Abstract
Influenza represents a threat to global health and health care workers (HCWs) have an increased risk of contracting the influenza virus in the workplace. The COVID-19 pandemic has brought back the importance of influenza vaccination, as the influenza virus can circulate together with SARS-CoV-2. The aim of this report is to describe the actual flu vaccination coverage among healthcare workers of a research hospital and the trend changes, with respect to the past flu vaccination campaigns, in light of the present pandemic and COVID-19 vaccination. A Pearson’s χ2 test was used to test the correlation of flu vaccination coverage, across all professional categories, between the last two years. A linear regression model was adopted to predict the total vaccination coverage of this year. A statistically significant decrease (p < 0.01) was observed in vaccination coverage among all the professional categories with a 50% reduction in vaccination trends between the last two years. Analyzing the data from the previous six flu vaccination campaigns, the expected value, according to the linear regression model, was estimated to be 38.5% while the observed value was 24%. The decrease in vaccination coverage may be due to the fear of the pandemic situation and especially to the uncertainty related to the consequences of a concurrent administration which may overload the immune system or may be more reactogenic. The COVID-19 pandemic represents an opportunity to promote and support large-scale influenza vaccination among HCWs through structured programs, adequate funding, and tailored communication strategies.
1. Introduction
Influenza represents a threat to global health in terms of mortality and morbidity. It is estimated that it can infect up to one billion individuals each year although severe cases are 3–5 million, with a death toll ranging from 290,000 to 650,000 [1].
Health care workers have an increased risk of contracting the influenza virus in the workplace, both from patients and from infected colleagues: they are at increased risk compared with the average healthy adult [2,3], and it is estimated that one in four healthcare workers may become infected during a mild flu season [2].
For this reason, the World Health Organization (WHO) considers healthcare workers a priority high-risk group for receiving influenza vaccination to protect themselves and their patients, and to ensure continuity of healthcare services [4].
The perception of risk towards influenza among healthcare workers varies according to the work setting (i.e., hospitals with high intensity of care or community hospitals) [5,6] and the care task performed: medical doctors show a greater acceptance of influenza vaccination, while nurses, midwives, nursing assistants, and nursing aides are less inclined to vaccination [5,7].
In addition, healthcare professionals employed in high-risk departments are more willing to be vaccinated, a phenomenon probably attributable to a greater perception of risk [8,9,10].
Although the optimal vaccination rate among health care professionals is 100%, a minimum rate of 80% is considered sufficient to prevent circulation of the virus [11,12].
However, healthcare professionals’ compliance with influenza vaccination and, consequently, vaccination coverages, are worryingly low [13].
For three consecutive vaccination seasons from 2015 to 2018, vaccination coverages among healthcare workers in 12 European Union states decreased, ranging from a minimum of 15.6% to a maximum of 63.2% [14]. These data are corroborated by several other studies, which have shown minimum coverages of even less than 10% [5,15,16].
In 2017, 119 countries and regions used flu vaccine, and 102 countries had policies in place to vaccinate health care workers [10,14,17].
Significantly low coverages are common among medical residents that begin to be part of the HCW risk group when they start their internships in medical-care facilities [18,19].
Only 18.2% of Italian medical residents underwent influenza vaccination in the 2016–2017 season, far from the coverages achieved in the United States [20] and France [21] in previous vaccination seasons and from the goals of the national vaccine prevention plan [22]. These coverages are similar or even lower than those reported among HCWs [18,19,23,24].
The main reasons for this low adherence are a poor perception of the risk of becoming infected, the belief that patients will still develop symptoms despite vaccination, a lack of awareness of being able to transmit the infection to their patients, a lack of time due to very long shifts, and doubts about their efficacy [25,26,27].
Medical residents in the medical area seem to be more inclined to vaccination, perhaps because of the type of patients they take care of [25,26].
Several strategies have been implemented to increase healthcare workers’ adherence to influenza vaccination [28]. The most effective has proven to be compulsory vaccination, especially for healthcare workers in contact with high-risk patients [29,30]; however, this measure burdens workers’ morale and has non-negligible ethical and legal implications [28,31,32].
The effectiveness of other strategies is proportional to the number of them employed, and includes the use of free vaccination, reminders, vaccination in the workplace, and educational material tailored to different classes of health workers [28].
The COVID-19 pandemic has brought back the importance of influenza vaccination [33], as the influenza virus can circulate together with SARS-CoV-2 [34,35].
Both viruses have a high societal impact in terms of mortality and morbidity [36,37,38], and since both are respiratory viruses with similar symptoms, differential diagnosis is complex [35].
Several studies have shown that the COVID-19 pandemic has influenced the attitude and perception of HCWs to influenza vaccination [36,39,40].
In this regard, Stöckeler et al. [39] report a rise in the influenza vaccination coverage from 31% in the 2016/2017 season to 59% in the 2020/2021 season; similarly, Wang et al. outline a more positive attitude towards influenza vaccination, possibly due to a raised awareness of the risks related to airborne infections [41].
Moreover, Di Pumpo et al. report an increase in vaccine coverage in some professional classes not directly involved in taking care of frail patients, such as administrative or auxiliary staff, suggesting a correlation between the fear of COVID-19 and the increase in vaccination rates [42].
The aim of this report is to describe the actual flu vaccination coverage among healthcare workers of a research hospital and the variations, over the past six flu vaccination campaigns, in light of the present pandemic and COVID-19 vaccination.
2. Materials and Methods
A retrospective cohort study was conducted to evaluate the flu vaccination coverage among the health workers of the Fondazione Policlinico Universitario Agostino Gemelli IRCCS, an Italian high complexity research hospital. All personnel were offered vaccination by the hospital hygiene unit from October 2021 to January 2022. The personnel working at hospital units who could give written informed consent were included. The study protocol was approved by the research hospital Ethical Board with the approval number 10755/22 ID 3706.
The vaccines were provided free of charge to the HCWs by the Local Health Unit according to the Italian “Piano Nazionale Prevenzione Vaccinale” [22]. Two vaccine hubs were set up in different areas of our research hospital to favor a major accessibility from the HCWs. The vaccine hubs were run by specialist medical doctors in hygiene and preventive medicine, occupational medicine, resident medical doctors of the same areas, and nurses who delivered vaccination.
Administrative hospital databases were queried to retrieve vaccination data for the assessed time horizon (i.e., from October 2021 to January 2022). A database was set up defining firstly a unique anonymous identifier code for each individual with the specification of the professional occupation. The individual employee tax code was used to obtain socio-demographic data as the age and sex whereas information about occupation was acquired from the research hospital human resources unit.
In relation to the vaccine coverage analysis, the findings were preliminary described through frequencies and percentages. A Pearson’s χ2 test was used to test the correlation of flu vaccination coverage, across all professional categories, between the last two years.
Furthermore, a multivariable logistic regression was performed to investigate the influence of gender, age, and occupation on the likelihood towards vaccination.
Based on the assumption of the model, the dependent variable was dichotomized into health workers who got vaccinated and those who did not. The Hosmer–Lemeshow (HL) goodness of fit test was run to test how well the data fits the logistic model [43]. A significance higher than 0.05 showed a good model fitness. Moreover, a receiver operating characteristic (ROC) curve was designed to analyze the area under this curve (AUC) to assess the overall measure of model fit [44].
In addition, a linear regression model was adopted to predict the total vaccination coverage of this year [45,46]. Five per cent was the statistical level chosen for all the statistical analyses which were run on STATA 17 (StataCorp LP, College Station, TX, USA).
3. Results
Between October 2021 and January 2022, 8221 hospital workers were observed. A total of 1979 individuals were vaccinated, while 6242 were unvaccinated. Of the observed hospital workers, 40% were male, 47% were older than 40 years old, and 42% were medical doctors. The median age at vaccination was 39.
Table 1 depicts a statistically significant decrease in vaccination coverage among all the professional categories with, approximately, a 50% reduction in vaccination trends between the last two years.

Table 1.
Vaccination coverage by occupation in the last two years.
The findings of the multivariate logistic regression showed that being a nurse was statistically significant associated with a lower vaccination uptake in comparison with being a physician (OR 2.35, 95% CI 2.02–2.73) or a resident medical doctor (OR 1.38, 95% CI 1.18–1.61). Moreover, the results highlighted that being aged between 40 and 59 (OR 1.26, 95% CI 1.11–1.43), compared with the youngest age class (i.e., between 20 and 39), was statistically significant associated with a higher uptake to vaccination. Interestingly, being male, is associated with a statistically significant reduction (OR 0.89, 95% CI 0.79–0.98) in vaccination uptake with respect to be female. According to the HL test, the model fitted quite well (p > 0.2). This result is also confirmed by AUC highlighting a good fit of the model (0.59, 95% CI 0.57–0.61).
Furthermore, analyzing the data from the previous six flu vaccination campaigns, the expected value, according to the linear regression model, was estimated to be 38.5%. However, the observed value was sharply lower, although not statistically significant, amounting to 24.0%.
Considering the data point of 20/21 (i.e., 54.6%) as an outlier, the coverage of the current vaccination campaign is similar to the one of the 19/20 campaign (Figure 1).
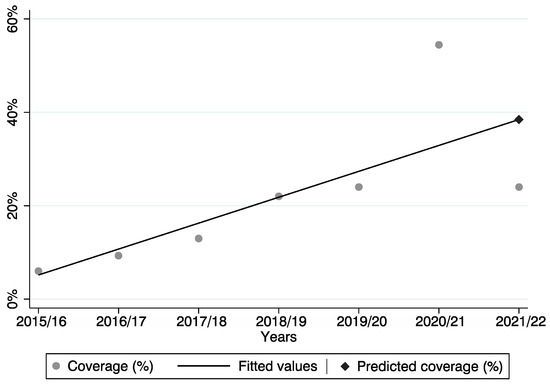
Figure 1.
Predicted and observed vaccination coverage across the six vaccination campaigns.
4. Discussion and Conclusions
Study findings show a major decline in the coverage achieved by influenza vaccination compared to the change of increasing coverage that can be described from 2016 onwards. The drop in coverage is even more pronounced when comparing with coverage for the 2020–2021 vaccination season, in which the absence of a SARS-CoV-2 vaccine prompted more healthcare workers to be vaccinated.
The results are in line with those reported by Public Health England, which found a decrease in influenza vaccination coverage among healthcare workers (76.8% in 2021 [47] vs. 60.5% in 2022 [48]), albeit less marked than that described in our study.
This trend, similar to that found in our study, was described for medical doctors (78.2% in 2020–2021 vs. 63.5% in 2021–2022), qualified nurses (76.7% in 2020–2021 vs. 61.5% in 2021–2022), other professionally qualified clinical staff (78.7% in 2020–2021 vs. 63.9% in 2021–2022), and support staff (75.5% in 2020–2021 vs. 56.6% in 2021–2022) [47,48].
The observed coverage is quite similar to the one reached in the year before pandemic. This is against the expected scenario based on the assumption that the COVID-19 pandemic was regarded as an incentive to a good public health practice such as flu vaccination among HCWs [42].
The period of influenza vaccination coincided with the administration of the booster dose against SARS-CoV-2. Although some healthcare workers even opted for the co-administration, many others expressed concerns about the administration within a short period of time, therefore preferring to prioritize the SARS-CoV-2 vaccination and, thus, avoiding the flu one. The main reasons [49] seem to be the fear of the pandemic situation and especially in the uncertainty related to the consequences of a concurrent administration which may overload the immune system or may be more reactogenic, despite the availability of evidence-based recommendations demonstrating its safety and immunogenicity [50]. Moreover, another reason might be the spread of anti-vaccine movements, deriving from the COVID-19 vaccination campaign, even among HCWs, which might also affect the flu vaccination.
Therefore, in order to increase the coverage of influenza vaccination in the next vaccination seasons, it would be advisable to think, in case it would be necessary a booster dose for COVID-19, of a single vaccine to be administered with a single injection as well as to implement timely and innovative organizational approaches.
The differences in vaccine attitudes between physicians and nurses among health care professionals are not only seen in Western countries, such as Italy, but also in East Asian countries, such as Japan. In line with our findings, physicians seem to have a higher willingness to vaccination in Western and Middle East countries [51,52,53,54,55,56]. The reasons underlying this difference might lie in the higher level of knowledge about influenza and influenza vaccines of physicians, the idea of maintaining a strong and healthy body, decisional autonomy, and a perception of untrustworthy environment held by nurses [54,55,56,57].
Besides, according to the evidence in the scientific literature, in Far East countries nurses have a lower vaccine hesitancy compared with physicians. The reason underlying this difference is still debated even though a few scholars have argued that medical doctors do not have enough time to secure vaccination due to their busy schedules [10,58,59].
Before and after the COVID-19 pandemic, the flu vaccination coverage was quite equivalent, implying that, once the acute phase of the emergency gone, HCWs seem to be unwilling to be vaccinated against flu due to the lack of a robust preventive culture. Hence, it is essential to set up and maintain high standards of evidence-based preventive policies (e.g., educational and promotional interventions and on-site vaccinations) [60,61], enhancing them with the lessons learnt from the pandemic experience.
The findings of our report should be assessed considering its limitations and strengths. One caveat is that the findings are based on data from only one hospital which might make the results less representative and biased.
However, our hospital shares common characteristics with other national and international research hospitals, such as a high levels of research activity and a higher internal commitment to guarantee continuous quality improvement so that the care activities are also oriented to innovation assessment and scientific production. Another limitation is the lack of consideration of HCWs vaccinated outside our research hospital; nonetheless, this report is ground-breaking in this field for this flu vaccination campaign (i.e., 2021/22). Finally, an additional limit might be the adoption of a simple linear regression model for fitting data. However, the statistical analysis was conducted according to the proper methodological frameworks and the evidence available in the scientific literature [45,46].
Further studies are required to explore the reasons for health workers’ vaccine hesitancy and to carry out a more incisive information campaign. Additional research, based on well-defined qualitative methods such as surveys, is needed to explore other factors influencing attitudes towards vaccination among HCWs.
It is of paramount importance to not undervalue this red flag. The COVID-19 pandemic represents an opportunity to promote and support large-scale influenza vaccination among HCWs through structured programs, adequate funding [62], and tailored, clear, and consistent communication strategies [63].
Author Contributions
Conceptualization and Project administration, D.P., M.C.N., G.D. and P.L.; Investigation, D.P. and M.C.N.; Methodology, D.P. and M.C.N.; Writing—original draft, D.P., M.C.N., A.L. and E.M.; Writing—review and editing, D.P., M.C.N., A.L., E.M., G.V., A.C., U.M., A.D.P., G.D. and P.L.; Visualization, D.P., M.C.N., A.L., E.M., G.V., A.C., U.M., A.D.P., G.D. and P.L.; Software, M.C.N.; Data curation, D.P., M.C.N., A.L. and E.M.; Formal analysis, M.C.N.; Resources: D.P., M.C.N., A.L., E.M. and A.D.P.; Validation, G.D. and P.L.; Supervision, G.V., A.C., U.M., G.D. and P.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was approved by the Ethics Committee (Prot. n. 10755/22.; ID 3706) of the Policlinico Universitario A. Gemelli IRCCS and by the Internal Board of Università Cattolica del Sacro Cuore.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data presented in this study are available upon request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- World Health Organization Global Influenza Strategy 2019–2030; World Health Organization: Geneva, Switzerland, 2019; ISBN 978-92-4-151532-0.
- Samyn, M.; Van Hal, G.; Vandevijvere, H.; Van Damme, P. The influenza vaccine for nursing and care professionals at emergency services in Flanders. Hum. Vaccines Immunother. 2021, 17, 2719–2722. [Google Scholar] [CrossRef]
- Galanakis, E.; Jansen, A.; Lopalco, P.L.; Giesecke, J. Ethics of mandatory vaccination for healthcare workers. Eurosurveillance 2013, 18, 20627. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization Vaccines against influenza WHO position paper—November 2012. Wkly. Epidemiol. Rec. 2012, 87, 461–476.
- Dini, G.; Toletone, A.; Sticchi, L.; Orsi, A.; Bragazzi, N.L.; Durando, P. Influenza vaccination in healthcare workers: A comprehensive critical appraisal of the literature. Hum. Vaccines Immunother. 2018, 14, 772–789. [Google Scholar] [CrossRef] [PubMed]
- Koh, Y.; Hegney, D.G.; Drury, V. Comprehensive systematic review of healthcare workers’ perceptions of risk and use of coping strategies towards emerging respiratory infectious diseases. Int. J. Evid. Based Healthc. 2011, 9, 403–419. [Google Scholar] [CrossRef] [PubMed]
- Boey, L.; Bral, C.; Roelants, M.; De Schryver, A.; Godderis, L.; Hoppenbrouwers, K.; Vandermeulen, C. Attitudes, believes, determinants and organisational barriers behind the low seasonal influenza vaccination uptake in healthcare workers—A cross-sectional survey. Vaccine 2018, 36, 3351–3358. [Google Scholar] [CrossRef] [PubMed]
- Hagemeister, M.H.; Stock, N.K.; Ludwig, T.; Heuschmann, P.; Vogel, U. Self-reported influenza vaccination rates and attitudes towards vaccination among health care workers: Results of a survey in a German university hospital. Public Health 2018, 154, 102–109. [Google Scholar] [CrossRef]
- Liu, H.; Tan, Y.; Zhang, M.; Peng, Z.; Zheng, J.; Qin, Y.; Guo, Z.; Yao, J.; Pang, F.; Ma, T.; et al. An Internet-Based Survey of Influenza Vaccination Coverage in Healthcare Workers in China, 2018/2019 Season. Vaccines 2019, 8, E6. [Google Scholar] [CrossRef]
- Yi, H.; Yang, Y.; Zhang, L.; Zhang, M.; Wang, Q.; Zhang, T.; Zhang, Y.; Qin, Y.; Peng, Z.; Leng, Z.; et al. Improved influenza vaccination coverage among health-care workers: Evidence from a web-based survey in China, 2019/2020 season. Hum. Vaccines Immunother. 2021, 17, 2185–2189. [Google Scholar] [CrossRef] [PubMed]
- Salgado, C.D.; Giannetta, E.T.; Hayden, F.G.; Farr, B.M. Preventing nosocomial influenza by improving the vaccine acceptance rate of clinicians. Infect. Control Hosp. Epidemiol. 2004, 25, 923–928. [Google Scholar] [CrossRef]
- Alame, M.; Kaddoura, M.; Kharroubi, S.; Ezzeddine, F.; Hassan, G.; Diab El-Harakeh, M.; Al Ariqi, L.; Abubaker, A.; Zaraket, H. Uptake rates, knowledge, attitudes, and practices toward seasonal influenza vaccination among healthcare workers in Lebanon. Hum. Vaccines Immunother. 2021, 17, 4623–4631. [Google Scholar] [CrossRef] [PubMed]
- Van Buynder, P.G.; Konrad, S.; Kersteins, F.; Preston, E.; Brown, P.D.; Keen, D.; Murray, N.J. Healthcare worker influenza immunization vaccinate or mask policy: Strategies for cost effective implementation and subsequent reductions in staff absenteeism due to illness. Vaccine 2015, 33, 1625–1628. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control. Seasonal Influenza Vaccination and Antiviral use in EU/EEA Member States—Overview of Vaccine Recommendations for 2017–2018 and Vaccination Coverage Rates for 2015–2016 and 2016–2017 Influenza Seasons; ECDC: Stockholm, Sweden, 2018; p. 45.
- Leone Roberti Maggiore, U.; Scala, C.; Toletone, A.; Debarbieri, N.; Perria, M.; D’Amico, B.; Montecucco, A.; Martini, M.; Dini, G.; Durando, P. Susceptibility to vaccine-preventable diseases and vaccination adherence among healthcare workers in Italy: A cross-sectional survey at a regional acute-care university hospital and a systematic review. Hum. Vaccines Immunother. 2017, 13, 470–476. [Google Scholar] [CrossRef]
- La Torre, G.; Mannocci, A.; Ursillo, P.; Bontempi, C.; Firenze, A.; Panico, M.G.; Sferrazza, A.; Ronga, C.; D’Anna, A.; Amodio, E.; et al. Prevalence of influenza vaccination among nurses and ancillary workers in Italy: Systematic review and meta analysis. Hum. Vaccines 2011, 7, 728–733. [Google Scholar] [CrossRef] [PubMed]
- Cherian, T.; Morales, K.F.; Mantel, C.; Lambach, P. Independent Expert Advisory Group (IEAG) for Health Worker Influenza Vaccination Factors and considerations for establishing and improving seasonal influenza vaccination of health workers: Report from a WHO meeting, January 16–17, Berlin, Germany. Vaccine 2019, 37, 6255–6261. [Google Scholar] [CrossRef] [PubMed]
- Saro-Buendía, M.; Marrero-Sánchez, Á.; García-Ruiz de Morales, D.; Chiara-Graciani, G.; Coderch-Carretero, J.; Pérez-Jacoiste Asín, M.A.; Silva, J.T.; Fernández-Ruiz, M.; Arrazola, P.; Aguado, J.M.; et al. Implementation of a program to improve influenza vaccination rates among medical students: A comparative study involving two university affiliated hospitals. Hum. Vaccines Immunother. 2021, 17, 3662–3669. [Google Scholar] [CrossRef]
- Machowicz, R.; Wyszomirski, T.; Ciechanska, J.; Mahboobi, N.; Wnekowicz, E.; Obrowski, M.; Zycinska, K.; Zielonka, T.M. Knowledge, attitudes, and influenza vaccination of medical students in Warsaw, Strasbourg, and Teheran. Eur. J. Med. Res. 2010, 15 (Suppl. 2), 235–240. [Google Scholar] [CrossRef]
- Bishburg, E.; Shah, M.; Mathis, A.S. Influenza vaccination among medical residents in a teaching hospital. Infect. Control Hosp. Epidemiol. 2008, 29, 89–91. [Google Scholar] [CrossRef]
- Mir, O.; Adam, J.; Gaillard, R.; Gregory, T.; Veyrie, N.; Yordanov, Y.; Berveiller, P.; Chousterman, B.; Loulergue, P. Vaccination coverage among medical residents in Paris, France. Clin. Microbiol. Infect. 2012, 18, E137–E139. [Google Scholar] [CrossRef][Green Version]
- Ministero della Salute Piano Nazionale Prevenzione Vaccinale. PNPV 2017-2019; Ministero della Salute: Rome, Itlay, 2017; p. 90.
- Mavros, M.N.; Mitsikostas, P.K.; Kontopidis, I.G.; Moris, D.N.; Dimopoulos, G.; Falagas, M.E. H1N1v influenza vaccine in Greek medical students. Eur. J. Public Health 2011, 21, 329–332. [Google Scholar] [CrossRef] [PubMed]
- Ryan, K.A.; Filipp, S.L.; Gurka, M.J.; Zirulnik, A.; Thompson, L.A. Understanding influenza vaccine perspectives and hesitancy in university students to promote increased vaccine uptake. Heliyon 2019, 5, e02604. [Google Scholar] [CrossRef] [PubMed]
- Barbara, A.; Mariani, M.; De Waure, C.; Anzelmo, V.; Piccoli, B.; Cambieri, A.; Damiani, G.; Ricciardi, W.; Laurenti, P. A campaign aimed at increasing seasonal influenza vaccination coverage among post graduate medical residents in an Italian teaching hospital. Hum. Vaccines Immunother. 2019, 15, 967–972. [Google Scholar] [CrossRef]
- Costantino, C.; Mazzucco, W.; Azzolini, E.; Baldini, C.; Bergomi, M.; Biafiore, A.D.; Bianco, M.; Borsari, L.; Cacciari, P.; Cadeddu, C.; et al. Influenza vaccination coverage among medical residents: An Italian multicenter survey. Hum. Vaccines Immunother. 2014, 10, 1204–1210. [Google Scholar] [CrossRef]
- Karafillakis, E.; Dinca, I.; Apfel, F.; Cecconi, S.; Wűrz, A.; Takacs, J.; Suk, J.; Celentano, L.P.; Kramarz, P.; Larson, H.J. Vaccine hesitancy among healthcare workers in Europe: A qualitative study. Vaccine 2016, 34, 5013–5020. [Google Scholar] [CrossRef] [PubMed]
- Hollmeyer, H.; Hayden, F.; Mounts, A.; Buchholz, U. Review: Interventions to increase influenza vaccination among healthcare workers in hospitals. Influenza Other Respir. Viruses 2013, 7, 604–621. [Google Scholar] [CrossRef] [PubMed]
- Wicker, S. Unvaccinated health care workers must wear masks during flu season-a possibility to improve influenza vaccination rates? Vaccine 2009, 27, 2631–2632. [Google Scholar] [CrossRef]
- Lytras, T.; Kopsachilis, F.; Mouratidou, E.; Papamichail, D.; Bonovas, S. Interventions to increase seasonal influenza vaccine coverage in healthcare workers: A systematic review and meta-regression analysis. Hum. Vaccines Immunother. 2016, 12, 671–681. [Google Scholar] [CrossRef] [PubMed]
- Finch, M. Point: Mandatory influenza vaccination for all heath care workers? Seven reasons to say “no.” Clin. Infect. Dis 2006, 42, 1141–1143. [Google Scholar] [CrossRef]
- Isaacs, D.; Leask, J. Should influenza immunisation be mandatory for healthcare workers? No. BMJ 2008, 337, a2140. [Google Scholar] [CrossRef] [PubMed]
- Perrone, P.M.; Biganzoli, G.; Lecce, M.; Campagnoli, E.M.; Castrofino, A.; Cinnirella, A.; Fornaro, F.; Gallana, C.; Grosso, F.M.; Maffeo, M.; et al. Influenza Vaccination Campaign during the COVID-19 Pandemic: The Experience of a Research and Teaching Hospital in Milan. Int. J. Environ. Res. Public Health 2021, 18, 5874. [Google Scholar] [CrossRef]
- Grech, V.; Borg, M. Influenza vaccination in the COVID-19 era. Early Hum. Dev. 2020, 148, 105116. [Google Scholar] [CrossRef] [PubMed]
- Chittano Congedo, E.; Paladino, M.E.; Riva, M.A.; Belingheri, M. Adherence, Perception of, and Attitude toward Influenza and Flu Vaccination: A Cross-Sectional Study among a Population of Future Healthcare Workers. Int. J. Environ. Res. Public Health 2021, 18, 13086. [Google Scholar] [CrossRef]
- Robbins, T.; Berry, L.; Wells, F.; Randeva, H.; Laird, S. Healthcare staff perceptions towards influenza and potential COVID-19 vaccination in the 2020 pandemic context. J. Hosp. Infect. 2021, 112, 45–48. [Google Scholar] [CrossRef] [PubMed]
- Iacobucci, G. Covid-19: Risk of death more than doubled in people who also had flu, English data show. BMJ 2020, 370, m3720. [Google Scholar] [CrossRef] [PubMed]
- Gianino, M.M.; Savatteri, A.; Politano, G.; Nurchis, M.C.; Pascucci, D.; Damiani, G. Burden of COVID-19: Disability-Adjusted Life Years (DALYs) across 16 European countries. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 5529–5541. [Google Scholar] [CrossRef] [PubMed]
- Stöckeler, A.-M.; Schuster, P.; Zimmermann, M.; Hanses, F. Influenza vaccination coverage among emergency department personnel is associated with perception of vaccination and side effects, vaccination availability on site and the COVID-19 pandemic. PLoS ONE 2021, 16, e0260213. [Google Scholar] [CrossRef] [PubMed]
- Bertoni, L.; Roncadori, A.; Gentili, N.; Danesi, V.; Massa, I.; Nanni, O.; Altini, M.; Gabutti, G.; Montella, M.T. How has COVID-19 pandemic changed flu vaccination attitudes among an Italian cancer center healthcare workers? Hum. Vaccines Immunother. 2022, 18, 1978795. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Wong, E.L.Y.; Ho, K.F.; Cheung, A.W.L.; Chan, E.Y.Y.; Yeoh, E.K.; Wong, S.Y.S. Intention of nurses to accept coronavirus disease 2019 vaccination and change of intention to accept seasonal influenza vaccination during the coronavirus disease 2019 pandemic: A cross-sectional survey. Vaccine 2020, 38, 7049–7056. [Google Scholar] [CrossRef]
- Di Pumpo, M.; Vetrugno, G.; Pascucci, D.; Carini, E.; Beccia, V.; Sguera, A.; Zega, M.; Pani, M.; Cambieri, A.; Nurchis, M.C.; et al. Is COVID-19 a Real Incentive for Flu Vaccination? Let the Numbers Speak for Themselves. Vaccines 2021, 9, 276. [Google Scholar] [CrossRef]
- Hosmer, D.W.; Lemeshow, S.; Klar, J. Goodness-of-Fit Testing for the Logistic Regression Model when the Estimated Probabilities are Small. Biom. J. 1988, 30, 911–924. [Google Scholar] [CrossRef]
- Walsh, S.J. Goodness-of-fit Issues in ROC Curve Estimation. Med. Decis. Mak. 1999, 19, 193–201. [Google Scholar] [CrossRef] [PubMed]
- Veljkovic, M.; Loncarevic, G.; Kanazir, M.; Kisic-Tepavcevic, D.; Gazibara, T. Trend in mandatory immunisation coverage: Linear and joinpoint regression approach, Serbia, 2000 to 2017. Euro. Surveill. 2021, 26, 2000417. [Google Scholar] [CrossRef] [PubMed]
- Amato, M.; Werba, J.P.; Frigerio, B.; Coggi, D.; Sansaro, D.; Ravani, A.; Ferrante, P.; Veglia, F.; Tremoli, E.; Baldassarre, D. Relationship between Influenza Vaccination Coverage Rate and COVID-19 Outbreak: An Italian Ecological Study. Vaccines 2020, 8, E535. [Google Scholar] [CrossRef]
- Public Health England Seasonal Flu Vaccine Uptake in Healthcare Workers: Monthly Data, 2020 to 2021. Available online: https://www.gov.uk/government/statistics/seasonal-flu-vaccine-uptake-in-healthcare-workers-monthly-data-2020-to-2021 (accessed on 16 April 2022).
- Public Health England Seasonal Flu and COVID-19 Vaccine Uptake in Frontline Healthcare Workers: Monthly Data, 2021 to 2022. Available online: https://www.gov.uk/government/statistics/seasonal-flu-and-covid-19-vaccine-uptake-in-frontline-healthcare-workers-monthly-data-2021-to-2022 (accessed on 16 April 2022).
- Domnich, A.; Orsi, A.; Trombetta, C.-S.; Guarona, G.; Panatto, D.; Icardi, G. COVID-19 and Seasonal Influenza Vaccination: Cross-Protection, Co-Administration, Combination Vaccines, and Hesitancy. Pharmaceuticals 2022, 15, 322. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, R.; Baos, S.; Cappel-Porter, H.; Carson-Stevens, A.; Clout, M.; Culliford, L.; Emmett, S.R.; Garstang, J.; Gbadamoshi, L.; Hallis, B.; et al. Safety and immunogenicity of concomitant administration of COVID-19 vaccines (ChAdOx1 or BNT162b2) with seasonal influenza vaccines in adults in the UK (ComFluCOV): A multicentre, randomised, controlled, phase 4 trial. Lancet 2021, 398, 2277–2287. [Google Scholar] [CrossRef]
- Jędrzejek, M.J.; Mastalerz-Migas, A. Influenza Vaccination Coverage, Motivators for, and Barriers to Influenza Vaccination among Healthcare Workers in Wroclaw, Poland. Int. J. Environ. Res. Public Health 2022, 19, 1586. [Google Scholar] [CrossRef]
- Nutman, A.; Yoeli, N. Influenza vaccination motivators among healthcare personnel in a large acute care hospital in Israel. Isr. J. Health Policy Res. 2016, 5, 52. [Google Scholar] [CrossRef]
- Christini, A.B.; Shutt, K.A.; Byers, K.E. Influenza vaccination rates and motivators among healthcare worker groups. Infect. Control Hosp. Epidemiol. 2007, 28, 171–177. [Google Scholar] [CrossRef]
- Wicker, S.; Rabenau, H.F.; Doerr, H.W.; Allwinn, R. Influenza Vaccination Compliance Among Health Care Workers in a German University Hospital. Infection 2009, 37, 197–202. [Google Scholar] [CrossRef]
- Abramson, Z.H.; Levi, O. Influenza vaccination among primary healthcare workers. Vaccine 2008, 26, 2482–2489. [Google Scholar] [CrossRef]
- Awadalla, N.J.; Al-Musa, H.M.; Al-Musa, K.M.; Asiri, A.M.; Albariqi, A.A.; Majrashi, H.M.; Alasim, A.A.; Almuslah, A.S.; Alshehri, T.K.; AlFlan, M.A.; et al. Seasonal influenza vaccination among primary health care workers in Southwestern Saudi Arabia. Hum. Vaccines Immunother. 2020, 16, 321–326. [Google Scholar] [CrossRef] [PubMed]
- Pless, A.; McLennan, S.R.; Nicca, D.; Shaw, D.M.; Elger, B.S. Reasons why nurses decline influenza vaccination: A qualitative study. BMC Nurs. 2017, 16, 20. [Google Scholar] [CrossRef] [PubMed]
- Honda, H.; Sato, Y.; Yamazaki, A.; Padival, S.; Kumagai, A.; Babcock, H. A successful strategy for increasing the influenza vaccination rate of healthcare workers without a mandatory policy outside of the United States: A multifaceted intervention in a Japanese tertiary care center. Infect. Control Hosp. Epidemiol. 2013, 34, 1194–1200. [Google Scholar] [CrossRef]
- Honda, H.; Padival, S.; Shimamura, Y.; Babcock, H.M. Changes in influenza vaccination rates among healthcare workers following a pandemic influenza year at a Japanese tertiary care centre. J. Hosp. Infect. 2012, 80, 316–320. [Google Scholar] [CrossRef] [PubMed]
- Barbara, A.; La Milia, D.I.; Di Pumpo, M.; Tognetto, A.; Tamburrano, A.; Vallone, D.; Viora, C.; Cavalieri, S.; Cambieri, A.; Moscato, U.; et al. Strategies to Increase Flu Vaccination Coverage among Healthcare Workers: A 4 Years Study in a Large Italian Teaching Hospital. Vaccines 2020, 8, E85. [Google Scholar] [CrossRef]
- Tognetto, A.; Zorzoli, E.; Franco, E.; Gervasi, G.; Paglione, L.; Di Ninno, F.; De Soccio, P.; Barbara, A.; Orsi, G.B.; De Vito, C.; et al. Seasonal influenza vaccination among health-care workers: The impact of different tailored programs in four University hospitals in Rome. Hum. Vaccines Immunother. 2020, 16, 81–85. [Google Scholar] [CrossRef] [PubMed]
- Seale, H. The COVID-19 pandemic momentum: Can it be used to support improvements in healthcare worker influenza vaccination? Expert Rev. Vaccines 2021, 20, 919–920. [Google Scholar] [CrossRef] [PubMed]
- Van Buynder, P.G.; Newbound, A.; MacIntyre, C.R.; Kennedy, A.T.; Clarke, C.; Anderson, J. Australian experience of the SH21 flu vaccination program during the COVID-19 vaccine program. Hum. Vaccines Immunother. 2021, 17, 4611–4616. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).