Factors Associated with Willingness to Receive a COVID-19 Vaccine in Adult Polish Population—A Cross-Sectional Survey
Abstract
1. Introduction
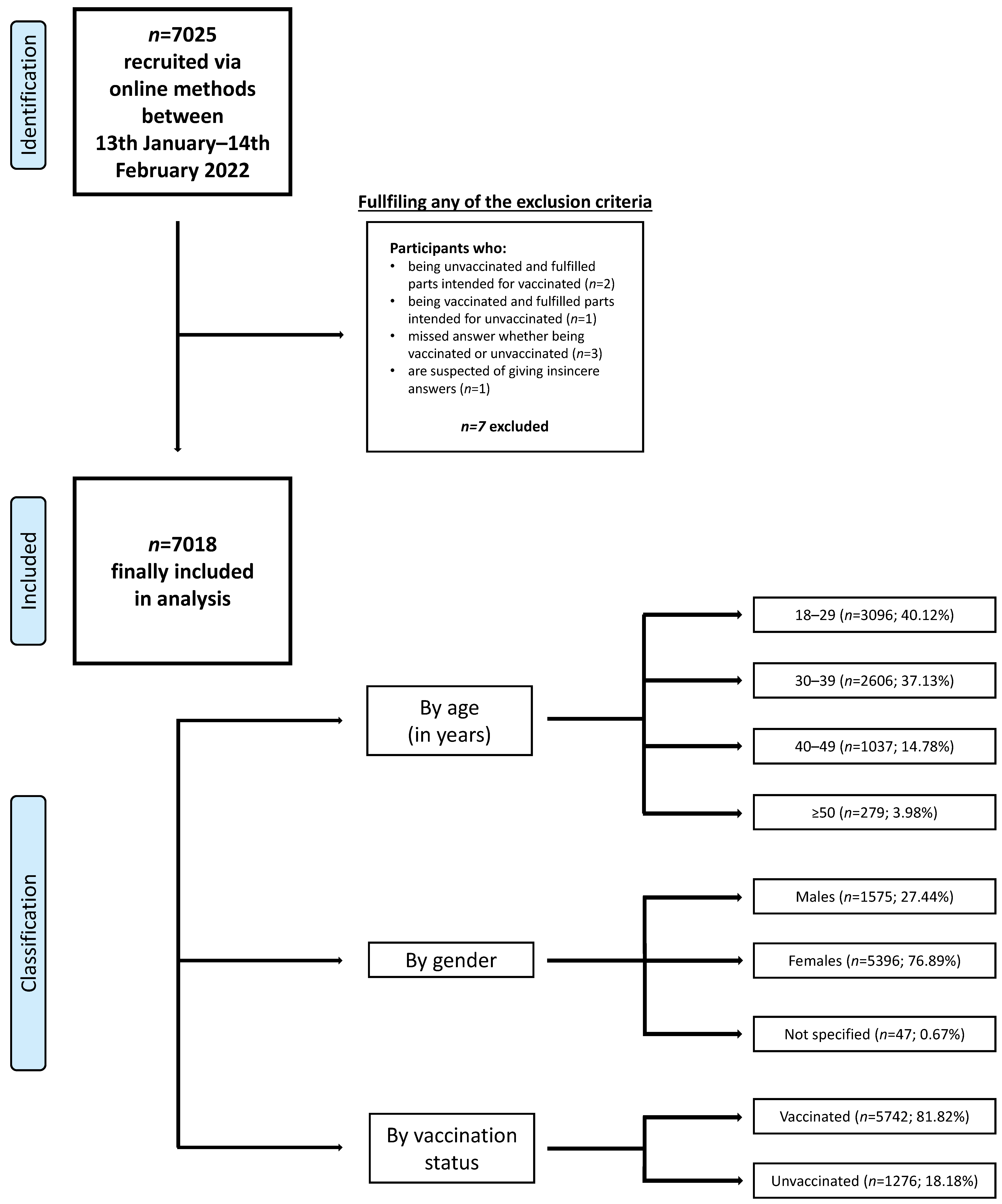
2. Materials and Methods
2.1. Study Design and Instrument
2.2. Ethics
2.3. Data Analysis
3. Results
3.1. Sociodemographic Characteristics
3.2. Chronic Co-Morbidities
3.3. Factors Associated with COVID-19 Vaccination
4. Discussion
5. Practical Implications
6. Further Studies Directions
7. Limitations
8. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gruba, G.; Kasiak, P.S.; Gębarowska, J.; Adamczyk, N.; Sikora, Z.; Jodczyk, A.M.; Mamcarz, A.; Śliż, D. PaLS Study of Sleep Deprivation and Mental Health Consequences of the COVID-19 Pandemic among University Students: A Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2021, 18, 9581. [Google Scholar] [CrossRef]
- Jodczyk, A.M.; Gruba, G.; Sikora, Z.; Kasiak, P.S.; Gębarowska, J.; Adamczyk, N.; Mamcarz, A.; Śliż, D. PaLS Study: How Has the COVID-19 Pandemic Influenced Physical Activity and Nutrition? Observations a Year after the Outbreak of the Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 9632. [Google Scholar] [CrossRef]
- Jodczyk, A.M.; Kasiak, P.S.; Adamczyk, N.; Gębarowska, J.; Sikora, Z.; Gruba, G.; Mamcarz, A.; Śliż, D. PaLS Study: Tobacco, Alcohol and Drugs Usage among Polish University Students in the Context of Stress Caused by the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 1261. [Google Scholar] [CrossRef]
- Kasiak, P.S.; Adamczyk, N.; Jodczyk, A.M.; Kaproń, A.; Lisowska, A.; Mamcarz, A.; Śliż, D. COVID-19 Pandemic Consequences among Individuals with Eating Disorders on a Clinical Sample in Poland—A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 8484. [Google Scholar] [CrossRef]
- Xing, K.; Tu, X.-Y.; Liu, M.; Liang, Z.-W.; Chen, J.-N.; Li, J.-J.; Jiang, L.-G.; Xing, F.-Q.; Jiang, Y. Efficacy and safety of COVID-19 vaccines: A systematic review. Zhongguo Dang Dai Er Ke Za Zhi 2021, 23, 221–228. [Google Scholar]
- Tagliabue, F.; Galassi, L.; Mariani, P. The “Pandemic” of Disinformation in COVID-19. SN Compr Clin. Med. 2020, 2, 1287–1289. [Google Scholar] [CrossRef]
- Braczkowska, B.; Kowalska, M.; Braczkowski, R.; Barański, K. Determinants of vaccine hesitancy. Przegl Epidemiol. 2017, 71, 227–236. [Google Scholar] [PubMed]
- Włodarska, A.; Gujski, M.; Pinkas, J.; Raciborski, F. The influence of socio-demographic characteristics on attitudes towards prophylactic vaccination in Poland. Int. J. Occup. Med. Environ. Health 2021, 34, 121–132. [Google Scholar] [CrossRef]
- Dredze, M.; Broniatowski, D.A.; Smith, M.C.; Hilyard, K.M. Understanding Vaccine Refusal: Why We Need Social Media Now. Am. J. Prev. Med. 2016, 50, 550–552. [Google Scholar] [CrossRef]
- Mrożek-Budzyn, D.; Kiełtyka, A.; Majewska, R.; Mróz, E. What mother know about vaccine preventable diseases? Przegl Epidemiol. 2017, 71, 595–602. [Google Scholar]
- European Centre for Disease Prevention and Control (ECDC). COVID-19 Situation Update Worldwide. Available online: https://www.ecdc.europa.eu/en/geographical-distribution-2019-ncov-cases (accessed on 5 December 2021).
- Raciborski, F.; Jankowski, M.; Gujski, M.; Pinkas, J.; Samel-Kowalik, P. Changes in Attitudes towards the COVID-19 Vaccine and the Willingness to Get Vaccinated among Adults in Poland: Analysis of Serial, Cross-Sectional, Representative Surveys, January–April 2021. Vaccines 2021, 9, 832. [Google Scholar] [CrossRef] [PubMed]
- GUS. Polska w Liczbach 2022. Available online: https://stat.gov.pl/obszary-tematyczne/inne-opracowania/inne-opracowania-zbiorcze/polska-w-liczbach-2022,14,15.html (accessed on 17 September 2022).
- Franic, J. What Lies Behind Substantial Differences in COVID-19 Vaccination Rates between EU Member States? Front. Public Health 2022, 10, 858265. [Google Scholar] [CrossRef] [PubMed]
- Della Polla, G.; Pelullo, C.P.; Di Giuseppe, G.; Angelillo, I.F. Changes in Behaviors and Attitudes in Response to COVID-19 Pandemic and Vaccination in Healthcare Workers and University Students in Italy. Vaccines 2021, 9, 1276. [Google Scholar] [CrossRef]
- Fisher, K.A.; Bloomstone, S.J.; Walder, J.; Crawford, S.; Fouayzi, H.; Mazor, K.M. Attitudes toward a Potential SARS-CoV-2 Vaccine: A Survey of U.S. Adults. Ann. Intern. Med. 2020, 173, 964–973. [Google Scholar] [CrossRef] [PubMed]
- Paradis, S.; Roussel, J.; Bosson, J.-L.; Kern, J.-B. Use of Smartphone Health Apps among Patients Aged 18 to 69 Years in Primary Care: Population-Based Cross-sectional Survey. JMIR Form. Res. 2022, 6, e34882. [Google Scholar] [CrossRef]
- Subramanian, S.; Huijts, T.; Avendano, M. Self-reported health assessments in the 2002 World Health Survey: How do they cor-relate with education? Bull. World Health Organ. 2010, 88, 131–138. [Google Scholar] [CrossRef]
- The Act of 5 December 1996 on the Professions of Doctor and Dentist (Journal of Laws of 2021, Item 790 and 1559). Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahUKEwj7oKTUrbf6AhWRjYsKHUBVD3EQFnoE-CAgQAQ&url=https%3A%2F%2Fec.europa.eu%2Fgrowth%2Ftools-databases%2Ftris%2Findex.cfm%2Fen%2Fsearch%2F%3Ftrisaction%3Dsearch.detail%26year%3D2021%26num% (accessed on 28 September 2022).
- Kachurka, R.; Krawczyk, M.; Rachubik, J. Persuasive Messages Will Not Increase COVID-19 Vaccine Acceptance: Evidence from a Nationwide Online Experiment. Vaccines 2021, 9, 1113. [Google Scholar] [CrossRef]
- Rzymski, P.; Poniedziałek, B.; Fal, A. Willingness to Receive the Booster COVID-19 Vaccine Dose in Poland. Vaccines 2021, 9, 1286. [Google Scholar] [CrossRef]
- Raciborski, F.; Samel-Kowalik, P.; Gujski, M.; Pinkas, J.; Arcimowicz, M.; Jankowski, M. Factors Associated with a Lack of Willingness to Vaccinate against COVID-19 in Poland: A 2021 Nationwide Cross-Sectional Survey. Vaccines 2021, 9, 1000. [Google Scholar] [CrossRef]
- MacDonald, N.E.; SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- Wolfe, R.M.; Sharp, L.K. Anti-vaccinationists past and present. BMJ 2002, 325, 430–432. [Google Scholar] [CrossRef]
- Jemielniak, D.; Krempovych, Y. An analysis of AstraZeneca COVID-19 vaccine misinformation and fear mongering on Twitter. Public Health 2021, 200, 4–6. [Google Scholar] [CrossRef] [PubMed]
- Wawrzuta, D.; Jaworski, M.; Gotlib, J.; Panczyk, M. What Arguments against COVID-19 Vaccines Run on Facebook in Poland: Content Analysis of Comments. Vaccines 2021, 9, 481. [Google Scholar] [CrossRef] [PubMed]
- Vaccination Schedule for Poland. Available online: https://immunizationdata.who.int/pages/schedule-by-country/pol.html (accessed on 29 August 2022).
- The Main Statistical Office in Poland, Report on Vaccination against COVID-19. Available online: https://www.gov.pl/web/szczepimysie/raport-szczepien-przeciwko-covid-19 (accessed on 29 August 2022).
- National Institute of Public Health NIH—National Research Institute Department of Epidemiology and Surveillance of Infec-tious Diseases, Vaccinations in Poland in 2020. 2021. Available online: http://wwwold.pzh.gov.pl/oldpage/epimeld/2020/Sz_2020.pdf (accessed on 29 August 2022).
- Wang, Q.; Yang, L.; Jin, H.; Lin, L. Vaccination against COVID-19: A systematic review and meta-analysis of acceptability and its predictors. Prev. Med. 2021, 150, 106694. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, J.V.; Ratzan, S.C.; Palayew, A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Kimball, S.; El-Mohandes, A. A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 2021, 27, 225–228. [Google Scholar] [CrossRef]
- Pijls, B.G.; Jolani, S.; Atherley, A.; Derckx, R.T.; Dijkstra, J.I.R.; Franssen, G.H.L.; Hendriks, S.; Richters, A.; Venemans-Jellema, A.; Zalpuri, S.; et al. Demographic risk factors for COVID-19 infection, severity, ICU admission and death: A meta-analysis of 59 studies. BMJ Open 2021, 11, e044640. [Google Scholar] [CrossRef]
- Lazarus, J.V.; Wyka, K.; Rauh, L.; Rabin, K.; Ratzan, S.; Gostin, L.O.; Larson, H.J.; El-Mohandes, A. Hesitant or Not? The Association of Age, Gender, and Ed-ucation with Potential Acceptance of a COVID-19 Vaccine: A Country-level Analysis. J. Health Commun. 2020, 25, 799–807. [Google Scholar] [CrossRef] [PubMed]
- Manolescu, L.S.C.; Zaharia, C.N.; Dumitrescu, A.I.; Prasacu, I.; Radu, M.C.; Boeru, A.C.; Boidache, L.; Nita, I.; Necsulescu, A.; Chivu, R.D. Early COVID-19 Vaccination of Romanian Medical and Social Personnel. Vaccines 2021, 9, 1127. [Google Scholar] [CrossRef] [PubMed]
- Dombrádi, V.; Joó, T.; Palla, G.; Pollner, P.; Belicza, É. Comparison of hesitancy between COVID-19 and seasonal influenza vac-cinations within the general Hungarian population: A cross-sectional study. BMC Public Health 2021, 21, 2317. [Google Scholar] [CrossRef]
- Dombrádi, V.; Joó, T.; Palla, G.; Pollner, P.; Belicza, É.C.; De Giorgio, A.; Kuvačić, G.; Maleš, D.; Vecchio, I.; Tornali, C.; et al. Willingness to Receive COVID-19 Booster Vaccine: Associations between Green-Pass, Social Media Information, Anti-Vax Beliefs, and Emotional Balance. Vaccines 2022, 10, 481. [Google Scholar]
- Fajar, J.K.; Sallam, M.; Soegiarto, G.; Sugiri, Y.J.; Anshory, M.; Wulandari, L.; Kosasih, S.A.P.; Ilmawan, M.; Kusnaeni, K.; Fikri, M.; et al. Global Prevalence and Potential Influencing Factors of COVID-19 Vaccination Hesitancy: A Meta-Analysis. Vaccines 2022, 10, 1356. [Google Scholar] [CrossRef] [PubMed]
- Ulbrichtova, R.; Svihrova, V.; Tatarkova, M.; Hudeckova, H.; Svihra, J. Acceptance of COVID-19 Vaccination among Healthcare and Non-Healthcare Workers of Hospitals and Outpatient Clinics in the Northern Region of Slovakia. Int. J. Environ. Res. Public Health 2021, 18, 12695. [Google Scholar] [CrossRef]
- Luo, C.; Yang, Y.; Liu, Y.; Zheng, D.; Shao, L.; Jin, J.; He, Q. Intention to COVID-19 vaccination and associated factors among health care workers: A systematic review and meta-analysis of cross-sectional studies. Am. J. Infect. Control 2021, 49, 1295–1304. [Google Scholar] [CrossRef]
- Wang, J.; Jing, R.; Lai, X.; Zhang, H.; Lyu, Y.; Knoll, M.D.; Fang, H. Acceptance of COVID-19 Vaccination during the COVID-19 Pandemic in China. Vaccines 2020, 8, 482. [Google Scholar] [CrossRef] [PubMed]
- Malik, A.A.; McFadden, S.M.; Elharake, J.; Omer, S.B. Determinants of COVID-19 vaccine acceptance in the US. eClinicalMedicine 2020, 26, 100495. [Google Scholar] [CrossRef]
- Gallè, F.; Sabella, E.A.; Roma, P.; De Giglio, O.; Caggiano, G.; Tafuri, S.; Da Molin, G.; Ferracuti, S.; Montagna, M.T.; Liguori, G.; et al. Knowledge and Acceptance of COVID-19 Vaccination among Undergraduate Students from Central and Southern Italy. Vaccines 2021, 9, 638. [Google Scholar] [CrossRef] [PubMed]
- Schmid, P.; Rauber, D.; Betsch, C.; Lidolt, G.; Denker, M.-L. Barriers of Influenza Vaccination Intention and Behavior—A Systematic Review of Influenza Vaccine Hesitancy, 2005–2016. PLoS ONE 2017, 12, e0170550. [Google Scholar] [CrossRef] [PubMed]
- Bagić, D.; Šuljok, A.; Ančić, B. Determinants and reasons for coronavirus disease 2019 vaccine hesitancy in Croatia. Croat. Med. J. 2022, 63, 89–97. [Google Scholar] [CrossRef]
- Urrunaga-Pastor, D.; Bendezu-Quispe, G.; Herrera-Añazco, P.; Uyen-Cateriano, A.; Toro-Huamanchumo, C.J.; Rodriguez-Morales, A.J.; Hernandez, A.V.; Benites-Zapata, V.A. Cross-sectional analysis of COVID-19 vaccine intention, perceptions and hesitancy across Latin America and the Caribbean. Travel Med. Infect. Dis. 2021, 41, 102059. [Google Scholar] [CrossRef]
- Farrar, D.S.; Drouin, O.; Hepburn, C.M.; Baerg, K.; Chan, K.; Cyr, C.; Donner, E.J.; Embree, J.E.; Farrell, C.; Forgie, S.; et al. Risk factors for severe COVID-19 in hospitalized children in Canada: A national prospective study from March 2020–May 2021. Lancet Reg. Health-Am. 2022, 15, 100337. [Google Scholar] [CrossRef]
- Fresán, U.; Guevara, M.; Trobajo-Sanmartín, C.; Burgui, C.; Ezpeleta, C.; Castilla, J. Hypertension and Related Comorbidities as Potential Risk Factors for COVID-19 Hospitalization and Severity: A Prospective Population-Based Cohort Study. J. Clin. Med. 2021, 10, 1194. [Google Scholar] [CrossRef]
- Antoon, J.W.; Grijalva, C.G.; Thurm, C.; Richardson, T.; Spaulding, A.B.; Ii, R.J.T.; Reyes, A.M.; Shah, S.S.; Burns, E.J.; Kenyon, C.C.; et al. Factors Associated with COVID-19 Disease Severity in US Children and Adolescents. J. Hosp. Med. 2021, 16, 603–610. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Sattar, N.; McInnes, I.B.; McMurray, J.J. Obesity Is a Risk Factor for Severe COVID-19 Infection. Am. Heart Assoc. 2020, 142, 4–6. [Google Scholar] [CrossRef] [PubMed]
- Demeulemeester, F.; de Punder, K.; van Heijningen, M.; van Doesburg, F. Obesity as a Risk Factor for Severe COVID-19 and Complications: A Review. Cells 2021, 10, 933. [Google Scholar] [CrossRef] [PubMed]
- Kara, Z.; Akçin, R.; Demir, A.N.; Dinç, H.Ö.; Taşkın, H.E.; Kocazeybek, B.; Yumuk, V.D. Antibody Response to SARS-CoV-2 Vaccines in People with Severe Obesity. Obes Surg. 2022, 32, 2987–2993. [Google Scholar] [CrossRef]
- Redondo Margüello, E.; Trilla, A.; Munguira, I.L.B.; López-Herce, A.J.; Cotarelo Suárez, M. Knowledge, attitudes, beliefs and barriers of healthcare professionals and adults ≥ 65 years about vaccine-preventable diseases in Spain: The Adult Vaccination Drivers and Barriers (ADVISE) study. Hum. Vaccin. Immunother. 2022, 18, 2025007. [Google Scholar] [CrossRef] [PubMed]
- Benites-Zapata, V.A.; Herrera-Añazco, P.; Benites-Meza, J.K.; Bonilla-Aguilar, K.; Urrunaga-Pastor, D.; Bendezu-Quispe, G.; Uyen-Cateriano, A.; Rodriguez-Morales, A.J.; Hernandez, A.V. Prevalence of parents’ non-intention to vaccinate their children and adolescents against COVID-19: A comparative analysis in Colombia and Peru. Vaccine X 2022, 12, 100198. [Google Scholar] [CrossRef]
- Seale, H.; Heywood, A.E.; Leask, J.; Sheel, M.; Durrheim, D.N.; Bolsewicz, K.; Kaur, R. Examining Australian public perceptions and be-haviors towards a future COVID-19 vaccine. BMC Infect. Dis. 2021, 21, 120. [Google Scholar] [CrossRef]
- Kunze, C.; Großmann, U.; Stork, W.; Müller-Glaser, K. Application of Ubiquitous Computing in Personal Health Monitoring Systems. Biomed. Eng./Biomed. Tech. 2002, 47, 360–362. [Google Scholar] [CrossRef] [PubMed]
- Moses, J.; Adibi, S.; Islam, S.S.; Wickramasinghe, N.; Nguyen, L. Application of Smartphone Technologies in Disease Monitoring: A Systematic Review. Healthcare 2021, 9, 889. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.S.; Gvozdanovic, A.; Knight, M.; Gagnon, J. Mobile App–Based Remote Patient Monitoring in Acute Medical Conditions: Prospective Feasibility Study Exploring Digital Health Solutions on Clinical Workload During the COVID Crisis. JMIR Form. Res. 2021, 5, e23190. [Google Scholar] [CrossRef] [PubMed]
- Rabbi, M.; Pfammatter, A.; Zhang, M.; Spring, B.; Choudhury, T. Automated Personalized Feedback for Physical Activity and Dietary Behavior Change with Mobile Phones: A Randomized Controlled Trial on Adults. JMIR Mhealth Uhealth 2015, 3, e42. [Google Scholar] [CrossRef]
- Popa, A.D.; Enache, A.I.; Popa, I.V.; Antoniu, S.A.; Dragomir, R.A.; Burlacu, A. Determinants of the Hesitancy toward COVID-19 Vaccination in Eastern European Countries and the Relationship with Health and Vaccine Literacy: A Literature Review. Vaccines 2022, 10, 672. [Google Scholar] [CrossRef]
- Gallè, F.; Sabella, E.A.; Roma, P.; Ferracuti, S.; Da Molin, G.; Diella, G.; Montagna, M.T.; Orsi, G.B.; Liguori, G.; Napoli, C. Knowledge and Lifestyle Behaviors Related to COVID-19 Pandemic in People over 65 Years Old from Southern Italy. Int. J. Environ. Res. Public Health 2021, 18, 10872. [Google Scholar] [CrossRef]
- COVID-19 Vaccine Hesitancy among Pregnant Women: A Systematic Review and Meta-Analysis|BMJ Open [Internet]. Available online: https://bmjopen.bmj.com/content/12/8/e061477.long (accessed on 2 October 2022).
- Gheorghe, A.S.; Negru, Ş.M.; Nițipir, C.; Mazilu, L.; Marinca, M.; Gafton, B.; Ciuleanu, T.E.; Schenker, M.; Dragomir, R.D.; Gheorghe, A.D.; et al. Knowledge, attitudes and practices related to the COVID-19 outbreak among Romanian adults with cancer: A cross-sectional national survey. ESMO Open 2021, 6, 100027. [Google Scholar] [CrossRef]
- Ljivo, A.; Ćetković, A.; Abdulkhaliq, A.; Kiseljaković, M.A.S.; Kulo, A. COVID-19 vaccination knowledge, attitudes and practices among residents of Bosnia and Herzegovina during the third wave of COVID-19 outbreak. Ann. Ig. 2022, 34, 490–500. [Google Scholar]
- Kwok, K.O.; Lai, F.; Wei, W.I.; Wong, S.Y.S.; Tang, J.W.T. Herd immunity—Estimating the level required to halt the COVID-19 epidemics in affected countries. J. Infect. 2020, 80, e32–e33. [Google Scholar] [CrossRef]
- Andrade, C. The Limitations of Online Surveys. Indian J. Psychol. Med. 2020, 42, 575–576. [Google Scholar] [CrossRef]
- Steyerberg, E.W.; Borsboom, G.J.J.M.; van Houwelingen, H.C.; Eijkemans, M.J.C.; Habbema, J.D.F. Validation and updating of predictive logistic regression models: A study on sample size and shrinkage. Stat. Med. 2004, 23, 2567–2586. [Google Scholar] [CrossRef] [PubMed]
- Toll, D.; Janssen, K.; Vergouwe, Y.; Moons, K. Validation, updating and impact of clinical prediction rules: A review. J. Clin. Epidemiol. 2008, 61, 1085–1094. [Google Scholar] [CrossRef] [PubMed]
- Dowrick, A.S.; Wootten, A.C.; Murphy, D.G.; Costello, A.J. “We Used a Validated Questionnaire”: What Does This Mean and Is It an Accurate Statement in Urologic Research? Urology 2015, 85, 1304–1311. [Google Scholar] [CrossRef] [PubMed]
| Variable | Vaccinated against COVID-19 [n = 5742, 81.82%] | Unvaccinated against COVID-19 [n = 1276, 18.18%] | p-Value | |
|---|---|---|---|---|
| Mean age (SD) | 31 (18–75) | 30 (18–73) | <0.001 | |
| Gender | Male [n = 1575, 22.44%] | 1236 (78.48%) | 339 (21.52%) | <0.001 |
| Female [n = 5396, 76.89%] | 4466 (82.77%) | 930 (17.23%) | ||
| Do not specify [n = 47, 0.67%] | 40 (85.11%) | 7 (14.89%) | ||
| Marital status | Married [n = 2916, 41.55% | 2417 (82.89%) | 499 (17.11%) | 0.007 |
| Single [n = 2054, 29.27%] | 1629 (79.31%) | 425 (20.69%) | ||
| Divorced [n = 227, 3.23%] | 186 (81.94%) | 41 (18.06%) | ||
| Widow [n = 13, 0.19%] | 9 (69.23%) | 4 (30.77%) | ||
| Cohabitation [n = 1808, 25.76%] | 1501 (83.02%) | 307 (16.98%) | ||
| Education status | Higher [n = 5087, 72.49%] | 4258 (83.70%) | 829 (16.30%) | <0.001 |
| Middle [n = 1764, 25.14%] | 1369 (77.61%) | 395 (22.39%) | ||
| Primary [n = 28, 0.40%] | 25 (89.29%) | 3 (10.71%) | ||
| Basic vocational [n = 60, 0.85%] | 35 (58.33%) | 25 (41.67%) | ||
| Lower secondary [n = 79, 1.13%] | 55 (69.62%) | 24 (30.38%) | ||
| Occupation | Services [n = 5291, 75.39%] | 4345 (82.12%) | 946 (17.88%) | 0.376 |
| Industry [n = 711, 10.13% | 574 (80.73%) | 137 (19.27%) | ||
| Agriculture [n = 41, 0.58%] | 30 (73.17%) | 11 (26.83%) | ||
| Unemployed [n = 975, 13.89%] | 793 (81.33%) | 182 (18.67%) | ||
| Residence area | Up to 50,000 [n = 925, 13.18%] | 722 (78.05%) | 203 (21.95%) | <0.001 |
| 50,000–150,000 [n = 846, 12.05%] | 622 (73.52%) | 224 (26.48%) | ||
| 150,000–500,000 [n = 1158, 16.50%] | 941 (81.26%) | 217 (18.74%) | ||
| More than 500,000 [n = 3170, 45.17%] | 2745 (86.59%) | 425 (13.41%) | ||
| Village [n = 919, 13.09%] | 712 (77.48%) | 207 (22.52%) | ||
| Children | Yes [n = 2826, 40.27%] | 2279 (39,69%) | 547 (42,87%) | 0.013 |
| No [n = 4192, 59.73%] | 3463 (60,31%) | 729 (57,13%) | ||
| Overall lifestyle assessment | Healthy [n = 4056, 57.79%] | 3221 (79.41%) | 835 (20.59%) | <0.001 |
| Unhealthy [n = 1136, 16.19%] | 981 (86.36%) | 155 (13.64%) | ||
| I do not know [n = 1826, 26.02%] | 1540 (84.34%) | 286 (15.66%) | ||
| Overall health assessment | Excellent [n = 461, 6.57%] | 313 (67.90%) | 148 (32.10%) | <0.001 |
| Very good [n = 3000, 42.75%] | 2393 (79.77%) | 607 (20.23%) | ||
| Good [n = 3079, 43.87%] | 2642 (85.81%) | 437 (14.19%) | ||
| Not too good [435, 6.20%] | 361 (82.99%) | 74 (17.01%) | ||
| Bad [43, 0.61%] | 33 (76.74%) | 10 (23.26%) | ||
| Variable | Type of Answer | Vaccinated against COVID-19 [n = 5742, 81.82%] | Unvaccinated against COVID-19 [n = 1276, 18.18%] | p-Value |
|---|---|---|---|---|
| Obesity | Yes [n = 785, 11.19%] | 689 (87.77%) | 96 (12.23%) | <0.001 |
| No [n = 6233, 88.81%] | 5053 (81.07%) | 1180 (18.93%) | ||
| Diabetes | Yes [n = 125, 1.78%] | 95 (76%) | 30 (24%) | 0.089 |
| No [n = 6893, 98.22%] | 5647 (90.60%) | 1246 (9.40%) | ||
| Hypertension | Yes [n = 354, 5.04%] | 314 (88.70%) | 40 (11.30%) | <0.001 |
| No [n = 6664, 94.96%] | 5428 (81.45%) | 1236 (18.55%) | ||
| Cancer | Yes [n = 81, 1.15%] | 67 (82.72%) | 14 (17.28%) | 0.833 |
| No [n = 6937, 98.85%] | 5675 (81.81%) | 1262 (18.19%) | ||
| Respiratory diseases | Yes [n = 447, 6.37%] | 371 (83.00%) | 76 (17%) | 0.504 |
| No [n = 6571, 93.63%] | 5371 (81.74%) | 1200 (18.26%) | ||
| Autoimmune diseases | Yes [n = 1141, 16.26%] | 954 (83.61%) | 187 (16.39%) | 0.086 |
| No [n = 5877, 83.74%] | 4788 (81.47%) | 1089 (18.53%) | ||
| Psychiatric diseases | Yes [n = 983, 14.01%] | 867 (88.20%) | 116 (11.80%) | <0.001 |
| No [n = 6035, 85.99%] | 4875 (80.78%) | 1160 (18.22%) |
| Odds Ratio (95% Cl) | ||
|---|---|---|
| Gender | Male | 0.83 (0.72–0.97) |
| Do not specify | 0.94 (0.41–2.18) | |
| Female * | 1.00 | |
| Age | >50 | 0.95 (0.64–1.41) |
| 40–49 | 1.12 (0.90–1.41) | |
| 30–39 | 0.95 (0.81–1.12) | |
| 18–29 * | 1.00 | |
| Education status | Primary | 2.23 (0.64–7.73) |
| Middle | 0.77 (0.65–0.90) | |
| Basic vocational | 0.38 (0.22–0.66) | |
| Lower secondary | 0.56 (0.33–0.96) | |
| Higher * | 1.00 | |
| Marital status | Cohabitation | 1.10 (0.92–1.32) |
| Single | 0.89 (0.74–1.05) | |
| Divorced | 0.88 (0.60–1.28) | |
| Widow | 0.50 (0.14–1.73) | |
| Married * | 1.00 | |
| Occupation | Unemployed | 1.30 (1.05–1.59) |
| Industry | 1.01 (0.82–1.24) | |
| Agriculture | 0.82 (0.38–1.74) | |
| Services * | 1.00 | |
| Residence area | 150,000–500,000 | 0.73 (0.61–0.88) |
| up to 50,000 | 0.59 (0.48–0.71) | |
| 50,000–150,000 | 0.47 (0.39–0.57) | |
| village | 0.57 (0.47–0.70) | |
| more than 500,000 * | 1.00 | |
| Chronic comorbidities | Yes | 1.46 (1.28–1.66) |
| No * | 1.00 | |
| Use of health monitoring application | Yes | 1.56 (1.37–1.77) |
| No * | 1.00 | |
| Receive the flu vaccine in 2021 or 2022 | Yes | 24.51 (15.50–38.76) |
| No * | 1.00 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ulaszewska, K.; Jodczyk, A.M.; Długołęcki, P.; Emerla, S.; Stańska, W.; Kasiak, P.S.; Gąsior, J.S.; Parol, D.; Mamcarz, A.; Śliż, D. Factors Associated with Willingness to Receive a COVID-19 Vaccine in Adult Polish Population—A Cross-Sectional Survey. Vaccines 2022, 10, 1715. https://doi.org/10.3390/vaccines10101715
Ulaszewska K, Jodczyk AM, Długołęcki P, Emerla S, Stańska W, Kasiak PS, Gąsior JS, Parol D, Mamcarz A, Śliż D. Factors Associated with Willingness to Receive a COVID-19 Vaccine in Adult Polish Population—A Cross-Sectional Survey. Vaccines. 2022; 10(10):1715. https://doi.org/10.3390/vaccines10101715
Chicago/Turabian StyleUlaszewska, Katarzyna, Alicja Monika Jodczyk, Piotr Długołęcki, Sara Emerla, Wiktoria Stańska, Przemysław Seweryn Kasiak, Jakub S. Gąsior, Damian Parol, Artur Mamcarz, and Daniel Śliż. 2022. "Factors Associated with Willingness to Receive a COVID-19 Vaccine in Adult Polish Population—A Cross-Sectional Survey" Vaccines 10, no. 10: 1715. https://doi.org/10.3390/vaccines10101715
APA StyleUlaszewska, K., Jodczyk, A. M., Długołęcki, P., Emerla, S., Stańska, W., Kasiak, P. S., Gąsior, J. S., Parol, D., Mamcarz, A., & Śliż, D. (2022). Factors Associated with Willingness to Receive a COVID-19 Vaccine in Adult Polish Population—A Cross-Sectional Survey. Vaccines, 10(10), 1715. https://doi.org/10.3390/vaccines10101715








