Abstract
Background: We estimated real-world vaccine effectiveness (VE) against COVID-19 infection, hospitalization, ICU admission, and death up to 13 months after vaccination. VE before and after the emergence of Omicron was investigated. Methods: We used registered data from the entire Swedish population above age 12 (n = 9,153,456). Cox regression with time-varying exposure was used to estimate weekly/monthly VE against COVID-19 outcomes from 27 December 2020 to 31 January 2022. The analyses were stratified by age, sex, and vaccine type (BNT162b2, mRNA-1273, and AZD1222). Results: Two vaccine doses offered good long-lasting protection against infection before Omicron (VE were above 85% for all time intervals) but limited protection against Omicron infection (dropped to 43% by week four and no protection by week 14). For severe COVID-19 outcomes, higher VE was observed during the entire follow-up period. Among individuals above age 65, the mRNA vaccines showed better VE against infection than AZD1222 but similar high VE against hospitalization. Conclusions: Our findings provide strong evidence for long-term maintained protection against severe COVID-19 by the basic two-dose schedule, supporting more efforts to encourage unvaccinated persons to get the basic two doses, and encourage vaccinated persons to get a booster to ensure better population-level protection.
1. Introduction
With the rapid evolution of SARS-CoV-2 and vaccine approvals [1,2], concerns remain about long-term vaccine effectiveness (VE) against new variants and for newly approved vaccines. A meta-analysis of 18 studies until November 2021 reported waning VE against COVID-19 infection from 83% in the first month to 22% at five months or longer. Effectiveness against hospitalization or more severe outcomes was higher [3]. However, the meta-analysis did not include the period with Omicron, which was first detected in November 2021 and quickly became the dominant variant globally [4,5]. A rapid increase in COVID-19 infections, even in vaccinated populations, was seen in many countries and triggered concerns about the effectiveness of approved vaccines against Omicron. Early laboratory data also reported lower antibody response to Omicron than other strains of SARS-CoV-2 [6,7]. Several early studies with real-world settings further revealed lower VE and faster waning against Omicron infection in the UK, Qatar, and Malaysia [8,9,10].
In Sweden, vaccination was initiated in the elderly population on 27 December 2020 and reached larger and younger populations in 2021 and 2022 [11]. We used comprehensive Swedish register data to estimate the time-varying VE in reducing the risks of COVID-19 infection, hospitalization, intensive care unit (ICU) admission, and death in a 13-month follow-up and compared the pattern of time-varying VE before and after the emergence of Omicron.
2. Material and Methods
2.1. Study Design and Population
This study is part of the RECOVAC (Register-based large-scale national population study to monitor COVID-19 vaccination effectiveness and safety) study within the larger SCIFI-PEARL (Swedish COVID-19 Investigation for Future Insights—a Population Epidemiology Approach using Register Linkage) project with regularly updated data from various National Registers [12]. The current study included the whole Swedish population ≥ 12 years old in 2021, representing the approved population for COVID-19 vaccination in Sweden. We followed the cohort from 1 January 2020 (before the start of the pandemic) to 31 January 2022, with vaccines being introduced during the follow-up (first vaccination on 27 December 2020). The end of follow-up coincides with the termination of large-scale COVID-19 polymerase chain reactions (PCR) testing in Sweden. For COVID-19 ICU admission, the end of follow-up was 31 December 2021 due to data availability. The first Omicron case was diagnosed on 29 November 2021 in Sweden and quickly became the dominating variant (Figure S1) [13]. Consequently, we also subdivided the follow-up into before and after 1 December 2021, representing the emergence of Omicron. This study focused on two doses of vaccine, which was the originally recommended basic COVID-19 vaccination strategy.
2.2. Data Sources
We obtained data from multiple National Registers. Vaccination data came from the National Vaccination Register (NVR). All individuals with their first positive SARS-CoV-2 PCR test were identified from SmiNet, the national register of notifiable communicable diseases. PCR testing was introduced in 2020, and large-scale testing started in mid-2020. All individuals with symptoms of COVID-19 were encouraged to get tested, free of cost, until February 2022. COVID-19 diagnoses from outpatient specialist visits and inpatient care records were obtained from the Swedish National Patient Registry (NPR). COVID-19-related ICU data came from the Swedish Intensive care Register (SIR). The date and cause of death were obtained from the Register of Total Population (RTB) and the National Cause-of-Death Register (NCDR).
A complete medical history from 2015 was obtained from NPR and drug history for prescription drugs from 2018 from the National Prescribed Drug Register (NPDR). Sociodemographic data, including education, family situation, income, and occupation from 2015, were obtained from Statistics Sweden (SCB). Information on elderly subjects living at special care facilities and/or receiving home care services was obtained from the National Social Service Register.
3. Exposure and Outcomes
The exposure variables were vaccination status (unvaccinated, dose one, dose two), time intervals after each vaccination, and different vaccines (BNT162b2, mRNA-1273, and AZD1222), based on data from NVR. The first dose was defined as each individual’s first record in NVR. The second and third doses were defined as the following records with a predefined minimum time gap between doses (details see Section S1 in Supplemental Material).
Four different COVID-19 outcomes were investigated: COVID-19 infection; hospitalization; ICU admission; and death. COVID-19 infection was defined as the first of either a positive PCR test from SmiNet, a COVID-19 diagnosis code (ICD10: U07.1/U07.2) from NPR, an ICU admission from SIR, or death due to COVID-19 (underlying or contributing cause of death) from NCDR. Most COVID-19 infection cases (98.4%) were defined by positive PCR tests. The onset date of infection was set to two days before the registered date of any component event based on an estimated minimum incubation time [14]. For hospitalization and severe COVID-19 outcomes (ICU admission and death), the actual, registered date was used as the event date.
4. Covariates
The procedure of covariate selection was performed in 10% random samples of the data due to computational challenges related to the large population and dataset (Section S3, Table S1). We included the following covariates in the final models: age (modeled by restricted cubic spline with four knots), sex, country of birth (Sweden/other countries), health care workers (yes/no), income (tertiles of the study populations), education (primary, secondary, tertiary, unknown), marital status (married, unmarried, unknown), living at special housing and/or receiving home services for the elderly (yes/no), and prior comorbidities and treatments (yes/no). Prior comorbidities, including cardiovascular diseases, stroke, hypertension, diabetes, obstructive respiratory diseases, chronic kidney diseases, obesity, autoimmune diseases, dementia, psychiatric conditions, and cancer, were defined based on five-year prior medical history from NPR and prior treatments based on one-year prior prescription drug history from NPDR. Other covariates were defined with information retrieved from Statistics Sweden (Section S2).
5. Statistical Analysis
We studied the first occurrence of each outcome during the pandemic; therefore, the VE estimates apply to the first occurrence of an outcome event after vaccination, compared to unvaccinated individuals, in individuals previously free of this event.
Cox proportional hazard models with time-varying exposure were used [15]. In the model, each individual’s follow-up time was first divided according to vaccination status (unvaccinated, first dose, and second dose), and then vaccination exposure periods were further divided into time intervals after each dose until the transition to the next dose (Section S3). Since the fine division of follow-up time was computationally challenging, some modeling steps were performed in 10% random samples of the data to support the final full-scale analyses (Section S3, Tables S1 and S2).
This paper focused on the VE for two doses of vaccine. In this analysis, the time period under the first dose was treated as a loss to follow-up, meaning subjects were observed during the unvaccinated period (since the study started to the time when receiving their first dose) and then again observed when receiving their second dose to the end of follow up, which occurred at an outcome event or censoring that is defined as third dose, emigration, death, or study ended, whichever came first. We also estimated the VE for one dose and reported results in the Appendix (Section S3, Tables S3 and S4).
To explore and illustrate VE trends in a smoother manner, we used an unrestricted cubic spline with five selected knots in extended Cox regression. We chose an unrestricted cubic spline for more flexibility in the two tails to adequately reflect the real-world data trends and ensure a better model fit. To cover the follow-up time since vaccination well, the five knots were selected at the 20th, 35th, 65th, 95th, and 99th percentiles.
We estimated time-varying VE for the entire follow-up, for the period before Omicron (until 30 November 2021) and for the Omicron period, respectively. For analysis of the Omicron period, we modeled the entire follow-up period, but only events after 1 December 2021 were considered as incident cases for estimation, and individuals with earlier events were censored at their event.
Additionally, stratified analyses were performed for COVID-19 infection and hospitalization by sex or age group (12–17, 18–39, 40–59, 60–64, 65–79, and 80+) and in subjects who received two doses of homologous BNT162b2, mRNA-1273, or AZD1222. As AZD1222 was primarily used in older individuals, stratified analyses were restricted to those aged 65 and older.
From the estimated hazard ratios (HR), results were presented as VE with 95% confidence intervals (CI), with VE calculated as 100 × (1 − HR). Chi-square tests were used to check the model fit, and all models showed p values < 0.0001. All analyses were performed in STATA MP 17 (StataCorp. 2021. Stata: Release 17).
6. Results
6.1. Study Population
Among 9,153,456 study individuals, 15% remained unvaccinated during the entire study period, 85% had at least one dose of vaccine, 82% had two doses, and 45% had ≥three doses as of 31 January 2022 (Table 1). Most individuals received two doses of BNT162b2 (78%) or mRNA-1273 (12%). Only 8% had two doses of AZD1222, and most (86%) were ≥65 years (Table 2). The average interval between the first and second and second and third doses was seven and 28 weeks, respectively. For homologous AZD1222, the interval between the first and second doses was slightly longer (ten weeks) and between the second and third doses slightly shorter (25 weeks) (Table S5). Vaccine uptake trends are presented in Figures S2 and S3.

Table 1.
Sociodemographic and comorbidity characteristics of the study cohort according to vaccine uptake and COVID-19 outcomes by 31 January 2022.

Table 2.
Sociodemographic and comorbidity characteristics of people receiving two doses according to vaccine type.
From 1 January 2020 to 31 January 2022, 2,002,024 first-time COVID-19 infections were reported (Table 1), representing 22% of the cohort. The corresponding figures for hospitalizations, ICU admissions, and deaths were 0.9%, 0.1%, and 0.2%, respectively.
6.2. VE during a 13-Month Follow-Up Period
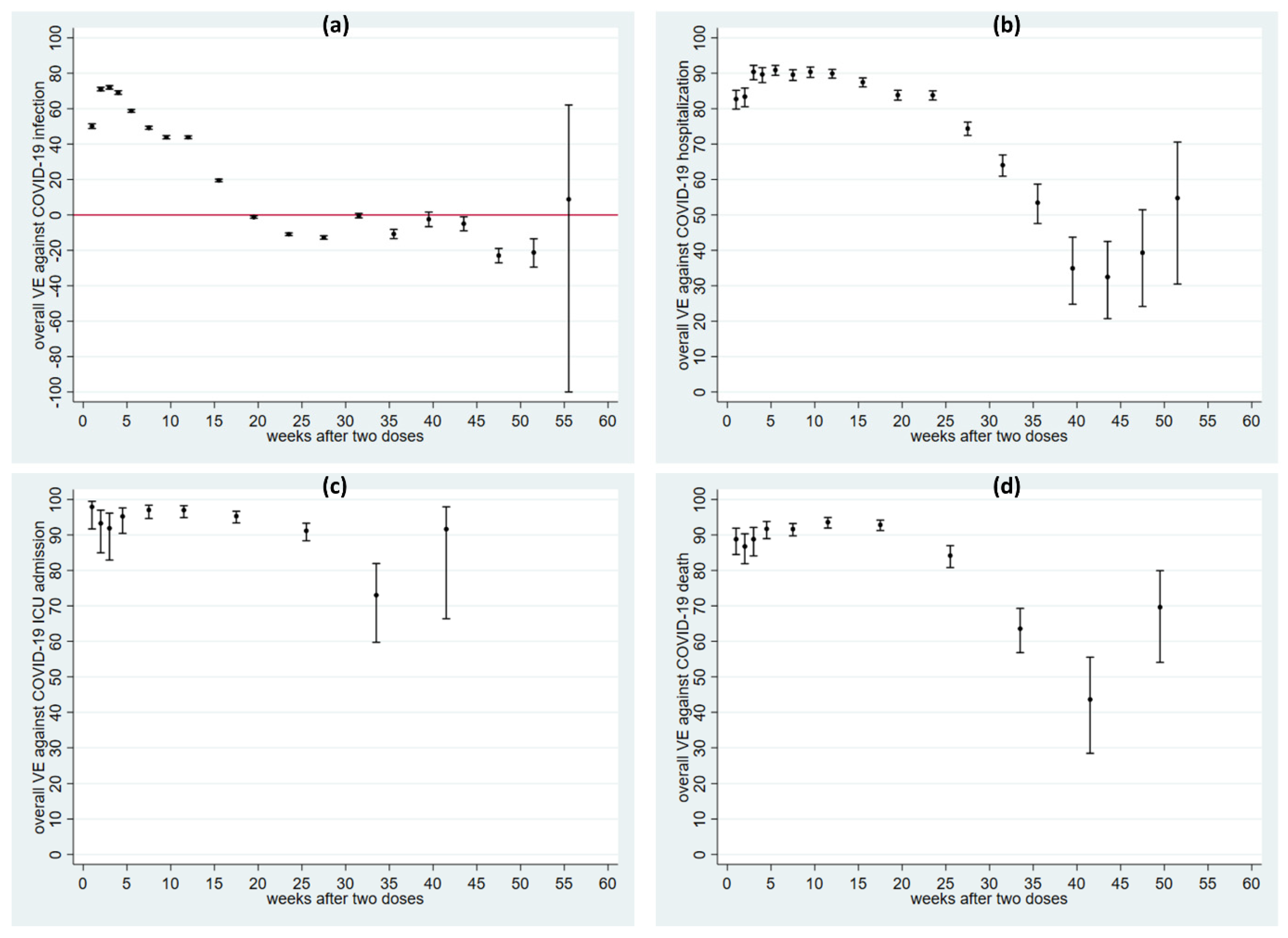
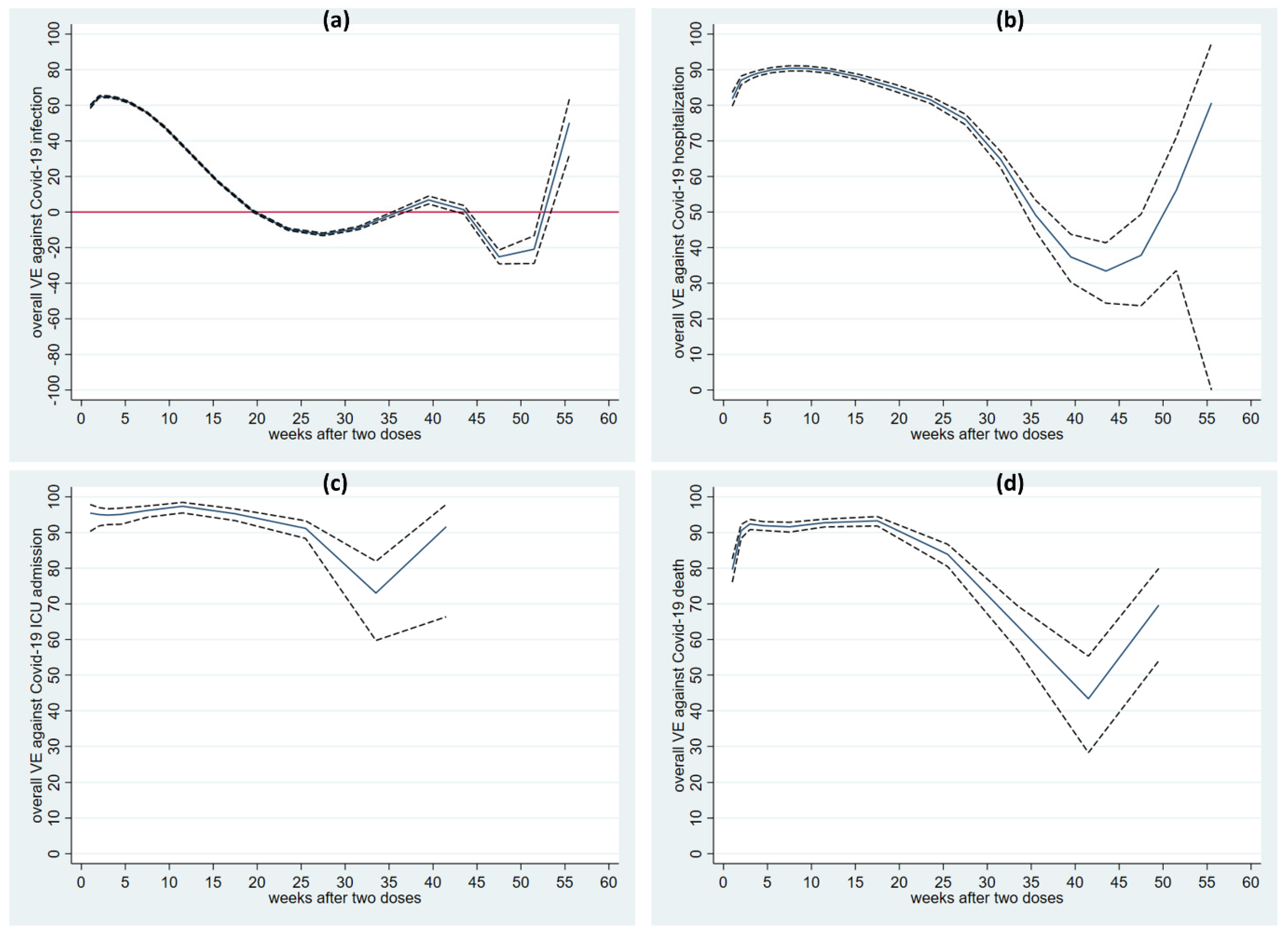
The initial analysis was performed for the entire follow-up (13 months). After two doses of any vaccine, VE against COVID-19 infection peaked at week three at 72.0% (95%CI 71.0–73.0%) but then dropped quickly to 19.5% (18.8–20.2%) by weeks 14–17 and showed no protection from week 18 (Figure 1a, Table S6). VE against hospitalization was above 82% from weeks one to 25 and peaked above 90% at weeks five to six (Figure 1b, Table S6). VE after two doses against severe COVID-19 outcomes (ICU admission and death) was even higher and more durable (Figure 1c,d, Table S7). Figure 2 shows unrestricted spline curves illustrating smoothed trends for all COVID-19 outcomes. The smoothed trends corresponded well with the time interval estimates shown in Figure 1. For the later period (e.g., after week 40), the curves are less stable as the last two knots are at the 95th and 99th percentiles in a time period with fewer data. Therefore, VE estimates from both time interval analysis and spline analysis during the later period should be interpreted with appropriate caution.
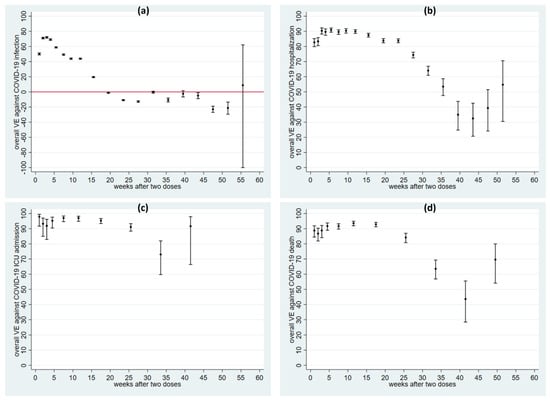
Figure 1.
Adjusted vaccine effectiveness (dots) with 95% CI (capped spikes) against COVID-19 infection (panel (a)), hospitalization (b), severe outcomes [ICU admission (c), and death (d)] at each time interval after two doses. Note that the y-axis scales are different for infection (a) and the other outcomes. Legend: VE denotes vaccine effectiveness. The red line in (a) indicates VE = 0.
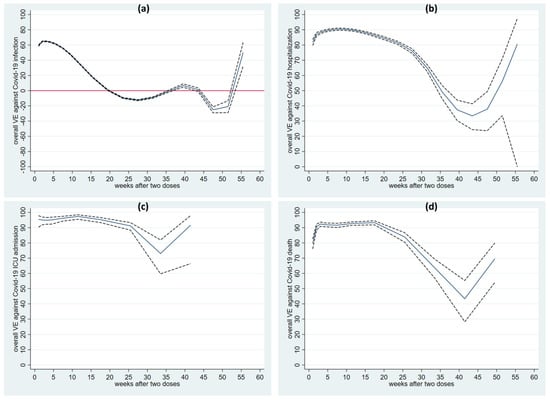
Figure 2.
Unrestricted cubic splines of vaccine effectiveness against COVID-19 infection (panel (a)), hospitalization (b), severe outcomes [ICU admission (c), and death (d)] after two doses. Legend: VE denotes vaccine effectiveness. The area within the dotted line indicates 95% confidence intervals. Note that the y-axis scales are different for infection (a) and the others. The red line in (a) indicates VE = 0.
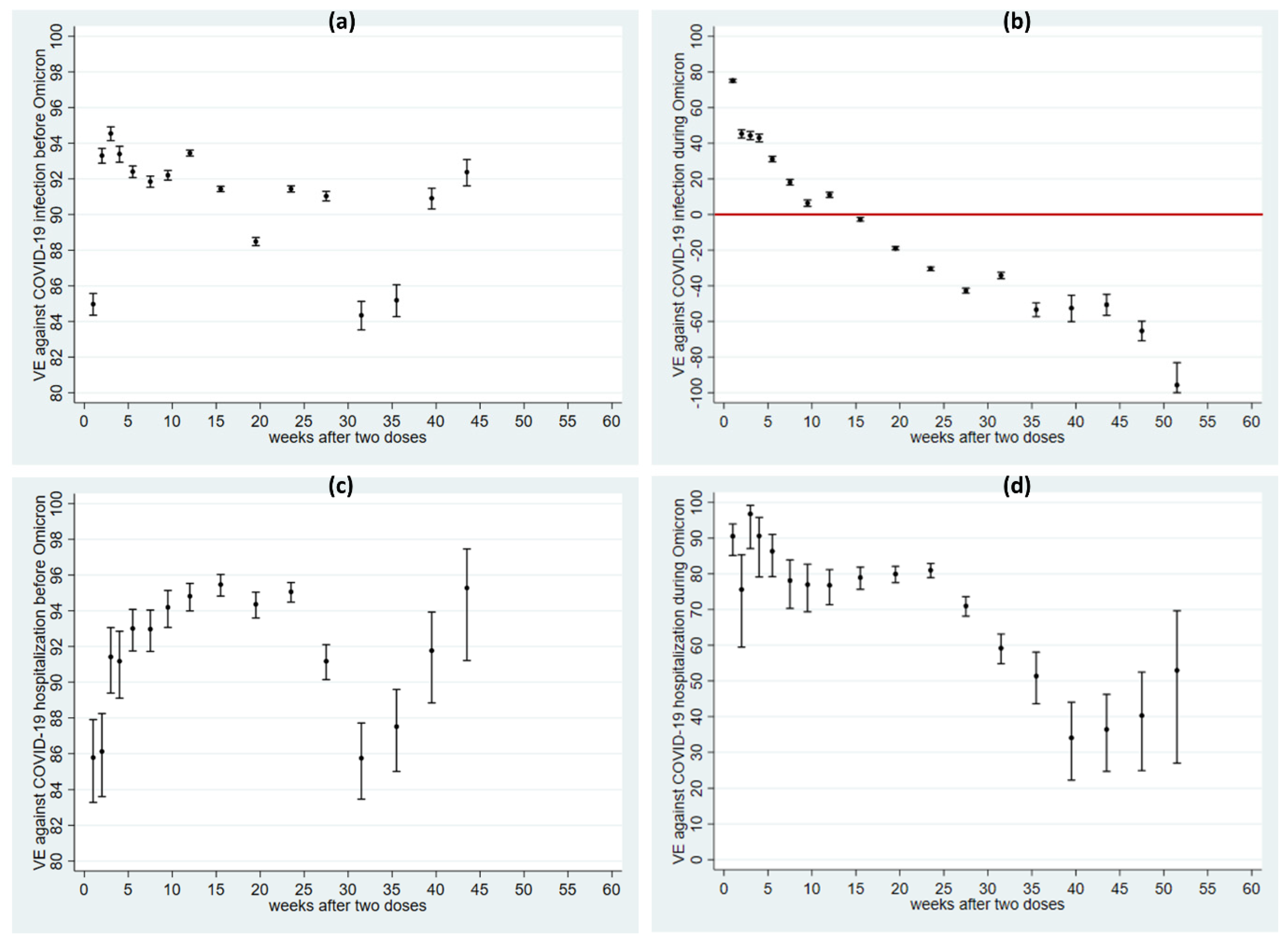
6.3. VE after Two Doses before and after the Emergence of Omicron
The more fast-waning VE observed for the entire follow-up than in other earlier published data appeared to be related to the emergence of Omicron. It is, therefore, important to analyze the pre-Omicron and Omicron periods separately. There was a large difference in VE against infection before and after the emergence of Omicron. VE was above 85% before Omicron in most time intervals (Figure 3a, Table S8), whereas VE was lower and decreased rapidly during the Omicron period and two doses of the vaccine showed no protection against infection by week 14 (Figure 3b, Table S8).
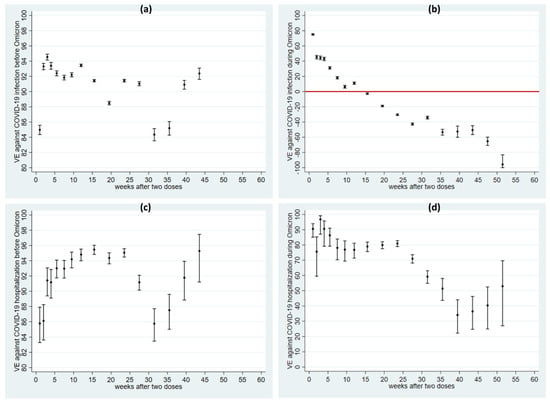
Figure 3.
Adjusted vaccine effectiveness (dots) with 95% CI (capped spikes) of vaccine effectiveness before and after Omicron against COVID-19 infection (a,b) and COVID-19 hospitalization (c,d). Note that the y-axis scales are quite different. Legend: VE denotes vaccine effectiveness. The red line in (b) indicates VE = 0.
A difference in the VE between the pre-Omicron and Omicron period was also observed for hospitalization, but it was not as large as for infection (Figure 3c,d, Table S9). Before Omicron, VE was stable, durable, and high (above 85%), while VE against hospitalization caused by Omicron was about 80% up to week 25 and then decreased but showed some protection against hospitalization during the entire follow-up.
6.4. VE after Two Doses by Age, Sex, and Vaccine Type
The overall VE trends against infection were relatively similar across age groups, although VE against infection was somewhat higher in older age groups (Figure S5). VE against hospitalization showed relatively few differences, with only a slightly higher VE being observed in the 40–60 and 60–65-year age groups (Figure S5). There was a slight sex difference (Figure S6), with lower VE in males. AZD1222 showed lower VE against infection than the mRNA vaccines (Figure S7). In terms of hospitalization, the three vaccines showed similar higher VEs in the early weeks, with AZD1222 showing an earlier decrease (Figure S7).
7. Discussion
This study examined the time-varying VE against infection, hospitalization, and severe COVID-19 outcomes over 13 months, including the emergence of the Omicron variant in Sweden. We modeled exposure over time with high granularity (first weekly, then monthly after vaccination) to provide a more detailed VE investigation than the previous vaccine studies. The most important finding was a difference in the pattern of VE during the pre-Omicron and Omicron periods. We found a high and stable VE (in the range of 85–95%) against infection when restricting the analysis to the pre-Omicron period, which was similar to a US study with over 10 million North Carolina residents and a nine-month follow-up until September 2021. They estimated monthly VE after two doses of the two mRNA vaccines, with a peak VE of about 95% at two months after the first dose, decreasing to 70–80% at seven months [16]. However, in a pre-Omicron Swedish study that included 1,685,948 individuals with 1:1 matching of vaccinated to unvaccinated, they found more progressively waning was observed with an estimated peak (92%) at 15–30 days, declining to no effect after eight months with two doses of vaccine [17]. The difference between our study and that study is likely due to the different target populations, as our study examined the whole population, while that study investigated only 30% of vaccinated individuals who could be matched [17].
We observed, however, very rapidly waning effectiveness during the Omicron period, which dropped to zero protection by week 14. Several studies have also reported lower and more rapid VE waning with Omicron [8,9,10,18,19]. All of these studies used a test-negative case-control study design with potential limitations such as being sensitive to the test sensitivity and specificity [20]. In a UK study [9], with two doses of mRNA vaccines, the VE dropped from 65–70% to 10% by 25 weeks and was even lower and less durable with two doses of AZD1222 (from 45–50% to no effect by 20 weeks). This is broadly consistent with our results.
Our data showed negative VE against Omicron infection from week 14, indicating that vaccinated individuals experienced a higher risk of infection than those unvaccinated. This is likely to be due to unbalanced susceptibility among vaccinated and unvaccinated individuals who had not developed COVID-19 by that time. In time-to-event analyses such as in this study, when an event is inevitable or very common, a protective effect in one group in the short term would be expected to reverse to increased risk at later time points as a reflection of the delay in disease onset in the protected group. The sudden emergence of the highly infective and less severe Omicron variant, with vaccine escape properties [21], represents a sudden change of the COVID-19 infection to a situation where it transitions from a moderately common infection to an almost ubiquitous infection that essentially everyone can expect to contract eventually, as reflected in the drastic VE reversal that we document in our study. Protection against severe disease, however, remains substantial.
Our analysis for the entire follow-up showed an overall lower peak VE than in previous studies, including phase-three trials [22,23,24,25,26,27] and observational studies [16,17]. This was due to the long follow-up period that covered the emergence of Omicron and the difference in VE during the pre-Omicron and Omicron periods. More importantly, greater and longer protection was seen against hospitalization and severe COVID-19 (ICU admission and death) than against COVID-19 infection in this study, as previously reported in other studies [16,17,28]. This study also confirms that VE against hospitalization remained high and durable even during the Omicron period [8,29].
In line with previous trials and real-world observational studies showing lower VE of AZD1222 than mRNA-1273 or BNT162b2 [17,28,30], we observed lower VE after two doses of homologous AZD1222 than the two mRNA vaccines among individuals ≥ 65 years. We restricted the age range in this analysis based on the Swedish vaccine strategy, where AZD1222 was offered to the older population and stopped in mid-2021 (Figure S3). For COVID-19 hospitalization, the three vaccines showed similar VE in the early period, with homologous AZD1222 waning faster from week 20. Overall, we saw similar satisfactory VE across sex and age groups, but we did observe a somewhat unexpected suggested higher VE for infection among older ages. This may be time-related since vaccinations were started with older age groups, and during that period, other social restrictions were stricter than later when vaccination was opened for younger ages. The early variants were also less easily infectious than Omicron. This observation emphasizes that real-life observed VE for being infected is a function of the biological vaccine effect and other aspects of infection spread.
The analysis in this study focused on two doses, as this was originally recommended basic vaccination schedule we wished to study. Despite the introduction of a third booster dose, some individuals and groups have considered themselves adequately covered by two doses, and the coverage of three vaccine doses has been relatively low to date. In addition, dose three had substantially fewer outcomes and a shorter follow-up period, which precludes a detailed time-related analysis such as the one we conducted here for two doses.
The population-based character of our study reduces the potential for selection bias. Additionally, we used Cox regression, considering both time-varying exposure (from unvaccinated to one dose and then two doses) and time-varying effects (period effects for each dose). This approach avoids difficult assumptions about the interval between doses, as in the mentioned US study [16]. However, our results can be influenced by human behaviors related to vaccination. Those who chose to be vaccinated later, or not at all, may behave differently from those who chose to be vaccinated earlier, a potential bias that is difficult to address. Additionally, as the number of home-based tests and antigen tests increases, there is a risk of missing COVID-19 infection cases. However, suboptimal sensitivity of outcome assessment is relevant for all observational studies, and the Swedish register data system nonetheless remains among the best in the world, capturing a broad range of outcomes, including COVID-19, with high accuracy.
8. Conclusions
This study provides more detailed long-term data on time-varying VE against COVID-19 in a complete general population. The progressively waning protection against Omicron infection after two vaccine doses underscores the need for additional efforts to encourage people to get a booster dose to ensure better population-level protection. With respect to hospitalization and severe COVID-19, although waning was stronger during the Omicron period than the pre-Omicron period, two doses of vaccine continued to provide very good and long-lasting protection, emphasizing the need to continue to encourage persons not yet vaccinated to receive their basic two-dose vaccination.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/vaccines10122074/s1, Section S1: Data cleaning of vaccine data obtained from the National Vaccine Register (NVR). Section S2: Data Source of covariates and definition of prior comorbidities and treatments. Section S3: Statistical Analysis. Section S4: Results and Discussion on vaccine effectiveness for first dose [31]. Table S1. Comparison between models without and with adjusting covariates in 10% randomly selected individuals. Analyses were performed for COVID-19 infection, estimating vaccine effectiveness (VE) after two doses. Table S2. Analysis performed in dose 1 and dose 2 separately and analysis including two doses simultaneously with an interaction term between dose and time interval. Analyses were performed for COVID-19 infection in 10% randomly selected individuals. Table S3. Vaccine effectiveness (VE) against COVID-19 infection and hospitalization per time interval after one dose. Table S4. Vaccine effectiveness (VE) against COVID-19 ICU admission and death per time interval after one dose. Table S5. Intervals between vaccine doses among individuals who received at least two doses of vaccination. Table S6. Vaccine effectiveness (VE) against COVID-19 infection and hospitalization per time interval after two doses. Table S7. Vaccine effectiveness (VE) against COVID-19 ICU admission and death per time interval after two doses. Table S8. Vaccine effectiveness (VE) against COVID-19 infection during pre-Omicron and Omicron period, per time interval after two doses. Table S9. Vaccine effectiveness (VE) against COVID-19 hospitalization during pre-Omicron and Omicron period, per time interval after two doses. Figure S1. Trend of COVID-19 infection (a) and hospitalization (b) from 1 January 2020 to 31 January 2022. Figure S2. Cumulative proportion of vaccine uptake over time among the whole Swedish population (a) and 65+ (b). Figure S3. Cumulative count of homologous vaccine type over time. Figure S4. Vaccine effectiveness against COVID-19 infection (a), hospitalization (b), and severe outcomes [ICU admission (c), death (d)] after one dose. Figure S5. Vaccine effectiveness against COVID-19 infection (a,c) and hospitalization (b,d) after two doses in each age group. Figure S6. Overall vaccine effectiveness against COVID-19 infection (a) and hospitalization (b) after two doses in each sex stratum. Figure S7. Overall vaccine effectiveness against COVID-19 infection (a) and hospitalization (b) by different homologous vaccine type among individuals above age 65.
Author Contributions
All authors participated in the literature searches and conceived and designed the study. F.N. acquired the funding. H.L., F.N. and B.K. collected and verified the underlying data. Y.X. performed analysis and drafted the original draft. F.N. supervised the work. All authors interpreted the results and critically reviewed and edited the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This study was made possible by funding from the SciLifeLab National COVID-19 Research Program, financed by the Knut and Alice Wallenberg Foundation (grants KAW 2021-0010/VC2021.0018 and KAW 2020.0299/VC 2022.0008), and the Swedish Research Council (grants 2021-05045 and 2021-05450). The SCIFI-PEARL study also has basic funding based on grants from the Swedish state under the agreement between the Swedish government and the county councils, the ALF agreement (grants ALFGBG-938453, ALFGBG-971130, ALFGBG-978954) and from FORMAS (Research Council for Environment, Agricultural Sciences and Spatial Planning), a Swedish Research Council for Sustainable Development (grant 2020-02828).
Institutional Review Board Statement
This study was approved by the Swedish Ethical Review Authority (Dnr: 2020–01800 and 2021-02106).
Informed Consent Statement
This is a register-based study; no written informed consent from the study participants is needed.
Data Availability Statement
This study used pseudonymized individual-level data from Swedish healthcare registers that are not publicly available according to Swedish legislation. The data can be obtained from the respective Swedish data holders on the basis of ethics approval for the research in question, subject to relevant legislation, processes, and data protection.
Acknowledgments
We are grateful to the following Swedish register agency: Statistics Sweden, Socialstyrelsen, and Public Health Agency of Sweden for providing register data. We also thank everyone who is involved in this study.
Conflicts of Interest
The authors have potential conflict of interest. Gisslén M. reports personal fees (DSMB) from AstraZeneca, Gilead, GSK/ViiV, MSD, Biogen, Novocure, Amgen, and Novo Nordisk, outside the submitted work. Leach S. reports consulting for Scandinavian Biopharma. Vanfleteren LEGW. has received grants and personal fees from AstraZeneca and personal fees from GSK, Novartis, Boehringer-Ingelheim, Menarini, Resmed, Chiesi, AGA Linde, Zambon, and Pulmonx. Nyberg F. reports prior employment at AstraZeneca until 2019 and ownership of some AstraZeneca shares. Kirui B, Wettermark B, Santosa A, Li H, and Xu Y have nothing to disclose.
References
- Li, L.; Guo, P.; Zhang, X.; Yu, Z.; Zhang, W.; Sun, H. SARS-CoV-2 vaccine candidates in rapid development. Hum. Vaccines Immunother. 2021, 17, 644–653. [Google Scholar] [CrossRef] [PubMed]
- Phan, T. Genetic diversity and evolution of SARS-CoV-2. Infect. Genet. Evol. 2020, 81, 104260. [Google Scholar] [CrossRef]
- Ssentongo, P.; Ssentongo, A.E.; Voleti, N.; Groff, D.; Sun, A.; Ba, D.M.; Nunez, J.; Parent, L.J.; Chinchilli, V.M.; Paules, C.I. SARS-CoV-2 vaccine effectiveness against infection, symptomatic and severe COVID-19: A systematic review and meta-analysis. BMC Infect. Dis. 2022, 22, 439. [Google Scholar] [CrossRef] [PubMed]
- Classification of Omicron (B.1.1.529): SARS-CoV-2 Variant of Concern. Available online: https://www.who.int/news/item/26-11-2021-classification-of-omicron-(b.1.1.529)-sars-cov-2-variant-of-concern (accessed on 20 August 2022).
- European Centre for Disease Prevention and Control. Epidemiological Update: Omicron Variant of Concern (VOC)—Data as of 16 December 2021 (12:00). 2021. Available online: https://www.ecdc.europa.eu/en/news-events/epidemiological-update-omicron-data-16-december (accessed on 20 August 2022).
- Cele, S.; Jackson, L.; Khoury, D.S.; Khan, K.; Moyo-Gwete, T.; Tegally, H.; San, J.E.; Cromer, D.; Scheepers, C.; Amoako, D.; et al. SARS-CoV-2 Omicron has extensive but incomplete escape of Pfizer BNT162b2 elicited neutralization and requires ACE2 for infection. arXiv 2021. [Google Scholar] [CrossRef]
- Dejnirattisai, W.; Huo, J.; Zhou, D.; Zahradník, J.; Supasa, P.; Liu, C.; Duyvesteyn, H.M.E.; Ginn, H.M.; Mentzer, A.J.; Tuekprakhon, A.; et al. SARS-CoV-2 Omicron-B.1.1.529 leads to widespread escape from neutralizing antibody responses. Cell 2022, 185, 467–484.e15. [Google Scholar] [CrossRef] [PubMed]
- Altarawneh, H.N.; Chemaitelly, H.; Ayoub, H.H.; Tang, P.; Hasan, M.R.; Yassine, H.M.; Al-Khatib, H.A.; Smatti, M.K.; Coyle, P.; Al-Kanaani, Z.; et al. Effects of Previous Infection and Vaccination on Symptomatic Omicron Infections. N. Engl. J. Med. 2022, 387, 21–34. [Google Scholar] [CrossRef]
- Andrews, N.; Stowe, J.; Kirsebom, F.; Toffa, S.; Rickeard, T.; Gallagher, E.; Gower, C.; Kall, M.; Groves, N.; O’Connell, A.-M.; et al. COVID-19 Vaccine Effectiveness against the Omicron (B.1.1.529) variant. N. Engl. J. Med. 2022, 386, 1532–1546. [Google Scholar] [CrossRef]
- Suah, J.L.; Tng, B.H.; Tok, P.S.K.; Husin, M.; Thevananthan, T.; Peariasamy, K.M.; Sivasampu, S. Real-world effectiveness of homologous and heterologous BNT162b2, CoronaVac, and AZD1222 booster vaccination against Delta and Omicron SARS-CoV-2 infection. Emerg. Microbes Infect. 2022, 11, 1343–1345. [Google Scholar] [CrossRef]
- Ljung, R.; Sundström, A.; Grünewald, M.; Backman, C.; Feltelius, N.; Gedeborg, R.; Zethelius, B. The profile of the COVID-19 VACcination register SAFEty study in Sweden (CoVacSafe-SE). Ups. J. Med. Sci. 2021, 126. [Google Scholar] [CrossRef]
- Nyberg, F.; Franzén, S.; Lindh, M.; Vanfleteren, L.; Hammar, N.; Wettermark, B.; Sundström, J.; Santosa, A.; Björck, S.; Gisslén, M. Swedish COVID-19 Investigation for Future Insights—A Population Epidemiology Approach Using Register Linkage (SCIFI-PEARL). Clin. Epidemiol. 2021, 13, 649–659. [Google Scholar] [CrossRef]
- Vecka 52, 2021—Statistik om förekomst av misstänkta fall av SARS-CoV-2 virusvarianten omicron—Folkhälsomyndigheten. Available online: https://www.folkhalsomyndigheten.se/smittskydd-beredskap/utbrott/aktuella-utbrott/covid-19/statistik-och-analyser/sars-cov-2-virusvarianter-av-sarskild-betydelse/statistik-om-forekomst-av-misstankta-fall-av-sars-cov-2-virusvarianten-omikron/vecka-52-2021/ (accessed on 23 August 2022).
- Zaki, N.; Mohamed, E.A. The estimations of the COVID-19 incubation period: A scoping reviews of the literature. J. Infect. Public Health 2021, 14, 638–646. [Google Scholar] [CrossRef] [PubMed]
- Kleinbaum, D.G.; Klein, M. Survival Analysis: A Self-Learning Text; Springer: New York, NY, USA, 2012; Volume 3. [Google Scholar]
- Lin, D.-Y.; Gu, Y.; Wheeler, B.; Young, H.; Holloway, S.; Sunny, S.-K.; Moore, Z.; Zeng, D. Effectiveness of COVID-19 Vaccines over a 9-Month Period in North Carolina. N. Engl. J. Med. 2022, 386, 933–941. [Google Scholar] [CrossRef] [PubMed]
- Nordström, P.; Ballin, M.; Nordström, A. Risk of infection, hospitalisation, and death up to 9 months after a second dose of COVID-19 vaccine: A retrospective, total population cohort study in Sweden. Lancet 2022, 399, 814–823. [Google Scholar] [CrossRef] [PubMed]
- Horne, E.M.F.; Hulme, W.J.; Keogh, R.H.; Palmer, T.M.; Williamson, E.J.; Parker, E.P.K.; Green, A.; Walker, V.; Walker, A.J.; Curtis, H.; et al. Waning effectiveness of BNT162b2 and ChAdOx1 COVID-19 vaccines over six months since second dose: OpenSAFELY cohort study using linked electronic health records. BMJ 2022, 378, e071249. [Google Scholar] [CrossRef] [PubMed]
- Kirsebom, F.C.M.; Andrews, N.; Stowe, J.; Toffa, S.; Sachdeva, R.; Gallagher, E.; Groves, N.; O’Connell, A.-M.; Chand, M.; Ramsay, M.; et al. COVID-19 vaccine effectiveness against the omicron (BA.2) variant in England. Lancet Infect. Dis. 2022, 22, 931–933. [Google Scholar] [CrossRef]
- Chua, H.; Feng, S.; Lewnard, J.A.; Sullivan, S.G.; Blyth, C.C.; Lipsitch, M.; Cowling, B.J. The use of test-negative controls to monitor vaccine effectiveness: A systematic review of methodology. Epidemiology 2020, 31, 43–64. [Google Scholar] [CrossRef]
- Garcia-Beltran, W.F.; St Denis, K.J.; Hoelzemer, A.; Lam, E.C.; Nitido, A.D.; Sheehan, M.L.; Berrios, C.; Ofoman, O.; Chang, C.C.; Hauser, B.M.; et al. mRNA-based COVID-19 vaccine boosters induce neutralizing immunity against SARS-CoV-2 Omicron variant. Cell 2022, 185, 457–466.e4. [Google Scholar] [CrossRef]
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Marc, G.P.; Moreira, E.D.; Zerbini, C.; et al. Safety and Efficacy of the BNT162b2 mRNA COVID-19 Vaccine. N. Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef]
- Thomas, S.J.; Moreira, E.D., Jr.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Pérez Marc, G.; Polack, F.P.; Zerbini, C.; et al. Safety and Efficacy of the BNT162b2 mRNA COVID-19 Vaccine through 6 Months. N. Engl. J. Med. 2021, 385, 1761–1773. [Google Scholar] [CrossRef]
- Baden, L.R.; El Sahly, H.M.; Essink, B.; Kotloff, K.; Frey, S.; Novak, R.; Diemert, D.; Spector, S.A.; Rouphael, N.; Creech, B.; et al. Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine. N. Engl. J. Med. 2021, 384, 403–416. [Google Scholar] [CrossRef]
- El Sahly, H.M.; Baden, L.R.; Essink, B.; Doblecki-Lewis, S.; Martin, J.M.; Anderson, E.J.; Campbell, T.B.; Clark, J.; Jackson, L.A.; Fichtenbaum, C.J.; et al. Efficacy of the mRNA-1273 SARS-CoV-2 Vaccine at Completion of Blinded Phase. N. Engl. J. Med. 2021, 385, 1774–1785. [Google Scholar] [CrossRef] [PubMed]
- Falsey, A.R.; Sobieszczyk, M.E.; Hirsch, I.; Sproule, S.; Robb, M.L.; Corey, L.; Neuzil, K.M.; Hahn, W.; Hunt, J.; Mulligan, M.J.; et al. Phase 3 Safety and Efficacy of AZD1222 (ChAdOx1 nCoV-19) COVID-19 Vaccine. N. Engl. J. Med. 2021, 385, 2348–2360. [Google Scholar] [CrossRef] [PubMed]
- Voysey, M.; Clemens, S.A.C.; Madhi, S.A.; Weckx, L.Y.; Folegatti, P.M.; Aley, P.K.; Angus, B.; Baillie, V.L.; Barnabas, S.L.; Bhorat, Q.E.; et al. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: An interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet 2021, 397, 99–111. [Google Scholar] [CrossRef]
- Katikireddi, S.V.; Cerqueira-Silva, T.; Vasileiou, E.; Robertson, C.; Amele, S.; Pan, J.; Taylor, B.; Boaventura, V.; Werneck, G.L.; Flores-Ortiz, R.; et al. Two-dose ChAdOx1 nCoV-19 vaccine protection against COVID-19 hospital admissions and deaths over time: A retrospective, population-based cohort study in Scotland and Brazil. Lancet 2022, 399, 25–35. [Google Scholar] [CrossRef] [PubMed]
- Björk, J.; Bonander, C.; Moghaddassi, M.; Rasmussen, M.; Malmqvist, U.; Inghammar, M.; Kahn, F. COVID-19 vaccine effectiveness against severe disease from SARS-CoV-2 Omicron BA.1 and BA.2 subvariants—Surveillance results from southern Sweden, December 2021 to March 2022. Eurosurveillance 2022, 27, 2200322. [Google Scholar] [CrossRef] [PubMed]
- Andrews, N.; Tessier, E.; Stowe, J.; Gower, C.; Kirsebom, F.; Simmons, R.; Gallagher, E.; Thelwall, S.; Groves, N.; Dabrera, G.; et al. Duration of Protection against Mild and Severe Disease by COVID-19 Vaccines. N. Engl. J. Med. 2022, 386, 340–350. [Google Scholar] [CrossRef] [PubMed]
- Ostropolets, A.; Hripcsak, G. COVID-19 vaccination effectiveness rates by week and sources of bias: A retrospective cohort study. BMJ open 2022, 12, e061126. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).