Immunogenicity of Intradermal Versus Intramuscular BNT162b2 COVID-19 Booster Vaccine in Patients with Immune-Mediated Dermatologic Diseases: A Non-Inferiority Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
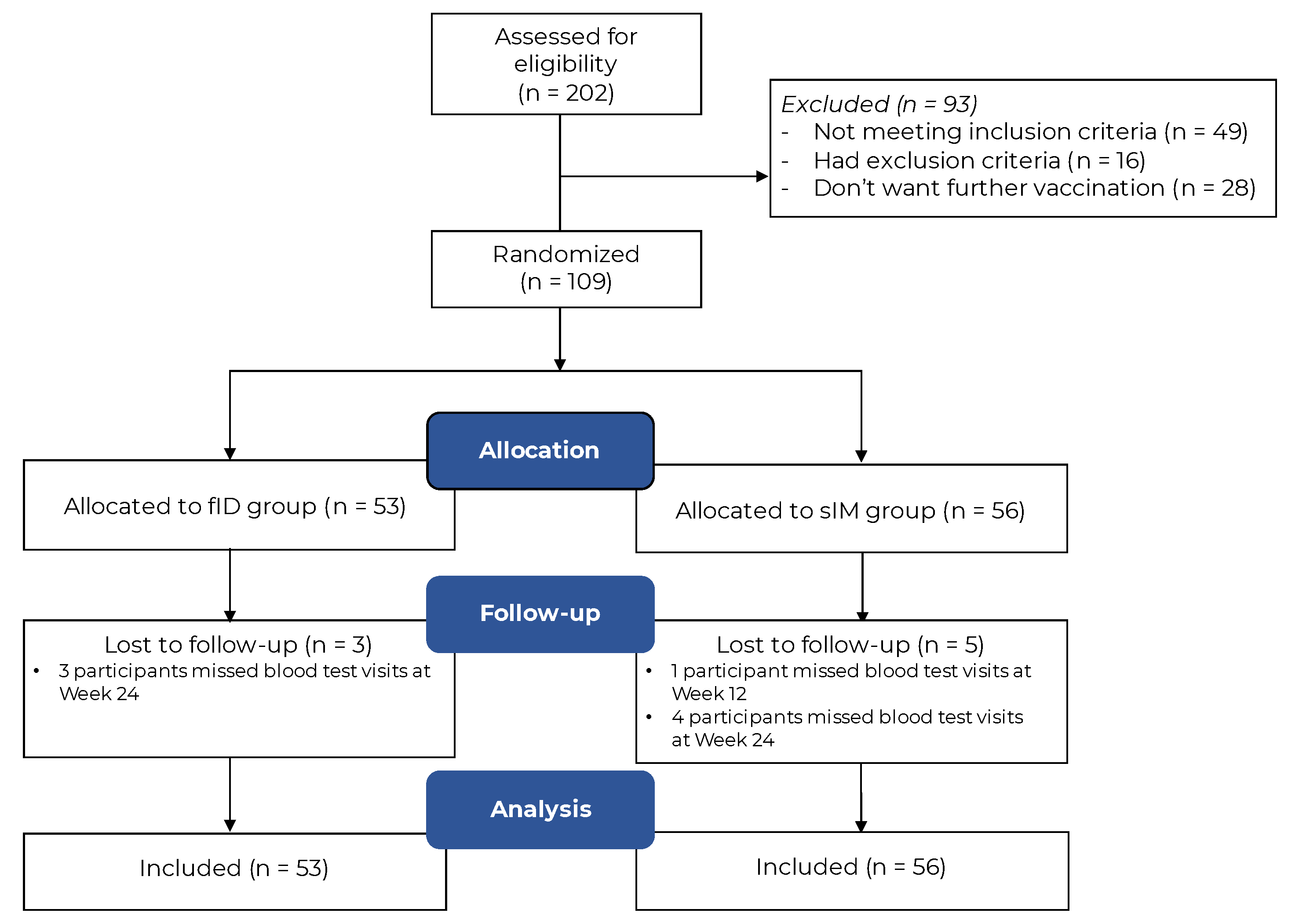
2.1. Study Design and Participants
2.2. Interventions
2.3. Randomization, Allocation, Concealment, and Blinding
2.4. Study Outcomes
2.5. Assay Sensitivity Evaluation
2.6. Statistical Analysis
2.7. Sample Size Calculation
3. Results
3.1. Study Participants
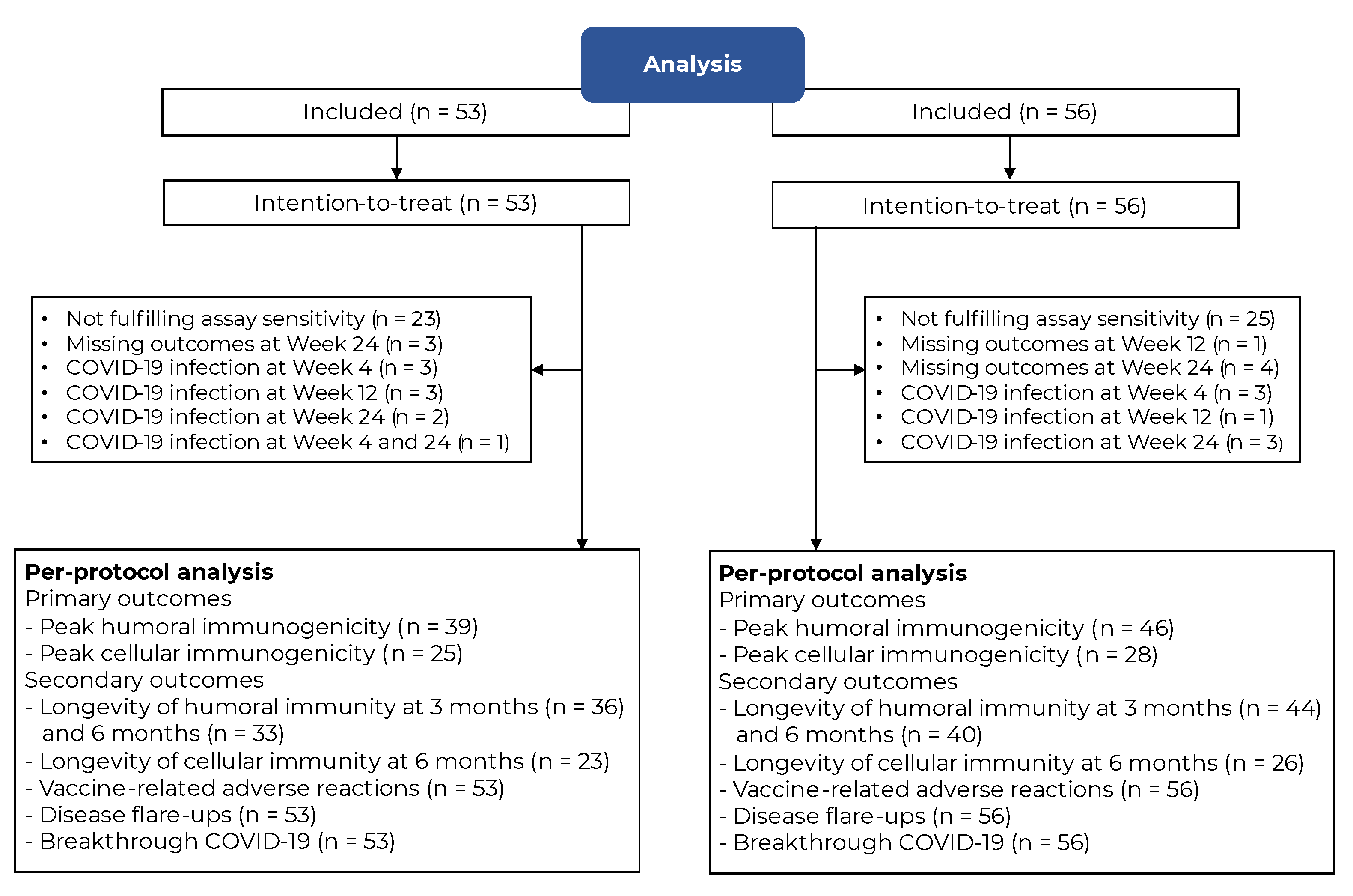
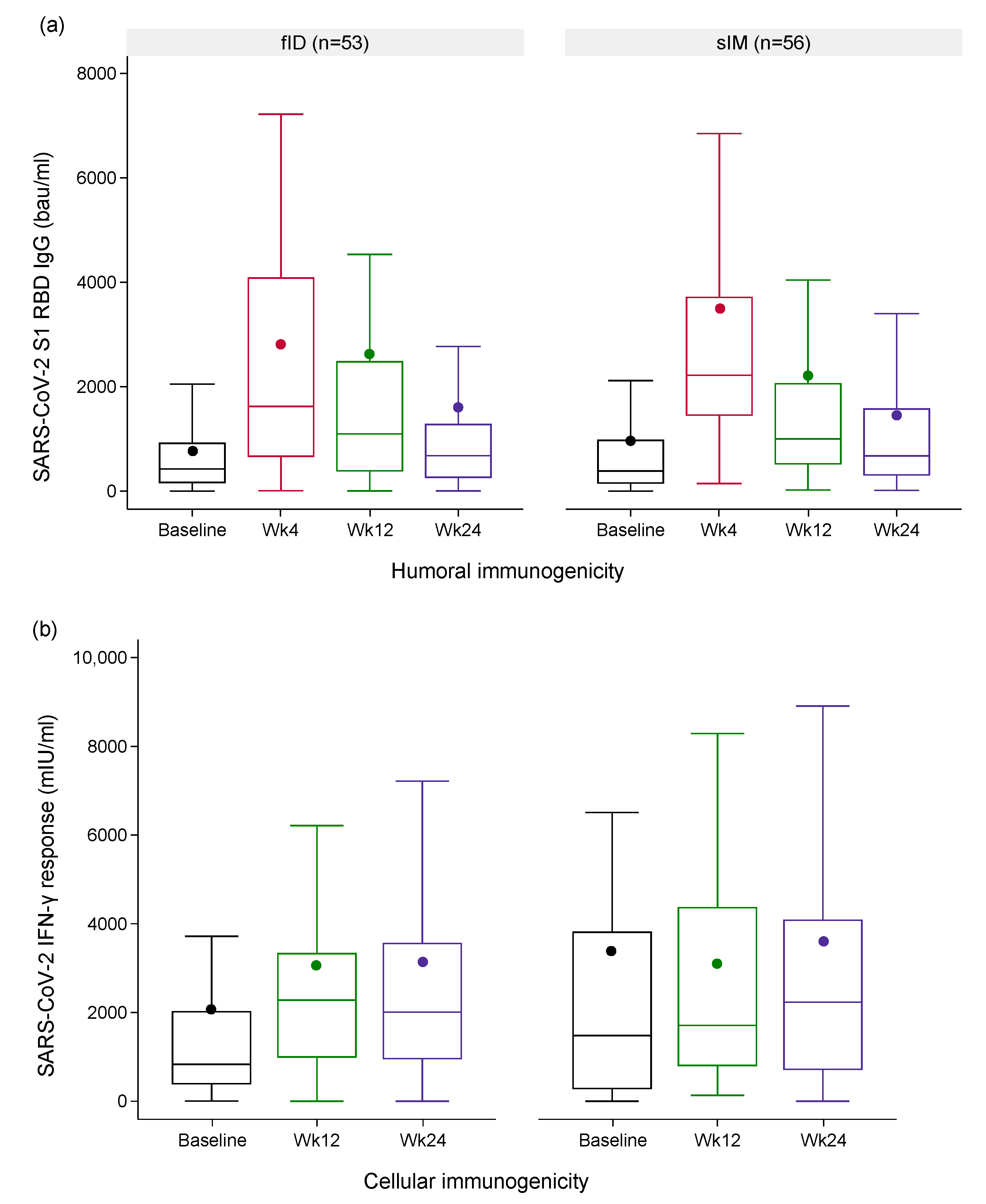
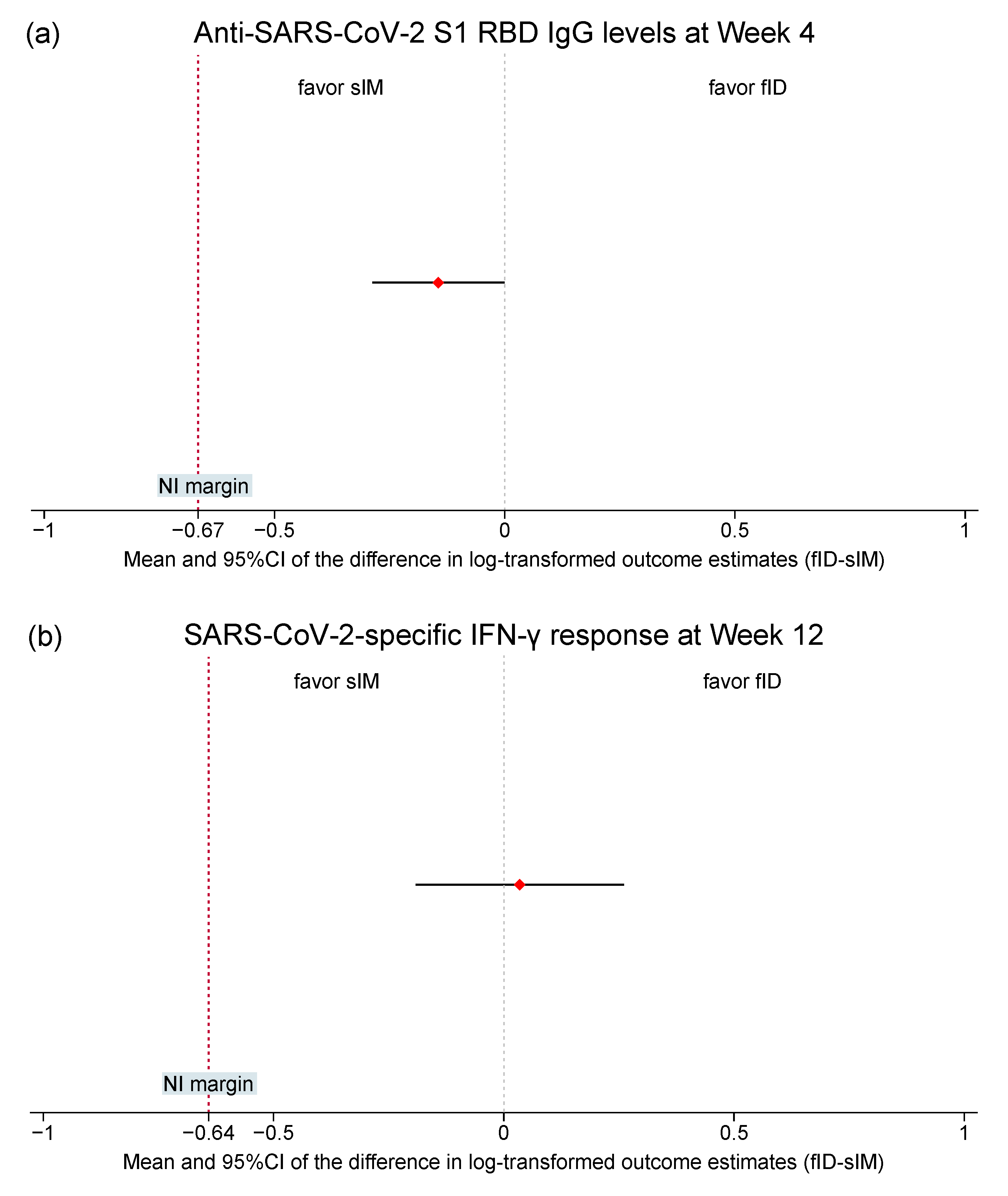
3.2. Immunogenicity Outcomes
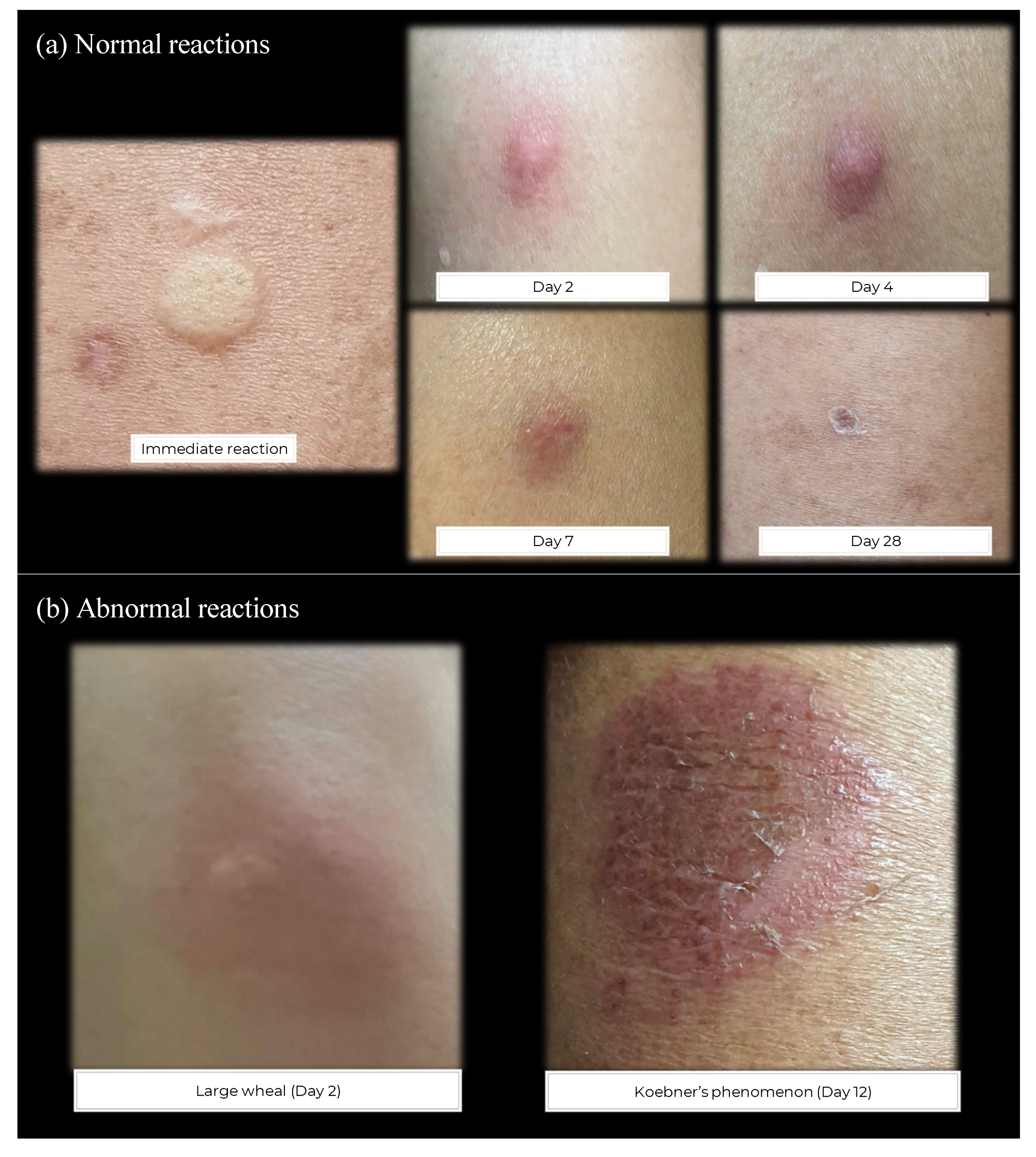
3.3. Vaccine-Related Adverse Reactions and Breakthrough COVID-19
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Townsend, J.P.; Hassler, H.B.; Dornburg, A. Infection by SARS-CoV-2 with alternate frequencies of mRNA vaccine boosting. J. Med. Virol. 2023, 95, e28461. [Google Scholar] [CrossRef] [PubMed]
- Mungmunpuntipantip, R.; Wiwanitkit, V. Cost-utility-safety analysis of alternative intradermal versus classical intramuscular COVID-19 vaccination. Int. J. Physiol. Pathophysiol. Pharmacol. 2022, 14, 129–133. [Google Scholar] [PubMed]
- Nantanee, R.; Aikphaibul, P.; Jaru-Ampornpan, P.; Sodsai, P.; Himananto, O.; Theerawit, T.; Sophonphan, J.; Tovichayathamrong, P.; Manothummetha, K.; Laohasereekul, T.; et al. Immunogenicity and reactogenicity after booster dose with AZD1222 via intradermal route among adult who had received CoronaVac. Vaccine 2022, 40, 3320–3329. [Google Scholar] [CrossRef] [PubMed]
- Intapiboon, P.; Seepathomnarong, P.; Ongarj, J.; Surasombatpattana, S.; Uppanisakorn, S.; Mahasirimongkol, S.; Sawaengdee, W.; Phumiamorn, S.; Sapsutthipas, S.; Sangsupawanich, P.; et al. Immunogenicity and Safety of an Intradermal BNT162b2 mRNA Vaccine Booster after Two Doses of Inactivated SARS-CoV-2 Vaccine in Healthy Population. Vaccines 2021, 9, 1375. [Google Scholar] [CrossRef] [PubMed]
- Pinpathomrat, N.; Intapiboon, P.; Seepathomnarong, P.; Ongarj, J.; Sophonmanee, R.; Hengprakop, J.; Surasombatpattana, S.; Uppanisakorn, S.; Mahasirimongkol, S.; Sawaengdee, W.; et al. Immunogenicity and safety of an intradermal ChAdOx1 nCoV-19 boost in a healthy population. NPJ Vaccines 2022, 7, 52. [Google Scholar] [CrossRef] [PubMed]
- Tawinprai, K.; Siripongboonsitti, T.; Porntharukchareon, T.; Wittayasak, K.; Thonwirak, N.; Soonklang, K.; Sornsamdang, G.; Auewarakul, C.; Mahanonda, N. Immunogenicity and safety of an intradermal fractional third dose of ChAdOx1 nCoV-19/AZD1222 vaccine compared with those of a standard intramuscular third dose in volunteers who previously received two doses of CoronaVac: A randomized controlled trial. Vaccine 2022, 40, 1761–1767. [Google Scholar] [CrossRef] [PubMed]
- Temtanakitpaisan, Y.; Saengnipanthkul, S.; Sarakosol, N.; Maskasame, S.; Mongkon, S.; Buranrat, B.; Thammawat, S.; Patamatamkul, S.; Nernsai, P. Reactogenicity and immunogenicity of the intradermal administration of BNT162b2 mRNA vaccine in healthy adults who were primed with an inactivated SARS-CoV-2 vaccine. Vaccine X 2022, 12, 100242. [Google Scholar] [CrossRef] [PubMed]
- Chatsiricharoenkul, S.; Niyomnaitham, S.; Posen, H.J.; Toh, Z.Q.; Licciardi, P.V.; Wongprompitak, P.; Duangchinda, T.; Pakchotanon, P.; Chantima, W.; Chokephaibulkit, K. Safety and immunogenicity of intradermal administration of fractional dose CoronaVac((R)), ChAdOx1 nCoV-19 and BNT162b2 as primary series vaccination. Front. Immunol. 2022, 13, 1010835. [Google Scholar] [CrossRef]
- Roozen, G.V.T.; Prins, M.L.M.; van Binnendijk, R.; den Hartog, G.; Kuiper, V.P.; Prins, C.; Janse, J.J.; Kruithof, A.C.; Feltkamp, M.C.W.; Kuijer, M.; et al. Safety and Immunogenicity of Intradermal Fractional Dose Administration of the mRNA-1273 Vaccine: A Proof-of-Concept Study. Ann. Intern. Med. 2022, 175, 1771–1774. [Google Scholar] [CrossRef]
- Gaur, P.; Agrawat, H.; Shukla, A. COVID-19 vaccine hesitancy in patients with systemic autoimmune rheumatic disease: An interview-based survey. Rheumatol. Int. 2021, 41, 1601–1605. [Google Scholar] [CrossRef]
- Chanprapaph, K.; Seree-aphinan, C.; Rattanakaemakorn, P.; Pomsoong, C.; Ratanapokasatit, Y.; Setthaudom, C.; Thitithanyanont, A.; Suriyo, A.; Suangtamai, T.; Suchonwanit, P.; et al. A real-world prospective cohort study of immunogenicity and reactogenicity of ChAdOx1-S[recombinant] among patients with immune-mediated dermatological diseases. Br. J. Dermatol. 2022, 188, 268–277. [Google Scholar] [CrossRef] [PubMed]
- Seree-Aphinan, C.; Chanprapaph, K.; Rattanakaemakorn, P.; Setthaudom, C.; Suangtamai, T.; Pomsoong, C.; Ratanapokasatit, Y.; Suchonwanit, P. Inactivated COVID-19 Vaccine Induces a Low Humoral Immune Response in a Subset of Dermatological Patients Receiving Immunosuppressants. Front. Med. 2021, 8, 769845. [Google Scholar] [CrossRef]
- Seree-aphinan, C.; Suchonwanit, P.; Rattanakaemakorn, P.; Pomsoong, C.; Ratanapokasatit, Y.; Setthaudom, C.; Suangtamai, T.; Chanprapaph, K.; COVIDVAC-DERM Study Group. Risk–benefit profiles associated with receiving Moderna COVID-19 (mRNA-1273) vaccine as an additional pre-booster dose in immune-mediated dermatologic disease patients with low SARS-CoV-2-specific immunity following the primary series: A prospective cohort study. J. Eur. Acad. Dermatol. Venereol. 2023, 37, e572–e575. [Google Scholar] [CrossRef]
- Seree-Aphinan, C.; Ratanapokasatit, Y.; Suchonwanit, P.; Rattanakaemakorn, P.; O-Charoen, P.; Pisitkun, P.; Suangtamai, T.; Setthaudom, C.; Chirasuthat, S.; Chanprapaph, K. Optimal time for COVID-19 vaccination in rituximab-treated dermatologic patients. Front. Immunol. 2023, 14, 1138765. [Google Scholar] [CrossRef] [PubMed]
- Falotico, J.M.; Desai, A.D.; Shah, A.; Ricardo, J.W.; Lipner, S.R. Curbing COVID-19 Vaccine Hesitancy from a Dermatological Standpoint: Analysis of Cutaneous Reactions in the Vaccine Adverse Event Reporting System (VAERS) Database. Am. J. Clin. Dermatol. 2022, 23, 729–737. [Google Scholar] [CrossRef] [PubMed]
- Valencia López, M.J.; Meineke, A.; Stephan, B.; Rustenbach, S.J.; Kis, A.; Thaçi, D.; Mrowietz, U.; Reich, K.; Staubach-Renz, P.; von Kiedrowski, R.; et al. SARS-CoV-2 vaccination status and adverse events among patients with psoriasis-Data from the German Registries PsoBest and CoronaBest. J. Eur. Acad. Dermatol. Venereol. 2023, 37, e831–e833. [Google Scholar] [CrossRef]
- Adams, L.; Nakafero, G.; Grainge, M.J.; Card, T.; Mallen, C.D.; Van-Tam, J.S.N.; Williams, H.C.; Abhishek, A. Is vaccination against COVID-19 associated with psoriasis or eczema flare? Self-controlled case series analysis using data from the Clinical Practice Research Datalink (Aurum). Br. J. Dermatol. 2023, 188, 297–299. [Google Scholar] [CrossRef]
- Abhishek, A.; Boyton, R.J.; Peckham, N.; McKnight, A.; Coates, L.C.; Bluett, J.; Barber, V.; Cureton, L.; Francis, A.; Appelbe, D.; et al. Effect of a 2-week interruption in methotrexate treatment versus continued treatment on COVID-19 booster vaccine immunity in adults with inflammatory conditions (VROOM study): A randomised, open label, superiority trial. Lancet Respir. Med. 2022, 10, 840–850. [Google Scholar] [CrossRef]
- Weschawalit, S.; Pongcharoen, P.; Suthiwartnarueput, W.; Srivilaithon, W.; Daorattanachai, K.; Jongrak, P.; Chakkavittumrong, P. Cutaneous Adverse Events After COVID-19 Vaccination. Clin. Cosmet. Investig. Dermatol. 2023, 16, 1473–1484. [Google Scholar] [CrossRef]
- Wiecek, W.; Ahuja, A.; Chaudhuri, E.; Kremer, M.; Simoes Gomes, A.; Snyder, C.M.; Tabarrok, A.; Tan, B.J. Testing fractional doses of COVID-19 vaccines. Proc. Natl. Acad. Sci. USA 2022, 119, e2116932119. [Google Scholar] [CrossRef]
- Huzly, D.; Panning, M.; Smely, F.; Enders, M.; Komp, J.; Falcone, V.; Steinmann, D. Accuracy and real life performance of a novel interferon-γ release assay for the detection of SARS-CoV2 specific T cell response. J. Clin. Virol. 2022, 148, 105098. [Google Scholar] [CrossRef] [PubMed]
- Saad Albichr, I.; Mzougui, S.; Devresse, A.; Georgery, H.; Goffin, E.; Kanaan, N.; Yombi, J.C.; Belkhir, L.; De Greef, J.; Scohy, A.; et al. Evaluation of a commercial interferon-γ release assay for the detection of SARS-CoV-2 T-cell response after vaccination. Heliyon 2023, 9, e17186. [Google Scholar] [CrossRef] [PubMed]
- Boongird, S.; Setthaudom, C.; Kitpermkiat, R.; Prasongtanakij, S.; Srisala, S.; Chuengsaman, P.; Nongnuch, A.; Assanatham, M.; Kiertiburanakul, S.; Malathum, K.; et al. Durability of Humoral and Cellular Immunity after an Extended Primary Series with Heterologous Inactivated SARS-CoV-2 Prime-Boost and ChAdOx1 nCoV-19 in Dialysis Patients (ICON3). Vaccines 2022, 10, 1064. [Google Scholar] [CrossRef] [PubMed]
- Gilboa, M.; Regev-Yochay, G.; Mandelboim, M.; Indenbaum, V.; Asraf, K.; Fluss, R.; Amit, S.; Mendelson, E.; Doolman, R.; Afek, A.; et al. Durability of Immune Response After COVID-19 Booster Vaccination and Association With COVID-19 Omicron Infection. JAMA Netw. Open 2022, 5, e2231778. [Google Scholar] [CrossRef]
- Regev-Yochay, G.; Gonen, T.; Gilboa, M.; Mandelboim, M.; Indenbaum, V.; Amit, S.; Meltzer, L.; Asraf, K.; Cohen, C.; Fluss, R.; et al. Efficacy of a Fourth Dose of Covid-19 mRNA Vaccine against Omicron. N. Engl. J. Med. 2022, 386, 1377–1380. [Google Scholar] [CrossRef] [PubMed]
- Alu, A.; Chen, L.; Lei, H.; Wei, Y.; Tian, X.; Wei, X. Intranasal COVID-19 vaccines: From bench to bed. EBioMedicine 2022, 76, 103841. [Google Scholar] [CrossRef] [PubMed]
- Horvath, D.; Temperton, N.; Mayora-Neto, M.; Da Costa, K.; Cantoni, D.; Horlacher, R.; Gunther, A.; Brosig, A.; Morath, J.; Jakobs, B.; et al. Novel intranasal vaccine targeting SARS-CoV-2 receptor binding domain to mucosal microfold cells and adjuvanted with TLR3 agonist Riboxxim elicits strong antibody and T-cell responses in mice. Sci. Rep. 2023, 13, 4648. [Google Scholar] [CrossRef]
- Zhu, F.; Huang, S.; Liu, X.; Chen, Q.; Zhuang, C.; Zhao, H.; Han, J.; Jaen, A.M.; Do, T.H.; Peter, J.G.; et al. Safety and efficacy of the intranasal spray SARS-CoV-2 vaccine dNS1-RBD: A multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Respir. Med. 2023, 11, 1075–1088. [Google Scholar] [CrossRef] [PubMed]
- Niyomnaitham, S.; Chatsiricharoenkul, S.; Toh, Z.Q.; Senawong, S.; Pheerapanyawaranun, C.; Phumiamorn, S.; Licciardi, P.V.; Chokephaibulkit, K. Evaluation of the Safety and Immunogenicity of Fractional Intradermal COVID-19 Vaccines as a Booster: A Pilot Study. Vaccines 2022, 10, 1497. [Google Scholar] [CrossRef]
- Zhang, L.; Wang, W.; Wang, S. Effect of vaccine administration modality on immunogenicity and efficacy. Expert. Rev. Vaccines 2015, 14, 1509–1523. [Google Scholar] [CrossRef]
- Xie, C.; Yao, R.; Xia, X. The advances of adjuvants in mRNA vaccines. NPJ Vaccines 2023, 8, 162. [Google Scholar] [CrossRef]
- Gyldenløve, M.; Skov, L.; Hansen, C.B.; Garred, P. Recurrent injection-site reactions after incorrect subcutaneous administration of a COVID-19 vaccine. J. Eur. Acad. Dermatol. Venereol. 2021, 35, e545–e546. [Google Scholar] [CrossRef] [PubMed]
- Ng, J.Y. Inadvertent subcutaneous injection of COVID-19 vaccine. Postgrad. Med. J. 2021, 97, 400. [Google Scholar] [CrossRef] [PubMed]
- Cook, I.F. Subcutaneous vaccine administration—An outmoded practice. Hum. Vaccines Immunother. 2021, 17, 1329–1341. [Google Scholar] [CrossRef] [PubMed]
- Wilck, M.B.; Seaman, M.S.; Baden, L.R.; Walsh, S.R.; Grandpre, L.E.; Devoy, C.; Giri, A.; Kleinjan, J.A.; Noble, L.C.; Stevenson, K.E.; et al. Safety and immunogenicity of modified vaccinia Ankara (ACAM3000): Effect of dose and route of administration. J. Infect. Dis. 2010, 201, 1361–1370. [Google Scholar] [CrossRef] [PubMed]
- Schnyder, J.L.; De Pijper, C.A.; Garcia Garrido, H.M.; Daams, J.G.; Goorhuis, A.; Stijnis, C.; Schaumburg, F.; Grobusch, M.P. Fractional dose of intradermal compared to intramuscular and subcutaneous vaccination—A systematic review and meta-analysis. Travel Med. Infect. Dis. 2020, 37, 101868. [Google Scholar] [CrossRef]
- Pileggi, C.; Lotito, F.; Bianco, A.; Nobile, C.G.; Pavia, M. Immunogenicity and safety of intradermal influenza vaccine in immunocompromized patients: A meta-analysis of randomized controlled trials. BMC Infect. Dis. 2015, 15, 427. [Google Scholar] [CrossRef] [PubMed]
- Troy, S.B.; Kouiavskaia, D.; Siik, J.; Kochba, E.; Beydoun, H.; Mirochnitchenko, O.; Levin, Y.; Khardori, N.; Chumakov, K.; Maldonado, Y. Comparison of the Immunogenicity of Various Booster Doses of Inactivated Polio Vaccine Delivered Intradermally Versus Intramuscularly to HIV-Infected Adults. J. Infect. Dis. 2015, 211, 1969–1976. [Google Scholar] [CrossRef]
- Assantachai, P.; Niyomnaitham, S.; Chatthanawaree, W.; Intalapaporn, S.; Muangpaisan, W.; Phannarus, H.; Saichompoo, R.B.; Sura-Amonrattana, U.; Wongprompitak, P.; Toh, Z.Q.; et al. Immunogenicity and reactogenicity of mRNA COVID-19 vaccine booster administered by intradermal or intramuscular route in Thai Older adults. J. Infect. Dis. 2023, 228, 868–877. [Google Scholar] [CrossRef]
- Sophonmanee, R.; Ongarj, J.; Seeyankem, B.; Seepathomnarong, P.; Intapiboon, P.; Surasombatpattana, S.; Uppanisakorn, S.; Sangsupawanich, P.; Chusri, S.; Pinpathomrat, N. T-Cell Responses Induced by an Intradermal BNT162b2 mRNA Vaccine Booster Following Primary Vaccination with Inactivated SARS-CoV-2 Vaccine. Vaccines 2022, 10, 1494. [Google Scholar] [CrossRef]
- Rha, M.-S.; Shin, E.-C. Activation or exhaustion of CD8+ T cells in patients with COVID-19. Cell. Mol. Immunol. 2021, 18, 2325–2333. [Google Scholar] [CrossRef] [PubMed]
- Diao, B.; Wang, C.; Tan, Y.; Chen, X.; Liu, Y.; Ning, L.; Chen, L.; Li, M.; Liu, Y.; Wang, G.; et al. Reduction and Functional Exhaustion of T Cells in Patients With Coronavirus Disease 2019 (COVID-19). Front. Immunol 2020, 11, 827. [Google Scholar] [CrossRef]
- Azim Majumder, M.A.; Razzaque, M.S. Repeated vaccination and ‘vaccine exhaustion’: Relevance to the COVID-19 crisis. Expert. Rev. Vaccines 2022, 21, 1011–1014. [Google Scholar] [CrossRef]
- Gao, Z.; Feng, Y.; Xu, J.; Liang, J. T-cell exhaustion in immune-mediated inflammatory diseases: New implications for immunotherapy. Front. Immunol. 2022, 13, 977394. [Google Scholar] [CrossRef]
- Benitez Fuentes, J.D.; Mohamed Mohamed, K.; de Luna Aguilar, A.; Jimenez Garcia, C.; Guevara-Hoyer, K.; Fernandez-Arquero, M.; Rodriguez de la Pena, M.A.; Garciia Bravo, L.; Jimenez Ortega, A.F.; Flores Navarro, P.; et al. Evidence of exhausted lymphocytes after the third anti-SARS-CoV-2 vaccine dose in cancer patients. Front. Oncol. 2022, 12, 975980. [Google Scholar] [CrossRef] [PubMed]
- Martora, F.; Battista, T.; Ruggiero, A.; Scalvenzi, M.; Villani, A.; Megna, M.; Potestio, L. The Impact of COVID-19 Vaccination on Inflammatory Skin Disorders and Other Cutaneous Diseases: A Review of the Published Literature. Viruses 2023, 15, 1423. [Google Scholar] [CrossRef] [PubMed]
- Wu, P.C.; Huang, I.H.; Wang, C.W.; Tsai, C.C.; Chung, W.H.; Chen, C.B. New Onset and Exacerbations of Psoriasis Following COVID-19 Vaccines: A Systematic Review. Am. J. Clin. Dermatol. 2022, 23, 775–799. [Google Scholar] [CrossRef]
- Ju, H.J.; Lee, J.Y.; Han, J.H.; Lee, J.H.; Bae, J.M.; Lee, S. Risk of autoimmune skin and connective tissue disorders after mRNA-based COVID-19 vaccination. J. Am. Acad. Dermatol. 2023, 89, 685–693. [Google Scholar] [CrossRef]
- Harries, M.; Macbeth, A.E.; Holmes, S.; Chiu, W.S.; Gallardo, W.R.; Nijher, M.; de Lusignan, S.; Tziotzios, C.; Messenger, A.G. The epidemiology of alopecia areata: A population-based cohort study in UK primary care. Br. J. Dermatol. 2022, 186, 257–265. [Google Scholar] [CrossRef]
- Cheong, W.L.; Mohan, D.; Warren, N.; Reidpath, D.D. Multiple Sclerosis in the Asia Pacific Region: A Systematic Review of a Neglected Neurological Disease. Front. Neurol. 2018, 9, 432. [Google Scholar] [CrossRef]
- Hittle, M.; Culpepper, W.J.; Langer-Gould, A.; Marrie, R.A.; Cutter, G.R.; Kaye, W.E.; Wagner, L.; Topol, B.; LaRocca, N.G.; Nelson, L.M.; et al. Population-Based Estimates for the Prevalence of Multiple Sclerosis in the United States by Race, Ethnicity, Age, Sex, and Geographic Region. JAMA Neurol. 2023, 80, 693–701. [Google Scholar] [CrossRef] [PubMed]
- Tian, D.C.; Zhang, C.; Yuan, M.; Yang, X.; Gu, H.; Li, Z.; Wang, Y.; Shi, F.D. Incidence of multiple sclerosis in China: A nationwide hospital-based study. Lancet Reg. Health West. Pac. 2020, 1, 100010. [Google Scholar] [CrossRef] [PubMed]
- Hertel, M.; Heiland, M.; Nahles, S.; von Laffert, M.; Mura, C.; Bourne, P.E.; Preissner, R.; Preissner, S. Real-world evidence from over one million COVID-19 vaccinations is consistent with reactivation of the varicella-zoster virus. J. Eur. Acad. Dermatol. Venereol. 2022, 36, 1342–1348. [Google Scholar] [CrossRef] [PubMed]
- Ziegler, L.; Klemis, V.; Schmidt, T.; Schneitler, S.; Baum, C.; Neumann, J.; Becker, S.L.; Gärtner, B.C.; Sester, U.; Sester, M. Differences in SARS-CoV-2 specific humoral and cellular immune responses after contralateral and ipsilateral COVID-19 vaccination. EBioMedicine 2023, 95, 104743. [Google Scholar] [CrossRef]
| Investigational Arms | p | ||
|---|---|---|---|
| fID (n = 53) | sIM (n = 56) | ||
| Age group, n (%) | 0.700 a | ||
| <65 | 35 (66.0) | 35 (62.5) | |
| ≥65 | 18 (34.0) | 21 (37.5) | |
| Female, n (%) | 28 (52.8) | 31 (55.4) | 0.791 a |
| Immune-mediated dermatologic diseases, n (%) | 0.887 a | ||
| Autoimmune bullous diseases | 31 (58.5) | 32 (57.1) | |
| Psoriasis | 22 (41.5) | 24 (42.9) | |
| Systemic immunosuppressants used before intervention | |||
| Prednisolone, n (%) | 19 (35.9) | 17 (30.4) | 0.542 a |
| Dose (mg/day), median (IQR) | 6.3 (3.8–10.0) | 5.0 (3.8–7.5) | 0.501 b |
| Azathioprine, n (%) | 24 (45.3) | 17 (30.4) | 0.108 a |
| Dose (mg/day), median (IQR) | 62.5 (30.4–100) | 50.0 (25.0–75.0) | 0.257 b |
| Methotrexate, n (%) | 12 (22.6) | 13 (23.2) | 0.943 a |
| Dose (mg/week), median (IQR) | 10.0 (5.0–16.3) | 12.5 (10.0–12.5) | 0.599 b |
| Mycophenolate mofetil, n (%) | 0 | 3 (5.4) | 0.088 a |
| Dose (mg/day), median (IQR) | 0 | 1000 (1000–3000) | NA |
| Cyclophosphamide, n (%) | 1 (1.9) | 0 | 0.302 a |
| Dose (mg/day), median (IQR) | 14.3 (14.3–14.3) | 0 | NA |
| Cyclosporin, n (%) | 3 (5.7) | 2 (3.6) | 0.602 a |
| Dose (mg/day), median (IQR) | 50 (50–100) | 125 (100–150) | 0.128 b |
| Sulfasalazine, n (%) | 4 (7.6) | 2 (3.6) | 0.363 a |
| Dose (mg/day), median (IQR) | 2500 (1500–3000) | 2500 (2000–3000) | 0.803 b |
| Leflunomide, n (%) | 2 (3.8) | 1 (1.8) | 0.526 a |
| Dose (mg/day), median (IQR) | 20 (20–20) | 20 (20–20) | 1.000 b |
| Recent rituximab use: c, n (%) | 13 (24.5) | 10 (17.9) | 0.394 a |
| Interleukin 17/interleukin 23 inhibitors d, n (%) | 12 (22.6) | 6 (10.7) | 0.094 a |
| Tumor necrotic factor inhibitors d, n (%) | 1 (1.9) | 0 | 0.302 a |
| No systemic immunosuppressants were used, n (%) | 5 (9.4) | 14 (25.0) | 0.032 a,* |
| Previous COVID-19 vaccination, n (%) | |||
| Primary series | 0.487 a | ||
| Viral vector vaccines | 38 (71.7) | 41 (73.2) | |
| Inactivated vaccines | 9 (17.0) | 9 (16.1) | |
| Heterologous vaccines | 4 (7.6) | 6 (10.7) | |
| mRNA vaccines | 2 (3.8) | 0 | |
| Third dose | 0.693 a | ||
| mRNA vaccines | 51 (96.2) | 53 (94.6) | |
| Viral vector vaccines | 2 (3.8) | 3 (5.4) | |
| Interval between the third and fourth doses (days), median (IQR) | 148 (130–178) | 155 (136.0–183.5) | 0.507 b |
| Baseline SARS-CoV-2-specific immunity levels, median (IQR) | |||
| Anti-SARS-CoV-2 S1 RBD IgG (bau/mL) | 422.7 (153.5–927.1) | 385.0 (142.2–985.1) | 0.974 b |
| % Participants tested negative (<7.1 bau/mL) | 5 (9.4) | 3 (5.4) | 0.415 a |
| IFN-γ measured from SARS-CoV-2 IGRA (mIU/mL) | 831.3 (379.5–2031.3) | 1481.4 (270.1–3822.3) | 0.403 b |
| % Participants tested negative (≤200 mIU/mL) | 8 (15.1) | 10 (17.9) | 0.698 a |
| Participants whose immunogenicity data did not fulfil the assay sensitivity assumption, n (%) | |||
| Humoral immunogenicity outcome | 1 (1.9) | 1 (1.8) | 0.969 a |
| Cellular immunogenicity outcome | 21 (39.6) | 24 (43.6) | 0.672 a |
| Investigational Arms | p | ||
|---|---|---|---|
| fID (n = 53) | sIM (n = 56) | ||
| Vaccine-related local adverse reactions | |||
| Acute immunization site pain | 40 (75.5) | 41 (73.2) | 0.787 a |
| Pain score (possible range: 1–10), median (IQR) | 3 (2–5) | 2 (1–4) | 0.493 b |
| Delayed immunization site pain | 9 (17.0) | 13 (23.2) | 0.418 a |
| Pain score (possible range: 1–10), median (IQR) | 3 (3–3) | 5 (4–6) | 0.270 b |
| Itching, n (%) | 12 (22.6) | 0 | <0.001 a,* |
| Induration, n (%) | 6 (11.3) | 4 (7.1) | 0.336 a |
| Swelling of limb, n (%) | 0 | 1 (1.8) | 0.514 a |
| Nodule at injection site, n (%) | 0 | 0 | NA |
| Abscess or cellulitis, n (%) | 0 | 0 | NA |
| Ipsilateral lymph node enlargement or lymphadenitis, n (%) | 0 | 0 | NA |
| Bleeding at injection site, n (%) | 0 | 0 | NA |
| Local reaction persisting for > 3 days, n (%) | 3 (5.7) | 2 (3.6) | 0.474 a |
| Local reaction extending beyond the nearest joint, n (%) | 0 | 0 | NA |
| Koebner’s phenomenon, n (%) | 2 (3.8) | 0 | 0.234 a |
| Vaccine-related systemic adverse reactions | |||
| Fever, n (%) | |||
| No fever | 52 (98.1) | 49 (87.5) | |
| Fever < 38 °C | 0 | 6 (10.7) | 0.027 a,* |
| Fever ≥ 38 °C | 1 (1.9) | 1 (1.8) | |
| Headache, n (%) | 2 (3.8) | 3 (5.4) | 0.234 a |
| Chills, n (%) | 0 | 0 | NA |
| Arthritis, n (%) | 0 | 2 (3.6) | 0.262 a |
| Muscle pain, n (%) | 4 (7.6) | 11 (19.6) | 0.067 a |
| Fatigue or tiredness, n (%) | 0 | 4 (7.1) | 0.119 a |
| Drowsiness, n (%) | 0 | 2 (3.6) | 0.496 a |
| Dizziness, n (%) | 1 (1.9) | 2 (3.6) | 0.262 a |
| Upper respiratory symptoms, n (%) | 1 (1.9) | 1 (1.8) | 0.738 a |
| Others: fainting, gastrointestinal symptoms, neurological conditions, systemic cutaneous reactions, anaphylaxis, thrombocytopenia, toxic shock syndrome, sepsis, n (%) | 0 | 0 | NA |
| Duration of vaccine-related adverse reactions, n (%) | |||
| ≤1 week | 21 (39.6) | 24 (42.9) | 0.732 a |
| >1–2 weeks | 4 (7.5) | 5 (8.9) | 0.535 a |
| >2–3 weeks | 0 | 2 (3.6) | 0.262a |
| Disease activity, n (%) | |||
| Participants diagnosed with flare-ups during the study period | 4 (7.5) | 8 (14.3) | 0.261a |
| Diagnosed in less than 1 month post-intervention | 0 | 4 (7.1) | 0.066 a |
| Diagnosed after 1 month but less than 3 months post-intervention | 0 | 2 (3.6) | 0.262 a |
| Diagnosed after 3 months post-intervention | 4 (7.5) | 2 (3.6) | 0.313 a |
| Participants with dose escalation of systemic immunosuppressants despite not fulfilling flare definitions | 4 (7.5) | 5 (8.9) | 0.793 a |
| Participants with breakthrough COVID-19 during the study period, n (%) | 9 (17.0) | 7 (12.5) | 0.509 a |
| Diagnosed in less than 1 month post-intervention | 4 (7.5) | 3 (5.4) | 0.641 a |
| Diagnosed after 1 month but less than 3 months post-intervention | 3 (5.7) | 1 (1.8) | 0.288 a |
| Diagnosed after 3 months post-intervention | 3 (5.7) | 3 (5.4) | 0.634 a |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seree-aphinan, C.; Rattanakaemakorn, P.; Suchonwanit, P.; Thadanipon, K.; Ratanapokasatit, Y.; Yongpisarn, T.; Malathum, K.; Simaroj, P.; Setthaudom, C.; Lohjai, O.; et al. Immunogenicity of Intradermal Versus Intramuscular BNT162b2 COVID-19 Booster Vaccine in Patients with Immune-Mediated Dermatologic Diseases: A Non-Inferiority Randomized Controlled Trial. Vaccines 2024, 12, 73. https://doi.org/10.3390/vaccines12010073
Seree-aphinan C, Rattanakaemakorn P, Suchonwanit P, Thadanipon K, Ratanapokasatit Y, Yongpisarn T, Malathum K, Simaroj P, Setthaudom C, Lohjai O, et al. Immunogenicity of Intradermal Versus Intramuscular BNT162b2 COVID-19 Booster Vaccine in Patients with Immune-Mediated Dermatologic Diseases: A Non-Inferiority Randomized Controlled Trial. Vaccines. 2024; 12(1):73. https://doi.org/10.3390/vaccines12010073
Chicago/Turabian StyleSeree-aphinan, Chutima, Ploysyne Rattanakaemakorn, Poonkiat Suchonwanit, Kunlawat Thadanipon, Yanisa Ratanapokasatit, Tanat Yongpisarn, Kumthorn Malathum, Pornchai Simaroj, Chavachol Setthaudom, Onchuma Lohjai, and et al. 2024. "Immunogenicity of Intradermal Versus Intramuscular BNT162b2 COVID-19 Booster Vaccine in Patients with Immune-Mediated Dermatologic Diseases: A Non-Inferiority Randomized Controlled Trial" Vaccines 12, no. 1: 73. https://doi.org/10.3390/vaccines12010073
APA StyleSeree-aphinan, C., Rattanakaemakorn, P., Suchonwanit, P., Thadanipon, K., Ratanapokasatit, Y., Yongpisarn, T., Malathum, K., Simaroj, P., Setthaudom, C., Lohjai, O., Tanrattanakorn, S., & Chanprapaph, K., on behalf of COVIDVAC-DERM Study Group. (2024). Immunogenicity of Intradermal Versus Intramuscular BNT162b2 COVID-19 Booster Vaccine in Patients with Immune-Mediated Dermatologic Diseases: A Non-Inferiority Randomized Controlled Trial. Vaccines, 12(1), 73. https://doi.org/10.3390/vaccines12010073





