Strengthening the Link between Vaccine Predispositions and Vaccine Advocacy through Certainty
Abstract
1. Introduction
2. Study 1
2.1. Materials and Methods
2.2. Predictor Variables
2.3. Dependent Variable
2.4. Data Analysis
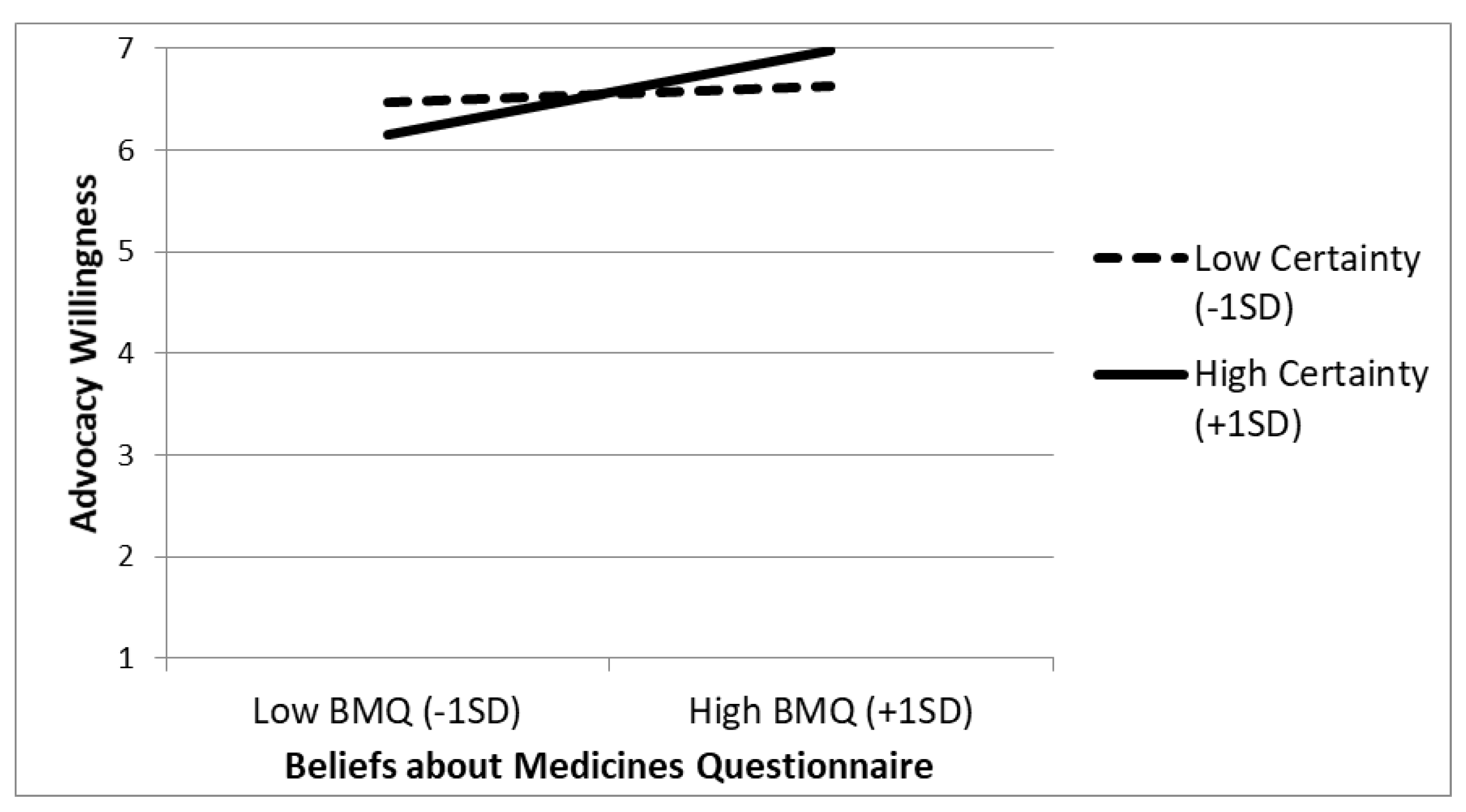
2.5. Results
2.6. Discussion
3. Study 2
3.1. Materials and Methods
3.2. Predictor Variables
3.3. Dependent Variable
3.4. Data Analysis
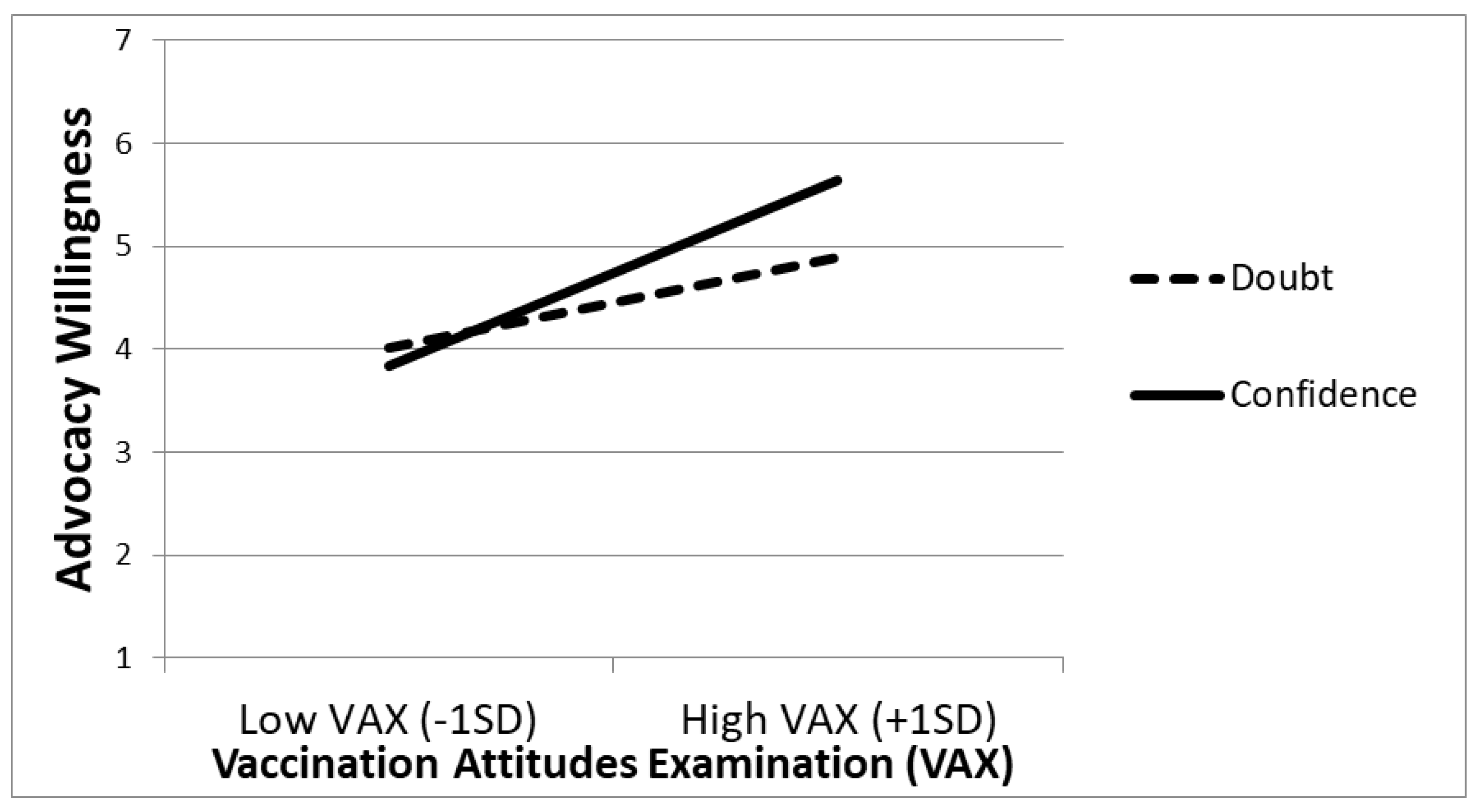
3.5. Results
3.6. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Orenstein, W.A.; Ahmed, R. Simply put: Vaccination saves lives. Proc. Natl. Acad. Sci. USA 2017, 114, 4031–4033. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Immunization. Available online: https://www.who.int/news-room/facts-in-pictures/detail/immunization (accessed on 14 July 2022).
- Meslé, M.M.; Brown, J.; Mook, P.; Hagan, J.; Pastore, R.; Bundle, N.; Spiteri, G.; Ravasi, G.; Nicolay, N.; Andrews, N.; et al. Estimated number of deaths directly averted in people 60 years and older as a result of COVID-19 vaccination in the WHO European Region, December 2020 to November 2021. Eurosurveillance 2021, 26, 2101021. [Google Scholar] [CrossRef] [PubMed]
- Carrasco, R.; Cárdaba, M.A.; Villar, E. Citizen participation in Twitter: Anti-vaccine controversies in times of COVID-19. Comunicar 2021, 69, 21–31. [Google Scholar] [CrossRef]
- Fusick, A.J.; Gunther, S.; Sullivan, G. The anti-vaccination movement: When does a belief become delusional? J. Public Health 2021, 29, 1301–1302. [Google Scholar] [CrossRef]
- Pertwee, E.; Simas, C.; Larson, H.J. An epidemic of uncertainty: Rumors, conspiracy theories and vaccine hesitancy. Nat. Med. 2022, 28, 456–459. [Google Scholar] [CrossRef] [PubMed]
- Ashby, B.; Best, A. Herd immunity. Curr. Biol. 2021, 31, R174–R177. [Google Scholar] [CrossRef]
- Bechler, C.J.; Tormala, Z.L.; Rucker, D.D. Choosing persuasion targets: How expectations of qualitative change increase advocacy intentions. J. Exp. Soc. Psychol. 2020, 86, 103911. [Google Scholar] [CrossRef]
- Cheatham, L.; Tormala, Z.L. Attitude certainty and attitudinal advocacy: The unique roles of clarity and correctness. Pers. Soc. Psychol. Bull. 2015, 41, 1537–1550. [Google Scholar] [CrossRef]
- Teeny, J.D.; Petty, R.E. Attributions of emotion and reduced attitude openness prevent people from engaging others with opposing views. J. Exp. Soc. Psychol. 2022, 102, 104373. [Google Scholar] [CrossRef]
- Berger, J. Word of mouth and interpersonal communication: A review and directions for future research. J. Consum. Psychol. 2014, 24, 586–607. [Google Scholar] [CrossRef]
- Shi, J.; Hu, P.; Lai, K.K.; Chen, G. Determinants of users’ information dissemination behavior on social networking sites: An elaboration likelihood model perspective. Internet Res. 2018, 28, 393–418. [Google Scholar] [CrossRef]
- Phelps, J.E.; Lewis, R.; Mobilio, L.; Perry, D.; Raman, N. Viral marketing or electronic word-of-mouth advertising: Examining consumer responses and motivations to pass along email. J. Advert. Res. 2004, 44, 333–348. [Google Scholar] [CrossRef]
- Hildreth, J.E.; Alcendor, D.J. Targeting COVID-19 vaccine hesitancy in minority populations in the US: Implications for herd immunity. Vaccines 2021, 9, 489. [Google Scholar] [CrossRef]
- Albrecht, D. Vaccination, politics and COVID-19 impacts. BMC Public Health 2022, 22, 96. [Google Scholar] [CrossRef]
- World Health Organization. Ten Threats to Global Health in 2019. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 25 July 2022).
- Jarrett, C.; Wilson, R.; O’Leary, M.; Eckersberger, E.; Larson, H.J. Strategies for addressing vaccine hesitancy–A systematic review. Vaccine 2015, 33, 4180–4190. [Google Scholar] [CrossRef]
- McGee, L.U.; Suh, J. Communication Strategies to Address Vaccine Hesitancy in Healthcare Settings and on Social Media. J. Appl. Res. Child. 2019, 10, 7. [Google Scholar]
- Spiliotopoulos, N.; Spiliotopoulou, M. The anti-vaccination movement: A serious threat to public health. HAPSc Policy Briefs Ser. 2021, 2, 208–213. [Google Scholar] [CrossRef]
- Horne, R.; Weinman, J.; Hankins, M. The beliefs about medicines questionnaire: The development and evaluation of a new method for assessing the cognitive representation of medication. Psychol. Health 1999, 14, 1–24. [Google Scholar] [CrossRef]
- Martin, L.R.; Petrie, K.J. Understanding the dimensions of anti-vaccination attitudes: The vaccination attitudes examination (VAX) Scale. Ann. Behav. Med. 2017, 51, 652–660. [Google Scholar] [CrossRef]
- Shapiro, G.K.; Tatar, O.; Dube, E.; Amsel, R.; Knauper, B.; Naz, A.; Perez, S.; Rosberger, Z. The vaccine hesitancy scale: Psychometric properties and validation. Vaccine 2018, 36, 660–667. [Google Scholar] [CrossRef]
- Zingg, A.; Siegrist, M. Measuring people’s knowledge about vaccination: Developing a one-dimensional scale. Vaccine 2012, 30, 3771–3777. [Google Scholar] [CrossRef] [PubMed]
- Briñol, P.; Petty, R.E. Self-validation theory: An integrative framework for understanding when thoughts become consequential. Psychol. Rev. 2022, 129, 340–367. [Google Scholar] [CrossRef] [PubMed]
- Petty, R.E.; Krosnick, J.A. Attitude Strength: Antecedents and Consequences; Erlbaum: Hillsdale, NY, USA, 1995. [Google Scholar]
- Rucker, D.D.; Tormala, Z.L.; Petty, R.E.; Briñol, P. Consumer conviction and commitment: An appraisal-based framework for attitude certainty. J. Consum. Psychol. 2014, 24, 119–136. [Google Scholar] [CrossRef]
- Tormala, Z.L.; Rucker, D.D. Attitude certainty: Antecedents, consequences, and new directions. Consum. Psychol. Rev. 2018, 1, 72–89. [Google Scholar] [CrossRef]
- Petty, R.E.; Briñol, P.; Tormala, Z.L.; Wegener, D.T. The Role of Meta-Cognition in Social Judgment. In Social Psychology: Handbook of Basic Principles, 2nd ed.; Higgins, E.T., Kruglanski, A.W., Eds.; Guilford Press: New York, NY, USA, 2007; pp. 254–284. [Google Scholar]
- Shoots-Reinhard, B.; Petty, R.E.; DeMarree, K.G.; Rucker, D.D. Personality certainty and politics: Increasing the predictive utility of individual difference inventories. Polit. Psychol. 2015, 36, 415–430. [Google Scholar] [CrossRef]
- Jarvis, W.B.G.; Petty, R.E. The need to evaluate. J. Pers. Soc. Psychol. 1996, 70, 172–194. [Google Scholar] [CrossRef]
- Vitriol, J.A.; Tagar, M.R.; Federico, C.M.; Sawicki, V. Ideological uncertainty and investment of the self in politics. J. Exp. Soc. Psychol. 2019, 82, 85–97. [Google Scholar] [CrossRef]
- Paredes, B.; Santos, D.; Briñol, P.; Gómez, Á.; Petty, R.E. The role of meta-cognitive certainty on the relationship between identity fusion and endorsement of extreme pro-group behavior. Self Identity 2020, 19, 804–824. [Google Scholar] [CrossRef]
- Paredes, B.; Martínez, L.; Cuesta, U.; Briñol, P.A.; Petty, R.E.; Moreno, L.M. The role of meta-cognitive certainty on pornography consumption. Psicothema 2021, 33, 442–448. [Google Scholar] [CrossRef]
- Santos, D.; Briñol, P.; Petty, R.E.; Gandarillas, B.; Mateos, R. Trait aggressiveness predicting aggressive behavior: The moderating role of meta-cognitive certainty. Aggress. Behav. 2019, 45, 255–264. [Google Scholar] [CrossRef]
- Koriat, A.; Undorf, M.; Newman, E.; Schwarz, N. Subjective confidence in the response to personality questions: Some insight into the construction of people’s responses to test items. Front. Psychol. 2020, 11, 1250. [Google Scholar] [CrossRef]
- Moreno, L.; Briñol, P.; Petty, R.E. Metacognitive confidence can increase but also decrease performance in academic settings. Metacogn. Learn. 2022, 17, 139–165. [Google Scholar] [CrossRef]
- Wichman, A.L.; Briñol, P.; Petty, R.E.; Rucker, D.D.; Tormala, Z.L.; Weary, G. Doubting one’s doubt: A formula for confidence. J. Exp. Soc. Psychol. 2010, 46, 350–355. [Google Scholar] [CrossRef]
- Horcajo, J.; Santos, D.; Higuero, G. The effects of self-efficacy on physical and cognitive performance: An analysis of meta-certainty. Psychol. Sport Exerc. 2022, 58, 102063. [Google Scholar] [CrossRef]
- Resnick, S.G.; Rosenheck, R.A. Integrating peer-provided services: A quasi-experimental study of recovery orientation, confidence, and empowerment. Psychiatr. Serv. 2008, 59, 1307–1314. [Google Scholar] [CrossRef]
- Martin, A.E.; North, M.S. Equality for (almost) all: Egalitarian advocacy predicts lower endorsement of sexism and racism, but not ageism. J. Pers. Soc. Psychol. 2021, 123, 373–399. [Google Scholar] [CrossRef]
- Chadwick, A.; Kaiser, J.; Vaccari, C.; Freeman, D.; Lambe, S.; Loe, B.S.; Vanderslott, S.; Lewandowsky, S.; Conroy, M.; Ross, A.R.N.; et al. Online social endorsement and COVID-19 vaccine hesitancy in the United Kingdom. Soc. Media. Soc. 2021, 7, 1–17. [Google Scholar] [CrossRef]
- Sturgis, P.; Brunton-Smith, I.; Jackson, J. Trust in science, social consensus and vaccine confidence. Nat. Hum. Behav. 2021, 5, 1528–1534. [Google Scholar] [CrossRef]
- Briñol, P.; McCaslin, M.J.; Petty, R.E. Self-generated persuasion: Effects of the target and direction of arguments. J. Pers. Soc. Psychol. 2012, 102, 925–940. [Google Scholar] [CrossRef]
- Hartley, K.; Vu, M.K. Fighting fake news in the COVID-19 era: Policy insights from an equilibrium model. Policy Sci. 2020, 53, 735–758. [Google Scholar] [CrossRef]
- Paredes, B.; Cárdaba, M.A.; Cuesta, U.; Martinez, L. Validity of the Spanish Version of the Vaccination Attitudes Examination Scale. Vaccines 2021, 9, 1237. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Evers, A.; Muñiz Fernández, J.; Hagemeister, C.; Hstmaelingen, A.; Lindley, P.; Sjöberg, A.; Bartram, D. Assessing the quality of tests: Revision of the EFPA review model. Psicothema 2013, 25, 283–291. [Google Scholar] [CrossRef] [PubMed]
- Balluerka, N.; Gorostiaga, A.; Alonso-Arbiol, I.; Haranburu, M. Test adaptation to other cultures: A practical approach. Psicothema 2007, 19, 124–133. [Google Scholar] [PubMed]
- Ferguson, E.; Cox, T. Exploratory Factor Analysis: A Users’ Guide. Int. J. Sel. Assess. 1993, 1, 84–94. [Google Scholar] [CrossRef]
- Mosleh, M.; Pennycook, G.; Rand, D.G. Self-reported willingness to share political news articles in online surveys correlates with actual sharing on Twitter. PLoS ONE 2020, 15, e0228882. [Google Scholar] [CrossRef]
- Bin Naeem, S.; Kamel Boulos, M.N. COVID-19 misinformation online and health literacy: A brief overview. Int. J. Env. Res. Public Health 2021, 18, 8091. [Google Scholar] [CrossRef]
- Loman, J.; Müller, B.C.; Beverborg, A.O.; van Baaren, R.B.; Buijzen, M. Self-persuasion in media messages: Reducing alcohol consumption among students with open-ended questions. J. Exp. Psychol. Appl. 2018, 24, 81–91. [Google Scholar] [CrossRef]
- Gal, D.; Rucker, D.D. When in doubt, shout! Paradoxical influences of doubt on proselytizing. Psychol. Sci. 2010, 21, 1701–1707. [Google Scholar] [CrossRef]
- Ashokkumar, A.; Talaifar, S.; Fraser, W.T.; Landabur, R.; Buhrmester, M.; Gómez, Á.; Paredes, B.; Swann, W.B. Censoring political opposition online: Who does it and why. J. Exp. Soc. Psychol. 2020, 91, 104031. [Google Scholar] [CrossRef]
- Taylor, L. COVID-19 misinformation sparks threats and violence against doctors in Latin America. BMJ 2020, 370, m3088. [Google Scholar] [CrossRef]
- Sa’ait, N.; Kanyan, A.; Nazrin, M.F. The effect of e-WOM on customer purchase intention. IAR J. Soc. Sci. 2016, 2, 73–80. [Google Scholar]
- Bataineh, A.Q. The impact of perceived e-WOM on purchase intention: The mediating role of corporate image. Int. J. Mark. Stud. 2015, 7, 126. [Google Scholar] [CrossRef]
- Vallée-Tourangeau, G.; Promberger, M.; Moon, K.; Wheelock, A.; Sirota, M.; Norton, C.; Sevdalis, N. Motors of influenza vaccination uptake and vaccination advocacy in healthcare workers: Development and validation of two short scales. Vaccine 2018, 36, 6540–6545. [Google Scholar] [CrossRef]
- Cohen, J.; Cohen, P. Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences; Erlbaum: Hillsdale, NY, USA, 1983. [Google Scholar]
- Paul, E.; Steptoe, A.; Fancourt, D. Attitudes towards vaccines and intention to vaccinate against COVID-19: Implications for public health communications. Lancet Reg. Health Eur. 2021, 1, 100012. [Google Scholar] [CrossRef]
- Bruno, F.; Laganà, V.; Pistininzi, R.; Tarantino, F.; Martin, L.; Servidio, R. Validation and psychometric properties of the Italian Vaccination Attitudes Examination (VAX-I) scale. Curr. Psychol. 2022, 1–11. [Google Scholar] [CrossRef]
- Huza, G. The Psychometric Properties of a Romanian Version of the Vaccination Attitudes Examination (VAX) Scale. Int. J. HIV/AIDS Preven. Edu. Behav. Sci. 2020, 6, 25. [Google Scholar] [CrossRef]
- Tomietto, M.; Comparcini, D.; Simonetti, V.; Papappicco, C.A.M.; Stefanizzi, P.; Mercuri, M.; Cicolini, G. Attitudes toward COVID-19 vaccination in the nursing profession: Validation of the Italian version of the VAX scale and descriptive study. Ann. Ig. Med. Prev. Comunita 2022, 34, 572–584. [Google Scholar] [CrossRef]
- Yildiz, E.; Gungormus, Z.; Dayapoglu, N. Assessment of validity and reliability of the turkish version of the vaccination attitudes examination (VAX) scale. Int. J. Caring Sci. 2021, 14, 261–268. [Google Scholar]
- Petty, R.E.; Briñol, P.; Tormala, Z.L. Thought confidence as a determinant of persuasion: The self-validation hypothesis. J. Per. Soc. Psychol. 2002, 82, 722–741. [Google Scholar] [CrossRef]
- Jin, S.-A.A.; Phua, J. Following celebrities’ tweets about brands: The impact of twitter-based electronic Word-of-Mouth on consumers’ source credibility perception, buying intention, and social identification with celebrities. J. Advert. 2014, 43, 181–195. [Google Scholar] [CrossRef]
- Mishra, A.; Maheswarappa, S.S.; Maity, M.; Samu, S. Adolescent’s eWOM intentions: An investigation into the roles of peers, the Internet and gender. J. Bus. Res. 2017, 86, 394–405. [Google Scholar] [CrossRef]
- DeMarree, K.G.; Petty, R.E.; Briñol, P.; Xia, J. Documenting individual differences in the propensity to hold attitudes with certainty. J. Pers. Soc. Psychol. 2020, 119, 1239–1265. [Google Scholar] [CrossRef] [PubMed]
- Falces, C.; Briñol, P.; Sierra, B.; Becerra, A.; Alier, E. Validación de la escala de Necesidad de Cognición y aplicación al estudio del cambio de actitudes. Psicothema 2001, 13, 647–653. [Google Scholar]
- Briñol, P.; Petty, R.E. A history of attitudes and persuasion research. In Handbook of the History of Social Psychology; Psychology Press: New York, NY, USA, 2012; pp. 283–320. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Paredes, B.; Cárdaba, M.A.M.; Moreno, L.; Cano, N.; Briñol, P.; Cuesta, U.; Petty, R.E. Strengthening the Link between Vaccine Predispositions and Vaccine Advocacy through Certainty. Vaccines 2022, 10, 1970. https://doi.org/10.3390/vaccines10111970
Paredes B, Cárdaba MAM, Moreno L, Cano N, Briñol P, Cuesta U, Petty RE. Strengthening the Link between Vaccine Predispositions and Vaccine Advocacy through Certainty. Vaccines. 2022; 10(11):1970. https://doi.org/10.3390/vaccines10111970
Chicago/Turabian StyleParedes, Borja, Miguel A. Martín Cárdaba, Lorena Moreno, Nerea Cano, Pablo Briñol, Ubaldo Cuesta, and Richard E. Petty. 2022. "Strengthening the Link between Vaccine Predispositions and Vaccine Advocacy through Certainty" Vaccines 10, no. 11: 1970. https://doi.org/10.3390/vaccines10111970
APA StyleParedes, B., Cárdaba, M. A. M., Moreno, L., Cano, N., Briñol, P., Cuesta, U., & Petty, R. E. (2022). Strengthening the Link between Vaccine Predispositions and Vaccine Advocacy through Certainty. Vaccines, 10(11), 1970. https://doi.org/10.3390/vaccines10111970





