Vaccine Hesitancy towards the COVID-19 Vaccine in a Random National Sample of Belgian Nursing Home Staff Members
Abstract
:1. Introduction
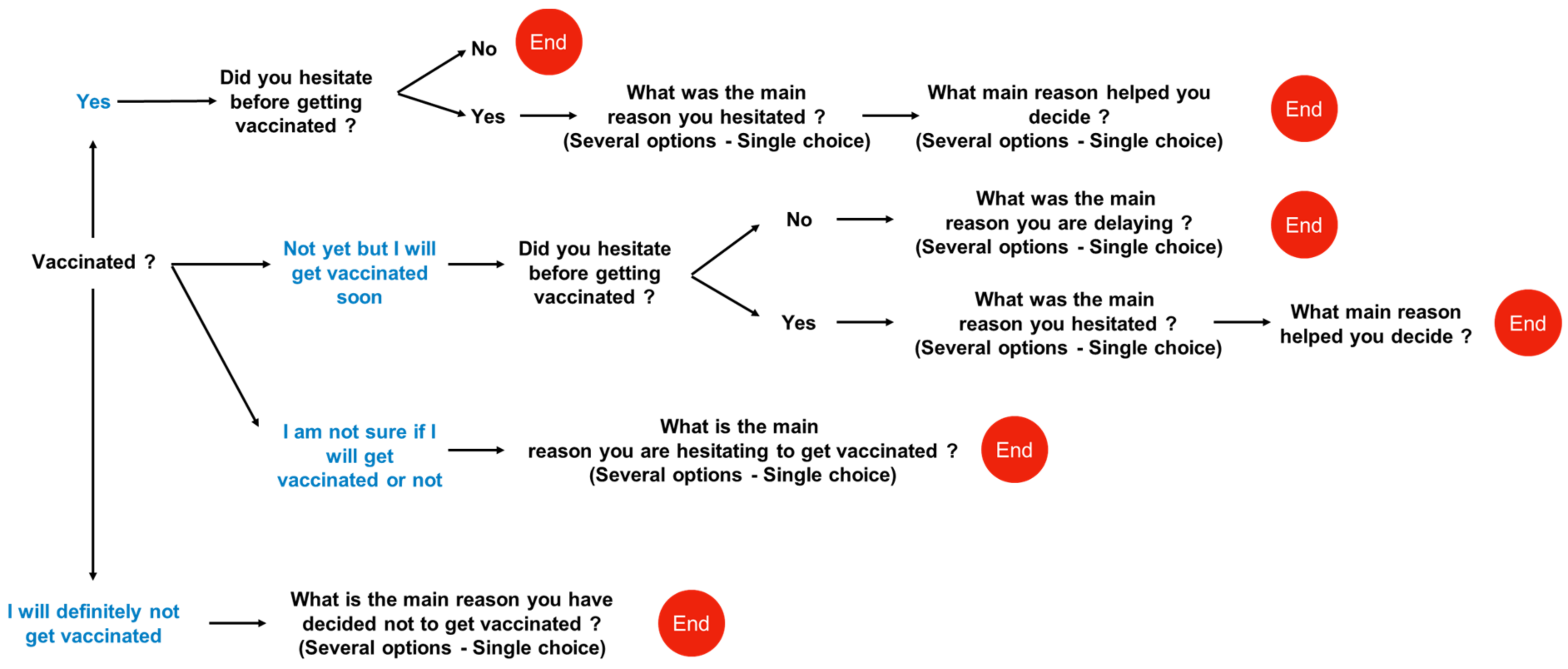
2. Methods
2.1. Study Design and Population
2.2. Ethics Approval and Consent to Participate
2.3. Data Collection
2.4. Data and Statistical Analysis
3. Results
3.1. Description of the Study Cohort
3.2. Distribution of Nursing Home Staff Members by Vaccine Hesitancy Question (Profile) and Association with Individual Characteristics
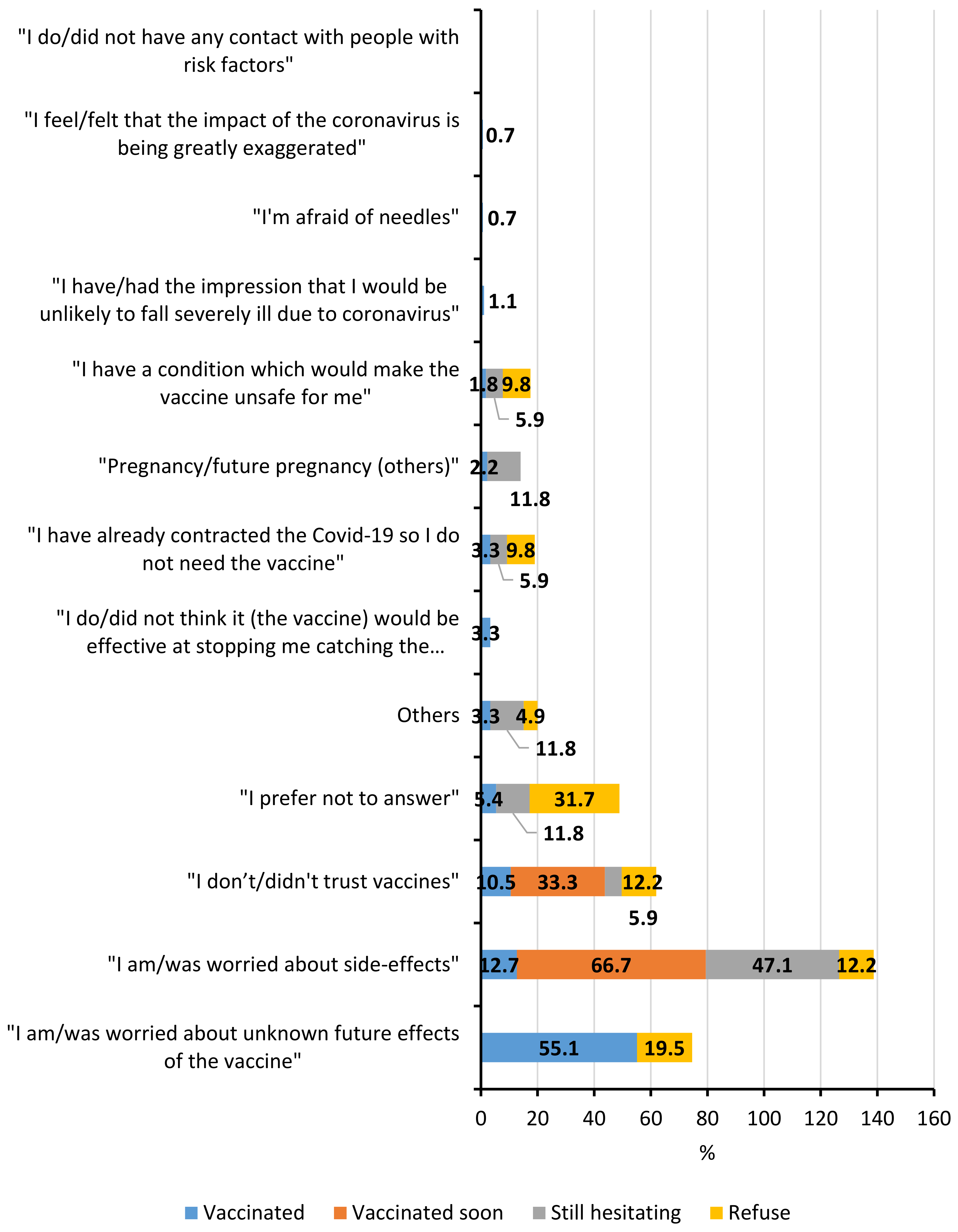
3.3. Principal Reasons for Hesitation/Refusal of COVID–19 Vaccination and Comparison between the Different Profiles Identified
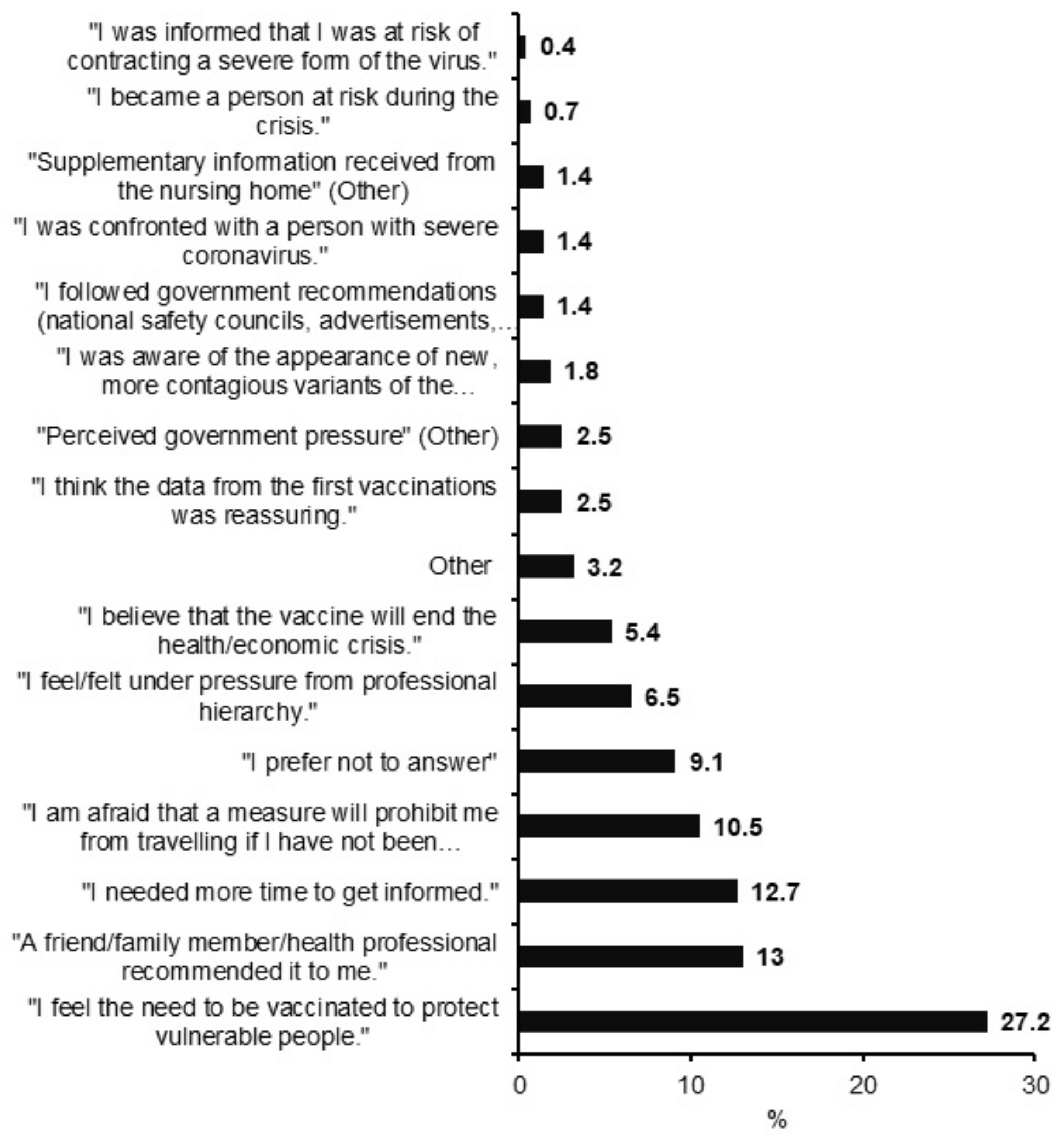
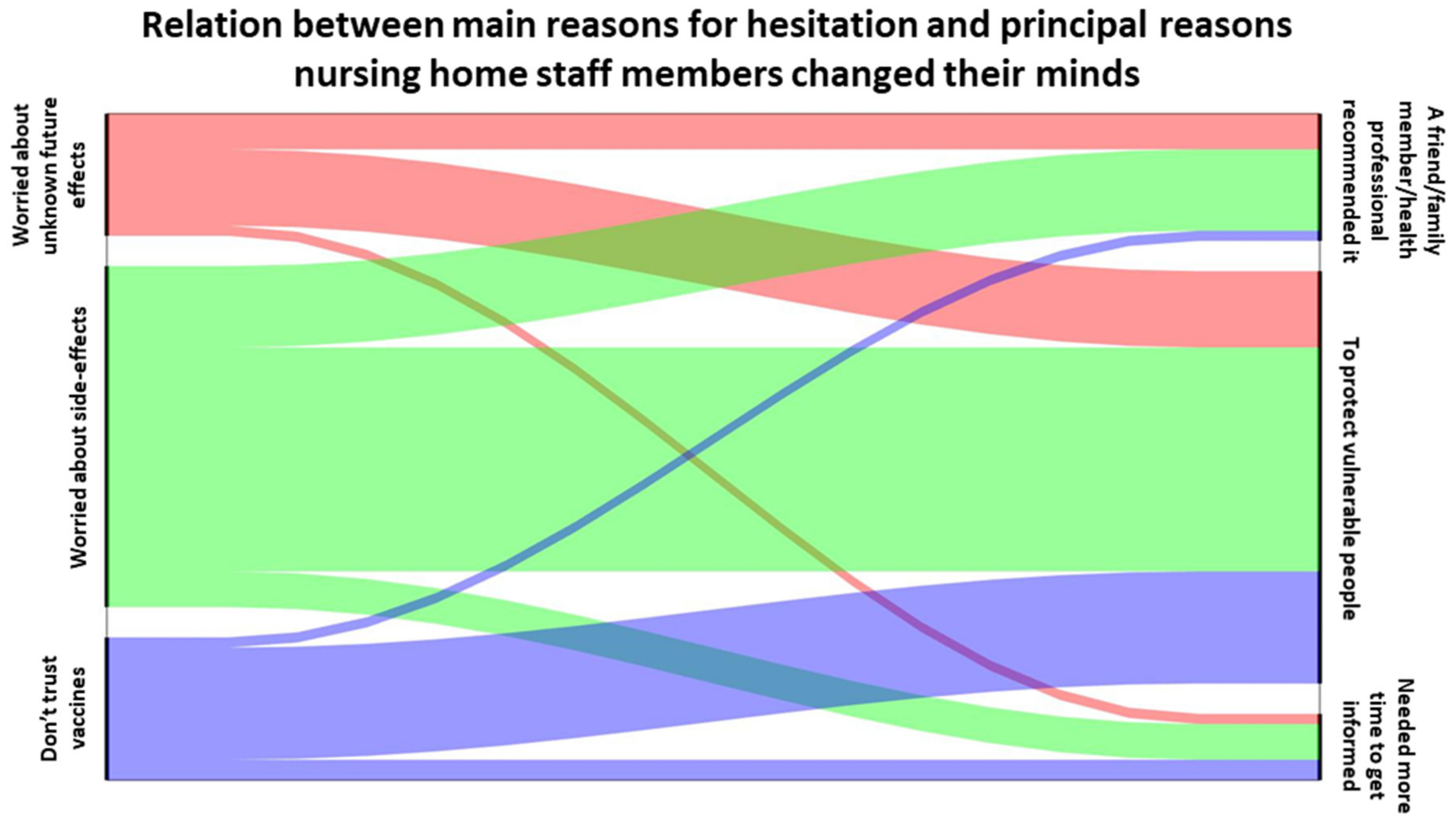
3.4. Principal Reasons Given by Participants, That Hesitated but Eventually Accepted Vaccination, to Decide to Get Vaccinated
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19) 16–24 February 2020; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Callies, M.; Int Panis, L.; Dequeker, S.; Latour, K.; Rebolledo Gonzalez, J.; Vandael, E.; Sierra, B.N.; der Heyden, V.J. Surveillance in Nursing Homes. Report Week 35 (Data through 31 August 2021). 2021. Available online: https://www.info-coronavirus.be/nl/ (accessed on 17 November 2021).
- Catteau, L.; Haarhuis, F.; Dequeker, S.; Vandael, E.; Stouten, V.; Litzroth, A.; Wyndham, T. Thematisch Rapport: Surveillance Van De COVID-19 Vaccinatie in Belgische Woonzorgcentra. 2021. Available online: https://covid-19.sciensano.be/sites/default/files/Covid19/COVID-19_THEMATICREPORT_SURVEILLANCEVANDEVACCINATIEINBELGISCHEWOONZORGCENTRA.pdf (accessed on 7 June 2021).
- Meyers, E.; Deschepper, E.; Duysburgh, E.; De Rop, L.; De Burghgraeve, T.; Van Ngoc, P.; Di Gregorio, M.; Delogne, S.; Coen, A.; De Clercq, N.; et al. SARS-CoV-2 Seroprevalence among Vaccinated Nursing Home Residents and Staff in Belgium in August 2021 Brief Communication on Preliminary Results of The Scope Study. 2021. Available online: https://www.sciensano.be/sites/default/files/sars-cov-2_among_nh_residents_brief_communication_20210831_1.pdf (accessed on 14 February 2022).
- Daugherty, J.D.; Blake, S.C.; Grosholz, J.M.; Omer, S.B.; Polivka-West, L.; Howard, D.H. Influenza Vaccination Rates and Beliefs about vaccination Among Nursing Home Employees. Am. J. Infect. Control 2015, 43, 100–106. Available online: http://www.ajicjournal.org/article/S0196655314011432/fulltext (accessed on 17 November 2021). [CrossRef] [PubMed]
- Leshem, E.; Lopman, B.A. Population Immunity and Vaccine Protection against Infection. Lancet 2021, 397, 1685–1687. Available online: http://www.thelancet.com/article/S0140673621008709/fulltext (accessed on 16 November 2021). [CrossRef]
- ECDC. Overview of the Implementation of COVID-19 Vaccination Strategies and Vaccine Deployment Plans in the EU and EEA; ECDC: Stockholm, Sweden, 2021. [Google Scholar]
- World Health Organization. Ten Threats to Global Health in 2019; WHO: Geneva, Switzerland, 2019; Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 17 November 2021).
- Nohl, A.; Afflerbach, C.; Lurz, C.; Brune, B.; Ohmann, T.; Weichert, V.; Zeiger, S.; Dudda, M. Acceptance of COVID-19 vaccination among front-line health care workers: A nationwide survey of emergency medical services personnel from Germany. Vaccines 2021, 9, 424. [Google Scholar] [CrossRef] [PubMed]
- Soares, P.; Rocha, J.V.; Moniz, M.; Gama, A.; Laires, P.A.; Pedro, A.R.; Dias, S.; Leite, A.; Nunes, C. Factors associated with COVID-19 vaccine hesitancy. Vaccines 2021, 9, 300. [Google Scholar] [CrossRef] [PubMed]
- Holzmann-Littig, C.; Braunisch, M.C.; Kranke, P.; Popp, M.; Seeber, C.; Fichtner, F.; Littig, B.; Carbajo-Lozoya, J.; Allwang, C.; Frank, T.; et al. COVID-19 vaccination acceptance and hesitancy among healthcare workers in Germany. Vaccines 2021, 9, 777. [Google Scholar] [CrossRef] [PubMed]
- Robertson, E.; Reeve, K.S.; Niedzwiedz, C.L.; Moore, J.; Blake, M.; Green, M.; Katikireddi, S.V.; Benzeval, M.J. Predictors of COVID-19 Vaccine Hesitancy in the UK Household Longitudinal Study. Brain. Behav. Immun. 2021, 94, 41–50. Available online: https://pubmed.ncbi.nlm.nih.gov/33713824/ (accessed on 29 November 2021). [CrossRef] [PubMed]
- Fisher, K.A.; Bloomstone, S.J.; Walder, J.; Crawford, S.; Fouayzi, H.; Mazor, K.M. Attitudes Toward a Potential SARS-CoV-2 Vaccine: A Survey of U.S. Adults. Ann. Intern. Med. 2020, 173, 964–973. Available online: https://pubmed.ncbi.nlm.nih.gov/32886525/ (accessed on 29 November 2021). [CrossRef] [PubMed]
- Verger, P.; Scronias, D.; Dauby, N.; Adedzi, K.A.; Gobert, C.; Bergeat, M.; Gagneur, A.; Dubé, E. Attitudes of Healthcare Workers towards COVID-19 Vaccination: A Survey in France and French-Speaking Parts of Belgium and Canada, 2020. Eurosurveillance 2021, 26, 1. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7848677/ (accessed on 5 October 2021). [CrossRef] [PubMed]
- Di Giuseppe, G.; Pelullo, C.P.; Della Polla, G.; Montemurro, M.V.; Napolitano, F.; Pavia, M.; Angelillo, I.F. Surveying Willingness toward SARS-CoV-2 Vaccination of Healthcare Workers in Italy. Expert Rev. Vaccines 2021, 20, 881–889. Available online: https://pubmed.ncbi.nlm.nih.gov/33900148/ (accessed on 28 March 2022). [CrossRef] [PubMed]
- Wang, J.; Lu, X.; Lai, X.; Lyu, Y.; Zhang, H.; Fenghuang, Y.; Jing, R.; Li, L.; Yu, W.; Fang, H. The Changing Acceptance of COVID-19 Vaccination in Different Epidemic Phases in China: A Longitudinal Study. Vaccines 2021, 9, 191. [Google Scholar] [CrossRef] [PubMed]
- Spinewine, A.; Pétein, C.; Evrard, P.; Vastrade, C.; Laurent, C.; Delaere, B.; Henrard, S. Attitudes towards COVID-19 Vaccination among Hospital Staff-Understanding What Matters to Hesitant People. Vaccines 2021, 9, 469. [Google Scholar] [CrossRef] [PubMed]
- Valckx, S.; Crèvecoeur, J.; Verelst, F.; Vranckx, M.; Hendrickx, G.; Hens, N.; Van Damme, P.; Pepermans, K.; Beutels, P.; Neyens, T. Individual Factors Influencing COVID-19 Vaccine Acceptance in between and During Pandemic Waves (July–December 2020). Vaccine 2021, 40, 151–161. Available online: https://pubmed.ncbi.nlm.nih.gov/34863621/ (accessed on 20 December 2021). [CrossRef] [PubMed]
- Kessels, R.; Luyten, J.; Tubeuf, S. Willingness to Get Vaccinated against COVID-19 and Attitudes toward Vaccination in General. Vaccine 2021, 39, 4716–4722. Available online: https://pubmed.ncbi.nlm.nih.gov/34119349/ (accessed on 20 December 2021). [CrossRef] [PubMed]
- Sciensano Protocol: SARS-CoV-2 Seroprevalence among Nursing Home Staff and Residents in Belgium. Available online: https://www.sciensano.be/sites/default/files/v6.2_2021-06-23_proposal_sars-cov-2_seroprevalence_study_in_belgian_nh.pdf (accessed on 14 February 2022).
- Larson, H.J.; Jarrett, C.; Schulz, W.S.; Chaudhuri, M.; Zhou, Y.; Dube, E.; Schuster, M.; Macdonald, N.E.; Wilson, R. Measuring Vaccine Hesitancy: The Development of a Survey Tool. Vaccine 2015, 33, 4165–4175. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Unroe, K.T.; Evans, R.; Weaver, L.; Rusyniak, D.; Blackburn, J. Willingness of Long-Term Care Staff to Receive a COVID-19 Vaccine: A Single State Survey. J. Am. Geriatr. Soc. 2021, 69, 593–599. Available online: https://onlinelibrary.wiley.com/doi/full/10.1111/jgs.17022 (accessed on 8 December 2021). [CrossRef] [PubMed]
- Catteau, L.; Van Loenhout, J.; Stouten, V.; Billuart, M.; Hubin, P.; Haarhuis, F.; Wyndham, C. Rapport Thématique: Couverture Vaccinale Et Impact Epidémiologique De La Campagne De Vaccination COVID-19 En Belgique. 2021. Available online: https://covid-19.sciensano.be/sites/default/files/Covid19/COVID-19_THEMATIC_REPORT_VaccineCoverageAndImpactReport_FR.pdf (accessed on 24 January 2022).
- Paul, E.; Steptoe, A.; Fancourt, D. Attitudes towards vaccines and intention to vaccinate against COVID-19: Implications for public health communications. Lancet Reg. Health-Eur. 2021, 1, 100012. [Google Scholar] [CrossRef] [PubMed]
- Robson, C. Real World Research A Resource for Social Scientists and Practitioner-Researchers, 2nd ed.; Oxford Blackwell Publishers Ltd.: Oxford, UK, 2002. [Google Scholar]
- AVIQ Certificat Numérique Covid Safe Ticket|AVIQ. Available online: https://covid.aviq.be/fr/covidsafeticket (accessed on 2 February 2022).
- Gezondheid, A.Z. en Covid Safe Ticket (CST) Als Toegangsvoorwaarde|Vlaanderen.be. Available online: https://www.vlaanderen.be/covid-safe-ticket-cst-als-toegangsvoorwaarde (accessed on 14 February 2022).
- Porat, T.; Burnell, R.; Calvo, R.A.; Ford, E.; Paudyal, P.; Baxter, W.L.; Parush, A. “Vaccine Passports” May Backfire: Findings from a Cross-Sectional Study in the UK and Israel on Willingness to Get Vaccinated against COVID-19. Vaccines 2021, 9, 902. [Google Scholar] [CrossRef] [PubMed]
- Gallè, F.; Sabella, E.A.; Roma, P.; Da Molin, G.; Diella, G.; Montagna, M.T.; Ferracuti, S.; Liguori, G.; Orsi, G.B.; Napoli, C. Acceptance of COVID-19 Vaccination in the Elderly: A Cross-Sectional Study in Southern Italy. Vaccines 2021, 9, 1222. [Google Scholar] [CrossRef] [PubMed]
- Stojanovic, J.; Boucher, V.G.; Gagne, M.; Gupta, S.; Joyal-Desmarais, K.; Paduano, S.; Aburub, A.S.; Sheinfeld Gorin, S.N.; Kassianos, A.P.; Ribeiro, P.A.B.; et al. Global Trends and Correlates of COVID-19 Vaccination Hesitancy: Findings from the iCARE Study. Vaccines 2021, 9, 661. [Google Scholar] [CrossRef] [PubMed]
| N (%) | |
|---|---|
| TOTAL | 1142 |
| Age | |
| 18–40 | 444 (38.9) |
| >40 | 629 (55.1) |
| Gender | |
| Male | 158 (13.8) |
| Female | 961 (84.2) |
| Unknown | 23 (2) |
| Region | |
| Brussels | 80 (7) |
| Flanders | 678 (59.4) |
| Wallonia | 384 (33.6) |
| Type of job | |
| Nursing | 582 (51) |
| Paramedical | 147 (12.9) |
| Cleaning staff | 128 (11.2) |
| Catering | 90 (7.9) |
| Administration | 99 (8.7) |
| Hairdresser/pedicure | 2 (0.2) |
| Other | 47 (4.1) |
| Comorbidity | |
| Cardiovascular disease | 35 (3.1) |
| Diabetes | 35 (3.1) |
| Hypertension | 120 (10.5) |
| Respiratory disorders | 21 (1.8) |
| Immunosuppression | 22 (1.9) |
| Cancer | 7 (0.6) |
| None | 893 (78.2) |
| Influenza vaccination | |
| Yes | 546 (47.8) |
| No | 549 (48.1) |
| COVID-19 vaccine hesitancy | |
| Vaccinated, no hesitation before | 805 (70.5) |
| Vaccinated, hesitation before | 276 (24.2) |
| Vaccinated soon, hesitation before | 3 (0.2) |
| Not yet vaccinated, still hesitating | 17 (1.5) |
| Refuse | 41 (3.6) |
| Vaccinated, No Hesitation before | Vaccinated, Hesitation before | Not Yet Vaccinated or Soon, (Still) Hesitating | Refuse | p | Vc | |
|---|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | N (%) | |||
| Age (years) | <0.0001 | 0.14 | ||||
| 18–40 | 281 (63.3) | 137 (30.8) | 9 (2) | 17 (3.8) | ||
| >40 | 480 (76.3) | 121 (19.2) | 9 (1.4) | 19 (3) | ||
| Gender | 0.006 | 0.10 | ||||
| Female | 661 (68.8) | 249 (25.8) | 17 (1.6) | 34 (3.5) | ||
| Male | 129 (81.6) | 21 (13.3) | 2 (1.3) | 6 (3.8) | ||
| Region | <0.0001 | 0.18 | ||||
| Brussels | 54 (67.5) | 20 (25) | 2 (2.5) | 4 (5) | ||
| Flanders | 534 (78.8) | 131 (19.3) | 4 (0.6) | 9 (1.3) | ||
| Wallonia | 217 (56.5) | 125 (32.6) | 14 (3.7) | 28 (7.3) | ||
| Type of job | 0.0008 | 0.12 | ||||
| Medic. # | 495 (67.9) | 199 (27.3) | 14 (1.9) | 21 (2.9) | ||
| Non-medic. * | 284 (77.6) | 61 (16.7) | 5 (1.4) | 16 (4.4) | ||
| Comorbidity | 0.7233 | 0.03 | ||||
| No δ | 640 (71.7) | 210 (23.5) | 14 (1.5) | 29 (3.2) | ||
| Yes β | 139 (68.8) | 50 (24.7) | 5 (2.4) | 8 (3.9) | ||
| Influenza vaccination | <0.0001 | 0.33 | ||||
| Yes | 466 (85.3) | 79 (14.5) | 1 (0.2) | 0 | ||
| No | 313 (57) | 181 (33) | 18 (3.2) | 37 (6.7) | ||
| Unadjusted | Adjusted | |||
|---|---|---|---|---|
| No Hesitation before | Hesitation before/Still Hesitating/Refusing | OR [95% CI] | OR [95% CI] | |
| N | N | |||
| Age (years) | 761 | 312 | 0.96 [0.95, 0.97] | 0.96 [0.94, 0.97] |
| Gender | ||||
| Female (ref) | 661 | 300 | 1 | 1 |
| Male | 129 | 29 | 0.47 [0.31, 0.72] | 0.46 [0.29, 0.75] |
| Region | ||||
| Brussels | 54 | 26 | 1.75 [0.99, 3.10] | 0.90 [0.44, 1.85] |
| Flanders (ref) | 534 | 144 | 1 | 1 |
| Wallonia | 217 | 167 | 2.83 [2.07, 3.88] | 2.22 [1.57, 3.12] |
| Type of job | ||||
| Medic. (ref) | 495 | 234 | 1 | 1 |
| Non-medic. | 284 | 82 | 0.59 [0.44, 0.78] | 0.68 [0.49, 0.95] |
| Comorbidity | ||||
| No (ref) | 640 | 253 | 1 | 1 |
| Yes | 139 | 63 | 1.16 [0.84, 1.62] | 1.82 [1.23, 2.69] |
| Influenza vaccination | ||||
| Yes (ref) | 466 | 80 | 1 | 1 |
| No | 313 | 236 | 4.21 [3.12, 5.68] | 3.86 [2.81, 5.30] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Digregorio, M.; Van Ngoc, P.; Delogne, S.; Meyers, E.; Deschepper, E.; Duysburgh, E.; De Rop, L.; De Burghgraeve, T.; Coen, A.; De Clercq, N.; et al. Vaccine Hesitancy towards the COVID-19 Vaccine in a Random National Sample of Belgian Nursing Home Staff Members. Vaccines 2022, 10, 598. https://doi.org/10.3390/vaccines10040598
Digregorio M, Van Ngoc P, Delogne S, Meyers E, Deschepper E, Duysburgh E, De Rop L, De Burghgraeve T, Coen A, De Clercq N, et al. Vaccine Hesitancy towards the COVID-19 Vaccine in a Random National Sample of Belgian Nursing Home Staff Members. Vaccines. 2022; 10(4):598. https://doi.org/10.3390/vaccines10040598
Chicago/Turabian StyleDigregorio, Marina, Pauline Van Ngoc, Simon Delogne, Eline Meyers, Ellen Deschepper, Els Duysburgh, Liselore De Rop, Tine De Burghgraeve, Anja Coen, Nele De Clercq, and et al. 2022. "Vaccine Hesitancy towards the COVID-19 Vaccine in a Random National Sample of Belgian Nursing Home Staff Members" Vaccines 10, no. 4: 598. https://doi.org/10.3390/vaccines10040598
APA StyleDigregorio, M., Van Ngoc, P., Delogne, S., Meyers, E., Deschepper, E., Duysburgh, E., De Rop, L., De Burghgraeve, T., Coen, A., De Clercq, N., Sutter, A. D., Verbakel, J. Y., Cools, P., Heytens, S., Buret, L., & Scholtes, B. (2022). Vaccine Hesitancy towards the COVID-19 Vaccine in a Random National Sample of Belgian Nursing Home Staff Members. Vaccines, 10(4), 598. https://doi.org/10.3390/vaccines10040598








