Brazilian Adults’ Attitudes and Practices Regarding the Mandatory COVID-19 Vaccination and Their Hesitancy towards Childhood Vaccination
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Settings
2.2. Sample Size Determination
2.3. Ethical Issues
2.4. Variables
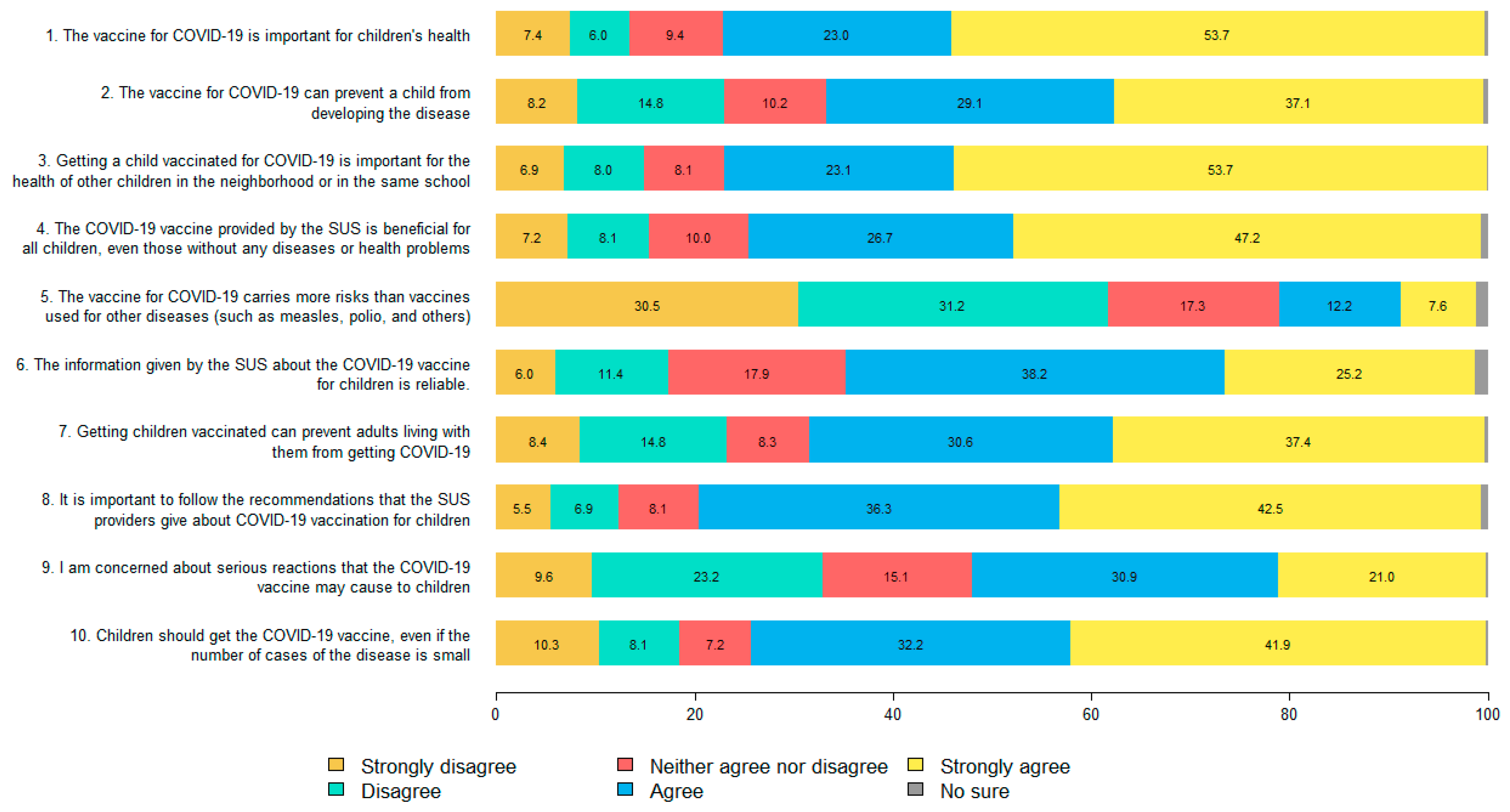
- The vaccine for COVID-19 is important for children’s health.
- The vaccine for COVID-19 can prevent a child from developing the disease.
- Getting a child vaccinated for COVID-19 is important for the health of other children in the neighborhood or in the same school.
- The COVID-19 vaccine provided by the SUS is beneficial for all children, even those without any disease or health problems.
- The vaccine for COVID-19 carries more risks than vaccines used for other diseases (such as measles, polio and others).
- The information given by the SUS about the COVID-19 vaccine for children is reliable.
- Getting children vaccinated can prevent adults living with them from getting COVID-19.
- It is important to follow the recommendations that the SUS providers give about COVID-19 vaccination for children.
- I am concerned about serious adverse reactions the COVID-19 vaccine may cause to children.
- Children should get the COVID-19 vaccine, even if the number of cases of the disease is small.
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dubé, E.; Laberge, C.; Guay, M.; Bramadat, P.; Roy, R.; Bettinger, J.A. Vaccine hesitancy: An overview. Hum. Vaccines Immunother. 2013, 9, 1763–1773. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Châtelet, I.P.; Antona, D.; Freymuth, F.; Muscat, M.; Halftermeyer-Zhou, F.; Maine, C.; Floret, D.; Lévy-Bruhl, D. Spotlight on measles 2010: Update on the ongoing measles outbreak in France, 2008–2010. Eurosurveillance 2010, 15, 19656. [Google Scholar]
- Serres, G.; Markowski, F.; Toth, E.; Landry, M.; Auger, D.; Mercier, M.; Bélanger, P.; Turmel, B.; Arruda, H.; Boulianne, N.; et al. Largest measles epidemic in North America in a decade-Quebec, Canada, 2011: Contribution of susceptibility, serendipity, and superspreading events. J. Infect. Dis. 2013, 207, 990–998. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oostvogel, P.M.; van Wijngaarden, J.K.; Van der Avoort, H.G.; Mulders, M.N.; Conyn-van Spaendonck, M.A.; Rümke, H.C.; van Steenis, G.; van Loon, A.M. Poliomyelitis outbreak in an unvaccinated community in The Netherlands, 1992–1993. Lancet 1994, 344, 665–670. [Google Scholar] [CrossRef]
- Falagas, M.E.; Zarkadoulia, E. Factors associated with suboptimal compliance to vaccinations in children in developed countries: A systematic review. Curr. Med. Res. Opin. 2008, 24, 1719–1741. [Google Scholar] [CrossRef]
- Sato, A.P.S. What is the importance of vaccine hesitancy in the drop of vaccination coverage in Brazil? Rev. Saude Publica 2018, 52, 96. [Google Scholar] [CrossRef] [Green Version]
- MacDonald, N.E.; SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- Dubé, E.; Gagnon, D.; Ouakki, M.; Bettinger, J.A.; Guay, M.; Halperin, S.; Wilson, K.; Graham, J.; Witteman, H.O.; MacDonald, S.; et al. Understanding vaccine hesitancy in Canada: Results of a consultation study by the Canadian Immunization Research Network. PLoS ONE 2016, 11, e0156118. [Google Scholar]
- Croda, J.; Oliveira, W.K.; Frutuoso, R.L.; Mandetta, L.H.; Baia-da-Silva, D.C.; Brito-Sousa, J.D.; Monteiro, W.M.; Lacerda, M.V.G. COVID-19 in Brazil: Advantages of a socialized unified health system and preparation to contain cases. Rev. Soc. Bras. Med. Trop. 2020, 53, e20200167. [Google Scholar] [CrossRef]
- Castro, R. Vacinas contra a COVID-19: O fim da pandemia? Physis 2021, 31, e310100. [Google Scholar] [CrossRef]
- Moura-Gabriel, I.W.; Oliveira, C.G.L.; Reis, A.O.A.; Pereira, Y.T.G.; Júnior, J.G.; Matos-Brasil, A.A.G.; Amorim, L.M.; Lima, N.N.R.; Neto, M.L.R. Deaths announced in Brazil-A dark sweetness: COVID-19 among children and adolescents. J. Pediatr. Nurs. 2022, 65, e22–e23. [Google Scholar] [CrossRef] [PubMed]
- Brazil, Portal do Governo. Indígena de 8 Anos Que Faz Tratamento de Saúde em SP é 1ª Criança Vacinada do Brasil. Available online: https://www.saopaulo.sp.gov.br/sala-de-imprensa/release/indigena-de-8-anos-que-faz-tratamento-de-saude-em-sp-e-1a-crianca-vacinada-do-brasil/ (accessed on 29 August 2022).
- Castro, D. Cartazes Chamam de ‘Veneno’ Vacinas Contra Covid Para Crianças No Interior de SP, Folha de São Paulo, 10 de fevereiro de 2022. Available online: https://www1.folha.uol.com.br/equilibrioesaude/2022/02/cartazes-chamam-de-veneno-vacinas-contra-covid-para-criancas-no-interior-de-sp.shtml (accessed on 29 August 2022).
- Moreira, M. Movimento Antivacina Impede Avanço na Imunização de Crianças, Correio do Estado, 11 de Fevereiro de 2022. Available online: https://www.correiodoestado.com.br/cidades/movimento-antivacina-impede-avanco-na-imunizacao-de-criancas/396463 (accessed on 29 August 2022).
- Paschoalotto, M.A.C.; Costa, E.P.P.A.; Almeida, S.V.; Cima, J.; Costa, J.G.; Santos, J.V.; Barros, P.P.; Passador, C.S.; Passador, J.L. Running away from the jab: Factors associated with COVID-19 vaccine hesitancy in Brazil. Rev. Saude Publica 2021, 55, 97. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, J. Após Seis Meses, 40% Das Crianças Ainda Não Receberam Nenhuma Dose de Vacina Contra Covid, Repórter Brasil. Available online: https://reporterbrasil.org.br/2022/06/apos-seis-meses-40-por-cento-das-criancas-ainda-nao-receberam-nenhuma-dose-de-vacina-contra-covid/ (accessed on 17 October 2022).
- Eysenbach, G. Improving the quality of Web surveys: The Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J. Med. Internet Res. 2004, 6, e132. [Google Scholar] [CrossRef] [PubMed]
- Patridge, E.F.; Bardyn, T.P. Research electronic data capture (REDCap). J. Med. Libr. Assoc. 2018, 106, 142–144. [Google Scholar] [CrossRef] [Green Version]
- Israel, G.D. Determining Sample Size; University of Florida: Gainesville, FL, USA, 1992. [Google Scholar]
- Zucoloto, M.L.; Meneghini, A.C.; Martinez, E.Z. Panorama of COVID-19, risk perception and vaccine confidence in São Paulo State population, Southeast Brazil. Health Soc. Care Community 2022. [Google Scholar] [CrossRef]
- Opel, D.J.; Mangione-Smith, R.; Taylor, J.A.; Korfiatis, C.; Wiese, C.; Catz, S.; Martin, D.P. Development of a survey to identify vaccine-hesitant parents: The parent attitudes about childhood vaccines survey. Hum. Vaccines 2011, 7, 419–425. [Google Scholar] [CrossRef] [Green Version]
- Larson, H.J.; Jarrett, C.; Schulz, W.S.; Chaudhuri, M.; Zhou, Y.; Dube, E.; Schuster, M.; MacDonald, N.E.; Wilson, R.; SAGE Working Group on Vaccine Hesitancy. Measuring vaccine hesitancy: The development of a survey tool. Vaccine 2015, 33, 4165–4175. [Google Scholar] [CrossRef] [Green Version]
- Opel, D.J.; Taylor, J.A.; Mangione-Smith, R.; Solomon, C.; Zhao, C.; Catz, S.; Martin, D. Validity and reliability of a survey to identify vaccine-hesitant parents. Vaccine 2011, 29, 6598–6605. [Google Scholar] [CrossRef]
- Sison, C.P.; Glaz, J. Simultaneous confidence intervals and sample size determination for multinomial proportions. J. Am. Stat. Assoc. 1995, 90, 366–369. [Google Scholar] [CrossRef]
- Hope, A.C.A. A simplified Monte Carlo significance test procedure. J. R. Stat. Soc. Ser. B Stat. Methodol. 1968, 30, 582–598. [Google Scholar] [CrossRef]
- Rea, L.M.; Parker, R.A. Designing and Conducting Survey Research; Jossey-Boss: San Francisco, CA, USA, 2014. [Google Scholar]
- Amrhein, V.; Greenland, S.; McShane, B. Scientists rise up against statistical significance. Nature 2019, 567, 305–307. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olejnik, S.; Algina, J. Generalized eta and omega squared statistics: Measures of effect size for some common research designs. Psychol. Methods 2003, 8, 434–447. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Science, 2nd ed.; Lawrence Erlbaum Associates: Hillsdale, MI, USA, 1988; pp. 284–288. [Google Scholar]
- Graeber, D.; Schmidt-Petri, C.; Schröder, C. Attitudes on voluntary and mandatory vaccination against COVID-19: Evidence from Germany. PloS One 2021, 16, e0248372. [Google Scholar] [CrossRef] [PubMed]
- Gagneux-Brunon, A.; Botelho-Nevers, E.; Bonneton, M.; Peretti-Watel, P.; Verger, P.; Launay, O.; Ward, J.K. Public opinion on a mandatory COVID-19 vaccination policy in France: A cross-sectional survey. Clin. Microbiol. Infect. 2022, 28, 433–439. [Google Scholar] [CrossRef]
- Soares, P.; Rocha, J.V.; Moniz, M.; Gama, A.; Laires, P.A.; Pedro, A.R.; Dias, S.; Leite, A.; Nunes, C. Factors associated with COVID-19 vaccine hesitancy. Vaccines 2021, 9, 300. [Google Scholar] [CrossRef]
- Savoia, E.; Harriman, N.W.; Piltch-Loeb, R.; Bonetti, M.; Toffolutti, V.; Testa, M.A. Exploring the association between misinformation endorsement, opinions on the government response, risk perception, and COVID-19 vaccine hesitancy in the US, Canada, and Italy. Vaccines 2022, 10, 671. [Google Scholar] [CrossRef]
- Zarbo, C.; Candini, V.; Ferrari, C.; d’Addazio, M.; Calamandrei, G.; Starace, F.; Caserotti, M.; Gavaruzzi, T.; Lotto, L.; Tasso, A.; et al. COVID-19 Vaccine Hesitancy in Italy: Predictors of Acceptance, Fence Sitting and Refusal of the COVID-19 Vaccination. Front. Public Health 2022, 10, 873098. [Google Scholar] [CrossRef]
- White, T.M.; Cash-Gibson, L.; Martin-Moreno, J.M.; Matesanz, R.; Crespo, J.; Alfonso-Sanchez, J.L.; Villapol, S.; El-Mohandes, A.; Lazarus, J.V. COVID-SCORE Spain: Public perceptions of key government COVID-19 control measures. Eur. J. Public Health 2021, 31, 1095–1102. [Google Scholar] [CrossRef]
- Boschiero, M.N.; Palamim, C.V.C.; Marson, F.A.L. COVID-19 vaccination on Brazil and the crocodile side-effect. Ethics Med. Public Health 2021, 17, 100654. [Google Scholar] [CrossRef]
- Daniels, J.P. Health experts slam Bolsonaro’s vaccine comments. Lancet 2021, 397, 361. [Google Scholar] [CrossRef]
- Barberia, L.G.; Gómez, E.J. Political and institutional perils of Brazil’s COVID-19 crisis. Lancet 2020, 396, 367–368. [Google Scholar] [CrossRef]
- Roman, Y.M.; Burela, P.A.; Pasupuleti, V.; Piscoya, A.; Vidal, J.E.; Hernandez, A.V. Ivermectin for the treatment of coronavirus disease 2019: A systematic review and meta-analysis of randomized controlled trials. Clin. Infect. Dis. 2022, 74, 1022–1029. [Google Scholar] [CrossRef] [PubMed]
- Farias, D.B.L.; Casarões, G.; Magalhães, D. Radical right populism and the politics of cruelty: The case of COVID-19 in Brazil under President Bolsonaro. Glob. Stud. Q. 2022, 2, ksab048. [Google Scholar] [CrossRef]
- Juen, C.M.; Jankowski, M.; Huber, R.A.; Frank, T.; Maaß, L.; Tepe, M. Who wants COVID-19 vaccination to be compulsory? The impact of party cues, left-right ideology, and populism. Politics 2021. [Google Scholar] [CrossRef]
- Rutjens, B.T.; Zarzeczna, N.; van der Lee, R. Science rejection in Greece: Spirituality predicts vaccine scepticism and low faith in science in a Greek sample. Public Underst. Sci. 2022, 31, 428–436. [Google Scholar] [CrossRef]
- Kuru, O.; Chan, M.P.; Lu, H.; Stecula, D.A.; Jamieson, K.H.; Albarracín, D. Religious affiliation and philosophical and moral beliefs about vaccines: A longitudinal study. J. Health Psychol. 2022, 27, 3059–3081. [Google Scholar] [CrossRef]
- Burity, J. The Brazilian conservative wave, the Bolsonaro administration, and religious actors. Braz. Political Sci. Rev. 2021, 15, 1–19. [Google Scholar] [CrossRef]
- Kibuuka, B.G.L. Complicity and synergy between Bolsonaro and Brazilian Evangelicals in COVID-19 times: Adherence to scientific negationism for political-religious reasons. Int. J. Lat. Am. Relig. 2020, 4, 288–317. [Google Scholar] [CrossRef]
- Capponi, G. Overlapping values: Religious and scientific conflicts during the COVID-19 crisis in Brazil. Soc. Anthropol. 2020, 28, 236–237. [Google Scholar] [CrossRef]
- Souza, A.R.; Simões, P. O enfrentamento espírita da pandemia do Covid-19 no Brasil. Teor. Cult. 2022, 17, 136–145. [Google Scholar]
- Evans, J.R.; Mathur, A. The value of online surveys. Internet Res. 2005, 15, 195–219. [Google Scholar] [CrossRef]
- Teotônio, I.; Hecht, M.; Castro, L.C.; Gandolfi, L.; Pratesi, R.; Nakano, E.Y.; Zandonadi, R.P.; Pratesi, C.B. Repercussion of COVID-19 pandemic on Brazilians’ quality of life: A nationwide cross-sectional study. Int. J. Environ. Res. Public Health 2020, 17, 8554. [Google Scholar] [CrossRef] [PubMed]
- Vancini, R.L.; Camargo-Neto, L.; de Lira, C.A.; Andrade, M.S.; Viana, R.B.; Nikolaidis, P.T.; Knechtle, B.; Gentil, P.; Piacezzi, L.H.V.; Lopes, M.C.B.T.; et al. Physical activity and sociodemographic profile of Brazilian people during COVID-19 outbreak: An online and cross-sectional survey. Int. J. Environ. Res. Public Health 2020, 17, 7964. [Google Scholar] [CrossRef] [PubMed]
- Cotrin, P.; Bahls, A.C.; da Silva, D.D.O.; Girão, V.M.P.; Pinzan-Vercelino, C.R.M.; de Oliveira, R.C.G.; Oliveira, R.C.; Carvalho, M.D.B.; Pelloso, S.M.; Valarelli, F.P.; et al. The use of facemasks during the COVID-19 pandemic by the Brazilian population. J. Multidiscip. Healthc. 2020, 13, 1169–1178. [Google Scholar] [CrossRef]
- Weigold, A.; Weigold, I.K.; Russell, E.J. Examination of the equivalence of self-report survey-based paper-and-pencil and internet data collection methods. Psychol. Methods 2013, 18, 53. [Google Scholar] [CrossRef]
- Penrod, J.; Preston, D.B.; Cain, R.E.; Starks, M.T. A discussion of chain referral as a method of sampling hard-to-reach populations. J. Transcult. Nurs. 2003, 14, 100–107. [Google Scholar] [CrossRef]
| Variable | Participants n (%) 1 | S95%CI for Proportions | Brazilian Population (%) 2 |
|---|---|---|---|
| Gender (n =1001) | |||
| Female | 725 (72.4) | (69.6, 75.2) | 51.8 |
| Male | 276 (27.6) | (24.8, 30.4) | 48.2 |
| Age group (years) (n =1004) | |||
| 18–24 | 177 (17.6) | (14.7, 20.7) | 14.9 |
| 25–30 | 136 (13.6) | (10.7, 16.6) | 12.7 |
| 31–35 | 138 (13.8) | (10.9, 16.8) | 10.6 |
| 36–40 | 145 (14.4) | (11.6, 17.5) | 10.9 |
| 41–50 | 207 (20.6) | (17.7, 23.7) | 18.3 |
| 51–60 | 132 (13.1) | (10.3, 16.2) | 14.8 |
| 61 or older | 69 (6.9) | (4.0, 9.9) | 17.8 |
| Education level (n =1006) | |||
| No schooling or incomplete elementary school | 2 (0.2) | (0, 3.1) | 38.7 |
| Completed elementary school or incomplete high school | 9 (0.9) | (0, 3.8) | 12.5 |
| Completed high school or incomplete higher education | 293 (29.1) | (26.2, 32.0) | 31.4 |
| Completed higher education | 702 (69.8) | (66.9, 72.7) | 17.5 |
| Brazilian Region (n =1006) | |||
| Southeast | 335 (33.3) | (30.1, 36.5) | 43.3 |
| Northeast | 234 (23.2) | (20.1, 26.5) | 26.3 |
| South | 201 (20.0) | (16.8, 23.2) | 14.8 |
| North | 128 (12.7) | (9.5, 16.0) | 7.8 |
| Central-West | 109 (10.8) | (7.6, 14.1) | 7.8 |
| Should the Vaccine for COVID-19 in Adults Be Mandatory? | |||||
|---|---|---|---|---|---|
| Total 1 | Yes n (%) | No n (%) | Not Sure n (%) | Effect Size 2 (p Value) 3 | |
| Gender (n = 999) | |||||
| Female | 723 | 503 (69.6) | 190 (26.3) | 30 (4.1) | 0.069 |
| Male | 276 | 172 (62.3) | 90 (32.6) | 14 (5.1) | (0.089) |
| Age groups (years) (n =1002) | |||||
| 18–24 | 177 | 150 (84.7) | 22 (12.4) | 5 (2.8) | 0.125 |
| 25–30 | 136 | 90 (66.2) | 41 (30.1) | 5 (3.7) | (<0.001) |
| 31–40 | 283 | 182 (64.3) | 88 (31.1) | 13 (4.6) | |
| 41–60 | 337 | 209 (62.0) | 110 (32.6) | 18 (5.3) | |
| 61 or older | 69 | 44 (63.8) | 22 (31.9) | 3 (4.3) | |
| Education level (n = 1004) | |||||
| No schooling or incomplete elementary school | 2 | 2 (100.0) | 0 (0.0) | 0 (0.0) | 0.057 |
| Completed elementary school or incomplete high school | 9 | 6 (66.7) | 3 (33.3) | 0 (0.0) | (0.308) |
| Completed high school or incomplete higher education | 292 | 212 (72.6) | 69 (23.6) | 11 (3.8) | |
| Completed higher education | 701 | 457 (65.2) | 211 (30.1) | 33 (4.7) | |
| Brazilian Region (n = 1005) | |||||
| Southeast | 335 | 209 (62.4) | 105 (31.3) | 21 (6.3) | 0.079 |
| Northeast | 234 | 170 (72.6) | 58 (24.8) | 6 (2.6) | (0.129) |
| South | 201 | 130 (64.7) | 64 (31.8) | 7 (3.5) | |
| North | 127 | 92 (72.4) | 29 (22.8) | 6 (4.7) | |
| Central-West | 108 | 76 (70.4) | 28 (25.9) | 4 (3.7) | |
| Are you a religious person? (n = 969) | |||||
| Very religious | 148 | 87 (58.8) | 57 (38.5) | 4 (2.7) | 0.086 |
| Moderately religious | 441 | 295 (66.9) | 126 (28.6) | 20 (4.5) | (0.025) |
| A little religious | 250 | 181 (72.4) | 56 (22.4) | 13 (5.2) | |
| Non-religious | 130 | 95 (73.1) | 30 (23.1) | 5 (3.8) | |
| Have a religion (n = 976) | |||||
| Catholic | 385 | 265 (68.8) | 102 (26.5) | 18 (4.7) | 0.108 |
| No religion, but believe in God | 197 | 140 (71.1) | 47 (23.9) | 10 (5.1) | (0.198) |
| Evangelic | 114 | 65 (57.0) | 44 (38.6) | 5 (4.4) | |
| Spiritist | 97 | 70 (72.2) | 24 (24.7) | 3 (3.1) | |
| Atheist | 63 | 50 (79.4) | 12 (19.0) | 1 (1.6) | |
| Protestant | 33 | 17 (51.5) | 13 (39.4) | 3 (9.1) | |
| Spiritualist | 31 | 19 (61.3) | 11 (35.5) | 1 (3.2) | |
| Umbandist | 17 | 12 (70.6) | 5 (29.4) | 0 (0.0) | |
| Buddhist | 6 | 5 (83.3) | 1 (16.7) | 0 (0.0) | |
| Other religions | 33 | 22 (66.7) | 11 (33.3) | 0 (0.0) | |
| Have you ever had COVID-19? (n = 1004) | |||||
| No | 415 | 297 (71.6) | 95 (22.9) | 23 (5.5) | 0.094 |
| Yes | 519 | 344 (66.3) | 159 (30.6) | 16 (3.1) | (0.001) |
| Not sure | 70 | 36 (51.4) | 29 (41.4) | 5 (7.1) | |
| Have you received a vaccination for COVID-19? (n = 995) | |||||
| No | 37 | 0 (0.0) | 37 (100.0) | 0 (0.0) | 0.327 |
| Yes, but only one dose | 55 | 6 (10.9) | 48 (87.3) | 1 (1.8) | (<0.001) |
| Yes, all doses available | 903 | 670 (74.2) | 191 (21.2) | 42 (4.7) | |
| Self-perception of risk (n = 1002) | |||||
| Very high | 75 | 52 (69.3) | 21 (28.0) | 2 (2.7) | 0.147 |
| High | 243 | 162 (66.7) | 68 (28.0) | 13 (5.3) | (<0.001) |
| Low | 436 | 320 (73.4) | 103 (23.6) | 13 (3.0) | |
| Very low | 161 | 102 (63.4) | 51 (31.7) | 8 (5.0) | |
| No risk at all | 19 | 3 (15.8) | 15 (78.9) | 1 (5.3) | |
| Not sure | 68 | 37 (54.4) | 24 (35.3) | 7 (10.3) | |
| Do you consider your knowledge of COVID-19 satisfactory? (n = 1003) | |||||
| Yes | 830 | 546 (65.8) | 250 (30.1) | 34 (4.1) | 0.090 |
| No | 92 | 62 (67.4) | 22 (23.9) | 8 (8.7) | (0.005) |
| Not sure | 81 | 68 (84.0) | 12 (14.8) | 1 (1.2) | |
| How do you evaluate the federal government’s performance in combating COVID-19? (n = 993) | |||||
| Very good | 116 | 38 (32.8) | 75 (64.7) | 3 (2.6) | 0.301 |
| Good | 163 | 81 (49.7) | 71 (43.6) | 11 (6.7) | (<0.001) |
| Average | 193 | 123 (63.7) | 64 (33.2) | 6 (3.1) | |
| Bad | 155 | 117 (75.5) | 31 (20.0) | 7 (4.5) | |
| Very bad | 366 | 318 (86.9) | 32 (8.7) | 16 (4.4) | |
| Do you agree that COVID-19 will finally be successfully controlled? (n = 1001) | |||||
| Yes | 514 | 320 (62.3) | 176 (34.2) | 18 (3.5) | 0.133 |
| No | 227 | 158 (69.6) | 63 (27.8) | 6 (2.6) | (<0.001) |
| Not sure | 260 | 199 (76.5) | 41 (15.8) | 20 (7.7) | |
| Have all your children between 5 and 11 years old received the COVID-19 vaccine? (n = 257) 4 | |||||
| Yes | 168 | 120 (71.5) | 37 (22.0) | 11 (6.5) | 0.489 |
| No | 89 | 21 (23.6) | 64 (71.9) | 4 (4.5) | (<0.001) |
| Should Parents and Guardians Be Free to Decide Whether Their Children Will Receive Vaccinations? | |||||
|---|---|---|---|---|---|
| Total 1 | Yes n (%) | No n (%) | Not Sure n (%) | Effect Size 2 (p Value) 3 | |
| Gender (n = 997) | |||||
| Female | 722 | 366 (50.7) | 288 (39.9) | 68 (9.4) | 0.029 |
| Male | 275 | 148 (53.8) | 104 (37.8) | 23 (8.4) | (0.662) |
| Age groups (years) (n = 1000) | |||||
| 18–24 | 176 | 63 (35.8) | 84 (47.7) | 29 (16.5) | 0.135 |
| 25–30 | 136 | 66 (48.5) | 58 (42.6) | 12 (8.8) | (<0.001) |
| 31–40 | 281 | 144 (51.2) | 112 (39.9) | 25 (8.9) | |
| 41–60 | 339 | 205 (60.5) | 113 (33.3) | 21 (6.2) | |
| 61 or older | 68 | 38 (55.9) | 27 (39.7) | 3 (4.4) | |
| Education level (n = 1002) | |||||
| No schooling or incomplete elementary school | 2 | 2 (100.0) | 0 (0.0) | 0 (0.0) | 0.055 |
| Completed elementary school or incomplete high school | 8 | 5 (62.5) | 3 (37.5) | 0 (0.0) | (0.397) |
| Completed high school or incomplete higher education | 292 | 145 (49.7) | 113 (38.7) | 34 (11.6) | |
| Completed higher education | 700 | 365 (52.1) | 279 (39.9) | 56 (8.0) | |
| Brazilian Region (n = 1003) | |||||
| Southeast | 334 | 167 (50.0) | 139 (41.6) | 28 (8.4) | 0.078 |
| Northeast | 233 | 105 (45.1) | 102 (43.8) | 26 (11.2) | (0.146) |
| South | 201 | 108 (53.7) | 77 (38.3) | 16 (8.0) | |
| North | 128 | 79 (61.7) | 40 (31.2) | 9 (7.0) | |
| Central-West | 107 | 58 (54.2) | 37 (34.6) | 12 (11.2) | |
| Are you a religious person? (n = 967) | |||||
| Very religious | 147 | 96 (65.3) | 40 (27.2) | 11 (7.5) | 0.183 |
| Moderately religious | 440 | 258 (58.6) | 145 (33.0) | 37 (8.4) | (<0.001) |
| A little religious | 250 | 102 (40.8) | 117 (46.8) | 31 (12.4) | |
| Non-religious | 130 | 37 (28.5) | 82 (63.1) | 11 (8.5) | |
| Have a religion (n = 974) | |||||
| Catholic | 386 | 212 (54.9) | 141 (36.5) | 33 (8.5) | 0.194 |
| No religion, but believe in God | 196 | 84 (42.9) | 88 (44.9) | 24 (12.2) | (<0.001) |
| Evangelic | 115 | 83 (72.2) | 24 (20.9) | 8 (7.0) | |
| Spiritist | 95 | 45 (47.4) | 42 (44.2) | 8 (8.4) | |
| Atheist | 63 | 10 (15.9) | 45 (71.4) | 8 (12.7) | |
| Protestant | 32 | 23 (71.9) | 6 (18.8) | 3 (9.4) | |
| Spiritualist | 31 | 16 (51.6) | 12 (38.7) | 3 (9.7) | |
| Umbandist | 17 | 7 (41.2) | 9 (52.9) | 1 (5.9) | |
| Buddhist | 6 | 4 (66.7) | 2 (33.3) | 0 (0.0) | |
| Other religions | 33 | 15 (45.5) | 17 (51.5) | 1 (3.0) | |
| Have you ever had COVID-19? (n = 1002) | |||||
| No | 413 | 195 (47.2) | 184 (44.6) | 34 (8.2) | 0.067 |
| Yes | 519 | 282 (54.3) | 189 (36.4) | 48 (9.2) | (0.064) |
| Not sure | 70 | 39 (55.7) | 22 (31.4) | 9 (12.9) | |
| Have you received a vaccination for COVID-19? (n = 993) | |||||
| No | 37 | 36 (97.3) | 1 (2.7) | 0 (0.0) | 0.197 |
| Yes, but only one dose | 55 | 51 (92.7) | 3 (5.5) | 1 (1.8) | (<0.001) |
| Yes, all doses available | 901 | 420 (46.6) | 391 (43.4) | 90 (10.0) | |
| Self-perception of risk (n = 1000) | |||||
| Very high | 75 | 36 (48.0) | 37 (49.3) | 2 (2.7) | 0.109 |
| High | 243 | 123 (50.6) | 98 (40.3) | 22 (9.1) | (0.009) |
| Low | 435 | 207 (47.6) | 182 (41.8) | 46 (10.6) | |
| Very low | 161 | 88 (54.7) | 57 (35.4) | 16 (9.9) | |
| No risk at all | 19 | 15 (78.9) | 4 (21.1) | 0 (0.0) | |
| Not sure | 67 | 46 (68.7) | 17 (25.4) | 4 (6.0) | |
| Do you consider your knowledge of COVID-19 satisfactory? (n = 1001) | |||||
| Yes | 828 | 432 (52.2) | 327 (39.5) | 69 (8.3) | 0.066 |
| No | 92 | 51 (55.4) | 29 (31.5) | 12 (13.0) | (0.066) |
| Not sure | 81 | 32 (39.5) | 39 (48.1) | 10 (12.3) | |
| How do you evaluate the federal government’s performance in combating COVID-19? (n = 992) | |||||
| Very good | 116 | 101 (87.1) | 8 (6.9) | 7 (6.0) | 0.366 |
| Good | 164 | 124 (75.6) | 27 (16.5) | 13 (7.9) | (<0.001) |
| Average | 191 | 121 (63.4) | 53 (27.7) | 17 (8.9) | |
| Bad | 155 | 70 (45.2) | 55 (35.5) | 30 (19.4) | |
| Very bad | 366 | 91 (24.9) | 252 (68.9) | 23 (6.3) | |
| Do you agree that COVID-19 will finally be successfully controlled? (n = 999) | |||||
| Yes | 513 | 296 (57.7) | 171 (33.3) | 46 (9.0) | 0.117 |
| No | 228 | 114 (50.0) | 101 (44.3) | 13 (5.7) | (<0.001) |
| Not sure | 258 | 103 (39.9) | 123 (47.7) | 32 (12.4) | |
| Have children between the ages of 5 and 11 (n = 990) | |||||
| Yes | 255 | 158 (62.0) | 78 (30.6) | 19 (7.5) | 0.127 |
| No | 735 | 349 (47.5) | 315 (42.9) | 71 (9.7) | (<0.001) |
| Have all your children between 5 and 11 years old received the COVID-19 vaccine? (n = 255) 4 | |||||
| Yes | 167 | 78 (46.7) | 72 (43.1) | 17 (10.2) | 0.433 |
| No | 88 | 80 (90.9) | 6 (6.8) | 2 (2.3) | (<0.001) |
| Total 1 | Mean (SD) | p Value 2 | ω2 Statistics 3 | |
|---|---|---|---|---|
| Gender (n = 962) | ||||
| Female | 698 | 13.70 (7.88) | 0.202 | <0.01 |
| Male | 264 | 14.83 (8.84) | ||
| Age groups (years) (n = 964) | ||||
| 18–24 | 168 | 11.31 (5.90) | <0.001 | 0.02 |
| 25–30 | 131 | 13.85 (7.81) | ||
| 31–40 | 273 | 13.88 (8.17) | ||
| 41–60 | 326 | 15.31 (8.74) | ||
| 61 or older | 66 | 15.36 (9.33) | ||
| Education level (n = 999) | ||||
| No schooling or incomplete elementary school | 2 | 14.50 (7.78) | 0.010 | <0.01 |
| Completed elementary school or incomplete high school | 8 | 12.12 (10.08) | ||
| Completed high school or incomplete higher education | 276 | 13.53 (7.01) | ||
| Completed higher education | 680 | 14.22 (8.58) | ||
| Brazilian Region (n = 967) | ||||
| Southeast | 328 | 14.63 (8.67) | 0.112 | <0.01 |
| South | 191 | 14.95 (8.93) | ||
| Northeast | 222 | 12.72 (7.35) | ||
| North | 121 | 13.84 (7.64) | ||
| Central-West | 105 | 13.45 (7.18) | ||
| Are you a religious person? (n = 933) | ||||
| Very religious | 143 | 16.71 (10.04) | <0.001 | 0.03 |
| Moderately religious | 423 | 14.65 (7.69) | ||
| A little religious | 242 | 12.19 (6.97) | ||
| Non-religious | 125 | 11.58 (7.81) | ||
| Have a religion (n = 939) | ||||
| Catholic | 374 | 13.68 (7.79) | <0.001 | 0.05 |
| No religion, but believe in God | 187 | 12.91 (8.11) | ||
| Evangelic | 110 | 17.58 (8.05) | ||
| Spiritist | 92 | 12.95 (7.50) | ||
| Atheist | 61 | 10.23 (5.82) | ||
| Protestant | 30 | 18.67 (8.40) | ||
| Spiritualist | 29 | 14.62 (9.47) | ||
| Umbandist | 17 | 15.41 (10.15) | ||
| Buddhist | 6 | 13.50 (11.33) | ||
| Other religions | 33 | 14.24 (7.86) | ||
| Have you ever had COVID-19? (n = 966) | ||||
| No | 402 | 12.79 (7.48) | <0.01 | 0.02 |
| Yes | 497 | 14.86 (8.46) | ||
| Not sure | 67 | 14.96 (8.96) | ||
| Have you received a vaccination for COVID-19? (n = 958) | ||||
| No | 34 | 32.79 (4.07) | <0.01 | 0.21 |
| Yes, but only one dose | 51 | 26.63 (7.85) | ||
| Yes, all doses available | 873 | 12.38 (6.42) | ||
| Self-perception of risk (n = 965) | ||||
| Very high | 72 | 11.90 (6.25) | <0.01 | 0.05 |
| High | 232 | 14.12 (7.68) | ||
| Low | 427 | 13.09 (7.51) | ||
| Very low | 157 | 14.37 (9.27) | ||
| No risk at all | 16 | 27.81 (9.94) | ||
| Not sure | 61 | 18.07 (8.54) | ||
| Do you consider your knowledge of COVID-19 satisfactory? (n = 965) | ||||
| Yes | 805 | 13.98 (8.43) | 0.14 | <0.01 |
| No | 84 | 15.07 (6.92) | ||
| Not sure | 76 | 13.07 (6.34) | ||
| How do you evaluate the federal government’s performance in combating COVID-19? (n = 959) | ||||
| Very good | 113 | 23.81 (8.87) | <0.01 | 0.04 |
| Good | 158 | 18.12 (7.38) | ||
| Average | 185 | 15.29 (7.39) | ||
| Bad | 147 | 12.12 (6.08) | ||
| Very bad | 356 | 8.99 (4.37) | ||
| Do you agree that COVID-19 will finally be successfully controlled? (n = 963) | ||||
| Yes | 493 | 14.86 (8.64) | 0.01 | <0.01 |
| No | 224 | 13.69 (8.20) | ||
| Not sure | 246 | 12.40 (6.59) | ||
| Have children between the ages of 5 and 11 (n = 957) | ||||
| Yes | 249 | 16.42 (9.30) | <0.01 | 0.02 |
| No | 708 | 13.05 (7.48) | ||
| Have all your children between 5 and 11 years old received the COVID-19 vaccine? (n = 249) 4 | ||||
| Yes | 167 | 11.75 (5.92) | <0.01 | 0.44 |
| No | 82 | 25.93 (7.51) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martinez, E.Z.; Zucoloto, M.L.; Ramos, V.P.; Dutra, C.D.C.; de Jesus, G.J.; Esteves, A.V.F.; Abreu, I.S.; Mombelli, M.A.; Reis, R.A.; Campoamor, M.M.; et al. Brazilian Adults’ Attitudes and Practices Regarding the Mandatory COVID-19 Vaccination and Their Hesitancy towards Childhood Vaccination. Vaccines 2022, 10, 1853. https://doi.org/10.3390/vaccines10111853
Martinez EZ, Zucoloto ML, Ramos VP, Dutra CDC, de Jesus GJ, Esteves AVF, Abreu IS, Mombelli MA, Reis RA, Campoamor MM, et al. Brazilian Adults’ Attitudes and Practices Regarding the Mandatory COVID-19 Vaccination and Their Hesitancy towards Childhood Vaccination. Vaccines. 2022; 10(11):1853. https://doi.org/10.3390/vaccines10111853
Chicago/Turabian StyleMartinez, Edson Zangiacomi, Miriane Lucindo Zucoloto, Vânia Pinheiro Ramos, Carla Daiane Costa Dutra, Giselle Juliana de Jesus, Arinete Véras Fontes Esteves, Isabella Schroeder Abreu, Monica Augusta Mombelli, Roberta Alvarenga Reis, Marilia Marcondes Campoamor, and et al. 2022. "Brazilian Adults’ Attitudes and Practices Regarding the Mandatory COVID-19 Vaccination and Their Hesitancy towards Childhood Vaccination" Vaccines 10, no. 11: 1853. https://doi.org/10.3390/vaccines10111853
APA StyleMartinez, E. Z., Zucoloto, M. L., Ramos, V. P., Dutra, C. D. C., de Jesus, G. J., Esteves, A. V. F., Abreu, I. S., Mombelli, M. A., Reis, R. A., Campoamor, M. M., da Silva, W. R., & dos Santos, C. B. (2022). Brazilian Adults’ Attitudes and Practices Regarding the Mandatory COVID-19 Vaccination and Their Hesitancy towards Childhood Vaccination. Vaccines, 10(11), 1853. https://doi.org/10.3390/vaccines10111853







