The Efficacy and Safety of Simultaneous Vaccination with Polysaccharide Conjugate Vaccines Against Pneumococcal (13-Valent Vaccine) and Haemophilus influenzae Type b Infections in Children with Juvenile Idiopathic Arthritis Without Systemic Manifestations: A Prospective Cohort Study
Abstract
1. Introduction
2. Methods
2.1. Study Design and Patient Selection
- -
- Diagnosis of JIA according to the ILAR (International League of Associations for Rheumatology) criteria [18];
- -
- Non-systemic JIA categories: oligoarthritis (persistent and extended), polyarthritis (rheumatoid factor positive and negative), enthesitis-related arthritis, and psoriatic arthritis;
- -
- Age at the study inclusion 2–18 years;
- -
- Treatment with either non-biologic or biologic disease-modified anti-rheumatic drugs (DMARDs) or their combination;
- -
- No previous vaccination against pneumococcal and Hemophilus influenza type b infection, except scheduled vaccination of this infection in the first year of life according to the national vaccine schedule [18].
- -
- Any information on vaccine intolerance in the past;
- -
- JIA with systemic onset or undifferentiated arthritis;
- -
- Patients with ongoing acute infection illness or 4 weeks before the baseline.
2.2. Vaccination
2.3. The Assessments of the Study
- (i)
- Demography
- (ii)
- Clinical assessment of JIA
- (iii)
- Laboratory assessment of JIA activity
- (iv)
- Assessment of the vaccine-specific antibodies
- (v)
- The safety of vaccination
- (a)
- Vaccine-associated AE included any acute reactions (first 30 min after injections) and delayed reactions (fever, malaise, fatigue, and injection-site reactions).
- (b)
- Disease-associated AE mentioned any clinical and/or laboratory signs of JIA flare or that required any changes in the treatment.
- (c)
- Common AEs included any events that occurred in the six-month follow-up period, except the abovementioned AEs.
- (vi)
- Respiratory infection episode analysis
2.4. The Study Outcomes
- (i)
- Analysis of seroconversion
- (ii)
- Assessment of JIA-related outcomes during this study: active joints, joints with limited motion, morning stiffness duration, MDVAS, pVAS, CHAQ, S-100 protein, CRP, hs-CRP, and ESR.
- (iii)
- The frequency of respiratory illness episodes and antibiotic administration at the end of the study were determined.
- (iv)
- Any AE during the six-month follow-up period after the baseline: fever and injection site reactions.
2.5. Statistical Analysis
2.6. Ethics
3. Results
3.1. The Demography of the Patients
3.2. Vaccine Seroconversion
3.3. Analysis of the Predictors of the Vaccination Outcome
3.4. JIA Outcomes During Vaccination
3.5. The Frequency of Acute Infectious Events and the Use of Antibacterial Therapy
3.6. Assessment of the Adverse Events
3.6.1. Mild Adverse Events
3.6.2. Severe AE
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Shenoi, S.; Horneff, G.; Aggarwal, A.; Ravelli, A. Treatment of non-systemic juvenile idiopathic arthritis. Nat. Rev. Rheumatol. 2024, 20, 170–181. [Google Scholar] [CrossRef] [PubMed]
- Weiss, J.E.; Ilowite, N.T. Juvenile idiopathic arthritis. Pediatr. Clin. N. Am. 2005, 52, 413–442. [Google Scholar] [CrossRef]
- Horneff, G. Update on biologicals for treatment of juvenile idiopathic arthritis. Expert Opin. Biol. Ther. 2013, 13, 361–376. [Google Scholar] [CrossRef]
- Swart, J.; Giancane, G.; Horneff, G.; Magnusson, B.; Hofer, M.; Alexeeva, E.; Panaviene, V.; Bader-Meunier, B.; Anton, J.; Nielsen, S.; et al. Pharmacovigilance in juvenile idiopathic arthritis patients treated with biologic or synthetic drugs: Combined data of more than 15,000 patients from Pharmachild and national registries. Arthritis Res. Ther. 2018, 20, 285. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Salonen, P.H.; Säilä, H.; Salonen, J.H.; Linna, M.; Helminen, M.; Kauppi, M.J. Pneumonia in children with juvenile idiopathic arthri-tis in Finland 1999–2014: A nationwide retrospective register linkage study. Clin. Exp. Rheumatol. 2019, 36, 502–507. [Google Scholar]
- Wakabayashi, A.; Ishiguro, T.; Takaku, Y.; Miyahara, Y.; Kagiyama, N.; Takayanagi, N. Clinical characteristics and prognostic factors of pneumonia in patients with and without rheumatoid arthritis. PLoS ONE 2018, 13, e0201799. [Google Scholar] [CrossRef] [PubMed]
- Ardura, M.I.; Toussi, S.S.; Siegel, J.D.; Lu, Y.; Bousvaros, A.; Crandall, W. NASPGHAN Clinical Report. J. Pediatr. Gastroenterol. Nutr. 2016, 63, 130–155. [Google Scholar] [CrossRef] [PubMed]
- Rosen, M.J.; Dhawan, A.; Saeed, S.A. Inflammatory Bowel Disease in Children and Adolescents. JAMA Pediatr. 2015, 169, 1053–1060. [Google Scholar] [CrossRef] [PubMed]
- Pneumococcal Disease. Surveillance and Reporting. Available online: https://www.cdc.gov/pneumococcal/php/surveillance/index.html (accessed on 9 February 2025).
- Available online: https://www.cdc.gov/hi-disease/php/surveillance/index.html (accessed on 9 February 2025).
- Jansen, M.H.A.; Rondaan, C.; Legger, G.E.; Minden, K.; Uziel, Y.; Toplak, N.; Maritsi, D.; Berg, L.V.D.; Berbers, G.A.M.; Bruijning, P.; et al. EULAR/PRES recommendations for vaccination of paediatric patients with autoimmune inflammatory rheumatic diseases: Update 2021. Ann. Rheum. Dis. 2023, 82, 35–47. [Google Scholar] [CrossRef] [PubMed]
- Bizjak, M.; Blazina, S.; Avramovic, M.Z.; Markelj, G.; Avcin, T.; Toplak, N. Vaccination coverage in children with rheumatic diseases. Clin. Exp. Rheumatol. 2020, 38, 164–170. [Google Scholar] [PubMed]
- Makarova, E.; Khabirova, A.; Volkova, N.; Gabrusskaya, T.; Ulanova, N.; Sakhno, L.; Revnova, M.; Kostik, M. Vaccination coverage in children with juvenile idiopathic arthritis, inflammatory bowel diseases, and healthy peers: Cross-sectional electronic survey data. World J. Clin. Pediatr. 2023, 12, 45–56. [Google Scholar] [CrossRef] [PubMed]
- Lassi, Z.S.; Naseem, R.; Salam, R.A.; Siddiqui, F.; Das, J.K. The Impact of the COVID-19 Pandemic on Immunization Campaigns and Programs: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 988. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Barbé-Tuana, F.; Funchal, G.; Schmitz, C.R.R.; Maurmann, R.M.; Bauer, M.E. The interplay between immunosenescence and age-related diseases. Semin. Immunopathol. 2020, 42, 545–557. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kostik, M.M.; Lubimova, N.A.; Fridman, I.V.; Goleva, O.V.; Kharit, S.M. The vaccine coverage and vaccine immunity status and risk factors of non-protective levels of antibodies against vaccines in children with juvenile idiopathic arthritis: Cross-sectional Russian tertiary Centre study. Pediatr. Rheumatol. 2021, 19, 108. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Conti, F.; Rezai, S.; Valesini, G. Vaccination and autoimmune rheumatic diseases. Autoimmun. Rev. 2008, 8, 124–128. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://immunizationdata.who.int/global/wiise-detail-page/vaccination-schedule-for-country_name?DISEASECODE=&TARGETPOP_GENERAL= (accessed on 9 February 2025).
- Nikishina, I.; Ruperto, N.; Kuzmina, N.; Shelepina, T.; Illarionova, O.; Salougina, S.; Kaleda, M.; Borodacheva, O.; Paediatric Rheumatology International Trials Organisation. The Russian version of the Childhood Health Assessment Questionnaire (CHAQ) and the Child Health Questionnaire (CHQ). Clin. Exp. Rheumatol. 2001, 19, S131–S135. [Google Scholar] [PubMed]
- Wallace, C.A.; Giannini, E.H.; Huang, B.; Itert, L.; Ruperto, N.; Childhood Arthritis Rheumatology Research Alliance; Pediatric Rheumatology Collaborative Study Group; Paediatric Rheumatology International Trials Organisation. American College of Rheumatology provisional criteria for defining clinical in-active disease in select categories of juvenile idiopathic arthritis. Arthritis Care Res. 2011, 63, 929–936. [Google Scholar] [CrossRef]
- Rákóczi, É.; Szekanecz, Z. Pneumococcal vaccination in autoimmune rheumatic diseases. RMD Open 2017, 3, e000484. [Google Scholar] [CrossRef]
- Clemente, D.; Leon, L.; Foster, H.; Carmona, L.; Minden, K. Transitional care for rheumatic conditions in Europe: Current clinical practice and available resources. Pediatr. Rheumatol. 2017, 15, 49. [Google Scholar] [CrossRef]
- Nakashima, K.; Aoshima, M.; Ohfuji, S.; Yamawaki, S.; Nemoto, M.; Hasegawa, S.; Noma, S.; Misawa, M.; Hosokawa, N.; Yaegashi, M.; et al. Immunogenicity of simultaneous versus sequential administration of a 23-valent pneumococcal polysaccharide vaccine and a quadrivalent influenza vaccine in older individuals: A randomized, open-label, non-inferiority trial. Hum. Vaccines Immunother. 2018, 14, 1923–1930. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Berho, J.; Monsalvez, M.-P.; Inostroza, J.; Rojas, J.; Quezada, A. Pneumococcal vaccine in patients with idiopathic juvenile arthritis in treatment with tumor necrosis factor inhibitors. Allergol. Immunopathol. 2021, 49, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Alexeeva, E.I.; Dvoryakovskaya, T.M.; Denisova, R.V.; Isaeva, K.B.; Soloshenko, M.A.; Mamutova, A.V.; Mayansky, N.A.; Tkachenko, N.E.; Zubkova, I.V.; Kaluzhnaya, T.A.; et al. Immunization With a Pneumococcal Polysaccharide Vaccine in Children With Juvenile Idiopathic Arthritis Without Systemic Manifestations: A Prospective Study. Curr. Pediatr. 2017, 16, 493–501. [Google Scholar] [CrossRef]
- Aikawa, N.E.; França, I.L.; Ribeiro, A.C.; Sallum, A.M.; Bonfa, E.; Silva, C.A. Short and long-term immunogenicity and safety following the 23-valent polysaccharide pneumococcal vaccine in juvenile idiopathic arthritis patients under conventional DMARDs with or without anti-TNF therapy. Vaccine 2015, 33, 604–609. [Google Scholar] [CrossRef] [PubMed]
- Rákóczi, É.; Perge, B.; Végh, E.; Csomor, P.; Pusztai, A.; Szamosi, S.; Bodnár, N.; Szántó, S.; Szücs, G.; Szekanecz, Z. Evaluation of the immunogenicity of the 13-valent conjugated pneumococcal vaccine in rheumatoid arthritis patients treated with etanercept. Jt. Bone Spine 2016, 83, 675–679. [Google Scholar] [CrossRef] [PubMed]
- Walker, U.A.; Hoffman, H.M.; Williams, R.; Kuemmerle-Deschner, J.; Hawkins, P.N. Brief Report: Severe Inflammation Following Vaccination Against Streptococcus pneumoniae in Patients With Cryopyrin-Associated Periodic Syndromes. Arthritis Rheumatol. 2016, 68, 516–520. [Google Scholar] [CrossRef]
- Hu, R.; Liu, Y.; Zhang, L.; Kang, G.; Xu, B.; Li, M.; Yu, J.; Zhu, Y.; Guo, H.; Wang, Z. Post-marketing safety surveillance for both CRM197 and TT carrier proteins PCV13 in Jiangsu, China. Front. Public Health 2023, 11, 1272562. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Keller, M.; Pittet, L.F.; Zimmermann, P. Immunogenicity and safety of routine vaccines in children and adolescents with rheumatic diseases on immunosuppressive treatment—A systematic review. Eur. J. Pediatr. 2022, 181, 1329–1362. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Alfayadh, N.M.; Gowdie, P.J.; Akikusa, J.D.; Easton, M.L.; Buttery, J.P. Vaccinations Do Not Increase Arthritis Flares in Juvenile Idiopathic Arthritis: A Study of the Relationship between Routine Childhood Vaccinations on the Australian Immunisation Schedule and Arthritis Activity in Children with Juvenile Idiopathic Arthritis. Int. J. Rheumatol. 2020, 2020, 1078914. [Google Scholar] [CrossRef]
- Koh, J.H.; Lee, J.; Kim, S.H.; Kwok, S.-K.; Ju, J.H.; Park, S.-H. Safety, and Humoral and Cell-mediated Immune Responses to Herpes Zoster Vaccine in Patients with Rheumatoid Arthritis. J. Rheumatol. 2018, 45, 465–469. [Google Scholar] [CrossRef] [PubMed]
- Nagra, D.; Bechman, K.; Russell, M.D.; Yang, Z.; Adas, M.; Subesinghe, S.; Rutherford, A.; Alveyn, E.; Patel, S.; Wincup, C.; et al. No Waning of Pneumococcal Vaccine Responses over Time in People with Inflammatory Arthritis: Findings from a Single Centre Cohort. Vaccines 2024, 12, 69. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]

| JIA Features | Results, n = 371 (%) |
|---|---|
| Demography | |
| Sex, female, n (%) | 234 (63) |
| Age at baseline *, years ± SD | 10.9 ± 4.2 |
| JIA category, n (%) | |
| Extended oligoarthritis | 2 (0.5) |
| Persistent oligoarthritis | 167 (45) |
| Polyarthritis, RF-negative | 164 (44.2) |
| Polyarthritis, RF-positive | 12 (3.2) |
| Psoriatic arthritis | 2 (0.5) |
| Enthesitis-related arthritis | 24 (6.5) |
| Uveitis, n (%) | 67 (18) |
| ENT diseases, n (%) | 119 (32) |
| Treatment at baseline | |
| NSAIDs, n (%) | 13 (3.5) |
| Oral corticosteroids, n (%) | 3 (0.8) |
| Methotrexate, n (%) | 136 (36.7) |
| Cyclosporine A, n (%) | 27 (5.9) |
| Sulfasalazine, n (%) | 8 (2.2) |
| Leflunomide, n (%) | 7 (1.9) |
| Mofetyl mycophenolate, n (%) | 1 (0.3) |
| Biologic treatment * | 217 (58.5) |
| Etanercept | 70 (18.9) |
| Adalimumab | 26 (7.0) |
| Tocilizumab | 6 (1.6) |
| Etanercept + nbDMARD | 54 (14.0) |
| Adalimumab + nbDMARD | 52 (14.0) |
| Tocilizumab + nbDMARD | 9 (2.4) |
| Parameters (n = 371) n (%)/Me (IQR) [Min; Max] | D1 | D22 | EOS | p1 | p2 | p3 | p Total |
|---|---|---|---|---|---|---|---|
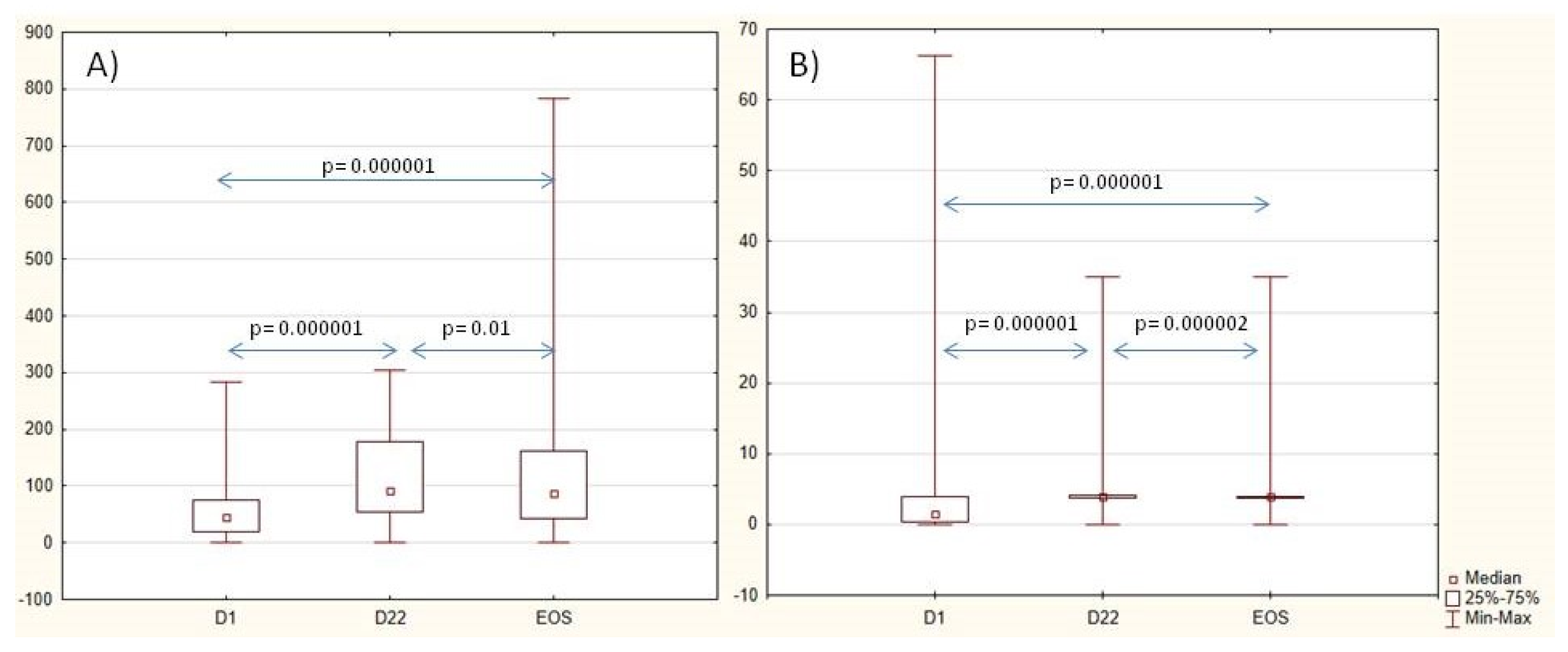
| Anti-SP IgG titer, U/mL * | 44 (19; 74) [0–283] | 90 (52; 179) [0–304] | 83 (40; 162) [0–784] | 0.000001 | 0.000001 | 0.01 | 0.000001 |
| Protective titer anti-SP IgG, n (%) 95% CI | 339 (91) [88; 94] | 359 (97) [95; 98] | 351 (95) [92; 97] | <0.001 | <0.001 | >0.05 | <0.001 |
| Patients with a two-fold-increased anti-SP titer, n (%) [95% CI] | - | 168 (45) [40; 51] | 185 (50) [45; 52] | - | <0.001 | <0.001 | <0.001 |
| Anti-Hib titer, U/mL, median (IQR) [min; max] | 1.2 (0.3; 4.0) [0.0; 66.3] | 4.0 (4.0; 4.0) [0; 35] | 4.0 (3.8; 4.0) [0.1; 35.0] | 0.000001 | 0.000001 | 0.00002 | 0.000001 |
| Patients with a protective anti-HIb titer, n (%) [95% CI] | 200 (54) [49; 59] | 355 (96) [93; 97] | 346 (94) [90; 97] | <0.001 | <0.001 | <0.001 | <0.001 |
| Patients with a two-fold-increased anti-HIb titer, n (%) [95% CI] | - | 209 (56) [51; 61] | 196 (53) [48; 58] | - | <0.001 | >0.05 | <0.001 |
| S-100 U/mL (n.v. > 2.9), Me (IQR) [min; max] | 2.3 (1.3; 3.9) [0.0; 95.0] | 2.6 (1.4; 4.4) [0.0; 169.0] | 0.67 (0.3; 1.7) [0.0; 168.0] | 0.024 | 0.001 | 0.001 | 0.000001 |
| hs-CRP, U/mL (n.v. > 8.2) Me (IQR) [min; max] | 0.6 (0.2; 1.6) [0.0; 61.5] | 0.7 (0.3; 1.9) [0.0; 69.0] | 0.78 (0.3; 2.0) [0.0; 41.3] | 0.001 | 0.179 | 0.182 | 0.001 |
| Active joints, Me (IQR) [min; max] | 0.0 (0.0; 1.0) [0.0; 44.0] | 0.0 (0.0;0.25) [0.0; 36.0] | 0.0 (0.0; 0.0) [0.0; 28.0] | 0.002 | 0.000001 | 0.000001 | 0.000001 |
| Joints with limited ROM, Me (IQR) [min; max] | 0.0 (0.0; 2.0) [0.0; 45.0] | 0.0 (0.0; 2.0) [0.0; 45.0] | 0.0 (0.0; 0.0) [0.0; 28.0] | 0.009 | 0.000001 | 0.000006 | 0.000001 |
| Morning stiffness, min, Me (IQR) [min; max] | 0 (0; 0) [0; 360] | 0 (0; 6) [0; 180] | 0 (0; 0) [0; 180] | 0.000003 | 0.000001 | 0.000001 | 0.000001 |
| MDVAS, mm, Me (IQR) [min; max] | 0 (0; 8) [0; 88] | 0 (0; 10) [0; 85] | 0 (0; 0) [0; 56] | 0.000003 | 0.0000001 | 0.0000001 | 0.000001 |
| Patient/parent VAS, mm, Me (IQR) [min; max] | 0 (0; 10) [0; 90] | 0 (0; 10) [0; 88] | 0 (0; 0) [0; 66] | 0.000001 | 0.0000001 | 0.0000001 | 0.000001 |
| CHAQ, points, Me (IQR) [min; max] | 0.0 (0.0;0.13) [0.0; 2.8] | 0.0 (0.0; 0.0) [0.0; 2.5] | 0.0 (0.0; 0.0) [0.0; 2.3] | 0.01 | 0.0000001 | 0.000001 | 0.000001 |
| ESR, mm/hr (n.v = 0–20) Me (IQR) [min; max] | 3 (2; 8) [0; 67] | 4 (2; 6) [0; 50] | 3 (2; 6) [0; 53] | 0.003 | 0.026 | 0.473 | 0.016 |
| CRP, mg/mL (n.v. < 5) Me (IQR) [min; max] | 1.0 (0.5; 1.2) [0.0; 74.1] | 1.0 (0.4; 1.1) [0.0; 105.1] | 0.7 (0.3; 1.3) [0.0; 40.2] | 0.024 | 0.0002 | 0.01 | 0.000001 |
| Characteristic | Univariate | Multivariate | ||
|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| bDMARD before vaccination | ||||
| did not receive bDMARD | — | — | ||
| received bDMARD | 0.75 (0.27: 1.87) | 0.5 | 0.73 (0.23; 2.42) | 0.6 |
| DMARD before vaccination | ||||
| did not receive methotrexate | — | — | ||
| methotrexate | 1.15 (0.42; 2.89) | 0.8 | 0.96 (0.30; 3.17) | >0.9 |
| S-100 before vaccination | 0.98 (0.95; 1.04) | 0.4 | 0.98 (0.94; 1.03) | 0.2 |
| CRP before vaccination | 1.03 (0.96; 1.21) | 0.6 | 0.97 (0.90; 1.11) | 0.5 |
| Active joints | 1.02 (0.93; 1.26) | 0.8 | 1.19 (0.96; 1.61) | 0.2 |
| CHAQ | 0.68 (0.31; 1.97) | 0.4 | 0.18 (0.04; 0.92) | 0.026 |
| ESR | 1.16 (1.02; 1.43) | 0.072 | 1.21 (1.05; 1.50) | 0.041 |
| Characteristic | Univariate | Multivariate | ||
|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| bDMARD before vaccination | ||||
| did not receive bDMARD | — | — | ||
| received bDMARD | 0.45 (0.16; 1.11) | 0.10 | 0.29 (0.10; 0.79) | 0.019 |
| DMARD before vaccination | ||||
| did not receive methotrexate | — | — | ||
| methotrexate | 0.69 (0.24; 1.69) | 0.4 | 0.39 (0.13; 1.05) | 0.072 |
| S-100 before vaccination | 1.11 (0.98; 1.37) | 0.2 | 1.08 (0.98; 1.33) | 0.3 |
| CRP before vaccination | 1.02 (0.96; 1.15) | 0.7 | 1.02 (0.95; 1.16) | 0.6 |
| Active joints | 0.97 (0.91; 1.06) | 0.3 | 0.91 (0.75; 1.06) | 0.2 |
| CHAQ | 0.89 (0.39; 2.81) | 0.8 | 2.34 (0.46; 25.5) | 0.4 |
| ESR | 1.0 (0.96; 1.07) | 0.9 | 1.0 (0.95; 1.07) | 0.9 |
| Infection Burden Indicators, Me (IQR) [Min; Max] | 6 Months Prior to Vaccination | 6 Months After Vaccination | p-Value |
|---|---|---|---|
| Duration of ARI episode *, days | 9.0 (5.0; 10.0) | 2.0 (1.0; 3.0) | <0.001 |
| [0.0; 19.0] | [0.0; 15.0] | ||
| The number of ARI episodes per patient * | 4.0 (3.0; 5.0) | 2.0 (1.0; 2.0) | <0.001 |
| [0.00; 9.00] | [0.0; 5.0] | ||
| The number of courses of antibacterial drugs * | 2.0 (2.0; 3.0) | 1.0 (0.0; 1.0) | <0.001 |
| [0.0; 6.0] | [0.0; 3.0] | ||
| Patients without ARI, n (%) | 21 (5.7) | 62 (16.7) | <0.001 |
| Patients did not require antibacterial drugs, n (%) | 40 (10.8) | 87 (23.5) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alexeeva, E.; Dvoryakovskaya, T.; Fetisova, A.; Kriulin, I.; Krekhova, E.; Kabanova, A.; Labinov, V.; Labinova, E.; Kostik, M. The Efficacy and Safety of Simultaneous Vaccination with Polysaccharide Conjugate Vaccines Against Pneumococcal (13-Valent Vaccine) and Haemophilus influenzae Type b Infections in Children with Juvenile Idiopathic Arthritis Without Systemic Manifestations: A Prospective Cohort Study. Vaccines 2025, 13, 177. https://doi.org/10.3390/vaccines13020177
Alexeeva E, Dvoryakovskaya T, Fetisova A, Kriulin I, Krekhova E, Kabanova A, Labinov V, Labinova E, Kostik M. The Efficacy and Safety of Simultaneous Vaccination with Polysaccharide Conjugate Vaccines Against Pneumococcal (13-Valent Vaccine) and Haemophilus influenzae Type b Infections in Children with Juvenile Idiopathic Arthritis Without Systemic Manifestations: A Prospective Cohort Study. Vaccines. 2025; 13(2):177. https://doi.org/10.3390/vaccines13020177
Chicago/Turabian StyleAlexeeva, Ekaterina, Tatyana Dvoryakovskaya, Anna Fetisova, Ivan Kriulin, Elizaveta Krekhova, Anna Kabanova, Vladimir Labinov, Elizaveta Labinova, and Mikhail Kostik. 2025. "The Efficacy and Safety of Simultaneous Vaccination with Polysaccharide Conjugate Vaccines Against Pneumococcal (13-Valent Vaccine) and Haemophilus influenzae Type b Infections in Children with Juvenile Idiopathic Arthritis Without Systemic Manifestations: A Prospective Cohort Study" Vaccines 13, no. 2: 177. https://doi.org/10.3390/vaccines13020177
APA StyleAlexeeva, E., Dvoryakovskaya, T., Fetisova, A., Kriulin, I., Krekhova, E., Kabanova, A., Labinov, V., Labinova, E., & Kostik, M. (2025). The Efficacy and Safety of Simultaneous Vaccination with Polysaccharide Conjugate Vaccines Against Pneumococcal (13-Valent Vaccine) and Haemophilus influenzae Type b Infections in Children with Juvenile Idiopathic Arthritis Without Systemic Manifestations: A Prospective Cohort Study. Vaccines, 13(2), 177. https://doi.org/10.3390/vaccines13020177







