Development of RT-PCR Assays for Simple Detection and Identification of Sabin Virus Contaminants in the Novel Oral Poliovirus Vaccines
Abstract
1. Introduction
2. Materials and Methods
2.1. Vaccine Viruses and nOPV Batches
2.2. Primers and TaqMan Oligoprobes
2.3. Extraction of Viral RNA
2.4. mosRT-PCR Amplification
2.5. panRT-PCR Amplification
2.6. Spiking Sample Preparation for Sensitivity Evaluation of the Assays
3. Results
3.1. Design of Specific Primers and Probes for Sabin Virus Detection in nOPV
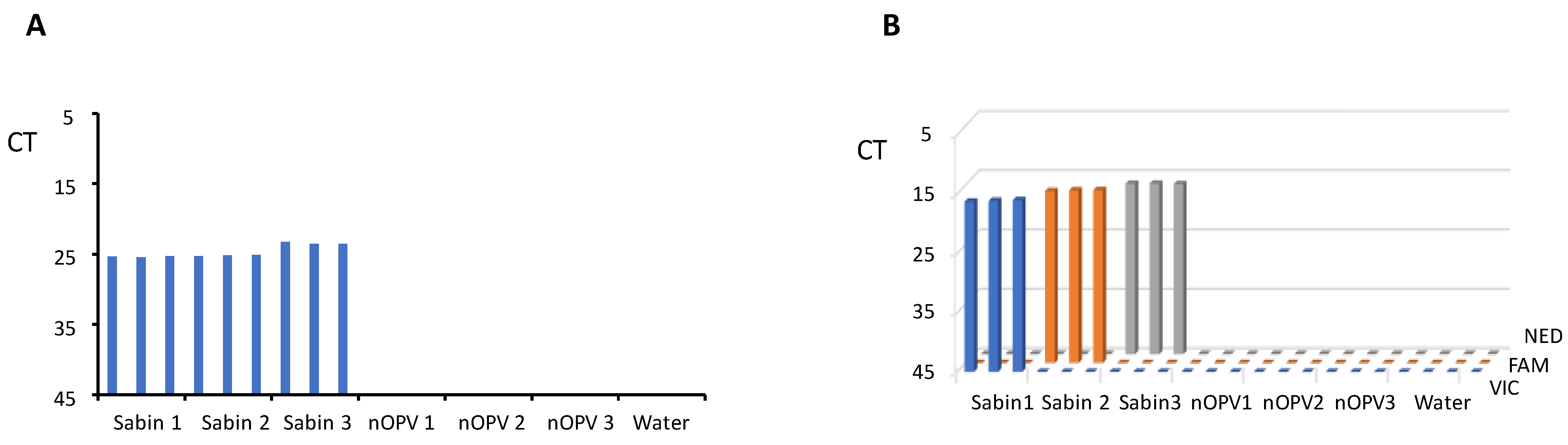
3.2. Evaluation of Assay Specificity
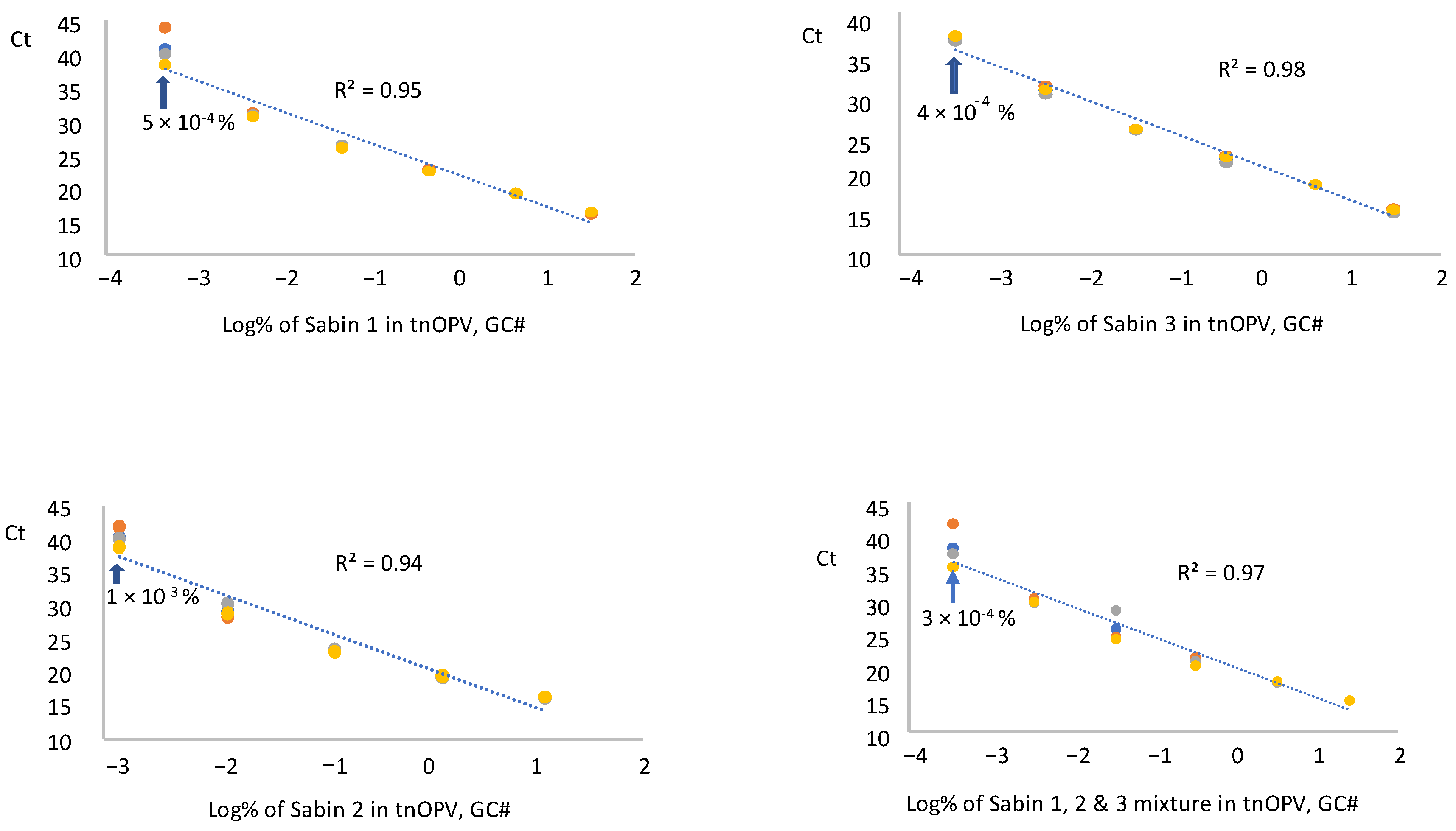
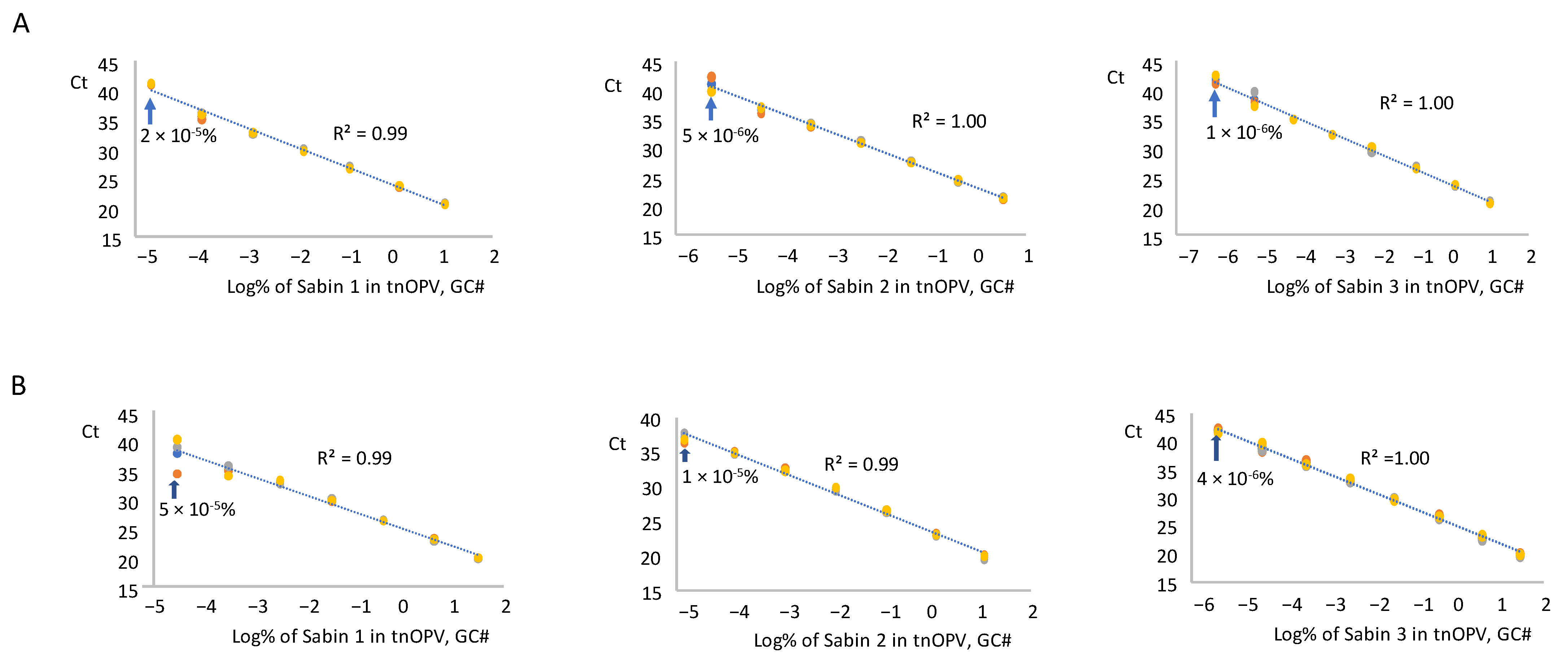
3.3. Sensitivity and Linearity
3.3.1. panRT-PCR Assay
3.3.2. mosRT-PCR Assay
3.4. Analysis of tnOPV Formulated Drug Product Lots (Mock Lots)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sutter, R.W.K.O.; Cochi, S.L.; Aylward, R.B. Poliovirus vaccine–live. In Vaccines, 6th ed.; Plotkin, S.A.O.W., Offit, P.A., Eds.; Elsevier: Amsterdam, The Netherlands, 1993; pp. 598–645. [Google Scholar]
- Yakovenko, M.L.; Korotkova, E.A.; Ivanova, O.E.; Eremeeva, T.P.; Samoilovich, E.; Uhova, I.; Gavrilin, G.V.; Agol, V.I. Evolution of the Sabin vaccine into pathogenic derivatives without appreciable changes in antigenic properties: Need for improvement of current poliovirus surveillance. J. Virol. 2009, 83, 3402–3406. [Google Scholar] [CrossRef] [PubMed]
- WHO. Global Eradication of Wild Poliovirus Type 2 Declared. Declaration Further Milestone for Globally-Coordinated Vaccineswitch in 2016. Available online: https://polioeradication.org/news/global-eradication-of-wild-poliovirus-type-2-declared/#:~:text=Global%20eradication%20of%20wild%20poliovirus,restricted%20to%20Pakistan%20and%20Afghanistan (accessed on 20 September 2015).
- WHO. Two out of Three Wild Poliovirus Strains Eradicated. Global Eradication of Wild Poliovirus Type 3 Declared on World Polio Day 2019. Available online: https://polioeradication.org/news/two-out-of-three-wild-poliovirus-strains-eradicated/ (accessed on 24 October 2019).
- John, J.; Giri, S.; Karthikeyan, A.S.; Iturriza-Gomara, M.; Muliyil, J.; Abraham, A.; Grassly, N.C.; Kang, G. Effect of a single inactivated poliovirus vaccine dose on intestinal immunity against poliovirus in children previously given oral vaccine: An open-label, randomised controlled trial. Lancet 2014, 384, 1505–1512. [Google Scholar] [CrossRef] [PubMed]
- Rubin, J.; Ottosen, A.; Ghazieh, A.; Fournier-Caruana, J.; Ntow, A.K.; Gonzalez, A.R. Managing the Planned Cessation of a Global Supply Market: Lessons Learned from the Global Cessation of the Trivalent Oral Poliovirus Vaccine Market. J. Infect. Dis. 2017, 216 (Suppl. S1), S40–S45. [Google Scholar] [CrossRef][Green Version]
- Henry, J.L.; Jaikaran, E.S.; Davies, J.R.; Tomlinson, A.J.; Mason, P.J.; Barnes, J.M.; Beale, A.J. A study of poliovaccination in infancy: Excretion following challenge with live virus by children given killed or living poliovaccine. J. Hyg. 1966, 64, 105–120. [Google Scholar] [CrossRef] [PubMed]
- Hird, T.R.; Grassly, N.C. Systematic review of mucosal immunity induced by oral and inactivated poliovirus vaccines against virus shedding following oral poliovirus challenge. PLoS Pathog. 2012, 8, e1002599. [Google Scholar] [CrossRef] [PubMed]
- Laassri, M.; Lottenbach, K.; Belshe, R.; Wolff, M.; Rennels, M.; Plotkin, S.; Chumakov, K. Effect of different vaccination schedules on excretion of oral poliovirus vaccine strains. J. Infect. Dis. 2005, 192, 2092–2098. [Google Scholar] [CrossRef]
- Brickley, E.B.; Strauch, C.B.; Wieland-Alter, W.F.; Connor, R.I.; Lin, S.; Weiner, J.A.; Ackerman, M.E.; Arita, M.; Oberste, M.S.; Weldon, W.C.; et al. Intestinal Immune Responses to Type 2 Oral Polio Vaccine (OPV) Challenge in Infants Previously Immunized with Bivalent OPV and Either High-Dose or Standard Inactivated Polio Vaccine. J. Infect. Dis. 2018, 217, 371–380. [Google Scholar] [CrossRef]
- Thompson, K.M.; Duintjer Tebbens, R.J. Lessons from the Polio Endgame: Overcoming the Failure to Vaccinate and the Role of Subpopulations in Maintaining Transmission. J. Infect. Dis. 2017, 216 (Suppl. S1), S176–S182. [Google Scholar] [CrossRef]
- Wright, P.F.; Connor, R.I.; Wieland-Alter, W.F.; Hoen, A.G.; Boesch, A.W.; Ackerman, M.E.; Oberste, M.S.; Gast, C.; Brickley, E.B.; Asturias, E.J.; et al. Vaccine-induced mucosal immunity to poliovirus: Analysis of cohorts from an open-label, randomised controlled trial in Latin American infants. Lancet Infect. Dis. 2016, 16, 1377–1384. [Google Scholar] [CrossRef]
- Wang, H. Why Have cVDPV2 Outbreaks Increased Globally After the Polio Immunization Strategy Switch: Challenges for the Polio Eradication Endgame. China CDC Wkly. 2020, 2, 176–179. [Google Scholar] [CrossRef]
- Blake, I.M.; Pons-Salort, M.; Molodecky, N.A.; Diop, O.M.; Chenoweth, P.; Bandyopadhyay, A.S.; Zaffran, M.; Sutter, R.W.; Grassly, N.C. Type 2 Poliovirus Detection after Global Withdrawal of Trivalent Oral Vaccine. N. Engl. J. Med. 2018, 379, 834–845. [Google Scholar] [CrossRef] [PubMed]
- Jorba, J.; Diop, O.M.; Iber, J.; Henderson, E.; Zhao, K.; Quddus, A.; Sutter, R.; Vertefeuille, J.F.; Wenger, J.; Wassilak, S.G.F.; et al. Update on Vaccine-Derived Poliovirus Outbreaks-Worldwide, January 2018–June 2019. MMWR Morb. Mortal. Wkly. Rep. 2019, 68, 1024–1028. [Google Scholar] [CrossRef] [PubMed]
- Yeh, M.T.; Bujaki, E.; Dolan, P.T.; Smith, M.; Wahid, R.; Konz, J.; Weiner, A.J.; Bandyopadhyay, A.S.; Van Damme, P.; De Coster, I.; et al. Engineering the Live-Attenuated Polio Vaccine to Prevent Reversion to Virulence. Cell Host Microbe 2020, 27, 736–751.e738. [Google Scholar] [CrossRef] [PubMed]
- Yeh, M.T.; Smith, M.; Carlyle, S.; Konopka-Anstadt, J.L.; Burns, C.C.; Konz, J.; Andino, R.; Macadam, A. Genetic stabilization of attenuated oral vaccines against poliovirus types 1 and 3. Nature 2023, 619, 135–142. [Google Scholar] [CrossRef] [PubMed]
- Manukyan, H.; Lal, M.; Zhu, C.; Singh, O.; Lin, T.L.; Tritama, E.; Chumakov, K.; Lee, S.M.; Laassri, M. Application of MPBT Assay for Multiplex Determination of Infectious Titers and for Selection of the Optimal Formulation for the Trivalent Novel Oral Poliovirus Vaccine. Viruses 2024, 16, 961. [Google Scholar] [CrossRef]
- WHO. Polio Eradication Strategy 2022–2026: Delivering on a Promise. 2021. pp. 1–67. Available online: https://www.who.int/publications/i/item/9789240031937 (accessed on 9 June 2021).
- Kilpatrick, D.R.; Yang, C.F.; Ching, K.; Vincent, A.; Iber, J.; Campagnoli, R.; Mandelbaum, M.; De, L.; Yang, S.J.; Nix, A.; et al. Rapid group-, serotype-, and vaccine strain-specific identification of poliovirus isolates by real-time reverse transcription-PCR using degenerate primers and probes containing deoxyinosine residues. J. Clin. Microbiol. 2009, 47, 1939–1941. [Google Scholar] [CrossRef]
- Manukyan, H.; Tritama, E.; Wahid, R.; Anstadt, J.; Konz, J.; Chumakov, K.; Laassri, M. Improvement of the qmosRT-PCR Assay and Its Application for the Detection and Quantitation of the Three Serotypes of the Novel Oral Polio Vaccine in Stool Samples. Vaccines 2023, 11, 1729. [Google Scholar] [CrossRef]
- Manukyan, H.; Tritama, E.; Wahid, R.; Ansari, A.; Konz, J.; Chumakov, K.; Laassri, M. Development of a Quantitative One-Step RT-PCR Method for the Detection of Sabin 2 Virus Contamination in a Novel Oral Poliovirus Vaccine Type 2. Vaccines 2021, 9, 1729. [Google Scholar] [CrossRef]
- WHO. Manual of laboratory methods for testing of vaccines used in the WHO Expanded Programme on Immunization. In Vaccine Supply and Quality Unit; World Health Organization: Geneva, Switzerland, 1997. [Google Scholar]
- Manukyan, H.; Wahid, R.; Ansari, A.; Tritama, E.; Macadam, A.; Konz, J.; Chumakov, K.; Laassri, M. Quantitative RT-PCR Assays for Quantification of Undesirable Mutants in the Novel Type 2 Oral Poliovirus Vaccine. Vaccines 2022, 10, 1394. [Google Scholar] [CrossRef]
- GPEI Press Release on nOPV2 Prequalification. Available online: https://polioeradication.org/news/gpei-press-release-on-nopv2-prequalification/ (accessed on 9 January 2024).
- Cooper, L.V.; Bandyopadhyay, A.S.; Gumede, N.; Mach, O.; Mkanda, P.; Ndoutabe, M.; Okiror, S.O.; Ramirez-Gonzalez, A.; Touray, K.; Wanyoike, S.; et al. Risk factors for the spread of vaccine-derived type 2 polioviruses after global withdrawal of trivalent oral poliovirus vaccine and the effects of outbreak responses with monovalent vaccine: A retrospective analysis of surveillance data for 51 countries in Africa. Lancet Infect. Dis. 2022, 22, 284–294. [Google Scholar]
- WHO. Statement Following the Thirty-Seventh Meeting of the IHR Emergency Committee for Polio. Available online: https://www.who.int/news/item/22-12-2023-statement-following-the-thirty-seventh-meeting-of-the-ihr-emergency-committee-for-polio (accessed on 22 December 2023).
- GPEI: Novel Oral Polio Vaccine Type 2 (nOPV2) Granted EUL Recommendation. Available online: https://polioeradication.org/news/novel-oral-polio-vaccine-type-2-nopv2-granted-interim-emergency-use-listing-recommendation/ (accessed on 13 November 2020).
- WHO. Meeting of the Strategic Advisory Group of Experts on Immunization, September 2023: Conclusions and recommendations. Wkly. Epidemiol. Rec. 2023, 98, 599–620. [Google Scholar]
- Bandyopadhyay, A.S.; Cooper, L.V.; Zipursky, S. One billion doses and WHO prequalification of nOPV2: Implications for the global polio situation and beyond. PLOS Glob. Public Health 2024, 4, e0002920. [Google Scholar] [CrossRef] [PubMed]
- GPEI. GPEI Statement on cVDPV2 Detections in Burundi and Democratic Republic of the Congo. Available online: https://polioeradication.org/news/gpei-statement-on-cvdpv2-detections-in-burundi-and-democratic-republic-of-the-congo/ (accessed on 16 March 2023).
- Harasawa, R.; Tomiyama, T. Evidence of pestivirus RNA in human virus vaccines. J. Clin. Microbiol. 1994, 32, 1604–1605. [Google Scholar] [CrossRef] [PubMed]
- Hussain, A.I.; Johnson, J.A.; Da Silva Freire, M.; Heneine, W. Identification and characterization of avian retroviruses in chicken embryo-derived yellow fever vaccines: Investigation of transmission to vaccine recipients. J. Virol. 2003, 77, 1105–1111. [Google Scholar] [CrossRef]
- Robertson, J.S.; Minor, P. Reverse transcriptase activity in vaccines derived from chick cells. Biologicals 1996, 24, 289–290. [Google Scholar] [CrossRef]
- Shah, K.; Nathanson, N. Human exposure to SV40: Review and comment. Am. J. Epidemiol. 1976, 103, 1–12. [Google Scholar] [CrossRef]
- De, L.; Nottay, B.; Yang, C.F.; Holloway, B.P.; Pallansch, M.; Kew, O. Identification of vaccine-related polioviruses by hybridization with specific RNA probes. J. Clin. Microbiol. 1995, 33, 562–571. [Google Scholar] [CrossRef]
- van der Avoort, H.G.; Hull, B.P.; Hovi, T.; Pallansch, M.A.; Kew, O.M.; Crainic, R.; Wood, D.J.; Mulders, M.N.; van Loon, A.M. Comparative study of five methods for intratypic differentiation of polioviruses. J. Clin. Microbiol. 1995, 33, 2562–2566. [Google Scholar] [CrossRef]
- Cheng, Y.W.; Stefaniuk, C.; Jakubowski, M.A. Real-time PCR and targeted next-generation sequencing in the detection of low level EGFR mutations: Instructive case analyses. Respir. Med. Case Rep. 2019, 28, 100901. [Google Scholar] [CrossRef]
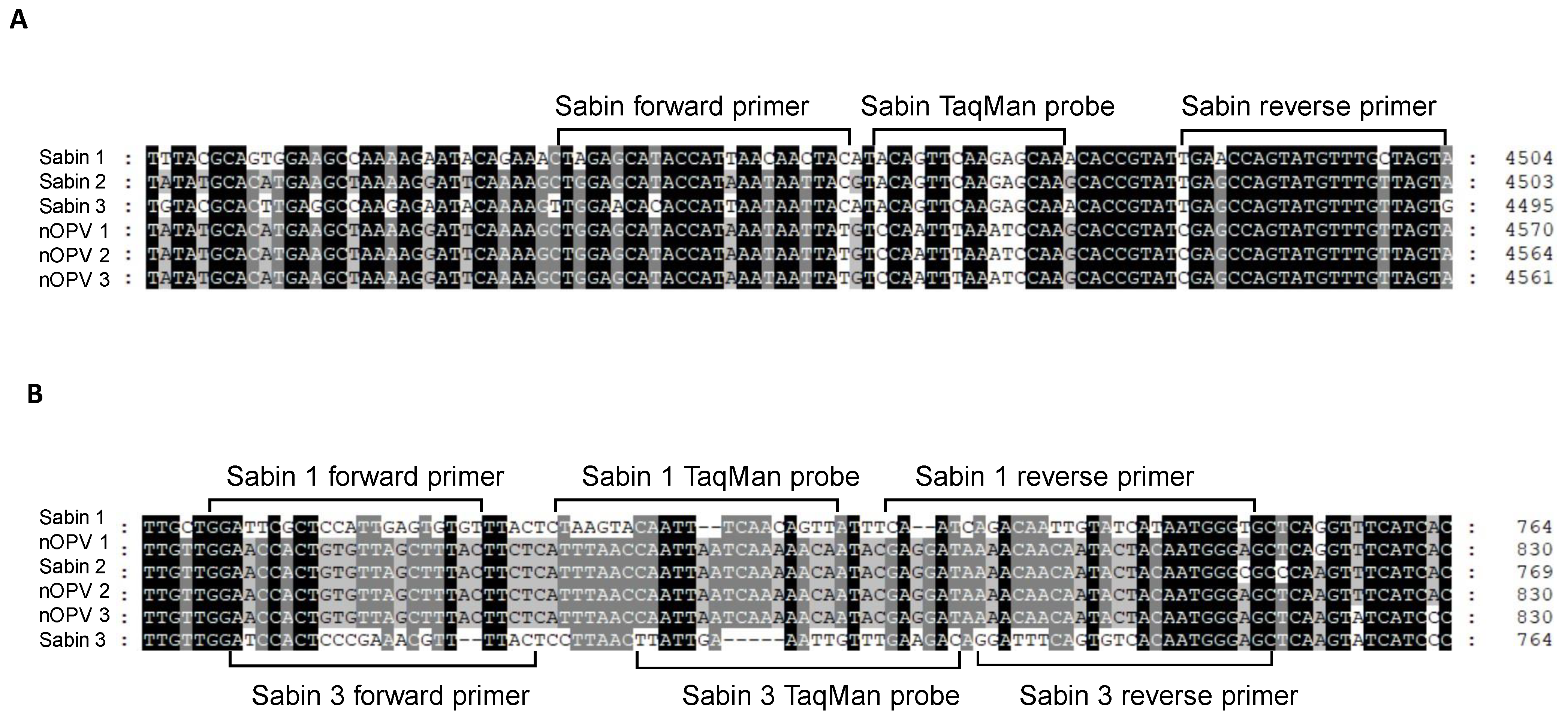
| Primer Name (Row Number) | Oligos Sequence 5′ --> 3′ | Location | Tm (Basic) | Size (nt) | Amplicon Size (bp) |
|---|---|---|---|---|---|
| Primers and TaqMan Probe for Universal Detection of Sabin Viruses in nOPV (panRT-PCR Assay) | |||||
| SabUprFv3 (3) | TRGARCAYACCATWAAYAAYTAC | 4434–4456 * | 45–54 | 23 | 70 |
| SabUprRv2 (4) | ACTARCAAACATACTGGYTCA | 4503–4483 * | 47–48 | 21 | |
| SabUprbFAM (5) | FAM-ACAGTTCAAGAGCAA-MGBNFQ | 4459–4473 * | 37 | 15 | |
| Primers and TaqMan Probe for Detection and Identification of Sabin 1 Virus in nOPV (mosRT-PCR Assay) | |||||
| Sab1-670F (7) | GGATTCGCTCCATTGAGTGTGT | 670–691 * | 55 | 22 | 79 |
| Sab1-812R (8) | ACCCATTATGATACAATTGTCTGATTG | 748–722 * | 54 | 27 | |
| Sab1PrbVIC (9) | VIC-TAAGTACAATTTCAACAGTT-AMGBNFQ | 698–718 * | 45 | 21 | |
| Primers and TaqMan Probe for Detection and Identification of Sabin 2 Virus in nOPV (mosRT-PCR Assay) | |||||
| Sab2-538F (11) | CGGAACAGGCGGTCGCGAA | 477–495 # | 58 | 19 | 68 |
| Sab2-605R (12) | GTAGTCGGTTCCGCCACA | 544–527 # | 57 | 18 | |
| Sab2PrbFAM (13) | FAM-TGACTGGCTTGTCGT- MGBNFQ | 500–514 # | 42 | 15 | |
| Primers and TaqMan Probe for Detection and Identification of Sabin 3 Virus in nOPV (mosRT-PCR Assay) | |||||
| Sab3-675F (15) | ATCCACTCCCGAAACGTTTTAC | 675–696 & | 55 | 23 | 75 |
| Sab3-749R (16) | CTCCCATTGTGACACTGAAATCC | 749–727 & | 55 | 23 | |
| Sab3PrbNED (17) | NED-TTATTGAAATTGTTTGAAGAC-MGBNFQ | 705–725 & | 43 | 21 | |
| % of Each of Sabin Strains Spiked in the Mixture of nOPV1, 2, & 3 | % of Sabin 1, 2, & 3 Strains Mixture Spiked in the Mixture of nOPV1, 2, & 3 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sabin 1 | Sabin 2 | Sabin 3 | Sabin 1 | Sabin 2 | Sabin 3 | Sabin 1, 2, & 3 | |||||||
| CCID50 | GC# | CCID50 | GC# | CCID50 | GC# | CCID50 | GC# | CCID50 | GC# | CCID50 | GC# | CCID50 | GC# |
| 28.41 | 31.93 | 4.50 | 12.37 | 42.63 | 29.73 | 9.48 | 11.63 | 1.13 | 3.50 | 17.75 | 10.49 | 28.35 | 25.62 |
| 3.82 | 4.48 | 0.47 | 1.39 | 6.92 | 4.06 | 1.27 | 1.51 | 0.15 | 0.45 | 2.38 | 1.36 | 3.81 | 3.33 |
| 0.40 | 0.47 | 0.05 | 0.14 | 0.74 | 0.42 | 0.13 | 0.16 | 0.02 | 0.05 | 0.25 | 0.14 | 0.39 | 0.34 |
| 0.04 | 0.05 | 5 × 10−3 | 0.01 | 0.07 | 0.04 | 0.01 | 0.02 | 2 × 10−3 | 5 × 10−3 | 0.02 | 0.01 | 0.04 | 0.03 |
| 4 × 10−3 | 5 × 10−3 | 5 × 10−4 | 1 × 10−3 | 7 × 10−3 | 4 × 10−3 | 1 × 10−3 | 2 × 10−3 | 2 × 10−4 | 5 × 10−4 | 2 × 10−4 | 1 × 10−3 | 4 × 10−3 | 3 × 10−3 |
| 4 × 10−4 | 5 × 10−4 | 5 × 10−5 | 1 × 10−4 | 7 × 10−4 | 4 × 10−4 | 1 × 10−4 | 2 × 10−4 | 2 × 10−5 | 5 × 10−5 | 2 × 10−5 | 1 × 10−4 | 4 × 10−4 | 3 × 10−4 |
| 4 × 10−5 | 5 × 10−5 | 5 × 10−6 | 1 × 10−5 | 7 × 10−5 | 4 × 10−5 | 1 × 10−5 | 2 × 10−5 | 2 × 10−6 | 5 × 10−6 | 2 × 10−6 | 1 × 10−5 | 4 × 10−5 | 3 × 10−5 |
| 4 × 10−6 | 5 × 10−6 | 5 × 10−7 | 1 × 10−6 | 7 × 10−6 | 4 × 10−6 | 1 × 10−6 | 2 × 10−6 | 2 × 10−7 | 5 × 10−7 | 2 × 10−7 | 1 × 10−6 | 4 × 10−6 | 3 × 10−6 |
| 4 × 10−7 | 5 × 10−7 | 5 × 10−8 | 1 × 10−7 | 7 × 10−7 | 4 × 10−7 | 1 × 10−7 | 2 × 10−7 | 2 × 10−8 | 5 × 10−8 | 2 × 10−8 | 1 × 10−7 | 4 × 10−7 | 3 × 10−7 |
| 4 × 10−8 | 5 × 10−8 | 5 × 10−9 | 1 × 10−8 | 7 × 10−8 | 4 × 10−8 | 1 × 10−8 | 2 × 10−8 | 2 × 10−9 | 5 × 10−9 | 2 × 10−9 | 1 × 10−8 | 4 × 10−8 | 3 × 10−8 |
| 4 × 10−9 | 5 × 10−9 | 5 × 10−10 | 1 × 10−9 | 7 × 10−9 | 4 × 10−9 | 1 × 10−9 | 2 × 10−9 | 2 × 10−10 | 5 × 10−10 | 2 × 10−10 | 1 × 10−9 | 4 × 10−9 | 3 × 10−9 |
| 4 × 10−10 | 5 × 10−10 | 5 × 10−11 | 1 × 10−10 | 7 × 10−10 | 4 × 10−10 | 1 × 10−10 | 2 × 10−10 | 2 × 10−11 | 5 × 10−11 | 2 × 10−11 | 1 × 10−10 | 4 × 10−10 | 3 × 10−10 |
| % (CCID50) | % (GC#) | Run 1 (Ct Repeats) | Run 2 (Ct Repeats) | Run 3 (Ct Repeats) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Ct1 | Ct2 | Ct3 | Ct1 | Ct2 | Ct3 | Ct1 | Ct2 | Ct3 | ||
| 4 × 10−3 | 3 × 10−3 | 29.72 | 29.05 | 29.68 | 30.15 | 30.34 | 30.48 | 30.44 | 30.14 | 30.16 |
| 4 × 10−4 | 3 × 10−4 | 36.84 | 34.94 | 36.02 | 36.92 | 37.30 | 36.64 | 35.60 | 35.23 | 35.30 |
| 4 × 10−5 | 3 × 10−5 | UD | 43.18 | 44.64 | UD | UD | UD | UD | UD | UD |
| 4 × 10−6 | 3 × 10−6 | UD | UD | UD | UD | UD | UD | UD | UD | UD |
| % (CCID50) | % (GC#) | Run 1 (Ct Repeats) | Run 2 (Ct Repeats) | Run 3 (Ct Repeats) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Ct1 | Ct2 | Ct3 | Ct1 | Ct2 | Ct3 | Ct1 | Ct2 | Ct3 | ||
| Sabin 1 Detection | ||||||||||
| 0.13 | 0.16 | 26.13 | 25.81 | 26.07 | 26.01 | 26.45 | 26.14 | 26.09 | 25.90 | 26.00 |
| 0.01 | 0.02 | 28.93 | 28.97 | 28.98 | 29.18 | 29.03 | 29.11 | 29.02 | 29.00 | 28.95 |
| 1 × 10−3 | 2 × 10−3 | 31.83 | 31.33 | 31.77 | 31.86 | 31.95 | 31.38 | 31.47 | 31.77 | 31.18 |
| 1 × 10−4 | 2 × 10−4 | 35.90 | 34.43 | 34.66 | 34.36 | 34.68 | 34.50 | 34.06 | 33.88 | 33.93 |
| 1 × 10−5 | 2 × 10−5 | 38.27 | 40.49 | 37.89 | 41.36 | UD | 41.38 | 41.57 | 41.29 | 37.15 |
| 1 × 10−6 | 2 × 10−6 | UD | UD | 39.09 | UD | UD | 43.11 | 43.06 | UD | UD |
| Sabin 2 Detection | ||||||||||
| 0.02 | 0.05 | 26.93 | 27.00 | 26.96 | 26.50 | 27.23 | 27.23 | 27.51 | 27.16 | 26.95 |
| 2 × 10−3 | 5 × 10−3 | 30.19 | 30.06 | 29.98 | 30.60 | 30.60 | 30.27 | 30.31 | 30.33 | 30.34 |
| 2 × 10−4 | 5 × 10−4 | 33.21 | 32.71 | 32.93 | 33.15 | 33.26 | 33.12 | 33.43 | 33.45 | 32.98 |
| 2 × 10−5 | 5 × 10−5 | 36.71 | 38.51 | 35.89 | 36.19 | UD | 36.41 | 35.69 | 37.14 | 36.01 |
| 2 × 10−6 | 5 × 10−6 | UD | 41.08 | UD | 41.01 | UD | UD | UD | UD | UD |
| 2 × 10−7 | 5 × 10−7 | UD | UD | UD | UD | UD | UD | UD | UD | 35.41 |
| Sabin 3 Detection | ||||||||||
| 0.25 | 0.14 | 25.68 | 25.61 | 25.38 | 25.62 | 25.89 | 25.70 | 25.92 | 25.90 | 25.56 |
| 0.02 | 0.01 | 28.68 | 28.62 | 28.25 | 28.88 | 28.95 | 28.62 | 28.55 | 28.84 | 28.37 |
| 2 × 10−3 | 1 × 10−3 | 31.09 | 31.19 | 30.95 | 31.27 | 31.77 | 31.32 | 31.10 | 31.26 | 30.89 |
| 2 × 10−4 | 1 × 10−4 | 34.00 | 34.59 | 34.35 | 34.62 | 34.60 | 33.62 | 33.85 | 33.44 | 33.52 |
| 2 × 10−5 | 1 × 10−5 | 36.35 | 36.77 | 37.71 | 37.77 | 37.16 | 36.16 | 36.46 | 36.73 | 36.14 |
| 2 × 10−6 | 1 × 10−6 | UD | UD | UD | UD | 37.93 | 38.66 | 38.92 | UD | 40.69 |
| tnOPV Lots (Formulation Lots) | Controls | ||||
|---|---|---|---|---|---|
| Sample Name | CT | Sample Name | CT | Sample Name | CT |
| BF-1 | UD | BF-8 | UD | Water | UD |
| BF-1 | UD | BF-8 | UD | Water | UD |
| BF-1 | UD | BF-8 | UD | Water | UD |
| BF-2 | UD | BF-9 | UD | nOPV1 | UD |
| BF-2 | UD | BF-9 | UD | nOPV1 | UD |
| BF-2 | UD | BF-9 | UD | nOPV1 | UD |
| BF-3 | UD | BF-10 | UD | nOPV2 | UD |
| BF-3 | UD | BF-10 | UD | nOPV2 | UD |
| BF-3 | UD | BF-10 | UD | nOPV2 | UD |
| BF-4 | UD | BF-11 | UD | nOPV3 | UD |
| BF-4 | UD | BF-11 | UD | nOPV3 | UD |
| BF-4 | UD | BF-11 | UD | nOPV3 | UD |
| BF-5 | UD | BF-12 | UD | Sabin1 | 16.24 |
| BF-5 | UD | BF-12 | UD | Sabin1 | 16.32 |
| BF-5 | UD | BF-12 | UD | Sabin1 | 16.48 |
| BF-6 | UD | Sabin2 | 16.56 | ||
| BF-6 | UD | Sabin2 | 16.61 | ||
| BF-6 | UD | Sabin2 | 16.72 | ||
| BF-7 | UD | Sabin3 | 15.29 | ||
| BF-7 | UD | Sabin3 | 15.11 | ||
| BF-7 | UD | Sabin3 | 15.46 | ||
| tnOPV Formulation Samples | Control Samples | ||||||
|---|---|---|---|---|---|---|---|
| tnOPV lot | Sabin1 (CT) | Sabin2 (CT) | Sabin3 (CT) | Sample Name | Sabin1 (CT) | Sabin2 (CT) | Sabin3 (CT) |
| BF-1 | UD | UD | UD | Water | UD | UD | UD |
| BF-1 | UD | UD | UD | Water | UD | UD | UD |
| BF-1 | UD | UD | UD | Water | UD | UD | UD |
| BF-2 | UD | UD | UD | nOPV1 | UD | UD | UD |
| BF-2 | UD | UD | UD | nOPV1 | UD | UD | UD |
| BF-2 | UD | UD | UD | nOPV1 | UD | UD | UD |
| BF-3 | UD | UD | UD | nOPV2 | UD | UD | UD |
| BF-3 | UD | UD | UD | nOPV2 | UD | UD | UD |
| BF-3 | UD | UD | UD | nOPV2 | UD | UD | UD |
| BF-4 | UD | UD | UD | nOPV3 | UD | UD | UD |
| BF-4 | UD | UD | UD | nOPV3 | UD | UD | UD |
| BF-4 | UD | UD | UD | nOPV3 | UD | UD | UD |
| BF-5 | UD | UD | UD | Sabin1 | 27.42 | UD | UD |
| BF-5 | UD | UD | UD | Sabin1 | 27.80 | UD | UD |
| BF-5 | UD | UD | UD | Sabin1 | 27.47 | UD | UD |
| BF-6 | UD | UD | UD | Sabin2 | UD | 27.64 | UD |
| BF-6 | UD | UD | UD | Sabin2 | UD | 28.16 | UD |
| BF-6 | UD | UD | UD | Sabin2 | UD | 27.84 | UD |
| BF-7 | UD | UD | UD | Sabin3 | UD | UD | 27.42 |
| BF-7 | UD | UD | UD | Sabin3 | UD | UD | 27.70 |
| BF-7 | UD | UD | UD | Sabin3 | UD | UD | 27.82 |
| BF-8 | UD | UD | UD | ||||
| BF-8 | UD | UD | UD | ||||
| BF-8 | UD | UD | UD | ||||
| BF-9 | UD | UD | UD | ||||
| BF-9 | UD | UD | UD | ||||
| BF-9 | UD | UD | UD | ||||
| BF-10 | UD | UD | UD | ||||
| BF-10 | UD | UD | UD | ||||
| BF-10 | UD | UD | UD | ||||
| BF-11 | UD | UD | UD | ||||
| BF-11 | UD | UD | UD | ||||
| BF-11 | UD | UD | UD | ||||
| BF-12 | UD | UD | UD | ||||
| BF-12 | UD | UD | UD | ||||
| BF-12 | UD | UD | UD | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Singh, O.; Manukyan, H.; Tritama, E.; Lee, S.-M.; Weir, J.P.; Laassri, M. Development of RT-PCR Assays for Simple Detection and Identification of Sabin Virus Contaminants in the Novel Oral Poliovirus Vaccines. Vaccines 2025, 13, 75. https://doi.org/10.3390/vaccines13010075
Singh O, Manukyan H, Tritama E, Lee S-M, Weir JP, Laassri M. Development of RT-PCR Assays for Simple Detection and Identification of Sabin Virus Contaminants in the Novel Oral Poliovirus Vaccines. Vaccines. 2025; 13(1):75. https://doi.org/10.3390/vaccines13010075
Chicago/Turabian StyleSingh, Olga, Hasmik Manukyan, Erman Tritama, Shwu-Maan Lee, Jerry P. Weir, and Majid Laassri. 2025. "Development of RT-PCR Assays for Simple Detection and Identification of Sabin Virus Contaminants in the Novel Oral Poliovirus Vaccines" Vaccines 13, no. 1: 75. https://doi.org/10.3390/vaccines13010075
APA StyleSingh, O., Manukyan, H., Tritama, E., Lee, S.-M., Weir, J. P., & Laassri, M. (2025). Development of RT-PCR Assays for Simple Detection and Identification of Sabin Virus Contaminants in the Novel Oral Poliovirus Vaccines. Vaccines, 13(1), 75. https://doi.org/10.3390/vaccines13010075





