The Health Belief Model Applied to COVID-19 Vaccine Hesitancy: A Systematic Review
Abstract
:1. Introduction
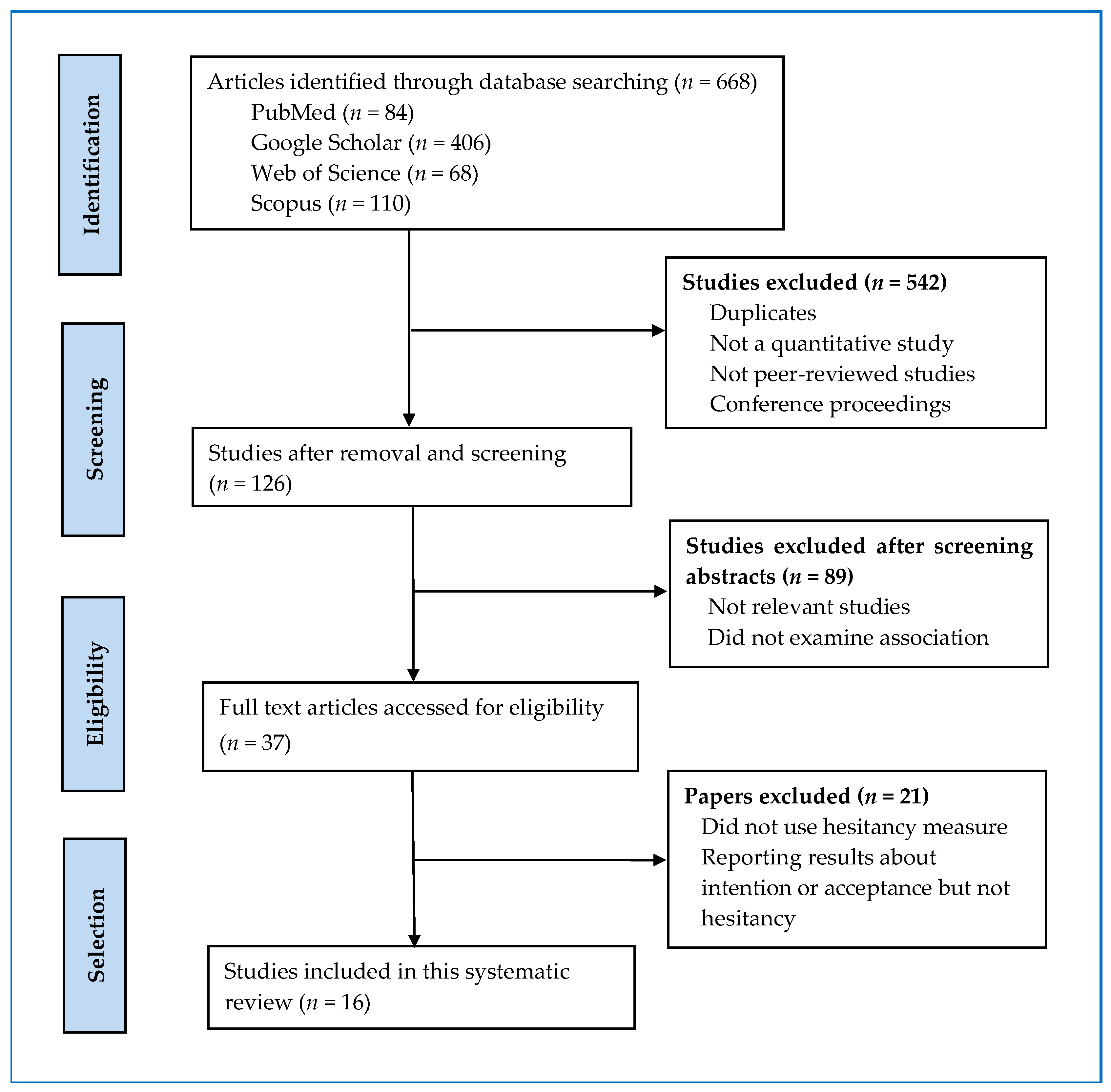
2. Methodology
2.1. Criteria for Inclusion and Exclusion
2.2. Search Strategy
2.3. Data Extraction and Analysis
3. Results
3.1. Characteristics of the Included Studies
3.2. Vaccination Hesitancy Rate
3.3. HBM Constructs Associated with Vaccine Hesitancy
3.4. Modifying HBM Constructs Associated with Vaccine Hesitancy
4. Discussion and Implications
5. Limitations and Future Research
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard. Available online: https://covid19.who.int (accessed on 30 December 2020).
- Kashte, S.; Gulbake, A.; El-Amin, S.F., III; Gupta, A. COVID-19 vaccines: Rapid development, implications, challenges and future prospects. Hum. Cell 2021, 34, 711–733. [Google Scholar] [CrossRef] [PubMed]
- Idris, I.O.; Ayeni, G.O.; Adebisi, Y.A. Why many African countries may not achieve the 2022 COVID-19 vaccination coverage target. Trop. Med. Health 2022, 50, 15. [Google Scholar] [CrossRef] [PubMed]
- Morens, D.M.; Folkers, G.K.; Fauci, A.S. The Concept of Classical Herd Immunity May Not Apply to COVID-19. J. Infect. Dis. 2022, jiac109. [Google Scholar] [CrossRef]
- CDC. Centers for Disease Control and Prevention. COVID Data Tracker. Atlanta, GA: US Department of Health and Human Services; 2022. Available online: https://covid.cdc.gov/covid-data-tracker (accessed on 10 February 2022).
- Guillon, M.; Kergall, P. Factors associated with COVID-19 vaccination intentions and attitudes in France. Public Health 2021, 198, 200–207. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, N.E.; Sage Working Group on Vaccine Hesitancy. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161. [Google Scholar] [CrossRef] [PubMed]
- Rosenstock, I. The health belief model and nutrition education. J. Can. Diet. Assoc. 1982, 43, 184–192. [Google Scholar]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009, 62, e1–e34. [Google Scholar] [CrossRef] [Green Version]
- Badr, H.; Zhang, X.; Oluyomi, A.; Woodard, L.D.; Adepoju, O.E.; Raza, S.A.; Amos, C.I. Overcoming COVID-19 Vaccine Hesitancy: Insights from an Online Population-Based Survey in the United States. Vaccines 2021, 9, 1100. [Google Scholar] [CrossRef]
- Chen, H.; Li, X.; Gao, J.; Liu, X.; Mao, Y.; Wang, R.; Zheng, P.; Xiao, Q.; Jia, Y.; Fu, H.; et al. Health Belief Model Perspective on the Control of COVID-19 Vaccine Hesitancy and the Promotion of Vaccination in China: Web-Based Cross-sectional Study. J. Med. Internet Res. 2021, 23, e29329. [Google Scholar] [CrossRef]
- Du, M.; Tao, L.; Liu, J. The Association Between Risk Perception and COVID-19 Vaccine Hesitancy for Children Among Reproductive Women in China: An Online Survey. Front. Med. 2021, 8, 1494. [Google Scholar] [CrossRef]
- Griva, K.; Tan, K.Y.K.; Chan, F.H.F.; Periakaruppan, R.; Ong, B.W.L.; Soh, A.S.E.; Chen, M.I. Evaluating Rates and Determinants of COVID-19 Vaccine Hesitancy for Adults and Children in the Singapore Population: Strengthening Our Community’s Resilience against Threats from Emerging Infections (SOCRATEs) Cohort. Vaccines 2021, 9, 1415. [Google Scholar] [CrossRef] [PubMed]
- Hosek, M.G.; Chidester, A.B.; Gelfond, J.; Taylor, B.S. Low Prevalence of COVID-19 Vaccine Hesitancy in Students Across Health Science Disciplines in Texas. Vaccine X 2022, 10, 100154. [Google Scholar] [CrossRef] [PubMed]
- Hossain, M.B.; Alam, M.Z.; Islam, M.S.; Sultan, S.; Faysal, M.M.; Rima, S.; Hossain, M.A.; Mamun, A.A. COVID-19 vaccine hesitancy among the adult population in Bangladesh: A nationwide cross-sectional survey. PLoS ONE 2021, 16, e0260821. [Google Scholar] [CrossRef] [PubMed]
- Hossain, M.B.; Alam, M.Z.; Islam, M.S.; Sultan, S.; Faysal, M.M.; Rima, S.; Hossain, M.A.; Mamun, A.A. Health belief model, theory of planned behavior, or psychological antecedents: What predicts COVID-19 vaccine hesitancy better among the Bangladeshi adults? Front. Public Health 2021, 9, 1172. [Google Scholar] [CrossRef]
- Huynh, G.; Nguyen, H.T.N.; Van Tran, K.; Le An, P.; Tran, T.D. Determinants of COVID-19 vaccine hesitancy among parents in Ho Chi Minh City, Vietnam. Postgrad. Med. 2022, 134, 303–308. [Google Scholar] [CrossRef]
- Jain, J.; Saurabh, S.; Kumar, P.; Verma, M.K.; Goel, A.D.; Gupta, M.K.; Bhardwaj, P.; Raghav, P.R. COVID-19 vaccine hesitancy among medical students in India. Epidemiol. Infect. 2021, 149, E132. [Google Scholar] [CrossRef]
- Le, C.N.; Nguyen, U.T.T.; Do, D.T.H. Predictors of COVID-19 vaccine acceptability among health professions students in Vietnam. BMC Public Health 2022, 22, 854. [Google Scholar] [CrossRef]
- Lee, M.; You, M. Direct and Indirect Associations of Media Use With COVID-19 Vaccine Hesitancy in South Korea: Cross-sectional Web-Based Survey. J. Med. Internet Res. 2022, 24, e32329. [Google Scholar] [CrossRef]
- Rehati, P.; Amaerjiang, N.; Yang, L.; Xiao, H.; Li, M.; Zunong, J.; Wang, L.; Vermund, S.H.; Hu, Y. COVID-19 Vaccine Hesitancy among Adolescents: Cross-Sectional School Survey in Four Chinese Cities Prior to Vaccine Availability. Vaccines 2022, 10, 452. [Google Scholar] [CrossRef]
- Toth-Manikowski, S.M.; Swirsky, E.S.; Gandhi, R.; Piscitello, G. COVID-19 vaccination hesitancy among health care workers, communication, and policy-making. Am. J. Infect. Control 2021, 50, 20–25. [Google Scholar] [CrossRef]
- Walsh, J.C.; Comar, M.; Folan, J.; Williams, S.; Kola-Palmer, S. The psychological and behavioural correlates of COVID-19 vaccine hesitancy and resistance in Ireland and the UK. Acta Psychol. 2022, 225, 103550. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Duan, L.; Li, M.; Wang, J.; Yang, J.; Song, C.; Li, J.; Wang, J.; Jia, J.; Xu, J. COVID-19 Vaccine Hesitancy and Associated Factors among Diabetes Patients: A Cross-Sectional Survey in Changzhi, Shanxi, China. Vaccines 2022, 10, 129. [Google Scholar] [CrossRef] [PubMed]
- Rosenstock, I. Historical Origins of the Health Belief Model. Health Educ. Monogr. 1974, 2, 328–335. [Google Scholar] [CrossRef]
- Wiysonge, C.S.; Ndwandwe, D.; Ryan, J.; Jaca, A.; Batouré, O.; Anya, B.P.; Cooper, S. Vaccine hesitancy in the era of COVID-19: Could lessons from the past help in divining the future? Hum. Vaccines Immunother. 2022, 18, 1–3. [Google Scholar] [CrossRef]
- Brewer, N.T.; Fazekas, K.I. Predictors of HPV vaccine acceptability: A theory-informed, systematic review. Prev. Med. 2007, 45, 107–114. [Google Scholar] [CrossRef] [PubMed]
- Yarbrough, S.S.; Braden, C.J. Utility of health belief model as a guide for explaining or predicting breast cancer screening behaviours. J. Adv. Nurs. 2001, 33, 677–688. [Google Scholar] [CrossRef] [PubMed]
- Reisi, M.; Javadzade, S.H.; Shahnazi, H.; Sharifirad, G.; Charkazi, A.; Moodi, M. Factors affecting cigarette smoking based on health-belief model structures in pre-university students in Isfahan, Iran. J. Educ. Health Promot. 2014, 3, 23. [Google Scholar] [CrossRef] [Green Version]
- Murphy, J.; Vallières, F.; Bentall, R.P.; Shevlin, M.; McBride, O.; Hartman, T.K.; McKay, R.; Bennett, K.; Mason, L.; Gibson-Miller, J.; et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat. Commun. 2021, 12, 29. [Google Scholar] [CrossRef]
- Pomares, T.D.; Buttenheim, A.M.; Amin, A.B.; Joyce, C.M.; Porter, R.M.; Bednarczyk, R.A.; Omer, S.B. Association of cognitive biases with human papillomavirus vaccine hesitancy: A cross-sectional study. Hum. Vaccines Immunother. 2019, 16, 1018–1023. [Google Scholar] [CrossRef]
- Browne, M.; Thomson, P.; Rockloff, M.J.; Pennycook, G. Going against the Herd: Psychological and Cultural Factors Underlying the ‘Vaccination Confidence Gap’. PLoS ONE 2015, 10, e0132562. [Google Scholar] [CrossRef] [Green Version]
- Hornsey, M.J.; Harris, E.A.; Fielding, K.S. The psychological roots of anti-vaccination attitudes: A 24-nation investigation. Health Psychol. 2018, 37, 307–315. [Google Scholar] [CrossRef] [PubMed]
| Search | Search Terms (Boolean Operators) |
|---|---|
| 1 | “health belief model” AND “vaccination hesitancy” AND “COVID-19” |
| 2 | “health belief model” AND “vaccination hesitancy” AND “coronavirus” |
| 3 | “health belief model” AND “vaccination hesitancy” AND “SARS-CoV-2” |
| 4 | “health belief model” AND “vaccine hesitancy” OR “vaccine hesitant”AND “COVID-19” “coronavirus” “SARS-CoV-2” |
| 5 | “health belief model” AND “booster” AND “COVID-19” “coronavirus” “SARS-CoV-2” |
| Authors | Year of Publication | Journal | Country | Vaccine Hesitancy % | Sample | N |
|---|---|---|---|---|---|---|
| Guillon and Kergall [6] | 2021 | Public Health | France | 60.6 | adult general population | 1146 |
| Badr et al. [10] | 2021 | Vaccines | USA | 43.5 | adult general population | 1208 |
| Chen et al. [11] | 2021 | Journal of Medical Internet Research | China | 44.3 | adult general population | 2531 |
| Du et al. [12] | 2021 | Frontiers in Medicine | China | 8.44 | reproductive women | 3011 |
| Griva et al. [13] | 2021 | Vaccines | Singapore | 9.9 | adult general population | 1623 |
| Hosek et al. [14] | 2022 | Vaccines | USA | 19.4 | students | 1030 |
| Hossain et al. [15] | 2021a | PLoS ONE | Bangladesh | 46.2 | adult general population | 1497 |
| Hossain et al. [16] | 2021b | Frontiers in Public Health | Bangladesh | 41.1 | adult general population | 1497 |
| Huynh et al. [17] | 2022 | Postgraduate Medicine | Vietnam | 26.2 | parents | 1015 |
| Jain et al. [18] | 2021 | Epidemiology and Infection | India | 10.6 | students | 1068 |
| Le et al. [19] | 2022 | BMC Public Health | Vietnam | 40.4 | students | 911 |
| Lee and You [20] | 2022 | Journal of Medical Internet Research | South Korea | 53.3 | adult general population | 1016 |
| Rehati et al. [21] | 2022 | Vaccines | China | 31.6 | students | 9153 |
| Toth-Manikowski et al. [22] | 2022 | American Journal of Infection Control | USA | 15 | health care workers | 1974 |
| Walsh et al. [23] | 2022 | Acta Psychologica | Ireland, UK | 24.75 | adult general population | 1079 |
| Wang et al. [24] | 2022 | Vaccines | China | 56.4 | patients | 483 |
| = 33.23, SD = 17.35 | = 1890.13, SD = 2039.1 |
| Authors and Year | Perceived Susceptibility | Perceived Severity | Perceived Benefits | Perceived Barriers | Cues to Action | Self Efficacy | Modifying Variables |
|---|---|---|---|---|---|---|---|
| Guillon and Kergall [6] | × (−) | × (+) | × (−) | Female (+) | |||
| Badr et al. [10] | × (−) | × (−) | Female (+) Higher Income (−) Unemployment (+) Marital status (−) Individuals who perceived vaccination as being convenient (−) | ||||
| Chen et al. [11] | × (+) | × (−) | × (+) | × (−) | × (−) | Female (+) Higher income (+) Health status: Poor self-rated health (+) Occupation: Non-medical personnel (+) | |
| Du et al. [12] | × (−) | × (−) | × (+) | Female (+) Region: Eastern China (+) Older people (over 45 years) (+) Lower than high school education level (+) Low score on knowledge of COVID-19 (+) | |||
| Griva et al. [13] | × (−) | × (+) | Female (+) Male (+) parental vaccine hesitancy for children Employed respondents Aged 31 to 40 years old Income between $5000 and $12,999 Absence of chronic illnesses (+) Living with people in poor health (−) Subjective norm (−) Moral norm (−) Perceived personal necessity of vaccination (−) | ||||
| Hosek et al. [14] | × (−) | × (−) | Medical discipline History of COVID-19 infection (+) | ||||
| Hossain et al. [15] | × (−) | × (+) | Geographic region Knowledge about the vaccine (−) Vaccination process (−) Negative attitudes towards the vaccine (+) Conspiracy beliefs towards COVID-19 vaccine (+) Country of origin | ||||
| Hossain et al. [16] | × (−) | × (−) | × (−) | × (+) | × (−) | ||
| Huynh et al. [17] | × (−) | × (−) | × (−) | × (+) | × (−) | Knowledge of COVID-19 | |
| Jain et al. [18] | × (−) | × (−) | × (+) | Lack of awareness regarding their eligibility for COVID-19 vaccination (+) Lack of trust in government agencies (+) | |||
| Le et al. [19] | × (−) | × (+) | × (−) | History of flu vaccination (−), Nationality (Vietnamese vs. Cambodian and Lao) (+) Major (pharmacy vs. physiotherapy (+) | |||
| Lee and You [20] | × (−) | × (−) | × (+) | Female (+) Age in 50s and age over 60s (+) Lower trust in government (+) History of flu vaccination (−) Seeking COVID-19 vaccine-related information via social media (+) | |||
| Rehati et al. [21] | × (−) | × (−) | Female (+) Geographic region History of flu vaccination (−) Higher COVID-19 vaccine price concerns (+) Convenience to vaccinate (−) Doctors’ recommendation to vaccinate (−) Lack of knowledge of COVID-19 (+) | ||||
| Toth-Manikowski et al. [22] | × (−) | × (+) | × (−) | Age: Younger (+) Occupation: Non-physicians (+) Ethnicity: Black or African American (+) Political affiliation: Republican (+) Allergic to any vaccine component | |||
| Walsh et al. [23] | × (−), UK sample × (−), Irish sample | × (−), UK sample × (−), Irish sample | × (−), UK sample × (−), Irish sample | Women (+) Age under age 30 (+) Negative vaccination attitudes (+) Peer influence (−) Government influence (−) Civic responsibility (+) | |||
| Wang et al. [24] | × (−) | × (+) | × (−) | Education (High school) Disagreement with physicians’ view that vaccination can reduce SARS-CoV-2 infection risk (+) Disagreement with the statement that relatives’ vaccination status would influence participants’ vaccination decision (+) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Limbu, Y.B.; Gautam, R.K.; Pham, L. The Health Belief Model Applied to COVID-19 Vaccine Hesitancy: A Systematic Review. Vaccines 2022, 10, 973. https://doi.org/10.3390/vaccines10060973
Limbu YB, Gautam RK, Pham L. The Health Belief Model Applied to COVID-19 Vaccine Hesitancy: A Systematic Review. Vaccines. 2022; 10(6):973. https://doi.org/10.3390/vaccines10060973
Chicago/Turabian StyleLimbu, Yam B., Rajesh K. Gautam, and Long Pham. 2022. "The Health Belief Model Applied to COVID-19 Vaccine Hesitancy: A Systematic Review" Vaccines 10, no. 6: 973. https://doi.org/10.3390/vaccines10060973
APA StyleLimbu, Y. B., Gautam, R. K., & Pham, L. (2022). The Health Belief Model Applied to COVID-19 Vaccine Hesitancy: A Systematic Review. Vaccines, 10(6), 973. https://doi.org/10.3390/vaccines10060973






