Development of a Chimeric Vaccine Providing Protection Against the Type A ASIA/Sea-97 FMDVs in East Asia
Abstract
1. Introduction
2. Materials and Methods
2.1. Cells
2.2. Viruses
2.3. Targeted Mutagenesis and Subcloning
2.4. Virus Recovery and Cell Culture
2.5. Viral Cultivation and Purification
2.6. Preparation of the Candidate Vaccines
2.7. Vaccination and Virus Challenge in Mice
2.8. Vaccination and Virus Challenge in Pigs
2.9. Evaluation of the Immune Response to the Candidate Vaccine in Pigs
2.10. Measurement of Structural Protein (SP)-Specific Antibody Levels
2.11. Virus Neutralization Assay
2.12. Virus Detection in Vaccinated and Challenged Pigs
2.13. Statistical Analysis
2.14. Ethics Statement
3. Results
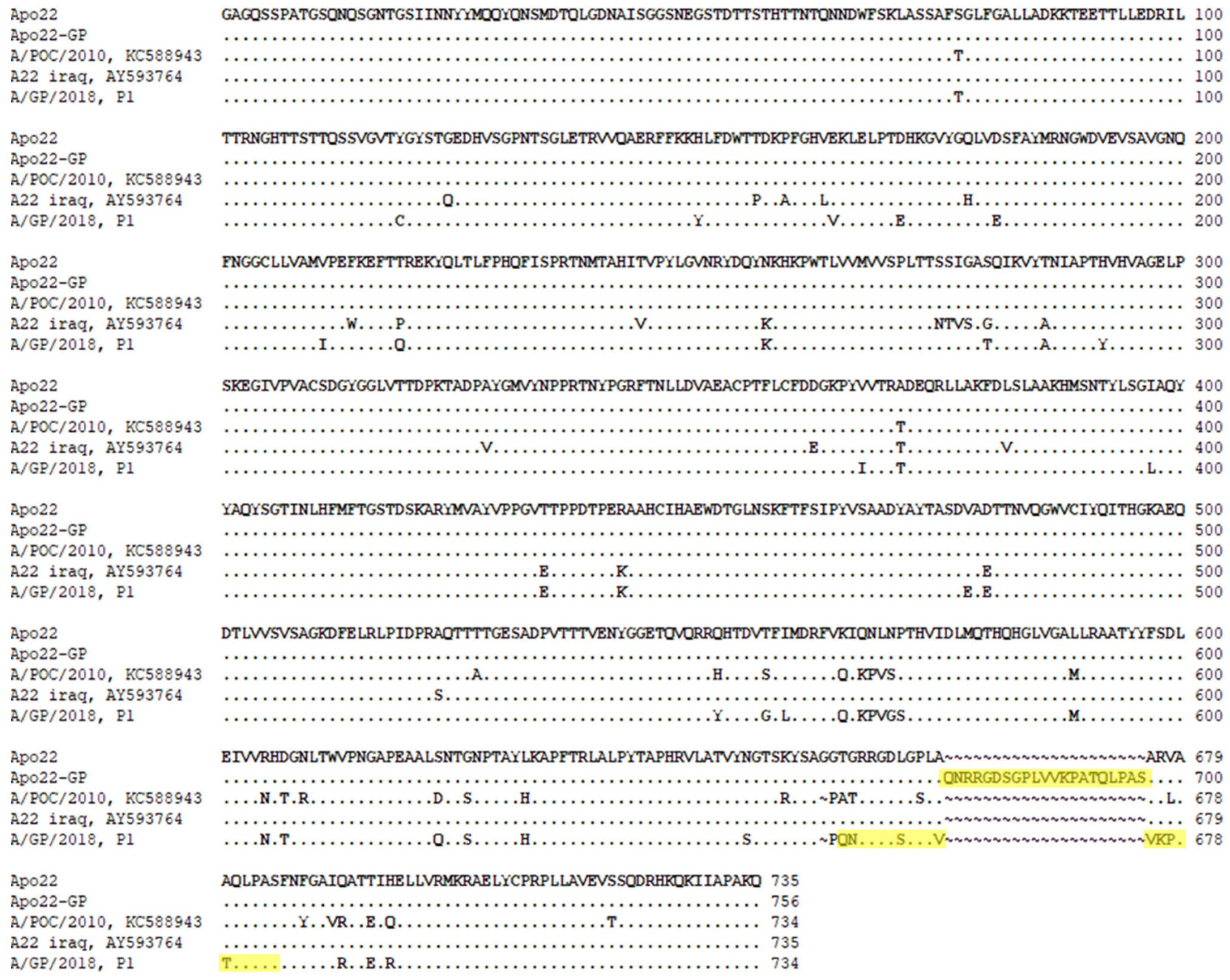
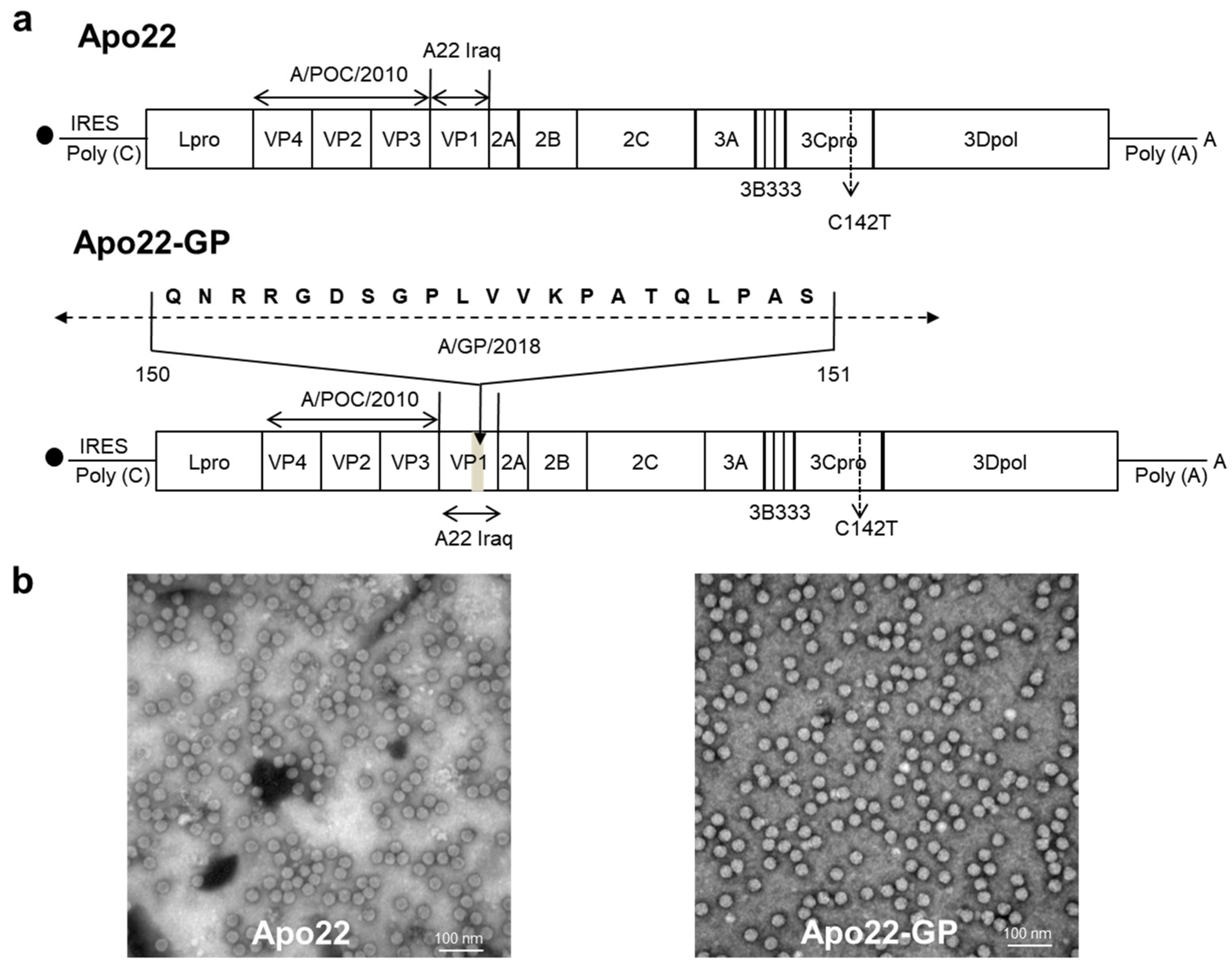
3.1. Comparison of the Amino Acid Sequences of the Apo22 and Apo22-GP SPs
3.2. Development of Chimeric Viruses
3.3. Protection of Candidate Vaccines in Mice Against Type A Viruses
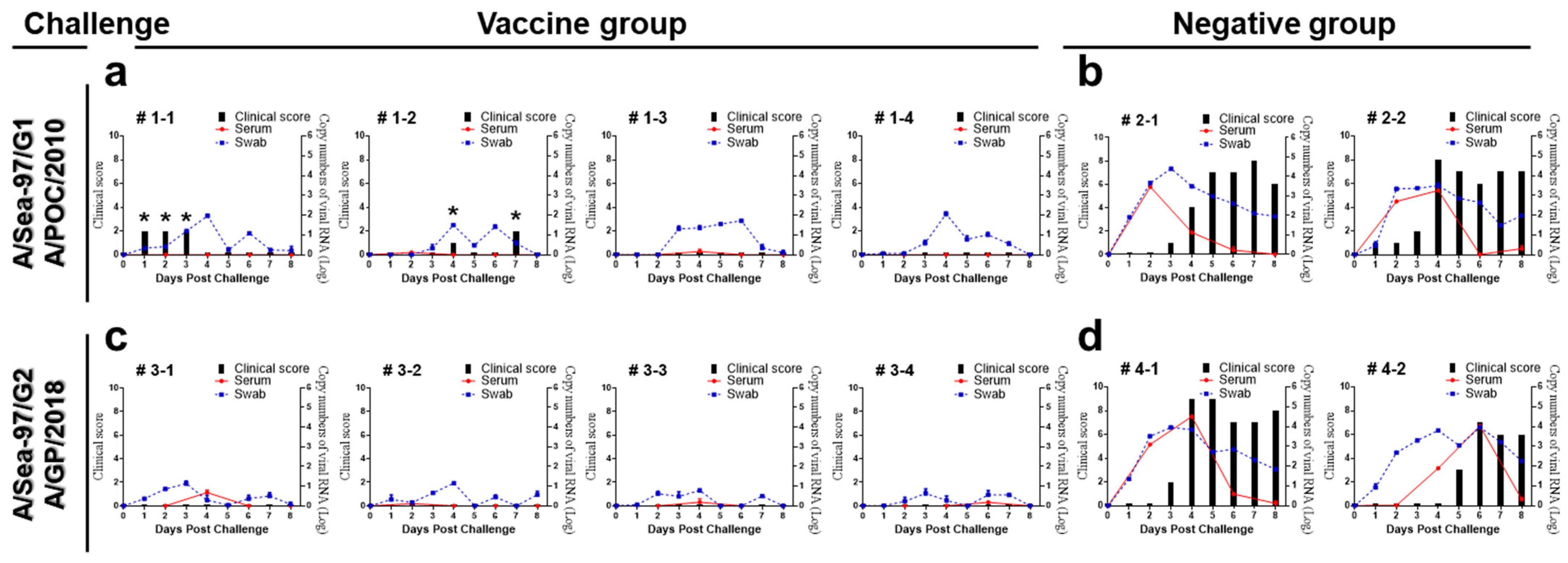
3.4. Protective Efficacy of the Apo22-GP Vaccine Against Type A FMDV Challenge in Pigs
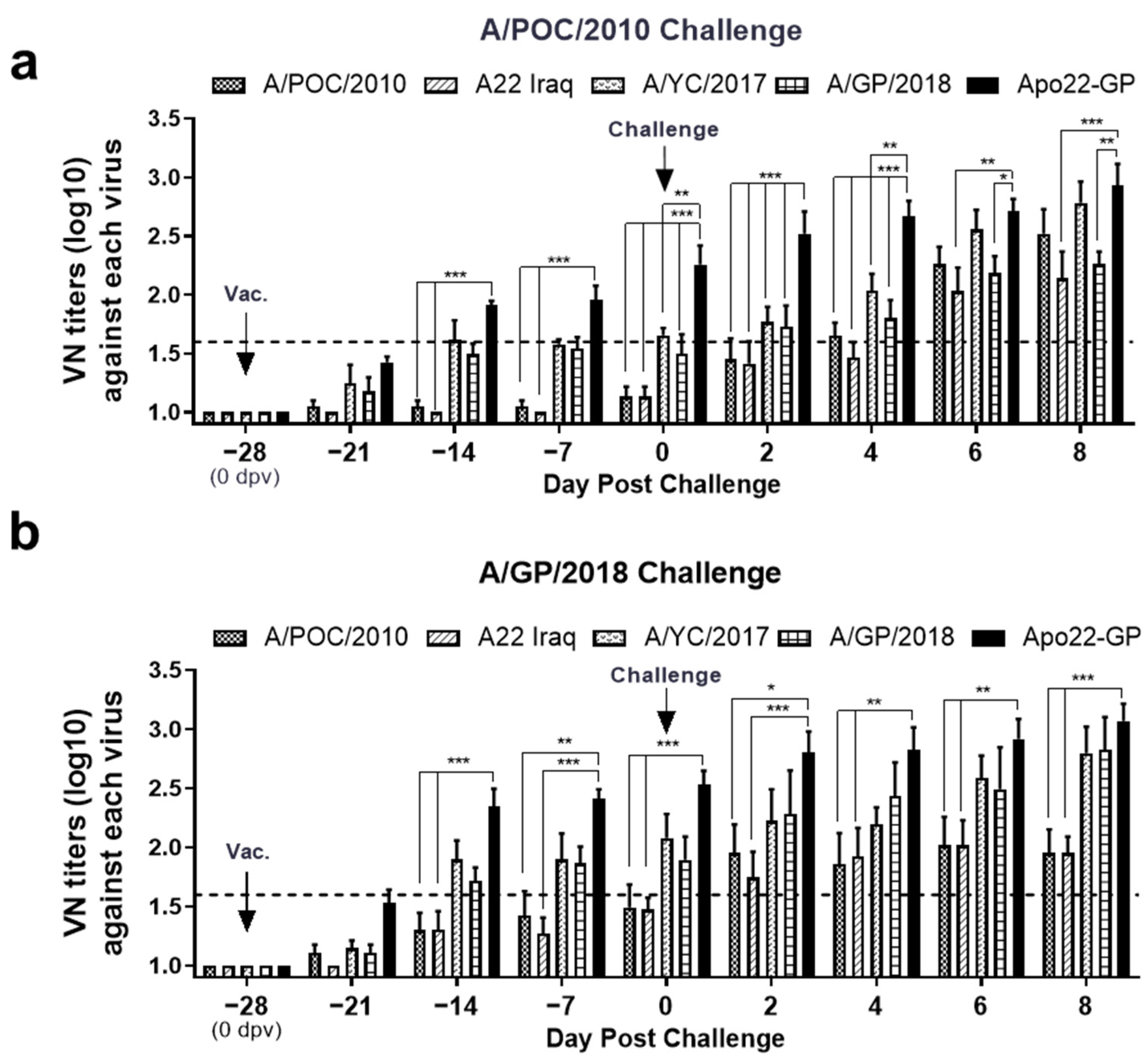
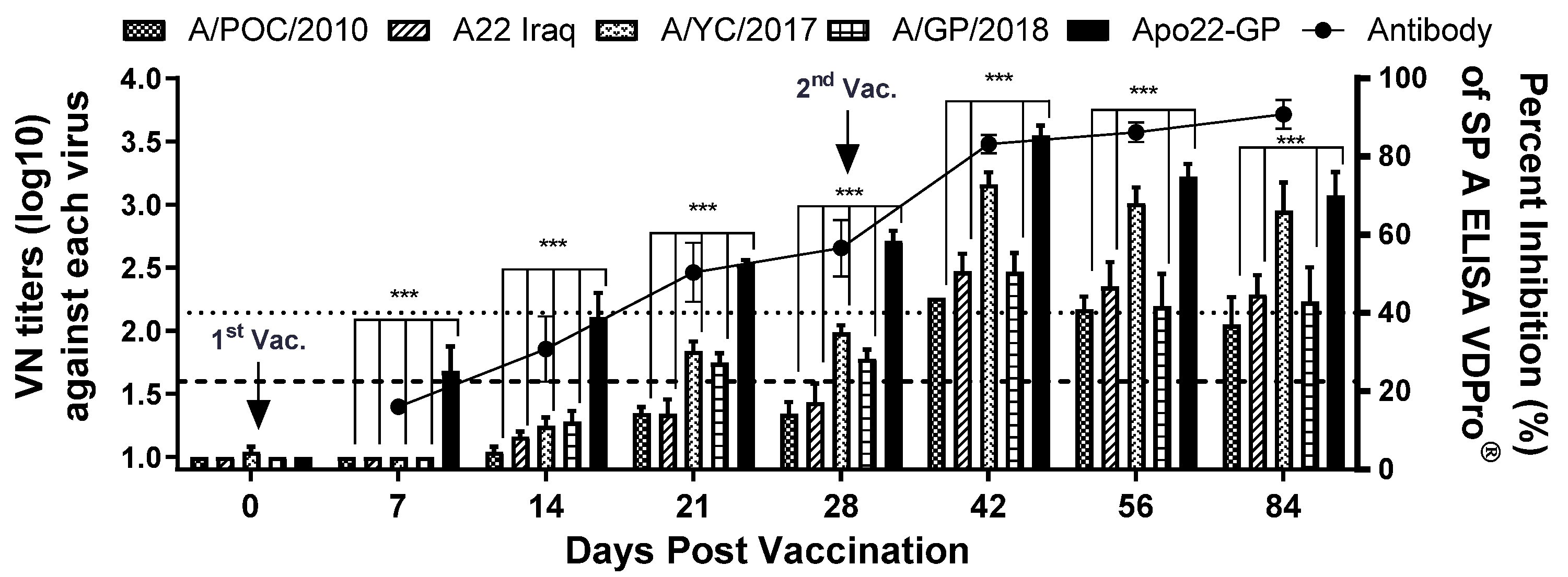
3.5. Neutralizing Antibody Response to Apo22-GP Vaccination and Type A Challenge in Pigs
3.6. Assessment of Neutralizing Antibodies Levels Induced by the Apo22-GP Vaccine in Pigs
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Abubakar, M.; Syed, Z.; Manzoor, S.; Arshed, M.J. Deciphering Molecular Dynamics of Foot and Mouth Disease Virus (FMDV): A Looming Threat to Pakistan’s Dairy Industry. Dairy 2022, 3, 123–136. [Google Scholar] [CrossRef]
- Jamal, S.M.; Belsham, G.J. Foot-and-mouth disease: Past, present and future. Vet. Res. 2013, 44, 116. [Google Scholar] [CrossRef]
- Paton, D.J.; Valarcher, J.F.; Bergmann, I.; Matlho, O.G.; Zakharov, V.M.; Palma, E.L.; Thomson, G.R. Selection of foot and mouth disease vaccine strains—A review. Rev. Sci. Tech. 2005, 24, 981–993. [Google Scholar] [CrossRef]
- Paton, D.J.; Sumption, K.J.; Charleston, B. Options for control of foot-and-mouth disease: Knowledge, capability and policy. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2009, 364, 2657–2667. [Google Scholar] [CrossRef]
- Silas Lendzele, S. Foot and Mouth Disease in Cameroon: A Systematic Review to Support its Progressive Control. J. Clin. Vet. Res. 2022, 2, 1–14. [Google Scholar] [CrossRef]
- Hammond, J.M.; Maulidi, B.; Henning, N. Targeted FMD Vaccines for Eastern Africa: The AgResults Foot and Mouth Disease Vaccine Challenge Project. Viruses 2021, 13, 1830. [Google Scholar] [CrossRef] [PubMed]
- Lyons, N.A.; Ludi, A.B.; Wilsden, G.; Hamblin, P.; Qasim, I.A.; Gubbins, S.; King, D.P. Evaluation of a polyvalent foot-and-mouth disease virus vaccine containing a Saudi-95 against field challenge on large-scale dairy farms in Saudi Arabia with the emerging A/ASIA/G-VII viral lineage. Vaccine 2017, 35, 6850–6857. [Google Scholar] [CrossRef]
- Mahapatra, M.; Parida, S. Foot and mouth disease vaccine strain selection: Current approaches and future perspectives. Expert Rev. Vaccines 2018, 17, 577–591. [Google Scholar] [CrossRef]
- Fernandez-Sainz, I.; Gavitt, T.D.; Koster, M.; Ramirez-Medina, E.; Rodriguez, Y.Y.; Wu, P.; Silbart, L.K.; de Los Santos, T.; Szczepanek, S.M. The VP1 G-H loop hypervariable epitope contributes to protective immunity against Foot and Mouth Disease Virus in swine. Vaccine 2019, 37, 3435–3442. [Google Scholar] [CrossRef] [PubMed]
- Mahapatra, M.; Statham, B.; Li, Y.; Hammond, J.; Paton, D.; Parida, S. Emergence of antigenic variants within serotype A FMDV in the Middle East with antigenically critical amino acid substitutions. Vaccine 2016, 34, 3199–3206. [Google Scholar] [CrossRef] [PubMed]
- Hwang, J.H.; Lee, G.; Kim, A.; Park, J.H.; Lee, M.J.; Kim, B.; Kim, S.M. A Vaccine Strain of the A/ASIA/Sea-97 Lineage of Foot-and-Mouth Disease Virus with a Single Amino Acid Substitution in the P1 Region That Is Adapted to Suspension Culture Provides High Immunogenicity. Vaccines 2021, 9, 308. [Google Scholar] [CrossRef] [PubMed]
- Bae, S.; Li, V.; Hong, J.; Kim, J.N.; Kim, H. Phylogenetic and evolutionary analysis of foot-and-mouth disease virus A/ASIA/Sea-97 lineage. Virus Genes 2021, 57, 443–447. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.W.; Cho, G.; Kim, H.; Lee, G.; Lim, T.G.; Kwak, H.Y.; Park, J.H.; Park, S.H. Immunogenicity and Protection against Foot-and-Mouth Disease Virus in Swine Intradermally Vaccinated with a Bivalent Vaccine of Foot-and-Mouth Disease Virus Type O and A. Vaccines 2023, 11, 815. [Google Scholar] [CrossRef]
- Shin, S.H.; Hwang, S.Y.; Kim, H.M.; Shin, S.H.; Ko, M.K.; Lee, M.J.; Kim, S.M.; Park, J.H. Evaluation of a Vaccine Candidate Designed for Broad-Spectrum Protection against Type A Foot-and-Mouth Disease in Asia. Vaccines 2024, 12, 64. [Google Scholar] [CrossRef]
- Lee, S.Y.; Lee, Y.J.; Kim, R.H.; Park, J.N.; Park, M.E.; Ko, M.K.; Choi, J.H.; Chu, J.Q.; Lee, K.N.; Kim, S.M.; et al. Rapid Engineering of Foot-and-Mouth Disease Vaccine and Challenge Viruses. J. Virol. 2017, 91, e00155-17. [Google Scholar] [CrossRef]
- Ito, N.; Takayama-Ito, M.; Yamada, K.; Hosokawa, J.; Sugiyama, M.; Minamoto, N. Improved recovery of rabies virus from cloned cDNA using a vaccinia virus-free reverse genetics system. Microbiol. Immunol. 2003, 47, 613–617. [Google Scholar] [CrossRef]
- WOAH. Manual of Diagnostic Tests and Vaccines for Terrestrial Animals, Chapter 3.1.8 Foot and Mouth Disease. Available online: https://www.woah.org/fileadmin/Home/eng/Health_standards/tahm/3.01.08_FMD.pdf (accessed on 27 July 2022).
- Aslam, M.; Alkheraije, K.A. The prevalence of foot-and-mouth disease in Asia. Front. Vet. Sci. 2023, 10, 1201578. [Google Scholar] [CrossRef]
- WRLFMD. Country Reports. Available online: https://www.wrlfmd.org/country-reports/east-and-southeast-asia (accessed on 16 October 2025).
- WRLFMD. Quarterly Reports. Available online: https://www.wrlfmd.org/2025-quarter-2-apr-jun (accessed on 17 October 2025).
- Parida, S.; Oh, Y.; Reid, S.M.; Cox, S.J.; Statham, R.J.; Mahapatra, M.; Anderson, J.; Barnett, P.V.; Charleston, B.; Paton, D.J. Interferon-gamma production in vitro from whole blood of foot-and-mouth disease virus (FMDV) vaccinated and infected cattle after incubation with inactivated FMDV. Vaccine 2006, 24, 964–969. [Google Scholar] [CrossRef]
- Oh, Y.; Fleming, L.; Statham, B.; Hamblin, P.; Barnett, P.; Paton, D.J.; Park, J.H.; Joo, Y.S.; Parida, S. Interferon-γ induced by in vitro re-stimulation of CD4+ T-cells correlates with in vivo FMD vaccine induced protection of cattle against disease and persistent infection. PLoS ONE 2012, 7, e44365. [Google Scholar] [CrossRef]
- Zhang, L.; Feng, X.; Jin, Y.; Ma, J.; Cai, H.; Zhang, X. Immunoprotective mechanisms in swine within the “grey zone” in antibody response after immunization with foot-and-mouth disease vaccine. Virus Res. 2016, 220, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Saeed, A.; Kanwal, S.; Arshad, M.; Ali, M.; Shaikh, R.S.; Abubakar, M. Foot-and-mouth disease: Overview of motives of disease spread and efficacy of available vaccines. J. Anim. Sci. Technol. 2015, 57, 10. [Google Scholar] [CrossRef] [PubMed]
- Childs, K.; Harvey, Y.; Waters, R.; Woma, T.; Wilsden, G.; Sun, H.; Sun, P.; Seago, J. Development of a quadrivalent foot-and-mouth disease vaccine candidate for use in East Africa. Vaccine 2023, 41, 6572–6578. [Google Scholar] [CrossRef]
- Shao, J.; Liu, W.; Gao, S.; Chang, H.; Guo, H. A recombinant multi-epitope trivalent vaccine for foot-and-mouth disease virus serotype O in pigs. Virology 2024, 596, 110103. [Google Scholar] [CrossRef] [PubMed]
- Zha, J.; Zhang, K.; Zhang, X.; Sun, P.; Li, D.; Cao, Y.; Bai, X.; Ma, X.; Li, K.; Yuan, H.; et al. Foot-and-mouth disease virus vaccine with VP1 G-H loop substitution of the Cathay strain broadens antigen spectrum. Appl. Microbiol. Biotechnol. 2025, 109, 199. [Google Scholar] [CrossRef] [PubMed]
| Group (Cage) | No. of Animals | Experimental Group | Challenge Virus (1 × 105 TCID50/0.1 mL) | Days of Blood Collection (dpc) | Days of Oral Swab Collection (dpc) | Comments |
|---|---|---|---|---|---|---|
| 1 (1) | 4 | Apo22-GP | A/POC/2010 | −28, −21, −14, −7, 0, 2, 4, 6, 8 | 0~8 | Animals exhibiting clinical signs after challenge were isolated in an empty cage. |
| 2 (1) | 2 | Negative group | ||||
| 3 (2) | 4 | Apo22-GP | A/GP/2018 | |||
| 4 (2) | 2 | Negative group |
| Vaccine Candidate | Challenge Viruses (PD50) | |||
|---|---|---|---|---|
| G1 (A/POC/2010) (1) | A22 IRAQ (1) | G2 (A/YC/2017) (2) | G2 (A/GP/2018) (2) | |
| Apo22 | >128.0 * | >128.0 * | 107.6 | 238.9 |
| Apo22-GP | >128.0 * | >128.0 * | >362.0 | >362.0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shin, S.; Hwang, S.Y.; Ko, M.-K.; Lee, M.J.; Kim, S.-M.; Kim, J.; Park, J.-H. Development of a Chimeric Vaccine Providing Protection Against the Type A ASIA/Sea-97 FMDVs in East Asia. Vaccines 2025, 13, 1104. https://doi.org/10.3390/vaccines13111104
Shin S, Hwang SY, Ko M-K, Lee MJ, Kim S-M, Kim J, Park J-H. Development of a Chimeric Vaccine Providing Protection Against the Type A ASIA/Sea-97 FMDVs in East Asia. Vaccines. 2025; 13(11):1104. https://doi.org/10.3390/vaccines13111104
Chicago/Turabian StyleShin, Sungho, Seong Yun Hwang, Mi-Kyeong Ko, Min Ja Lee, Su-Mi Kim, Jaejo Kim, and Jong-Hyeon Park. 2025. "Development of a Chimeric Vaccine Providing Protection Against the Type A ASIA/Sea-97 FMDVs in East Asia" Vaccines 13, no. 11: 1104. https://doi.org/10.3390/vaccines13111104
APA StyleShin, S., Hwang, S. Y., Ko, M.-K., Lee, M. J., Kim, S.-M., Kim, J., & Park, J.-H. (2025). Development of a Chimeric Vaccine Providing Protection Against the Type A ASIA/Sea-97 FMDVs in East Asia. Vaccines, 13(11), 1104. https://doi.org/10.3390/vaccines13111104








