Comparison of COVID-19 Resilience Index and Its Associated Factors across 29 Countries during the Delta and Omicron Variant Periods
Abstract
:1. Introduction
2. Materials and Methods
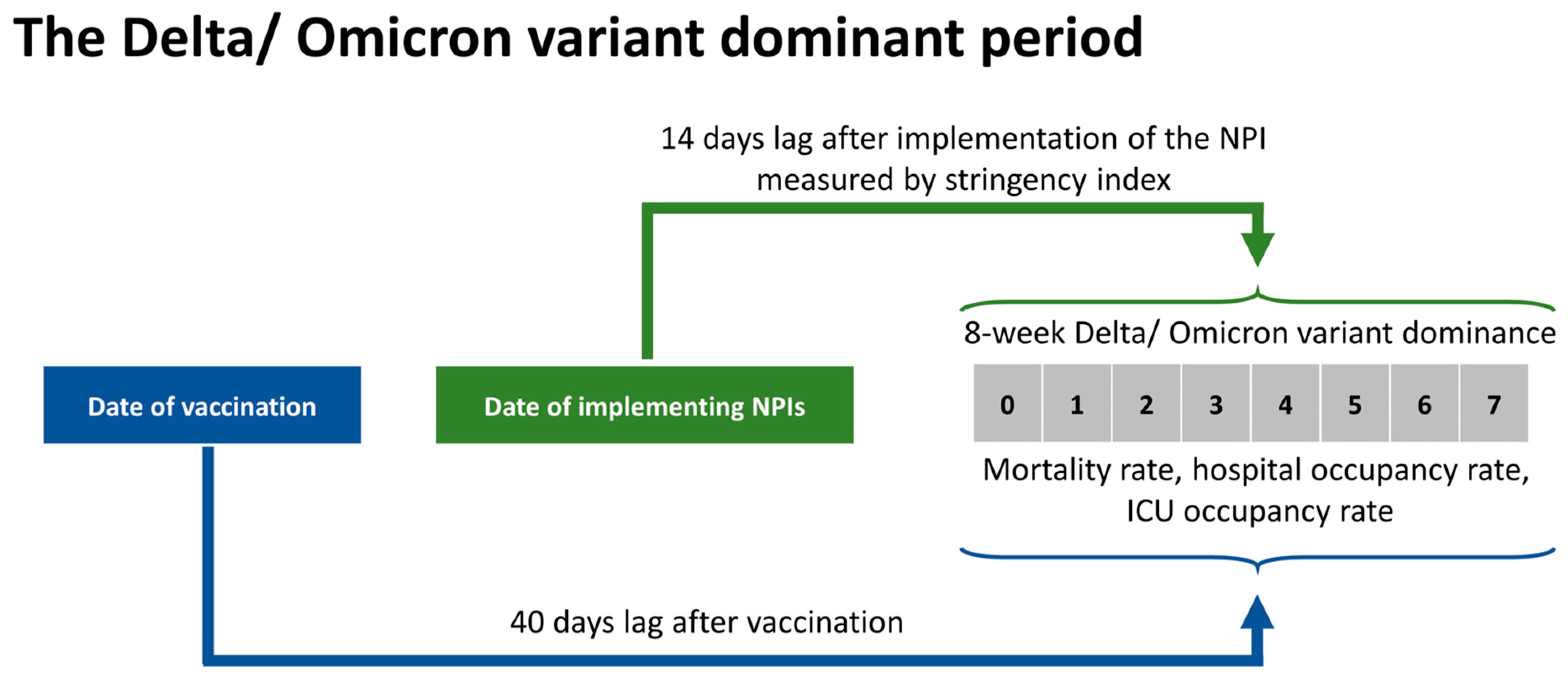
2.1. Study Design
2.2. Variables
- -
- COVID-19 interventions were measured by two indicators including stringency index and vaccine coverage. Stringency index measures the strictness of government response in terms of containment and closure policy [20]. We retrieved the vaccine data from the global vaccine databases, which consists of the percentage of population fully vaccinated, the percentage of population vaccinated with the booster dose [21].
- -
- Sociodemographic variables: population density, percentage of population living in urban areas, the percentage of population aged over 65 years, the GDP per capita. These data were extracted from World Bank indicators [22].
- -
- Government performance: government effectiveness index, government rule index, government quality index [22].
- -
- Population characteristics related to health: death rate of chronic diseases per 100,000 inhabitants, years lived with disability (YLD), health behavior and environment risks. Data were retrieved from the global burden of disease databases [23].
- -
2.3. Study Periods
2.4. Statistical Analysis
- -
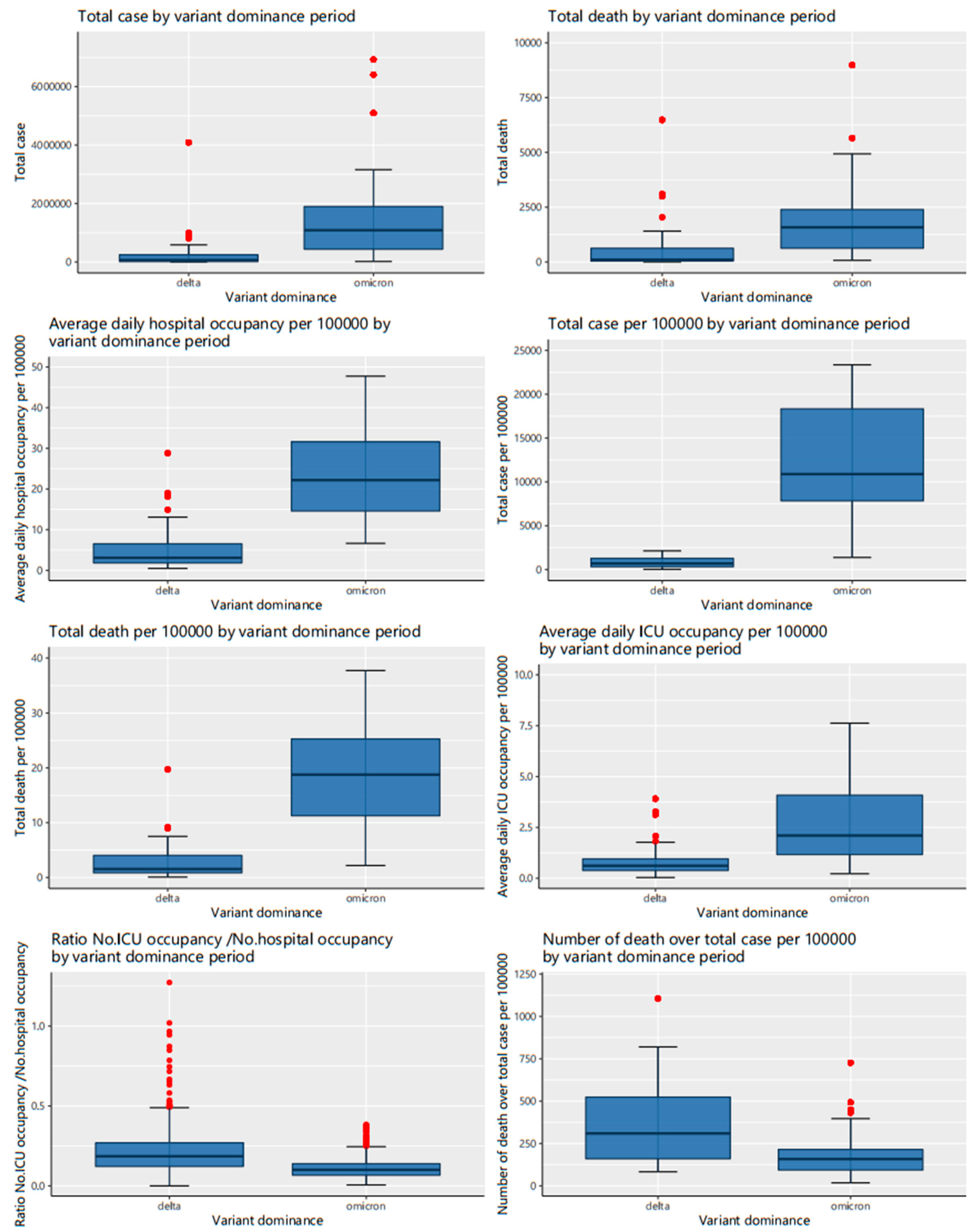
- Analysis of aggregate data of the 8-week Omicron period and the 8-week Delta period.
- -
- Longitudinal analysis
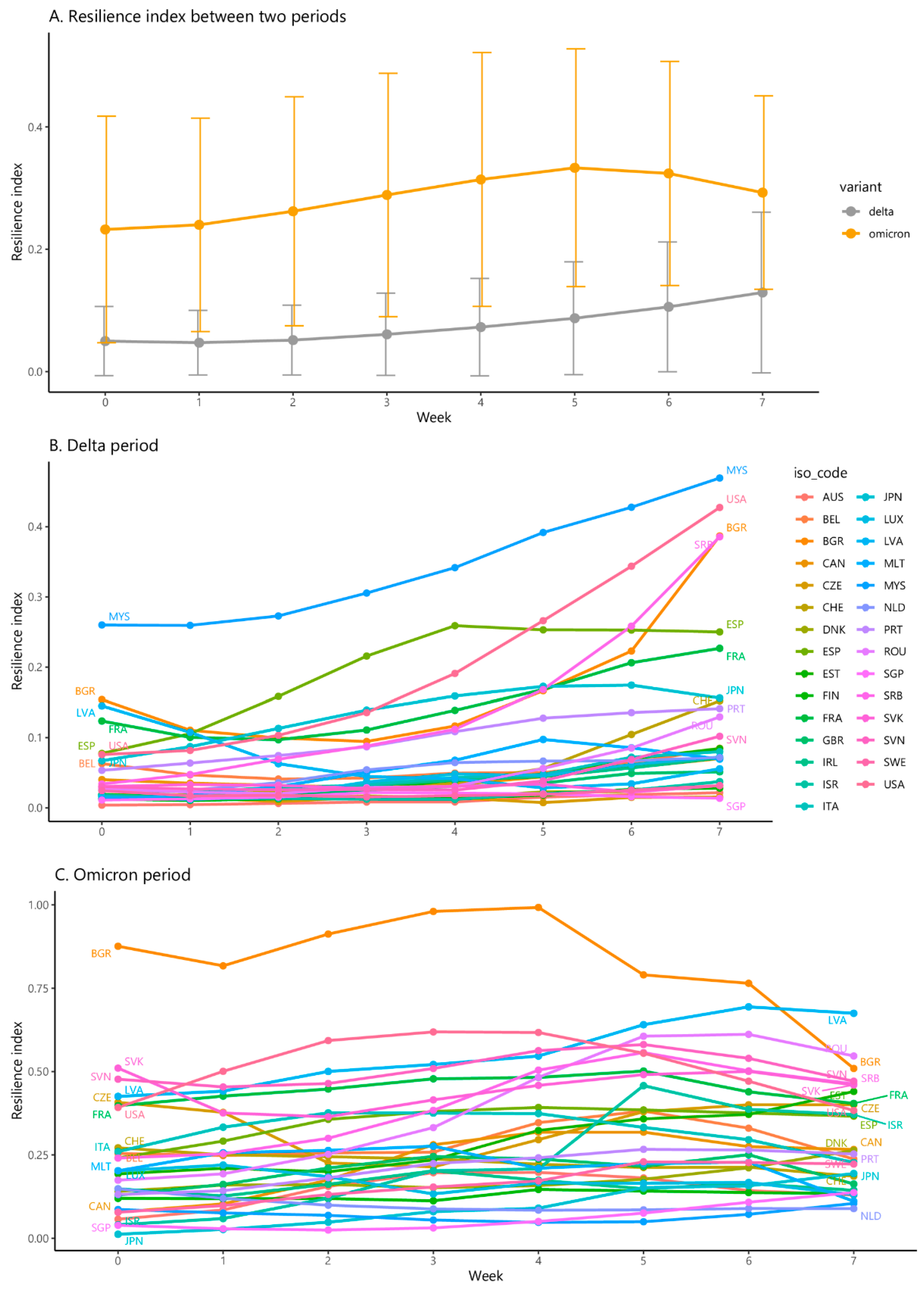
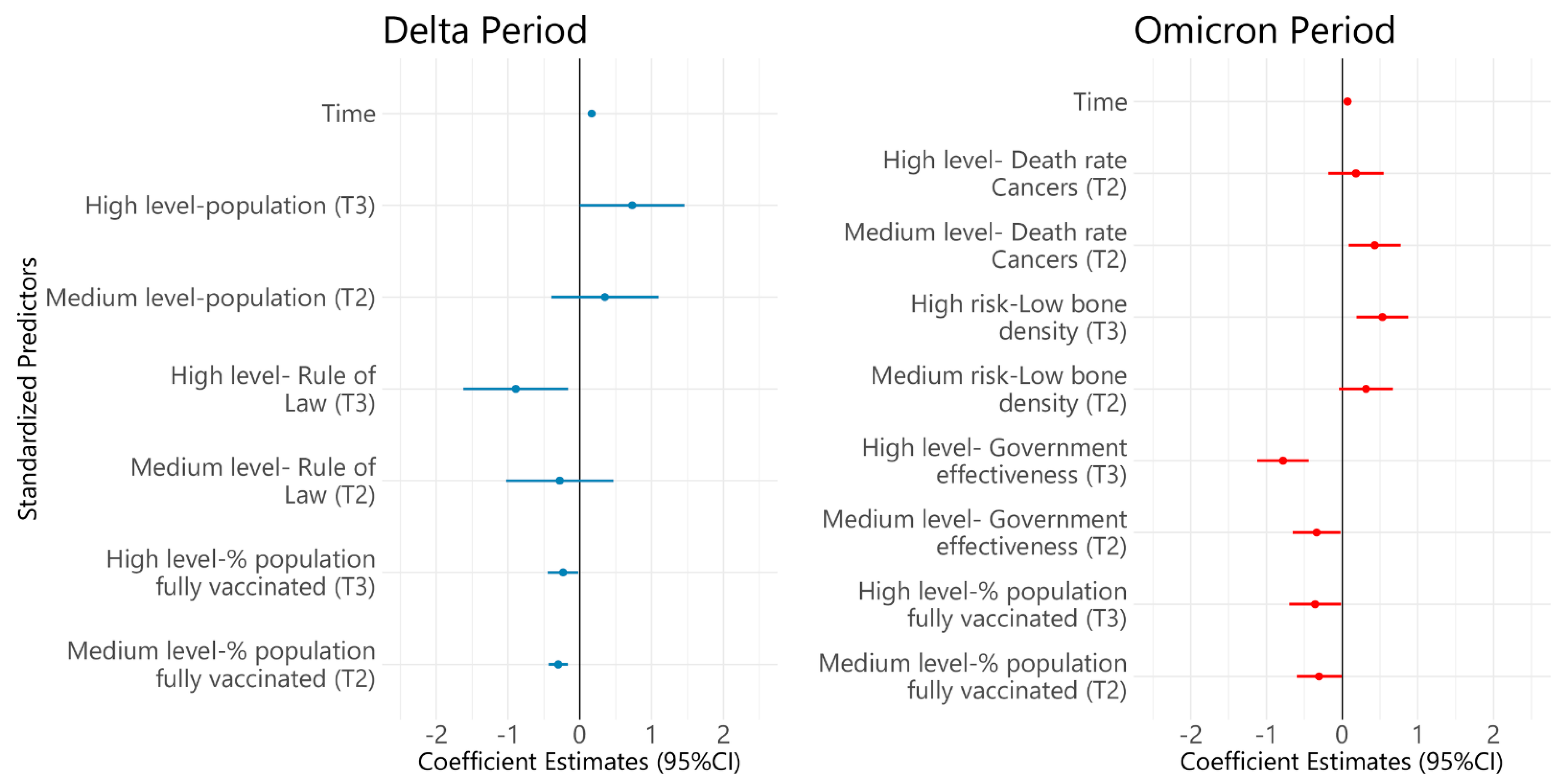
3. Results
Characteristics of Selected Countries
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Patel, M.D.; Rosenstrom, E.; Ivy, J.S.; Mayorga, M.E.; Keskinocak, P.; Boyce, R.M.; Hassmiller Lich, K.; Smith, R.L., III; Johnson, K.T.; Delamater, P.L.; et al. Association of Simulated COVID-19 Vaccination and Nonpharmaceutical Interventions with Infections, Hospitalizations, and Mortality. JAMA Netw. Open 2021, 4, e2110782. [Google Scholar] [CrossRef]
- Johns Hopkins Coronavirus Resource Center Pandemic Data Initiative. Available online: https://coronavirus.jhu.edu/pandemic-data-initiative (accessed on 19 May 2021).
- Lin, T.-Y.; Liao, S.-H.; Lai, C.-C.; Paci, E.; Chuang, S.-Y. Effectiveness of Non-Pharmaceutical Interventions and Vaccine for Containing the Spread of COVID-19: Three Illustrations before and after Vaccination Periods. J. Formos. Med. Assoc. 2021, 120 (Suppl. 1), S46–S56. [Google Scholar] [CrossRef] [PubMed]
- Jecker, N.S.; Au, D.K.S. Does Zero-COVID Neglect Health Disparities? J. Med. Ethics 2022, 48, 169–172. [Google Scholar] [CrossRef]
- Dyer, O. COVID-19: Omicron Is Causing More Infections but Fewer Hospital Admissions than Delta, South African Data Show. BMJ 2021, 375, n3104. [Google Scholar] [CrossRef]
- Karim, S.S.A.; Karim, Q.A. Omicron SARS-CoV-2 Variant: A New Chapter in the COVID-19 Pandemic. Lancet 2021, 398, 2126–2128. [Google Scholar] [CrossRef]
- Andrews, N.; Stowe, J.; Kirsebom, F.; Toffa, S.; Rickeard, T.; Gallagher, E.; Gower, C.; Kall, M.; Groves, N.; O’Connell, A.-M.; et al. COVID-19 Vaccine Effectiveness against the Omicron (B.1.1.529) Variant. N. Engl. J. Med. 2022, 386, 1532–1546. [Google Scholar] [CrossRef]
- Coccia, M. Preparedness of Countries to Face COVID-19 Pandemic Crisis: Strategic Positioning and Factors Supporting Effective Strategies of Prevention of Pandemic Threats. Environ. Res. 2022, 203, 111678. [Google Scholar] [CrossRef]
- Bo, Y.; Guo, C.; Lin, C.; Zeng, Y.; Li, H.B.; Zhang, Y.; Hossain, M.S.; Chan, J.W.M.; Yeung, D.W.; Kwok, K.O.; et al. Effectiveness of Non-Pharmaceutical Interventions on COVID-19 Transmission in 190 Countries from 23 January to 13 April 2020. Int. J. Infect. Dis. 2021, 102, 247–253. [Google Scholar] [CrossRef]
- Haug, N.; Geyrhofer, L.; Londei, A.; Dervic, E.; Desvars-Larrive, A.; Loreto, V.; Pinior, B.; Thurner, S.; Klimek, P. Ranking the Effectiveness of Worldwide COVID-19 Government Interventions. Nat. Hum. Behav. 2020, 4, 1303–1312. [Google Scholar] [CrossRef]
- Huy, L.D.; Nguyen, N.T.H.; Phuc, P.T.; Huang, C.-C. The Effects of Non-Pharmaceutical Interventions on COVID-19 Epidemic Growth Rate during Pre- and Post-Vaccination Period in Asian Countries. IJERPH 2022, 19, 1139. [Google Scholar] [CrossRef]
- Mugambe, R.K.; Ssekamatte, T.; Kisaka, S.; Wafula, S.T.; Isunju, J.B.; Nalugya, A.; Oputan, P.; Makanga, D.K.; Mukiibi, M.; Buregyeya, E.; et al. Extent of Compliance with COVID-19 Prevention and Control Guidelines among Supermarkets in Kampala Capital City and Mukono Municipality, Uganda. PLoS ONE 2021, 16, e0258840. [Google Scholar] [CrossRef]
- Petherick, A.; Goldszmidt, R.; Andrade, E.B.; Furst, R.; Hale, T.; Pott, A.; Wood, A. A Worldwide Assessment of Changes in Adherence to COVID-19 Protective Behaviours and Hypothesized Pandemic Fatigue. Nat. Hum. Behav. 2021, 5, 1145–1160. [Google Scholar] [CrossRef]
- Kim, J.; Hong, K.; Yum, S.; Gómez Gómez, R.E.; Jang, J.; Park, S.H.; Choe, Y.J.; Ryu, S.; Park, D.W.; Lee, Y.S.; et al. Factors Associated with the Difference between the Incidence and Case-Fatality Ratio of Coronavirus Disease 2019 by Country. Sci. Rep. 2021, 11, 18938. [Google Scholar] [CrossRef]
- Liang, L.-L.; Kao, C.-T.; Ho, H.J.; Wu, C.-Y. COVID-19 Case Doubling Time Associated with Non-Pharmaceutical Interventions and Vaccination: A Global Experience. J. Glob. Health 2021, 11, 05021. [Google Scholar] [CrossRef]
- Paital, B.; Agrawal, P.K. Air Pollution by NO2 and PM2.5 Explains COVID-19 Infection Severity by Overexpression of Angiotensin-Converting Enzyme 2 in Respiratory Cells: A Review. Environ. Chem. Lett. 2021, 19, 25–42. [Google Scholar] [CrossRef]
- Abdullah, F.; Myers, J.; Basu, D.; Tintinger, G.; Ueckermann, V.; Mathebula, M.; Ramlall, R.; Spoor, S.; de Villiers, T.; der Walt, Z.V.; et al. Decreased Severity of Disease during the First Global Omicron Variant COVID-19 Outbreak in a Large Hospital in Tshwane, South Africa. Int. J. Infect. Dis. 2022, 116, 38–42. [Google Scholar] [CrossRef]
- Elbe, S.; Buckland-Merrett, G. Data, Disease and Diplomacy: GISAID’s Innovative Contribution to Global Health: Data, Disease and Diplomacy. Glob. Chall. 2017, 1, 33–46. [Google Scholar] [CrossRef] [Green Version]
- Ritchie, H.; Mathieu, E.; Rodés-Guirao, L.; Appel, C.; Giattino, C.; Ortiz-Ospina, E.; Hasell, J.; Macdonald, B.; Beltekian, D.; Roser, M. Coronavirus Pandemic (COVID-19). Available online: https://ourworldindata.org/coronavirus (accessed on 29 March 2022).
- Hale, T.; Angrist, N.; Goldszmidt, R.; Kira, B.; Petherick, A.; Phillips, T.; Webster, S.; Cameron-Blake, E.; Hallas, L.; Majumdar, S.; et al. A Global Panel Database of Pandemic Policies (Oxford COVID-19 Government Response Tracker). Nat. Hum. Behav. 2021, 5, 529–538. [Google Scholar] [CrossRef]
- Mathieu, E.; Ritchie, H.; Ortiz-Ospina, E.; Roser, M.; Hasell, J.; Appel, C.; Giattino, C.; Rodés-Guirao, L. A Global Database of COVID-19 Vaccinations. Nat. Hum. Behav. 2021, 5, 947–953. [Google Scholar] [CrossRef]
- World Development Indicators. World Development Indicators—World Bank Collection. Available online: http://data.worldbank.org/data-catalog/world-development-indicators (accessed on 29 March 2022).
- Institute for Health Metrics and Evalution. GBD Results Tool; University of Washington: Seattle, WA, USA, 2022; Available online: https://ghdx.healthdata.org/gbd-results-tool (accessed on 29 March 2022).
- Bell, J.A.; Jennifer, B. Nuzzo GHS Index Report and Data. Available online: https://www.ghsindex.org/report-model/ (accessed on 29 March 2022).
- World Health Organization. Global Strategy on Human Resources for Health: Workforce 2030; World Health Organization: Geneva, Switzerland, 2016; ISBN 978-92-4-151113-1. [Google Scholar]
- UK Health Security Agency. COVID-19 Variants Identified in the UK. Available online: https://www.gov.uk/government/news/covid-19-variants-identified-in-the-uk (accessed on 29 March 2022).
- Li, H.; Wang, L.; Zhang, M.; Lu, Y.; Wang, W. Effects of Vaccination and Non-Pharmaceutical Interventions and Their Lag Times on the COVID-19 Pandemic: Comparison of Eight Countries. PLoS Negl. Trop. Dis. 2022, 16, e0010101. [Google Scholar] [CrossRef]
- Bates, D.; Mächler, M.; Bolker, B.; Walker, S. Fitting Linear Mixed-Effects Models Using Lme4. J. Stat. Soft. 2015, 67, 1–48. [Google Scholar] [CrossRef]
- Christensen, P.A.; Olsen, R.J.; Long, S.W.; Snehal, R.; Davis, J.J.; Ojeda Saavedra, M.; Reppond, K.; Shyer, M.N.; Cambric, J.; Gadd, R.; et al. Signals of Significantly Increased Vaccine Breakthrough, Decreased Hospitalization Rates, and Less Severe Disease in Patients with Coronavirus Disease 2019 Caused by the Omicron Variant of Severe Acute Respiratory Syndrome Coronavirus 2 in Houston, Texas. Am. J. Pathol. 2022, 192, 642–652. [Google Scholar] [CrossRef] [PubMed]
- Burki, T.K. Challenges in the Rollout of COVID-19 Vaccines Worldwide. Lancet Respir. Med. 2021, 9, e42–e43. [Google Scholar] [CrossRef]
- Bollyky, T.J.; Hulland, E.N.; Barber, R.M.; Collins, J.K.; Kiernan, S.; Moses, M.; Pigott, D.M.; Reiner Jr, R.C.; Sorensen, R.J.D.; Abbafati, C.; et al. Pandemic Preparedness and COVID-19: An Exploratory Analysis of Infection and Fatality Rates, and Contextual Factors Associated with Preparedness in 177 Countries, from Jan 1, 2020, to Sept 30, 2021. Lancet 2022, 399, 1489–1512. [Google Scholar] [CrossRef]
- Mendonca, D.; Fiedrich, F. Training for Improvisation in Emergency Management: Opportunities and Limits for Information Technology. Int. J. Emerg. Manag. 2006, 3, 348–363. [Google Scholar] [CrossRef]
- Geng, J.; Yu, X.; Bao, H.; Feng, Z.; Yuan, X.; Zhang, J.; Chen, X.; Chen, Y.; Li, C.; Yu, H. Chronic Diseases as a Predictor for Severity and Mortality of COVID-19: A Systematic Review with Cumulative Meta-Analysis. Front. Med. 2021, 8, 1442. [Google Scholar] [CrossRef]
- Campi, I.; Gennari, L.; Merlotti, D.; Mingiano, C.; Frosali, A.; Giovanelli, L.; Torlasco, C.; Pengo, M.F.; Heilbron, F.; Soranna, D.; et al. Vitamin D and COVID-19 Severity and Related Mortality: A Prospective Study in Italy. BMC Infect. Dis. 2021, 21, 566. [Google Scholar] [CrossRef]
- Mariani, J.; Giménez, V.M.M.; Bergam, I.; Tajer, C.; Antonietti, L.; Inserra, F.; Ferder, L.; Manucha, W. Association between Vitamin D Deficiency and COVID-19 Incidence, Complications, and Mortality in 46 Countries: An Ecological Study. Health Secur. 2021, 19, 302–308. [Google Scholar] [CrossRef]
- De Andrade, M.I.S.; de Macêdo, P.F.C.; de Oliveira, T.L.P.S.; da Silva Lima, N.M.; da Costa Ribeiro, I.; Santos, T.M. Vitamin A and D Deficiencies in the Prognosis of Respiratory Tract Infections: A Systematic Review with Perspectives for COVID-19 and a Critical Analysis on Supplementation. 2020. Available online: https://doi.org/10.1590/SciELOPreprints.839 (accessed on 29 March 2022).
- Tepasse, P.-R.; Vollenberg, R.; Fobker, M.; Kabar, I.; Schmidt, H.; Meier, J.A.; Nowacki, T.; Hüsing-Kabar, A. Vitamin A Plasma Levels in COVID-19 Patients: A Prospective Multicenter Study and Hypothesis. Nutrients 2021, 13, 2173. [Google Scholar] [CrossRef] [PubMed]
- Fiasca, F.; Minelli, M.; Maio, D.; Minelli, M.; Vergallo, I.; Necozione, S.; Mattei, A. Associations between COVID-19 Incidence Rates and the Exposure to PM2.5 and NO2: A Nationwide Observational Study in Italy. Int. J. Environ. Res. Public Health 2020, 17, 9318. [Google Scholar] [CrossRef]
| Characteristic | Mean (SD) | Median (25th Percentile, 75th Percentile) |
|---|---|---|
| Government indicators | ||
| Rule of law | 1.2 (0.6) | 1.4 (0.9, 1.7) |
| Regulatory quality | 1.3 (0.5) | 1.2 (0.8, 1.6) |
| Government effectiveness | 1.2 (0.6) | 1.3 (1.0, 1.6) |
| Socioeconomic characteristics | ||
| Population | 32,509,300.6 (64,315,654.6) | 10,160,159 (5,453,600, 32,776,195) |
| Population density | 458.3 (1460.4) | 112.371 (65.2, 231.4) |
| Life expectancy | 80.9 (2.9) | 82.1 (78.9, 82.8) |
| GDP per capita (USD per capita) | 40,988.8 (17,790.5) | 38,605.7 (30,155.2, 46,682.5) |
| % Population aged over 65 | 18.0 (3.9) | 18.8 (15.5, 19.7) |
| % Population living in urban area | 78.3 (13.5) | 80.7 (69.1, 88.0) |
| Health care capacity | ||
| UHC index | 79.9 (6.1) | 82 (76, 84) |
| No. physicians per 1000 | 3.7 (0.9) | 3.7 (3.0, 4.1) |
| No. nurses and midwives per 1000 | 10.4 (3.9) | 10.3 (7.4, 12.4) |
| % GDP for health expenditure | 8.7 (2.6) | 8.672 (7.0, 10.2) |
| GHS index | 58.8 (8.7) | 59.3 (54.4, 64.7) |
| Health burden of chronic diseases (death rate per 100,000) | ||
| Non-communicable diseases | 431.8 (139.1) | 383.7 (347.6, 484.6) |
| Diabetes | 9.8 (5.1) | 8.5 (6.4, 12.7) |
| Chronic respiratory diseases | 21.2 (8.6) | 19.9 (14.6, 27.6) |
| Cancers | 135.1 (18.9) | 137.4 (124.2, 145.9) |
| Chronic kidney diseases | 10.5 (4.8) | 9.7 (8.0, 11.1) |
| Cardiovascular diseases | 183.6 (117.8) | 132.4 (108.1, 232.2) |
| Health burden of environmental and health behavior risk (Years lived with disability (YLDs) per 100,000) | ||
| PM2.5 | 84.3 (57.3) | 69.0 (45.5, 118.3) |
| Tobacco | 551.6 (117.6) | 536.9 (470.5, 595.9) |
| Zinc deficiency | 0.05 (0.04) | 0.04 (0.03, 0.06) |
| Vitamin A deficiency | 1.1 (1.9) | 0.3 (0.2, 0.6) |
| Low bone density | 135.3 (35.2) | 137.0 (110.3, 149.2) |
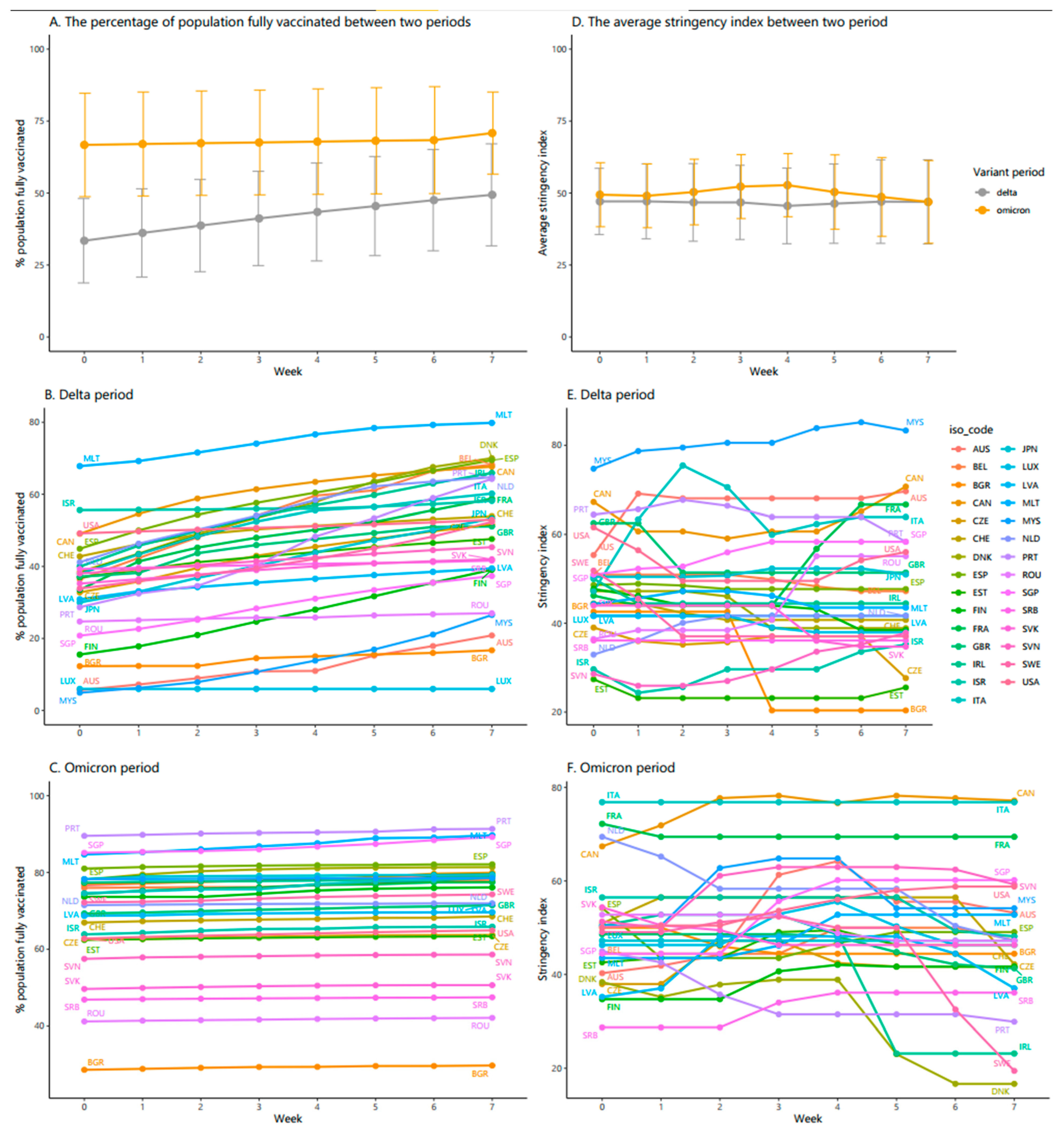
| Characteristic | Delta | Omicron | ||
|---|---|---|---|---|
| Mean (SD) | Median (Q1, Q3) | Mean (SD) | Median (Q1, Q3) | |
| Stringency index | 46.7 (12.6) | 45.1 (39.9, 53.3) | 50.0 (11.0) | 48.2 (44.2, 54.5) |
| % Population vaccinated at least one dose | 59.4 (15.7) | 62.9 (49.8, 72.3) | 73.5 (16.3) | 78.3 (69.71, 83.3) |
| % Population fully vaccinated | 49.4 (17.7) | 52.7 (39.5, 64.3) | 70.9 (14.3) | 74.3 (64.9, 79.2) |
| % Population vaccinated the booster dose | 0.3 (1.1) | 0 (0, 0.01) | 41.9 (18.8) | 43.8 (29.9, 55.8) |
| Country | Average Daily Hospital Occupancy per 100,000 Inhabitants (aHOSP) a | Average Daily ICU Occupancy per 100,000 Inhabitants (aICU) a | Average Daily Mortality Rate per 100,000 Inhabitants (aMOR) a | Average Resilience Index (aRESIDX) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Delta | Omicron | Change aHOSP (Rank) b | Delta | Omicron | Change aICU (Rank) c | Delta | Omicron | Change aMOR (Rank) d | Delta | Omicron | Change aRESIDX (Rank) e | |
| Australia | 0.006 | 0.152 | 0.146 (11) | 0.012 | 0.129 | 0.117 (11) | 0.012 | 0.141 | 0.129 (6) | 0.01 | 0.141 | 0.131 (8) |
| Belgium | 0.031 | 0.282 | 0.251 (18) | 0.106 | 0.389 | 0.283 (21) | 0.028 | 0.21 | 0.182 (13) | 0.055 | 0.294 | 0.239 (18) |
| Bulgaria | 0.187 | 0.824 | 0.637 (29) | 0.189 | 0.871 | 0.682 (28) | 0.113 | 0.79 | 0.677 (29) | 0.163 | 0.828 | 0.665 (29) |
| Canada | 0.018 | 0.191 | 0.173 (14) | 0.081 | 0.256 | 0.175 (16) | 0.025 | 0.195 | 0.17 (11) | 0.041 | 0.214 | 0.173 (15) |
| Czechia | 0.004 | 0.295 | 0.291 (21) | 0.014 | 0.4 | 0.386 (25) | 0.022 | 0.303 | 0.281 (21) | 0.013 | 0.333 | 0.32 (23) |
| Denmark | 0.012 | 0.173 | 0.161 (12) | 0.023 | 0.1 | 0.077 (7) | 0.019 | 0.239 | 0.22 (18) | 0.018 | 0.171 | 0.153 (12) |
| Estonia | 0.039 | 0.366 | 0.327 (24) | 0.044 | 0.164 | 0.12 (12) | 0.026 | 0.316 | 0.29 (22) | 0.036 | 0.282 | 0.246 (19) |
| Finland | 0.009 | 0.125 | 0.116 (6) | 0.02 | 0.095 | 0.075 (6) | 0.021 | 0.163 | 0.142 (9) | 0.017 | 0.128 | 0.111 (5) |
| France | 0.134 | 0.452 | 0.318 (22) | 0.221 | 0.592 | 0.371 (23) | 0.064 | 0.28 | 0.216 (17) | 0.14 | 0.441 | 0.301 (22) |
| Ireland | 0.026 | 0.158 | 0.132 (8) | 0.055 | 0.191 | 0.136 (15) | 0.032 | 0.127 | 0.095 (5) | 0.038 | 0.159 | 0.121 (7) |
| Israel | 0.015 | 0.259 | 0.244 (17) | 0.023 | 0.218 | 0.195 (18) | 0.018 | 0.216 | 0.198 (15) | 0.019 | 0.231 | 0.212 (17) |
| Italy | 0.042 | 0.332 | 0.29 (20) | 0.049 | 0.264 | 0.215 (19) | 0.039 | 0.367 | 0.328 (23) | 0.043 | 0.321 | 0.278 (21) |
| Japan | 0.159 | 0.131 | −0.028 (2) | 0.196 | 0.09 | −0.106 (2) | 0.03 | 0.053 | 0.023 (2) | 0.128 | 0.091 | −0.037 (2) |
| Latvia | 0.036 | 0.542 | 0.506 (28) | 0.115 | 0.56 | 0.445 (26) | 0.057 | 0.494 | 0.437 (28) | 0.069 | 0.532 | 0.463 (27) |
| Luxembourg | 0.022 | 0.117 | 0.095 (5) | 0.058 | 0.238 | 0.18 (17) | 0.027 | 0.164 | 0.137 (8) | 0.036 | 0.173 | 0.137 (10) |
| Malaysia | 0.305 | 0.091 | −0.214 (1) | 0.431 | 0.068 | −0.363 (1) | 0.255 | 0.05 | −0.205 (1) | 0.33 | 0.07 | −0.26 (1) |
| Malta | 0.052 | 0.194 | 0.142 (9) | 0.043 | 0.11 | 0.067 (5) | 0.055 | 0.32 | 0.265 (20) | 0.05 | 0.208 | 0.158 (13) |
| Netherlands | 0.021 | 0.072 | 0.051 (3) | 0.1 | 0.183 | 0.083 (9) | 0.028 | 0.061 | 0.033 (4) | 0.05 | 0.105 | 0.055 (4) |
| Portugal | 0.068 | 0.197 | 0.129 (7) | 0.155 | 0.172 | 0.017 (3) | 0.058 | 0.245 | 0.187 (14) | 0.094 | 0.205 | 0.111 (6) |
| Romania | 0.049 | 0.449 | 0.4 (26) | 0.049 | 0.401 | 0.352 (22) | 0.045 | 0.299 | 0.254 (19) | 0.048 | 0.383 | 0.335 (25) |
| Serbia | 0.178 | 0.519 | 0.341 (25) | 0.084 | 0.207 | 0.123 (13) | 0.113 | 0.451 | 0.338 (24) | 0.125 | 0.392 | 0.267 (20) |
| Singapore | 0.033 | 0.111 | 0.078 (4) | 0.004 | 0.025 | 0.021 (4) | 0.012 | 0.035 | 0.023 (3) | 0.016 | 0.057 | 0.041 (3) |
| Slovakia | 0.015 | 0.43 | 0.415 (27) | 0.058 | 0.517 | 0.459 (27) | 0.018 | 0.412 | 0.394 (26) | 0.03 | 0.453 | 0.423 (26) |
| Slovenia | 0.026 | 0.348 | 0.322 (23) | 0.061 | 0.761 | 0.7 (29) | 0.029 | 0.428 | 0.399 (27) | 0.039 | 0.512 | 0.473 (28) |
| Spain | 0.139 | 0.303 | 0.164 (13) | 0.336 | 0.46 | 0.124 (14) | 0.088 | 0.24 | 0.152 (10) | 0.188 | 0.334 | 0.146 (11) |
| Sweden | 0.016 | 0.158 | 0.142 (10) | 0.029 | 0.115 | 0.086 (10) | 0.017 | 0.193 | 0.176 (12) | 0.021 | 0.155 | 0.134 (9) |
| Switzerland | 0.032 | 0.231 | 0.199 (15) | 0.087 | 0.319 | 0.232 (20) | 0.023 | 0.156 | 0.133 (7) | 0.047 | 0.235 | 0.188 (16) |
| United Kingdom | 0.024 | 0.24 | 0.216 (16) | 0.039 | 0.117 | 0.078 (8) | 0.027 | 0.241 | 0.214 (16) | 0.03 | 0.199 | 0.169 (14) |
| United States | 0.123 | 0.379 | 0.256 (19) | 0.33 | 0.711 | 0.381 (24) | 0.098 | 0.458 | 0.36 (25) | 0.184 | 0.516 | 0.332 (24) |
| Factors | Country Performance a | Mean (SD) | Median (Q1,Q3) | p Value |
|---|---|---|---|---|
| Difference in intensity of stringency b | Worse | 9.3 (9.5) | 7.1 (2.2, 14.2) | 0.040 |
| Medium | 5.8 (12.8) | 3.8 (−2, 12.4) | ||
| Good | −5.2 (14.6) | −4 (−12, 2.7) | ||
| % Population vaccinated booster dose c | Worse | 30.5 (18) | 29.1 (27.1, 35.6) | 0.032 |
| Medium | 52.2 (10.8) | 55.4 (43.8, 61.5) | ||
| Good | 44.1 (20.4) | 50.9 (42, 56.8) | ||
| % Population fully vaccinated d | Worse | 58.3 (15.8) | 61.2 (48.3, 68.5) | 0.001 |
| Medium | 75.7 (8.8) | 78.1 (68.5, 81.4) | ||
| Good | 79.1 (6.6) | 78.9 (74.7, 79.4) | ||
| % Population vaccinated at least one dose e | Worse | 59.7 (19.7) | 62.8 (49.4, 75.2) | 0.001 |
| Medium | 78.9 (8.8) | 79.3 (72.1, 85.3) | ||
| Good | 82.5 (6.2) | 80.9 (78.8, 84.2) | ||
| Government indicators | ||||
| Rule of Law | Worse | 0.7 (0.6) | 0.8 (0.3, 1.1) | 0.000 |
| Medium | 1.4 (0.4) | 1.4 (1, 1.7) | ||
| Good | 1.6 (0.4) | 1.7 (1.5, 1.8) | ||
| Regulatory Quality | Worse | 0.8 (0.4) | 0.9 (0.5, 1.2) | 0.001 |
| Medium | 1.4 (0.3) | 1.5 (1.2, 1.6) | ||
| Good | 1.6 (0.5) | 1.7 (1.4, 1.8) | ||
| Government Effectiveness | Worse | 0.6 (0.6) | 0.7 (0.1, 1.1) | 0.000 |
| Medium | 1.4 (0.4) | 1.3 (1.1, 1.6) | ||
| Good | 1.6 (0.4) | 1.7 (1.5, 1.9) | ||
| Socio-economic characteristics | ||||
| Life expectancy | Worse | 78.6 (3.1) | 78.2 (76, 80.8) | 0.004 |
| Medium | 82 (1.6) | 82.4 (81.3, 83) | ||
| Good | 82.1 (2.3) | 82.3 (82.1, 83.3) | ||
| GDP per capita | Worse | 30,320.2 (11,305.1) | 30,778 (23,750.9, 34,566.5) | 0.017 |
| Medium | 40,435.7 (8456.5) | 39,753.2 (34,272.4, 44,017.6) | ||
| Good | 52,155.2 (22,977.9) | 45,799 (39,398.1, 62,619.6) | ||
| % Population aged over 65 | Worse | 18.7 (2.4) | 19 (17.5, 19.7) | 0.679 |
| Medium | 18 (2.5) | 18.6 (18.4, 19.4) | ||
| Good | 17.2 (5.8) | 17.1 (14, 20.9) | ||
| % Population living in Urban area | Worse | 67 (11.4) | 69.5 (55.2, 75) | 0.002 |
| Medium | 84.6 (9.6) | 83.7 (80.6, 92.5) | ||
| Good | 84 (11.8) | 86.9 (78.8, 91.6) | ||
| Population density | Worse | 97.9 (51.6) | 93.9 (69, 120.2) | 0.436 |
| Medium | 331.6 (443.9) | 214.2 (93.1, 375.6) | ||
| Good | 932.8 (2459) | 104.3 (36, 318.7) | ||
| Population | Worse | 51,371,999.9 (101,786,678.4) | 8,810,604 (5,804,839.3, 50,057,546.3) | 0.533 |
| Medium | 21,145,961.8 (23,967,521.1) | 9,291,000 (5,813,302, 38,067,913) | ||
| Good | 23,873,606.3 (37,291,513.1) | 10,164,041 (5,477,290.3, 23,634,436.3) | ||
| Health care capacity | ||||
| UHC index | Worse | 75.2 (6.3) | 76.5 (71.8, 78.8) | 0.005 |
| Medium | 82.9 (3.9) | 83 (82, 84) | ||
| Good | 82 (4.8) | 83 (79, 86) | ||
| GHS index | Worse | 57.7 (9.7) | 57.2 (52.1, 61.9) | 0.768 |
| Medium | 58.1 (9.5) | 59.3 (55.5, 64.4) | ||
| Good | 60.4 (7.4) | 59 (55.6, 64.9) | ||
| No. physicians per 1000 | Worse | 3.8 (1) | 3.5 (3.1, 4.1) | 0.542 |
| Medium | 3.8 (0.7) | 4 (3.7, 4.3) | ||
| Good | 3.4 (1.1) | 3.6 (2.6, 4.1) | ||
| No. nurses and midwives per 1000 | Worse | 8.6 (2.7) | 7.5 (7.1, 9.6) | 0.156 |
| Medium | 12 (4.4) | 10.4 (9.5, 14.5) | ||
| Good | 10.9 (4) | 12 (8, 12.5) | ||
| % GDP for health expenditure | Worse | 8.8 (3.2) | 8.2 (7, 8.7) | 0.538 |
| Medium | 9.4 (1.6) | 10 (8.2, 10.7) | ||
| Good | 8 (2.8) | 9.3 (5.7, 10.1) | ||
| Health burden of chronic diseases | ||||
| Death rate of NCD per 100,000 | Worse | 542.1 (170.8) | 521.2 (408.9, 634.9) | 0.004 |
| Medium | 382.5 (63.2) | 356.6 (347.6, 409.9) | ||
| Good | 365.8 (81.7) | 364.6 (342.9, 384.9) | ||
| Death rate of diabetes per 100,000 | Worse | 11.9 (5.2) | 10.6 (7.8, 15) | 0.204 |
| Medium | 9.6 (5.1) | 8.1 (6.4, 11.8) | ||
| Good | 7.8 (4.6) | 7.5 (4.5, 9.2) | ||
| Death rate of chronic respiratory disease per 100,000 | Worse | 18.7 (8.2) | 17.6 (12.7, 20.7) | 0.506 |
| Medium | 23.4 (9.6) | 24.2 (15.4, 29) | ||
| Good | 21.8 (8.4) | 21.8 (15.4, 27.5) | ||
| Death rate of cancers per 100,000 | Worse | 148.7 (15) | 145.2 (141.2, 151.7) | 0.014 |
| Medium | 133.7 (16.9) | 133.3 (124.2, 144.8) | ||
| Good | 125.1 (18) | 124.5 (116.4, 130.2) | ||
| Death rate of chronic kidney diseases per 100,000 | Worse | 9.7 (4.6) | 8.2 (6.3, 12.8) | 0.818 |
| Medium | 10.8 (4.4) | 9.9 (9.5, 11.1) | ||
| Good | 11 (5.6) | 10 (8.9, 10.7) | ||
| Death rate of CVD per 100,000 | Worse | 278.3 (151.3) | 265.6 (152.6, 373.9) | 0.004 |
| Medium | 133.9 (53.4) | 118.6 (107.1, 132.4) | ||
| Good | 133.6 (50.2) | 121.9 (109.3, 137.1) | ||
| Heath burden of environmental and health behavior risk | ||||
| YLDs caused by PM2.5 | Worse | 126.9 (65.3) | 124.7 (85.8, 169.3) | 0.009 |
| Medium | 59.9 (24.9) | 59.5 (45.5, 77.6) | ||
| Good | 63.5 (48.1) | 56.4 (26.7, 73) | ||
| YLDs caused by tobacco | Worse | 626.9 (129.1) | 595 (516.5, 751.7) | 0.014 |
| Medium | 548.1 (78.2) | 536.9 (508.4, 595.9) | ||
| Good | 479.4 (93.8) | 468.3 (447.4, 557.4) | ||
| YLDs caused by zinc deficiency | Worse | 0.1 (0) | 0.1 (0, 0.1) | 0.284 |
| Medium | 0 (0) | 0 (0, 0.1) | ||
| Good | 0 (0) | 0 (0, 0) | ||
| YLDs caused by vitamin A deficiency | Worse | 2.5 (2.6) | 1.9 (0.3, 3.9) | 0.010 |
| Medium | 0.5 (0.8) | 0.3 (0.2, 0.4) | ||
| Good | 0.3 (0.2) | 0.2 (0.2, 0.3) | ||
| YLDs caused by low bone density | Worse | 156.1 (32.5) | 147.9 (140.8, 175.7) | 0.058 |
| Medium | 128.2 (25.9) | 123.9 (113, 133.1) | ||
| Good | 120.9 (38) | 120.5 (92.7, 140.7) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huy, L.D.; Shih, C.-L.; Chang, Y.-M.; Nguyen, N.T.H.; Phuc, P.T.; Ou, T.-Y.; Huang, C.-C. Comparison of COVID-19 Resilience Index and Its Associated Factors across 29 Countries during the Delta and Omicron Variant Periods. Vaccines 2022, 10, 940. https://doi.org/10.3390/vaccines10060940
Huy LD, Shih C-L, Chang Y-M, Nguyen NTH, Phuc PT, Ou T-Y, Huang C-C. Comparison of COVID-19 Resilience Index and Its Associated Factors across 29 Countries during the Delta and Omicron Variant Periods. Vaccines. 2022; 10(6):940. https://doi.org/10.3390/vaccines10060940
Chicago/Turabian StyleHuy, Le Duc, Chung-Liang Shih, Yao-Mao Chang, Nhi Thi Hong Nguyen, Phan Thanh Phuc, Tsong-Yih Ou, and Chung-Chien Huang. 2022. "Comparison of COVID-19 Resilience Index and Its Associated Factors across 29 Countries during the Delta and Omicron Variant Periods" Vaccines 10, no. 6: 940. https://doi.org/10.3390/vaccines10060940
APA StyleHuy, L. D., Shih, C.-L., Chang, Y.-M., Nguyen, N. T. H., Phuc, P. T., Ou, T.-Y., & Huang, C.-C. (2022). Comparison of COVID-19 Resilience Index and Its Associated Factors across 29 Countries during the Delta and Omicron Variant Periods. Vaccines, 10(6), 940. https://doi.org/10.3390/vaccines10060940







