Higher Immunological Response after BNT162b2 Vaccination among COVID-19 Convalescents—The Data from the Study among Healthcare Workers in an Infectious Diseases Center
Abstract
:1. Introduction
2. Methods
3. Results
4. Subgroup Analyses
5. Discussion
6. Conclusions
- The BNT162b2 vaccine is safe, VAEs may occur; however, in the study, none of these were severe, and none required hospitalization or medical care.
- The proportion of adverse events was comparable irrespective of the level of serological response to the first vaccination, which means that the serological response was not related to the vaccine reaction.
- The BNT162b2 vaccine is effective against symptomatic and severe COVID-19. In addition, none of the workers that acquired a SARS-CoV-2 infection after vaccination required hospitalization or medical care.
- Healthcare workers (HCWs) who had contracted COVID-19 before being vaccinated had a higher antibody response one week and three weeks after the first vaccine dose.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Origin of SARS-CoV-2. Available online: https://apps.who.int/iris/bitstream/handle/10665/332197/WHO-2019-nCoV-FAQ-Virus_origin-2020.1-eng.pdf?sequence=1&isAllowed=y (accessed on 5 August 2022).
- World Health Organisation. WHO Coronavirus (COVID-19). Available online: https://covid19.who.int/ (accessed on 5 August 2022).
- Skrzat-Klapaczyńska, A.; Bieńkowski, C.; Kowalska, J.; Paciorek, M.; Puła, J.; Krogulec, D.; Stengiel, J.; Pawełczyk, A.; Perlejewski, K.; Osuch, S.; et al. The Beneficial Effect of the COVID-19 Vaccine Booster Dose among Healthcare Workers in an Infectious Diseases Center. Vaccines 2022, 10, 552. [Google Scholar] [CrossRef] [PubMed]
- Vaccines and Related Biological Products Advisory Committee Meeting December 10, 2020. FDA Briefing Document Pfizer-BioNTech COVID-19 Vaccine Sponsor: Pfizer and BioNTech. Available online: https://www.fda.gov/media/144246/download (accessed on 17 May 2021).
- COVID-19 Vaccine Tracker. Available online: https://covid19.trackvaccines.org/country/poland/ (accessed on 5 August 2022).
- Gholami, M.; Fawad, I.; Shadan, S.; Rowaiee, R.; Ghanem, H.; Hassan Khamis, A.; Ho, S.B. COVID-19 and healthcare workers: A systematic review and meta-analysis. Int. J. Infect. Dis. 2021, 104, 335–346. [Google Scholar] [CrossRef] [PubMed]
- da Silva, P. Vaccination against COVID-19 in health care workers. Rev. Bras. Med. Trab. 2021, 19, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Rotondo, J.C.; Martini, F.; Maritati, M.; Mazziotta, C.; Di Mauro, G.; Lanzillotti, C.; Barp, N.; Gallerani, A.; Tognon, M.; Contini, C. SARS-CoV-2 Infection: New Molecular, Phylogenetic, and Pathogenetic Insights. Efficacy of Current Vaccines and the Potential Risk of Variants. Viruses 2021, 13, 1687. [Google Scholar] [CrossRef] [PubMed]
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Pérez Marc, G.; Moreira, E.D.; Zerbini, C.; et al. Safety and Efficacy of the BNT162b2 mRNA COVID-19 Vaccine. N. Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef] [PubMed]
- Thompson, M.G.; Burgess, J.L.; Naleway, A.L.; Tyner, H.L.; Yoon, S.K.; Meece, J.; Olsho, L.E.W.; Caban-Martinez, A.J.; Fowlkes, A.; Lutrick, K.; et al. Interim Estimates of Vaccine Effectiveness of BNT162b2 and mRNA-1273 COVID-19 Vaccines in Preventing SARS-CoV-2 Infection Among Health Care Personnel, First Responders, and Other Essential and Frontline Workers—Eight U.S. Locations, December 2020–March 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 495–500. [Google Scholar] [CrossRef]
- Benenson, S.; Oster, Y.; Cohen, M.J.; Nir-Paz, R. BNT162b2 mRNA COVID-19 Vaccine Effectiveness among Health Care Workers. N. Engl. J. Med. 2021, 384, 1775–1777. [Google Scholar] [CrossRef]
- Hall, V.J.; Foulkes, S.; Charlett, A.; Atti, A.; Monk, E.J.M.; Simmons, R.; Wellington, E.; Cole, M.J.; Saei, A.; Oguti, B.; et al. SARS-CoV-2 infection rates of antibody-positive compared with antibody-negative health-care workers in England: A large, multicentre, prospective cohort study (SIREN). Lancet 2021, 397, 1459–1469. [Google Scholar] [CrossRef]
- Regev-Yochay, G.; Amit, S.; Bergwerk, M.; Lipsitch, M.; Leshem, E.; Kahn, R.; Lustig, Y.; Cohen, C.; Doolman, R.; Ziv, A.; et al. Decreased infectivity following BNT162b2 vaccination: A prospective cohort study in Israel. Lancet Reg. Health Eur. 2021, 7, 100150. [Google Scholar] [CrossRef]
- Salo, J.; Hagg, M.; Kortelainen, M.; Leino, T.; Saxell, T.; Siikanen, M.; Saaksvuori, L. The indirect effect of mRNA-based COVID-19 vaccination on healthcare workers’ unvaccinated household members. Nat. Commun. 2022, 13, 1162. [Google Scholar] [CrossRef]
- Spitzer, A.; Angel, Y.; Marudi, O.; Zeltser, D.; Saiag, E.; Goldshmidt, H.; Goldiner, I.; Stark, M.; Halutz, O.; Gamzu, R.; et al. Association of a Third Dose of BNT162b2 Vaccine With Incidence of SARS-CoV-2 Infection Among Health Care Workers in Israel. JAMA 2022, 327, 341–349. [Google Scholar] [CrossRef] [PubMed]
- Goncalves, J.; Juliano, A.M.; Charepe, N.; Alenquer, M.; Athayde, D.; Ferreira, F.; Archer, M.; Amorim, M.J.; Serrano, F.; Soares, H. Secretory IgA and T cells targeting SARS-CoV-2 spike protein are transferred to the breastmilk upon mRNA vaccination. Cell Rep. Med. 2021, 2, 100468. [Google Scholar] [CrossRef] [PubMed]
- Serwis Rzeczypospolitej Polskiej. Available online: https://www.gov.pl/web/szczepimysie/narodowy-program-szczepien-przeciw-COVID-19 (accessed on 19 October 2022).
- Snibe Diagnostic. Available online: https://www.snibe.com/zh_en/en_newsView.aspx?id=647 (accessed on 29 October 2022).
- Infantino, M.; Pieri, M.; Nuccetelli, M.; Grossi, V.; Lari, B.; Tomassetti, F.; Calugi, G.; Pancani, S.; Benucci, M.; Casprini, P.; et al. The WHO International Standard for COVID-19 serological tests: Towards harmonization of anti-spike assays. Int. Immunopharmacol. 2021, 100, 108095. [Google Scholar] [CrossRef] [PubMed]
- Kaneko, S.; Kurosaki, M.; Sugiyama, T.; Takahashi, Y.; Yamaguchi, Y.; Nagasawa, M.; Izumi, N. The dynamics of quantitative SARS-CoV-2 antispike IgG response to BNT162b2 vaccination. J. Med. Virol. 2021, 93, 6813–6817. [Google Scholar] [CrossRef] [PubMed]
- Agrati, C.; Castilletti, C.; Goletti, D.; Meschi, S.; Sacchi, A.; Matusali, G.; Bordoni, V.; Petrone, L.; Lapa, D.; Notari, S.; et al. Coordinate Induction of Humoral and Spike Specific T-Cell Response in a Cohort of Italian Health Care Workers Receiving BNT162b2 mRNA Vaccine. Microorganisms 2021, 9, 1315. [Google Scholar] [CrossRef] [PubMed]
- Kim, N.; Minn, D.; Park, S.; Roh, E.Y.; Yoon, J.H.; Park, H.; Shin, S. Positivity of SARS-CoV-2 Antibodies among Korean Healthy Healthcare Workers 1 and 2 Weeks after Second Dose of Pfizer-BioNTech Vaccination. J. Korean Med. Sci. 2021, 36, e158. [Google Scholar] [CrossRef]
- Sahin, U.; Muik, A.; Vogler, I.; Derhovanessian, E.; Kranz, L.M.; Vormehr, M.; Quandt, J.; Bidmon, N.; Ulges, A.; Baum, A.; et al. BNT162b2 vaccine induces neutralizing antibodies and poly-specific T cells in humans. Nature 2021, 595, 572–577. [Google Scholar] [CrossRef]
- Lustig, Y.; Sapir, E.; Regev-Yochay, G.; Cohen, C.; Fluss, R.; Olmer, L.; Indenbaum, V.; Mandelboim, M.; Doolman, R.; Amit, S.; et al. BNT162b2 COVID-19 vaccine and correlates of humoral immune responses and dynamics: A prospective, single-centre, longitudinal cohort study in health-care workers. Lancet Respir. Med. 2021, 9, 999–1009. [Google Scholar] [CrossRef]
- Kosiorek, P.; Kazberuk, D.E.; Hryniewicz, A.; Milewski, R.; Stroz, S.; Stasiak-Barmuta, A. Systemic COVID-19 Vaccination Enhances the Humoral Immune Response after SARS-CoV-2 Infection: A Population Study from a Hospital in Poland Criteria for COVID-19 Reimmunization Are Needed. Vaccines 2022, 10, 334. [Google Scholar] [CrossRef]
- Zhang, R.; Khong, K.W.; Leung, K.Y.; Liu, D.; Fan, Y.; Lu, L.; Chan, P.C.; Chen, L.; To, K.K.; Chen, H.; et al. Antibody Response of BNT162b2 and CoronaVac Platforms in Recovered Individuals Previously Infected by COVID-19 against SARS-CoV-2 Wild Type and Delta Variant. Vaccines 2021, 9, 1442. [Google Scholar] [CrossRef]
- Tretyn, A.; Szczepanek, J.; Skorupa, M.; Jarkiewicz-Tretyn, J.; Sandomierz, D.; Dejewska, J.; Ciechanowska, K.; Jarkiewicz-Tretyn, A.; Koper, W.; Palgan, K. Differences in the Concentration of Anti-SARS-CoV-2 IgG Antibodies Post-COVID-19 Recovery or Post-Vaccination. Cells 2021, 10, 1952. [Google Scholar] [CrossRef] [PubMed]

| Time of Sample Collection MAIN GROUP | SARS-CoV-2 IgG Antibodies | SARS CoV-2 IgM Antibodies | SARS-CoV-2 IgG S-RBD Antibodies |
|---|---|---|---|
| The day of the first vaccination | + | + | + |
| The day of the second BNT162b2 mRNA vaccination dose | + | + | + |
| 14 days after the day of the second BNT162b2 mRNA vaccination dose | + | + | + |
| 6 months after the day of the second BNT162b2 mRNA vaccination dose | + | - | + |
| The day of the third BNT162b2 mRNA vaccination dose | + | - | + |
| 14 days after the day of the third BNT162b2 mRNA vaccination dose | + | - | + |
| 6 months after the day of the third BNT162b2 mRNA vaccination dose | + | - | + |
| SUBGROUP | |||
| 7 days after the day of the first BNT162b2 mRNA vaccination dose | + | + | + |
| 14 days after he day of the first BNT162b2 mRNA vaccination dose | + | + | + |
| 7 days after the day of the second BNT162b2 mRNA vaccination dose | + | + | + |
| N | IgM Positive, n (%) | N | IgG Positive, n (%) | N | S-RBD Positive, n (%) | |
|---|---|---|---|---|---|---|
| The day of 1st BNT162b2 mRNA dose vaccination, median [IQR] | 211 | 11 (5.2) | 221 | 45 (20.4) | 203 | 54 (26.6) |
| The day of 2nd BNT162b2 mRNA dose vaccination, median [IQR] | 46 | 19 (41.3) | 115 | 22 (19.1) | 114 | 111 (97.4) |
| 14 days after 2nd BNT162b2 mRNA dose vaccination, median [IQR] | 77 | 48 (62.3) | 119 | 20 (16.8) | 121 | 121 (100.0) |
| 6 months after 2nd BNT162b2 mRNA dose vaccination, median [IQR] | 10 | 1 (10.0) | 205 | 34 (16.6) | 209 | 209 (100.0) |
| The day of 3rd BNT162b2 mRNA dose vaccination, median [IQR] | N/A | N/A | 187 | 34 (18.8) | 184 | 184 (100.0) |
| 14 days after 3rd BNT162b2 mRNA dose vaccination, median [IQR] | N/A | N/A | 164 | 27 (16.5) | 165 | 165 (100.0) |
| 6 months after 3rd BNT162b2 mRNA dose vaccination, median [IQR] | N/A | N/A | 169 | 63 (37.3) | 170 | 170 (100.0) |
| Characteristic | N with Available Data | All | High Response N = 7 | Low Response N = 42 | p Value |
|---|---|---|---|---|---|
| VAE after the first vaccine dose, n (%) | 47 | 32 (68.09) | 6 (85.7) | 26 (61.9) | 0.403 |
| VAE after the second vaccine dose, n (%) | 42 | 35 (83.33) | 5 (71.4) | 30 (71.4) | 1.000 |
| VAE after the third vaccine dose, n (%) | 40 | 37 (92.50) | 6 (85.7) | 31 (77.5) | 0.447 |
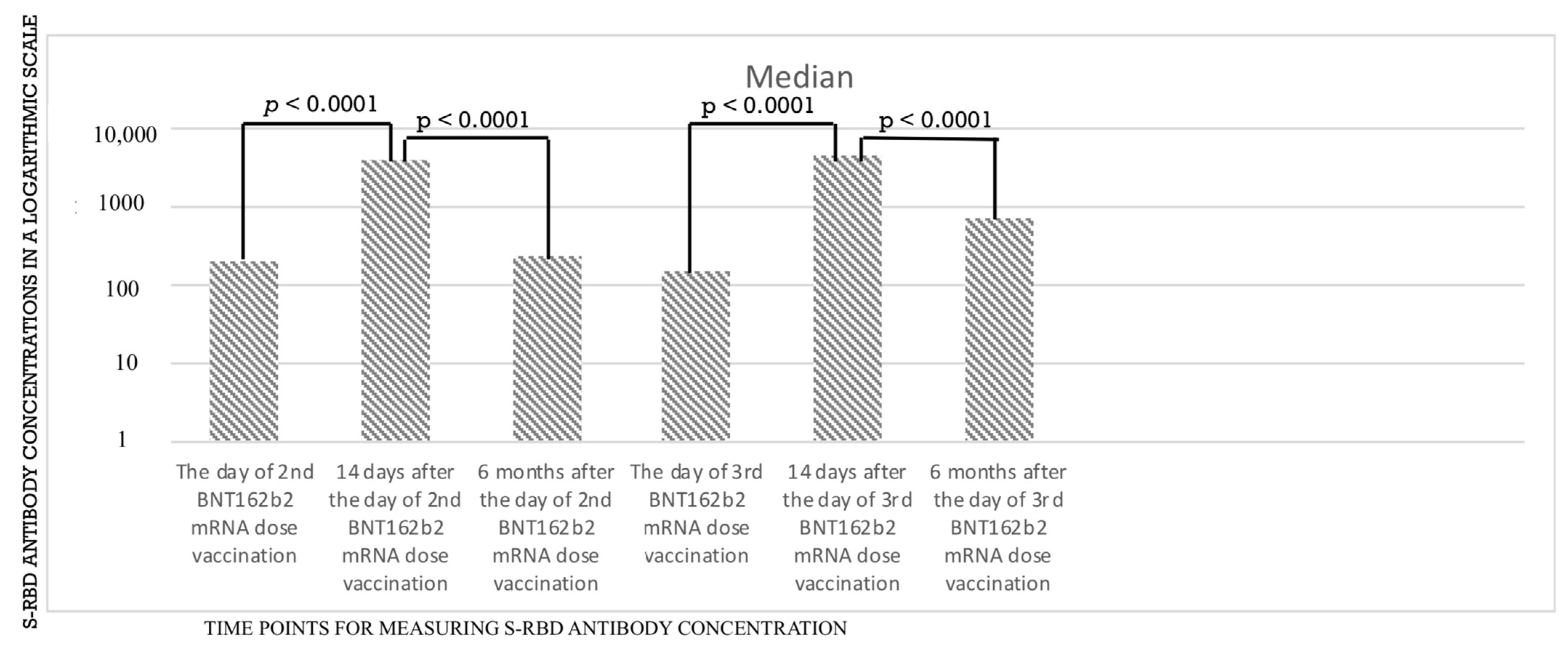
| Time Point | S-RBD (in BAU/mL) |
|---|---|
| Day of the 2nd vaccine dose, median, [IQR] | 226.600 [99.455–433.0] |
| 14 days after the 2nd vaccine dose, median [IQR] | 3338.2 [757.4–5791.0] |
| 6 months after the 2nd vaccine dose, median [IQR] | 224.9 [103.6–353.7] |
| Day of the 3rd vaccine dose, median [IQR] | 170.2 [68.7–396.6] |
| 14 days after the 3rd vaccine dose, median [IQR] | 4525.8 [2804.9–7712.6] |
| 6 months after the 3rd vaccine dose, median [IQR] | 817.9 [402.2–3124.9] |
| Time Point | S-RBD (in BAU/mL) |
|---|---|
| 7 days after the 1st vaccine dose, median, [IQR] | 1.85 [1.41–6.70] |
| 14 days after the 1st vaccine dose, median [IQR] | 77.51 [28.01–257.50] |
| Day of the 2nd vaccine dose, median [IQR] | 198.90 [95.99–338.40] |
| 7 days after the 2nd vaccine dose, median [IQR] | 3846.80 [894.20–7309.50] |
| 14 days after the 2nd vaccine dose, median [IQR] | 3962.70 [2314.30–6465.10] |
| 6 months after the 2nd vaccine dose, median [IQR] | 232.10 [132.30–381.35] |
| Day of the 3rd vaccine dose | 149.58 [77.16–388.62] |
| 14 days after the 3rd vaccine dose, median [IQR] | 4587.50 [3011.20–7478.00] |
| 6 months after the 3rd vaccine dose, median [IQR] | 701.05 [428.40–2265.6] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Skrzat-Klapaczyńska, A.; Kowalska, J.D.; Paciorek, M.; Puła, J.; Bieńkowski, C.; Krogulec, D.; Stengiel, J.; Pawełczyk, A.; Perlejewski, K.; Osuch, S.; et al. Higher Immunological Response after BNT162b2 Vaccination among COVID-19 Convalescents—The Data from the Study among Healthcare Workers in an Infectious Diseases Center. Vaccines 2022, 10, 2158. https://doi.org/10.3390/vaccines10122158
Skrzat-Klapaczyńska A, Kowalska JD, Paciorek M, Puła J, Bieńkowski C, Krogulec D, Stengiel J, Pawełczyk A, Perlejewski K, Osuch S, et al. Higher Immunological Response after BNT162b2 Vaccination among COVID-19 Convalescents—The Data from the Study among Healthcare Workers in an Infectious Diseases Center. Vaccines. 2022; 10(12):2158. https://doi.org/10.3390/vaccines10122158
Chicago/Turabian StyleSkrzat-Klapaczyńska, Agata, Justyna Dominika Kowalska, Marcin Paciorek, Joanna Puła, Carlo Bieńkowski, Dominika Krogulec, Jarosław Stengiel, Agnieszka Pawełczyk, Karol Perlejewski, Sylwia Osuch, and et al. 2022. "Higher Immunological Response after BNT162b2 Vaccination among COVID-19 Convalescents—The Data from the Study among Healthcare Workers in an Infectious Diseases Center" Vaccines 10, no. 12: 2158. https://doi.org/10.3390/vaccines10122158
APA StyleSkrzat-Klapaczyńska, A., Kowalska, J. D., Paciorek, M., Puła, J., Bieńkowski, C., Krogulec, D., Stengiel, J., Pawełczyk, A., Perlejewski, K., Osuch, S., Radkowski, M., & Horban, A. (2022). Higher Immunological Response after BNT162b2 Vaccination among COVID-19 Convalescents—The Data from the Study among Healthcare Workers in an Infectious Diseases Center. Vaccines, 10(12), 2158. https://doi.org/10.3390/vaccines10122158









