Air Quality in Dental Care Facilities: Update to Current Management and Control Strategies Implementing New Technologies: A Comprehensive Review
Abstract
:1. Introduction
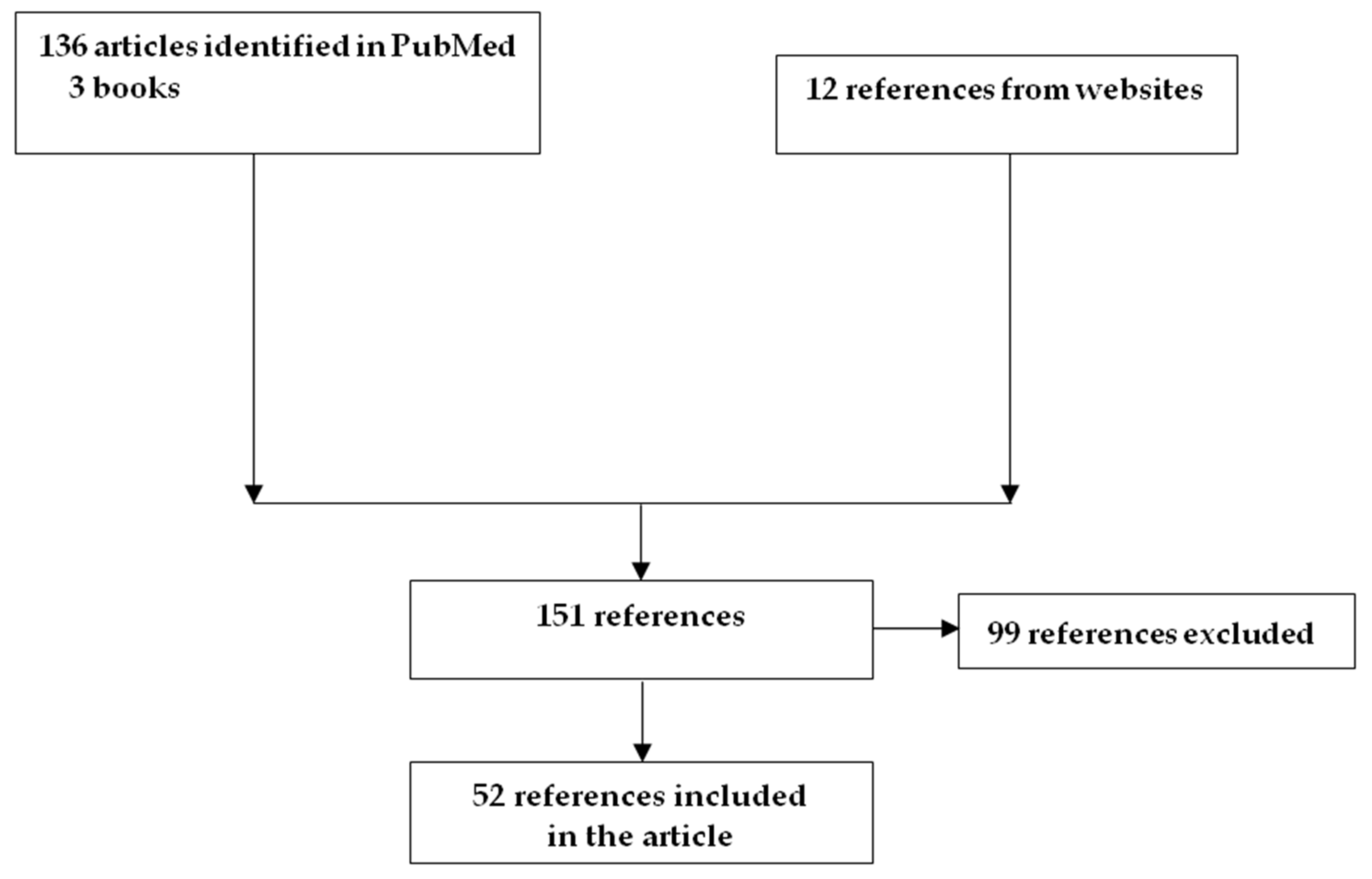
2. Methods
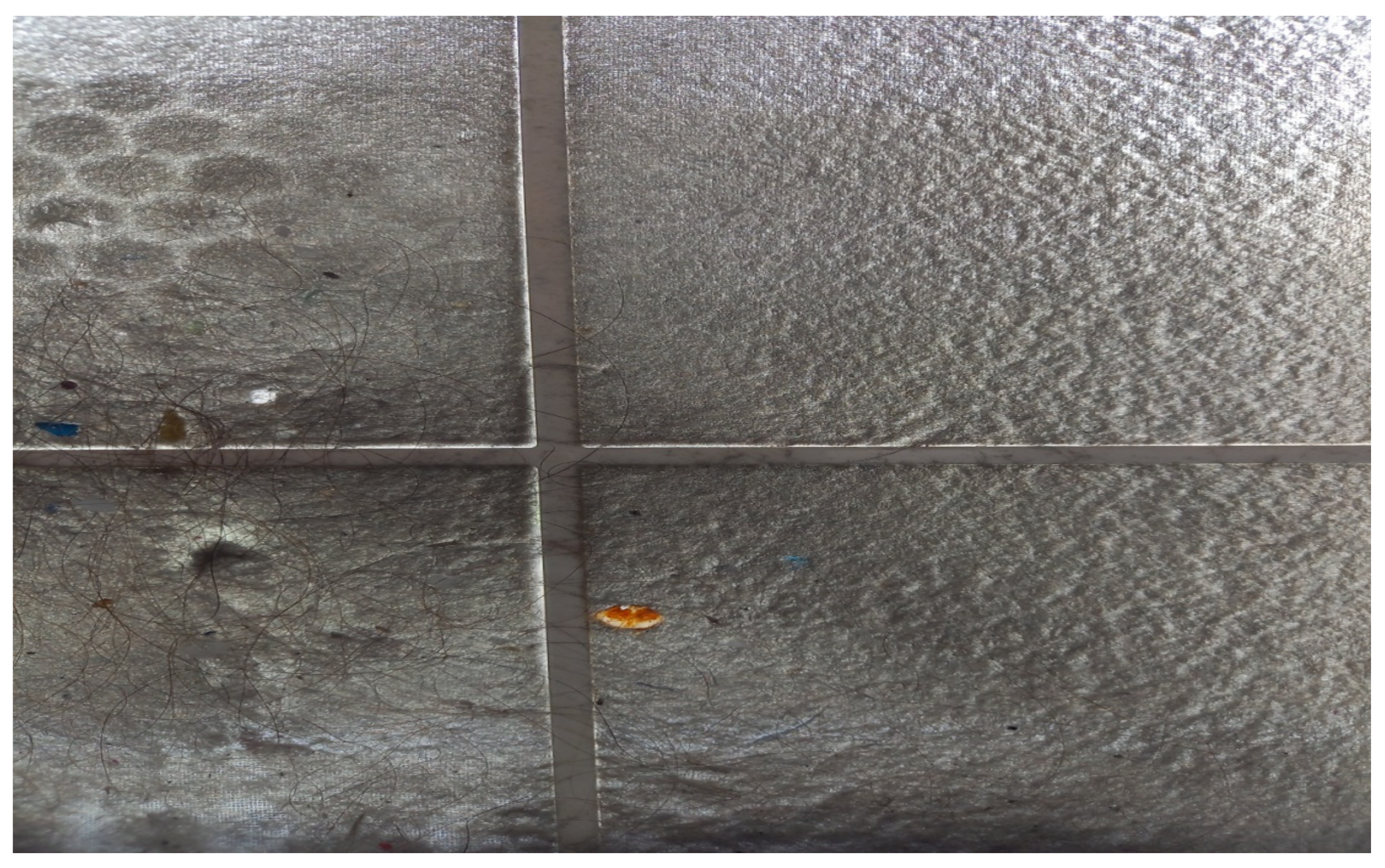
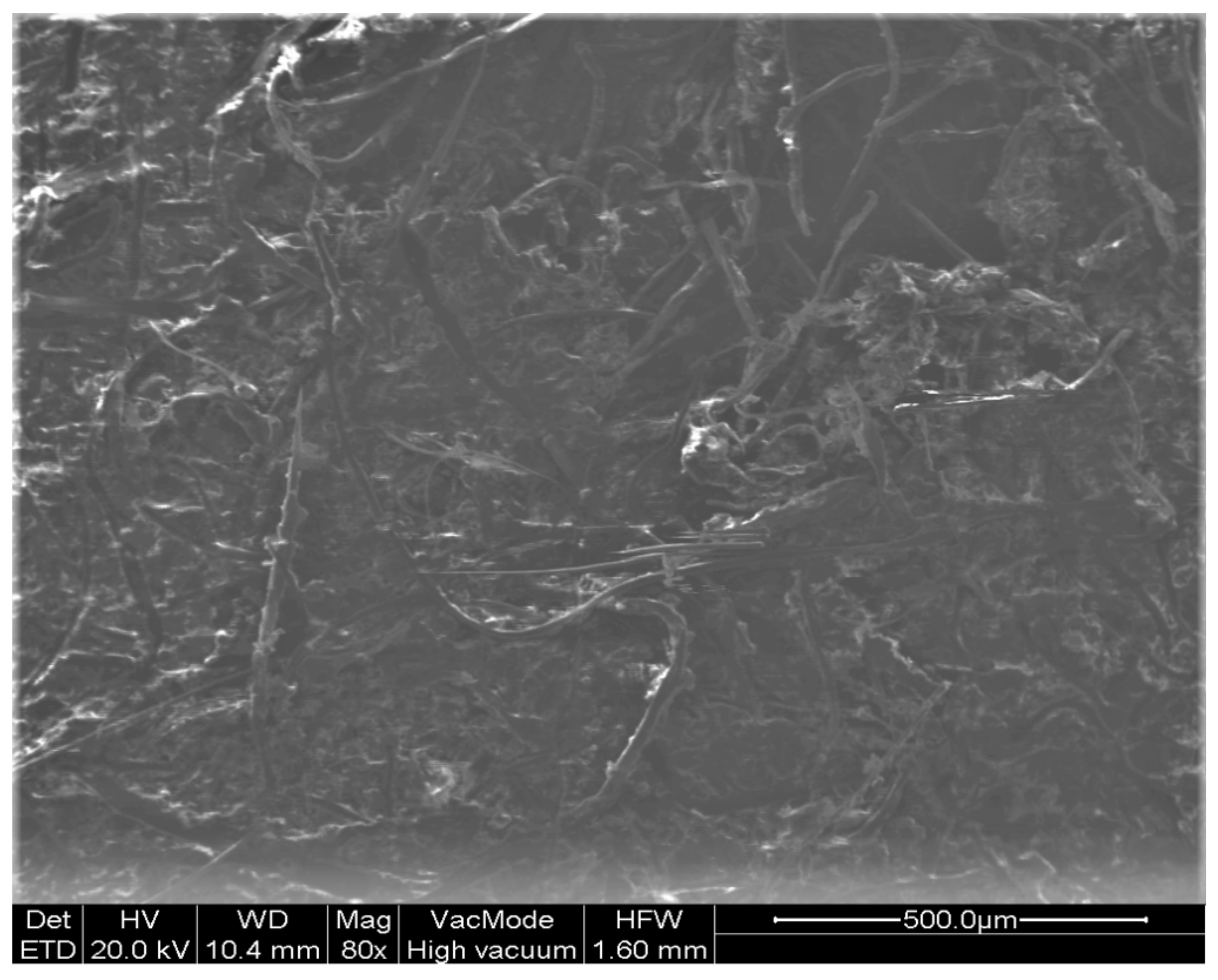
3. Characteristics of Air Splatters
4. Procedures of Air Splatter Production
5. Air Splatters Walking Management/Control
6. Air Splatter Technical Management
7. Utilization of UV Radiation for Air and Surface Sterilization
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Morgenstern, J. Aerosols, Droplets, and Airborne Spread. Everything you Could Possibly Want to Know. Available online: https://first10em.com/aerosols-droplets-and-airborne-spread/ (accessed on 16 May 2022).
- Maltezou, H.C.; Tseroni, M.; Vorou, R.; Koutsolioutsou, A.; Antoniadou, M.; Tzoutzas, I.; Panis, V.; Tzermpos, F.; Madianos, P. Preparing dental schools to refunction safely during the COVID-19 pandemic: An infection prevention and control perspective. J. Infect. Dev. Ctries 2021, 15, 22–31. [Google Scholar] [CrossRef]
- Li, Y.; Qian, H.; Hang, J.; Chen, X.; Cheng, P.; Ling, H.; Wang, S.; Liang, P.; Li, J.; Xiao, S.; et al. Probable airborne transmission of SARS-CoV-2 in a poorly ventilated restaurant. Build Environ. 2021, 196, 107788. [Google Scholar] [CrossRef]
- Cheng, V.C.C.; Fung, K.S.C.; Siu, G.K.H.; Wong, S.C.; Cheng, L.S.K.; Wong, M.S.; Lee, L.K.; Chan, W.M.; Chau, K.Y.; Leung, J.S.L.; et al. Nosocomial outbreak of COVID-19 by possible airborne transmission leading to a superspreading event. Clin. Infect. Dis. 2021, 73, e1356–e1364. [Google Scholar] [CrossRef]
- Miller, C. Infection Control and Management of Hazardous Materials for the Dental Team, 6th ed.; Elsevier Mosby: St. Louis, MO, USA, 2016; ISBN 9780323484282. [Google Scholar]
- Wood, P.R. Cross Infection Control in Dentistry, a Practical Illustrated Guide; Mosby: London, UK, 1992. [Google Scholar]
- Masia, M.D.; Dettori, M.; Deriu, G.M.; Soddu, S.; Deriu, M.; Arghittu, A.; Azara, A.; Castiglia, P. Microbial monitoring as a tool for preventing infectious risk in the operating room: Results of 10 years of activity. Atmosphere 2021, 12, 19. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention (CDC). Guidelines for Environmental Infection Control in Health-Care Facilities—Recommendation of CDC and the Healthcare Infection Control Practices Advisory Committee (HICPAC); U.S. Department of Health and Human Services: Atlanta, GA, USA, 2003. [Google Scholar]
- Helmis, C.G.; Tzoutzas, I.; Flocas, H.A.; Halios, C.H.; Stathopoulou, O.I.; Assimakopoulos, V.D.; Panis, V.; Apostolatou, M.; Sgouros, G.; Adam, E. Indoor air quality in a dentistry clinic. Sci. Total Environ. 2007, 377, 349–365. [Google Scholar] [CrossRef] [PubMed]
- Jungo, S.; Moreau, N.; Mazevet, M.E.; Ejeil, A.L.; Duplan, M.B.; Salmon, B.; Smail-Faugeron, V. Prevalence and risk indicators of first-wave COVID-19 among oral health-care workers: A French epidemiological survey. PLoS ONE 2021, 16, e0246586. [Google Scholar] [CrossRef] [PubMed]
- Chavis, S.E.; Hines, S.E.; Dyalram, D.; Cole Wilken, N.; Dalby, R.N. Can extraoral suction units minimize droplet spatter during a simulated dental procedure? J. Am. Dent. Assoc. 2021, 152, 157–165. [Google Scholar] [CrossRef]
- Petti, S. Tuberculosis: Occupational risk among dental healthcare workers and risk for infection among dental patients. A meta-narrative review. J. Dent. 2016, 49, 1–8. [Google Scholar] [CrossRef]
- Malsam, R.; Nienhaus, A. Occupational infections among dental health workers in Germany-14-year time trends. Int. J. Environ. Res. Public Health 2021, 18, 10128. [Google Scholar] [CrossRef]
- Singhal, S.; Warren, C.; Hobin, E.; Smith, B. How often are dental care workers exposed to occupational characteristics that put them at higher risk of exposure and transmission of COVID-19? A comparative analysis. J. Can. Dent. Assoc. 2021, 87, l16. [Google Scholar]
- Gallagher, J.E.; Sukriti, K.C.; Johnson, I.G.; Al-Yaseen, W.; Jones, R.; McGregor, S.; Robertson, M.; Harris, R.; Innes, N.; Wade, W.G. A systematic review of contamination (aerosol, splatter and droplet generation) associated with oral surgery and its relevance to COVID-19. BDJ Open 2020, 6, 25. [Google Scholar] [CrossRef]
- Nagraj, S.K.; Eachempati, P.; Paisi, M.; Nasser, M.; Sivaramakrishnan, G.; Verbeek, J.H. Interventions to reduce contaminated aerosols produced during dental procedures for preventing infectious diseases. Cochrane Database Syst. Rev. 2020, 10, CD013686. [Google Scholar]
- Jones, A.P. Indoor air quality and health. Atmos. Environ. 1999, 33, 4535–4564. [Google Scholar] [CrossRef]
- International WELL Building Institute. Air. Available online: https://standard.wellcertified.com/air (accessed on 16 May 2022).
- Tellier, R. Aerosol transmission of influenza A virus: A review of new studies. J. R. Soc. Interface 2009, 6 (Suppl. 6), S783S790. [Google Scholar] [CrossRef] [Green Version]
- Judson, S.D.; Munster, V.J. Nosocomial transmission of emerging viruses via aerosol-generating medical procedures. Viruses 2019, 11, 940. [Google Scholar] [CrossRef] [Green Version]
- Nicas, M.; Nazaroff, W.W.; Hubbard, A. Toward understanding the risk of secondary airborne infection: Emission of respirable pathogens. J. Occup. Environ. Hyg. 2005, 2, 143154. [Google Scholar] [CrossRef]
- Fiegel, J.; Clarke, R.; Edwards, D.A. Airborne infectious disease and the suppression of pulmonary bioaerosols. Drug Discov. Today 2006, 11, 5157. [Google Scholar] [CrossRef]
- Morawska, L. Droplet fate in indoor environments, or can we prevent the spread of infection? Indoor Air 2006, 16, 335347. [Google Scholar] [CrossRef] [Green Version]
- Xie, X.; Li, Y.; Chwang, A.T.; Ho, P.L.; Seto, W.H. How far droplets can move in indoor environments revisiting the Wells evaporation-falling curve. Indoor Air 2007, 17, 211225. [Google Scholar] [CrossRef]
- Hinds, W.C.; Cottone, J.A.; Terezhalmy, G.T.; Molinari, J.A. Practical Infection. In Aerosol Technology Properties, Behavior, and Measurement of Airborne Particles; Wiley: New York, NY, USA, 1982; Volume 68, p. 14. [Google Scholar]
- Chen, W.Q.; Ling, W.H.; Lu, C.Y.; Hao, Y.T.; Lin, Z.N.; Ling, L.; Huang, J.; Li, G.; Yan, G.M. Which preventive measures might protect health care workers from SARS? BMC Public Health 2009, 9, 81. [Google Scholar] [CrossRef] [Green Version]
- Asadi, S.; Wexler, A.S.; Cappa, C.D.; Barreda, S.; Bouvier, N.M.; Ristenpart, W.D. Aerosol emission and super emission during human speech increase with voice loudness. Sci. Rep. 2019, 9, 2348. [Google Scholar] [CrossRef] [Green Version]
- Noti, J.D.; Blachere, F.M.; McMillen, C.M.; Lindsley William, G.; Kashon, M.L.; Slaughter, D.R.; Beezhold, D.H. High humidity leads to loss of infectious influenza virus from simulated coughs. PLoS ONE 2013, 8, e57485. [Google Scholar] [CrossRef]
- Papineni, R.S.; Rosenthal, F.S. The size distribution of droplets in the exhaled breath of healthy human subjects. J. Aerosol. Med. 1997, 10, 105116. [Google Scholar] [CrossRef] [PubMed]
- Holliday, R.; Allison, J.R.; Currie, C.C.; Edwards, D.C.; Bowes, C.; Pickering, K.; Reay, S.; Durham, J.; Lumb, J.; Rostami, N.; et al. Evaluating contaminated dental aerosol and splatter in an open plan clinic environment: Implications for the COVID-19 pandemic. J. Dent. 2021, 105, 103565. [Google Scholar] [CrossRef] [PubMed]
- Bourouiba, L. Turbulent gas clouds and respiratory pathogen emissions: Potential implications for reducing transmission of COVID-19. JAMA 2020, 323, 1837–1838. [Google Scholar] [CrossRef] [PubMed]
- Hui, D.S.; Chan, M.T.; Chow, B. Aerosol dispersion during various respiratory therapies: A risk assessment model of nosocomial infection to health care workers. Hong Kong Med. J. 2014, 20 (Suppl. 4), 913. [Google Scholar]
- Loh, N.W.; Tan, Y.; Taculod, J.; Gorospe, B.; Teope, A.S.; Somani, J.; Tan, A.Y.H. The impact of high-flow nasal cannula (HFNC) on coughing distance: Implications on its use during the novel coronavirus disease outbreak. Can. J. Anaesth. 2020, 67, 893–894. [Google Scholar] [CrossRef] [Green Version]
- Cummings, K.J.; Martin, S.B., Jr.; Lindsley, W.G.; Othmpangat, S.; Blachere, F.M.; Noti, J.D.; Beezhold, D.H.; Roidad, N.; Parker, J.E.; Weissman, D.N. Exposure to influenza virus aerosols in the hospital setting: Is routine patient care an aerosol generating procedure? J. Infect. Dis. 2014, 210, 504505. [Google Scholar] [CrossRef] [Green Version]
- Bahl, P.; Doolan, C.; de Silva, C.; Chughtai, A.A.; Bourouiba, L.; MacIntyre, C.R. Airborne or droplet precautions for healthworkers treating COVID-19? J. Infect. Dis. 2020, 225, 1561–1568. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Joshi, S.M. The sick building syndrome. Indian J. Occup. Environ. Med. 2008, 12, 61–64. [Google Scholar] [CrossRef]
- Steiner, C.; Let Airflow Show Pathogens the Door (or Window or Vent). Infection Control Today. Available online: https://www.infectioncontroltoday.com/view/let-airflow-show-pathogens-the-door-or-window-or-vent- (accessed on 16 May 2022).
- Diamond, F.; Best Approach to Disinfecting Surfaces Amid Novel Coronavirus Outbreak. Infection Control Today. Available online: https://www.infectioncontroltoday.com/view/best-approach-disinfecting-surfaces-amid-novel-coronavirus-outbreak (accessed on 16 May 2022).
- Whyte, W.; Green, G.; Whyte, W.M. Removal of microbe carrying particles by high-efficiency air filters in clean rooms. Intern. J. Vent. 2012, 10, 339–351. [Google Scholar]
- Whyte, W.; Agricola, K.; Dercks, M. Airborne Particle Deposition in Clean Rooms. Deposition Mechanisms. Clean Air Contain. Rev. 2015, 24, 4–9. Available online: https://eprints.gla.ac.uk/111678/1/111678.pdf (accessed on 16 May 2022).
- Tzoutzas, I.; Maltezou, H.C.; Barbaressos, N.; Tasios, P.; Efthymiou, C.; Assimakopoulos, M.N.; Tseroni, M.; Vorou, R.; Tzermpos, F.; Antoniadou, M.; et al. Indoor air quality evaluation using mechanical ventilation and portable air purifiers in an academic dentistry clinic during the COVID-19 pandemic in Greece. Int. J. Environ. Res. Public Health 2021, 18, 8886. [Google Scholar] [CrossRef]
- Capparè, P.; D’Ambrosio, R.; De Cunto, R.; Darvizeh, A.; Nagni, M.; Gherlone, E. The usage of an air purifier device with HEPA 14 filter during dental procedures in COVID-19 pandemic: A randomized clinical trial. Int. J. Environ. Res. Public Health 2022, 19, 5139. [Google Scholar] [CrossRef]
- Tsoi, J.K.H.; Ding, H.; Hon, K.; Leung, Y.Y. The spread of droplets and aerosols of surgical motor handpiece irrigation using different suction systems. Front. Dent. Med. 2021, 2, 727111. [Google Scholar] [CrossRef]
- EMS Technical Properties. Airflow Prophylaxis Master. Available online: https://www.ems-dental.com/el/products/airflow-prophylaxis-master (accessed on 16 May 2022).
- EMS Treatment Recommendations. Guided Biofilm Therapy. Available online: ems-dental.com (accessed on 16 May 2022).
- Vyas, N.; Pecheva, E.; Dehghani, H.; Sammons, R.L.; Wang, Q.X.; Leppinen, D.M.; Walmsley, A.D. High speed imaging of cavitation around dental ultrasonic scaler tips. PLoS ONE 2016, 11, e0149804. [Google Scholar] [CrossRef]
- Pasquarella, C.; Veronesi, l.; Castiglia, P.; Liguori, G.; Montagna, M.T.; Napoli, C.; Rizzetto, R.; Torre, I.; Masia, M.D.; Di Onofrio, V.; et al. Italian multicentre study on microbial environmental contamination in dental clinics: A pilot study. Sci. Total Environ. 2010, 408, 4045–4051. [Google Scholar] [CrossRef]
- Cumbo, E.; Gallina, G.; Messina, P.; Scardina, G.A. Alternative methods of sterilization in dental practices against COVID-19. Int. J. Environ. Res. Public Health 2020, 17, 5736. [Google Scholar] [CrossRef]
- Advanced Biotechnologies Inc. Is UV Sterilization Effective for Viruses and Bacteria? Available online: https://abionline.com/is-uv-sterilization-effective-for-viruses-and-bacteria/ (accessed on 16 May 2022).
- Rensair. Clean Air for Every Space. Available online: https://rensair.com (accessed on 16 May 2022).
- Abu-Hammad, O.; Alnazzawi, A.; Babkair, H.; Jambi, S.; Mirah, M.; Abdouh, I.; Aljohani, R.S.; Ayeq, R.; Ghazi, L.; Al-Subhi, H.; et al. COVID-19 infection in academic dental hospital personnel: A cross-sectional survey in Saudi Arabia. Int. J. Environ. Res. Public Health 2021, 18, 10911. [Google Scholar] [CrossRef]
- Hellenic Society for Research on Air Splatters. The Significance of Indoor Air Quality in Controlling COVID-19. Available online: https://youtu.be/fFdDM_33bVE (accessed on 16 May 2022).



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tzoutzas, I.; Karoussis, I.; Maltezou, H.C. Air Quality in Dental Care Facilities: Update to Current Management and Control Strategies Implementing New Technologies: A Comprehensive Review. Vaccines 2022, 10, 847. https://doi.org/10.3390/vaccines10060847
Tzoutzas I, Karoussis I, Maltezou HC. Air Quality in Dental Care Facilities: Update to Current Management and Control Strategies Implementing New Technologies: A Comprehensive Review. Vaccines. 2022; 10(6):847. https://doi.org/10.3390/vaccines10060847
Chicago/Turabian StyleTzoutzas, Ioannis, Ioannis Karoussis, and Helena C. Maltezou. 2022. "Air Quality in Dental Care Facilities: Update to Current Management and Control Strategies Implementing New Technologies: A Comprehensive Review" Vaccines 10, no. 6: 847. https://doi.org/10.3390/vaccines10060847
APA StyleTzoutzas, I., Karoussis, I., & Maltezou, H. C. (2022). Air Quality in Dental Care Facilities: Update to Current Management and Control Strategies Implementing New Technologies: A Comprehensive Review. Vaccines, 10(6), 847. https://doi.org/10.3390/vaccines10060847






