Advances in Nanotechnology for Cancer Immunoprevention and Immunotherapy: A Review
Abstract
:1. Introduction
2. Role of Immune System in Cancer
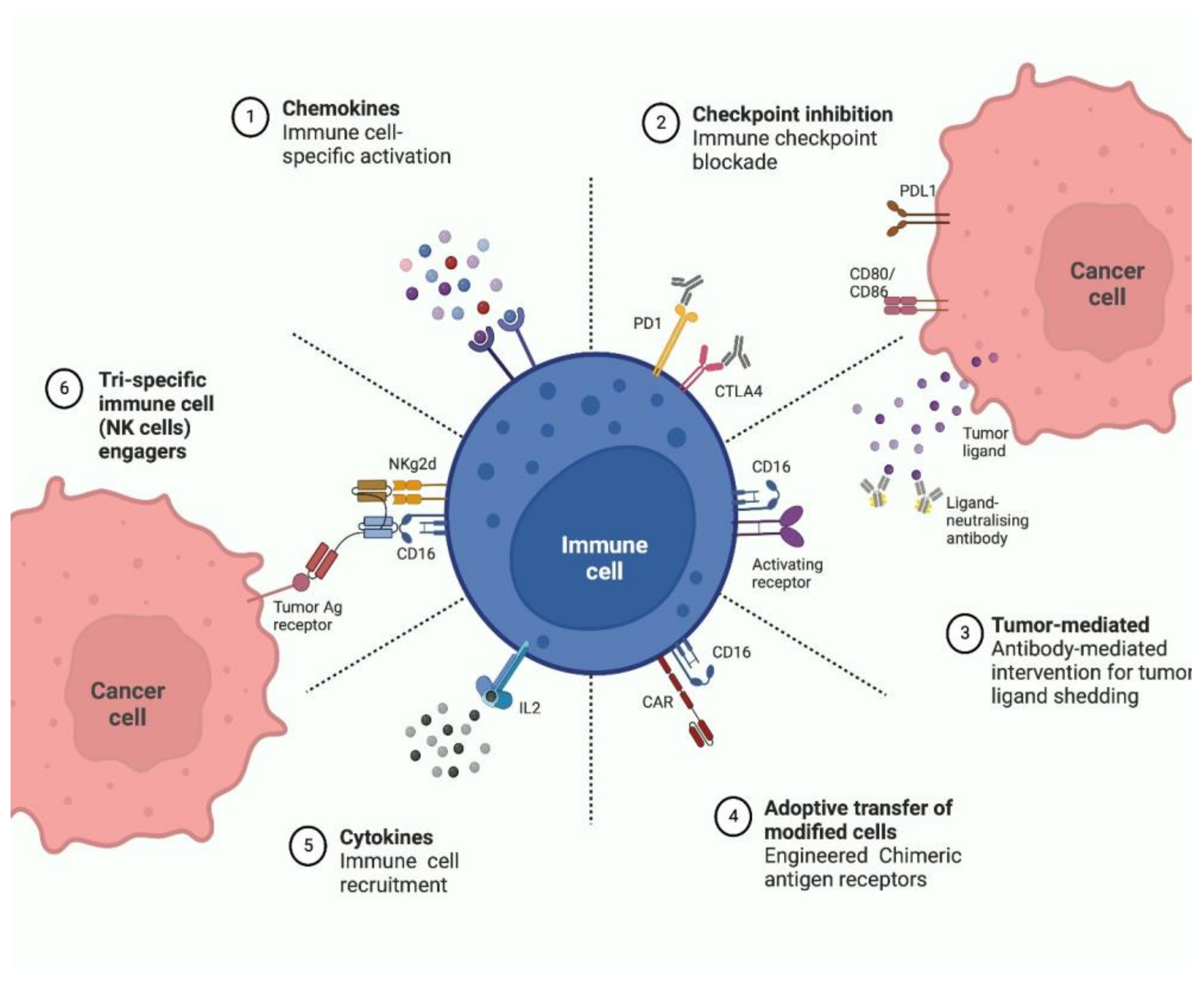
3. Distinguishing Premalignant from Malignant Lesions
4. Immunotherapy and Cancer
4.1. Monoclonal Antibodies
4.2. Checkpoint Blockade
4.3. Non-Specific Immunotherapies
4.4. Immunotherapy Vaccine
4.5. Oncolytic virus Immunotherapy
4.6. Adoptive Cell Therapy
5. Immunotherapy for Cancer: Overcoming the Challenges
6. Nanotechnology in Cancer Immunotherapy
6.1. Nanoparticle-Based Delivery of Anticancer Antigen
6.2. Nanoparticle-Mediated Adjuvant Delivery
6.3. Nanoparticle-Mediated Modulation of the Immunosuppressive TME
7. Cancer Immunoprevention and Its Strategies
7.1. Vaccines in Cancer Immunoprevention
7.2. Immunoprevention and Virally-Induced Tumors
7.3. Tumor Antigens in Cancer Immunoprevention
7.4. Immunomodulators in Cancer Immunoprevention
7.5. Immune Checkpoint Inhibitors in Immunoprevention
7.6. Nanoparticle-Based Cancer Immunoprevention
8. Nanotechnology and Cancer Immunoprevention
9. Applications of Nanotechnology in Cancer Vaccines
9.1. Nanotechnology in Peptide-Based Vaccines
9.2. Nanotechnology in Nucleic Acid-Based Vaccines
9.3. Nanotechnology in Tumor Cell or Lysate-Based Vaccines
10. Future Prospects and Challenges in Cancer Immunoprevention
11. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Dwyer-Lindgren, L.; Bertozzi-Villa, A.; Stubbs, R.W.; Morozoff, C.; Kutz, M.J.; Huynh, C.; Barber, R.M.; Shackelford, K.A.; Mackenbach, J.P.; Van Lenthe, F.J.; et al. US County-Level Trends in Mortality Rates for Major Causes of Death, 1980-2014. JAMA-J. Am. Med. Assoc. 2016, 316, 2385–2401. [Google Scholar] [CrossRef] [Green Version]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global Cancer Statistics 2018: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA. Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [Green Version]
- Farrow, N.E.; Turner, M.C.; Salama, A.K.S.; Beasley, G.M. Overall Survival Improved for Contemporary Patients with Melanoma: A 2004–2015 National Cancer Database Analysis. Oncol. Ther. 2020, 8, 261–275. [Google Scholar] [CrossRef]
- Pishvaian, M.J.; Blais, E.M.; Brody, P.J.R.; Dearbeloa, P.; Hendifar, A.; Mikhail, S.; Sahai, V.; Sohal, D.P.S.; Bellakbira, S.; Rahib, L.; et al. Overall Survival in Patients with Pancreatic Cancer Receiving Matched Therapies Following Molecular Profiling: A Retrospective Analysis of the Know Your Tumor Registry Trial. Lancent Oncol. 2020, 21, 508–518. [Google Scholar] [CrossRef]
- Yu, D.P.; Cheng, X.; Liu, Z.D.; Xu, S.F. Comparative Beneficiary Effects of Immunotherapy against Chemotherapy in Patients with Advanced NSCLC: Meta-Analysis and Systematic Review. Oncol. Lett. 2017, 14, 1568–1580. [Google Scholar] [CrossRef] [Green Version]
- Kensler, T.W.; Spira, A.; Garber, J.E.; Szabo, E.; Lee, J.J.; Dong, Z.; Dannenberg, A.J.; Hait, W.N.; Blackburn, E.; Davidson, N.E.; et al. Transforming Cancer Prevention through Precision Medicine and Immune-Oncology. Cancer Prev. Res. 2016, 9, 2–10. [Google Scholar] [CrossRef] [Green Version]
- Ravery, V. Chemotherapy of Premalignant Lesions: New Insights. BJU Int. 2007, 100, 18–21. [Google Scholar] [CrossRef]
- Magee, D.E.; Hird, A.E.; Klaassen, Z.; Sridhar, S.S.; Nam, R.K.; Wallis, C.J.D.; Kulkarni, G.S. Adverse Event Profile for Immunotherapy Agents Compared with Chemotherapy in Solid Organ Tumors: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Ann. Oncol. 2020, 31, 50–60. [Google Scholar] [CrossRef] [Green Version]
- Kirman, J.R.; Quinn, K.M.; Seder, R.A. Immunological Memory. Immunol. Cell Biol. 2019, 97, 615–616. [Google Scholar] [CrossRef] [PubMed]
- Varadé, J.; Magadán, S.; González-Fernández, Á. Human Immunology and Immunotherapy: Main Achievements and Challenges. Cell. Mol. Immunol. 2021, 18, 805–828. [Google Scholar] [CrossRef]
- Umar, A. Cancer Immunoprevention: A New Approach to Intercept Cancer Early. Cancer Prev. Res. 2014, 1067–1072. [Google Scholar] [CrossRef] [Green Version]
- McCarthy, E.F. The Toxins of William B. Coley and the Treatment of Bone and Soft-Tissue Sarcomas. Iowa Orthop. J. 2006, 26, 154–158. [Google Scholar]
- Coley, W.B. Contribution To the Knowledge of Sarcoma. Ann. Surg. 1891, 14, 199–220. [Google Scholar] [CrossRef]
- Kasten, F.H. Paul Ehrlich: Pathfinder in Cell Biology 1. Chronicle of His Life and Accomplishments in Immunology, Cancer Research, and Chemotherapy. Biotech. Histochem. 1996, 71, 2–37. [Google Scholar] [CrossRef]
- Burnet, M. Cancer-A Biological Approach* Iii. Viruses Associated With Neoplastic Conditions. Br. Med. J. 1957, 1, 841. [Google Scholar] [CrossRef]
- Dunn, B.K.; Kramer, B.S. Cancer Prevention: Lessons Learned and Future Directions. Physiol. Behav. 2017, 176, 139–148. [Google Scholar] [CrossRef] [Green Version]
- Nowell, M.; Williams, A.S.; Carty, S.A.; Scheller, J.; Hayes, A.J.; Jones, G.W.; Richards, P.J.; Slinn, S.; Ernst, M.; Jenkins, B.J.; et al. Therapeutic Targeting of IL-6 Trans Signaling Counteracts STAT3 Control of Experimental Inflammatory Arthritis. J. Immunol. 2009, 182, 613–622. [Google Scholar] [CrossRef] [Green Version]
- Sansone, P.; Storci, G.; Tavolari, S.; Guarnieri, T.; Giovannini, C.; Taffurelli, M.; Ceccarelli, C.; Santini, D.; Paterini, P.; Marcu, K.B.; et al. IL-6 Triggers Malignant Features in Mammospheres from Human Ductal Breast Carcinoma and Normal Mammary Gland. J. Clin. Investig. 2007, 117, 3988–4002. [Google Scholar] [CrossRef]
- Atkins, D.; Breuckmann, A.; Schmahl, G.E.; Binner, P.; Ferrone, S.; Krummenauer, F.; Störkel, S.; Seliger, B. MHC Class I Antigen Processing Pathway Defects, Ras Mutations and Disease Stage in Colorectal Carcinoma. Int. J. Cancer 2004, 109, 265–273. [Google Scholar] [CrossRef]
- Maher, J.; Davies, E.T. Targeting Cytotoxic T Lymphocytes for Cancer Immunotherapy. Br. J. Cancer 2004, 91, 817–821. [Google Scholar] [CrossRef] [Green Version]
- Zhao, Y.; Niu, C.; Cui, J. Gamma-Delta (Γδ) T Cells: Friend or Foe in Cancer Development. J. Transl. Med. 2018, 16, 1–13. [Google Scholar] [CrossRef]
- Krasnova, Y.; Putz, E.M.; Smyth, M.J.; Souza-Fonseca-Guimaraes, F. Bench to Bedside: NK Cells and Control of Metastasis. Clin. Immunol. 2017, 177, 50–59. [Google Scholar] [CrossRef]
- Bianchi, G.; Borgonovo, G.; Pistoia, V.; Raffaghello, L. Immunosuppressive Cells and Tumour Microenvironment: Focus on Mesenchymal Stem Cells and Myeloid Derived Suppressor Cells. Histol. Histopathol. 2011, 26, 941–951. [Google Scholar] [CrossRef]
- Beatty, G.L.; Gladney, W.L. Immune Escape Mechanisms as a Guide for Cancer Immunotherapy Gregory. Mil. Med. 2006, 171, 844–848. [Google Scholar] [CrossRef] [Green Version]
- Raber, P.L.; Thevenot, P.; Sierra, R.; Wyczechowska, D.; Halle, D.; Ramirez, M.E.; Ochoa, A.C.; Fletcher, M.; Velasco, C.; Wilk, A.; et al. Subpopulations of Myeloid-Derived Suppressor Cells Impair T Cell Responses through Independent Nitric Oxide-Related Pathways. Int. J. Cancer 2014, 134, 2853–2864. [Google Scholar] [CrossRef]
- Facciabene, A.; Motz, G.T.; Coukos, G. T Regulatory Cells: Key Players in Tumor Immune Escape and Angiogenesis. Mol. Cell. Biochem. 2012, 23, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Martinez, F.O.; Sica, A.; Mantovani, A.; Locati, M. Macrophage Activation and Polarization. Bioscience 2008, 13, 453–461. [Google Scholar] [CrossRef] [Green Version]
- Blank, C.; Kuball, J.; Voelkl, S.; Wiendl, H.; Becker, B.; Walter, B.; Majdic, O.; Gajewski, T.F.; Theobald, M.; Andreesen, R.; et al. Blockade of PD-L1 (B7-H1) Augments Human Tumor-Specific T Cell Responses in Vitro. Int. J. Cancer 2006, 119, 317–327. [Google Scholar] [CrossRef]
- Dong, H.; Strome, S.E.; Salomao, D.R.; Tamura, H.; Hirano, F.; Flies, D.B.; Roche, P.C.; Lu, J.; Zhu, G.; Tamada, K.; et al. Tumor-Associated B7-H1 Promotes T-Cell Apoptosis: A Potential Mechanism of Immune Evasion. Nat. Med. 2002, 8, 793–800. [Google Scholar] [CrossRef]
- Schwartz, R.H. Costimulation of T Lymphocytes: The Role of CD28, CTLA-4, and B7/BB1 in Interleukin-2 Production and Immunotherapy. Cell 1992, 71, 1065–1068. [Google Scholar] [CrossRef]
- Tirapu, I.; Huarte, E.; Guiducci, C.; Anna, A.; Zaratiegui, M.; Murillo, O.; Gonzalez, A.; Berasain, C.; Berraondo, P.; Fortes, P.; et al. Low Surface Expression of B7-1 (CD80) Is an Immunoescape Mechanism of Colon Carcinoma. Cancer Res. 2006, 66, 2442–2450. [Google Scholar] [CrossRef] [PubMed]
- Upreti, M.; Jyoti, A.; Sethi, P. Tumor Microenvironment and Nanotherapeutics Meenakshi. Transl. Cancer Res. 2013, 2, 309–319. [Google Scholar] [CrossRef] [PubMed]
- Kelloff, G.J.; Sullivan, D.C.; Baker, H.; Clarke, L.P.; Nordstrom, R.; Tatum, J.L.; Dorfman, G.S.; Jacobs, P.; Berg, C.D.; Pomper, M.G.; et al. Workshop on Imaging Science Development for Cancer Prevention and Preemption. Cancer Biomark. 2007, 3, 1–33. [Google Scholar] [CrossRef] [Green Version]
- Vincent, T.L.; Gatenby, R.A. An Evolutionary Model for Initiation, Promotion and Progression in Carcinogenesis. Int. J. Oncol. 2008, 32, 729–737. [Google Scholar]
- Di Tomaso, E.; Capen, D.; Haskell, A.; Hart, J.; Logie, J.J.; Jain, R.K.; McDonald, D.M.; Jones, R.; Munn, L.L. Mosaic Tumor Vessels: Cellular Basis and Ultrastructure of Focal Regions Lacking Endothelial Cell Markers. Cancer Res. 2005, 65, 5740–5749. [Google Scholar] [CrossRef] [Green Version]
- Krop, I.; März, A.; Carlsson, H.; Li, X.; Bloushtain-Qimron, N.; Hu, M.; Gelman, R.; Sabel, M.S.; Schnitt, S.; Ramaswamy, S.; et al. A Putative Role for Psoriasin in Breast Tumor Progression. Cancer Res. 2005, 65, 11326–11334. [Google Scholar] [CrossRef] [Green Version]
- Bigler, S.A.; Deering, R.E.; Brawer, M.K. Comparison of Microscopic Vascularity in Benign and Malignant Prostate Tissue. Hum. Pathol. 1993, 24, 220–226. [Google Scholar] [CrossRef]
- Lowe, S.W.; Lin, A.W. Apoptosis in Cancer. Acta Soc. Med. Ups. 1959, 64, 313–321. [Google Scholar]
- Brouwers, F.M.; Elkahloun, A.G.; Munson, P.J.; Eisenhofer, G.; Barb, J.; Linehan, W.M.; Lenders, J.W.M.; De Krijger, R.; Mannelli, M.; Udelsman, R.; et al. Gene Expression Profiling of Benign and Malignant Pheochromocytoma. Physiol. Behav. 2017, 176, 139–148. [Google Scholar] [CrossRef] [Green Version]
- Raghavan, R.; Koyande, N.; Beher, R.; Chetlangia, N.; Ramadwar, M.; Pawade, S.; Thorat, R.; van Hengel, J.; Sklyarova, T.; van Roy, F.; et al. Plakophilin3 Loss Leads to Increased Adenoma Formation and Rectal Prolapse in APCmin Mice. Biochem. Biophys. Res. Commun. 2022, 586, 14–19. [Google Scholar] [CrossRef]
- Ugolkov, A.V.; Eisengart, L.J.; Luan, C.; Yang, X.J. Expression Analysis of Putative Stem Cell Markers in Human Benign and Malignant Prostate. Prostate 2011, 71, 18–25. [Google Scholar] [CrossRef]
- Sager, R. Tumor Suppressor Genes: The Puzzle and the Promise. Science 1989, 246, 1406–1412. [Google Scholar] [CrossRef]
- Fischer, H.; Taylor, N.; Allerstorfer, S.; Grusch, M.; Sonvilla, G.; Holzmann, K.; Setinek, U.; Elbling, L.; Cantonati, H.; Grasl-Kraupp, B.; et al. Fibroblast Growth Factor Receptor-Mediated Signals Contribute to the Malignant Phenotype of Non-Small Cell Lung Cancer Cells: Therapeutic Implications and Synergism with Epidermal Growth Factor Receptor Inhibition. Mol. Cancer Ther. 2008, 7, 3408–3419. [Google Scholar] [CrossRef]
- Waldman, A.D.; Fritz, J.M.; Lenardo, M.J. A Guide to Cancer Immunotherapy: From T Cell Basic Science to Clinical Practice. Nat. Rev. Immunol. 2020, 20, 651–668. [Google Scholar] [CrossRef]
- Park, W.; Heo, Y.J.; Han, D.K. New Opportunities for Nanoparticles in Cancer Immunotherapy. Biomater. Res. 2018, 22, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Zahavi, D.; Weiner, L. Monoclonal Antibodies in Cancer Therapy. Antibodies 2020, 9, 34. [Google Scholar] [CrossRef]
- Berger, M.; Shankar, V.; Vafai, A. Therapeutic Applications of Monoclonal Antibodies. Am. J. Med. Sci. 2002, 324, 14–30. [Google Scholar] [CrossRef]
- Koprowski, H.; Steplewski, Z.; Herlyn, D.; Herlyn, M. Study of Antibodies against Human Melanoma Produced by Somatic Cell Hybrids. Proc. Natl. Acad. Sci. USA 1978, 75, 3405–3409. [Google Scholar] [CrossRef] [Green Version]
- Scott, A.M.; Allison, J.P.; Wolchok, J.D. Monoclonal Antibodies in Cancer Therapy. Cancer Immun. 2012, 12, 1–20. [Google Scholar]
- Franzin, R.; Netti, G.S.; Spadaccino, F.; Porta, C.; Gesualdo, L.; Stallone, G.; Castellano, G.; Ranieri, E. The Use of Immune Checkpoint Inhibitors in Oncology and the Occurrence of AKI: Where Do We Stand? Front. Immunol. 2020, 11, 1–20. [Google Scholar] [CrossRef]
- Monjazeb, A.M.; Hsiao, H.H.; Sckisel, G.D.; Murphy, W.J. The Role of Antigen-Specific and Non-Specific Immunotherapy in the Treatment of Cancer. J. Immunotoxicol. 2012, 9, 248–258. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bonfim, M.; Vasconcelos, S.; Mengel, J.; Castello-branco, L.R.R.; Pinho, R.T. Bacillus Calmette–Gu é Rin Immunotherapy for Cancer. Vaccines 2021, 9, 439. [Google Scholar]
- Khong, H.; Overwijk, W.W. Adjuvants for Peptide-Based Cancer Vaccines. J. Immunother. Cancer 2016, 4, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Tiptiri-Kourpeti, A.; Spyridopoulou, K.; Pappa, A.; Chlichlia, K. DNA Vaccines to Attack Cancer: Strategies for Improving Immunogenicity and Efficacy. Pharmacol. Ther. 2016, 165, 32–49. [Google Scholar] [CrossRef]
- Liu, J.; Fu, M.; Wang, M.; Wan, D.; Wei, Y.; Wei, X. Cancer Vaccines as Promising Immuno-Therapeutics: Platforms and Current Progress. J. Hematol. Oncol. 2022, 15, 1–26. [Google Scholar] [CrossRef]
- Hollingsworth, R.E.; Jansen, K. Turning the Corner on Therapeutic Cancer Vaccines. NPJ Vaccines 2019, 4, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Hege, K.M.; Jooss, K.; Pardoll, D. GM-CSF Gene-Modifed Cancer Cell Immunotherapies: Of Mice and Men. Int. Rev. Immunol. 2006, 25, 321–352. [Google Scholar] [CrossRef]
- Hemminki, O.; Dos Santos, J.M.; Hemminki, A. Oncolytic Viruses for Cancer Immunotherapy. J. Hematol. Oncol. 2020, 13, 1–15. [Google Scholar] [CrossRef]
- Salloum, A.; Koblinski, J.; Bazzi, N.; Zeitouni, N.C. Talimogene Laherparepvec in Non-Melanoma Cancers. J. Clin. Aesthet. Dermatol. 2021, 14, 18. [Google Scholar]
- Valpione, S.; Campana, L.G. Immunotherapy for Advanced Melanoma: Future Directions. Immunotherapy 2016, 8, 199–209. [Google Scholar] [CrossRef]
- Zhang, Q.; Ping, J.; Huang, Z.; Zhang, X.; Zhou, J.; Wang, G.; Shaoyang, L.; Jianjun, M. CAR-T Cell Therapy in Cancer: Tribulations and Road Ahead. J. Immunol. Res. 2020, 2020, 1924379. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee Ventola, C. Cancer Immunotherapy, Part 3: Challenges and Future Trends. P T 2017, 42, 514–521. [Google Scholar]
- Chiriva-Internati, M.; Bot, A. A New Era in Cancer Immunotherapy: Discovering Novel Targets and Reprogramming the Immune System. Int. Rev. Immunol. 2015, 34, 101–103. [Google Scholar] [CrossRef] [PubMed]
- Pardoll, D. Cancer and the Immune System: Basic Concepts and Targets for Intervention. Semin. Oncol. 2015, 42, 523–538. [Google Scholar] [CrossRef] [Green Version]
- Zugazagoitia, J.; Guedes, C.; Ponce, S.; Ferrer, I.; Molina-Pinelo, S.; Paz-Ares, L. Current Challenges in Cancer Treatment. Clin. Ther. 2016, 38, 1551–1566. [Google Scholar] [CrossRef] [Green Version]
- Goldberg, M.S. Improving Cancer Immunotherapy through Nanotechnology. Nat. Rev. Cancer 2019, 19, 587–602. [Google Scholar] [CrossRef]
- Gong, N.; Sheppard, N.C.; Billingsley, M.M.; June, C.H.; Mitchell, M.J. Nanomaterials for T-Cell Cancer Immunotherapy. Nat. Nanotechnol. 2021, 16, 25–36. [Google Scholar] [CrossRef]
- Song, N.; Guo, H.; Ren, J.; Hao, S.; Wang, X. Synergistic Anti-Tumor Effects of Dasatinib and Dendritic Cell Vaccine on Metastatic Breast Cancer in a Mouse Model. Oncol. Lett. 2018, 15, 6831–6838. [Google Scholar] [CrossRef]
- Li, S.; Jiang, Q.; Liu, S.; Zhang, Y.; Tian, Y.; Song, C.; Wang, J.; Zou, Y.; Anderson, G.J.; Han, J.Y.; et al. A DNA Nanorobot Functions as a Cancer Therapeutic in Response to a Molecular Trigger in Vivo. Nat. Biotechnol. 2018, 36, 258–264. [Google Scholar] [CrossRef]
- Liu, S.; Jiang, Q.; Zhao, X.; Zhao, R.; Wang, Y.; Wang, Y.; Liu, J.; Shang, Y.; Zhao, S.; Wu, T.; et al. A DNA Nanodevice-Based Vaccine for Cancer Immunotherapy. Nat. Mater. 2021, 20, 421–430. [Google Scholar] [CrossRef]
- Zhang, P.; Meng, J.; Li, Y.; Yang, C.; Hou, Y.; Tang, W.; McHugh, K.J.; Jing, L. Nanotechnology-Enhanced Immunotherapy for Metastatic Cancer. Innovation 2021, 2, 100174. [Google Scholar] [CrossRef]
- Zhang, Y.; Lin, S.; Wang, X.-Y.; Zhu, G. Nanovaccines for Cancer Immunotherapy. WIREs Nanomed. Nanobiotechnol. 2019, 11, 139–148. [Google Scholar] [CrossRef]
- Fan, H.; Zhang, I.; Chen, X.; Zhang, L.; Wang, H.; Da Fonseca, A.; Manuel, E.R.; Diamond, D.J.; Raubitschek, A.; Badie, B. Intracerebral CpG Immunotherapy with Carbon Nanotubes Abrogates Growth of Subcutaneous Melanomas in Mice. Clin. Cancer Res. 2013, 18, 5628–5638. [Google Scholar] [CrossRef] [Green Version]
- Sun, Z.; Liu, Z.; Meng, J.; Meng, J.; Duan, J.; Xie, S.; Lu, X.; Zhu, Z.; Wang, C.; Chen, S.; et al. Carbon Nanotubes Enhance Cytotoxicity Mediated by Human Lymphocytes in Vitro. PLoS ONE 2011, 6, e21073. [Google Scholar] [CrossRef] [Green Version]
- Chen, T.; Guo, J.; Yang, M.; Zhu, X.; Cao, X. Chemokine-Containing Exosomes Are Released from Heat-Stressed Tumor Cells via Lipid Raft-Dependent Pathway and Act as Efficient Tumor Vaccine. J. Immunol. 2011, 186, 2219–2228. [Google Scholar] [CrossRef] [Green Version]
- Lin, A.Y.; Mattos Almeida, J.P.; Bear, A.; Liu, N.; Luo, L.; Foster, A.E.; Drezek, R.A. Gold Nanoparticle Delivery of Modified CpG Stimulates Macrophages and Inhibits Tumor Growth for Enhanced Immunotherapy. PLoS ONE 2013, 8, e63550. [Google Scholar] [CrossRef] [Green Version]
- Lee, I.H.; Kwon, H.K.; An, S.; Kim, D.; Kim, S.; Yu, M.K.; Lee, J.H.; Lee, T.S.; Im, S.H.; Jon, S. Imageable Antigen-Presenting Gold Nanoparticle Vaccines for Effective Cancer Immunotherapy in Vivo. Angew. Chemie-Int. Ed. 2012, 51, 8800–8805. [Google Scholar] [CrossRef]
- Kim, S.-Y.; Heo, M.B.; Hwang, G.-S.; Jung, Y.; Choi, D.Y.; Park, Y.-M.; Lim, Y.T. Multivalent Polymer Nanocomplex Targeting Endosomal Receptor of Immune Cells for Enhanced Antitumor and Systemic Memory Response. Angew. Chemie 2015, 127, 8257–8261. [Google Scholar] [CrossRef]
- Cho, N.H.; Cheong, T.C.; Min, J.H.; Wu, J.H.; Lee, S.J.; Kim, D.; Yang, J.S.; Kim, S.; Kim, Y.K.; Seong, S.Y. A Multifunctional Core-Shell Nanoparticle for Dendritic Cell-Based Cancer Immunotherapy. Nat. Nanotechnol. 2011, 6, 675–682. [Google Scholar] [CrossRef]
- Xu, Z.; Ramishetti, S.; Tseng, Y.C.; Guo, S.; Wang, Y.; Huang, L. Multifunctional Nanoparticles Co-Delivering Trp2 Peptide and CpG Adjuvant Induce Potent Cytotoxic T-Lymphocyte Response against Melanoma and Its Lung Metastasis. J. Control. Release 2013, 172, 259–265. [Google Scholar] [CrossRef]
- Luo, M.; Wang, H.; Wang, Z.; Cai, H.; Lu, Z.; Li, Y.; Du, M.; Huang, G.; Wang, C.; Chen, X.; et al. A STING-Activating Nanovaccine for Cancer Immunotherapy. Nat. Nanotechnol. 2017, 12, 648–654. [Google Scholar] [CrossRef]
- Wiederschain, D.; Chen, L.; Johnson, B.; Bettano, K.; Jackson, D.; Taraszka, J.; Wang, Y.K.; Jones, M.D.; Morrissey, M.; Deeds, J.; et al. Contribution of Polycomb Homologues Bmi-1 and Mel-18 to Medulloblastoma Pathogenesis. Mol. Cell. Biol. 2007, 27, 4968–4979. [Google Scholar] [CrossRef] [Green Version]
- Cui, Z.; Han, S.J.; Vangasseri, D.P.; Huang, L. Immunostimulation Mechanism of LPD Nanoparticle as a Vaccine Carrier. Mol. Pharm. 2005, 2, 22–28. [Google Scholar] [CrossRef]
- Nakamura, T.; Yamazaki, D.; Yamauchi, J.; Harashima, H. The Nanoparticulation by Octaarginine-Modified Liposome Improves α-Galactosylceramide-Mediated Antitumor Therapy via Systemic Administration. J. Control. Release 2013, 171, 216–224. [Google Scholar] [CrossRef] [Green Version]
- Hamdy, S.; Molavi, O.; Ma, Z.; Haddadi, A.; Alshamsan, A.; Gobti, Z.; Elhasi, S.; Samuel, J.; Lavasanifar, A. Co-Delivery of Cancer-Associated Antigen and Toll-like Receptor 4 Ligand in PLGA Nanoparticles Induces Potent CD8+ T Cell-Mediated Anti-Tumor Immunity. Vaccine 2008, 26, 5046–5057. [Google Scholar] [CrossRef]
- Thomas, S.N.; Vokali, E.; Lund, A.W.; Hubbell, J.A.; Swartz, M.A. Targeting the Tumor-Draining Lymph Node with Adjuvanted Nanoparticles Reshapes the Anti-Tumor Immune Response. Biomaterials 2014, 35, 814–824. [Google Scholar] [CrossRef] [Green Version]
- Choi, B.; Moon, H.; Hong, S.J.; Shin, C.; Do, Y.; Ryu, S.; Kang, S. Effective Delivery of Antigen-Encapsulin Nanoparticle Fusions to Dendritic Cells Leads to Antigen-Specific Cytotoxic T Cell Activation and Tumor Rejection. ACS Nano 2016, 10, 7339–7350. [Google Scholar] [CrossRef]
- Lizotte, P.H.; Wen, A.M.; Sheen, M.R.; Fields, J.; Rojanasopondist, P.; Steinmetz, N.F.; Fiering, S. In Situ Vaccination with Cowpea Mosaic Virus Nanoparticles Suppresses Metastatic Cancer. Nat. Nanotechnol. 2016, 11, 295–303. [Google Scholar] [CrossRef]
- Kageyama, S.; Kitano, S.; Hirayama, M.; Nagata, Y.; Imai, H.; Shiraishi, T.; Akiyoshi, K.; Scott, A.M.; Murphy, R.; Hoffman, E.W.; et al. Humoral Immune Responses in Patients Vaccinated with 1-146 HER2 Protein Complexed with Cholesteryl Pullulan Nanogel. Cancer Sci. 2008, 99, 601–607. [Google Scholar] [CrossRef]
- Kranz, L.M.; Diken, M.; Haas, H.; Kreiter, S.; Loquai, C.; Reuter, K.C.; Meng, M.; Fritz, D.; Vascotto, F.; Hefesha, H.; et al. Systemic RNA Delivery to Dendritic Cells Exploits Antiviral Defence for Cancer Immunotherapy. Nature 2016, 534, 396–401. [Google Scholar] [CrossRef]
- Goldinger, S.M.; Dummer, R.; Baumgaertner, P.; Mihic-Probst, D.; Schwarz, K.; Hammann-Haenni, A.; Willers, J.; Geldhof, C.; Prior, J.O.; Kündig, T.M.; et al. Nano-Particle Vaccination Combined with TLR-7 and -9 Ligands Triggers Memory and Effector CD8 + T-Cell Responses in Melanoma Patients. Eur. J. Immunol. 2012, 42, 3049–3061. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Speiser, D.E.; Schwarz, K.; Baumgaertner, P.; Manolova, V.; Devevre, E.; Sterry, W.; Walden, P.; Zippelius, A.; Conzett, K.B.; Senti, G.; et al. Memory and Effector CD8 T-Cell Responses after Nanoparticle Vaccination of Melanoma Patients. J. Immunother. 2010, 33, 848–858. [Google Scholar] [CrossRef] [PubMed]
- Escudier, B.; Dorval, T.; Chaput, N.; André, F.; Caby, M.P.; Novault, S.; Flament, C.; Leboulaire, C.; Borg, C.; Amigorena, S.; et al. Vaccination of Metastatic Melanoma Patients with Autologous Dendritic Cell (DC) Derived-Exosomes: Results of the First Phase 1 Clinical Trial. J. Transl. Med. 2005, 3, 1–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, L.-x.; Xie, X.-x.; Liu, D.-q.; Xu, Z.P.; Liu, R.-t. Efficient Co-Delivery of Neo-Epitopes Using Dispersion-Stable Layered Double Hydroxide Nanoparticles for Enhanced Melanoma Immunotherapy. Biomaterials 2018, 174, 54–66. [Google Scholar] [CrossRef]
- Foged, C.; Brodin, B.; Frokjaer, S.; Sundblad, A. Particle Size and Surface Charge Affect Particle Uptake by Human Dendritic Cells in an in Vitro Model. Int. J. Pharm. 2005, 298, 315–322. [Google Scholar] [CrossRef]
- Yoon, H.Y.; Selvan, S.T.; Yang, Y.; Kim, M.J.; Yi, D.K.; Kwon, I.C.; Kim, K. Engineering Nanoparticle Strategies for Effective Cancer Immunotherapy. Biomaterials 2018, 178, 597–607. [Google Scholar] [CrossRef]
- Noh, Y.W.; Kim, S.Y.; Kim, J.E.; Kim, S.; Ryu, J.; Kim, I.; Lee, E.; Um, S.H.; Lim, Y.T. Multifaceted Immunomodulatory Nanoliposomes: Reshaping Tumors into Vaccines for Enhanced Cancer Immunotherapy. Adv. Funct. Mater. 2017, 27, 1605398. [Google Scholar] [CrossRef]
- Jeanbart, L.; Swartz, M.A. Engineering Opportunities in Cancer Immunotherapy. Proc. Natl. Acad. Sci. USA 2015, 112, 14467–14472. [Google Scholar] [CrossRef] [Green Version]
- Pardoll, D.M. Spinning Molecular Immunology into Successful Immunotherapy. Nat. Rev. Immunol. 2002, 2, 227–238. [Google Scholar] [CrossRef]
- Patterson, S.L.; Maresso, K.C.; Hawk, E. Cancer Chemoprevention: Successes and Failures. Clin. Chem. 2013, 59, 94–101. [Google Scholar] [CrossRef] [Green Version]
- Vogel, V.G.; Costantino, J.P.; Wickerham, D.L.; Cronin, W.M.; Cecchini, R.S.; Atkins, J.N.; Bevers, T.B.; Fehrenbacher, L.; Pajon, E.R.; Wade, J.L.; et al. Effects of Tamoxifen vs Raloxifene on the Risk of Developing Invasive Breast Cancer and Other Disease Outcomes: The NSABP Study of Tamoxifen and Raloxifene (STAR) P-2 Trial. J. Am. Med. Assoc. 2006, 295, 2727–2741. [Google Scholar] [CrossRef] [Green Version]
- Fisher, B.; Costantino, J.P.; Wickerham, D.L.; Redmond, C.K.; Kavanah, M.; Cronin, W.M.; Vogel, V.; Robidoux, A.; Dimitrov, N.; Atkins, J.; et al. Tamoxifen for Prevention of Breast Cancer: Report of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J. Natl. Cancer Inst. 1998, 90, 1504. [Google Scholar] [CrossRef] [Green Version]
- Phillips, R.K.S.; Wallace, M.H.; Lynch, P.M.; Hawk, E.; Gordon, G.B.; Saunders, B.P.; Wakabayashi, N.; Shen, Y.; Zimmerman, S.; Godio, L.; et al. A Randomised, Double Blind, Placebo Controlled Study of Celecoxib, a Selective Cyclooxygenase 2 Inhibitor, on Duodenal Polyposis Familial Adenomatous Polyposis. Gut 2002, 50, 857–860. [Google Scholar] [CrossRef]
- Searle, G.D.; Anderson, T.M.D.; Miguel, A.; Jester, S.L.; King, K.L.; Schumacher, M.; Abbruzzese, J.; Raymond, N. The Effect of Celecoxib, a Cyclooxygenase-2 Inhibitor, in Familial Adenomatous Polyposis. N. Engl. J. Med. 2000, 1946–1952. [Google Scholar] [CrossRef]
- Steinberg, G.; Bahnson, R.; Brosman, S.; Middleton, R.; Wajsman, Z.; Wehle, M.; Auerbach, S.; Blute, M.; Bohnert, W.; Brendler, C.; et al. Efficacy and Safety of Valrubicin for the Treatment of Bacillus Calmette-Guerin Refractory Carcinoma in Situ of the Bladder. J. Urol. 2000, 163, 761–767. [Google Scholar] [CrossRef]
- Shankaran, V.; Ikeda, H.; Bruce, A.T.; White, J.M.; Swanson, P.E.; Old, L.J.; Shreiber, R.D. IFNgamma and Lympohcytes Prevent Primary Tomour Development and Shape Tomour Immunogenicity. Nature 2001, 410, 1107–1111. [Google Scholar] [CrossRef]
- Roeser, J.C.; Leach, S.D.; Mcallister, F. Emerging Strategies for Cancer Immunoprevention. Oncogene 2015, 34, 6029–6039. [Google Scholar] [CrossRef]
- O’Donnell, J.S.; Teng, M.W.L.; Smyth, M.J. Cancer Immunoediting and Resistance to T Cell-Based Immunotherapy. Nat. Rev. Clin. Oncol. 2019, 16, 151–167. [Google Scholar] [CrossRef]
- Finn, O.J.; Beatty, P.L. Cancer Immunoprevention. Curr. Opin. Immunol. 2016, 39, 52–58. [Google Scholar] [CrossRef] [Green Version]
- Mukherjee, P.; Pathangey, L.B.; Bradley, J.B.; Tinder, T.L.; Basu, G.D.; Akporiaye, E.T.; Gendler, S.J. MUC1-Specific Immune Therapy Generates a Strong Anti-Tumor Response in a MUC1-Tolerant Colon Cancer Model. Vaccine 2008, 25, 1607–1618. [Google Scholar] [CrossRef] [Green Version]
- Kimura, T.; McKolanis, J.R.; Dzubinski, L.A.; Islam, K.; Potter, D.M.; Salazar, A.M.; Schoen, R.E.; Finn, O.J. MUC1 Vaccine for Individuals with Advanced Adenoma of the Colon: A Cancer Immunoprevention Feasibility Study. Cancer Prev. Res. 2013, 6, 18–26. [Google Scholar] [CrossRef] [Green Version]
- De Vos Van Steenwijk, P.J.; Van Poelgeest, M.I.E.; Ramwadhdoebe, T.H.; Löwik, M.J.G.; Berends-Van Der Meer, D.M.A.; Van Der Minne, C.E.; Loof, N.M.; Stynenbosch, L.F.M.; Fathers, L.M.; Valentijn, A.R.P.M.; et al. The Long-Term Immune Response after HPV16 Peptide Vaccination in Women with Low-Grade Pre-Malignant Disorders of the Uterine Cervix: A Placebo-Controlled Phase II Study. Cancer Immunol. Immunother. 2014, 63, 147–160. [Google Scholar] [CrossRef]
- Chiang, C.L.-L.; Benencia, F.; Coukos, G.; Chiang, C.L.L.; Benencia, F.; Coukos, G. Whole Tumor Antigen Vaccines. Semin. Immunol. 2010, 22, 132–143. [Google Scholar] [CrossRef] [Green Version]
- Pandha, H.S.; John, R.J.; Hutchinson, J.; James, N.; Whelan, M.; Corbishley, C.; Dalgleish, A.G. Dendritic Cell Immunotherapy for Urological Cancers Using Cryopreserved Allogeneic Tumour Lysate-Pulsed Cells: A Phase I/II Study. BJU Int. 2004, 94, 412–418. [Google Scholar] [CrossRef]
- Kantoff, P.W.; Higano, C.S.; Shore, N.D.; Berger, E.R.; Small, E.J.; Penson, D.F.; Redfern, C.H.; Ferrari, A.C.; Dreicer, R.; Sims, R.B.; et al. Sipuleucel-T Immunotherapy for Castration-Resistant Prostate Cancer. J. N. Engl. Med. 2010, 363, 411–422. [Google Scholar] [CrossRef] [Green Version]
- Jorritsma, S.H.T.; Gowans, E.J.; Grubor-Bauk, B.; Wijesundara, D.K. Delivery Methods to Increase Cellular Uptake and Immunogenicity of DNA Vaccines. Vaccine 2016, 34, 5488–5494. [Google Scholar] [CrossRef]
- DiPaola, R.; Plante, M.; Kaufman, H.; Petrylak, D.; Israeli, R.; Lattime, E.; Manson, K.; Schuetz, T. A Phase I Trial of Pox PSA Vaccines (PROSTVAC®-VF) with B7-1, ICAM-1, and LFA-3 Co-Stimulatory Molecules (TRICOMTM) in Patients with Prostate Cancer. J. Transl. Med. 2006, 4, 1–10. [Google Scholar] [CrossRef]
- Farinati, F.; Cardin, R.; Bortolami, M.; Burra, P.; Russo, F.P.; Rugge, M.; Guido, M.; Sergio, A.; Naccarato, R. Hepatitis C Virus: From Oxygen Free Radicals to Hepatocellular Carcinoma. J. Viral Hepat. 2007, 14, 821–829. [Google Scholar] [CrossRef] [PubMed]
- Zur Hausen, H.; Schulte-holthausen, H.; Klein, G.; Henle, G.; Henle, W.; Clifford, P.; Santesson, L. Epstein-Barr Virus in Burkitt’s Lymphoma and Nasopharyngeal Carcinoma. [Ii] EBV DNA in Biopsies of Burkitt Tumours and Anaplastic Carcinomas of the Nasopharynx. Nat. Publ. Gr. 1970, 228, 1056–1058. [Google Scholar] [CrossRef]
- Yoshida, M.; Miyoshi, I.; Hinuma, Y. Isolation and Characterization of Retrovirus from Cell Lines of Human Adult T-Cell Leukemia and Its Implication in the Disease. Proc. Natl. Acad. Sci. USA 1982, 79, 2031–2035. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chang, Y.; Cesarman, E.; Pessin, M.S.; Lee, F.; Culpepper, J.; Knowles, M.; Moore, P.S. Identification of Herpesvirus-Like DNA Sequences in AIDS-Associated Kaposi’s Sarcoma. Adv. Sci. 2009, 266, 1865–1869. [Google Scholar] [CrossRef]
- Parsonnet, J.; Vandersteen, D.; Goates, J.; Sibley, R.K.; Pritikin, J.; Chang, Y. Helicobacter Pylori Infection in Intestinal- and Diffuse-Type Gastric Adenocarcinomas. J. Natl. Cancer Inst. 1991, 83, 640–643. [Google Scholar] [CrossRef]
- De Martel, C.; Ferlay, J.; Franceschi, S.; Vignat, J.; Bray, F.; Forman, D.; Plummer, M. Global Burden of Cancers Attributable to Infections in 2008: A Review and Synthetic Analysis. Lancet Oncol. 2012, 13, 607–615. [Google Scholar] [CrossRef]
- Schiller, J.; Castellsague, X.; Garland, S. A Review of Clinical Trials of Human Papillomavirus Prophylactic Vaccines. Vaccine 2012, 30, 1–42. [Google Scholar] [CrossRef] [Green Version]
- Trepo, C. A Brief History of Hepatitis Milestones. Liver Int. 2014, 34, 29–37. [Google Scholar] [CrossRef]
- Kao, J.H. Hepatitis B Vaccination and Prevention of Hepatocellular Carcinoma. Best Pract. Res. Clin. Gastroenterol. 2015, 29, 907–917. [Google Scholar] [CrossRef]
- Toh, Z.Q.; Licciardi, P.V.; Russell, F.M.; Garland, S.M.; Batmunkh, T.; Mulholland, E.K. Cervical Cancer Prevention through HPV Vaccination in Low- and Middle-Income Countries in Asia. Asian Pac. J. Cancer Prev. 2017, 18, 2339–2343. [Google Scholar] [CrossRef]
- Buck, C.B.; Day, P.M.; Trus, B.L. The Papillomavirus Major Capsid Protein L1. Virology 2013, 445, 169–174. [Google Scholar] [CrossRef] [Green Version]
- Drolet, M.; Bénard, É; Pérez, N.; Brisson, M. Population-Level Impact and Herd Effects Following the Introduction of Human Papillomavirus Vaccination Programmes: Updated Systematic Review and Meta-Analysis. Physiol. Behav. 2019, 176, 497–509. [Google Scholar] [CrossRef] [Green Version]
- Lei, J.; Ploner, A.; Elfström, K.M.; Wang, J.; Roth, A.; Fang, F.; Sundström, K.; Dillner, J.; Sparén, P. HPV Vaccination and the Risk of Invasive Cervical Cancer. N. Engl. J. Med. 2020, 383, 1340–1348. [Google Scholar] [CrossRef]
- Walker, C.M. Designing an HCV Vaccine: A Unique Convergence of Prevention and Therapy? Curr. Opin. Virol. 2017, 23, 113–119. [Google Scholar] [CrossRef] [Green Version]
- Zilberberg, J.; Feinman, R.; Korngold, R. Strategies for the Identification of T Cell-Recognized Tumor Antigens in Hematological Malignancies for Improved Graft-versus-Tumor Responses after Allogeneic Blood and Marrow Transplantation. Biol. Blood Marrow Transplant. 2015, 21, 1000–1007. [Google Scholar] [CrossRef] [Green Version]
- Feng, H.; Shuda, M.; Chang, Y.; Moore, P.S. Clonal Integration of a Polyomavirus in Human Merkel Cell Carcinoma. Science 2009, 319, 1096–1100. [Google Scholar] [CrossRef] [Green Version]
- Dalet, A.; Robbins, P.F.; Stroobant, V.; Vigneron, N.; Li, Y.F.; El-Gamil, M.; Hanada, K.I.; Yang, J.C.; Rosenberg, S.A.; Van Den Eyndea, B.J. An Antigenic Peptide Produced by Reverse Splicing and Double Asparagine Deamidation. Proc. Natl. Acad. Sci. USA 2011, 108, 323–331. [Google Scholar] [CrossRef] [Green Version]
- Chu, N.J.; Armstrong, T.D.; Jaffee, E.M. Nonviral Oncogenic Antigens and the Inflammatory Signals Driving Early Cancer Development as Targets for Cancer Immunoprevention. Clin. Cancer Res. 2015, 21, 1549–1557. [Google Scholar] [CrossRef] [Green Version]
- Traversari, C.; van der Bruggen, P.; Luescher, I.F.; Lurquin, C.; Chomez, P.; Van Pel, A.; De Plaen, E.; Amar-Costesec, A.; Boon, T. A Nonapeptide Encoded by Human Gene MAGE-1 Is Recognized on HLAA1 by Cytolytic t Lymphocytes Directed against Tumor Antigen MZ2-E. J. Exp. Med. 1992, 176, 1453–1457. [Google Scholar] [CrossRef] [Green Version]
- Hombrink, P.; Hassan, C.; Kester, M.G.D.; de Ru, A.H.; van Bergen, C.A.M.; Nijveen, H.; Drijfhout, J.W.; Falkenburg, J.H.F.; Heemskerk, M.H.M.; van Veelen, P.A. Discovery of T Cell Epitopes Implementing HLA-Peptidomics into a Reverse Immunology Approach. J. Immunol. 2013, 190, 3869–3877. [Google Scholar] [CrossRef]
- Popović, J.; Li, A.P.; Kloetzel, P.M.; Leisegang, M.; Uckert, W.; Blankenstein, T. The Only Proposed T-Cell Epitope Derived from the TEL-AML1 Translocation Is Not Naturally Processed. Blood 2011, 118, 946–954. [Google Scholar] [CrossRef]
- Engelhard, V.H.; Bullock, T.N.J.; Colella, T.A.; Sheasley, S.L.; Mullins, D.W. Antigens Derived from Melanocyte Differentiation Proteins: Self-Tolerance, Autoimmunity, and Use for Cancer Immunotherapy. Immunol. Rev. 2002, 188, 136–146. [Google Scholar] [CrossRef]
- Kessler, J.H.; Melief, C.J.M. Identification of T-Cell Epitopes for Cancer Immunotherapy. Leukemia 2007, 21, 1859–1874. [Google Scholar] [CrossRef]
- Khong, H.T.; Wang, Q.J.; Rosenberg, S.A. Identification of Multiple Antigens Recognized by Tumor-Infiltrating Lymphocytes from a Single Patient: Tumor Escape by Antigen Loss and Loss of MHC Expression. J. Immunother. 2004, 27, 184–190. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cavallo, F.; Calogero, R.A.; Forni, G. Are Oncoantigens Suitable Targets for Anti-Tumour Therapy? Nat. Rev. Cancer 2007, 7, 707–713. [Google Scholar] [CrossRef] [PubMed]
- Rolih, V.; Barutello, G.; Iussich, S.; De Maria, R.; Quaglino, E.; Buracco, P.; Cavallo, F.; Riccardo, F. CSPG4: A Prototype Oncoantigen for Translational Immunotherapy Studies. J. Transl. Med. 2017, 15, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Lollini, P.-L.; Nicoletti, G.; Landuzzi, L.; Cavallo, F.; Forni, G.; De Giovanni, C.; Nanni, P. Vaccines and Other Immunological Approaches for Cancer Immunoprevention. Curr. Drug Targets 2011, 12, 1957–1973. [Google Scholar] [CrossRef]
- Farkas, A.M.; Finn, O.J. Vaccines Based on Abnormal Self-Antigens as Tumor-Associated Antigens: Immune Regulation. Semin. Immunol. 2010, 22, 125–131. [Google Scholar] [CrossRef]
- Ieni, A.; Barresi, V.; Rigoli, L.; Caruso, R.A.; Tuccari, G. HER2 Status in Premalignant, Early, and Advanced Neoplastic Lesions of the Stomach. Dis. Markers 2015, 2015, 234851. [Google Scholar] [CrossRef] [Green Version]
- Al-Khayal, K.; Abdulla, M.; Al-Obaid, O.; Zubaidi, A.; Vaali-Mohammed, M.A.; Alsheikh, A.; Ahmad, R. Differential Expression of Mucins in Middle Eastern Patients with Colorectal Cancer. Oncol. Lett. 2016, 12, 393–400. [Google Scholar] [CrossRef]
- Chhieng, D.C.; Benson, E.; Eltoum, I.; Eloubeidi, M.A.; Jhala, N.; Jhala, D.; Siegal, G.P.; Grizzle, W.E.; Manne, U. MUC1 and MUC2 Expression in Pancreatic Ductal Carcinoma Obtained by Fine-Needle Aspiration. Cancer 2003, 99, 365–371. [Google Scholar] [CrossRef]
- Kesari, M.V.; Gaopande, V.L.; Joshi, A.R.; Babanagare, S.V.; Gogate, B.P.; Khadilkar, A.V. Immunohistochemical Study of MUC1, MUC2 and MUC5AC in Colorectal Carcinoma and Review of Literature. Indian J. Gastroenterol. 2015, 34, 63–67. [Google Scholar] [CrossRef]
- McGuckin, M.A.; Walsh, M.D.; Hohn, B.G.; Ward, B.G.; Wright, R.G. Prognostic Significance of Muc1 Epithelial Mucin Expression in Breast Cancer. Hum. Pathol. 1995, 26, 432–439. [Google Scholar] [CrossRef]
- Qu, C.F.; Li, Y.; Song, Y.J.; Rizvi, S.M.A.; Raja, C.; Zhang, D.; Samra, J.; Smith, R.; Perkins, A.C.; Apostolidis, C.; et al. MUC1 Expression in Primary and Metastatic Pancreatic Cancer Cells for in Vitro Treatment by 213Bi-C595 Radioimmunoconjugate. Br. J. Cancer 2004, 91, 2086–2093. [Google Scholar] [CrossRef] [Green Version]
- Rakha, E.A.; Boyce, R.W.G.; El-Rehim, D.A.; Kurien, T.; Green, A.R.; Paish, E.C.; Robertson, J.F.R.; Ellis, I.O. Expression of Mucins (MUC1, MUC2, MUC3, MUC4, MUC5AC and MUC6) and Their Prognostic Significance in Human Breast Cancer. Mod. Pathol. 2005, 18, 1295–1304. [Google Scholar] [CrossRef] [Green Version]
- Molaei, M.; Mansoori, B.K.; Mashayekhi, R.; Vahedi, M.; Pourhoseingholi, M.A.; Fatemi, S.R.; Zali, M.R. Mucins in Neoplastic Spectrum of Colorectal Polyps: Can They Provide Predictions? BMC Cancer 2010, 10, 537. [Google Scholar] [CrossRef] [Green Version]
- Maitra, A.; Adsay, N.V.; Argani, P.; Iacobuzio-Donahue, C.; De Marzo, A.; Cameron, J.L.; Yeo, C.J.; Hruban, R.H. Multicomponent Analysis of the Pancreatic Adenocarcinoma Progression Model Using a Pancreatic Intraepithelial Neoplasia Tissue Microarray. Mod. Pathol. 2003, 16, 902–912. [Google Scholar] [CrossRef] [Green Version]
- Hammarstrom, S. The Carcinoembryonic Antigen CEA Family: Structures, Suggested Functions and Expression in Normal and Malignant Tissues. Cancer Biol. 1999, 9, 67–81. [Google Scholar] [CrossRef]
- Buie, W.D.; Attard, J.A.P. Follow-up Recommendations for Colon Cancer. Clin. Colon Rectal Surg. 2005, 18, 232–243. [Google Scholar] [CrossRef] [Green Version]
- Schiemann, U.; Günther, S.; Gross, M.; Henke, G.; Müller-Koch, Y.; König, A.; Muders, M.; Folwaczny, C.; Mussack, T.; Holinski-Feder, E. Preoperative Serum Levels of the Carcinoembryonic Antigen in Hereditary Non-Polyposis Colorectal Cancer Compared to Levels in Sporadic Colorectal Cancer. Cancer Detect. Prev. 2005, 29, 356–360. [Google Scholar] [CrossRef]
- Javan, S.; Andalib, A.; Bereshneh, A.H.; Emami, M.H.; Salehi, R.; Karami, F. Frequent Novel Variations within Msh2 and Mlh1 Genes in a Subset of Iranian Families with Hereditary Non-Polyposis Colorectal Cancer. Acta Med. Iran. 2019, 57, 147–151. [Google Scholar] [CrossRef]
- Park, K.; Han, S.; Kim, H.J.; Kim, J.; Shin, E. HER2 Status in Pure Ductal Carcinoma in Situ and in the Intraductal and Invasive Components of Invasive Ductal Carcinoma Determined by Fluorescence in Situ Hybridization and Immunohistochemistry. Histopathology 2006, 48, 702–707. [Google Scholar] [CrossRef]
- Slamon, D.J.; Clark, G.M.; Wong, S.G.; Levin, W.J.; Ullrich, A.; McGuire, W.L. Human Breast Cancer: Correlation of Relapse and Survival with Amplification of the HER-2/Neu Oncogene. Science 1987, 235, 182–191. [Google Scholar] [CrossRef] [Green Version]
- Roozeboom, M.H.; Arits, A.H.H.M.; Nelemans, P.J.; Kelleners-Smeets, N.W.J. Overall Treatment Success after Treatment of Primary Superficial Basal Cell Carcinoma: A Systematic Review and Meta-Analysis of Randomized and Nonrandomized Trials. Br. J. Dermatol. 2012, 167, 733–756. [Google Scholar] [CrossRef]
- Bhatia, S.; Tykodi, S.S.; Thompson, J.A. Treatment of Metastatic Melanoma: An Overview. Oncology 2009, 23, 488–496. [Google Scholar]
- Lamm, D.L.; Riggs, D.R. Immunotherapy of Superficial Bladder Cancer. Clin. Immunother. 1994, 2, 331–341. [Google Scholar] [CrossRef]
- Quist, S.R.; Gollnick, H.P. Imiquimod 3.75% Cream (Zyclara) for the Treatment of Actinic Keratoses. J. Am. Acad. Dermatol. 2000, 42, 451–461. [Google Scholar] [CrossRef]
- Nooka, A.K.; Wang, M.L.; Yee, A.J.; Kaufman, J.L.; Bae, J.; Peterkin, D.; Richardson, P.G.; Raje, N.S. Assessment of Safety and Immunogenicity of PVX-410 Vaccine With or Without Lenalidomide in Patients With Smoldering Multiple Myeloma: A Nonrandomized Clinical Trial. JAMA Oncol. 2018, 4, 1–5. [Google Scholar] [CrossRef]
- Corral, L.G.; Haslett, P.A.J.; Muller, G.W.; Chen, R.; Wong, L.M.; Ocampo, C.J.; Patterson, R.T.; Stirling, D.I.; Kaplan, G. Differential Cytokine Modulation and T Cell Activation by Two Distinct Classes of Thalidomide Analogues That Are Potent Inhibitors of TNF-Alpha. J. Immunol. 1999, 163, 380–386. [Google Scholar]
- Kotla, V.; Goel, S.; Nischal, S.; Heuck, C.; Vivek, K.; Das, B.; Verma, A. Mechanism of Action of Lenalidomide in Hematological Malignancies. J. Hematol. Oncol. 2009, 2, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Hemmi, H.; Kaisho, T.; Takeuchi, O.; Sato, S.; Sanjo, H.; Hoshino, K.; Horiuchi, T.; Tomizawa, H.; Takeda, K.; Akira, S. Small-Antiviral Compounds Activate Immune Cells via the TLR7 MyD88-Dependent Signaling Pathway. Nat. Immunol. 2002, 3, 196–200. [Google Scholar] [CrossRef]
- Miller, R.L.; Gerster, J.F.; Owens, M.L.; Slade, H.B.; Tomai, M.A. Imiquimod Applied Topically: A Novel Immune Response Modifier and New Class of Drug. Int. J. Immunopharmacol. 1999, 21, 1–14. [Google Scholar] [CrossRef]
- Keshavarz-Fathi, M.; Rezaei, N. Cancer Immunoprevention: Current Status and Future Directions. Arch. Immunol. Ther. Exp. 2021, 69, 1–19. [Google Scholar] [CrossRef]
- Dave, K.; Ali, A.; Magalhaes, M. Increased Expression of PD-1 and PD-L1 in Oral Lesions Progressing to Oral Squamous Cell Carcinoma: A Pilot Study. Sci. Rep. 2020, 10, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Yagyuu, T.; Hatakeyama, K.; Imada, M.; Kurihara, M.; Matsusue, Y.; Yamamoto, K.; Obayashi, C.; Kirita, T. Programmed Death Ligand 1 (PD-L1) Expression and Tumor Microenvironment: Implications for Patients with Oral Precancerous Lesions. Oral Oncol. 2017, 68, 36–43. [Google Scholar] [CrossRef] [PubMed]
- Dhodapkar, M.V.; Sexton, R.; Das, R.; Dhodapkar, K.M.; Zhang, L.; Sundaram, R.; Soni, S.; Crowley, J.J.; Orlowski, R.Z.; Barlogie, B. Prospective Analysis of Antigen-Specific Immunity, Stem-Cell Antigens, and Immune Checkpoints in Monoclonal Gammopathy. Blood 2015, 126, 2475–2478. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, J.; Xie, T.; Wang, B.; William, W.N., Jr.; Heymach, J.V.; El-Naggar, A.K.; Myers, J.N.; Caulin, C. PD-1 Blockade Prevents the Development and Progression of Carcinogen-Induced Oral Premalignant Lesions. Rev. Col. Am. Cardiol. 2017, 72, 2964–2979. [Google Scholar] [CrossRef] [Green Version]
- Zhang, D.; Lin, Z.; Wu, M.; Cai, Z.; Zheng, Y.; He, L.; Li, Z.; Zhou, J.; Sun, L.; Chen, G.; et al. Cytosolic Delivery of Thiolated Neoantigen Nano-Vaccine Combined with Immune Checkpoint Blockade to Boost Anti-Cancer T Cell Immunity. Adv. Sci. 2021, 8, 1–12. [Google Scholar] [CrossRef]
- Nair, H.B.; Sung, B.; Yadav, V.R.; Kannappan, R.; Chaturvedi, M.M.; Aggarwal, B.B. Delivery of Anti-Inflammatory Nutraceuticals by Nanoparticles for the Prevention and Treatment of Cancer. Biochem. Pharmacol. 2011, 80, 1833–1843. [Google Scholar] [CrossRef] [Green Version]
- Zhang1, M.; Viennois, E.; Prasad, M.; Zhang, Y.; Wang, L.; Zhang, Z.; Han, M.K.; Xiao, B.; Xu, C.; Srinivasan, S.; et al. Edible Ginger-Derived Nanoparticles: A Novel Therapeutic Approach for the Prevention and Treatment of Inflammatory Bowel Disease and Colitis-Associated Cancer Mingzhen. Physiol. Behav. 2016, 176, 139–148. [Google Scholar] [CrossRef] [Green Version]
- Xu, Z.; Wang, Y.; Zhang, L.; Huang, L. Nanoparticle-Delivered Transforming Growth Factor-β SiRNA Enhances Vaccination against Advanced Melanoma by Modifying Tumor Microenvironment. ACS Nano 2014, 8, 3636–3645. [Google Scholar] [CrossRef]
- Milicic, A.; Kaur, R.; Reyes-Sandoval, A.; Tang, C.K.; Honeycutt, J.; Perrie, Y.; Hill, A.V.S. Small Cationic DDA:TDB Liposomes as Protein Vaccine Adjuvants Obviate the Need for Tlr Agonists in Inducing Cellular and Humoral Responses. PLoS ONE 2012, 7, 1–10. [Google Scholar] [CrossRef]
- Bal, S.M.; Hortensius, S.; Ding, Z.; Jiskoot, W.; Bouwstra, J.A. Co-Encapsulation of Antigen and Toll-like Receptor Ligand in Cationic Liposomes Affects the Quality of the Immune Response in Mice after Intradermal Vaccination. Vaccine 2011, 29, 1045–1052. [Google Scholar] [CrossRef] [Green Version]
- Park, J.; Wrzesinski, S.H.; Stern, E.; Look, M.; Criscione, J.; Ragheb, R.; Jay, S.M.; Demento, S.L.; Agawu, A.; Licona Limon, P.; et al. Combination Delivery of TGF-β Inhibitor and IL-2 by Nanoscale Liposomal Polymeric Gels Enhances Tumour Immunotherapy. Nat. Mater. 2012, 11, 895–905. [Google Scholar] [CrossRef]
- Wilson, J.T.; Keller, S.; Manganiello, M.J.; Cheng, C.; Lee, C.C.; Opara, C.; Convertine, A.; Stayton, P.S. PH-Responsive Nanoparticle Vaccines for Dual-Delivery of Antigens and Immunostimulatory Oligonucleotides. ACS Nano 2013, 7, 3912–3925. [Google Scholar] [CrossRef]
- Macho-Fernandez, E.; Cruz, L.J.; Ghinnagow, R.; Fontaine, J.; Bialecki, E.; Frisch, B.; Trottein, F.; Faveeuw, C. Targeted Delivery of α-Galactosylceramide to CD8α + Dendritic Cells Optimizes Type I NKT Cell–Based Antitumor Responses. J. Immunol. 2014, 193, 961–969. [Google Scholar] [CrossRef] [Green Version]
- Falo, L.D.; Kovacsovics-Bankowski, M.; Thompson, K.; Rock, K.L. Targeting Antigen into the Phagocytic Pathway in Vivo Induces Protective Tumour Immunity. Nat. Med. 1995, 1, 649–653. [Google Scholar] [CrossRef]
- Fifis, T.; Gamvrellis, A.; Crimeen-Irwin, B.; Pietersz, G.A.; Li, J.; Mottram, P.L.; McKenzie, I.F.C.; Plebanski, M. Size-Dependent Immunogenicity: Therapeutic and Protective Properties of Nano-Vaccines against Tumors. J. Immunol. 2004, 173, 3148–3154. [Google Scholar] [CrossRef] [Green Version]
- Uto, T.; Wang, X.; Sato, K.; Haraguchi, M.; Akagi, T.; Akashi, M.; Baba, M. Targeting of Antigen to Dendritic Cells with Poly(γ-Glutamic Acid) Nanoparticles Induces Antigen-Specific Humoral and Cellular Immunity. J. Immunol. 2007, 178, 2979–2986. [Google Scholar] [CrossRef] [Green Version]
- Fang, R.H.; Hu, C.M.J.; Luk, B.T.; Gao, W.; Copp, J.A.; Tai, Y.; O’Connor, D.E.; Zhang, L. Cancer Cell Membrane-Coated Nanoparticles for Anticancer Vaccination and Drug Delivery. Nano Lett. 2014, 14, 2181–2188. [Google Scholar] [CrossRef]
- Oelke, M.; Maus, M.V.; Didiano, D.; June, C.H.; Mackensen, A.; Schneck, J.P. Ex Vivo Induction and Expansion of Antigen-Specific Cytotoxic T Cells by HLA-Ig-Coated Artificial Antigen-Presenting Cells. Nat. Med. 2003, 9, 619–624. [Google Scholar] [CrossRef]
- Shen, C.; Cheng, K.; Miao, S.; Wang, W.; He, Y.; Meng, F.; Zhang, J. Latex Bead-Based Artificial Antigen-Presenting Cells Induce Tumor-Specific CTL Responses in the Native T-Cell Repertoires and Inhibit Tumor Growth. Immunol. Lett. 2013, 150, 1–11. [Google Scholar] [CrossRef]
- Perica, K.; De León Medero, A.; Durai, M.; Chiu, Y.L.; Bieler, J.G.; Sibener, L.; Niemöller, M.; Assenmacher, M.; Richter, A.; Edidin, M.; et al. Nanoscale Artificial Antigen Presenting Cells for T Cell Immunotherapy. Nanomedicine 2014, 23, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Ugel, S.; Zoso, A.; De Santo, C.; Li, Y.; Marigo, I.; Scarselli, E.; Cipriani, B.; Oelke, M.; Jonathan, P.; Bronte, V. In Vivo Administration of Artificial Antigen Presenting Cells Activates Low Avidity T Cells for Treatment of Cancer. Cancer Res. 2010, 69, 9376–9384. [Google Scholar] [CrossRef] [Green Version]
- Yazdi, M.H.; Mahdavi, M.; Kheradmand, E.; Shahverdi, A.R. The Preventive Oral Supplementation of a Selenium Nanoparticle-Enriched Probiotic Increases the Immune Response and Lifespan of 4T1 Breast Cancer Bearing Mice. Arzneimittel-Forschung/Drug Res. 2012, 62, 525–531. [Google Scholar] [CrossRef]
- Zhang, Z.; Tongchusak, S.; Mizukami, Y.; Kang, Y.J.; Ioji, T.; Touma, M.; Reinhold, B.; Keskin, D.B.; Reinherz, E.L.; Sasada, T. Induction of Anti-Tumor Cytotoxic T Cell Responses through PLGA-Nanoparticle Mediated Antigen Delivery. Biomaterials 2011, 32, 3666–3678. [Google Scholar] [CrossRef]
- Yu, X.; Gao, D.; Gao, L.; Lai, J.; Zhang, C.; Zhao, Y.; Zhong, L.; Jia, B.; Wang, F.; Chen, X.; et al. Inhibiting Metastasis and Preventing Tumor Relapse by Triggering Host Immunity with Tumor-Targeted Photodynamic Therapy Using Photosensitizer-Loaded Functional Nanographenes. ACS Nano 2017, 11, 10147–10158. [Google Scholar] [CrossRef]
- Pan, J.; Zhang, Q.; Palen, K.; Wang, L.; Qiao, L.; Johnson, B.; Sei, S.; Shoemaker, R.H.; Lubet, R.A.; Wang, Y.; et al. Potentiation of Kras Peptide Cancer Vaccine by Avasimibe, a Cholesterol Modulator. EBioMedicine 2019, 49, 72–81. [Google Scholar] [CrossRef] [Green Version]
- Liu, J.; Miao, L.; Sui, J.; Hao, Y.; Huang, G. Nanoparticle Cancer Vaccines: Design Considerations and Recent Advances. Asian J. Pharm. Sci. 2020, 15, 576–590. [Google Scholar] [CrossRef]
- Khoobchandani, M.; Khan, A.; Katti, K.K.; Thipe, V.C.; Al-Yasiri, A.Y.; MohanDoss, D.K.D.; Nicholl, M.B.; Lugão, A.B.; Hans, C.P.; Katti, K.V. Green Nanotechnology of MGF-AuNPs for Immunomodulatory Intervention in Prostate Cancer Therapy. Sci. Rep. 2021, 11, 1–30. [Google Scholar] [CrossRef]
- Hess, P.R.; Boczkowski, D.; Nair, S.K.; Snyder, D.; Gilboa, E. Vaccination with MRNAs Encoding Tumor-Associated Antigens and Granulocyte-Macrophage Colony-Stimulating Factor Efficiently Primes CTL Responses, but Is Insufficient to Overcome Tolerance to a Model Tumor/Self Antigen. Cancer Immunol. Immunother. 2006, 55, 672–683. [Google Scholar] [CrossRef]
- Mockey, M.; Bourseau, E.; Chandrashekhar, V.; Chaudhuri, A.; Lafosse, S.; Le Cam, E.; Quesniaux, V.F.J.; Ryffel, B.; Pichon, C.; Midoux, P. MRNA-Based Cancer Vaccine: Prevention of B16 Melanoma Progression and Metastasis by Systemic Injection of MART1 MRNA Histidylated Lipopolyplexes. Cancer Gene Ther. 2007, 14, 802–814. [Google Scholar] [CrossRef] [PubMed]
- Oberli, M.A.; Reichmuth, A.M.; Dorkin, J.R.; Mitchell, M.J.; Fenton, O.S.; Jaklenec, A.; Anderson, D.G.; Langer, R.; Blankschtein, D. Lipid Nanoparticle Assisted MRNA Delivery for Potent Cancer Immunotherapy. Nano Lett. 2017, 17, 1326–1335. [Google Scholar] [CrossRef] [PubMed]
- Perche, F.; Benvegnu, T.; Berchel, M.; Lebegue, L.; Pichon, C.; Jaffrès, P.A.; Midoux, P. Enhancement of Dendritic Cells Transfection in Vivo and of Vaccination against B16F10 Melanoma with Mannosylated Histidylated Lipopolyplexes Loaded with Tumor Antigen Messenger RNA. Nanomed. Nanotechnol. Biol. Med. 2011, 7, 445–453. [Google Scholar] [CrossRef] [PubMed]
- Pollard, C.; Rejman, J.; De Haes, W.; Verrier, B.; Van Gulck, E.; Naessens, T.; De Smedt, S.; Bogaert, P.; Grooten, J.; Vanham, G.; et al. Type i IFN Counteracts the Induction of Antigen-Specific Immune Responses by Lipid-Based Delivery of MRNA Vaccines. Mol. Ther. 2013, 21, 251–259. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yuba, E.; Harada, A.; Sakanishi, Y.; Watarai, S.; Kono, K. A Liposome-Based Antigen Delivery System Using PH-Sensitive Fusogenic Polymers for Cancer Immunotherapy. Biomaterials 2013, 34, 3042–3052. [Google Scholar] [CrossRef] [PubMed]
- Almeida, J.P.M.; Lin, A.Y.; Figueroa, E.R.; Foster, A.E.; Drezek, R.A. In Vivo Gold Nanoparticle Delivery of Peptide Vaccine Induces Anti-Tumor Immune Response in Prophylactic and Therapeutic Tumor Models. Small 2015, 11, 1453–1459. [Google Scholar] [CrossRef] [Green Version]
- Tao, Y.; Ju, E.; Li, Z.; Ren, J.; Qu, X. Engineered CpG-Antigen Conjugates Protected Gold Nanoclusters as Smart Self-Vaccines for Enhanced Immune Response and Cell Imaging. Adv. Funct. Mater. 2014, 24, 1004–1010. [Google Scholar] [CrossRef]
- Zhang, P.; Chiu, Y.C.; Tostanoski, L.H.; Jewell, C.M. Polyelectrolyte Multilayers Assembled Entirely from Immune Signals on Gold Nanoparticle Templates Promote Antigen-Specific T Cell Response. ACS Nano 2015, 9, 6465–6477. [Google Scholar] [CrossRef] [Green Version]
- Xiang, J.; Xu, L.; Gong, H.; Zhu, W.; Wang, C.; Xu, J.; Feng, L.; Cheng, L.; Peng, R.; Liu, Z. Antigen-Loaded Upconversion Nanoparticles for Dendritic Cell Stimulation, Tracking, and Vaccination in Dendritic Cell-Based Immunotherapy. ACS Nano 2015, 9, 6401–6411. [Google Scholar] [CrossRef]
- Li, X.; Aldayel, A.M.; Cui*, Z. Aluminum Hydroxide Nanoparticles Show a Stronger Vaccine Adjuvant Activity than Traditional Aluminum Hydroxide Microparticles. J. Control. Release 2014, 173, 148–157. [Google Scholar] [CrossRef] [Green Version]
- Koppolu, B.; Zaharoff, D.A. The Effect of Antigen Encapsulation in Chitosan Particles on Uptake, Activation and Presentation by Antigen Presenting Cells. Biomaterials 2013, 34, 2359–2369. [Google Scholar] [CrossRef]
- Kurosaki, T.; Kitahara, T.; Nakamura, T.; Nishida, K.; Fumoto, S.; Kodama, Y.; Nakagawa, H.; Higuchi, N.; Sasaki, H. Development of Effective Cancer Vaccine Using Targeting System of Antigen Protein to APCs. Pharm. Res. 2012, 29, 483–489. [Google Scholar] [CrossRef] [Green Version]
- Meleshko, A.N.; Petrovskaya, N.A.; Savelyeva, N.; Vashkevich, K.P.; Doronina, S.N.; Sachivko, N.V. Phase I Clinical Trial of Idiotypic DNA Vaccine Administered as a Complex with Polyethylenimine to Patients with B-Cell Lymphoma. Hum. Vaccines Immunother. 2017, 13, 1398–1403. [Google Scholar] [CrossRef] [Green Version]
- Khlebtsov, N.; Dykmana, L. Biodistribution and Toxicity of Engineered Gold Nanoparticles: A Review of in Vitro and in Vivo Studies. Chem. Soc. Rev. 2011, 40, 1647–1671. [Google Scholar] [CrossRef]
- Tsai, S.J.; Amerman, A.; Jewell, C.M. Altering Antigen Charge to Control Self-Assembly and Processing of Immune Signals During Cancer Vaccination. Front. Immunol. 2021, 11, 1–14. [Google Scholar] [CrossRef]
- Heuts, J.; Jiskoot, W.; Ossendorp, F.; Maaden, K. Cationic nanoparticle-based cancer vaccines. Pharmaceutics 2021, 13, 596. [Google Scholar] [CrossRef]
- Emran, T.B.; Shahriar, A.; Mahmud, A.R.; Rahman, T.; Abir, M.H.; Siddiquee, M.F.-R.; Ahmed, H.; Rahman, N.; Nainu, F.; Wahyudin, E.; et al. Multidrug Resistance in Cancer: Understanding Molecular Mechanisms, Immunoprevention and Therapeutic Approaches. Front. Oncol. 2022, 12, 1–38. [Google Scholar] [CrossRef]
- Smith, A.A.A.; Gale, E.C.; Roth, G.A.; Maikawa, C.L.; Correa, S.; Yu, A.C.; Appel, E.A. Nanoparticles Presenting Potent TLR7/8 Agonists Enhance Anti-PD-L1 Immunotherapy in Cancer Treatment. Biomacromolecules 2020, 21, 3704–3712. [Google Scholar] [CrossRef]
- Chen, J.; Qiu, M.; Ye, Z.; Nyalile, T.; Li, Y.; Glass, Z.; Zhao, X.; Yang, L.; Chen, J.; Xu, Q. In Situ Cancer Vaccination Using Lipidoid Nanoparticles. Sci. Adv. 2021, 7, 1–14. [Google Scholar] [CrossRef]
- Minigo, G.; Scholzen, A.; Tang, C.K.; Hanley, J.C.; Kalkanidis, M.; Pietersz, G.A.; Apostolopoulos, V.; Plebanski, M. Poly-l-Lysine-Coated Nanoparticles: A Potent Delivery System to Enhance DNA Vaccine Efficacy. Vaccine 2007, 25, 1316–1327. [Google Scholar] [CrossRef]
- Demuth, P.C.; Min, Y.; Huang, B.; Kramer, J.A.; Miller, A.D.; Barouch, D.H.; Hammond, P.T.; Irvine, D.J. Polymer Multilayer Tattooing for Enhanced DNA Vaccination. Nat. Mater. 2013, 12, 367–376. [Google Scholar] [CrossRef]
- Liu, Z.; Lv, D.; Liu, S.; Gong, J.; Wang, D.; Xiong, M.; Chen, X.; Xiang, R.; Tan, X. Alginic Acid-Coated Chitosan Nanoparticles Loaded with Legumain DNA Vaccine: Effect against Breast Cancer in Mice. PLoS ONE 2013, 8, e60190. [Google Scholar] [CrossRef] [Green Version]
- Ma, Y.F.; Yang, Y.W. Delivery of DNA-Based Cancer Vaccine with Polyethylenimine. Eur. J. Pharm. Sci. 2010, 40, 75–83. [Google Scholar] [CrossRef]
- Loomans-Kropp, H.A.; Umar, A. Cancer Prevention and Screening: The next Step in the Era of Precision Medicine. NPJ Precis. Oncol. 2019, 3, 3. [Google Scholar] [CrossRef] [Green Version]
- Uleberg, K.-E.; Øvestad, I.T.; Munk, A.C.; Brede, C.; van Diermen, B.; Gudlaugsson, E.; Janssen, E.A.M.; Hjelle, A.; Baak, J.P.A. Prediction of Spontaneous Regression of Cervical Intraepithelial Neoplasia Lesions Grades 2 and 3 by Proteomic Analysis. Int. J. Proteom. 2014, 2014, 129064. [Google Scholar] [CrossRef]



| Characteristics | Premalignant Lesions | Malignant Tumors |
|---|---|---|
| Genetic abnormalities | Few | Many |
| Apoptosis | Partially effective | Ineffective |
| Tumor suppressive genes | Partially active | Inactive |
| Cell proliferation | Normal | Increased |
| Stem and progenitor cells | Semi-increased | Increased population |
| Invasion status | Noninvasive lesion | Invasive |
| Basement membrane | Intact | Breached and disorganized |
| Cell morphology | Dysplasia: similar to the tissue of tumor origin | Anaplasia: revert to undifferentiated form |
| Neovascularization | Normal | Increased |
| Nanoparticle | Active Agent | Delivery Method | Cancer Type | Effect/Inference | Clinical Trial Status | References |
|---|---|---|---|---|---|---|
| CNT-CpG | CpG ODN | i.tm. | Subcutaneous Melanomas | Eradicated glioma and increased tumor immunity | Pre-clinical (in vivo study) | [73] |
| CNT | Tumor lysate | Human NSCLC | Promoted lymphocyte mediated cytotoxicity by NF-ΚB | Pre-clinical (in vitro study) | [74] | |
| HS-TEX | Chemokines (CCL2, CCL3, CCL4, CCL5, and CCL20) | i.tm. | Lung and skin cancer | Increased activation of T cell and dendritic cells | Pre-clinical (in vivo study) | [75] |
| AuNPs | CpG ODN | i.tm. | B16 melanoma | Promoted macrophage and dendritic cell invasion into tumor, inhibited tumor growth and increased survival. | Pre-clinical (in vivo studies) | [76,77] |
| Hyaluronic acid | CpG ODN | i.tm. | Lymphoma | Enhanced anti-tumor activity and immune memory | Pre-clinical (in vivo study) | [78] |
| Iron Oxide NPs | CpG ODN | i.p. | Colon cancer | Increased t cell responses and decreased tumor growth | Pre-clinical (in vivo study) | [79] |
| Liposomes | Trp2 peptide | i.v. | B16 melanoma and lung metastasis | Enhance T cell responses | Pre-clinical (in vivo study) | [80] |
| Polymeric NPs (PC7A NP) | Ovalbumin | i.v. | Melanoma, lung, and colon tumor | Improved delivery of tumor antigen, increased surface presentation and inhibited tumor growth | Pre-clinical (in vivo study) | [81] |
| Oligonucleotide Nanoring | Anti-Bmi1 and anti-Mel 18 shRNA with CpG ODN | i.tm. | Medulloblastoma | Inhibited tumor proliferation and growth | Pre-clinical (in vivo study) | [82] |
| Liposomes | E7 peptide | s.c. | Lung cancer | Activate antigen presenting cells and stimulate DCs | Pre-clinical (in vivo study) | [83] |
| R8-Lip | α-galactosylceramide | i.v. | Lung cancer and malignant B16 melanoma | Activated NK cells and increased anti-tumor immune reesponse | Pre-clinical (in vivo study) | [84] |
| PLGA-NPs | TRP2180-188 and 7-acyl lipid A | s.c. | B16 Melanoma | Induced interferon secretion, activated T cell responses, and decreased tumor size. | Pre-clinical (in vivo study) | [85] |
| Polymeric NPs | CpG ODN | i.d. | B16 Melanoma | Activated DCs and inhibited tumor growth | Pre-clinical (in vivo study) | [86] |
| Protein cage NPs | Ovalbumin | i.v. | B16 Melanoma | Activated cytotoxic T cells and suppressed tumor growth | Pre-clinical (in vivo study) | [87] |
| Cowpea mosaic virus nanoparticles | i.t. | Melanoma, colon, breast, lung and ovarian cancer | Prevented lung melanoma and generated anti-tumor immunity | Pre-clinical (in vivo study) | [88] | |
| CHP nanogel | Truncated 146HER2 protein | s.c. | HER2 expressing tumor patients | Induced HER2-specific humoral responses in patients with HER2-expressing tumors | Phase I | [89] |
| Liposomes | RNA encoding tumor antigens | i.v. | Melanoma | Induced effector and memory T cell responses, caused INF-α release from macrophages, | Phase I | [90] |
| Virus-like NPs (MelQbG10) | Melan-A/MART-1 Peptides with Montanide and Imiquimod | i.ln | Melanoma (Stage III-IV) | Enhanced memory and effector CD8+ T-cell responses | Phase IIa | [91] |
| Virus-like NPs | Melan-A/MART-1 Peptides | i.d | Melanoma (Stage II-IV) | Increased antigen presentation to DC cells and enhanced T cell responses | Phase IIa | [92] |
| Exosomes | MAGE 3 peptides | i.d. | Melanoma (Stage III-IV) | Promoted tumor rejection and increased T cell responses | Phase II | [93] |
| Nanoparticle | Active Agent | Delivery Method | Cancer Type | Effect/Inference | Clinical Trial Status | References |
|---|---|---|---|---|---|---|
| Iron oxide beads | Ovalbumin | s.c. | B16 Melanoma | Induced CD8 dependent protective immunity in vivo | Pre-clinical (in vivo study) | [184] |
| Polystyrene microspheres | Ovalbumin | s.c. | T cell Lymphoma | Protected against tumor growth and treated existing tumors | Pre-clinical (in vivo study) | [185] |
| LPH-NPs | TGF-β si-RNA | i.v. | Melanoma | Knockdown of TGF-β and inhibited tumor growth by 52%. Increased activity of cytotoxic T cell and decreased level of T regs cells | Pre-clinical (in vivo study) | [178] |
| Iron oxide-zinc oxide NPs | CEA | i.v. | colon adenocarcinoma | Enhanced T cell responses, reduced tumor growth and better survival | Pre-clinical (in vivo study) | [79] |
| γ-PGA NPs | Ovalbumin | Nasal | Induced antigen specific cellular and humoral immunity | Pre-clinical (in vivo study) | [186] | |
| Liposomes | CpG-ODN | i.m. | B-cell lymphoma | Induced strong cellular and humoral immunity | Pre-clinical (in vivo study) | [179] |
| Cationic liposomes | CpG | i.d. | Melanoma | Increased DC maturation | Pre-clinical (in vivo study) | [180] |
| Liposomal polymeric gels | Cyclodextrins, TGF-β inhibitor and IL-2 | i.tm. | Melanoma | Delayed tumor growth and increased tumor survival | Pre-clinical (in vivo study) | [181] |
| Cationic liposomes | TLR agonist (CpG ODN) and Ovalbumin | s.c. or i.d. | Melanoma | Increased antigen presentation and enhanced T cell responses | Pre-clinical (in vivo study) | [182] |
| Cationic liposomes | α-GalCer with CpG and Ovalbumin | s.c. | B16 Melanoma | Increased activation of NK, DC and T cells | Pre-clinical (in vivo study) | [183] |
| Tumor cell membrane coated PLGA NPs | Ovalbumin and PAM or CpG | Melanoma | Increased antigen presentation and immune responses | Pre-clinical (in vitro study) | [187] | |
| Tumor cell membrane coated NPs | HLA-Ig and anti-CD28 | Melanoma | Promoted tumor specific immune response and induced antigen specific activation of T cell | Pre-clinical (in vitro study) | [188] | |
| Latex beads | Trp2 peptide and CpG | s.c. and i.v. | Melanoma | Inhibited tumor growth and enhanced T cell responses | Pre-clinical (in vivo study) | [189] |
| iron-dextran particles and quantum dot nanocrystals | HLA-Ig and anti-CD28 | i.p and i.v | Melanoma | Generation of antigen specific cytotoxic T lymphocytes | Pre-clinical (in vivo study) | [190] |
| aAPCs | Trp-2 peptide | i.v. | Melanoma and lung metastasis | Enhanced T cell responses and reduced tumor growth | Pre-clinical (in vivo study) | [191] |
| Nanoparticle | Active Agent | Delivery Method | Cancer Type | Effect/Inference | Clinical Trial Status | References |
|---|---|---|---|---|---|---|
| Au-NPs | Mangiferin | i.v. | Prostate cancer | Enhanced levels of anti-tumor cytokines with reduced pro-tumor cytokines | Pre-clinical (in vivo study) | [197] |
| GDNPs 2 | Ginger bioactive constituents | Oral and i.p. | Colitis-Associated Cancer | Control immune response and chronic inflammation | Pre-clinical (in vivo study) | [177] |
| Se-NPs-enriched Probiotic | Lactobacillus plantarum strain | Oral and i.v. | Breast cancer murine | Levels of proinflammatory cytokines increased and increased NK cell activity. Decreased tumor volume and increased survival | Pre-clinical (in vivo study) | [192] |
| Thiolated nano-vaccine | Neoantigen and CpGODN | i.v. | Hepatocellular carcinoma | Bypassed endo-/lysosome degradation, increased antigen uptake and presentation. Increased T cell immunity, inhibition of tumor growth and increased survival | Pre-clinical (in vivo study) | [175] |
| PLGA-NP | hgp10025e33 and TRP2180e188 | i.d. | Melanoma | Increased T cell responses and decreased tumor growth | Pre-clinical (in vivo study) | [193] |
| Kras peptide vaccine | KRAS-specific antigens and avasimibe | i.p and i.g. | Lung cancer | Decreased Treg cells and increased cytotoxic T cell tumor infiltration | Pre-clinical (in vivo study) | [195] |
| Cationic liposomes | TAA encoding mRNA | i.v. and i.d. | Prostate cancer | Increase T cell response | Pre-clinical (in vivo study) | [198] |
| Liposomes | MART1 mRNA | i.v. | B16 melanoma | Cellular immune response and induction of anti-tumor cytokines | Pre-clinical (in vivo study) | [199,200] |
| Mannosylated NPs- Liposomes | EPGF and MART1 mRNA | i.v. | B16F10 melanoma | Increased DC activity and anti-tumor immune response | Pre-clinical (in vivo study) | [201] |
| Cationic liposomes | HIV 1 mRNA | i.t. | HIV induced cancer | Increased T cell responses and anti-cancer cytokines | Pre-clinical (in vivo study) | [202] |
| Liposomes | Ovalbumin | Nasal | Melanoma | Increased cytotoxic T cell activity | Pre-clinical (in vivo study) | [203] |
| Au-NPs | Ovalbumin | i.v. | B16 melanoma | Increased anti-tumor activity and survival | Pre-clinical (in vivo study) | [204,205,206] |
| Antigen-loaded NPs | Ovalbumin | Increased DC activity | Pre-clinical (in vitro study) | [207] | ||
| Aluminum hydroxide nanoparticles | Ovalbumin | i.v. | B16 melanoma | Increased antigen-antibody recognition | Pre-clinical (in vivo study) | [208] |
| Chitosan NPs | Ovalbumin and FITC-BSA | Nasal | B16 melanoma | Increased uptake and presentation of antigen to APCs | Pre-clinical (in vivo study) | [209] |
| -γ-PGA NPs | Ovalbumin | i.d. | B16 melanoma | Helper T cell and cytotoxic T cell response increased | Pre-clinical (in vivo study) | [210] |
| Linear polyethylenimine NPs | MIP3α DNA | i.m. | B-cell non-Hodgkin’s lymphoma | Enhanced Humoral and T cell immune responses | Phase 1 | [211] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Koyande, N.P.; Srivastava, R.; Padmakumar, A.; Rengan, A.K. Advances in Nanotechnology for Cancer Immunoprevention and Immunotherapy: A Review. Vaccines 2022, 10, 1727. https://doi.org/10.3390/vaccines10101727
Koyande NP, Srivastava R, Padmakumar A, Rengan AK. Advances in Nanotechnology for Cancer Immunoprevention and Immunotherapy: A Review. Vaccines. 2022; 10(10):1727. https://doi.org/10.3390/vaccines10101727
Chicago/Turabian StyleKoyande, Navami Prabhakar, Rupali Srivastava, Ananya Padmakumar, and Aravind Kumar Rengan. 2022. "Advances in Nanotechnology for Cancer Immunoprevention and Immunotherapy: A Review" Vaccines 10, no. 10: 1727. https://doi.org/10.3390/vaccines10101727
APA StyleKoyande, N. P., Srivastava, R., Padmakumar, A., & Rengan, A. K. (2022). Advances in Nanotechnology for Cancer Immunoprevention and Immunotherapy: A Review. Vaccines, 10(10), 1727. https://doi.org/10.3390/vaccines10101727








