; Aguilera, S.; Alexander, T.; Amoura, Z.; Antunes, A.M.; Arnaud, L.; Avcin, T.; Beretta, L.; Bombardieri, S.; Burmester, G.R.; et al. The impact of COVID-19 on rare and complex connective tissue diseases: The experience of ERN ReCONNET. Nat. Rev. Rheumatol. 2021, 17, 177–184. [Google Scholar] [CrossRef]
- Shukla, P.; Lee, M.; Whitman, S.A.; Pine, K.H. Delay of routine health care during the COVID-19 pandemic: A theoretical model of individuals’ risk assessment and decision making. Soc. Sci. Med. 2022, 307, 115164. [Google Scholar] [CrossRef]
- Gianfrancesco, M.; Hyrich, K.L.; Al-Adely, S.; Carmona, L.; Danila, M.I.; Gossec, L.; Izadi, Z.; Jacobsohn, L.; Katz, P.; Lawson-Tovey, S.; et al. Characteristics associated with hospitalisation for COVID-19 in people with rheumatic disease: Data from the COVID-19 Global Rheumatology Alliance physician-reported registry. Ann. Rheum. Dis. 2020, 79, 859–866. [Google Scholar] [CrossRef] [PubMed]
- Pablos, J.L.; Galindo, M.; Carmona, L.; Lledó, A.; Retuerto, M.; Blanco, R.; Gonzalez-Gay, M.A.; Martinez-Lopez, D.; Castrejón, I.; Alvaro-Gracia, J.M.; et al. Clinical outcomes of hospitalised patients with COVID-19 and chronic inflammatory and autoimmune rheumatic diseases: A multicentric matched cohort study. Ann. Rheum. Dis. 2020, 79, 1544–1549. [Google Scholar] [CrossRef] [PubMed]
- Ramirez, G.A.; Argolini, L.M.; Bellocchi, C.; Moroni, L.; Della-Torre, E.; Farina, N.; Caporali, R.F.; Beretta, L.; Gerosa, M.; Bozzolo, E.P.; et al. Impact of the COVID-19 pandemic in patients with systemic lupus erythematosus throughout one year. Clin. Immunol. 2021, 231, 108845. [Google Scholar] [CrossRef]
- Mathian, A.; Breillat, P.; Dorgham, K.; Bastard, P.; Charre, C.; Lhote, R.; Quentric, P.; Moyon, Q.; Mariaggi, A.A.; Mouries-Martin, S.; et al. Lower disease activity but higher risk of severe COVID-19 and herpes zoster in patients with systemic lupus erythematosus with pre-existing autoantibodies neutralising IFN-α. Ann. Rheum. Dis. 2022, 81, 1695–1703. [Google Scholar] [CrossRef]
- Bastard, P.; Rosen, L.B.; Zhang, Q.; Michailidis, E.; Hoffmann, H.H.; Zhang, Y.; Dorgham, K.; Philippot, Q.; Rosain, J.; Béziat, V.; et al. Autoantibodies against type I IFNs in patients with life-threatening COVID-19. Science 2020, 370, eabd4585. [Google Scholar] [CrossRef] [PubMed]
- Joo, Y.B.; Kim, K.J.; Park, K.S.; Park, Y.J. Influenza infection as a trigger for systemic lupus erythematosus flares resulting in hospitalization. Sci. Rep. 2021, 11, 4630. [Google Scholar] [CrossRef] [PubMed]
- Ramirez, G.A.; Calabrese, C.; Secci, M.; Moroni, L.; Gallina, G.D.; Benanti, G.; Bozzolo, E.P.; Matucci-Cerinic, M.; Dagna, L. Infection-Associated Flares in Systemic Lupus Erythematosus. Pathogens 2024, 13, 934. [Google Scholar] [CrossRef] [PubMed]
- Furer, V.; Rondaan, C.; Heijstek, M.W.; Agmon-Levin, N.; van Assen, S.; Bijl, M.; Breedveld, F.C.; D’Amelio, R.; Dougados, M.; Kapetanovic, M.C.; et al. 2019 update of EULAR recommendations for vaccination in adult patients with autoimmune inflammatory rheumatic diseases. Ann. Rheum. Dis. 2020, 79, 39–52. [Google Scholar] [CrossRef]
- Rappuoli, R.; Alter, G.; Pulendran, B. Transforming vaccinology. Cell 2024, 187, 5171–5194. [Google Scholar] [CrossRef]
- Kawano, Y.; Patel, N.J.; Wang, X.; Cook, C.E.; Vanni, K.M.; Kowalski, E.N.; Banasiak, E.P.; Qian, G.; DiIorio, M.; Hsu, T.Y.; et al. Temporal trends in COVID-19 outcomes among patients with systemic autoimmune rheumatic diseases: From the first wave through the initial Omicron wave. Ann. Rheum. Dis. 2022, 81, 1742–1749. [Google Scholar] [CrossRef]
- Baden, L.R.; El Sahly, H.M.; Essink, B.; Kotloff, K.; Frey, S.; Novak, R.; Diemert, D.; Spector, S.A.; Rouphael, N.; Creech, C.B.; et al. Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine. N. Engl. J. Med. 2021, 384, 403–416. [Google Scholar] [CrossRef]
- Katsoularis, I.; Jerndal, H.; Kalucza, S.; Lindmark, K.; Fonseca-Rodríguez, O.; Connolly, A.-M.F. Risk of arrhythmias following COVID-19: Nationwide self-controlled case series and matched cohort study. Eur. Heart J. Open 2023, 3, oead120. [Google Scholar] [CrossRef]
- Patone, M.; Mei, X.W.; Handunnetthi, L.; Dixon, S.; Zaccardi, F.; Shankar-Hari, M.; Watkinson, P.; Khunti, K.; Harnden, A.; Coupland, C.A.C.; et al. Risk of Myocarditis After Sequential Doses of COVID-19 Vaccine and SARS-CoV-2 Infection by Age and Sex. Circulation 2022, 146, 743–754. [Google Scholar] [CrossRef]
- Chang, R.; Yen-Ting Chen, T.; Wang, S.I.; Hung, Y.M.; Chen, H.Y.; Wei, C.J. Risk of autoimmune diseases in patients with COVID-19: A retrospective cohort study. eClinicalMedicine 2023, 56, 101783. [Google Scholar] [CrossRef]
- Flacco, M.E.; Acuti Martellucci, C.; Soldato, G.; Di Martino, G.; Carota, R.; De Benedictis, M.; Di Marco, G.; Parruti, G.; Di Luzio, R.; Caponetti, A.; et al. COVID-19 Vaccination Did Not Increase the Risk of Potentially Related Serious Adverse Events: 18-Month Cohort Study in an Italian Province. Vaccines 2022, 11, 31. [Google Scholar] [CrossRef]
- Thanborisutkul, K.; Kulalert, P.; Methaset, K.; Nanthapisal, S.; Chunthatikul, T.; Phangpanya, N.; Charoenying, P.; Atsawutmangkru, W.; Srijaroen, S.; Punyashthira, P.; et al. Incidence and Factors Associated with Self-Reported Skin Symptoms of Allergic Reactions to COVID-19 Vaccines. Vaccines 2025, 13, 289. [Google Scholar] [CrossRef]
- Nitz, J.N.; Ruprecht, K.K.; Henjum, L.J.; Matta, A.Y.; Shiferaw, B.T.; Weber, Z.L.; Jones, J.M.; May, R.; Baio, C.J.; Fiala, K.J.; et al. Cardiovascular Sequelae of the COVID-19 Vaccines. Cureus 2025, 17, e82041. [Google Scholar] [CrossRef] [PubMed]
- Sahoo, D.P. Causal Overgeneralization of COVID-19 Vaccine Adverse Events Undermines Scientific Integrity: A Technical Report. Cureus 2025, 17, e82121. [Google Scholar] [CrossRef]
- Solomon, D.H.; Bucala, R.; Kaplan, M.J.; Nigrovic, P.A. The “Infodemic” of COVID-19. Arthritis Rheumatol. 2020, 72, 1806–1808. [Google Scholar] [CrossRef]
- Horton, R. Offline: Managing the COVID-19 vaccine infodemic. Lancet 2020, 396, 1474. [Google Scholar] [CrossRef] [PubMed]
- Turner, P.J.; Larson, H.; Dubé, È.; Fisher, A. Vaccine Hesitancy: Drivers and How the Allergy Community Can Help. J. Allergy Clin. Immunol. Pract. 2021, 9, 3568–3574. [Google Scholar] [CrossRef] [PubMed]
- Gianfredi, V.; Berti, A.; Stefanizzi, P.; D’Amico, M.; De Lorenzo, V.; Moscara, L.; Di Lorenzo, A.; Venerito, V.; Castaldi, S. COVID-19 Vaccine Knowledge, Attitude, Acceptance and Hesitancy among Pregnancy and Breastfeeding: Systematic Review of Hospital-Based Studies. Vaccines 2023, 11, 1697. [Google Scholar] [CrossRef]
- Torrente López, A.; Hermosilla, J.; Navas, N.; Cuadros-Rodríguez, L.; Cabeza, J.; Salmerón, A. The Relevance of Monoclonal Antibodies in the Treatment of COVID-19. Vaccines 2021, 9, 557. [Google Scholar] [CrossRef]
- Wraith, D.C.; Goldman, M.; Lambert, P.H. Vaccination and autoimmune disease: What is the evidence? Lancet 2003, 362, 1659–1666. [Google Scholar] [CrossRef]
- Mormile, I.; Della Casa, F.; Petraroli, A.; Furno, A.; Granata, F.; Portella, G.; Rossi, F.W.; de Paulis, A. Immunogenicity and Safety of mRNA Anti-SARS-CoV-2 Vaccines in Patients with Systemic Lupus Erythematosus. Vaccines 2022, 10, 1221. [Google Scholar] [CrossRef] [PubMed]
- Petrou, D.; Marinaki, S.; Kriki, P.; Flouda, S.; Venetsanopoulou, A.; Voulgari, P.; Sardeli, A.; Drouzas, K.; Panagoutsos, S.; Liapis, G.; et al. Safety Profile of SARS-CoV-2 Vaccination in Patients with Lupus Nephritis: A Retrospective Study. J. Clin. Med. 2025, 14, 406. [Google Scholar] [CrossRef] [PubMed]
- Gerosa, M.; Schioppo, T.; Argolini, L.M.; Sciascia, S.; Ramirez, G.A.; Moroni, G.; Sinico, R.A.; Bonelli, G.; Alberici, F.; Mescia, F.; et al. The Impact of Anti-SARS-CoV-2 Vaccine in Patients with Systemic Lupus Erythematosus: A Multicentre Cohort Study. Vaccines 2022, 10, 663. [Google Scholar] [CrossRef] [PubMed]
- Aringer, M.; Costenbader, K.; Daikh, D.; Brinks, R.; Mosca, M.; Ramsey-Goldman, R.; Smolen, J.S.; Wofsy, D.; Boumpas, D.T.; Kamen, D.L.; et al. 2019 European League Against Rheumatism/American College of Rheumatology classification criteria for systemic lupus erythematosus. Ann. Rheum. Dis. 2019, 78, 1151–1159. [Google Scholar] [CrossRef]
- European-Commission. Article 29 Data Protection Working Party; 0829/14/EN WP216; European-Commission: Brussels, Belgium, 2014. [Google Scholar]
- Isenberg, D.A.; Rahman, A.; Allen, E.; Farewell, V.; Akil, M.; Bruce, I.N.; D’Cruz, D.; Griffiths, B.; Khamashta, M.; Maddison, P.; et al. BILAG 2004. Development and initial validation of an updated version of the British Isles Lupus Assessment Group’s disease activity index for patients with systemic lupus erythematosus. Rheumatology 2005, 44, 902–906. [Google Scholar] [CrossRef]
- Yamamura, Y.; Nakashima, C.; Kagawa, N.; Aoyama, Y.; Yamamoto, A.; Kawahira, H.; Kubota, Y.; Nakajima, S.; Nakahara, T.; Fuyuno, Y.; et al. Cutaneous Adverse Events Following COVID-19 Vaccination in Japan: A Questionnaire Survey. Cureus 2025, 17, e80257. [Google Scholar] [CrossRef]
- Yacoub, M.R.; Ferlito, A.; Nettis, E. Chronic urticaria: Not only after COVID-19 vaccination. Curr. Opin. Allergy Clin. Immunol. 2024, 24, 404–408. [Google Scholar] [CrossRef]
- Liu, A.; Liao, P.; Jiang, H.; Huang, S.; Li, S.; Wei, J.C.; Ying, Z. COVID- 19 vaccination reduces new-onset fibromyalgia risk in survivors. BMC Med. 2025, 23, 255. [Google Scholar] [CrossRef]
- Calabrese, L.H.; Calabrese, C. Long COVID for the Rheumatologist: Current Understanding and Approach to Management. Rheum. Dis. Clin. N. Am. 2025, 51, 29–43. [Google Scholar] [CrossRef]
- van Vollenhoven, R.F.; Bertsias, G.; Doria, A.; Isenberg, D.; Morand, E.; Petri, M.A.; Pons-Estel, B.A.; Rahman, A.; Ugarte-Gil, M.F.; Voskuyl, A.; et al. 2021 DORIS definition of remission in SLE: Final recommendations from an international task force. Lupus Sci. Med. 2021, 8, e000538. [Google Scholar] [CrossRef]
- Abdelahad, M.; Ta, E.; Kesselman, M.M.; Demory Beckler, M. A Review of the Efficacy of Influenza Vaccination in Autoimmune Disease Patients. Cureus 2021, 13, e15016. [Google Scholar] [CrossRef] [PubMed]
- Holvast, A.; Huckriede, A.; Wilschut, J.; Horst, G.; De Vries, J.J.; Benne, C.A.; Kallenberg, C.G.; Bijl, M. Safety and efficacy of influenza vaccination in systemic lupus erythematosus patients with quiescent disease. Ann. Rheum. Dis. 2006, 65, 913–918. [Google Scholar] [CrossRef] [PubMed]
- Adawi, M.; Bragazzi, N.L.; McGonagle, D.; Watad, S.; Mahroum, N.; Damiani, G.; Conic, R.; Bridgewood, C.; Mahagna, H.; Giacomelli, L.; et al. Immunogenicity, safety and tolerability of anti-pneumococcal vaccination in systemic lupus erythematosus patients: An evidence-informed and PRISMA compliant systematic review and meta-analysis. Autoimmun. Rev. 2019, 18, 73–92. [Google Scholar] [CrossRef]
- Iaccarino, L.; Bettio, S.; Reggia, R.; Zen, M.; Frassi, M.; Andreoli, L.; Gatto, M.; Piantoni, S.; Nalotto, L.; Franceschini, F.; et al. Effects of Belimumab on Flare Rate and Expected Damage Progression in Patients With Active Systemic Lupus Erythematosus. Arthritis Care Res. 2017, 69, 115–123. [Google Scholar] [CrossRef]
- Mok, C.C.; Chan, K.L.; Tse, S.M. Hesitancy for SARS-CoV-2 vaccines and post-vaccination flares in patients with systemic lupus erythematosus. Vaccine 2022, 40, 5959–5964. [Google Scholar] [CrossRef]
- Chehab, G.; Richter, J.G.; Brinks, R.; Fischer-Betz, R.; Winkler-Rohlfing, B.; Schneider, M. Vaccination coverage in systemic lupus erythematosus-a cross-sectional analysis of the German long-term study (LuLa cohort). Rheumatology 2018, 57, 1439–1447. [Google Scholar] [CrossRef] [PubMed]
- Rovere Querini, P.; De Lorenzo, R.; Conte, C.; Brioni, E.; Lanzani, C.; Yacoub, M.R.; Chionna, R.; Martinenghi, S.; Vitali, G.; Tresoldi, M.; et al. Post-COVID-19 follow-up clinic: Depicting chronicity of a new disease. Acta Biomed. 2020, 91, 22–28. [Google Scholar] [CrossRef]
- Song, S.; Guo, C.; Wu, R.; Zhao, H.; Li, Q.; Dou, J.H.; Guo, F.S.; Wei, J. Impact of the COVID-19 pandemic on cardiovascular mortality and contrast analysis within subgroups. Front. Cardiovasc. Med. 2024, 11, 1279890. [Google Scholar] [CrossRef]
- Mosca, M.; Andersen, J.; Wildman, P.; Manzi, S.; Amoura, Z.; Bultink, I.; Monticielo, O.A.; Navarra, S.; Pettersson, S. A charter to improve care for systemic lupus erythematosus. Clin. Exp. Rheumatol. 2025, 43, 517–525. [Google Scholar] [CrossRef]
- Ichikawa, T.; Kishida, D.; Shimojima, Y.; Yajima, N.; Oguro, N.; Yoshimi, R.; Sakurai, N.; Hidekawa, C.; Sada, K.-e.; Miyawaki, Y.; et al. Trust in Health Information Sources Among Patients With Systemic Lupus Erythematosus in the Social Networking Era: The TRUMP2-SLE Study. J. Rheumatol. 2025, 52, jrheum.2024-1088. [Google Scholar] [CrossRef]
- Miyachi, T.; Takita, M.; Senoo, Y.; Yamamoto, K. Lower trust in national government links to no history of vaccination. Lancet 2020, 395, 31–32. [Google Scholar] [CrossRef] [PubMed]
- Piga, M.; Tselios, K.; Viveiros, L.; Chessa, E.; Neves, A.; Urowitz, M.B.; Isenberg, D. Clinical patterns of disease: From early systemic lupus erythematosus to late-onset disease. Best Pract. Res. Clin. Rheumatol. 2023, 37, 101938. [Google Scholar] [CrossRef] [PubMed]
- Sim, J.J.L.; Lim, C.C. Influenza Vaccination in Systemic Lupus Erythematosus: Efficacy, Effectiveness, Safety, Utilization, and Barriers. Am. J. Med. 2022, 135, 286–296.e9. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Dhillon, N.; Pope, J. All-cause hospitalizations in systemic lupus erythematosus from a large Canadian referral centre. Rheumatology 2013, 52, 905–909. [Google Scholar] [CrossRef]
- Petri, M.; Genovese, M. Incidence of and risk factors for hospitalizations in systemic lupus erythematosus: A prospective study of the Hopkins Lupus Cohort. J. Rheumatol. 1992, 19, 1559–1565. [Google Scholar]
- Ramirez, G.A.; Gerosa, M.; Beretta, L.; Bellocchi, C.; Argolini, L.M.; Moroni, L.; Della Torre, E.; Artusi, C.; Nicolosi, S.; Caporali, R.; et al. COVID-19 in systemic lupus erythematosus: Data from a survey on 417 patients. Semin. Arthritis Rheum. 2020, 50, 1150–1157. [Google Scholar] [CrossRef]
- An, Z.; Figueroa-Parra, G.; Zhou, X.; Li, Y.; Jaquith, J.; McCarthy-Fruin, K.; Sletten, J.; Warrington, K.J.; Weyand, C.; Crowson, C.S.; et al. Immune responses and disease biomarker long-term changes following COVID-19 mRNA vaccination in a cohort of rheumatic disease patients. Front. Immunol. 2023, 14, 1224702. [Google Scholar] [CrossRef]
- Tani, C.; Cardelli, C.; Depascale, R.; Gamba, A.; Iaccarino, L.; Doria, A.; Bandeira, M.; Dinis, S.P.; Romão, V.C.; Gotelli, E.; et al. Long-term outcomes of COVID-19 vaccination in patients with rare and complex connective tissue diseases: The ERN-ReCONNET VACCINATE study. J. Transl. Autoimmun. 2023, 7, 100221. [Google Scholar] [CrossRef]
- Doskaliuk, B.; Ravichandran, N.; Sen, P.; Day, J.; Joshi, M.; Nune, A.; Nikiphorou, E.; Saha, S.; Tan, A.L.; Shinjo, S.K.; et al. Long-term safety of COVID vaccination in individuals with idiopathic inflammatory myopathies: Results from the COVAD study. Rheumatol. Int. 2023, 43, 1651–1664. [Google Scholar] [CrossRef]
- Carvajal, R.; Zabalza, A.; Carbonell-Mirabent, P.; Martínez-Gómez, X.; Esperalba, J.; Pappolla, A.; Rando, A.; Cobo-Calvo, A.; Tur, C.; Rodriguez, M.; et al. Vaccine Safety and Immunogenicity in Patients With Multiple Sclerosis Treated With Natalizumab. JAMA Netw. Open 2024, 7, e246345. [Google Scholar] [CrossRef]
- Ferri, C.; Ursini, F.; Gragnani, L.; Raimondo, V.; Giuggioli, D.; Foti, R.; Caminiti, M.; Olivo, D.; Cuomo, G.; Visentini, M.; et al. Impaired immunogenicity to COVID-19 vaccines in autoimmune systemic diseases. High prevalence of non-response in different patients’ subgroups. J. Autoimmun. 2021, 125, 102744. [Google Scholar] [CrossRef] [PubMed]
- Petri, M.; Joyce, D.; Haag, K.; Fava, A.; Goldman, D.W.; Zhong, D.; Xiao, S.; Milstone, A.; Magder, L.S. Effect of Systemic Lupus Erythematosus and Immunosuppressive Agents on COVID-19 Vaccination Antibody Response. Arthritis Care Res. 2023, 75, 1878–1885. [Google Scholar] [CrossRef] [PubMed]
- Draborg, A.H.; Duus, K.; Houen, G. Epstein-Barr virus and systemic lupus erythematosus. Clin. Dev. Immunol. 2012, 2012, 370516. [Google Scholar] [CrossRef]
- Angelini, M.; Teglia, F.; Astolfi, L.; Casolari, G.; Boffetta, P. Decrease of cancer diagnosis during COVID-19 pandemic: A systematic review and meta-analysis. Eur. J. Epidemiol. 2023, 38, 31–38. [Google Scholar] [CrossRef]
- Wong, H.J.; Morra, D.; Caesar, M.; Carter, M.W.; Abrams, H. Understanding hospital and emergency department congestion: An examination of inpatient admission trends and bed resources. Cjem 2010, 12, 18–26. [Google Scholar] [CrossRef] [PubMed]
- Eklund, K.; Wilhelmson, K. Outcomes of coordinated and integrated interventions targeting frail elderly people: A systematic review of randomised controlled trials. Health Soc. Care Community 2009, 17, 447–458. [Google Scholar] [CrossRef] [PubMed]
- Cassini, A.; Plachouras, D.; Eckmanns, T.; Abu Sin, M.; Blank, H.P.; Ducomble, T.; Haller, S.; Harder, T.; Klingeberg, A.; Sixtensson, M.; et al. Burden of Six Healthcare-Associated Infections on European Population Health: Estimating Incidence-Based Disability-Adjusted Life Years through a Population Prevalence-Based Modelling Study. PLoS Med. 2016, 13, e1002150. [Google Scholar] [CrossRef]
- Mosca, M.; Bruce, I.N.; Andersen, J.; Ugarte-Gil, M.F.; Arnaud, L. Challenges and opportunities in access to care for systemic lupus erythematosus patients across Europe and worldwide. Rheumatology 2024, 63, 1772–1778. [Google Scholar] [CrossRef]
| Hospitalised Patients by Cause of Hospitalisation: N (%) | CG (n = 45/223) | PVG (n = 61/284) | p-Value |
|---|---|---|---|
| Cardiovascular Events | 9 (20) | 5 (8) | 0.063 |
| Diagnostics | 5 (11) | 18 (30) | 0.999 |
| Infections | 11 (24) | 8 (13) | 0.843 |
| Flares | 3 (7) | 3 (5) | 0.073 |
| Neurological Event | 6 (13) | 2 (3) | 0.806 |
| Cancer | 9 (20) | 5 (8) | 0.631 |
| Kidney Transplant | 2 (4) | 1 (2) | 0.999 |
| C-section | 0 | 1 (2) | 0.999 |
| Orthopaedic Surgery | 3 (7) | 8 (13) | 0.367 |
| Other Surgery | 7 (15) | 10 (16) | 0.428 |
| Patients with New Manifestations: N (%) | CG (n = 34/223) | PVG (n = 26/284) | p-Value |
|---|---|---|---|
| Cardiopulmonary domain | 11 (32) | 3 (12) | 0.012 |
| Haematological domain | 12 (35) | 0 (0) | <0.001 |
| Musculoskeletal domain | 3 (1) | 17 (65) | 0.010 |
| Neuropsychiatric domain | 1 (3) | 0 (0) | 0.440 |
| Ophthalmic domain | 1 (3) | 0 (0) | 0.440 |
| Renal domain | 4 (11) | 3 (12) | 0.705 |
| Mucocutaneous domain | 4 (11) | 4 (15) | 0.754 |
| Incidence Rates (Events/100 Person-Months) | CG (n = 223) | PVG (n = 284) | p-Value |
|---|---|---|---|
| Cancer | 0.09 | 0.11 | 0.852 |
| Cardiovascular disorders | 0.35 | 0.07 | <0.001 |
| Cutaneous disorders | 0.03 | 0.01 | 0.850 |
| Fibromyalgia | 0.05 | 0.00 | 0.082 |
| Gonadal failure | 0.01 | 0.00 | 0.900 |
| Neurological disorders | 0.09 | 0.00 | 0.007 |
| Psychiatric disorders | 0.08 | 0.00 | 0.016 |
| Pulmonary disorders | 0.03 | 0.05 | 0.961 |
| Other autoimmune diseases | 0.07 | 0.06 | 0.892 |
| ESRD | 0.03 | 0.06 | 0.633 |
| Item | CG (n = 223) | PVG (n = 284) | p-Value |
|---|---|---|---|
| At least one pregnancy: N (%) | 15 (7) | 9 (3) | 0.054 |
| Number of pregnancies: N | 16 | 11 | - |
| Adverse foetal outcomes: N (%) * | 3 (19) | 2(18) | 0.999 |
| Adverse maternal events: N (%) * | 6 (38) | 3 (27) | 0.897 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Benanti, G.; Ramirez, G.A.; Schioppo, T.; Argolini, L.M.; Moroni, G.; Bonelli, G.; Sinico, R.A.; Alberici, F.; Mescia, F.; Moroni, L.; et al. Long Term Outcomes of Anti-COVID-19 Vaccines in Patients with Systemic Lupus Erythematosus: A Multicentre Study. Vaccines 2025, 13, 735. https://doi.org/10.3390/vaccines13070735
Benanti G, Ramirez GA, Schioppo T, Argolini LM, Moroni G, Bonelli G, Sinico RA, Alberici F, Mescia F, Moroni L, et al. Long Term Outcomes of Anti-COVID-19 Vaccines in Patients with Systemic Lupus Erythematosus: A Multicentre Study. Vaccines. 2025; 13(7):735. https://doi.org/10.3390/vaccines13070735
Chicago/Turabian StyleBenanti, Giovanni, Giuseppe A. Ramirez, Tommaso Schioppo, Lorenza Maria Argolini, Gabriella Moroni, Grazia Bonelli, Renato Alberto Sinico, Federico Alberici, Federica Mescia, Luca Moroni, and et al. 2025. "Long Term Outcomes of Anti-COVID-19 Vaccines in Patients with Systemic Lupus Erythematosus: A Multicentre Study" Vaccines 13, no. 7: 735. https://doi.org/10.3390/vaccines13070735
APA StyleBenanti, G., Ramirez, G. A., Schioppo, T., Argolini, L. M., Moroni, G., Bonelli, G., Sinico, R. A., Alberici, F., Mescia, F., Moroni, L., Gallina, G. D., Venerandi, B., Tamborini, F., Bellocchi, C., Beretta, L., Caporali, R., Bozzolo, E., Dagna, L., & Gerosa, M. (2025). Long Term Outcomes of Anti-COVID-19 Vaccines in Patients with Systemic Lupus Erythematosus: A Multicentre Study. Vaccines, 13(7), 735. https://doi.org/10.3390/vaccines13070735






