Factors Associated with Vaccination Uptake among Young Children: A Follow-Up Study of 1799 Toddlers
Abstract
1. Introduction
2. Materials and Methods
2.1. Subject Recruitment
2.2. Survey Instruments
2.3. Definition of Variables
2.4. Statistical Analysis
3. Results
3.1. Respondents’ Characteristics
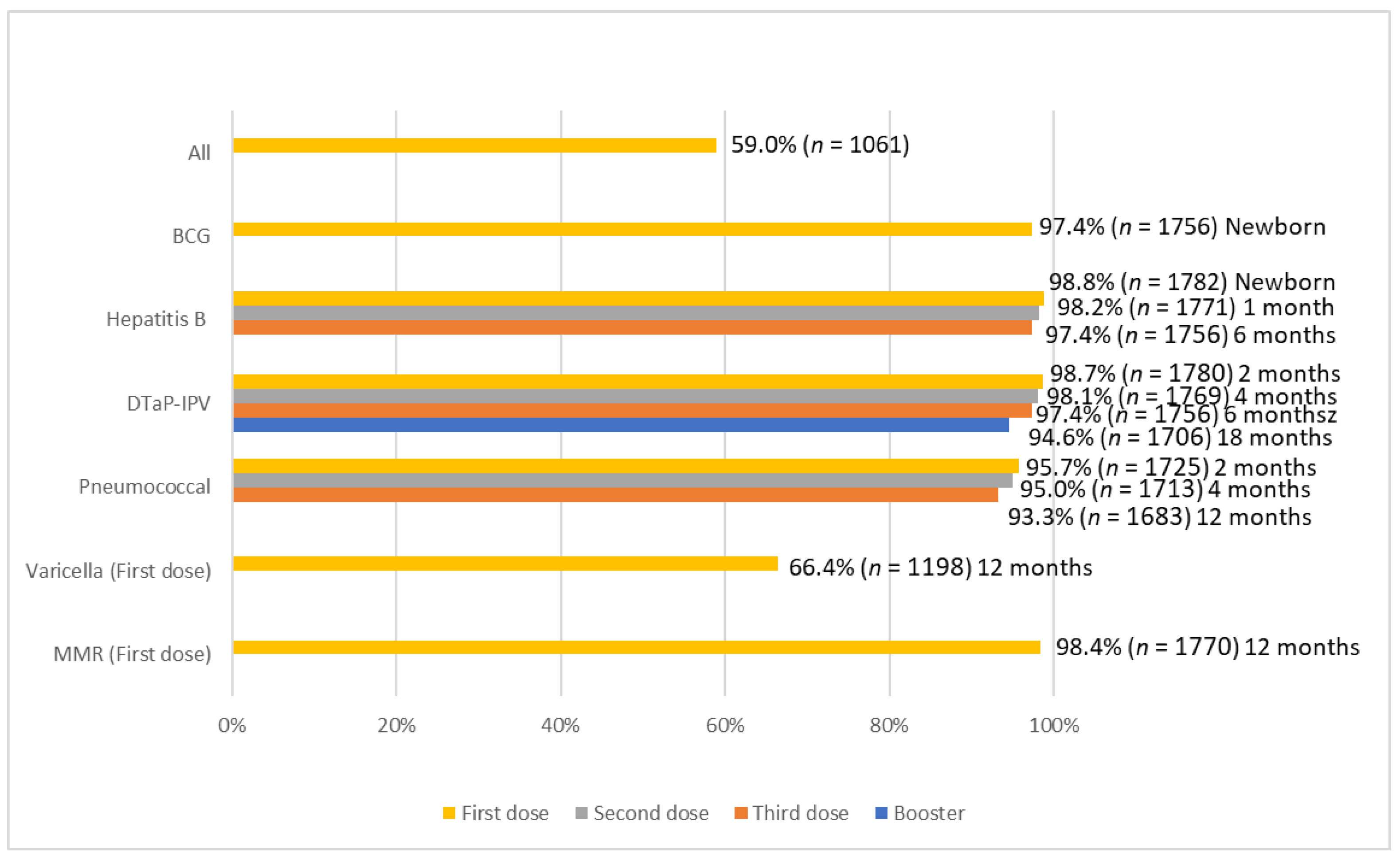
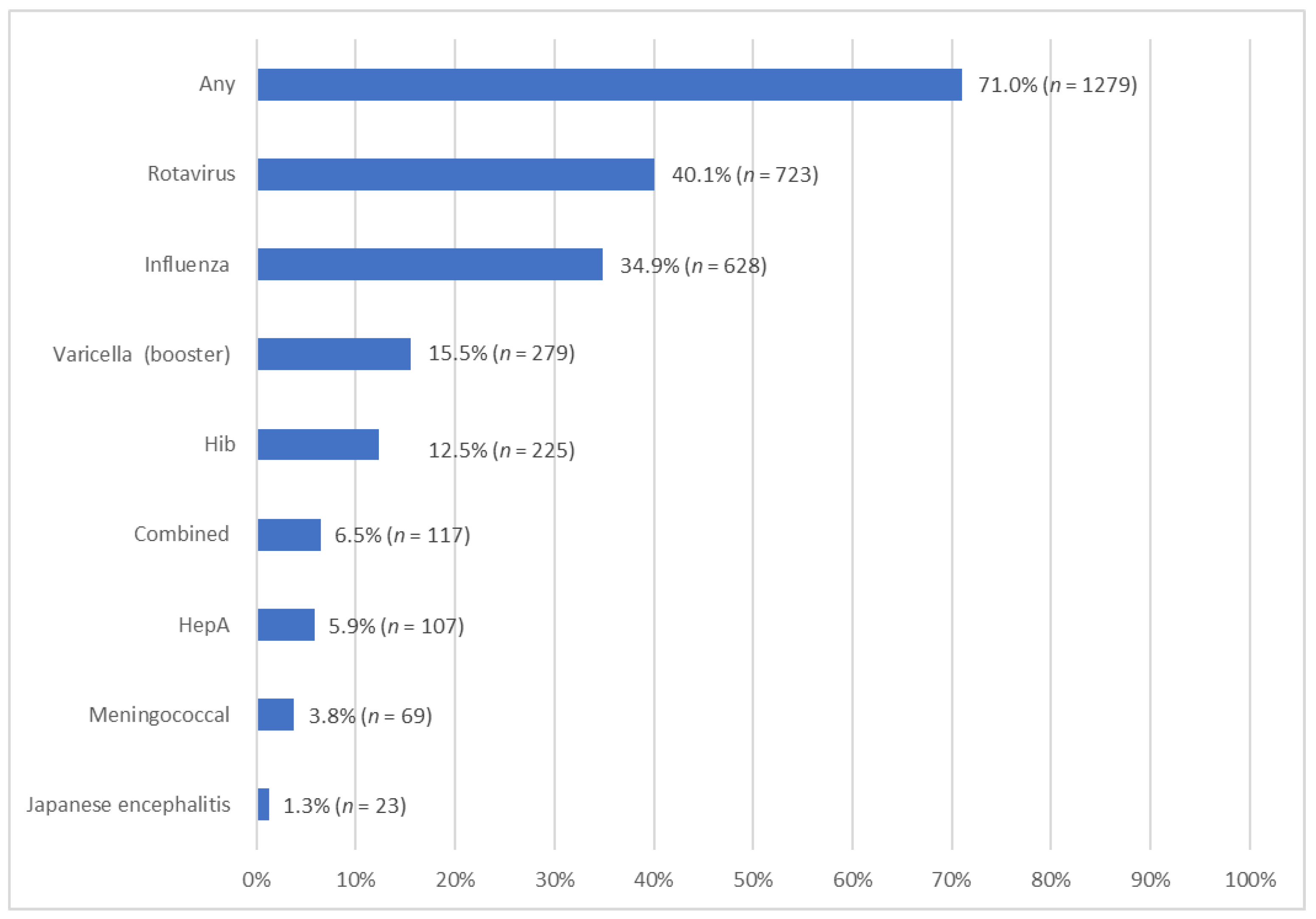
3.2. Prevalence of the Uptake of Vaccination
3.3. Factors Associated with Uptake of Vaccination
4. Discussion
4.1. Summary of Major Findings
4.2. Explanations and Comparisons with Previous Literature
4.3. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Vaccines and Immunization. 2022. Available online: https://www.who.int/health-topics/vaccines-and-immunization#tab=tab_1 (accessed on 29 December 2022).
- Nandi, A.; Shet, A. Why vaccines matter: Understanding the broader health, economic, and child development benefits of routine vaccination. Hum. Vaccines Immunother. 2020, 16, 1900–1904. [Google Scholar] [CrossRef] [PubMed]
- The Government of the Hong Kong Special Administrative Region. LCQ13: Childhood Immunisation Programme. Press Releases. Available online: https://www.info.gov.hk/gia/general/200802/20/P200802200145.htm (accessed on 29 December 2022).
- Family Health Service. Child Health. Schedule of Hong Kong Childhood Immunisation Programme. Sep 2022. Available online: https://www.fhs.gov.hk/english/main_ser/child_health/child_health_recommend.html (accessed on 29 December 2022).
- World Health Organization. Vaccines and Immunization: Myths and Misconceptions. Newsroom. Oct 2020. Available online: https://www.who.int/news-room/questions-and-answers/item/vaccines-and-immunization-myths-and-misconceptions (accessed on 29 December 2022).
- de Cantuária Tauil, M.; Sato, A.P.S.; Waldman, E.A. Factors associated with incomplete or delayed vaccination across countries: A systematic review. Vaccine 2016, 34, 2635–2643. [Google Scholar] [CrossRef] [PubMed]
- Cotter, J.J.; Bramble, J.D.; Bovbjerg, V.E.; Pugh, C.B.; McClish, D.K.; Tipton, G.; Smith, W.R. Timeliness of immunizations of children in a Medicaid primary care case management managed care program. J. Natl. Med. Assoc. 2002, 94, 833. [Google Scholar] [PubMed]
- Smith, L.E.; Amlôt, R.; Weinman, J.; Yiend, J.; Rubin, G.J. A systematic review of factors affecting vaccine uptake in young children. Vaccine 2017, 35, 6059–6069. [Google Scholar] [CrossRef]
- Wei, F.; Mullooly, J.P.; Goodman, M.; McCarty, M.C.; Hanson, A.M.; Crane, B.; Nordin, J.D. Identification and characteristics of vaccine refusers. BMC Pediatrics 2009, 9, 18. [Google Scholar] [CrossRef]
- Lau, Y.L.; Wong, W.H.S.; Hattangdi-Haridas, S.R.; Chow, C.B. Evaluating impact of school outreach vaccination programme in Hong Kong influenza season 2018–2019. Hum. Vaccines Immunother. 2020, 16, 823–826. [Google Scholar] [CrossRef]
- Wong, W.H.-S.; Peare, S.; Lam, H.Y.; Chow, C.B.; Lau, Y.L. The estimated age-group specific influenza vaccine coverage rates in Hong Kong and the impact of the school outreach vaccination program. Hum. Vaccines Immunother. 2022, 18, 1–5. [Google Scholar] [CrossRef]
- Rochon, J.; Gondan, M.; Kieser, M. To test or not to test: Preliminary assessment of normality when comparing two independent samples. BMC Med. Res. Methodol. 2012, 12, 81. [Google Scholar] [CrossRef]
- World Health Organization. Immunization Coverage. Jul 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/immunization-coverage (accessed on 29 December 2022).
- The Government of the Hong Kong Special Administrative Region. Chickenpox Vaccine to Incorporate into DH Childhood Immunisation Programme on July 2. Press Release. June 2014. Available online: https://www.info.gov.hk/gia/general/201406/24/P201406240290.htm (accessed on 29 December 2022).
- Hagemann, C.; Streng, A.; Kraemer, A.; Liese, J.G. Heterogeneity in coverage for measles and varicella vaccination in toddlers–analysis of factors influencing parental acceptance. BMC Public Health 2017, 17, 724. [Google Scholar] [CrossRef]
- Huber, A.; Gazder, J.; Dobay, O.; Mészner, Z.; Horváth, A. Attitudes towards varicella vaccination in parents and paediatric healthcare providers in Hungary. Vaccine 2020, 38, 5249–5255. [Google Scholar] [CrossRef]
- Centre for Health Protection. Number of Notifiable Infectious Diseases by Month in 2021. Statistics. Oct 2022. Available online: https://www.chp.gov.hk/en/statistics/data/10/26/43/6940.html (accessed on 29 December 2022).
- Centre for Health Protection. Japanese Encephalitis. Health Topics. Aug 2018. Available online: https://www.chp.gov.hk/en/healthtopics/content/24/28.html (accessed on 29 December 2022).
- Centre for Health Protection. Meningococcal Infection. Health Topics. Sep 2020. Available online: https://www.chp.gov.hk/en/healthtopics/content/24/2086.html (accessed on 29 December 2022).
- Centre for Health Protection. Haemophilus Influenzae Type b Infection. Health Topics. July 2019. Available online: https://www.chp.gov.hk/en/healthtopics/content/24/8870.html (accessed on 29 December 2022).
- Centre for Health Protection. Rotavirus Infection. Health Topics. July 2019. Available online: https://www.chp.gov.hk/en/healthtopics/content/24/38.html (accessed on 29 December 2022).
- Yawn, B.P.; Xia, Z.; Edmonson, L.; Jacobson, R.M.; Jacobsen, S.J. Barriers to immunization in a relatively affluent community. J. Am. Board Fam. Pract. 2000, 13, 325–332. [Google Scholar] [PubMed]
- Smith, P.J.; Humiston, S.G.; Parnell, T.; Vannice, K.S.; Salmon, D.A. The association between intentional delay of vaccine administration and timely childhood vaccination coverage. Public Health Rep. 2010, 125, 534–541. [Google Scholar] [CrossRef] [PubMed]
- Brunson, E.K. The impact of social networks on parents’ vaccination decisions. Pediatrics 2013, 131, e1397–e1404. [Google Scholar] [CrossRef] [PubMed]
- De Figueiredo, A.; Simas, C.; Karafillakis, E.; Paterson, P.; Larson, H.J. Mapping global trends in vaccine confidence and investigating barriers to vaccine uptake: A large-scale retrospective temporal modelling study. Lancet 2020, 396, 898–908. [Google Scholar] [CrossRef]
- Bell, C.A.; Simmonds, K.A.; MacDonald, S.E. Exploring the heterogeneity among partially vaccinated children in a population-based cohort. Vaccine 2015, 33, 4572–4578. [Google Scholar] [CrossRef]
- Antai, D. Gender inequities, relationship power, and childhood immunization uptake in Nigeria: A population-based cross-sectional study. Int. J. Infect. Dis. 2012, 16, e136–e145. [Google Scholar] [CrossRef]
- Baker, S.; Sanders, M.R.; Morawska, A. Who uses online parenting support? A cross-sectional survey exploring Australian parents’ internet use for parenting. J. Child Fam. Stud. 2017, 26, 916–927. [Google Scholar] [CrossRef]
- Wang, Y.; McKee, M.; Torbica, A.; Stuckler, D. Systematic literature review on the spread of health-related misinformation on social media. Soc. Sci. Med. 2019, 240, 112552. [Google Scholar] [CrossRef]
- Babirye, J.N.; Engebretsen, I.M.; Makumbi, F.; Fadnes, L.T.; Wamani, H.; Tylleskar, T.; Nuwaha, F. Timeliness of childhood vaccinations in Kampala Uganda: A community-based cross-sectional study. PLoS ONE 2012, 7, e35432. [Google Scholar] [CrossRef]
- Bondy, J.N.; Thind, A.; Koval, J.J.; Speechley, K.N. Identifying the determinants of childhood immunization in the Philippines. Vaccine 2009, 27, 169–175. [Google Scholar] [CrossRef]
- Bobo, J.K.; Gale, J.L.; Thapa, P.B.; Wassilak, S.G. Risk factors for delayed immunization in a random sample of 1163 children from Oregon and Washington. Pediatrics 1993, 91, 308–314. [Google Scholar] [CrossRef]
- Barata, R.B.; de Almeida Ribeiro, M.C.S.; de Moraes, J.C.; Flannery, B.; Vaccine Coverage Survey 2007 Group. Socioeconomic inequalities and vaccination coverage: Results of an immunisation coverage survey in 27 Brazilian capitals, 2007–2008. J. Epidemiol. Community Health 2012, 66, 934–941. [Google Scholar] [CrossRef] [PubMed]
- Pruckner, G.J.; Schneeweis, N.; Schober, T.; Zweimüller, M. Birth order, parental health investment, and health in childhood. J. Health Econ. 2021, 76, 102426. [Google Scholar] [CrossRef] [PubMed]
- Fathima, P.; Gidding, H.F.; Snelling, T.L.; McIntyre, P.B.; Blyth, C.C.; Sheridan, S.; Liu, B.; de Klerk, N.; Moore, H.C. Timeliness and factors associated with rotavirus vaccine uptake among Australian Aboriginal and non-Aboriginal children: A record linkage cohort study. Vaccine 2019, 37, 5835–5843. [Google Scholar] [CrossRef] [PubMed]
- Slack, M.; Thwaites, R. Timing of immunisation of premature infants on the neonatal unit and after discharge to the community. Commun. Dis. Public Health 2000, 3, 303–304. [Google Scholar] [PubMed]
- McKechnie, L.; Finlay, F. Uptake and timing of immunisations in preterm and term infants. Prof. Care Mother Child 1999, 9, 19–21. [Google Scholar]
- Sisson, H.; Gardiner, E.; Watson, R. Vaccination timeliness in preterm infants: An integrative review of the literature. J. Clin. Nurs. 2017, 26, 4094–4104. [Google Scholar] [CrossRef]
- Khader, Y.S.; Al-Akour, N.; AlZubi, I.M.; Lataifeh, I. The association between second hand smoke and low birth weight and preterm delivery. Matern. Child Health J. 2011, 15, 453–459. [Google Scholar] [CrossRef]
- Crane, J.; Keough, M.; Murphy, P.; Burrage, L.; Hutchens, D. Effects of environmental tobacco smoke on perinatal outcomes: A retrospective cohort study. BJOG Int. J. Obstet. Gynaecol. 2011, 118, 865–871. [Google Scholar] [CrossRef]
- Treyster, Z.; Gitterman, B. Second hand smoke exposure in children: Environmental factors, physiological effects, and interventions within pediatrics. Rev. Environ. Health 2011, 26, 187–195. [Google Scholar] [CrossRef]
- Ngo, C.Q.; Phan, P.T.; Vu, G.V.; Chu, H.T.; Nguyen, T.T.; Nguyen, M.H.; Phan, H.T.; Ong, B.M.Y.; Vu, G.T.; Pham, K.T.H.; et al. Prevalence and sources of second-hand smoking exposure among non-smoking pregnant women in an urban setting of Vietnam. Int. J. Environ. Res. Public Health 2019, 16, 5022. [Google Scholar] [CrossRef] [PubMed]
- Smith, P.J.; Marcuse, E.K.; Seward, J.F.; Zhao, Z.; Orenstein, W.A. Children and adolescents unvaccinated against measles: Geographic clustering, parents’ beliefs, and missed opportunities. Public Health Rep. 2015, 130, 485–504. [Google Scholar] [CrossRef] [PubMed]
- Kaur, B. Attitudes, Risks and Norms: Understanding Parents’ Measles-Mumps-Rubella (MMR) Immunisation Decision-Making. Ph.D. Thesis, University of Stirling, Scotland, UK, 2011. [Google Scholar]
- Huang, J.; Chan, S.C.; Ko, S.; Wang, H.H.X.; Yuan, J.; Xu, W.; Zheng, Z.-J.; Xue, H.; Zhang, L.; Jiang, J.Y.; et al. Factors Associated with Vaccination Intention against the COVID-19 Pandemic: A Global Population-Based Study. Vaccines 2022, 10, 1539. [Google Scholar] [CrossRef] [PubMed]
| n | Proportion% | |
|---|---|---|
| Sex | ||
| Female | 846 | 47.0% |
| Male | 953 | 53.0% |
| Age (mean ± SD) 3.42 ± 0.50 | ||
| Delivery | ||
| Vaginally and not induced (ref) | 962 | 58.3% |
| Vaginally and induced | 135 | 8.2% |
| Caesarean section | 552 | 33.5% |
| Weeks of pregnancy | ||
| 40 weeks or more (ref) | 590 | 35.8% |
| 37–39 weeks | 972 | 59.0% |
| 36 weeks or less | 85 | 5.2% |
| Order of birth | ||
| First-born (ref) | 1079 | 65.3% |
| Second-born | 476 | 28.8% |
| Third-born | 97 | 5.9% |
| Monthly household income | ||
| Below HKD 15,000 | 260 | 16.9% |
| HKD 15,000–HKD 29,999 | 472 | 30.6% |
| HKD 30,000 or above | 809 | 52.5% |
| Educational background of mother | ||
| Primary school or below | 33 | 2.0% |
| Secondary school | 797 | 48.8% |
| Post-secondary | 804 | 49.2% |
| Educational background of father | ||
| Primary school or below | 39 | 2.4% |
| Secondary school | 765 | 47.4% |
| Post-secondary | 809 | 50.2% |
| Age group of mother (mean ± SD) 32.79 ± 4.61 | ||
| 24 or below | 79 | 4.9% |
| 25–34 | 1025 | 63.1% |
| 35–39 | 422 | 26.0% |
| 40 or above | 98 | 6.0% |
| Age group of father (mean ± SD) 36.11 ± 6.30 | ||
| 24 or below | 24 | 1.5% |
| 25–34 | 716 | 44.9% |
| 35–39 | 503 | 31.6% |
| 40 or above | 351 | 22.0% |
| Drinking during pregnancy (mother) | ||
| No | 1572 | 97.0% |
| Yes | 48 | 3.0% |
| Smoking during pregnancy (mother) | ||
| No | 1605 | 97.7% |
| Yes | 38 | 2.3% |
| Smoking during pregnancy (father) | ||
| No | 1232 | 75.9% |
| Yes | 391 | 24.1% |
| Complications/health problems during pregnancy | ||
| No | 1240 | 75.1% |
| Yes | 411 | 24.9% |
| Hospitalization since birth (toddler) | ||
| Never or 1 time only | 1386 | 78.6% |
| 2 times or more | 377 | 21.4% |
| n | Prevalence % | Adjusted Odd Ratio (aOR) | 95% CI | p-Value | |
|---|---|---|---|---|---|
| Sex | |||||
| Female | 505 | 59.7% | 1 (ref) | ||
| Male | 556 | 58.3% | 0.939 | 0.745–1.184 | 0.595 |
| Age | 0.606 | 0.480–0.766 | <0.001 * | ||
| Delivery | |||||
| Vaginally and not induced (ref) | 560 | 58.2% | 1 (ref) | ||
| Vaginally and induced | 89 | 65.9% | 1.410 | 0.891–2.230 | 0.143 |
| Caesarean section | 333 | 60.3% | 0.919 | 0.708–1.194 | 0.528 |
| Weeks of Pregnancy | |||||
| 40 weeks or more (ref) | 314 | 53.2% | 1 (ref) | ||
| 37–39 weeks | 622 | 64.0% | 1.459 | 1.136–1.873 | 0.003 * |
| 36 weeks or less | 47 | 55.3% | 1.181 | 0.675–2.065 | 0.561 |
| Order of birth | |||||
| First-born (ref) | 693 | 64.2% | 1 (ref) | ||
| Second-born | 251 | 52.7% | 0.620 | 0.477–0.807 | <0.001 * |
| Third-born | 40 | 41.2% | 0.326 | 0.192–0.553 | <0.001* |
| Monthly household income | |||||
| Below HKD 15,000 | 101 | 38.8% | 1 (ref) | ||
| HKD 15,000-HKD 29,999 | 250 | 53.0% | 1.801 | 1.270–2.553 | 0.001 * |
| HKD 30,000 or above | 580 | 71.7% | 3.423 | 2.389–4.904 | <0.001 * |
| Educational background of mother | |||||
| Primary school or below | 9 | 27.3% | 1 (ref) | ||
| Secondary school | 425 | 53.3% | 2.110 | 0.759–5.863 | 0.152 |
| Post-secondary | 543 | 67.5% | 2.056 | 0.724–5.840 | 0.176 |
| Educational background of father | |||||
| Primary school or below | 15 | 38.5% | 1 (ref) | ||
| Secondary school | 415 | 54.2% | 1.624 | 0.687–3.844 | 0.270 |
| Post-secondary | 538 | 66.5% | 1.674 | 0.687–4.076 | 0.257 |
| Age group of mothers (at toddler’s birth) | |||||
| 24 or below | 31 | 39.7% | 1 (ref) | ||
| 25–34 | 609 | 59.5% | 1.870 | 0.993–3.521 | 0.053 |
| 35–39 | 263 | 62.3% | 2.449 | 1.217–4.930 | 0.012 * |
| 40 or above | 60 | 61.2% | 2.897 | 1.240–6.766 | 0.014 * |
| Age group of father (at toddler’s birth) | |||||
| 24 or below | 10 | 41.7% | 1 (ref) | ||
| 25–34 | 437 | 61.0% | 1.587 | 0.536–4.702 | 0.404 |
| 35–39 | 304 | 60.4% | 1.264 | 0.417–3.832 | 0.679 |
| 40 or above | 200 | 57.0% | 1.302 | 0.423–4.010 | 0.645 |
| Drinking during pregnancy (mother) | |||||
| No | 940 | 59.8% | 1 (ref) | ||
| Yes | 30 | 62.5% | 1.019 | 0.506–2.054 | 0.958 |
| Smoking during pregnancy (mother) | |||||
| No | 959 | 59.8% | 1 (ref) | ||
| Yes | 21 | 55.3% | 2.207 | 0.914–5.331 | 0.078 |
| Smoking during pregnancy (father) | |||||
| No | 774 | 62.8% | 1 (ref) | ||
| Yes | 198 | 50.6% | 0.960 | 0.713–1.292 | 0.786 |
| Complications/health problems during pregnancy | |||||
| No | 721 | 58.1% | 1 (ref) | ||
| Yes | 263 | 64.0% | 1.019 | 0.777–1.336 | 0.892 |
| Hospitalization since birth (toddler) | |||||
| Never or 1 time only | 819 | 59.1% | 1 (ref) | ||
| 2 times or more | 229 | 60.7% | 1.165 | 0.877–1.547 | 0.293 |
| n | Prevalence % | Adjusted Odd Ratio (aOR) | 95% CI | p-Value | |
|---|---|---|---|---|---|
| Sex | |||||
| Female | 599 | 70.6% | 1 (ref) | ||
| Male | 680 | 71.4% | 1.138 | 0.884–1.465 | 0.317 |
| Age | 1.315 | 1.018–1.698 | 0.036 * | ||
| Delivery | |||||
| Vaginally and not induced (ref) | 694 | 72.0% | 1 (ref) | ||
| Vaginally and induced | 92 | 68.1% | 0.646 | 0.409–1.021 | 0.061 |
| Caesarean section | 399 | 72.3% | 0.778 | 0.584–1.037 | 0.087 |
| Weeks of pregnancy | |||||
| 40 weeks or more (ref) | 399 | 67.6% | 1 (ref) | ||
| 37 – 39 weeks | 723 | 74.2% | 1.210 | 0.938–1.607 | 0.136 |
| 36 weeks or less | 62 | 72.9% | 1.907 | 0.970–3.747 | 0.061 |
| Order of birth | |||||
| First-born (ref) | 808 | 74.7% | 1 (ref) | ||
| Second-born | 318 | 66.8% | 0.742 | 0.556–0.991 | 0.043 * |
| Third-born | 60 | 61.9% | 0.552 | 0.319–0.955 | 0.034 * |
| Monthly household income | |||||
| Below HKD 15,000 | 158 | 60.3% | 1 (ref) | ||
| HKD 15,000-HKD 29,999 | 314 | 66.4% | 1.143 | 0.794–1.644 | 0.473 |
| HKD 30,000 or above | 644 | 79.6% | 1.612 | 1.095–2.372 | 0.016 * |
| Educational background of mother | |||||
| Primary school or below | 24 | 72.7% | 1 (ref) | ||
| Secondary school | 529 | 66.2% | 0.542 | 0.204–1.443 | 0.344 |
| Post-secondary | 625 | 77.8% | 0.630 | 0.229–1.734 | 0.371 |
| Educational background of father | |||||
| Primary school or below | 29 | 74.4% | 1 (ref) | ||
| Secondary school | 507 | 66.2% | 0.474 | 0.191–1.179 | 0.108 |
| Post-secondary | 627 | 77.5% | 0.738 | 0.286–1.906 | 0.530 |
| Age group of mothers (at toddler’s birth) | |||||
| 24 or below | 54 | 68.4% | 1 (ref) | ||
| 25–34 | 735 | 71.7% | 0.968 | 0.494–1.897 | 0.925 |
| 35–39 | 307 | 72.7% | 0.972 | 0.461–2.051 | 0.941 |
| 40 or above | 71 | 72.4% | 1.015 | 0.417–2.473 | 0.973 |
| Age group of father (at toddler’s birth) | |||||
| 24 or below | 15 | 60.0% | 1 (ref) | ||
| 25–34 | 529 | 73.8% | 1.722 | 0.593–4.996 | 0.317 |
| 35–39 | 377 | 74.8% | 1.938 | 0.648–5.795 | 0.236 |
| 40 or above | 230 | 65.7% | 1.254 | 0.414–3.795 | 0.689 |
| Drinking during pregnancy (mother) | |||||
| No | 1134 | 72.0% | 1 (ref) | ||
| Yes | 33 | 68.8% | 0.695 | 0.334–1.445 | 0.330 |
| Smoking during pregnancy (mother) | |||||
| No | 1154 | 71.8% | 1 (ref) | ||
| Yes | 27 | 71.1% | 1.194 | 0.463–3.079 | 0.714 |
| Smoking during pregnancy (father) | |||||
| No | 895 | 72.6% | 1 (ref) | ||
| Yes | 277 | 70.5% | 1.493 | 1.076–2.073 | 0.016 * |
| Complications/health problems during pregnancy | |||||
| No | 884 | 71.1% | 1 (ref) | ||
| Yes | 302 | 73.7% | 1.079 | 0.803–1.451 | 0.614 |
| Hospitalization since birth (toddler) | |||||
| Never or 1 time only | 979 | 70.5% | 1 (ref) | ||
| 2 times or more | 279 | 74.0% | 1.440 | 1.041–1.990 | 0.027 * |
| Fully vaccinated | |||||
| No | 421 | 57.1% | 1 (ref) | ||
| Yes | 856 | 80.8% | 2.763 | 2.121–3.601 | <0.001 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, J.; Cheung, C.K.M.; Keung, V.M.W.; Lo, A.S.C.; Chan, S.C.; Pang, W.S.; Li, Q.H.Y.; Mui, L.W.H.; Lee, A.; Wong, M.C.S. Factors Associated with Vaccination Uptake among Young Children: A Follow-Up Study of 1799 Toddlers. Vaccines 2023, 11, 535. https://doi.org/10.3390/vaccines11030535
Huang J, Cheung CKM, Keung VMW, Lo ASC, Chan SC, Pang WS, Li QHY, Mui LWH, Lee A, Wong MCS. Factors Associated with Vaccination Uptake among Young Children: A Follow-Up Study of 1799 Toddlers. Vaccines. 2023; 11(3):535. https://doi.org/10.3390/vaccines11030535
Chicago/Turabian StyleHuang, Junjie, Calvin K. M. Cheung, Vera M. W. Keung, Amelia S. C. Lo, Sze Chai Chan, Wing Sze Pang, Queenie H. Y. Li, Lancelot W. H. Mui, Albert Lee, and Martin C. S. Wong. 2023. "Factors Associated with Vaccination Uptake among Young Children: A Follow-Up Study of 1799 Toddlers" Vaccines 11, no. 3: 535. https://doi.org/10.3390/vaccines11030535
APA StyleHuang, J., Cheung, C. K. M., Keung, V. M. W., Lo, A. S. C., Chan, S. C., Pang, W. S., Li, Q. H. Y., Mui, L. W. H., Lee, A., & Wong, M. C. S. (2023). Factors Associated with Vaccination Uptake among Young Children: A Follow-Up Study of 1799 Toddlers. Vaccines, 11(3), 535. https://doi.org/10.3390/vaccines11030535










