Variations in COVID-19 Vaccine Attitudes and Acceptance among Refugees and Lebanese Nationals Pre- and Post-Vaccine Rollout in Lebanon
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Study Population
2.3. Survey Instrument
2.4. Survey Items and Health Beliefs Model Components
2.5. Primary Outcome
2.6. Data Analysis
3. Results
3.1. Participant Characteristics
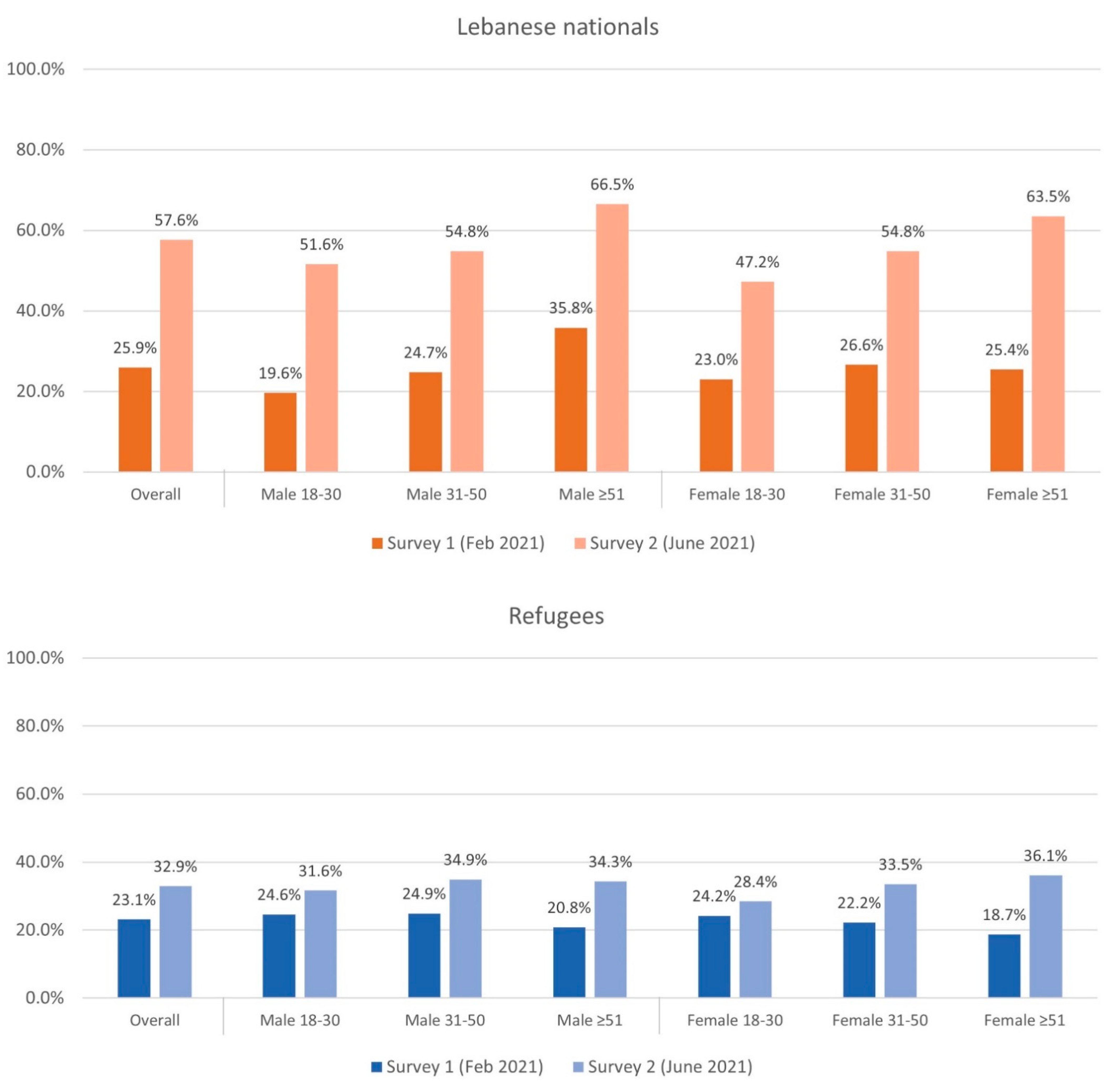
3.2. Vaccine Acceptance
3.3. Health Beliefs Model (HBM) Domains and Social Norms
3.4. Knowledge, Attitudes, and Beliefs
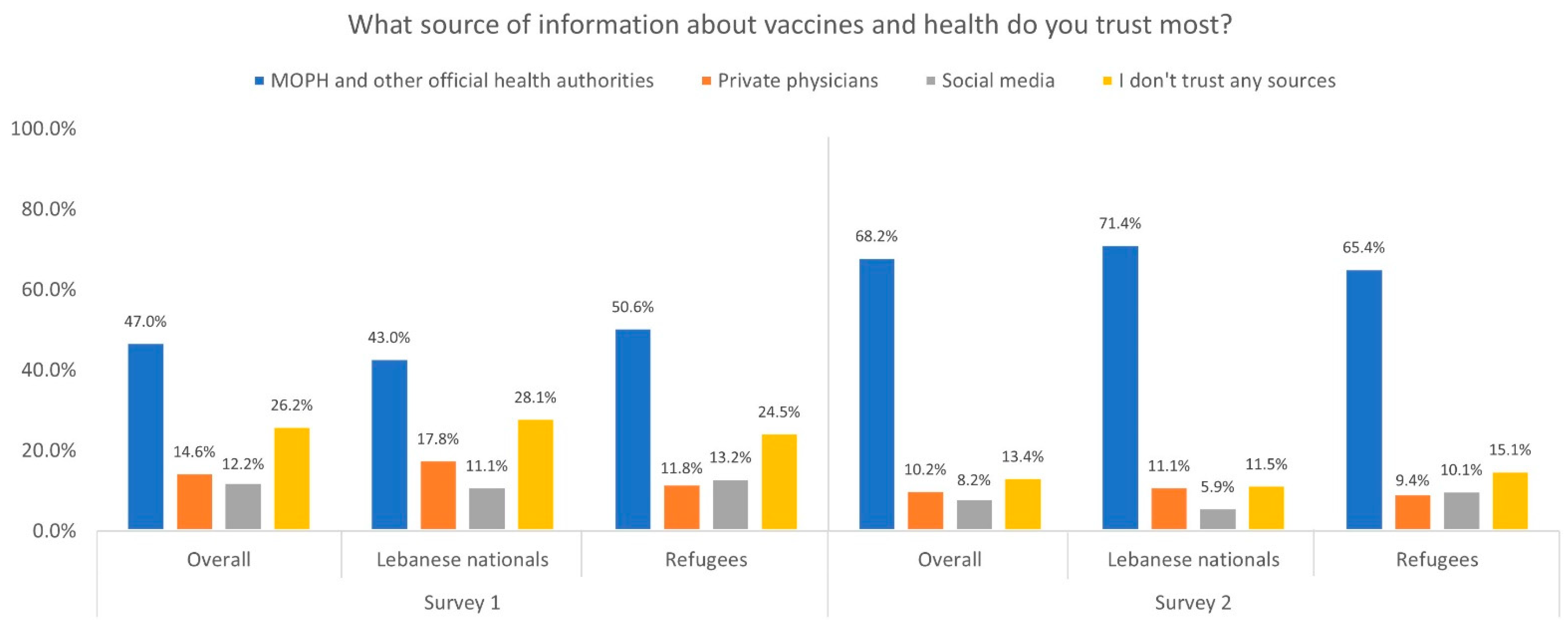
3.5. Communication
3.6. Barriers to Vaccination and Preferences for Vaccination Sites
3.7. Regression
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO Coronavirus (COVID-19) Dashboard|WHO Coronavirus (COVID-19) Dashboard with Vaccination Data. Available online: https://covid19.who.int/ (accessed on 22 August 2022).
- Coronavirus (COVID-19) Vaccinations—Our World in Data. Available online: https://ourworldindata.org/covid-vaccinations (accessed on 17 August 2022).
- Zard, M.; Lau, L.S.; Bowser, D.M.; Fouad, F.M.; Lucumí, D.I.; Samari, G.; Harker, A.; Shepard, D.S.; Zeng, W.; Moresky, R.T.; et al. Leave no one behind: Ensuring access to COVID-19 vaccines for refugee and displaced populations. Nat. Med. 2021, 27, 747–749. [Google Scholar] [CrossRef] [PubMed]
- The SAGE Working Group. Report of the Sage Working Group on Vaccine Hesitancy 12 November 2014. Sage Report (p. 9). 2014. Available online: https://www.who.int/immunization/sage/meetings/2014/october/SAGE_working_group_revised_report_vaccine_hesitancy.pdf?ua=1 (accessed on 22 August 2022).
- Lebanon: WHO Coronavirus Disease (COVID-19) Dashboard with Vaccination Data|WHO Coronavirus (COVID-19) Dashboard with Vaccination Data. Available online: https://covid19.who.int/region/emro/country/lb (accessed on 17 August 2022).
- Committee Covid-19 Vaccination National Coordination. Lebanon National Deployment and Vaccination Plan for COVID-19 Vaccines. Repub. Lebanon Ministy Public Health 2021, 1–62. [Google Scholar]
- 7. WHO Lebanon Exploison 2020 Update for Partners. 18 August 2020. Available online: https://www.who.int/emergencies/funding/appeals/lebanon-explosion-2020 (accessed on 17 August 2022).
- Blanchet, K.; Fouad, F.M.; Pherali, T. Syrian refugees in Lebanon: The search for universal health coverage. Confl. Health 2016, 10, 12. [Google Scholar] [CrossRef] [PubMed]
- Halabi, Z. Exclusion and identity in Lebanon’s Palestinian refugee camps: A story of sustained conflict. Environ. Urban. 2004, 16, 39–48. [Google Scholar] [CrossRef]
- Al Munajed, D.; Ekren, E. Exploring the impact of multidimensional refugee vulnerability on distancing as a protective measure against COVID-19: The case of Syrian refugees in Lebanon and Turkey. J. Migr. Health 2020, 1–2, 100023. [Google Scholar] [CrossRef]
- Lebanon’s Refugee Crisis, Part II: The Consequences of Lebanon’s Refugee Policies|Immigration and Human Rights Law Review. Available online: https://lawblogs.uc.edu/ihrlr/2020/04/30/lebanons-refugee-crisis-part-ii-the-consequences-of-lebanons-refugee-policies/ (accessed on 17 August 2022).
- Human Rights watch, Human Rights Watch World Report 2022, 32nd ed.; Human Rights Watch: New York, NY, USA, 2022; ISBN 9781644211212.
- Honein-AbouHaidar, G.; Noubani, A.; El Arnaout, N.; Ismail, S.; Nimer, H.; Menassa, M.; Coutts, A.P.; Rayes, D.; Jomaa, L.; Saleh, S.; et al. Informal healthcare provision in Lebanon: An adaptive mechanism among displaced Syrian health professionals in a protracted crisis. Confl. Health 2019, 13, 40. [Google Scholar] [CrossRef]
- Health Response Strategy (HRS) Maintaining Health Security, Preserving Population Health and Saving Children and Women Lives.|FAOLEX. Available online: https://www.fao.org/faolex/results/details/en/c/LEX-FAOC169761/ (accessed on 7 September 2022).
- Hemadeh, R.; Kdouh, O.; Hammoud, R.; Jaber, T.; Khalek, L.A. The primary healthcare network in Lebanon: A national facility assessment. East. Mediterr. Health J. 2020, 26, 700–707. [Google Scholar] [CrossRef]
- Mansour, Z.; Hamadeh, R.; Rady, A.; Danovaro-Holliday, M.C.; Fahmy, K.; Said, R.; Brandt, L.; Warrak, R.; Ammar, W. Vac-cination Coverage in Lebanon Following the Syrian Crisis: Results from the District-Based Immunization Coverage Evalu-ation Survey 2016. BMC Public Health 2019, 19, 58. [Google Scholar] [CrossRef]
- Roberton, T.; Weiss, W.; The Jordan Health Access Study Team; The Lebanon Health Access Study Team; Doocy, S. Challenges in Estimating Vaccine Coverage in Refugee and Displaced Populations: Results From Household Surveys in Jordan and Lebanon. Vaccines 2017, 5, 22. [Google Scholar] [CrossRef]
- Hajjar, M.S.; Abu-Sittah, G.S. The multidimensional burden of COVID-19 on Syrian refugees in Lebanon. J. Glob. Health 2021, 11, 05003. [Google Scholar] [CrossRef]
- Jawad, N.K.; Abu Taweeleh, L.; A Elharake, J.; Khamis, N.; Alser, O.; Karaki, F.M.; Aboukhater, L. Refugee access to COVID-19 vaccines in Lebanon. Lancet 2021, 397, 1884. [Google Scholar] [CrossRef]
- Lebanon: Refugees, Migrants Left Behind in Vaccine Rollout|Human Rights Watch. Available online: https://www.hrw.org/news/2021/04/06/lebanon-refugees-migrants-left-behind-vaccine-rollout (accessed on 17 August 2022).
- Kaloti, R.; Fouad, F.M. The politics of COVID-19 vaccine equity among refugee populations in Lebanon. J. Glob. Health Econ. Policy 2022, 2, e2022003. [Google Scholar] [CrossRef]
- Mumtaz, G.; El-Jardali, F.; Jabbour, M.; Harb, A.; Abu-Raddad, L.; Makhoul, M. Modeling the Impact of COVID-19 Vaccination in Lebanon: A Call to Speed-Up Vaccine Roll Out. Vaccines 2021, 9, 697. [Google Scholar] [CrossRef] [PubMed]
- Impact Open Data. Available online: https://impact.cib.gov.lb/home?dashboardName=vaccine&subsection=statistics (accessed on 17 August 2022).
- Saifee, J.; Franco-Paredes, C.; Lowenstein, S.R. Refugee Health During COVID-19 and Future Pandemics. Curr. Trop. Med. Rep. 2021, 8, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Al Halabi, C.K.; Obeid, S.; Sacre, H.; Akel, M.; Hallit, R.; Salameh, P.; Hallit, S. Attitudes of Lebanese adults regarding COVID-19 vaccination. BMC Public Health 2021, 21, 998. [Google Scholar] [CrossRef]
- Hanna, P.; Issa, A.; Noujeim, Z.; Hleyhel, M.; Saleh, N. Assessment of COVID-19 Vaccines Acceptance in the Lebanese Popu-lation: A National Cross-Sectional Study. J. Pharm. Policy Pract. 2022, 15, 5. [Google Scholar] [CrossRef]
- Salibi, N.; Abdulrahim, S.; El Haddad, M.; Bassil, S.; El Khoury, Z.; Ghattas, H.; McCall, S.J. COVID-19 vaccine acceptance in older Syrian refugees: Preliminary findings from an ongoing study. Prev. Med. Rep. 2021, 24, 101606. [Google Scholar] [CrossRef]
- Vaccine Hesitancy Survey Questions Related to SAGE Vaccine Hesitancy Matrix. Available online: https://cdn.who.int/media/docs/default-source/immunization/sage/2014/october/2-sage-appendicies-background-final.pdf?sfvrsn=2259f1bf_4 (accessed on 17 August 2022).
- Wagner, A.L.; Boulton, M.L.; Sun, X.; Mukherjee, B.; Huang, Z.; Harmsen, I.A.; Ren, J.; Zikmund-Fisher, B.J. Perceptions of measles, pneumonia, and meningitis vaccines among caregivers in Shanghai, China, and the health belief model: A cross-sectional study. BMC Pediatr. 2017, 17, 143. [Google Scholar] [CrossRef]
- Lu, J.; Luo, M.; Yee, A.Z.H.; Sheldenkar, A.; Lau, J.; Lwin, M.O. Do superstitious beliefs affect influenza vaccine uptake through shaping health beliefs? Vaccine 2019, 37, 1046–1052. [Google Scholar] [CrossRef]
- Hu, Y.; Wang, Y.; Liang, H.; Chen, Y. Seasonal Influenza Vaccine Acceptance among Pregnant Women in Zhejiang Province, China: Evidence Based on Health Belief Model. Int. J. Environ. Res. Public Health 2017, 14, 1551. [Google Scholar] [CrossRef]
- Mo, P.K.H.; Wong, C.H.W.; Lam, E.H.K. Can the Health Belief Model and moral responsibility explain influenza vaccination uptake among nurses? J. Adv. Nurs. 2018, 75, 1188–1206. [Google Scholar] [CrossRef] [PubMed]
- Fall, E.; Izaute, M.; Chakroun-Baggioni, N. How can the health belief model and self-determination theory predict both influenza vaccination and vaccination intention ? A longitudinal study among university students. Psychol. Health 2018, 33, 746–764. [Google Scholar] [CrossRef]
- Miller, P.D.E.; Forster, A.S.; de Silva, T.I.; Leonard, H.; Anthias, C.; Mayhew, M.; Klammer, M.; Paskar, S.; Hurst, E.; Peggs, K.; et al. Sociodemographic and psychological determinants of influenza vaccine intention among recipients of autologous and allogeneic haematopoietic stem cell transplant: A cross-sectional survey of UK transplant recipients using a modified health belief model. BMJ Open 2018, 8, e021222. [Google Scholar] [CrossRef] [PubMed]
- Mahmud, I.; Kabir, R.; Rahman, M.; Alradie-Mohamed, A.; Vinnakota, D.; Al-Mohaimeed, A. The Health Belief Model Predicts Intention to Receive the COVID-19 Vaccine in Saudi Arabia: Results from a Cross-Sectional Survey. Vaccines 2021, 9, 864. [Google Scholar] [CrossRef] [PubMed]
- Mercadante, A.R.; Law, A.V. Will they, or Won’t they? Examining patients’ vaccine intention for flu and COVID-19 using the Health Belief Model. Res. Soc. Adm. Pharm. 2020, 17, 1596–1605. [Google Scholar] [CrossRef]
- Shahnazi, H.; Ahmadi-Livani, M.; Pahlavanzadeh, B.; Rajabi, A.; Hamrah, M.S.; Charkazi, A. Assessing preventive health behaviors from COVID-19: A cross sectional study with health belief model in Golestan Province, Northern of Iran. Infect. Dis. Poverty 2020, 9, 157. [Google Scholar] [CrossRef]
- Guidry, J.P.; Laestadius, L.I.; Vraga, E.K.; Miller, C.A.; Perrin, P.B.; Burton, C.W.; Ryan, M.; Fuemmeler, B.F.; Carlyle, K.E. Willingness to get the COVID-19 vaccine with and without emergency use authorization. Am. J. Infect. Control 2020, 49, 137–142. [Google Scholar] [CrossRef]
- Hossain, M.B.; Alam, Z.; Islam, S.; Sultan, S.; Faysal, M.; Rima, S.; Hossain, A.; Al Mamun, A. Health Belief Model, Theory of Planned Behavior, or Psychological Antecedents: What Predicts COVID-19 Vaccine Hesitancy Better Among the Bangladeshi Adults? Front. Public Health 2021, 9, 711066. [Google Scholar] [CrossRef]
- Chen, H.; Li, X.; Gao, J.; Liu, X.; Mao, Y.; Wang, R.; Zheng, P.; Xiao, Q.; Jia, Y.; Fu, H.; et al. Health Belief Model Perspective on the Control of COVID-19 Vaccine Hesitancy and the Promotion of Vaccination in China: Web-Based Cross-sectional Study. J. Med. Internet Res. 2021, 23, e29329. [Google Scholar] [CrossRef]
- Wong, M.C.S.; Wong, E.L.Y.; Huang, J.; Cheung, A.W.L.; Law, K.; Chong, M.K.C.; Ng, R.W.Y.; Lai, C.K.C.; Boon, S.S.; Lau, J.T.F.; et al. Acceptance of the COVID-19 vaccine based on the health belief model: A population-based survey in Hong Kong. Vaccine 2021, 39, 1148–1156. [Google Scholar] [CrossRef]
- Wong, L.P.; Alias, H.; Wong, P.-F.; Lee, H.Y.; Abubakar, S. The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Hum. Vaccines Immunother. 2020, 16, 2204–2214. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.; Hu, Z.; Zhao, Q.; Alias, H.; Danaee, M.; Wong, L.P. Understanding COVID-19 vaccine demand and hesitancy: A nationwide online survey in China. PLoS Negl. Trop. Dis. 2020, 14, e0008961. [Google Scholar] [CrossRef]
- Sallam, M.; Dababseh, D.; Eid, H.; Al-Mahzoum, K.; Al-Haidar, A.; Taim, D.; Yaseen, A.; Ababneh, N.A.; Bakri, F.G.; Mahafzah, A. High Rates of COVID-19 Vaccine Hesitancy and Its Association with Conspiracy Beliefs: A Study in Jordan and Kuwait among Other Arab Countries. Vaccines 2021, 9, 42. [Google Scholar] [CrossRef]
- Albahri, A.H.; Alnaqbi, S.A.; Alshaali, A.O.; Shahdoor, S.M. COVID-19 Vaccine Acceptance in a Sample From the United Arab Emirates General Adult Population: A Cross-Sectional Survey, 2020. Front. Public Health 2021, 9, 614499. [Google Scholar] [CrossRef]
- Kaadan, M.I.; Abdulkarim, J.; Chaar, M.; Zayegh, O.; Keblawi, M.A. Determinants of COVID-19 vaccine acceptance in the Arab world: A cross-sectional study. Glob. Health Res. Policy 2021, 6, 23. [Google Scholar] [CrossRef] [PubMed]
- Tahir, A.I.; Ramadhan, D.S.; Piro, S.S.; Abdullah, R.Y.; Taha, A.A.; Radha, R.H. COVID-19 Vaccine Acceptance, Hesitancy and Refusal among Iraqi Kurdish Population. Int. J. Health Sci. 2022, 16, 10. [Google Scholar]
- World Health Organization COVID-19 Vaccines: Safety Manual; World Health Organization: Geneva, Switzerland, 2021; ISBN 9789240018280.
- Evoke the Right Emotions—Guide to COVID-19 Vaccine Communications. Available online: https://covid19vaccinescommunicationprinciples.org/the-principles/emotions/ (accessed on 17 August 2022).
- Seboka, B.T.; Yehualashet, D.E.; Belay, M.M.; Kabthymer, R.H.; Ali, H.; Hailegebreal, S.; Demeke, A.D.; Amede, E.S.; Tesfa, G.A. Factors Influencing COVID-19 Vaccination Demand and Intent in Resource-Limited Settings: Based on Health Belief Model. Risk Manag. Healthc. Policy 2021, 2021, 2743–2756. [Google Scholar] [CrossRef]
- Tao, L.; Wang, R.; Han, N.; Liu, J.; Yuan, C.; Deng, L.; Han, C.; Sun, F.; Liu, M.; Liu, J. Acceptance of a COVID-19 vaccine and associated factors among pregnant women in China: A multi-center cross-sectional study based on health belief model. Hum. Vaccines Immunother. 2021, 17, 2378–2388. [Google Scholar] [CrossRef]
- Kerr, J.; Freeman, A.; Marteau, T.; van der Linden, S. Effect of Information about COVID-19 Vaccine Effectiveness and Side Effects on Behavioural Intentions: Two Online Experiments. Vaccines 2021, 9, 379. [Google Scholar] [CrossRef]
- Lebanon Begins Vaccinations with Sceptics a Major Hurdle|Coronavirus Pandemic News|Al Jazeera. Available online: https://www.aljazeera.com/news/2021/2/16/lebanon-begins-vaccinations-with-sceptics-a-major-hurdle (accessed on 17 August 2022).
| Survey 1 (n = 3927) n (%) | Survey 2 (n = 4174) n (%) | p * | |
|---|---|---|---|
| Age Category | <0.001 | ||
| 18–30 years | 1436 (36.6) | 1222 (29.3) | |
| 31–50 years | 1567 (39.9) | 1695 (40.6) | |
| ≥51 years | 924 (23.5) | 1257 (30.1) | |
| Gender | 0.769 | ||
| Female | 2140 (54.5) | 2261 (54.2) | |
| Male | 1787 (45.5) | 1913 (45.8) | |
| Nationality | 0.724 | ||
| Lebanese | 1850 (47.1) | 1950 (46.7) | |
| Refugees | 2077 (52.9) | 2224 (53.3) | |
| Palestinian | - | 86 (2.1) | |
| Syrian | - | 2129 (51.0) | |
| Other | - | 9 (0.2) | |
| Location | |||
| Akkar | 545 (13.9) | 884 (21.2) | |
| Beirut | 713 (18.2) | 395 (9.5) | |
| Bekaa | 878 (22.4) | 743 (17.8) | |
| Deddeh lkoura | 1 (0.03) | - | |
| Mount Lebanon | 580 (14.8) | 439 (10.5) | |
| North Tripoli | 453 (11.5) | 624 (14.9) | |
| South | 750 (19.1) | 1089 (26.1) | |
| Missing | 7 (0.2) | - |
| Intention to Receive Vaccine | |||||
|---|---|---|---|---|---|
| Survey 1 | Survey 2 | ||||
| Domain | Yes Mean (SD) | Unsure/No Mean (SD) | Yes Mean (SD) | Unsure/No Mean (SD) | p * |
| Perceived Susceptibility (α = 0.67) | |||||
| I do not need to receive the vaccine because I have good health | 0.64 (0.83) | 1.31 (0.81) | 0.31 (0.66) | 1.24 (0.86) | <0.001 |
| I do not need to receive the vaccine if had been infected with COVID-19 and recovered | 0.62 (0.79) | 1.07 (0.80) | 0.38 (0.68) | 0.94 (0.84) | <0.001 |
| Perceived Severity | |||||
| I am not at risk of severe complications of COVID-19 so I will not take the vaccine (Yes/No) | <0.001 | ||||
| Yes | 1603 (54.0) | 294 (30.7) | 1133 (48.8) | 281 (15.2) | |
| No | 1365 (46.0) | 665 (69.3) | 1187 (51.2) | 1573 (84.8) | |
| Perceived Benefit (α = 0.85) | |||||
| I think the COVID-19 vaccine is safe | 1.48 (0.60) | 0.58 (0.56) | 1.70 (0.49) | 0.85 (0.61) | <0.001 |
| I think the COVID-19 vaccine is effective | 1.48 (0.57) | 0.66 (0.55) | 1.64 (0.51) | 0.86 (0.60) | <0.001 |
| Perceived Barrier (α = 0.79) | |||||
| I don’t trust COVID-19 vaccine because it was developed in a short period of time | 0.33 (0.47) | 0.78 (0.42) | 0.15 (0.36) | 0.69 (0.46) | <0.001 |
| I think COVID-19 vaccine would change your DNA | 0.68 (0.66) | 1.16 (0.64) | 0.45 (0.59) | 0.91 (0.67) | <0.001 |
| I am concerned about side effects or risks of the vaccine | 1.11 (0.84) | 1.78 (0.50) | 0.74 (0.78) | 1.70 (0.57) | <0.001 |
| I think the side effects of the COVID-19 vaccine are very serious/could lead to death | 0.72 (0.70) | 1.45 (0.61) | 0.48 (0.59) | 1.24 (0.70) | <0.001 |
| The COVID-19 vaccine will not succeed because the virus keeps changing | 0.90 (0.72) | 1.49 (0.64) | 0.60 (0.64) | 1.22 (0.68) | <0.001 |
| Cues to Action | |||||
| I would be more comfortable getting the vaccine if I saw neighbors, community leaders, religious leaders, doctors, celebrities, politicians receive the vaccine | 1.77 (0.55) | 0.90 (0.80) | 1.82 (0.50) | 1.00 (0.80) | 0.0293 |
| Social Norms | |||||
| Most people I know are going to receive the vaccine | 1.16 (0.76) | 0.54 (0.58) | 1.24 (0.68) | 0.70 (0.63) | 0.006 |
| Knowledge (total score 0–8) | 5.37 (2.12) | 4.47 (2.13) | 7.22 (1.23) | 6.23 (1.81) | <0.001 |
| Knowledge | ||||
|---|---|---|---|---|
| Agree | Unsure | Disagree | ||
| I have enough information about the COVID-19 vaccine and how it works | Survey 1 | 23.3% | 30.1% | 46.6% |
| Survey 2 | 65.0% | 19.5% | 15.6% | |
| I know that there are different COVID-19 vaccines | Survey 1 | 55.3% | 18.8% | 25.9% |
| Survey 2 | 85.1% | 8.4% | 6.5% | |
| I know that the COVID-19 vaccine is available for all nationalities and free of charge | Survey 1 | 51.8% | 29.7% | 18.5% |
| Survey 2 | 89.4% | 7.5% | 3.1% | |
| I am aware of the categories who are eligible to take the vaccine first | Survey 1 | 46.5% | 31.4% | 22.1% |
| Survey 2 | 64.5% | 23.8% | 11.7% | |
| The vaccine can be given to pregnant women | Survey 1 | - | - | - |
| Survey 2 | 27.9% | 29.0% | 43.2% | |
| Attitudes and Beliefs | Agree | Unsure | Disagree | |
| It is possible that I would accept a certain vaccine and refuse another | Survey 1 | 21.4% | 42.4% | 36.2% |
| Survey 2 | 47.6% | 29.8% | 22.6% | |
| Given the variety of vaccines and their evolution I would prefer to wait until they are proven to be safe | Survey 1 | 68.8% | 16.1% | 15.1% |
| Survey 2 | 53.9% | 16.3% | 29.9% | |
| I think there is a better way than the vaccine to fight COVID-19 | Survey 1 | 23.4% | 33.6% | 42.9% |
| Survey 2 | 15.8% | 33.8% | 50.4% | |
| If I receive the vaccine, I will not need to wear a mask anymore | Survey 1 | 17.5% | 26.6% | 55.9% |
| Survey 2 | 18.1% | 20.4% | 61.6% | |
| If a person has an allergy, they should not receive the vaccine | Survey 1 | 42.8% | 43.3% | 13.9% |
| Survey 2 | 39.7% | 28.8% | 31.5% | |
| I believe that the Lebanese health system is capable of ensuring safe administration of the COVID-19 vaccine | Survey 1 | 36.5% | - | 63.5% |
| Survey 2 | 50.2% | - | 49.8% |
| Survey 1 | Survey 2 | |||||
|---|---|---|---|---|---|---|
| Overall | Lebanese | Refugees | Overall | Lebanese | Refugees | |
| I prefer to receive the vaccine in Ministry of Public Health vaccination centers | 37.3% | 35.0% | 39.4% | 58.7% | 67.6% | 50.9% |
| I prefer to receive the vaccine in a private clinic/hospital even if it’s not free | 19.0% | 22.0% | 16.3% | 19.2% | 23.7% | 15.3% |
| I prefer to receive the vaccine in a primary health care center or dispensary near me | 32.7% | 29.4% | 35.6% | 40.3% | 44.0% | 37.1% |
| I prefer to receive the vaccine if provided at my residence (street or home or camp) | - | - | - | 29.3% | 34.6% | 24.7% |
| Survey 1 | Survey 2 | |||
|---|---|---|---|---|
| aOR (95% CI) | p | aOR (95% CI) | p | |
| Gender | 0.897 | 0.531 | ||
| Female | Ref | Ref | ||
| Male | 0.99 (0.79–1.22) | 1.06 (0.88–1.29) | ||
| Age Category | 0.563 | 0.049 | ||
| 18–30 years | Ref | Ref | ||
| 31–50 years | 1.13 (0.89–1.45) | 1.13 (0.90–1.43) | ||
| ≥51 years | 1.13 (0.84–1.52) | 1.37 (1.06–1.78) | ||
| Nationality | 0.427 | <0.001 | ||
| Lebanese | Ref | Ref | ||
| Refugees | 0.91 (0.73–1.14) | 0.50 (0.41–0.60) | ||
| Perceived Susceptibility | 1.24 (1.13–1.36) | <0.001 | 1.39 (1.28–1.51) | <0.001 |
| Perceived Severity | 0.93 (0.73–1.19) | 0.582 | 1.27 (1.00–1.61) | 0.052 |
| Perceived Benefits | 3.30 (2.89–3.81) | <0.001 | 2.26 (2.02–2.53) | <0.001 |
| Perceived Barriers | 0.69 (0.65–0.73) | <0.001 | 0.70 (0.66–0.74) | <0.001 |
| Cues to Action | 2.67 (2.26–3.16) | <0.001 | 2.55 (2.20–2.95) | <0.001 |
| Social Norms | 1.64 (1.38–1.95) | <0.001 | 1.31 (1.13–1.53) | <0.001 |
| Knowledge | 1.08 (1.03–1.15) | 0.004 | 1.05 (0.98–1.12) | 0.168 |
| Pseudo R2 | 0.642 | 0.684 | ||
| AUC 0.929 | VIF 3.04 | AUC 0.933 | VIF 4.92 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ali, Z.; Perera, S.M.; Garbern, S.C.; Diwan, E.A.; Othman, A.; Ali, J.; Awada, N. Variations in COVID-19 Vaccine Attitudes and Acceptance among Refugees and Lebanese Nationals Pre- and Post-Vaccine Rollout in Lebanon. Vaccines 2022, 10, 1533. https://doi.org/10.3390/vaccines10091533
Ali Z, Perera SM, Garbern SC, Diwan EA, Othman A, Ali J, Awada N. Variations in COVID-19 Vaccine Attitudes and Acceptance among Refugees and Lebanese Nationals Pre- and Post-Vaccine Rollout in Lebanon. Vaccines. 2022; 10(9):1533. https://doi.org/10.3390/vaccines10091533
Chicago/Turabian StyleAli, Zawar, Shiromi M. Perera, Stephanie C. Garbern, Elsie Abou Diwan, Alaa Othman, Javed Ali, and Nada Awada. 2022. "Variations in COVID-19 Vaccine Attitudes and Acceptance among Refugees and Lebanese Nationals Pre- and Post-Vaccine Rollout in Lebanon" Vaccines 10, no. 9: 1533. https://doi.org/10.3390/vaccines10091533
APA StyleAli, Z., Perera, S. M., Garbern, S. C., Diwan, E. A., Othman, A., Ali, J., & Awada, N. (2022). Variations in COVID-19 Vaccine Attitudes and Acceptance among Refugees and Lebanese Nationals Pre- and Post-Vaccine Rollout in Lebanon. Vaccines, 10(9), 1533. https://doi.org/10.3390/vaccines10091533





