Impact of COVID-19 Vaccination on Short-Term Perceived Change in Physical Performance among Elite Athletes: An International Survey
Abstract
1. Introduction
2. Methods
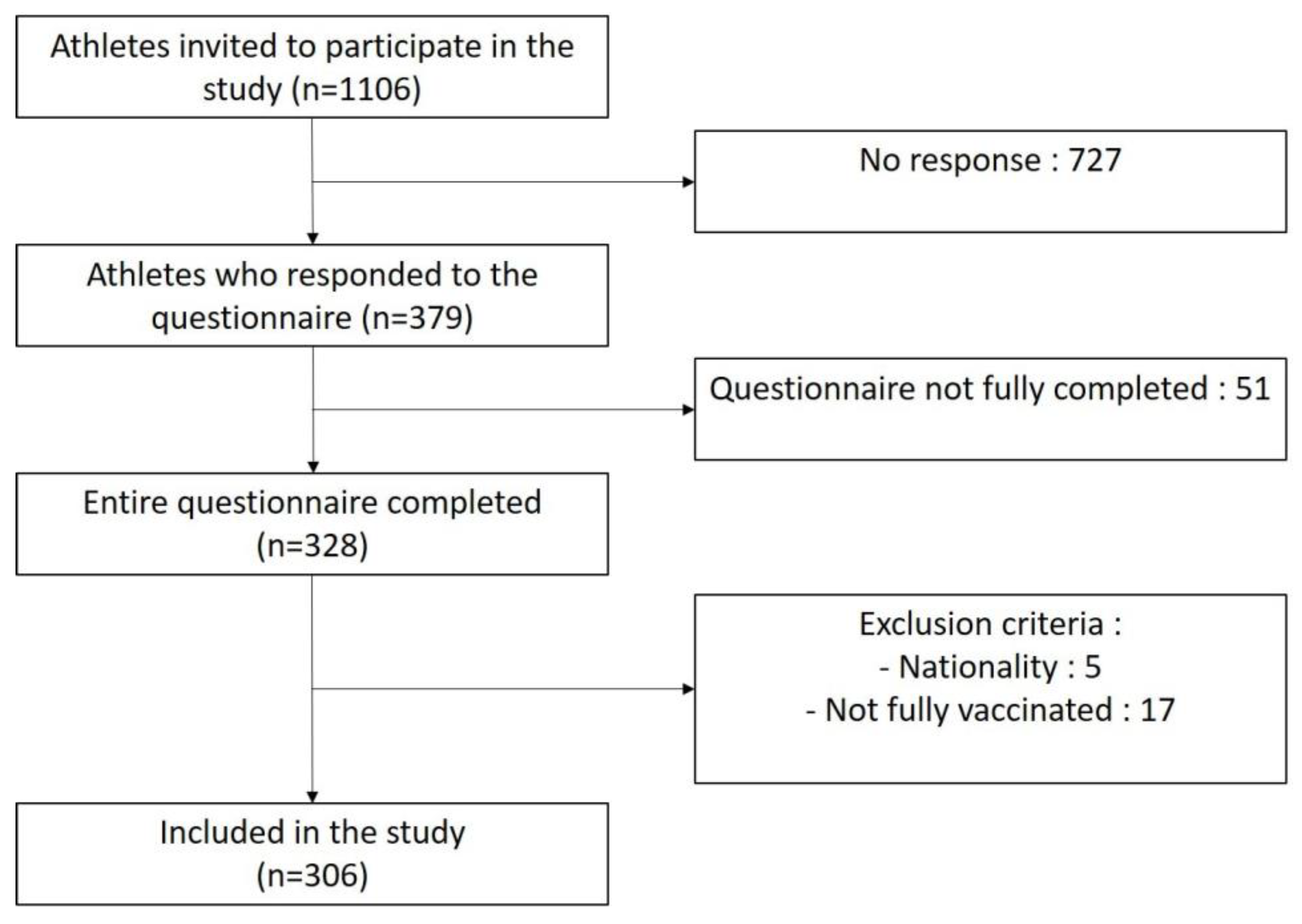
2.1. Study Procedures
2.2. Participant Recruitment
2.3. Questionnaire
2.4. Analyses
3. Results
3.1. Participant Characteristics
3.2. Perceived Change in Physical Performance Following COVID-19 Vaccination
3.3. Factors Associated with Perception of Negative Performance
3.4. Pressure to Get Vaccinated and Perception of Negative Performance
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Martens, G.; Delvaux, F.; Forthomme, B.; Kaux, J.F.; Urhausen, A.; Bieuzen, F.; Leclerc, S.; Winkler, L.; Brocherie, F.; Nedelec, M.; et al. Exercise-Based Injury Prevention in High-Level and Professional Athletes: Narrative Review and Proposed Standard Operating Procedure for Future Lockdown-Like Contexts after COVID-19. Front. Sport Act. Living 2021, 3, 745765. [Google Scholar] [CrossRef] [PubMed]
- Burki, T.K. Vaccination in the World’s Top Athletes. Lancet Respir. Med. 2022, 10, e33. [Google Scholar] [CrossRef] [PubMed]
- Hull, J.H.; Schwellnus, M.P.; Pyne, D.B.; Shah, A. COVID-19 Vaccination in Athletes: Ready, Set, Go…. Lancet Respir. Med. 2021, 9, 455–456. [Google Scholar] [CrossRef] [PubMed]
- Dighriri, I.M.; Alhusayni, K.M.; Mobarki, A.Y.; Aljerary, I.S.; Alqurashi, K.A.; Aljuaid, F.A.; Alamri, K.A.; Mutwalli, A.A.; Maashi, N.A.; Aljohani, A.M.; et al. Pfizer-BioNTech COVID-19 Vaccine (BNT162b2) Side Effects: A Systematic Review. Cureus 2022, 14, e23526. [Google Scholar] [CrossRef] [PubMed]
- Meyer, T.; Wolfarth, B.; Gärtner, B. Recommendations for Athletes to Vaccinate against SARS-CoV-2. Dtsch. Z. Sportmed./Ger. J. Sport Med. 2021, 72, E1–E4. [Google Scholar] [CrossRef]
- Narducci, D.M.; Diamond, A.B.; Bernhardt, D.T.; Roberts, W.O. COVID Vaccination in Athletes and Updated Interim Guidance on the Preparticipation Physical Examination During the SARS-CoV-2 Pandemic. Clin. J. Sport Med. 2022, 32, E1–E6. [Google Scholar] [CrossRef] [PubMed]
- Singer, M.E.; Taub, I.B.; Kaelber, D.C. Risk of Myocarditis from COVID-19 Infection in People Under Age 20: A Population-Based Analysis. medRxiv 2022. [Google Scholar] [CrossRef]
- Krzywański, J.; Mikulski, T.; Krysztofiak, H.; Pokrywka, A.; Sobierajski, T.; Młyńczak, M.; Piechuta, A.; Kuchar, E. Vaccine versus Infection—COVID-19-Related Loss of Training Time in Elite Athletes. J. Sci. Med. Sport 2022, 25, 950–959. [Google Scholar] [CrossRef] [PubMed]
- Hull, J.H.; Wootten, M.; Ranson, C. Tolerability and Impact of SARS-CoV-2 Vaccination in Elite Athletes. Lancet Respir. Med. 2022, 10, e5–e6. [Google Scholar] [CrossRef] [PubMed]
- Sobierajski, T.; Krzywański, J.; Mikulski, T.; Pokrywka, A.; Krysztofiak, H.; Kuchar, E. Sports Elite Means Vaccine Elite? Concerns and Beliefs Related to COVID-19 Vaccines among Olympians and Elite Athletes. Vaccines 2022, 10, 1676. [Google Scholar] [CrossRef] [PubMed]
- Martens, G.; Edouard, P.; Tscholl, P.; Bieuzen, F.; Winkler, L.; Cabri, J.; Urhausen, A.; Guilhem, G.; Croisier, J.L.; Thoreux, P.; et al. Document, Create and Translate Knowledge: The Mission of ReFORM, the Francophone IOC Research Centre for Prevention of Injury and Protection of Athlete Health. Br. J. Sport. Med. 2021, 55, 187. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The Janssen Ad26.COV2.S COVID-19 Vaccine: What You Need to Know. Available online: https://www.who.int/news-room/feature-stories/detail/the-j-j-covid-19-vaccine-what-you-need-to-know (accessed on 25 August 2022).
- Centers for Disease Control and Prevention. Clinical Guidance for COVID-19 Vaccination|CDC. Available online: https://www.cdc.gov/vaccines/covid-19/clinical-considerations/interim-considerations-us.html (accessed on 25 August 2022).
- Agha-Alinejad, H.; Hekmatikar, A.H.A.; Ruhee, R.T.; Shamsi, M.M.; Rahmati, M.; Khoramipour, K.; Suzuki, K. A Guide to Different Intensities of Exercise, Vaccination, and Sports Nutrition in the Course of Preparing Elite Athletes for the Management of Upper Respiratory Infections during the COVID-19 Pandemic: A Narrative Review. Int. J. Environ. Res. Public Health 2022, 19, 1888. [Google Scholar] [CrossRef] [PubMed]
- Colloca, L.; Barsky, A.J. Placebo and Nocebo Effects. N. Engl. J. Med. 2020, 382, 554–561. [Google Scholar] [CrossRef] [PubMed]
- Meeusen, R.; Roelands, B.; Spriet, L.L. Caffeine, Exercise and the Brain. Nestle Nutr. Inst. Workshop Ser. 2013, 76, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Batatinha, H.; Baker, F.L.; Smith, K.A.; Zúñiga, T.M.; Pedlar, C.R.; Burgess, S.C.; Katsanis, E.; Simpson, R.J. Recent COVID-19 Vaccination Has Minimal Effects on the Physiological Responses to Graded Exercise in Physically Active Healthy People. J. Appl. Physiol. 2022, 132, 275–282. [Google Scholar] [CrossRef] [PubMed]
- Rubio, V.J.; Sánchez-Iglesias, I.; Bueno, M.; Martin, G. Athletes’ Psychological Adaptation to Confinement Due to COVID-19: A Longitudinal Study. Front. Psychol. 2020, 11, 613495. [Google Scholar] [CrossRef] [PubMed]
- Van Gelder, M.M.H.J.; Bretveld, R.W.; Roeleveld, N. Web-Based Questionnaires: The Future in Epidemiology? Am. J. Epidemiol. 2010, 172, 1292–1298. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Patiño, M.J.; Lopez, F.J.B.; Dubois, M.; Vilain, E.; Fuentes-García, J.P. Effects of COVID-19 Home Confinement on Behavior, Perception of Threat, Stress and Training Patterns of Olympic and Paralympic Athletes. Int. J. Environ. Res. Public Health 2021, 18, 12780. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Number | Frequency (%) | Median (P25–P75) | |
|---|---|---|---|---|
| Sociodemographic | ||||
| Age (years) | <18 | 48 | 15.7 | |
| 18–25 | 157 | 51.3 | ||
| >25 | 101 | 33.0 | ||
| Nationality | Belgium | 178 | 58.2 | |
| Canada | 49 | 16.0 | ||
| France | 60 | 19.6 | ||
| Luxembourg | 19 | 6.2 | ||
| Sport | Collective | 86 | 28.1 | |
| Individual | 220 | 71.9 | ||
| Sport by week (hours) | Between 5 and 10 | 16 | 5.2 | |
| Between 11 and 20 | 151 | 49.4 | ||
| Between 21 and 35 | 127 | 41.5 | ||
| Between 36 and 50 | 12 | 3.9 | ||
| COVID-19 positive | Yes | 114 | 37.3 | |
| No | 192 | 62.7 | ||
| COVID-19 positive before | Yes | 58 | 50.9 | |
| first dose of vaccine | No | 56 | 49.1 | |
| COVID-19 vaccination | ||||
| First dose of vaccine (n = 306) | ||||
| Vaccine type | AstraZeneca | 7 | 2.3 | |
| Johnson & Johnson | 28 | 9.1 | ||
| Moderna | 15 | 4.9 | ||
| Pfizer/BioNTech | 256 | 83.7 | ||
| Level of vaccine reactions (VAS) | 10 (2.5–40) | |||
| Duration of vaccine reactions | No reaction | 88 | 28.8 | |
| Less than 1 day | 61 | 19.9 | ||
| Between 1 and 3 days | 133 | 43.5 | ||
| More than 3 days | 24 | 7.8 | ||
| Impact of vaccine reactions on training (VAS) | 50 (20–50) | |||
| Second dose of vaccine (n = 294) | ||||
| Vaccine type | AstraZeneca | 6 | 2.0 | |
| Johnson & Johnson | 3 | 1.0 | ||
| Moderna | 19 | 6.5 | ||
| Pfizer/BioNTech | 266 | 90.5 | ||
| Level of vaccine reactions (VAS) | 10 (0–50) | |||
| Duration of vaccine reactions | No side reaction | 104 | 35.4 | |
| Less than 1 day | 42 | 14.3 | ||
| Between 1 and 3 days | 104 | 35.4 | ||
| More than 3 days | 44 | 14.9 | ||
| Impact of vaccine reactions on training (VAS) | 46 (20–50) |
| Perceived Impact on Physical Performance | |||
|---|---|---|---|
| Duration of Vaccine Reactions | |||
| No Performance Impact | Negative Impact | Positive Impact | |
| No reaction | 221 (72.2%) | ||
| Reaction less than 1 day | 2 (0.7%) | 1 (0.3%) | |
| Between 1 and 3 days | 15 (4.9%) | 3 (1.0%) | |
| Between 4 and 7 days | 12 (3.9%) | 3 (1.0%) | |
| Between 8 and 30 days | 23 (7.5%) | 1 (0.3%) | |
| More than 30 days | 20 (6.5%) | 5 (1.7%) | |
| Characteristics | No Negative Impact or Negative Impact <3 Days (n = 251) | Negative Impact >3 Days (n = 55) | p-Value |
|---|---|---|---|
| Age (years) | |||
| <18 | 45 (17.9%) | 3 (5.5%) | 0.006 |
| 18–25 | 132 (52.6%) | 25 (45.4%) | |
| >25 | 74 (29.5%) | 27 (49.1%) | |
| Sport | |||
| Collective | 82 (32.7%) | 4 (8.9%) | <0.0001 |
| Individual | 169 (67.3%) | 51 (91.1%) | |
| Training hours per week | |||
| Between 5 and 10 | 15 (6.0%) | 1 (1.8%) | 0.15 |
| Between 11 and 20 | 129 (51.4%) | 22 (40.0%) | |
| Between 21 and 35 | 97 (38.6%) | 30 (54.6%) | |
| Between 36 and 50 | 10 (4.0%) | 2 (3.6%) | |
| Type of vaccine | 0.94 | ||
| AstraZeneca | 6 (2.4%) | 1 (1.8%) | |
| Johnson & Johnson | 25 (9.9%) | 3 (5.5%) | |
| Moderna | 13 (5.2%) | 2 (3.6%) | |
| Pfizer/BioNTech | 207 (82.5%) | 49 (89.1%) | |
| First dose of vaccine (n = 306) | |||
| Level of vaccine reactions (VAS) | 10 (0–40) | 30 (10–70) | <0.0001 |
| Duration of vaccine reactions | |||
| No vaccine reaction | 83 (33.1%) | 5 (9.1%) | <0.0001 |
| Less than 1 day | 57 (22.7%) | 4 (7.3%) | |
| Between 1 and 3 days | 106 (42.2%) | 27 (49.1%) | |
| More than 3 days | 5 (2.0%) | 19 (34.5%) | |
| Impact on training (VAS) | 50 (30–50) | 20 (0–50) | <0.0001 |
| Second dose of vaccine (n = 294) | |||
| Level of vaccine reactions (VAS) | 10 (0–30) | 70 (40–90) | <0.0001 |
| Duration of vaccine reactions | |||
| No vaccine reaction | 100 (41.8%) | 4 (7.3%) | <0.0001 |
| Less than 1 day | 38 (15.9%) | 4 (7.3%) | |
| Between 1 and 3 days | 88 (36.8%) | 16 (29.1%) | |
| More than 3 days | 13 (5.4%) | 31 (56.4%) | |
| Impact on training (VAS) | 49 (30–50) | 10 (0–30) | <0.0001 |
| Injury since vaccination | |||
| Yes | 84 (35.1%) | 20 (36.4%) | 0.86 |
| No | 155 (64.9%) | 35 (63.6%) | |
| Pressure to get vaccinated | 30 (0–70) | 80 (60–100) | <0.0001 |
| Positive for COVID-19 before first dose | |||
| Yes | 50 (19.9%) | 8 (14.5%) | 0.36 |
| No | 201 (80.1%) | 47 (85.5%) |
| Characteristics | OR (IC95%) | p-Value |
|---|---|---|
| Age (years) Ref: <18 | ||
| 18–25 | 1.54 (0.33–9.34) | 0.60 |
| >25 | 1.89 (0.39–11.73) | 0.45 |
| Sport Ref: collective | ||
| Individual | 5.56 (1.51–27.64) | 0.02 |
| First vaccine | ||
| Level of vaccine reactions | 0.98 (0.95–1.00) | 0.09 |
| Duration of vaccine reaction Ref: No reaction | ||
| Less than 1 day | 1.21 (0.20–6.75) | 0.83 |
| Between 1 and 3 days | 3.47 (0.76–17.43) | 0.12 |
| More than 3 days | 61.58 (5.93–840.91) | 0.001 |
| Impact on training | 0.99 (0.96–1.01) | 0.29 |
| Second vaccine | ||
| Level of vaccine reactions | 1.03 (1.01–1.06) | 0.004 |
| Duration of vaccine reaction Ref: No reaction | ||
| Less than 1 day | 0.92 (0.15–5.37) | 0.92 |
| Between 1 and 3 days | 0.34 (0.06–2.05) | 0.23 |
| More than 3 days | 0.93 (0.10–8.62) | 0.94 |
| Impact on training | 0.98 (0.96–1.01) | 0.21 |
| Pressure to get vaccinated | 1.02 (1.01–1.04) | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bruyère, O.; Martens, G.; Demonceau, C.; Urhausen, A.; Seil, R.; Leclerc, S.; Le Garrec, S.; Le Van, P.; Edouard, P.; Tscholl, P.M.; et al. Impact of COVID-19 Vaccination on Short-Term Perceived Change in Physical Performance among Elite Athletes: An International Survey. Vaccines 2023, 11, 796. https://doi.org/10.3390/vaccines11040796
Bruyère O, Martens G, Demonceau C, Urhausen A, Seil R, Leclerc S, Le Garrec S, Le Van P, Edouard P, Tscholl PM, et al. Impact of COVID-19 Vaccination on Short-Term Perceived Change in Physical Performance among Elite Athletes: An International Survey. Vaccines. 2023; 11(4):796. https://doi.org/10.3390/vaccines11040796
Chicago/Turabian StyleBruyère, Olivier, Géraldine Martens, Céline Demonceau, Axel Urhausen, Romain Seil, Suzanne Leclerc, Sébastien Le Garrec, Philippe Le Van, Pascal Edouard, Philippe M Tscholl, and et al. 2023. "Impact of COVID-19 Vaccination on Short-Term Perceived Change in Physical Performance among Elite Athletes: An International Survey" Vaccines 11, no. 4: 796. https://doi.org/10.3390/vaccines11040796
APA StyleBruyère, O., Martens, G., Demonceau, C., Urhausen, A., Seil, R., Leclerc, S., Le Garrec, S., Le Van, P., Edouard, P., Tscholl, P. M., Delvaux, F., Toussaint, J.-F., & Kaux, J.-F., on behalf of the Réseau Francophone Olympique de la Recherche en Médecine du Sport (ReFORM) Research Centre. (2023). Impact of COVID-19 Vaccination on Short-Term Perceived Change in Physical Performance among Elite Athletes: An International Survey. Vaccines, 11(4), 796. https://doi.org/10.3390/vaccines11040796








