Widening Disparities in Teen HPV Vaccinations during COVID-19 Pandemic: A Case Study from Veneto Region (Italy)
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Shet, A.; Carr, K.; Danovaro-Holliday, M.C.; Sodha, S.V.; Prosperi, C.; Wunderlich, J.; Wonodi, C.; Reynolds, H.W.; Mirza, I.; Gacic-Dobo, M.; et al. Impact of the SARS-CoV-2 pandemic on routine immunisation services: Evidence of disruption and recovery from 1 70 countries and territories. Lancet Glob. Health 2022, 10, e186–e194. [Google Scholar] [CrossRef]
- Daniels, V.; Saxena, K.; Roberts, C.; Kothari, S.; Corman, S.; Yao, L.; Niccolai, L. Impact of reduced human papillomavirus vaccination coverage rates due to COVID-19 in the United States: A model based analysis. Vaccine 2021, 39, 2731–2735. [Google Scholar] [CrossRef] [PubMed]
- Ryan, G.; Gilbert, P.A.; Ashida, S.; Charlton, M.E.; Scherer, A.; Askelson, N.M. Challenges to Adolescent HPV Vaccination and Implementation of Evidence-Based Interventions to Promote Vaccine Uptake During the COVID-19 Pandemic: “HPV Is Probably Not at the Top of Our List”. Prev. Chronic Dis. 2022, 19, E15. [Google Scholar] [CrossRef] [PubMed]
- Gabutti, G.; d’Anchera, E.; De Motoli, F.; Savio, M.; Stefanati, A. Human Papilloma Virus Vaccination: Focus on the Italian Situation. Vaccines 2021, 9, 1374. [Google Scholar] [CrossRef] [PubMed]
- Fisher, H.; Trotter, C.L.; Audrey, S.; MacDonald-Wallis, K.; Hickman, M. Inequalities in the uptake of human papillomavirus vaccination: A systematic review and meta-analysis. Int. J. Epidemiol. 2013, 42, 896–908. [Google Scholar] [CrossRef]
- Brearley, L.; Eggers, R.; Steinglass, R.; Vandelaer, J. Applying an equity lens in the Decade of Vaccines. Vaccine 2013, 31 (Suppl. 2), B103–B107. [Google Scholar] [CrossRef]
- Radisic, G.; Chapman, J.; Flight, I.; Wilson, C. Factors associated with parents’ attitudes to the HPV vaccination of their adolescent sons: A systematic review. Prev. Med. 2017, 95, 26–37. [Google Scholar] [CrossRef]
- Newman, P.A.; Logie, C.H.; Lacombe-Duncan, A.; Baiden, P.; Tepjan, S.; Rubincam, C.; Doukas, N.; Asey, F. Parents’ uptake of human papillomavirus vaccines for their children: A systematic review and meta-analysis of observational studies. BMJ Open 2018, 8, e019206. [Google Scholar] [CrossRef]
- Kempe, A.; O’Leary, S.T.; Markowitz, L.E.; Crane, L.A.; Hurley, L.P.; Brtnikova, M.; Beaty, B.L.; Meites, E.; Stokley, S.; Lindley, M.C. HPV Vaccine Delivery Practices by Primary Care Physicians. Pediatrics 2019, 144, e20191475. [Google Scholar] [CrossRef]
- Napolitano, F.; Navaro, M.; Vezzosi, L.; Santagati, G.; Angelillo, I.F. Primary care pediatricians’ attitudes and practice towards HPV vaccination: A nationwide survey in Italy. PLoS ONE 2018, 13, e0194920. [Google Scholar] [CrossRef]
- Sackey, M.E.; Markey, K.; Grealish, A. Healthcare professional’s promotional strategies in improving Human papillomavirus (HPV) vaccination uptake in adolescents: A systematic review. Vaccine 2022, 40, 2656–2666. [Google Scholar] [CrossRef] [PubMed]
- Sackey, M.E.; Markey, K.; Grealish, A. Healthcare professional’s promotional strategies in improving Human papillomavirus (HPV) vaccination uptake in adolescents: A systematic review. Vaccine 2022, 40, 2656–2666. [Google Scholar] [CrossRef] [PubMed]
- Kulczycki, A.; Qu, H.; Shewchuk, R. Recommend, but also Discuss: Different Patterns of Physician-Perceived Barriers to Discussing HPV Vaccination and Their Association with Vaccine Administration in 11–12 Year-Old Girls. Matern. Child Health J. 2016, 20, 2539–2547. [Google Scholar] [CrossRef]
- Ji, C.; Piché-Renaud, P.P.; Apajee, J.; Stephenson, E.; Forte, M.; Friedman, J.N.; Science, M.; Zlotkin, S.; Morris, S.K.; Tu, K. Impact of the COVID-19 pandemic on routine immunization coverage in children under 2 years old in Ontario, Canada: A retrospective cohort study. Vaccine 2002, 40, 1790–1798. [Google Scholar] [CrossRef] [PubMed]
- Hoang, U.; de Lusignan, S.; Joy, M.; Sherlock, J.; Williams, J.; Bankhead, C.; Howsam, G.; Thomas, M.; Snape, M.D.; Hobbs, F.D.R.; et al. National rates and disparities in childhood vaccination and vaccine-preventable disease during the COVID-19 pandemic: English sentinel network retrospective database study. Arch. Dis. Child. 2022, 107, 733–739. [Google Scholar] [CrossRef] [PubMed]
- Moreno-Montoya, J.; Ballesteros, S.M.; Rojas Sotelo, J.C.; Bocanegra Cervera, C.L.; Barrera-López, P.; De la Hoz-Valle, J.A. Impact of the COVID-19 pandemic on routine childhood immunisation in Colombia. Arch. Dis Child. 2022, 107, e4. [Google Scholar] [CrossRef]
- Spencer, N.; Markham, W.; Johnson, S.; Arpin, E.; Nathawad, R.; Gunnlaugsson, G.; Homaira, N.; Rubio, M.L.M.; Trujillo, C.J. The Impact of COVID-19 Pandemic on Inequity in Routine Childhood Vaccination Coverage: A Systematic Review. Vaccines 2022, 10, 1013. [Google Scholar] [CrossRef]
- Rosano, A.; Pacelli, B.; Zengarini, N.; Costa, G.; Cislaghi, C.; Caranci, N. Aggiornamento e revisione dell’indice di deprivazione italiano 2011 a livello di sezione di censimento [Update and review of the 2011 Italian deprivation index calculated at the census section level]. Epidemiol. Prev. 2020, 44, 162–170. [Google Scholar]
- Merlo, J.; Wagner, P.; Ghith, N.; Leckie, G. An Original Stepwise Multilevel Logistic Regression Analysis of Discriminatory Accuracy: The Case of Neighbourhoods and Health. PLoS ONE 2016, 11, e0153778. [Google Scholar] [CrossRef]
- Norbury, M.; Fawkes, N.; Guthrie, B. Impact of the GP contract on inequalities associated with influenza retrospective population-database analysis. Br. J. Gen. Pract. 2011, 61, e379–e385. [Google Scholar] [CrossRef]
- Ackerson, B.K.; Sy, L.S.; Glenn, S.C.; Qian, L.; Park, C.H.; Riewerts, R.J.; Jacobsen, S.J. Pediatric Vaccination During the COVID-19 Pandemic. Pediatrics 2021, 148, e2020047092. [Google Scholar] [CrossRef] [PubMed]
- de Munter, A.C.; Klooster, T.M.S.T.; van Lier, A.; Akkermans, R.; de Melker, H.E.; Ruijs, W.L.M. Determinants of HPV-vaccination uptake and subgroups with a lower uptake in the Netherlands. BMC Public Health 2021, 21, 1848. [Google Scholar] [CrossRef] [PubMed]
- Dixon, B.E.; Zimet, G.D.; Xiao, S.; Tu, W.; Lindsay, B.; Church, A.; Downs, S.M. An educational intervention to improve HPV vaccination: A cluster randomized trial. Pediatrics 2019, 143, e20181457. [Google Scholar] [CrossRef]
- Brewer, N.T.; Hall, M.E.; Malo, T.L.; Gilkey, M.B.; Quinn, B.; Lathren, C. Announcements versus conversations to improve HPV vaccination coverage: A randomized trial. Pediatrics 2017, 139, e20161764. [Google Scholar] [CrossRef]
- Dempsey, A.F.; Pyrznawoski, J.; Lockhart, S.; Barnard, J.; Campagna, E.J.; Garrett, K.; Fisher, A.; Dickinson, L.M.; O’Leary, S.T. Effect of a health care professional communication training intervention on adolescent human papillomavirus vaccination: A cluster randomized clinical trial. JAMA Pediatr. 2018, 172, e180016. [Google Scholar] [CrossRef] [PubMed]
- Szilagyi, P.G.; Humiston, S.G.; Stephens-Shields, A.J.; Localio, R.; Breck, A.; Kelly, M.K.; Wright, M.; Grundmeier, R.W.; Albertin, C.; Shone, L.P.; et al. Effect of Training Pediatric Clinicians in Human Papillomavirus Communication Strategies on Human Papillomavirus Vaccination Rates: A Cluster Randomized Clinical Trial. JAMA Pediatr. 2021, 175, 901–910. [Google Scholar] [CrossRef]
- NHS England and NHS Improvement. Standard General Medical Services Contract. January 2022. Available online: https://www.england.nhs.uk/wp-content/uploads/2022/01/B1210_i_Standard-General-Medical-Services-Contract-06012022.pdf (accessed on 19 January 2022).
- Gilkey, M.B.; Bednarczyk, R.A.; Gerend, M.A.; Kornides, M.L.; Perkins, R.B.; Saslow, D.; Sienko, J.; Zimet, G.D.; Brewer, N.T. Getting Human Papillomavirus Vaccination Back on Track: Protecting Our National Investment in Human Papillomavirus Vaccination in the COVID-19 Era. J. Adolesc. Health 2020, 67, 633–634. [Google Scholar] [CrossRef]
- Cates, J.R.; Diehl, S.J.; Crandell, J.L.; Coyne-Beasley, T. Intervention effects from a social marketing campaign to promote HPV vaccination in preteen boys. Vaccine 2014, 32, 4171–4178. [Google Scholar] [CrossRef]
- Feiring, B.; Laake, I.; Molden, T.; Cappelen, I.; Håberg, S.E.; Magnus, P.; Steingrímsdóttir, Ó.A.; Strand, B.H.; Stålcrantz, J.; Trogstad, L. Do parental education and income matter? A nationwide register-based study on HPV vaccine uptake in the school-based immunisation programme in Norway. BMJ Open 2015, 5, e006422. [Google Scholar] [CrossRef]
- Sinka, K.; Kavanagh, K.; Gordon, R.; Love, J.; Potts, A.; Donaghy, M.; Robertson, C. Achieving high and equitable coverage of adolescent HPV vaccine in Scotland. J. Epidemiol. Community Health 2014, 68, 57–63. [Google Scholar] [CrossRef]
- Potts, A.; Sinka, K.; Love, J.; Gordon, R.; McLean, S.; Malcolm, W.; Ross, D.; Donaghy, M. High uptake of HPV immunisation in Scotland—Perspectives on maximising uptake. Euro Surveill. 2013, 18, 20593. [Google Scholar] [CrossRef] [PubMed]
- Lefevere, E.; Theeten, H.; Hens, N.; De Smet, F.; Top, G.; Van Damme, P. From non school-based, co-payment to school-based, free Human Papillomavirus vaccination in Flanders (Belgium): A retrospective cohort study describing vaccination coverage, age-specific coverage and socio-economic inequalities. Vaccine 2015, 33, 5188–5195. [Google Scholar] [CrossRef] [PubMed]
- Boyce, T.; Holmes, A. Addressing health inequalities in the delivery of the human papillomavirus vaccination programme: Examining the role of the school nurse. PLoS ONE 2012, 7, e43416. [Google Scholar] [CrossRef] [PubMed]
- Icardi, G.; Costantino, C.; Guido, M.; Zizza, A.; Restivo, V.; Amicizia, D.; Tassinari, F.; Piazza, M.F.; Paganino, C.; Casuccio, A.; et al. Burden and Prevention of HPV. Knowledge, Practices and Attitude Assessment Among Pre-Adolescents and their Parents in Italy. Curr. Pharm. Des. 2020, 26, 326–342. [Google Scholar] [CrossRef]
- Costantino, C.; Amodio, E.; Vitale, F.; Trucchi, C.; Maida, C.M.; Bono, S.E.; Caracci, F.; Sannasardo, C.E.; Scarpitta, F.; Vella, C.; et al. Human Papilloma Virus Infection and Vaccination: Pre-Post Interven-tion Analysis on Knowledge, Attitudes and Willingness to Vaccinate Among Preadolescents Attending Secondary Schools of Palermo, Sicily. Int. J. Environ. Res. Public Health 2020, 17, 5362. [Google Scholar] [CrossRef]
- Crocker-Buque, T.; Edelstein, M.; Mounier-Jack, S. Interventions to reduce inequalities in vaccine uptake in children and adolescents aged <19 years: A systematic review. J. Epidemiol. Community Health 2017, 71, 87–97. [Google Scholar]
| 2006 Cohort, Vaccinated by Dept. of Prevention | 2008 Cohort, Vaccinated by PCPs (Jul 2021–April 2022) | Chi2 | |||||
|---|---|---|---|---|---|---|---|
| N | % | N | % | Value; df | p | ||
| Gender | Female | 1268 | 46.0% | 1066 | 48.3% | 2.46; 1 df | 0.117 |
| Male | 1486 | 54.0% | 1142 | 51.7% | |||
| Citizenship | Italian | 205 | 7.4% | 159 | 7.2% | 0.11; 1 df | 0.745 |
| Foreign | 2549 | 92.6% | 2049 | 92.8% | |||
| North African | No | 2735 | 99.3% | 2155 | 97.6% | 25.1; 1 df | 0.000 |
| Yes | 19 | 0.7% | 53 | 2.4% | |||
| Municipal deprivation index | 1st tertile | 894 | 32.5% | 721 | 32.7% | 4.54; 3 df | 0.209 |
| 2nd tertile | 1009 | 36.6% | 792 | 35.9% | |||
| 3rd tertile | 756 | 27.5% | 639 | 28.9% | |||
| Missing | 95 | 3.4% | 56 | 2.5% | |||
| Vaccinated for COVID-19 (Jul 2021–April 2022) | No | - | - | 653 | 29.6% | - | - |
| Yes | - | - | 1555 | 70.4% | |||
| COVID-19 positive (Jul 2021–April 2022) | No | - | - | 1394 | 63.1% | - | - |
| Yes | - | - | 814 | 36.9% | |||
| Males | Female | Total | RR Males vs. Females | 2008 vs. 2006 Cohort | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | RR | IC 95% | RRR | IC 95% | ||||
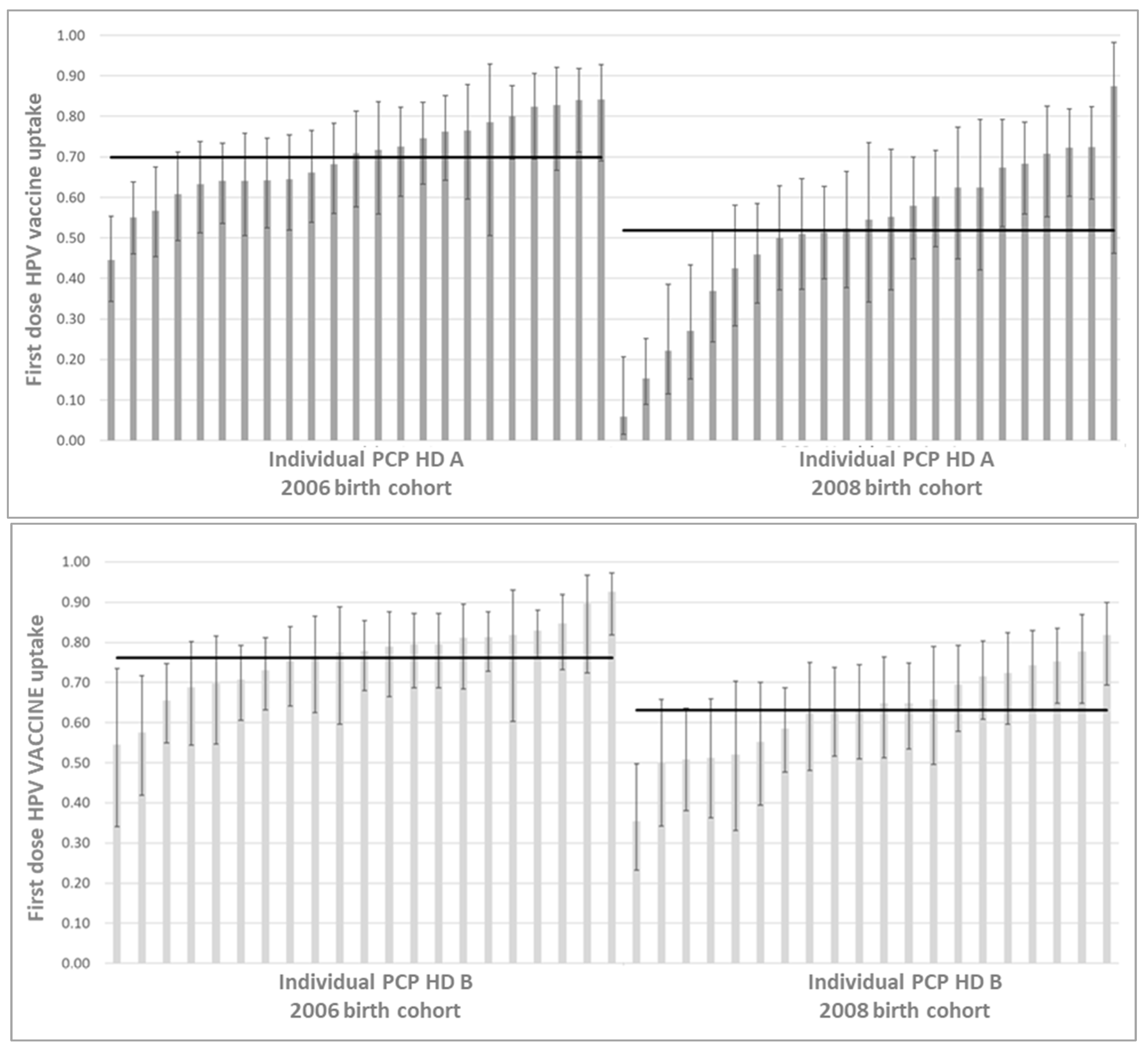
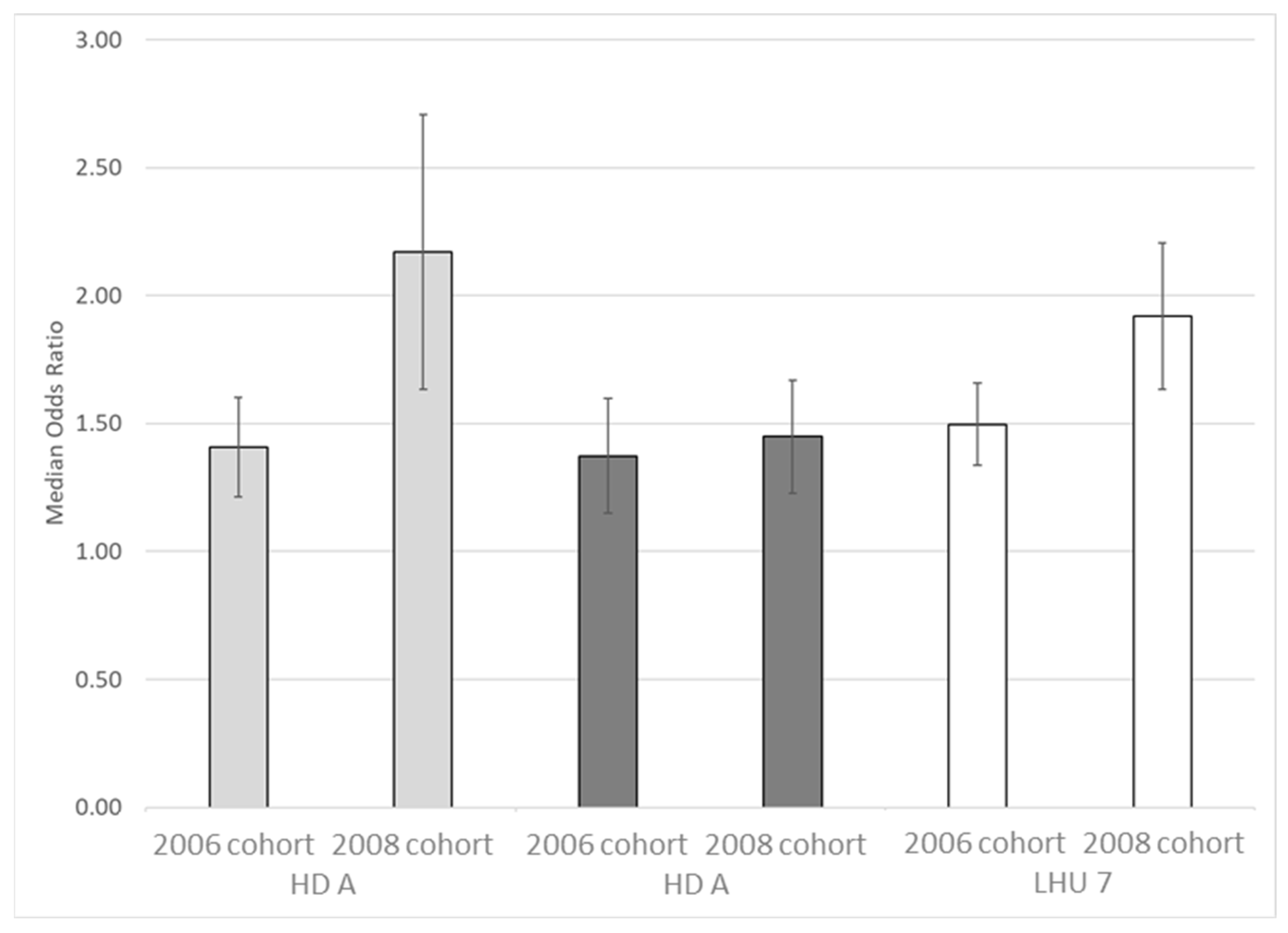
| HD A | 2006 Cohort | 471 | 65% | 419 | 69% | 890 | 67% | 0.93 | 0.87 | 1.01 | 0.85 | 0.73 | 0.98 |
| 2008 Cohort | 219 | 44% | 253 | 57% | 472 | 50% | 0.77 | 0.68 | 0.88 | ||||
| HD B | 2006 Cohort | 577 | 76% | 519 | 78% | 1096 | 77% | 0.97 | 0.92 | 1.03 | 0.87 | 0.78 | 0.96 |
| 2008 Cohort | 380 | 59% | 429 | 69% | 809 | 64% | 0.86 | 0.79 | 0.93 | ||||
| LHU 7 | 2006 Cohort | 1048 | 71% | 938 | 74% | 1986 | 72% | 0.95 | 0.91 | 1.00 | 0.86 | 0.79 | 0.94 |
| 2008 Cohort | 599 | 52% | 682 | 64% | 1281 | 58% | 0.82 | 0.76 | 0.88 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Perin, L.; Dal Zotto, A.; Savio, M.; Stano, A.; Bulegato, L.; Tribbia, L.; Donà, R.; Tomasi, M.; Fietta, S.; Ferro, A.; et al. Widening Disparities in Teen HPV Vaccinations during COVID-19 Pandemic: A Case Study from Veneto Region (Italy). Vaccines 2022, 10, 2120. https://doi.org/10.3390/vaccines10122120
Perin L, Dal Zotto A, Savio M, Stano A, Bulegato L, Tribbia L, Donà R, Tomasi M, Fietta S, Ferro A, et al. Widening Disparities in Teen HPV Vaccinations during COVID-19 Pandemic: A Case Study from Veneto Region (Italy). Vaccines. 2022; 10(12):2120. https://doi.org/10.3390/vaccines10122120
Chicago/Turabian StylePerin, Luca, Alessandra Dal Zotto, Marta Savio, Antonio Stano, Lorenzo Bulegato, Luca Tribbia, Roberta Donà, Matilde Tomasi, Silvia Fietta, Antonio Ferro, and et al. 2022. "Widening Disparities in Teen HPV Vaccinations during COVID-19 Pandemic: A Case Study from Veneto Region (Italy)" Vaccines 10, no. 12: 2120. https://doi.org/10.3390/vaccines10122120
APA StylePerin, L., Dal Zotto, A., Savio, M., Stano, A., Bulegato, L., Tribbia, L., Donà, R., Tomasi, M., Fietta, S., Ferro, A., Baldo, V., Saugo, M., & Cocchio, S. (2022). Widening Disparities in Teen HPV Vaccinations during COVID-19 Pandemic: A Case Study from Veneto Region (Italy). Vaccines, 10(12), 2120. https://doi.org/10.3390/vaccines10122120








