Age and Comorbidities as Risk Factors for Severe COVID-19 in Mexico, before, during and after Massive Vaccination
Abstract
:1. Introduction
2. Materials and Methods
2.1. Bibliographic Review of Risk Factors Reported before Vaccination
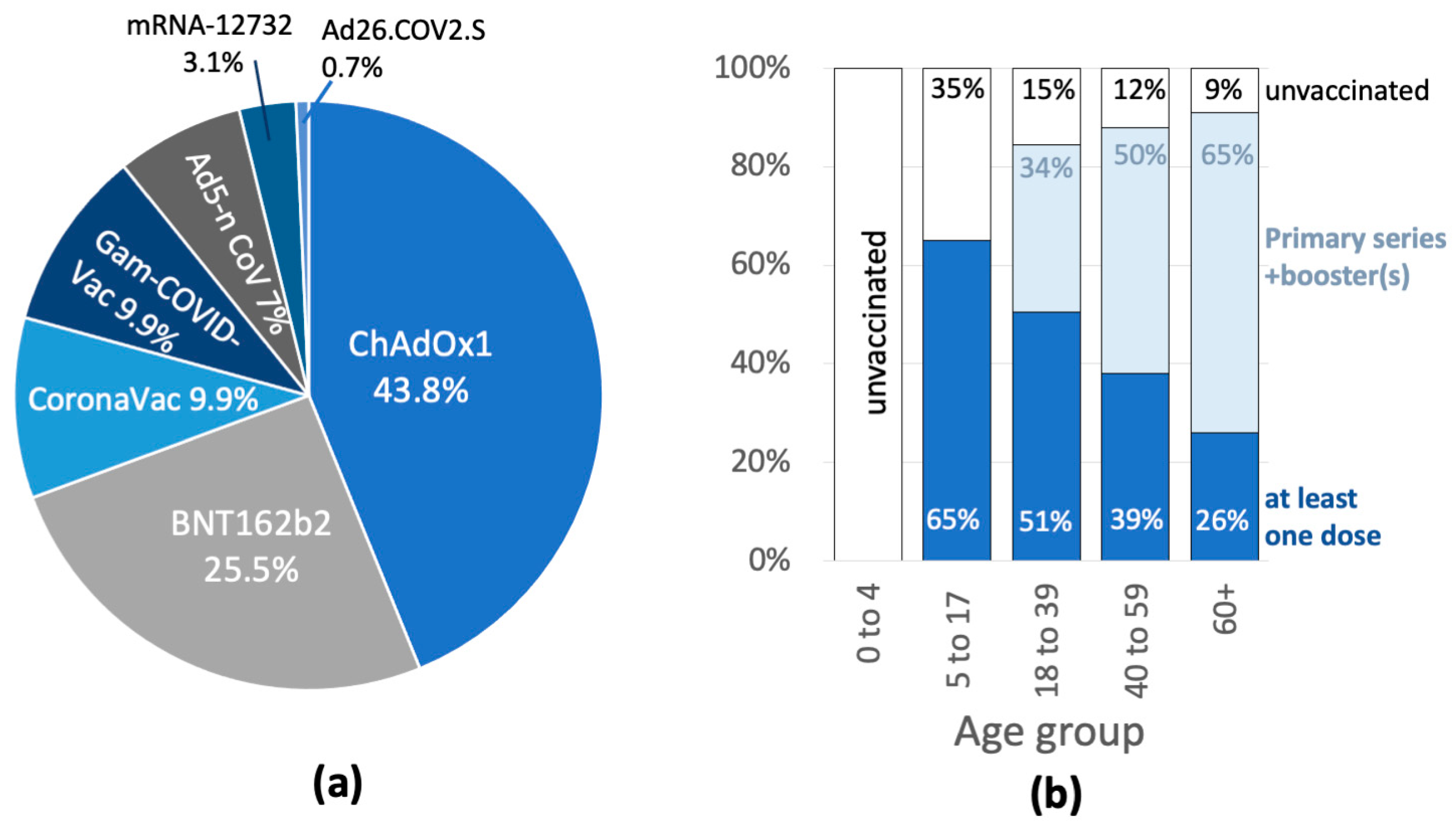
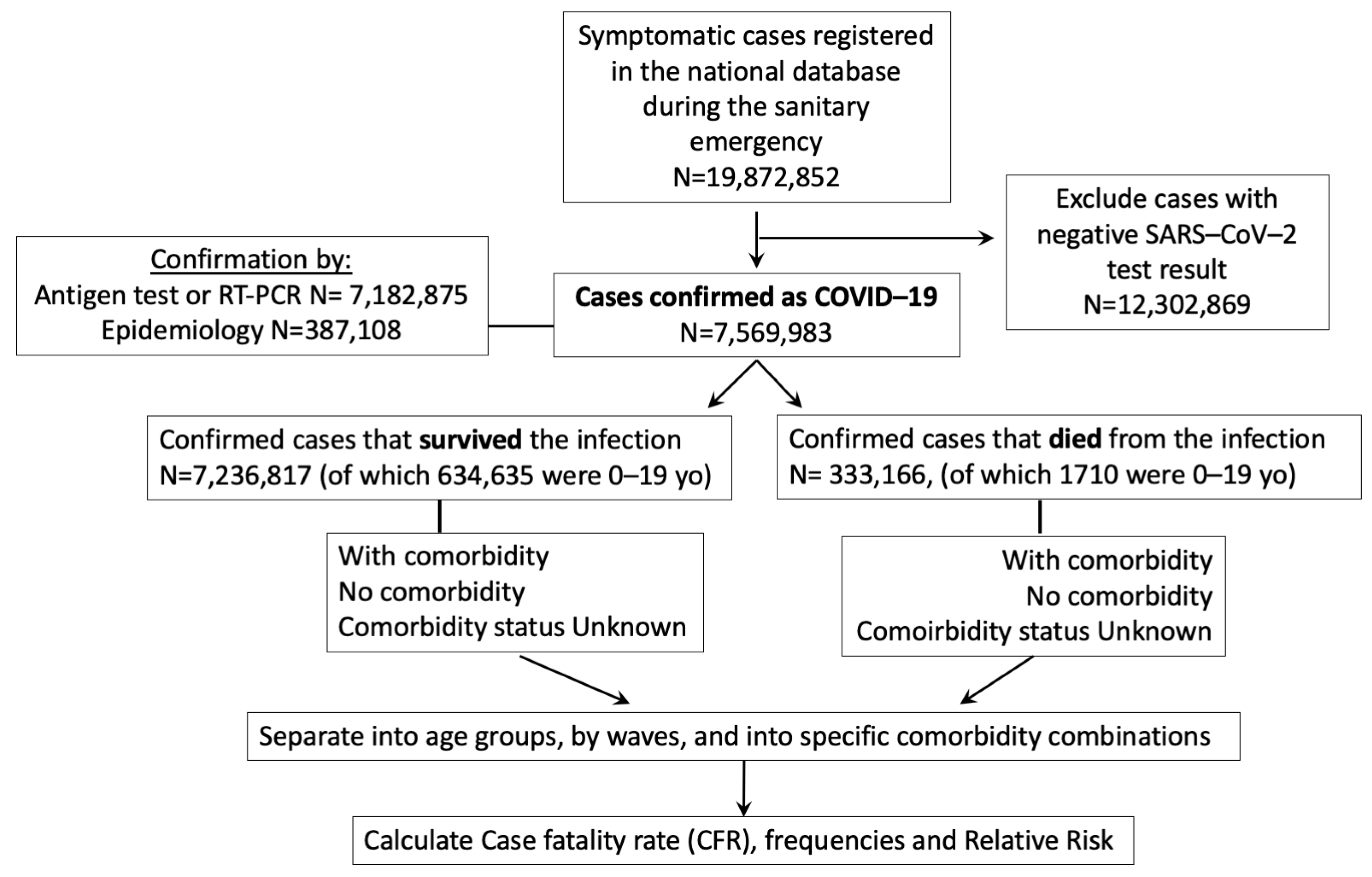
2.2. Analysis of the COVID-19 Sanitary Emergency in Mexico, from the National Dataset
3. Results
3.1. Factors Associated with Severe COVID-19, before Vaccination in Mexico, from the Published Literature
3.1.1. COVID-19 Hospitalization, Pneumonia, AMV and ICU
3.1.2. Factors Associated with COVID-19 Death
3.2. Risk of COVID-19 Death in Cases with Comorbidity by Age Group, before, during and after Vaccine Introduction
3.3. Gender Differences in COVID-19 Deaths, before and after Vaccination
3.4. Frequency and Age Distribution of COVID-19 Cases and Deaths with and without Comorbidity in Mexico, before and after Vaccine Introduction
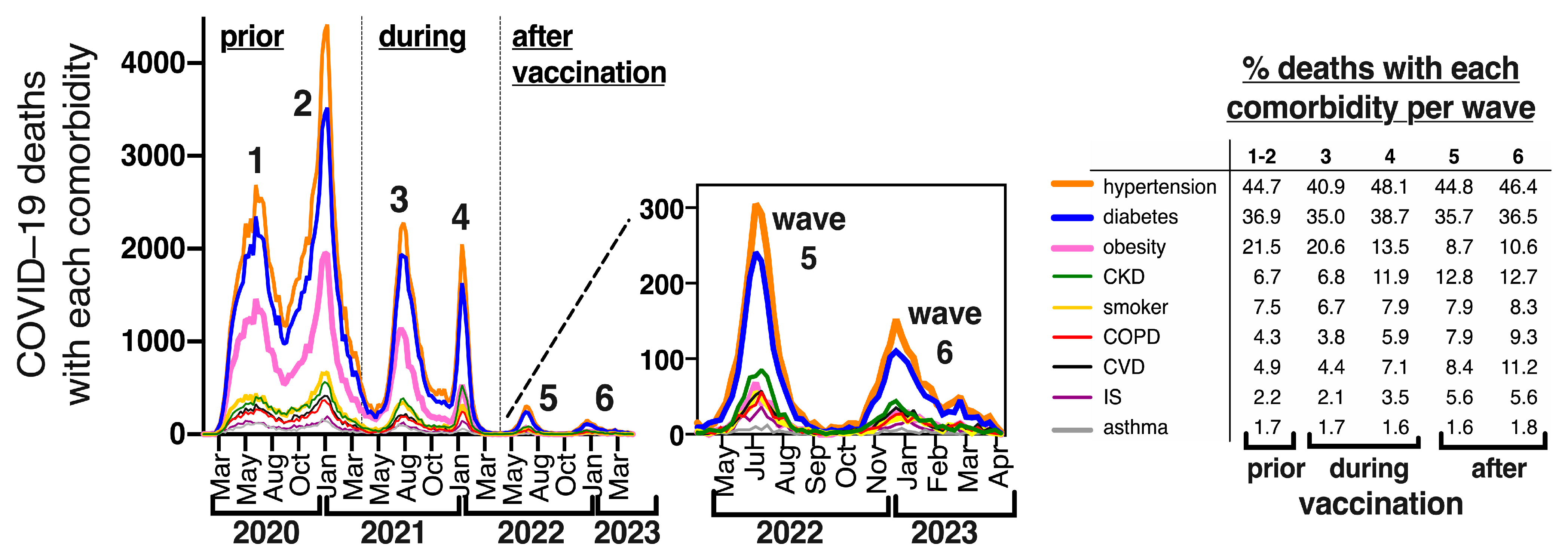
3.5. Frequency of Specific Comorbidities in COVID-19 Deaths in Mexico, before and after Vaccination
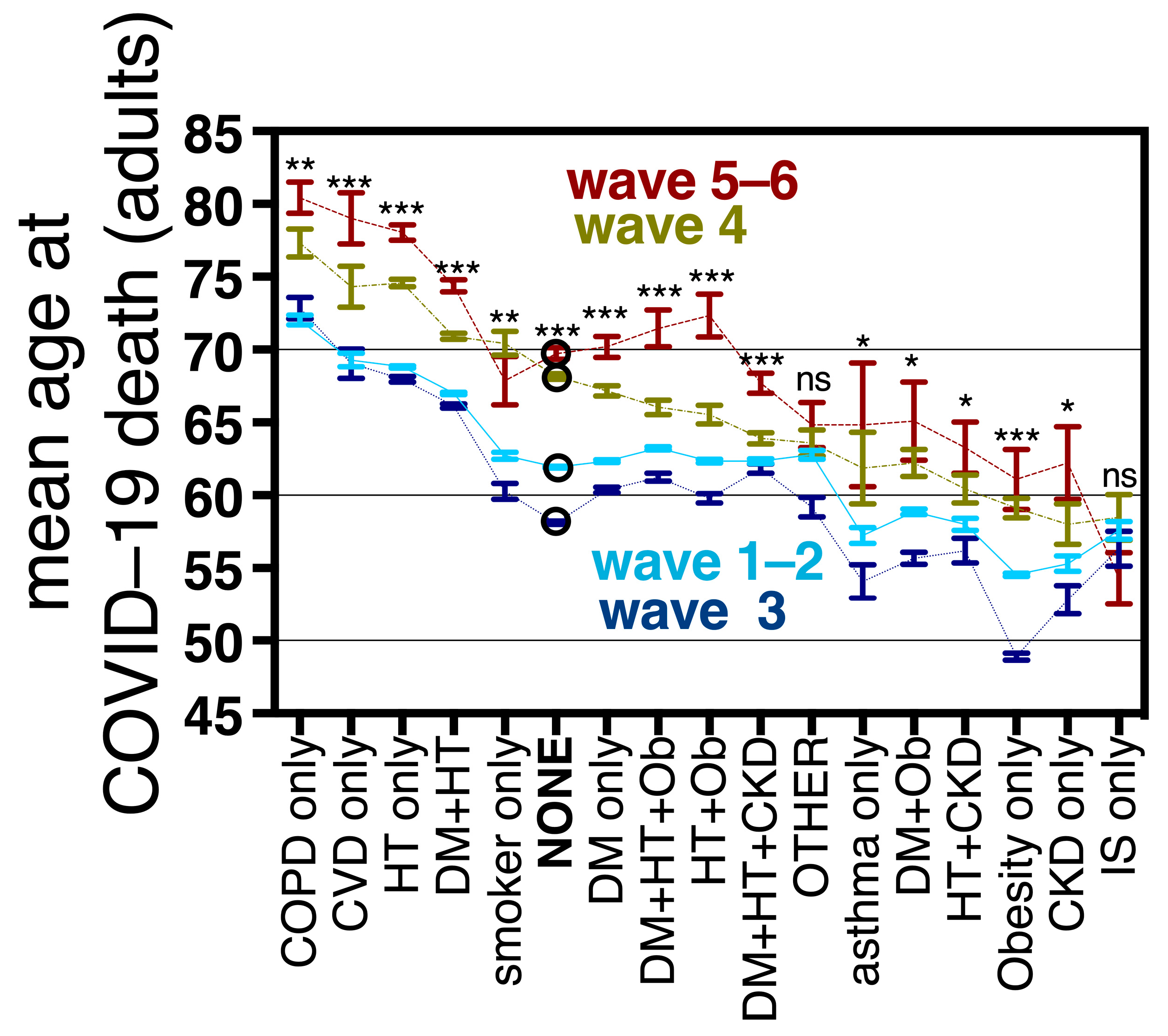
3.6. Mean Age at COVID-19 Death in Adults with and without Comorbidities
3.7. Relative Risk for COVID-19 Death in Adults, Derived from Specific Comorbidity Combinations, before, during and after Vaccination in Mexico
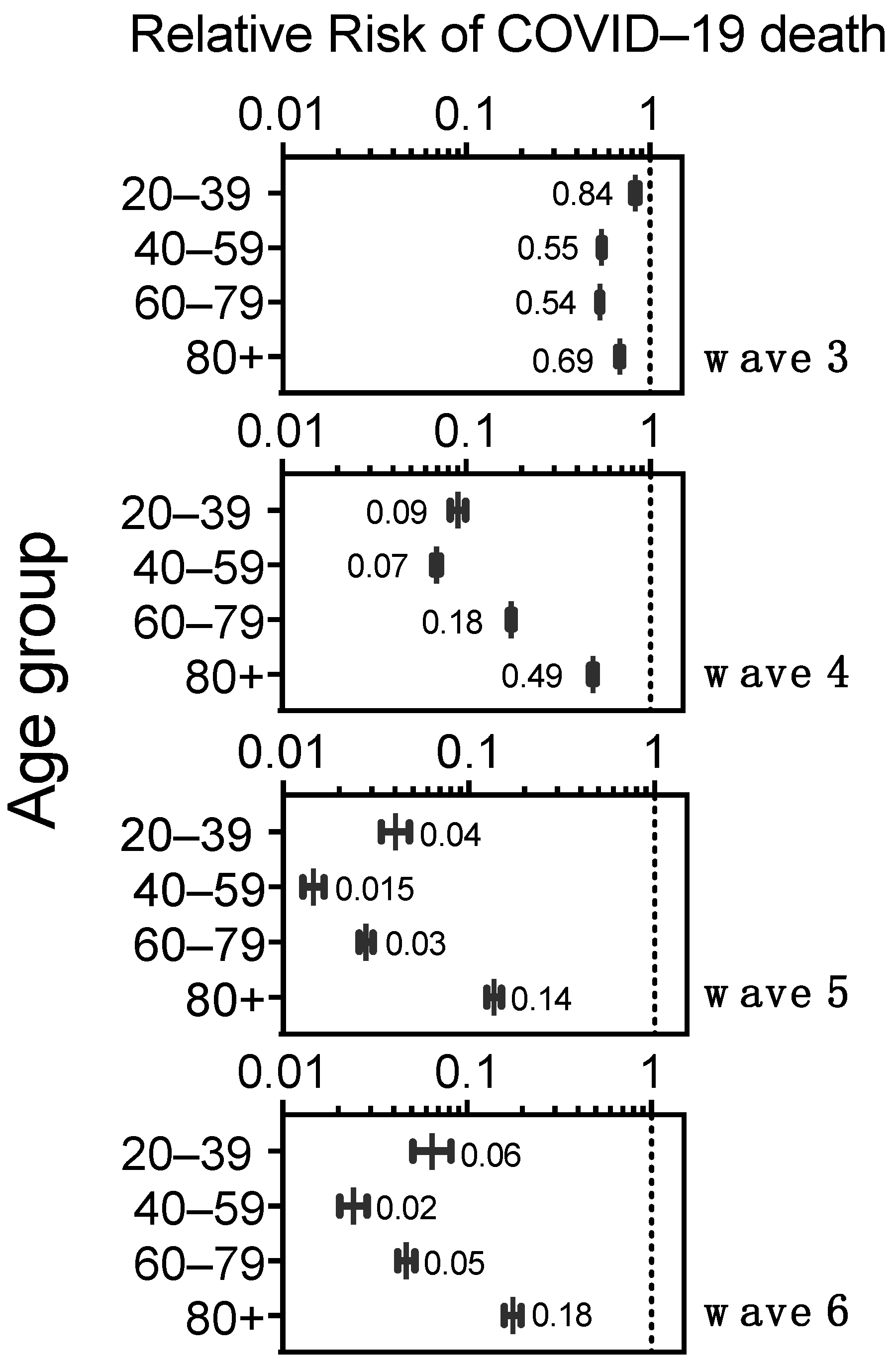
3.8. Risk of Death in COVID-19 Cases without Comorbidity by Age Group, before and after Vaccination in Mexico
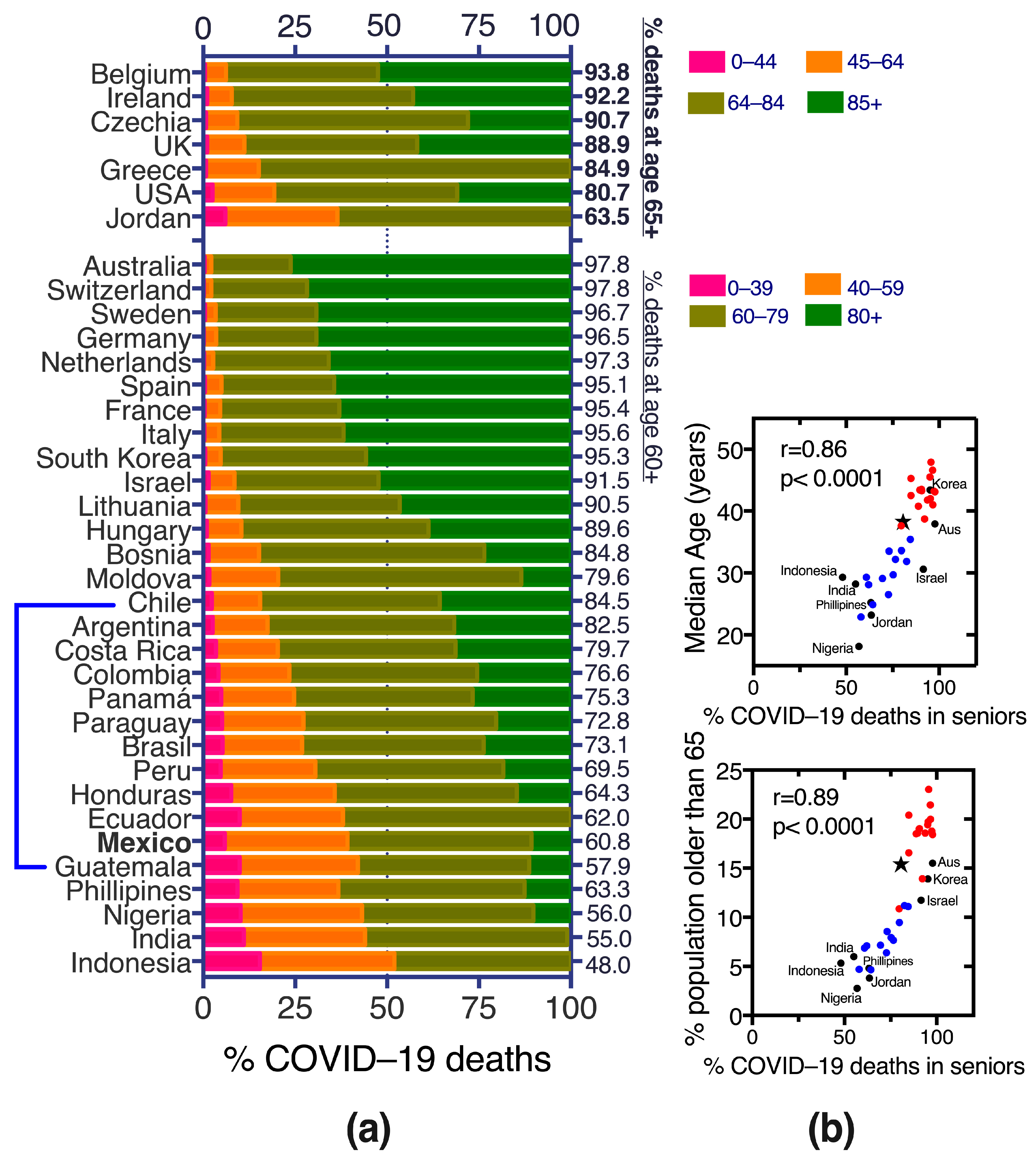
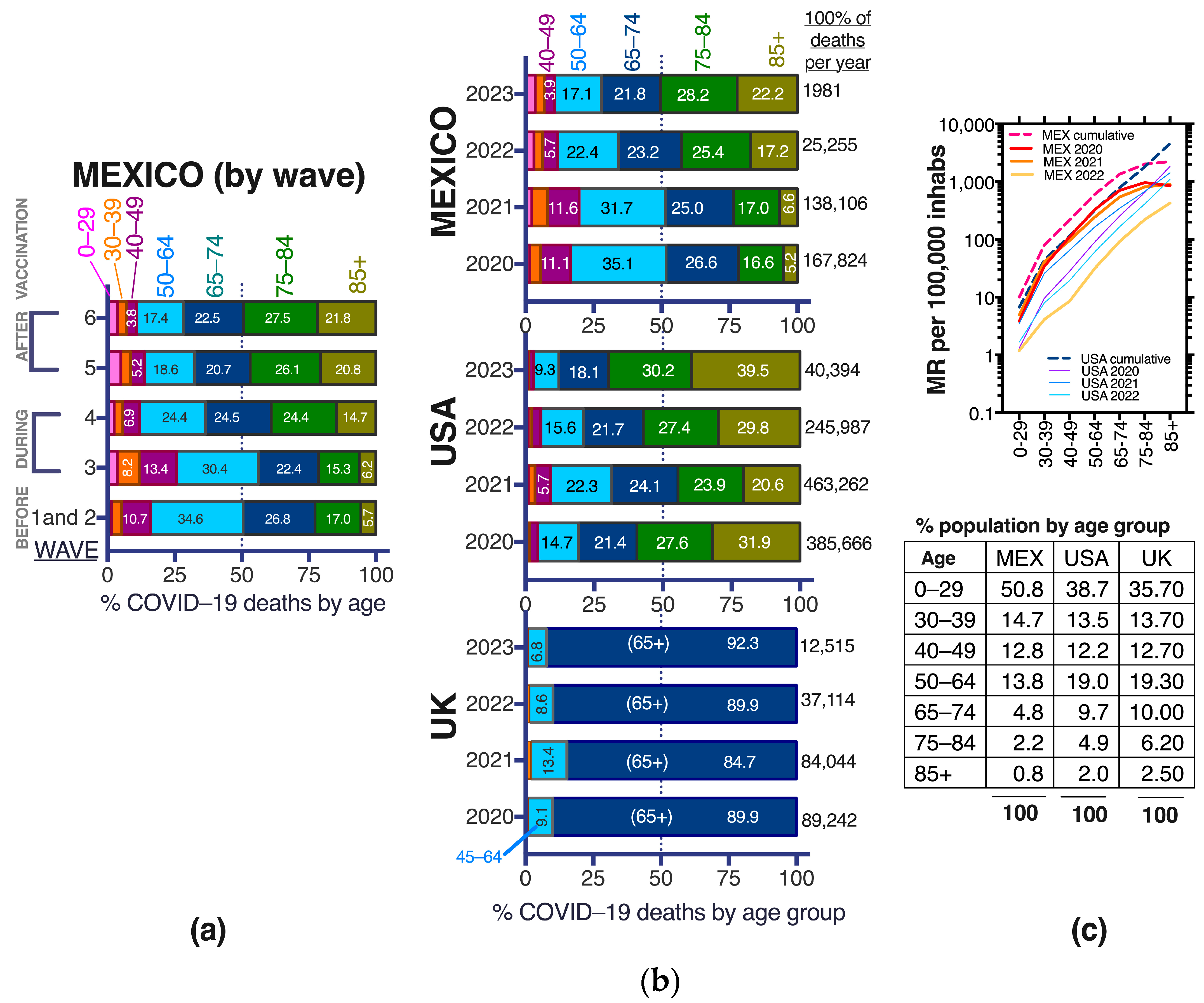
3.9. COVID-19 Deaths in the Middle-Aged in Mexico, before, during and after Vaccination
4. Discussion
- Mean ages at COVID-19 death increased with vaccination, both in sub-populations with and without comorbidities (Figure 7). This effect required that all adults accessed vaccination and was not present during wave 3 (produced by the Delta variant) when only the 60+ had accessed vaccines. In wave 3, the age of COVID-19 death actually decreased for most comorbidities, in particular obesity (Figure 7) and the proportion of young deaths grew, reaching its maximum in the epidemic (Figure 11a). This highlights the importance of vaccine access to all adults, even the youngest for epidemic control.
- Population access to vaccines/hybrid immunity protected all adult age groups from severe disease including the elderly (Figure 9). This protection was lower in the 80+ than for other adult groups but was maintained despite no new boosters applied in the year previous to this analysis. Lethality didn’t increase during the sixth wave (Figure 2c), despite a longer time since the last boosters, again suggesting that the protection from vaccines/hybrid immunity persisted through this wave.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| Ad5-nCoV | Cansino Biologics COVID-19 vaccine (against ancestral strains) |
| ALT | Alanine transaminase |
| AMV | Assisted mechanical ventilation |
| BA.2 | Omicron sub-lineage |
| BA.5 | Omicron sub-lineage |
| BMI | Body Mass Index |
| BNT162b2 | Pfizer Bio-NTech COVID-19 vaccine (against ancestral strains) |
| BQ.1 | Omicron sub-lineage |
| BW.1 | Omicron sub-lineage |
| CDC | Centers for Disease Control and Prevention, USA |
| CFR | Case fatality rate |
| ChAdOx1-S/nCoV-19 AZD1222 | University of Oxford/Astra Zeneca’s COVID-19 vaccine (against ancestral strains) |
| CI | Confidence interval |
| CIGB-66/Abdala | COVID-19 vaccine developed by Centro de Ingeniería Genética y Biotecnología del Ministerio de Salud Pública (Cuba) |
| CKD | Chronic kidney disease |
| COPD | Chronic obstructive pulmonary disease |
| COVID-19 | Coronavirus disease 2019 |
| CPK | Creatine phosphokinase |
| CVD | Cardiovascular disease |
| DM | Diabetes Mellitus |
| FiO2 | Fraction of inspired oxygen (from a gas mixture) |
| Gam-COVID-Vac/Sputnik | Gamaleya Research Institute’s COVID-19 vaccine (against ancestral strains) |
| HR | Hazard Ratio |
| HT | Systemic hypertension |
| ICU | Intensive care unit |
| IMSS | Instituto Mexicano del Seguro Social |
| IS | Immunosuppression |
| LDH | Lactate dehydrogenase |
| MR | Crude Mortality rate |
| mRNA | Messenger RNA |
| Ob | Obesity |
| OECD | Organization for the Economic Cooperation and Development |
| OR | Odd Ratio |
| RR | Relative risk |
| RT-PCR | Reverse transcription-polymerase chain reaction test |
| SARS-CoV-2 | Severe Acute Respiratory Syndrome Coronavirus 2 |
| SpO2 | Oxygen saturation |
| XBB.1 | Omicron sub-lineage |
| yo | Years old |
Appendix A


References
- Carnalla, M.; Basto-Abreu, A.; Stern, D.; Colchero, M.A.; Bautista-Arredondo, S.; Alpuche-Aranda, C.M.; Martínez-Barnetche, J.; Romero-Martínez, M.; Cortés-Alcalá, R.; López-Martínez, I.; et al. Prevalencia de Anticuerpos y Vacunación Contra SARS-CoV-2 En 2022 En México. Salud Pública México 2023, 65, s135–s145. [Google Scholar] [CrossRef]
- Bello-Chavolla, O.Y.; Antonio-Villa, N.E.; Valdés-Ferrer, S.I.; Fermín-Martínez, C.A.; Fernández-Chirino, L.; Vargas-Vázquez, A.; Ramírez-García, D.; Mancilla-Galindo, J.; Kammar-García, A.; Ávila-Funes, J.A.; et al. Effectiveness of a Nationwide COVID-19 Vaccination Program in Mexico against Symptomatic COVID-19, Hospitalizations, and Death: A Retrospective Analysis of National Surveillance Data. Int. J. Infect. Dis. 2023, 129, 188–196. [Google Scholar] [CrossRef]
- Domínguez-Ramírez, L.; Solis-Tejeda, I.; Ayon-Aguilar, J.; Mayoral-Ortiz, A.; Sosa-Jurado, F.; Pelayo, R.; Santos-López, G.; Cortes-Hernandez, P. Decrease in COVID-19 Adverse Outcomes in Adults during the Delta and Omicron SARS-CoV-2 Waves, after Vaccination in Mexico. Front. Public Health 2022, 10, 1010256. [Google Scholar] [CrossRef]
- Genómica, C.M.d.V. CoViGen-Mex. Available online: http://mexcov2.ibt.unam.mx:8080/COVID-TRACKER/ (accessed on 6 June 2023).
- Population Pyramids of the World from 1950 to 2100. Database: Population Pyramid. Available online: https://www.populationpyramid.net/mexico/2020/ (accessed on 10 September 2023).
- Campos-Nonato, I.; Galván-Valencia, Ó.; Hernández-Barrera, L.; Oviedo-Solís, C.; Barquera, S. Prevalencia de Obesidad y Factores de Riesgo Asociados En Adultos Mexicanos: Resultados de La Ensanut 2022. Salud Pública México 2023, 65, s238–s247. [Google Scholar] [CrossRef]
- Datos Abiertos–Dirección General de Epidemiología | Secretaría de Salud. Available online: https://www.gob.mx/salud/documentos/datos-abiertos-152127?idiom=es (accessed on 10 September 2023).
- Denova-Gutiérrez, E.; Lopez-Gatell, H.; Alomia-Zegarra, J.L.; López-Ridaura, R.; Zaragoza-Jimenez, C.A.; Dyer-Leal, D.D.; Cortés-Alcala, R.; Villa-Reyes, T.; Gutiérrez-Vargas, R.; Rodríguez-González, K.; et al. The Association of Obesity, Type 2 Diabetes, and Hypertension with Severe Coronavirus Disease 2019 on Admission among Mexican Patients. Obesity 2020, 28, 1826–1832. [Google Scholar] [CrossRef]
- Li, G.; Liu, Y.; Jing, X.; Wang, Y.; Miao, M.; Tao, L.; Zhou, Z.; Xie, Y.; Huang, Y.; Lei, J.; et al. Mortality Risk of COVID-19 in Elderly Males with Comorbidities: A Multi-Country Study. Aging 2020, 13, 27–60. [Google Scholar] [CrossRef]
- Soto-Mota, A.; Marfil-Garza, B.A.; Rodríguez, E.M.; Rodríguez, J.O.B.; Romo, A.E.L.; Minutti, P.A.; Loya, J.V.A.; Talavera, F.E.P.; Cervera, F.J.Á.; Burciaga, A.V.; et al. The Low-Harm Score for Predicting Mortality in Patients Diagnosed with COVID-19: A Multicentric Validation Study. J. Am. Coll. Emerg. Physicians Open 2020, 1, 1436–1443. [Google Scholar] [CrossRef]
- Mejía-Vilet, J.M.; Córdova-Sánchez, B.M.; Fernández-Camargo, D.A.; Méndez-Pérez, R.A.; Morales-Buenrostro, L.E.; Hernández-Gilsoul, T. A Risk Score to Predict Admission to the Intensive Care Unit in Patients with COVID-19: The ABC-GOALS Score. Salud Pública México 2020, 63, 1–11. [Google Scholar] [CrossRef]
- Mancilla-Galindo, J.; Vera-Zertuche, J.M.; Navarro-Cruz, A.R.; Segura-Badilla, O.; Reyes-Velázquez, G.; Tepepa-López, F.J.; Aguilar-Alonso, P.; Vidal-Mayo, J.d.J.; Kammar-García, A. Development and Validation of the Patient History COVID-19 (PH-Covid19) Scoring System: A Multivariable Prediction Model of Death in Mexican Patients with COVID-19. Epidemiol. Infect. 2020, 148, e286. [Google Scholar] [CrossRef]
- Carrillo-Vega, M.F.; Salinas-Escudero, G.; García-Peña, C.; Gutiérrez-Robledo, L.M.; Parra-Rodríguez, L. Early Estimation of the Risk Factors for Hospitalization and Mortality by COVID-19 in Mexico. PLoS ONE 2020, 15, e0238905. [Google Scholar] [CrossRef]
- Kammar-García, A.; Vidal-Mayo, J.d.J.; Vera-Zertuche, J.M.; Hernández, M.L.-; Vera-López, O.; Segura-Badilla, O.; Aguilar-Alonso, P.; Navarro-Cruz, A.R. Impact of Comorbidities in Mexican SARS-CoV-2-Positive Patients: A Retrospective Analysis in a National Cohort. Rev. Investig. Clin. 2020, 72, 151–158. [Google Scholar] [CrossRef] [PubMed]
- Vera-Zertuche, J.M.; Mancilla-Galindo, J.; Tlalpa-Prisco, M.; Aguilar-Alonso, P.; Aguirre-García, M.M.; Segura-Badilla, O.; Lazcano-Hernández, M.; Rocha-González, H.I.; Navarro-Cruz, A.R.; Kammar-García, A.; et al. Obesity Is a Strong Risk Factor for Short-Term Mortality and Adverse Outcomes in Mexican Patients with COVID-19: A National Observational Study. Epidemiol. Infect. 2021, 149, e109. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Galdamez, D.R.; González-Block, M.Á.; Romo-Dueñas, D.K.; Lima-Morales, R.; Hernández-Vicente, I.A.; Lumbreras-Guzmán, M.; Méndez-Hernández, P. Increased Risk of Hospitalization and Death in Patients with COVID-19 and Pre-Existing Noncommunicable Diseases and Modifiable Risk Factors in Mexico. Arch. Méd. Res. 2020, 51, 683–689. [Google Scholar] [CrossRef] [PubMed]
- Bello-Chavolla, O.Y.; Bahena-López, J.P.; Antonio-Villa, N.E.; Vargas-Vázquez, A.; González-Díaz, A.; Márquez-Salinas, A.; Fermín-Martínez, C.A.; Naveja, J.J.; Aguilar-Salinas, C.A. Predicting Mortality Due to SARS-CoV-2: A Mechanistic Score Relating Obesity and Diabetes to COVID-19 Outcomes in Mexico. J. Clin. Endocrinol. Metab. 2020, 105, dgaa346. [Google Scholar] [CrossRef]
- Parra-Bracamonte, G.M.; Lopez-Villalobos, N.; Parra-Bracamonte, F.E. Clinical Characteristics and Risk Factors for Mortality of Patients with COVID-19 in a Large Data Set from Mexico. Ann. Epidemiol. 2020, 52, 93–98. [Google Scholar] [CrossRef]
- Murillo-Zamora, E.; Hernandez-Suarez, C.M. Survival in Adult Inpatients with COVID-19. Public Health 2021, 190, 1–3. [Google Scholar] [CrossRef]
- Hernández-Vásquez, A.; Azañedo, D.; Vargas-Fernández, R.; Bendezu-Quispe, G. Association of Comorbidities With Pneumonia and Death among COVID-19 Patients in Mexico: A Nationwide Cross-Sectional Study. J. Prev. Med. Public Health 2020, 53, 211–219. [Google Scholar] [CrossRef]
- Dominguez-Ramirez, L.; Rodriguez-Perez, F.; Sosa-Jurado, F.; Santos-Lopez, G.; Cortes-Hernandez, P. The Role of Metabolic Comorbidity in COVID-19 Mortality of Middle-Aged Adults. The Case of Mexico. medRxiv 2020. [Google Scholar] [CrossRef]
- Rivas-Ruiz, R.; Roy-Garcia, I.A.; Ureña-Wong, K.; Aguilar-Ituarte, F.; Anda, G.F.V.-D.; Gutiérrez-Castrellón, P.; Mancilla-Ramírez, J.; Moreno-Espinosa, S. Factors Associated with Death in Children with COVID-19 in Mexico. Gac. Médica México 2020, 156, 516–522. [Google Scholar] [CrossRef]
- Vidal-Cevallos, P.; Higuera-De-La-Tijera, F.; Chávez-Tapia, N.C.; Sanchez-Giron, F.; Cerda-Reyes, E.; Rosales-Salyano, V.H.; Servin-Caamaño, A.; Vázquez-Medina, M.U.; Méndez-Sánchez, N. Lactate-Dehydrogenase Associated with Mortality in Hospitalized Patients with COVID-19 in Mexico: A Multi-Centre Retrospective Cohort Study. Ann. Hepatol. 2021, 24, 100338. [Google Scholar] [CrossRef]
- Rizo-Téllez, S.A.; Méndez-García, L.A.; Rivera-Rugeles, A.C.; Miranda-García, M.; Manjarrez-Reyna, A.N.; Viurcos-Sanabria, R.; Solleiro-Villavicencio, H.; Becerril-Villanueva, E.; Carrillo-Ruíz, J.D.; Cota-Arce, J.M.; et al. The Combined Use of Cytokine Serum Values with Laboratory Parameters Improves Mortality Prediction of COVID-19 Patients: The Interleukin-15-to-Albumin Ratio. Microorganisms 2021, 9, 2159. [Google Scholar] [CrossRef] [PubMed]
- Salinas-Escudero, G.; Carrillo-Vega, M.F.; Granados-García, V.; Martínez-Valverde, S.; Toledano-Toledano, F.; Garduño-Espinosa, J. A Survival Analysis of COVID-19 in the Mexican Population. BMC Public Health 2020, 20, 1616. [Google Scholar] [CrossRef]
- Suárez, V.; Quezada, M.S.; Ruiz, S.O.; Jesús, E.R.D. Epidemiology of COVID-19 in Mexico: From the 27th of February to the 30th of April 2020. Rev. Clin. Esp. 2020, 220, 463–471. [Google Scholar] [CrossRef] [PubMed]
- Galván-Tejada, C.E.; Zanella-Calzada, L.A.; Villagrana-Bañuelos, K.E.; Moreno-Báez, A.; Luna-García, H.; Celaya-Padilla, J.M.; Galván-Tejada, J.I.; Gamboa-Rosales, H. Demographic and Comorbidities Data Description of Population in Mexico with SARS-CoV-2 Infected Patients(COVID19): An Online Tool Analysis. Int. J. Environ. Res. Public Health 2020, 17, 5173. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Garduño, E. Obesity Is the Comorbidity More Strongly Associated for COVID-19 in Mexico. A Case-Control Study. Obes. Res. Clin. Pract. 2020, 14, 375–379. [Google Scholar] [CrossRef]
- Albarrán-Sánchez, A.; Ramírez-Rentería, C.; Anda-Garay, J.C.; Noyola-García, M.E.; Alberti-Minutti, P.; Flores-Padilla, G.; Guizar-García, L.A.; Contreras-García, C.E.; Marrero-Rodríguez, D.; Taniguchi-Ponciano, K.; et al. Differences in Mortality Rate among Patients Hospitalized with Severe COVID-19 According to Their Body Mass Index. Obes. Res. Clin. Pract. 2022, 8, 423–432. [Google Scholar] [CrossRef]
- Murillo-Zamora, E.; Trujillo, X.; Huerta, M.; Ríos-Silva, M.; Mendoza-Cano, O. Male Gender and Kidney Illness Are Associated with an Increased Risk of Severe Laboratory-Confirmed Coronavirus Disease. BMC Infect. Dis. 2020, 20, 674. [Google Scholar] [CrossRef]
- Martín-del-Campo, F.; Ruvalcaba-Contreras, N.; Velázquez-Vidaurri, A.L.; Cueto-Manzano, A.M.; Rojas-Campos, E.; Cortés-Sanabria, L.; Espinel-Bermúdez, M.C.; Hernández-González, S.O.; Nava-Zavala, A.H.; Fuentes-Orozco, C.; et al. Morbid Obesity Is Associated with Mortality and Acute Kidney Injury in Hospitalized Patients with COVID-19. Clin. Nutr. ESPEN 2021, 45, 200–205. [Google Scholar] [CrossRef]
- Lawrence, J.M.; Divers, J.; Isom, S.; Saydah, S.; Imperatore, G.; Pihoker, C.; Marcovina, S.M.; Mayer-Davis, E.J.; Hamman, R.F.; Dolan, L.; et al. Trends in Prevalence of Type 1 and Type 2 Diabetes in Children and Adolescents in the US, 2001–2017. JAMA 2021, 326, 717–727. [Google Scholar] [CrossRef]
- Comunicacion, S. Características de las Defunciones Registradas en México Durante 2021; Comunicado de Prensa; INEGI: Mexico city, México, 2023; p. 90. [Google Scholar]
- Analystics & Visualization Taks Force and CDC CPR DEO Situational Awareness Public Healt Science Team. Available online: https://covid.cdc.gov/covid-data-tracker/#demographicsovertime (accessed on 4 October 2023).
- OECD.Stat. Available online: https://stats.oecd.org/Index.aspx?QueryId=104975# (accessed on 24 October 2023).
- Mathieu, E.; Ritchie, H.; Rodés-Guirao, L.; Appel, C.; Giattino, C.; Hasell, J.; Macdonald, B.; Dattani, S.; Beltekian, D.; Roser, E.O.-O.; et al. Coronavirus Pandemic (COVID-19). Available online: https://ourworldindata.org/covid-vaccinations (accessed on 24 October 2023).
- Centers for Disease Control and Prevention. COVID Data Tracker. Available online: https://covid.cdc.gov/covid-data-tracker/#vaccinations_vacc-people-booster-percent-pop5 (accessed on 24 October 2023).
- Montes-González, J.A.; Zaragoza-Jiménez, C.A.; Antonio-Villa, N.E.; Fermín-Martínez, C.A.; Ramírez-García, D.; Vargas-Vázquez, A.; Gutiérrez-Vargas, R.I.; García-Rodríguez, G.; López-Gatell, H.; Valdés-Ferrer, S.I.; et al. Protection of Hybrid Immunity against SARS-CoV-2 Reinfection and Severe COVID-19 during Periods of Omicron Variant Predominance in Mexico. Front. Public Health 2023, 11, 1146059. [Google Scholar] [CrossRef]
- Gobierno de México. Exceso de Mortalidad En México. Available online: https://coronavirus.gob.mx/exceso-de-mortalidad-en-mexico/ (accessed on 5 October 2023).
- Romo-Rodríguez, R.; Anda, K.G.; López-Blanco, J.A.; Zamora-Herrera, G.; Cortés-Hernández, P.; Santos-López, G.; Márquez-Domínguez, L.; Vilchis-Ordoñez, A.; Ramírez-Ramírez, D.; Balandrán, J.C.; et al. Chronic Comorbidities in Middle Aged Patients Contribute to Ineffective Emergency Hematopoiesis in COVID-19 Fatal Outcomes. Arch. Med. Res. 2023, 54, 197–210. [Google Scholar] [CrossRef] [PubMed]
- Fuentes, E.; Fuentes, M.; Alarcón, M.; Palomo, I. Immune System Dysfunction in the Elderly. An. Acad. Bras. Ciências 2017, 89, 285–299. [Google Scholar] [CrossRef] [PubMed]
- Pera, A.; Campos, C.; López, N.; Hassouneh, F.; Alonso, C.; Tarazona, R.; Solana, R. Immunosenescence: Implications for Response to Infection and Vaccination in Older People. Maturitas 2015, 82, 50–55. [Google Scholar] [CrossRef] [PubMed]
- Weng, N.; Pawelec, G. Validation of the Effectiveness of SARS-CoV-2 Vaccines in Older Adults in “Real-World” Settings. Immun. Ageing 2021, 18, 36. [Google Scholar] [CrossRef]
- Ottone, M.; Bartolini, L.; Bonvicini, L.; Rossi, P.G.; Paolo Giorgi Rossi Reggio Emilia COVID-19 working group; Costantini, M.; Grilli, R.; Marino, M.; Formoso, G.; Formisano, D.; et al. The Effect of Diabetes on COVID-19 Incidence and Mortality: Differences between Highly-Developed-Country and High-Migratory-Pressure-Country Populations. Front. Public Health 2023, 11, 969143. [Google Scholar] [CrossRef]
- Shestakova, M.V.; Vikulova, O.K.; Elfimova, A.R.; Deviatkin, A.A.; Dedov, I.I.; Mokrysheva, N.G. Risk Factors for COVID-19 Case Fatality Rate in People with Type 1 and Type 2 Diabetes Mellitus: A Nationwide Retrospective Cohort Study of 235,248 Patients in the Russian Federation. Front. Endocrinol. 2022, 13, 909874. [Google Scholar] [CrossRef]
- Singh, A.K.; Khunti, K. COVID-19 and Diabetes. Annu. Rev. Med. 2021, 73, 129–147. [Google Scholar] [CrossRef]
- Shahid, Z.; Kalayanamitra, R.; McClafferty, B.; Kepko, D.; Ramgobin, D.; Patel, R.; Aggarwal, C.S.; Vunnam, R.; Sahu, N.; Bhatt, D.; et al. COVID-19 and Older Adults: What We Know. J. Am. Geriatr. Soc. 2020, 68, 926–929. [Google Scholar] [CrossRef]





| Risk Factor for Hospitalization | Odds Ratio (95% CI) | Reference |
|---|---|---|
| Detected pneumonia | 33 (29–38) | [13] |
| CKD + DM | 6.6 (2.4–18.3) | [14] |
| CKD + HT | 4.3 (2.0–9.3) | [14] |
| Age ≥ 75 | 3.8 (2.9–5.1) | [13] |
| IS + Ob | 4.2 (1.8–9.8) | [15] |
| 3.7 (1.6–8.8) | ||
| CKD | 3.5 (2.6–4.6) | [14] |
| 2.4 (1.4–4.3) | [13,15,16] | |
| IS | 2.9 (1.9–4.6) | [15] |
| 2.4 (1.9–3.2) | [16] | |
| Age ≥ 65 | 2.8 (2.7–2.9) | [17] |
| DM + Ob | 2.7 (2.1–3.5) | [14,15] |
| 1.7 (1.2–2.6) | [13] | |
| DM | 2.6 (2.2–3.0) | [14,15] |
| 2.0 (1.9–2.01) | [13,16,17] | |
| DM + HT | 2.5 (2.0–3.0) | [13,14] |
| Ob + COPD | 2.5 (1.1–6.2) | [14] |
| Age ≥ 50–74 | 2.0 (1.8–2.3) | [13] |
| DM and age < 40 | 2.0 (1.8–2.2) | [17] |
| Ob + HT | 1.9 (1.5–2.3) | [13,14,15] |
| Ob | 1.9 (1.7–2.1) | [15] |
| 1.6 (1.3–1.9) | [13,14] | |
| 1.4 (1.2–1.6) | [16,17] | |
| COPD | 1.9 (1.5–2.4) | [14] |
| 1.7 (1.2–2.5) | [13,17] | |
| DM + HT+ Ob | 1.8 (1.3–2.5) | [13] |
| Male | 1.7 (1.5–1.8) | [17] |
| 1.5 (1.4–1.7) | [13] | |
| HT | 1.5 (1.3–1.9) | [13,14] |
| 1.3 (1.2–1.6) | [15,16] |
| Risk Factor for COVID-19 Death | OR (95% CI) | Reference |
|---|---|---|
| Age > 80 | 12.5 (10–15) | [18] |
| AMV | 8.7 (3.2–24) | [13] |
| Age 61–79 | 7.7 (6.6–9.2) | [18] |
| 3.7 (2.8–4.9) | [13] | |
| Hospitalization | 7.1 (6.8–7.6) | [18] |
| 5.0 (3.8–6.5) | [13] | |
| Age 41–60 | 3.7 (2.9–4.6) | [18] |
| 1.9 (1.6–2.3) | [13] | |
| Pregnancy | 3.5 (1.1–10) | [13] |
| Detected pneumonia | 3.4 (3.2–3.5) | [18] |
| 2.5 (2.1–3.1) | [13] | |
| 6.4 (2–20) ped | [22] | |
| DM + HT + Ob | 2.1 (1.5–2.9) | [13] |
| DM + Ob | 2.0 (1.4–3.1) | [13] |
| CKD | 1.8 (1.2–1.3) | [18] |
| 1.4 (1.1–2.1) | [13] | |
| IS HR | 1.8 (1.6–2.0) | [18] |
| 1.1 (1.0–1.16) | [19] | |
| Ob + HT | 1.8 (1.3–2.6) | [13] |
| Ob | 1.7 (1.4–2.2) | [13] |
| 1.3 (1.15–1.4) | [18] | |
| DM | 1.5 (1.13–1.98) | [13,18] |
| HT | 1.5 (1.15–1.92) | [13,18] |
| Male | 1.5 (1.3–1.8) | [13,18] |
| COPD HR | 1.4 (1.3–1.5) | [17] |
| 1.12 (1.07–1.18) | [19] |
| Before Vaccination Wave 1–2 | During Vaccination Wave 3 | During Vaccination Wave 4 | After Vaccination Wave 5–6 | Entire Emergency | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | Comorbidity | % CFR | OR (95% CI) | % CFR | OR (95% CI) | % CFR | OR (95% CI) | % CFR | OR (95% CI) | % CFR | OR (95% CI) |
| 20–39 | yes | 2.94 | 4.59 (4.42–4.77) * | 2.82 | 5.27 (5.02–5.52) * | 0.50 | 8.4 (7.45–9.47) * | 0.17 | 5.65 (4.65–6.87) * | 1.87 | 6.06 (5.89–6.23) * |
| no | 0.66 | 0.55 | 0.06 | 0.03 | 0.31 | ||||||
| 40–59 | yes | 12.50 | 2.79 (2.75–2.83) * | 9.19 | 3.68 (3.58–3.79) * | 2.03 | 6.14 (5.78–6.52) * | 0.42 | 5.08 (4.47–5.76) * | 7.51 | 3.92 (3.86–3.97) * |
| no | 4.87 | 2.67 | 0.34 | 0.08 | 2.03 | ||||||
| 60–79 | yes | 34.75 | 1.73 (1.71–1.76) * | 24.75 | 2.28 (2.22–2.35) * | 12.11 | 3.20 (3.06–3.34) * | 2.72 | 3.52 (3.25–3.81) * | 24.04 | 2.44 (2.41–2.47) * |
| no | 23.52 | 12.59 | 4.13 | 0.79 | 11.50 | ||||||
| 80+ | yes | 51.13 | 1.38 (1.34–1.43) * | 40.48 | 1.62 (1.53–1.72) * | 31.79 | 1.75 (1.64–1.86) * | 11.32 | 1.83 (1.68–2.00) * | 38.85 | 1.70 (1.66–1.75) * |
| no | 43.06 | 29.58 | 21.08 | 6.51 | 27.17 | ||||||
| All adults | yes | 17.82 | 4.07 (4.03–4.11) * | 11.48 | 5.84 (5.74–5.94) * | 4.40 | 8.44 (8.21–8.68) * | 1.30 | 7.33 (6.97–7.71) * | 11.01 | 5.94 (5.89–5.98) * |
| no | 5.06 | 2.17 | 0.54 | 0.18 | 2.04 | ||||||
| All conditions | 10.31 | - | 4.79 | - | 1.45 | - | 0.46 | - | 4.78 | - | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Domínguez-Ramírez, L.; Sosa-Jurado, F.; Díaz-Sampayo, G.; Solis-Tejeda, I.; Rodríguez-Pérez, F.; Pelayo, R.; Santos-López, G.; Cortes-Hernandez, P. Age and Comorbidities as Risk Factors for Severe COVID-19 in Mexico, before, during and after Massive Vaccination. Vaccines 2023, 11, 1676. https://doi.org/10.3390/vaccines11111676
Domínguez-Ramírez L, Sosa-Jurado F, Díaz-Sampayo G, Solis-Tejeda I, Rodríguez-Pérez F, Pelayo R, Santos-López G, Cortes-Hernandez P. Age and Comorbidities as Risk Factors for Severe COVID-19 in Mexico, before, during and after Massive Vaccination. Vaccines. 2023; 11(11):1676. https://doi.org/10.3390/vaccines11111676
Chicago/Turabian StyleDomínguez-Ramírez, Lenin, Francisca Sosa-Jurado, Guadalupe Díaz-Sampayo, Itzel Solis-Tejeda, Francisco Rodríguez-Pérez, Rosana Pelayo, Gerardo Santos-López, and Paulina Cortes-Hernandez. 2023. "Age and Comorbidities as Risk Factors for Severe COVID-19 in Mexico, before, during and after Massive Vaccination" Vaccines 11, no. 11: 1676. https://doi.org/10.3390/vaccines11111676
APA StyleDomínguez-Ramírez, L., Sosa-Jurado, F., Díaz-Sampayo, G., Solis-Tejeda, I., Rodríguez-Pérez, F., Pelayo, R., Santos-López, G., & Cortes-Hernandez, P. (2023). Age and Comorbidities as Risk Factors for Severe COVID-19 in Mexico, before, during and after Massive Vaccination. Vaccines, 11(11), 1676. https://doi.org/10.3390/vaccines11111676







