Safety of Live Immunization in DiGeorge Syndrome: A Retrospective Single-Center Study in Korea, 2005–2021
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Characteristics
2.2. Definition of AEFLI
2.3. Statistical Analysis
3. Results
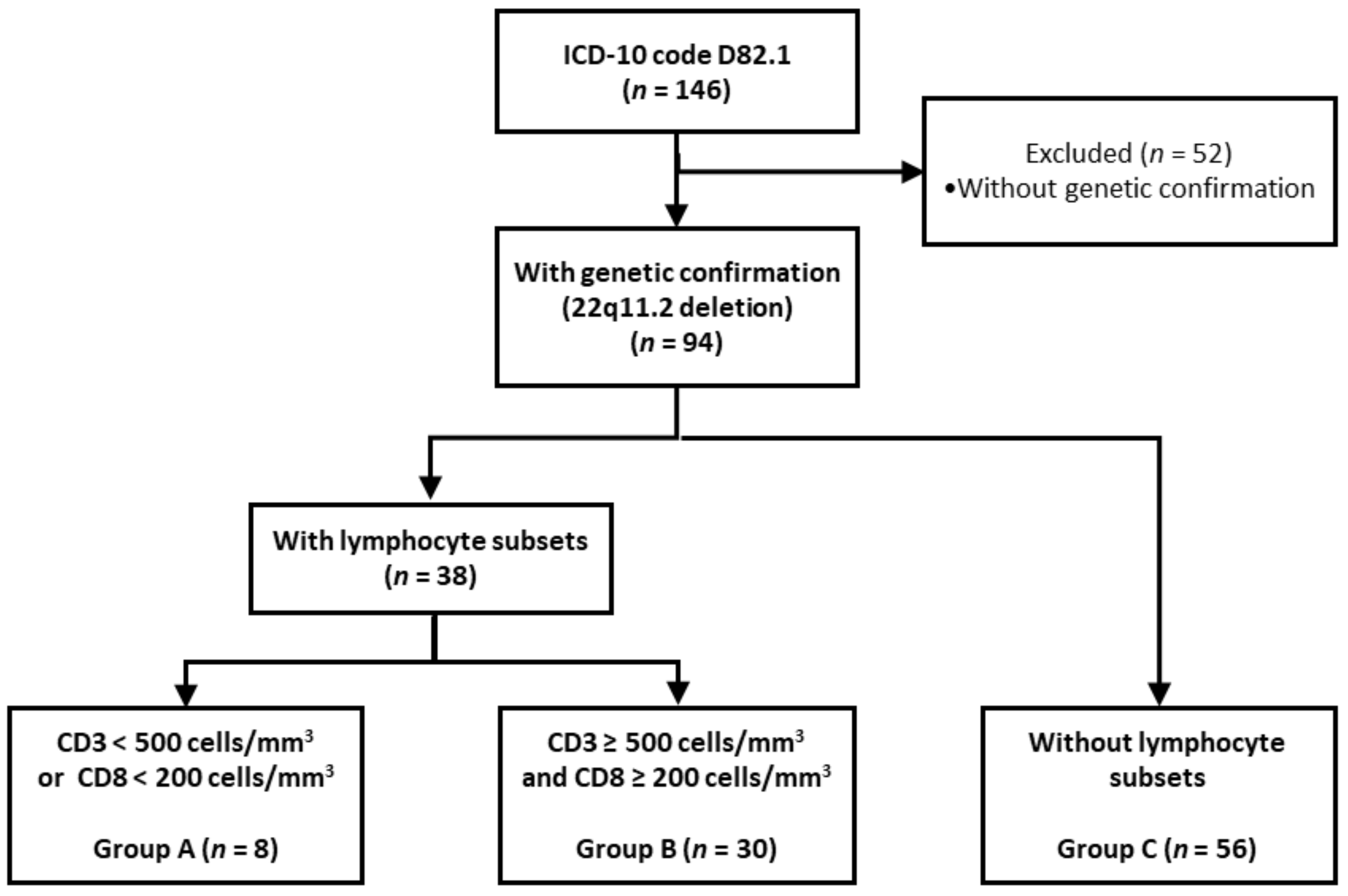
3.1. Study Population
3.2. Immunization Coverage
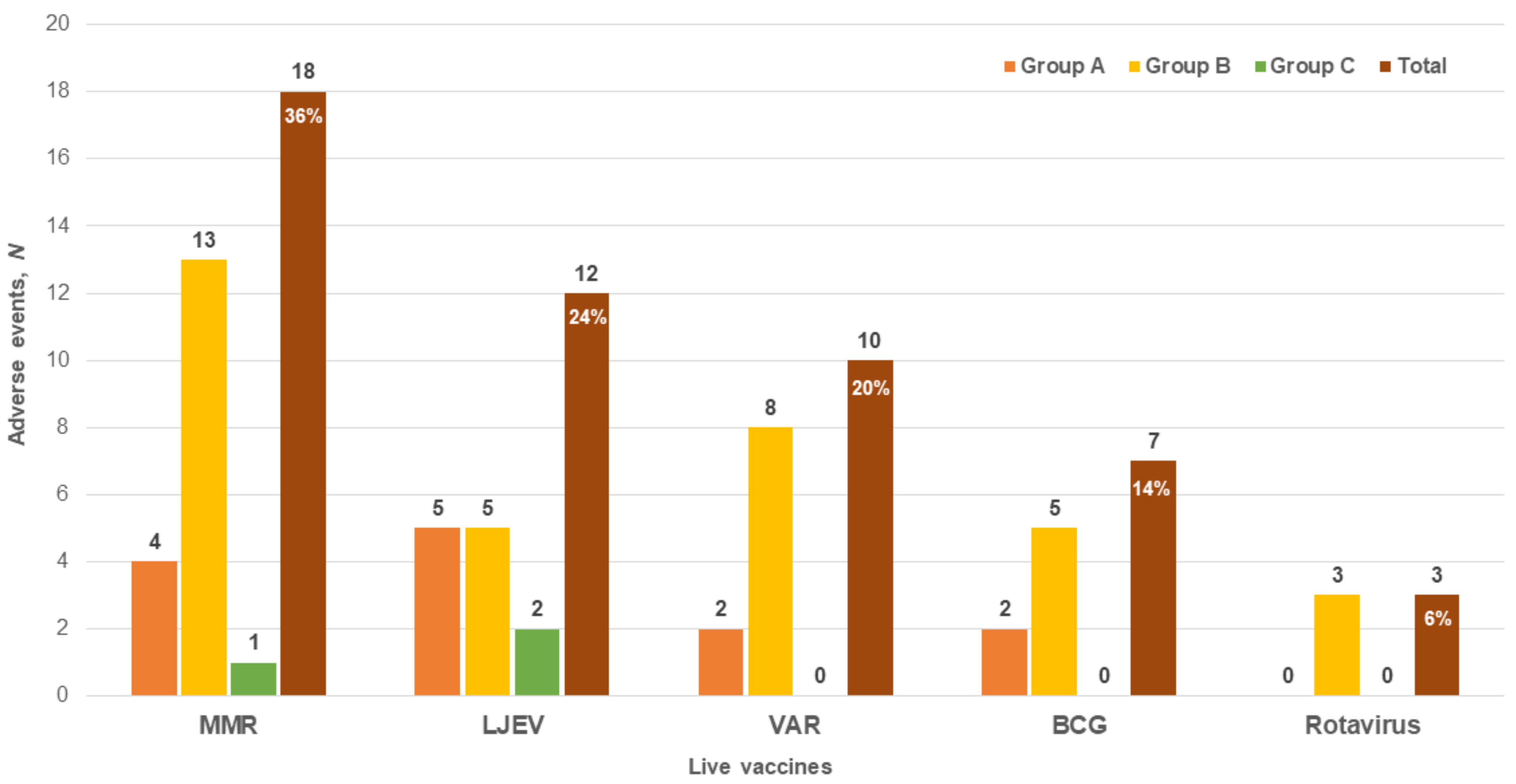
3.3. AEFLI
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kobrynski, L.J.; Sullivan, K.E. Velocardiofacial syndrome, DiGeorge syndrome: The chromosome 22q11.2 deletion syndromes. Lancet 2007, 370, 1443–1452. [Google Scholar] [CrossRef] [PubMed]
- Nissan, E.; Katz, U.; Levy-Shraga, Y.; Frizinsky, S.; Carmel, E.; Gothelf, D.; Somech, R. Clinical Features in a Large Cohort of Patients With 22q11.2 Deletion Syndrome. J. Pediatr. 2021, 238, 215–220. [Google Scholar] [CrossRef] [PubMed]
- McDonald-McGinn, D.M.; Sullivan, K.E. Chromosome 22q11.2 deletion syndrome (DiGeorge syndrome/velocardiofacial syndrome). Medicine 2011, 90, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Jawad, A.F.; Prak, E.L.; Boyer, J.; McDonald-McGinn, D.M.; Zachai, E.; McDonald, K.; Sullivan, K.E. A prospective study of influenza vaccination and a comparison of immunologic parameters in children and adults with chromosome 22q11.2 deletion syndrome (digeorge syndrome/velocardiofacial syndrome). J. Clin. Immunol. 2011, 31, 927–935. [Google Scholar] [CrossRef] [PubMed]
- Gennery, A.R. Immunological aspects of 22q11.2 deletion syndrome. Cell. Mol. Life. Sci. 2012, 69, 17–27. [Google Scholar] [CrossRef] [PubMed]
- Morsheimer, M.; Brown Whitehorn, T.F.; Heimall, J.; Sullivan, K.E. The immune deficiency of chromosome 22q11.2 deletion syndrome. Am. J. Med. Genet. A 2017, 173, 2366–2372. [Google Scholar] [CrossRef] [PubMed]
- Monafo, W.J.; Haslam, D.B.; Roberts, R.L.; Zaki, S.R.; Bellini, W.J.; Coffin, C.M. Disseminated measles infection after vaccination in a child with a congenital immunodeficiency. J. Pediatr. 1994, 124, 273–276. [Google Scholar] [CrossRef]
- Patel, N.C.; Hertel, P.M.; Estes, M.K.; Morena, M.; Petru, A.M.; Noroski, L.M.; Revell, P.A.; Hanson, I.C.; Paul, M.E.; Rosenblatt, H.M.; et al. Vaccine-acquired rotavirus in infants with severe combined immunodeficiency. N. Engl. J. Med. 2010, 362, 314–319. [Google Scholar] [CrossRef]
- Sarmiento, J.D.; Villada, F.; Orrego, J.C.; Franco, J.L.; Trujillo-Vargas, C.M. Adverse events following immunization in patients with primary immunodeficiencies. Vaccine 2016, 34, 1611–1616. [Google Scholar] [CrossRef]
- Marciano, B.E.; Huang, C.Y.; Joshi, G.; Rezaei, N.; Carvalho, B.C.; Allwood, Z.; Ikinciogullari, A.; Reda, S.M.; Gennery, A.; Thon, V.; et al. BCG vaccination in patients with severe combined immunodeficiency: Complications, risks, and vaccination policies. J. Allergy Clin. Immunol. 2014, 133, 1134–1141. [Google Scholar] [CrossRef]
- Chaves, S.S.; Haber, P.; Walton, K.; Wise, R.P.; Izurieta, H.S.; Schmid, D.S.; Seward, J.F. Safety of varicella vaccine after licensure in the United States: Experience from reports to the vaccine adverse event reporting system, 1995–2005. J. Infect. Dis. 2008, 197 (Suppl. S2), S170–S177. [Google Scholar] [CrossRef] [PubMed]
- Waters, V.; Peterson, K.S.; LaRussa, P. Live viral vaccines in a DiGeorge syndrome patient. Arch. Dis. Child. 2007, 92, 519–520. [Google Scholar] [CrossRef] [PubMed]
- National Center for Immunization and Respiratory Disease. General recommendations on immunization: Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm. Rep. 2011, 60, 1–64. [Google Scholar]
- Perez, E.E.; Bokszczanin, A.; McDonald-McGinn, D.; Zackai, E.H.; Sullivan, K.E. Safety of live viral vaccines in patients with chromosome 22q11.2 deletion syndrome (DiGeorge syndrome/velocardiofacial syndrome). Pediatrics 2003, 112, e325. [Google Scholar] [CrossRef]
- Al-Sukaiti, N.; Reid, B.; Lavi, S.; Al-Zaharani, D.; Atkinson, A.; Roifman, C.M.; Grunebaum, E. Safety and efficacy of measles, mumps, and rubella vaccine in patients with DiGeorge syndrome. J. Allergy Clin. Immunol. 2010, 126, 868–869. [Google Scholar] [CrossRef]
- Hofstetter, A.M.; Jakob, K.; Klein, N.P.; Dekker, C.L.; Edwards, K.M.; Halsey, N.A.; Baxter, R.; Williams, S.E.; Graham, P.L., 3rd; LaRussa, P. Live vaccine use and safety in DiGeorge syndrome. Pediatrics 2014, 133, e946–e954. [Google Scholar] [CrossRef]
- Kimberlin, D.W. Red Book: 2018–2021 Report of the Committee on Infectious Diseases, 31st ed.; American Academy of Pediatrics: Itasca, IL, USA, 2018; ISBN 978-161-002-1463. [Google Scholar]
- Rubin, L.G.; Levin, M.J.; Ljungman, P.; Davies, E.G.; Avery, R.; Tomblyn, M.; Bousvaros, A.; Dhanireddy, S.; Sung, L.; Keyserling, H.; et al. 2013 IDSA clinical practice guideline for vaccination of the immunocompromised host. Clin. Infect. Dis. 2014, 58, e44–e100. [Google Scholar] [CrossRef]
- Lee, J.; Jeong, H.; Kim, S.; Yu, J.; Kim, G. National childhood vaccination coverage among children aged 1–3 and 6 years in Korea, 2018. Public Health Wkly. Rep. 2019, 12, 1548–1558. [Google Scholar]
- Lee, S.G.; Jeon, S.Y.; Park, K.S. Rotavirus Vaccine Coverage and Related Factors. J. Korean Soc. Matern. Child Health 2019, 23, 175–184. [Google Scholar] [CrossRef]
- Choi, E.W.; Park, S.E.; Kim, Y.J.; Jo, D.S.; Kim, Y.K.; Eun, B.W.; Lee, T.J.; Lee, J.; Kim, K.H.; Cho, H.K. Immunization Guideline: 2018 Report of the Committee on Infectious Diseases, 9th ed.; The Korean Pediatric Society: Seoul, Republic of Korea, 2018; pp. 32–33. [Google Scholar]
- World Health Organization. Global Manual on Surveillance of Adverse Events Following Immunization, 2016 update ed.; World Health Organization: Geneva, Switzerland, 2014; ISBN 978-92-4-150776-9. [Google Scholar]
- World Health Organization. Regional Office for the Western Pacific. Immunization Safety Surveillance: Guidelines for Managers of Immunization Programmes on Reporting and Investigating Adverse Events Following Immunization; World Health Organization: Geneva, Switzerland, 1999; ISBN 9290611820. [Google Scholar]
- World Health Organization. Causality Assessment of an Adverse Event Following Immunization (AEFI): User Manual for the Revised WHO Classification, 2nd ed.; World Health Oragnization: Geneva, Switzerland, 2019; ISBN 978-92-4-151699-0. [Google Scholar]
- Moylett, E.H.; Wasan, A.N.; Noroski, L.M.; Shearer, W.T. Live viral vaccines in patients with partial DiGeorge syndrome: Clinical experience and cellular immunity. Clin. Immunol. 2004, 112, 106–112. [Google Scholar] [CrossRef]
- Seward, J.F.; Watson, B.M.; Peterson, C.L.; Mascola, L.; Pelosi, J.W.; Zhang, J.X.; Maupin, T.J.; Goldman, G.S.; Tabony, L.J.; Brodovicz, K.G.; et al. Varicella disease after introduction of varicella vaccine in the United States, 1995–2000. JAMA 2002, 287, 606–611. [Google Scholar] [CrossRef] [PubMed]
- Miranda, M.; Matrins, A.T.; Carvalho, S.; Serra-Caetano, A.; Esteves, I.; Marques, J.G. Live Vaccine in Children with DiGeorge/22q11.2 Deletion Syndrome. Acta. Med. Port. 2019, 32, 514–519. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.K.; Lee, Y.K.; Kim, T.E.; Kong, I.; Yang, H.J.; Suh, E.S. Surveillance and compensation claims for adverse events following immunization from 2011 to 2016 in the Republic of Korea. Clin. Exp. Vaccine Res. 2017, 6, 146–155. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | N (%) or Median (IQR) |
|---|---|
| Sex (Male), n (%) | 51 (54.3) |
| Age of disease confirmation, median (IQR), month | 7.9 (0.7–104.3) |
| Chromosome 22q11.2 deletion, n (%) | 94 (100) |
| FISH | 54 (57.4) |
| MLPA | 26 (27.7) |
| Others | 14 (14.9) |
| Cardiac disease, n (%) | 69 (73.4) |
| Ventricular septal defect | 25 (36.2) |
| Tetralogy of Fallot | 22 (31.9) |
| Interrupted aortic arch | 9 (13.0) |
| Others | 13 (18.8) |
| S/p operation | 61 (88.4) |
| Hypocalcemia, n (%) | 30 (31.9) |
| Facial dysmorphism, n (%) | 50 (53.2) |
| Developmental delay, n (%) | 38 (40.4) |
| Epilepsy, n (%) | 6 (6.4) |
| Schizophrenia, n (%) | 2 (2.1) |
| Death, n (%) | 5 (5.3) |
| No. of lymphocyte subsets test, n (%) | 38 (40.4) |
| Age at test, median (IQR), month | 2.8 (1.0–75.5) |
| CD3 ≥ 500 and CD8 ≥ 200 (cells/mm3), n (%) | 30 (79) |
| CD3 (cells/mm3), median (range) | 1425 (536–4234) |
| CD8 (cells/mm3), median (range) | 421 (242–2001) |
| CD4 (cells/mm3), median (range) | 938 (231–3001) |
| CD3 < 500 or CD8 < 200 (cells/mm3), n (%) | 8 (21) |
| CD3 (cells/mm3), median (range) | 378 (205–497) |
| CD8 (cells/mm3), median (range) | 179 (35–198) |
| CD4 (cells/mm3), median (range) | 245 (139–345) |
| <50 CD3 (cells/mm3), n (%) | 0 (0) |
| Mitogen response, n (%) | 2 (2.1) |
| >10 | 1 (50) |
| ≤10 | 1 (50) |
| Thymus screening, n (%) | 28 (29.7) |
| Hypoplasia or absent | 11 (39.3) |
| Normal | 17 (60.7) |
| Group A (n = 8) a | Group B (n = 30) b | Group C (n = 56) c | Total (n = 94) | |||||
|---|---|---|---|---|---|---|---|---|
| Immunized Patients, N (%) | Vaccine Doses (N) | Immunized Patients, N (%) | Vaccine Doses (N) | Immunized Patients, N (%) | Vaccine Doses (N) | Immunized Patients, N (%) | Vaccine Doses (N) | |
| BCG | 4 (50) | 4 | 18 (60) | 18 | 23 (41) | 23 | 45 (48) | 45 |
| Rotavirus | 1 (13) | 2 | 11 (37) | 25 | 11 (20) | 26 | 23 (24) | 53 |
| MMR | 5 (63) | 10 | 22 (73) | 32 | 39 (70) | 59 | 66 (70) | 101 |
| VAR | 5 (63) | 7 | 19 (63) | 20 | 23 (41) | 26 | 47 (50) | 53 |
| LJEV | 3 (38) | 6 | 9 (30) | 17 | 6 (11) | 11 | 18 (19) | 34 |
| Total d | 6 (75) | 29 | 24 (80) | 112 | 43 (77) | 145 | 73 (78) | 286 |
| Group a | Sex | Age (Months) | Vaccination Type | Adverse Events | Interval Day(s) b | Algorithm c | Causality 2019 c | Causality 1999 d |
|---|---|---|---|---|---|---|---|---|
| A | F | 96 | LJEV | fever | 1 | consistent | A1 | very likely |
| A | M | 13 | LJEV | fever (UTI) | 35 | inconsistent | C | unlikely |
| A | M | 13 | LJEV | cough | 35 | indeterminate | B2 | unlikely |
| A | F | 12 | MMR | fever | 8 | indeterminate | B1 | unlikely |
| A | F | 12 | MMR | diarrhea | 8 | indeterminate | B2 | possible |
| A | F | 12 | VAR | diarrhea | 8 | indeterminate | B2 | unlikely |
| A | F | 12 | VAR | fever | 8 | indeterminate | B1 | possible |
| A | F | 12 | LJEV | fever | 8 | indeterminate | B1 | possible |
| A | F | 12 | LJEV | diarrhea | 8 | indeterminate | B2 | unlikely |
| A | F | 3 | BCG | fever (rhinovirus) | 15 | inconsistent | C | unrelated |
| A | F | 3 | BCG | cough (rhinovirus) | 15 | inconsistent | C | unrelated |
| A | M | 12 | MMR | fever | 19 | indeterminate | B1 | unlikely |
| A | M | 12 | MMR | cough | 19 | indeterminate | B2 | unlikely |
| B | M | 3 | BCG | injection site pus e | 47 | consistent | A1 | very likely |
| B | F | 1 | BCG | rash | 94 | indeterminate | B2 | possible |
| B | F | 12 | MMR | fever | 1 | consistent | A1 | very likely |
| B | F | 13 | MMR | fever | 8 | indeterminate | B1 | possible |
| B | M | 59 | MMR | fever | 19 | indeterminate | B2 | unlikely |
| B | F | 16 | MMR | cough | 28 | indeterminate | B2 | unlikely |
| B | F | 16 | MMR | fever | 28 | indeterminate | B2 | unlikely |
| B | F | 12 | VAR | fever | 0 | consistent | A1 | very likely |
| B | F | 13 | VAR | fever | 8 | indeterminate | B1 | possible |
| B | M | 12 | VAR | fever | 13 | indeterminate | B2 | unlikely |
| B | M | 28 | LJEV | fever | 2 | consistent | A1 | very likely |
| B | M | 16 | LJEV | febrile convulsion f | 51 | indeterminate | B2 | unlikely |
| B | M | 0 | BCG | fever (UTI) | 52 | inconsistent | C | unrelated |
| B | F | 6 | BCG | fever (RSV) | 119 | inconsistent | C | unrelated |
| B | F | 6 | BCG | cough (RSV) | 119 | inconsistent | C | unrelated |
| B | M | 7 | Rota | fever (UTI) | 37 | inconsistent | C | unrelated |
| B | F | 7 | Rota | cough | 49 | indeterminate | B2 | unlikely |
| B | F | 7 | Rota | fever | 49 | indeterminate | B2 | unlikely |
| B | M | 12 | MMR | fever | 13 | indeterminate | B2 | unlikely |
| B | M | 12 | MMR | cough (RSV) | 25 | inconsistent | C | unrelated |
| B | M | 12 | MMR | fever (RSV) | 25 | inconsistent | C | unrelated |
| B | M | 13 | MMR | thrombocytopenia g (post cardiac operation condition) | 30 | inconsistent | C | unrelated |
| B | F | 12 | MMR | rash | 33 | indeterminate | B2 | probable |
| B | F | 12 | MMR | thrombocytopenia | 33 | indeterminate | B2 | probable |
| B | F | 12 | MMR | fever | 33 | indeterminate | B2 | unlikely |
| B | M | 56 | MMR | fever (rhinovirus) | 48 | inconsistent | C | unlikely |
| B | M | 12 | VAR | cough (RSV) | 25 | inconsistent | C | unrelated |
| B | M | 12 | VAR | fever (RSV) | 25 | inconsistent | C | unrelated |
| B | F | 12 | VAR | rash | 33 | indeterminate | B1 | probable |
| B | F | 12 | VAR | thrombocytopenia | 33 | indeterminate | B2 | unlikely |
| B | F | 12 | VAR | fever | 33 | indeterminate | B2 | unlikely |
| B | M | 25 | LJEV | fever | 21 | inconsistent | C | unrelated |
| B | F | 28 | LJEV | cough | 21 | indeterminate | B2 | unlikely |
| B | M | 16 | LJEV | fever | 51 | inconsistent | C | unrelated |
| C | M | 13 | MMR | fever | 8 | indeterminate | B1 | unlikely |
| C | M | 27 | LJEV | fever | 1 | consistent | A1 | very likely |
| C | M | 27 | LJEV | diarrhea | 1 | indeterminate | B1 | probable |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lim, S.M.; Shin, J.H.; Baek, J.Y.; Lee, J.Y.; Kang, J.-M.; Ahn, J.G. Safety of Live Immunization in DiGeorge Syndrome: A Retrospective Single-Center Study in Korea, 2005–2021. Vaccines 2022, 10, 2165. https://doi.org/10.3390/vaccines10122165
Lim SM, Shin JH, Baek JY, Lee JY, Kang J-M, Ahn JG. Safety of Live Immunization in DiGeorge Syndrome: A Retrospective Single-Center Study in Korea, 2005–2021. Vaccines. 2022; 10(12):2165. https://doi.org/10.3390/vaccines10122165
Chicago/Turabian StyleLim, Sung Min, Je Hee Shin, Jee Yeon Baek, Ji Young Lee, Ji-Man Kang, and Jong Gyun Ahn. 2022. "Safety of Live Immunization in DiGeorge Syndrome: A Retrospective Single-Center Study in Korea, 2005–2021" Vaccines 10, no. 12: 2165. https://doi.org/10.3390/vaccines10122165
APA StyleLim, S. M., Shin, J. H., Baek, J. Y., Lee, J. Y., Kang, J.-M., & Ahn, J. G. (2022). Safety of Live Immunization in DiGeorge Syndrome: A Retrospective Single-Center Study in Korea, 2005–2021. Vaccines, 10(12), 2165. https://doi.org/10.3390/vaccines10122165





