Impact of HLA Polymorphism on the Immune Response to Bacillus Anthracis Protective Antigen in Vaccination versus Natural Infection
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethics Statement
2.2. HLA Class II Transgenic Mice
2.3. Live B. anthracis Challenge
2.4. Expression and Purification of PA Antigens
2.5. PA Epitope Mapping in Transgenic Mice
2.6. PA Epitope Mapping with Human Donor PBMC Samples
2.7. HLA-Peptide Binding Assay
3. Results
3.1. CD4+ T Cell Responses to B. anthracis PA Epitopes in Anthrax-Recovered Patients and Vaccinees
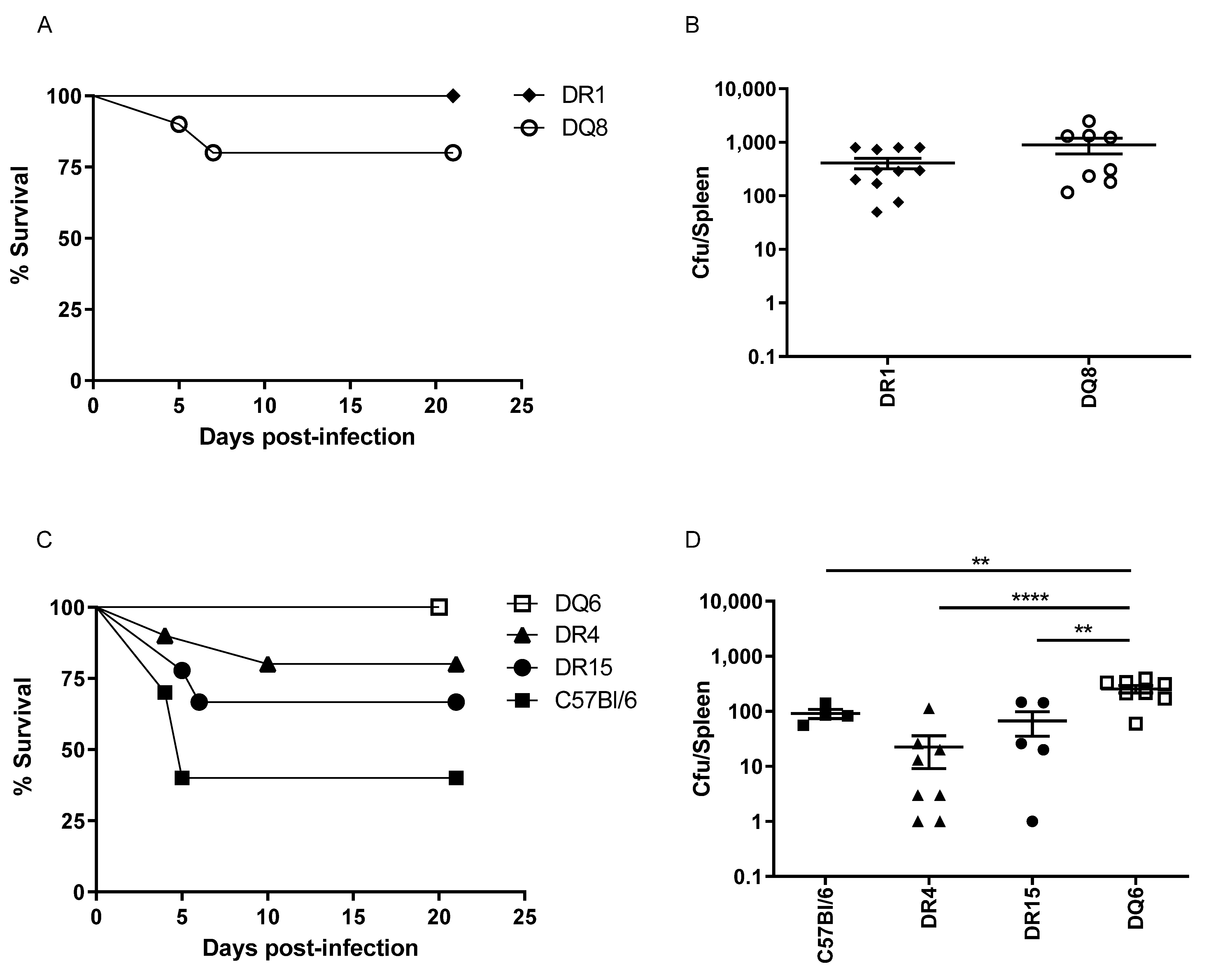
3.2. Differential Susceptibility to B. anthracis Challenge in HLA Transgenic Mice
3.3. CD4+ T Cell Responses to B. anthracis PA Epitopes in HLA Transgenic Mice
3.4. The Differential PA Peptide Binding across Distinct HLA Polymorphisms
3.5. Figures and Tables
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Goel, A.K. Anthrax: A disease of biowarfare and public health importance. World J. Clin. Cases 2015, 3, 20–33. [Google Scholar] [CrossRef] [PubMed]
- Dixon, T.C.; Meselson, M.; Guillemin, J.; Hanna, P.C. Anthrax. N. Engl. J. Med. 1999, 341, 815–826. [Google Scholar] [CrossRef] [PubMed]
- Green, M.S.; LeDuc, J.; Cohen, D.; Franz, D.R. Confronting the threat of bioterrorism: Realities, challenges, and defensive strategies. Lancet Infect. Dis. 2019, 19, e2–e13. [Google Scholar] [CrossRef]
- Abbara, A.; Brooks, T.; Taylor, G.P.; Nolan, M.; Donaldson, H.; Manikon, M.; Holmes, A. Lessons for control of heroin-associated anthrax in Europe from 2009–2010 outbreak case studies, London, UK. Emerg. Infect. Dis. 2014, 20, 1115–1122. [Google Scholar] [CrossRef]
- Revich, B.A.; Podolnaya, M.A. Thawing of permafrost may disturb historic cattle burial grounds in East Siberia. Glob. Health Action 2011, 4, 8482. [Google Scholar] [CrossRef]
- Baillie, L.W.; Fowler, K.; Turnbull, P.C. Human immune responses to the UK human anthrax vaccine. J. Appl. Microbiol. 1999, 87, 306–308. [Google Scholar] [CrossRef]
- Chitlaru, T.; Altboum, Z.; Reuveny, S.; Shafferman, A. Progress and novel strategies in vaccine development and treatment of anthrax. Immunol. Rev. 2011, 239, 221–236. [Google Scholar] [CrossRef]
- Enstone, J.E.; Wale, M.C.; Nguyen-Van-Tam, J.S.; Pearson, J.C. Adverse medical events in British service personnel following anthrax vaccination. Vaccine 2003, 21, 1348–1354. [Google Scholar] [CrossRef]
- Brey, R.N. Molecular basis for improved anthrax vaccines. Adv. Drug Deliv. Rev. 2005, 57, 1266–1292. [Google Scholar] [CrossRef]
- Hopkins, R.J.; Kalsi, G.; Montalvo-Lugo, V.M.; Sharma, M.; Wu, Y.; Muse, D.D.; Sheldon, E.A.; Hampel, F.C.; Lemiale, L. Randomized, double-blind, active-controlled study evaluating the safety and immunogenicity of three vaccination schedules and two dose levels of AV7909 vaccine for anthrax post-exposure prophylaxis in healthy adults. Vaccine 2016, 34, 2096–2105. [Google Scholar] [CrossRef] [Green Version]
- Baillie, L.W. Past, imminent and future human medical countermeasures for anthrax. J. Appl. Microbiol. 2006, 101, 594–606. [Google Scholar] [CrossRef] [PubMed]
- England, P.H. Anthrax: Green Book, Chapter 13; UK Health Security Agency: London, UK, 2017.
- Brown, B.K.; Cox, J.; Gillis, A.; VanCott, T.C.; Marovich, M.; Milazzo, M.; Antonille, T.S.; Wieczorek, L.; McKee, K.T., Jr.; Metcalfe, K.; et al. Phase I study of safety and immunogenicity of an Escherichia coli-derived recombinant protective antigen (rPA) vaccine to prevent anthrax in adults. PLoS ONE 2010, 5, e13849. [Google Scholar] [CrossRef] [PubMed]
- Campbell, J.D.; Clement, K.H.; Wasserman, S.S.; Donegan, S.; Chrisley, L.; Kotloff, K.L. Safety, reactogenicity and immunogenicity of a recombinant protective antigen anthrax vaccine given to healthy adults. Hum. Vaccines 2007, 3, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Gorse, G.J.; Keitel, W.; Keyserling, H.; Taylor, D.N.; Lock, M.; Alves, K.; Kenner, J.; Deans, L.; Gurwith, M. Immunogenicity and tolerance of ascending doses of a recombinant protective antigen (rPA102) anthrax vaccine: A randomized, double-blinded, controlled, multicenter trial. Vaccine 2006, 24, 5950–5959. [Google Scholar] [CrossRef]
- Hewetson, J.F.; Little, S.F.; Ivins, B.E.; Johnson, W.M.; Pittman, P.R.; Brown, J.E.; Norris, S.L.; Nielsen, C.J. An in vivo passive protection assay for the evaluation of immunity in AVA-vaccinated individuals. Vaccine 2008, 26, 4262–4266. [Google Scholar] [CrossRef]
- Smith, K.; Crowe, S.R.; Garman, L.; Guthridge, C.J.; Muther, J.J.; McKee, E.; Zheng, N.Y.; Farris, A.D.; Guthridge, J.M.; Wilson, P.C.; et al. Human monoclonal antibodies generated following vaccination with AVA provide neutralization by blocking furin cleavage but not by preventing oligomerization. Vaccine 2012, 30, 4276–4283. [Google Scholar] [CrossRef]
- Reuveny, S.; White, M.D.; Adar, Y.Y.; Kafri, Y.; Altboum, Z.; Gozes, Y.; Kobiler, D.; Shafferman, A.; Velan, B. Search for correlates of protective immunity conferred by anthrax vaccine. Infect. Immun. 2001, 69, 2888–2893. [Google Scholar] [CrossRef]
- Crowe, S.R.; Ash, L.L.; Engler, R.J.; Ballard, J.D.; Harley, J.B.; Farris, A.D.; James, J.A. Select human anthrax protective antigen epitope-specific antibodies provide protection from lethal toxin challenge. J. Infect. Dis. 2010, 202, 251–260. [Google Scholar] [CrossRef]
- Quinn, C.P.; Sabourin, C.L.; Niemuth, N.A.; Li, H.; Semenova, V.A.; Rudge, T.L.; Mayfield, H.J.; Schiffer, J.; Mittler, R.S.; Ibegbu, C.C.; et al. A three-dose intramuscular injection schedule of anthrax vaccine adsorbed generates sustained humoral and cellular immune responses to protective antigen and provides long-term protection against inhalation anthrax in rhesus macaques. Clin. Vaccine Immunol. 2012, 19, 1730–1745. [Google Scholar] [CrossRef]
- McBride, B.W.; Mogg, A.; Telfer, J.L.; Lever, M.S.; Miller, J.; Turnbull, P.C.; Baillie, L. Protective efficacy of a recombinant protective antigen against Bacillus anthracis challenge and assessment of immunological markers. Vaccine 1998, 16, 810–817. [Google Scholar] [CrossRef]
- Williamson, E.D.; Beedham, R.J.; Bennett, A.M.; Perkins, S.D.; Miller, J.; Baillie, L.W. Presentation of protective antigen to the mouse immune system: Immune sequelae. J. Appl. Microbiol. 1999, 87, 315–317. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Qiu, J.; Zhou, Y.; Farhangfar, F.; Hester, J.; Lin, A.Y.; Decker, W.K. Plasmid-based vaccination with candidate anthrax vaccine antigens induces durable type 1 and type 2 T-helper immune responses. Vaccine 2008, 26, 614–622. [Google Scholar] [CrossRef] [PubMed]
- Doolan, D.L.; Freilich, D.A.; Brice, G.T.; Burgess, T.H.; Berzins, M.P.; Bull, R.L.; Graber, N.L.; Dabbs, J.L.; Shatney, L.L.; Blazes, D.L.; et al. The US capitol bioterrorism anthrax exposures: Clinical epidemiological and immunological characteristics. J. Infect. Dis. 2007, 195, 174–184. [Google Scholar] [CrossRef] [PubMed]
- Glomski, I.J.; Corre, J.P.; Mock, M.; Goossens, P.L. Cutting Edge: IFN-gamma-producing CD4 T lymphocytes mediate spore-induced immunity to capsulated Bacillus anthracis. J. Immunol. 2007, 178, 2646–2650. [Google Scholar] [CrossRef]
- Ingram, R.J.; Metan, G.; Maillere, B.; Doganay, M.; Ozkul, Y.; Kim, L.U.; Baillie, L.; Dyson, H.; Williamson, E.D.; Chu, K.K.; et al. Natural exposure to cutaneous anthrax gives long-lasting T cell immunity encompassing infection-specific epitopes. J. Immunol. 2010, 184, 3814–3821. [Google Scholar] [CrossRef]
- Ascough, S.; Ingram, R.J.; Chu, K.K.; Reynolds, C.J.; Musson, J.A.; Doganay, M.; Metan, G.; Ozkul, Y.; Baillie, L.; Sriskandan, S.; et al. Anthrax Lethal Factor as an Immune Target in Humans and Transgenic Mice and the Impact of HLA Polymorphism on CD4(+) T Cell Immunity. PLoS Pathog. 2014, 10, e1004085. [Google Scholar] [CrossRef]
- Ascough, S.; Ingram, R.J.; Abarra, A.; Holmes, A.J.; Maillere, B.; Altmann, D.M.; Boyton, R.J. Injectional anthrax infection due to heroin use induces strong immunological memory. J. Infect. 2014, 68, 200–203. [Google Scholar] [CrossRef]
- Nojima, M.; Ihara, H.; Kyo, M.; Hashimoto, M.; Ito, K.; Kunikata, S.; Nakatani, T.; Hayashi, R.; Ueda, H.; Ichikawa, Y.; et al. The significant effect of HLA-DRB1 matching on acute rejection in kidney transplants. Transpl. Int. 1996, 9 (Suppl. 1), S11–S15. [Google Scholar] [CrossRef]
- Ellmerich, S.; Takacs, K.; Mycko, M.; Waldner, H.; Wahid, F.; Boyton, R.J.; Smith, P.A.; Amor, S.; Baker, D.; Hafler, D.A.; et al. Disease-related epitope spread in a humanized T cell receptor transgenic model of multiple sclerosis. Eur. J. Immunol. 2004, 34, 1839–1848. [Google Scholar] [CrossRef]
- Ellmerich, S.; Mycko, M.; Takacs, K.; Waldner, H.; Wahid, F.N.; Boyton, R.J.; King, R.H.; Smith, P.A.; Amor, S.; Herlihy, A.H.; et al. High incidence of spontaneous disease in an HLA-DR15 and TCR transgenic multiple sclerosis model. J. Immunol. 2005, 174, 1938–1946. [Google Scholar] [CrossRef] [Green Version]
- Boyton, R.J.; Lohmann, T.; Londei, M.; Kalbacher, H.; Halder, T.; Frater, A.J.; Douek, D.C.; Leslie, D.G.; Flavell, R.A.; Altmann, D.M. Glutamic acid decarboxylase T lymphocyte responses associated with susceptibility or resistance to type I diabetes: Analysis in disease discordant human twins, non-obese diabetic mice and HLA-DQ transgenic mice. Int. Immunol. 1998, 10, 1765–1776. [Google Scholar] [CrossRef]
- Flick-Smith, H.C.; Walker, N.J.; Gibson, P.; Bullifent, H.; Hayward, S.; Miller, J.; Titball, R.W.; Williamson, E.D. A recombinant carboxy-terminal domain of the protective antigen of Bacillus anthracis protects mice against anthrax infection. Infect. Immun. 2002, 70, 1653–1656. [Google Scholar] [CrossRef] [PubMed]
- Texier, C.; Pouvelle, S.; Busson, M.; Herve, M.; Charron, D.; Menez, A.; Maillere, B. HLA-DR restricted peptide candidates for bee venom immunotherapy. J. Immunol. 2000, 164, 3177–3184. [Google Scholar] [CrossRef] [PubMed]
- Pancre, V.; Georges, B.; Angyalosi, G.; Castelli, F.; Delanoye, A.; Delacre, M.; Hachulla, E.; Maillere, B.; Bouzidi, A.; Auriault, C. Novel promiscuous HLA-DQ HIV Nef peptide that induces IFN-gamma-producing memory CD4+ T cells. Clin. Exp. Immunol. 2002, 129, 429–437. [Google Scholar] [CrossRef] [PubMed]
- Ascough, S.; Ingram, R.J.; Chu, K.K.; Musson, J.A.; Moore, S.J.; Gallagher, T.; Baillie, L.; Williamson, E.D.; Robinson, J.H.; Maillere, B.; et al. CD4+ T Cells Targeting Dominant and Cryptic Epitopes from Bacillus anthracis Lethal Factor. Front. Microbiol. 2015, 6, 1506. [Google Scholar] [CrossRef]
- Ingram, R.J.; Ascough, S.; Reynolds, C.J.; Metan, G.; Doganay, M.; Baillie, L.; Williamson, D.E.; Robinson, J.H.; Maillere, B.; Boyton, R.J.; et al. Natural cutaneous anthrax infection, but not vaccination, induces a CD4(+) T cell response involving diverse cytokines. Cell Biosci. 2015, 5, 20. [Google Scholar] [CrossRef]
- Petosa, C.; Collier, R.J.; Klimpel, K.R.; Leppla, S.H.; Liddington, R.C. Crystal structure of the anthrax toxin protective antigen. Nature 1997, 385, 833–838. [Google Scholar] [CrossRef]
- Ascough, S.; Altmann, D.M. Anthrax in injecting drug users: The need for increased vigilance in the clinic. Expert Rev. Anti Infect. Ther. 2015, 13, 681–684. [Google Scholar] [CrossRef]
- Laws, T.R.; Kuchuloria, T.; Chitadze, N.; Little, S.F.; Webster, W.M.; Debes, A.K.; Saginadze, S.; Tsertsvadze, N.; Chubinidze, M.; Rivard, R.G.; et al. A Comparison of the Adaptive Immune Response between Recovered Anthrax Patients and Individuals Receiving Three Different Anthrax Vaccines. PLoS ONE 2016, 11, e0148713. [Google Scholar] [CrossRef]
- Altmann, D.M. Host immunity to Bacillus anthracis lethal factor and other immunogens: Implications for vaccine design. Expert Rev. Vaccines 2015, 14, 429–434. [Google Scholar] [CrossRef]
- Williamson, E.D.; Hodgson, I.; Walker, N.J.; Topping, A.W.; Duchars, M.G.; Mott, J.M.; Estep, J.; Lebutt, C.; Flick-Smith, H.C.; Jones, H.E.; et al. Immunogenicity of recombinant protective antigen and efficacy against aerosol challenge with anthrax. Infect. Immun. 2005, 73, 5978–5987. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Schiffer, J.M.; Dalton, S.; Sabourin, C.L.; Niemuth, N.A.; Plikaytis, B.D.; Quinn, C.P. Comprehensive analysis and selection of anthrax vaccine adsorbed immune correlates of protection in rhesus macaques. Clin. Vaccine Immunol. 2014, 21, 1512–1520. [Google Scholar] [CrossRef] [PubMed]
- Glomski, I.J.; Piris-Gimenez, A.; Huerre, M.; Mock, M.; Goossens, P.L. Primary involvement of pharynx and peyer’s patch in inhalational and intestinal anthrax. PLoS Pathog. 2007, 3, e76. [Google Scholar] [CrossRef] [PubMed]
- Ingram, R.; Baillie, L. It’s in the genes! Human genetic diversity and the response to anthrax vaccines. Expert Rev. Vaccines 2012, 11, 633–635. [Google Scholar] [CrossRef] [PubMed]
- Garman, L.; Dumas, E.K.; Kurella, S.; Hunt, J.J.; Crowe, S.R.; Nguyen, M.L.; Cox, P.M.; James, J.A.; Farris, A.D. MHC class II and non-MHC class II genes differentially influence humoral immunity to Bacillus anthracis lethal factor and protective antigen. Toxins 2012, 4, 1451–1467. [Google Scholar] [CrossRef]
- Pajewski, N.M.; Parker, S.D.; Poland, G.A.; Ovsyannikova, I.G.; Song, W.; Zhang, K.; McKinney, B.A.; Pankratz, V.S.; Edberg, J.C.; Kimberly, R.P.; et al. The role of HLA-DR-DQ haplotypes in variable antibody responses to anthrax vaccine adsorbed. Genes. Immun. 2011, 12, 457–465. [Google Scholar] [CrossRef]
- Li, Z.K.; Nie, J.J.; Li, J.; Zhuang, H. The effect of HLA on immunological response to hepatitis B vaccine in healthy people: A meta-analysis. Vaccine 2013, 31, 4355–4361. [Google Scholar] [CrossRef]
- Posteraro, B.; Pastorino, R.; Di Giannantonio, P.; Ianuale, C.; Amore, R.; Ricciardi, W.; Boccia, S. The link between genetic variation and variability in vaccine responses: Systematic review and meta-analyses. Vaccine 2014, 32, 1661–1669. [Google Scholar] [CrossRef]
- Agrawal, A.; Lingappa, J.; Leppla, S.H.; Agrawal, S.; Jabbar, A.; Quinn, C.; Pulendran, B. Impairment of dendritic cells and adaptive immunity by anthrax lethal toxin. Nature 2003, 424, 329–334. [Google Scholar] [CrossRef]


| PA Peptide Sequence | HLA Transgenic Strain Responding to Epitope after PA Immunisation | Human Cohort Responding to Epitope (>20% Cohort Responding) | Relative Binding of HLA Class II | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| DR1 | DR3 | DR4 | DR7 | DR11 | DR13 | DR15 | DQ6 | DQ8 | |||
| 21GYYFSDLNFQAPMVVTSSTT40 | - | Vaccinee, Infected | 23 | 60 | 0.3 | 22 | 53 | >1908 | 118 | ND | ND |
| 31APMVVTSSTTGDLSIPSSEL50 | DR4 | - | ND | ND | ND | ND | ND | ND | ND | ND | ND |
| 41GDLSIPSSELENIPSENQYF60 | DR1 | Infected | 3312 | >728 | 46 | 424 | >1288 | >1288 | 134 | ND | ND |
| 51ENIPSENQYFQSAIWSGFIK70 | DR4 | Infected | 3 | 600 | 1 | 2 | 2 | >2733 | 55 | ND | ND |
| 61QSAIWSGFIKVKKSDEYTFA80 | - | Infected | 617 | 12 | 650 | 89 | 14 | 4 | 1 | ND | ND |
| 71VKKSDEYTFATSADNHVTMW90 | DR4 | Infected | 11 | 8 | 1 | 2 | 118 | >2733 | 45 | ND | ND |
| 91VDDQEVINKASNSNKIRLEK110 | - | Infected | 1333 | 283 | 992 | 36 | >1357 | 245 | 164 | ND | ND |
| 121QRENPTEKGLDFKLYWTDSQ140 | DR4 | Infected | >2563 | 800 | 6 | 1549 | >1357 | >2733 | 119 | ND | ND |
| 141NKKEVISSDNLQLPELKQKS160 | DQ8 | Infected | 131 | 26 | 48 | 28 | 849 | >2733 | 1 | >3054 | >166 |
| 148SDNLQLPELKQKSSNSRKKR167 | - | Infected | ND | ND | ND | ND | ND | ND | ND | ND | ND |
| 151LQLPELKQKSSNSRKKRSTS170 | DQ8 | Infected | >6667 | >667 | >1788 | >1543 | 701 | 177 | >511 | >3054 | >166 |
| 161SNSRKKRSTSAGPTVPDRDN180 | - | Infected | >6667 | >667 | >1788 | >1543 | >1336 | >1908 | >511 | ND | ND |
| 168STSAGPTVPDRDNDGIPDSL187 | - | Infected | >6667 | >667 | >1788 | >1543 | >1336 | >1908 | >511 | ND | ND |
| 171AGPTVPDRDNDGIPDSLEVE190 | - | Infected | 149 | 211 | 10 | 1167 | 7 | 51 | 95 | ND | ND |
| 191GYTVDVKNKRTFLSPWISNI210 | DQ8 | Infected | 216 | 0.2 | 190 | 11 | 231 | 0.5 | 15 | 2488 | >166 |
| 201TFLSPWISNIHEKKGLTKYK220 | DQ8 | - | 3162 | >667 | 1400 | 873 | 327 | 306 | 14 | 3077 | >166 |
| 221SSPEKWSTASDPYSDFEKVT240 | DR4 | - | ND | ND | ND | ND | ND | ND | ND | ND | ND |
| 241GRIDKNVSPEARHPLVAAYP260 | DQ8 | Vaccinee, Infected | 2828 | 15 | 55 | 833 | 567 | 9 | 9 | 899 | >166 |
| 261IVHVDMENIILSKNEDQSTQ280 | - | Infected | >6667 | >667 | 167 | >1543 | >1336 | >1908 | >511 | ND | ND |
| 281NTDSETRTISKNTSTSRTHT300 | - | Infected | >6667 | 23 | 179 | 707 | 535 | 60 | >511 | ND | ND |
| 301SEVHGNAEVHASFFDIGGSV320 | DQ8 | Vaccinee, Infected | >6667 | >667 | >1788 | 327 | >1336 | >1908 | >511 | 3 | 7 |
| 321SAGFSNSNSSTVAIDHSLSL340 | DR4 | Infected | 279 | 1 | 6 | 0.4 | 935 | >1908 | 95 | ND | ND |
| 331TVAIDHSLSLAGERTWAETM350 | DR4, DQ8 | Infected | 176 | 0.3 | 10 | 11 | 30 | 4 | 120 | 1056 | 0.1 |
| 361NANIRYVNTGTAPIYNVLPT380 | DR1 | Vaccinee, Infected | 15 | >728 | 0.4 | 1 | 12 | >1288 | 3 | ND | ND |
| 371TAPIYNVLPTTSLVLGKNQT390 | DR1, DR4 | Infected | 1 | 12 | 2 | 0.4 | 78 | 300 | 6 | ND | ND |
| 391LATIKAKENQLSQILAPNNY410 | - | Infected | 89 | 176 | 7 | 179 | 46 | 43 | 0.2 | ND | ND |
| 421LNAQDDFSSTPITMNYNQFL440 | - | Infected | >6667 | >667 | 1265 | 22 | >1336 | >1908 | 77 | ND | ND |
| 431PITMNYNQFLELEKTKQLRL450 | - | Vaccinee, Infected | 15 | 25 | 38 | 1 | 2 | 7 | 0.1 | ND | ND |
| 451DTDQVYGNIATYNFENGRVR470 | DR4 | Infected | 200 | >667 | 293 | 30 | >1336 | >1908 | 2 | ND | ND |
| 461TYNFENGRVRVDTGSNWSEV480 | DR4 | - | ND | ND | ND | ND | ND | ND | ND | ND | ND |
| 481LPQIQETTARIIFNGKDLNL500 | DQ8 | Infected | 2 | 5 | 886 | 0.3 | 37 | 2 | 1 | 240 | 6 |
| 491IIFNGKDLNLVERRIAAVNP510 | DQ8 | - | 3801 | 31 | 327 | 267 | 0.1 | 7 | 95 | 693 | 75 |
| 501VERRIAAVNPSDPLETTKPD520 | DQ8 | Vaccinee, Infected | 721 | 75 | 69 | 55 | >1288 | >1288 | 145 | 2506 | 29 |
| 511SDPLETTKPDMTLKEALKIA530 | - | Infected | 211 | 10 | 1800 | 401 | 1000 | 10 | 37 | ND | ND |
| 521MTLKEALKIAFGFNEPNGNL540 | - | Infected | 1155 | 18 | >1788 | 98 | 189 | 10 | 77 | ND | ND |
| 531FGFNEPNGNLQYQGKDITEF550 | - | Infected | >6667 | >667 | 207 | >1543 | 1134 | >1908 | 63 | ND | ND |
| 541QYQGKDITEFDFNFDQQTSQ560 | - | Infected | >2563 | 25 | 306 | >3365 | >1357 | >2733 | 44 | ND | ND |
| 551DFNFDQQTSQNIKNQLAELN570 | - | Infected | 249 | 82 | 239 | 267 | >1336 | 250 | 200 | ND | ND |
| 561NIKNQLAELNATNIYTVLDK580 | DR1 | - | 2 | >728 | 76 | 8 | 137 | 64 | 8 | ND | ND |
| 571ATNIYTVLDKIKLNAKMNIL590 | - | Infected | 31 | 5 | 278 | 19 | 0.5 | 3 | 11 | ND | ND |
| 581IKLNAKMNILIRDKRFHYDR600 | - | Infected | 2160 | 0.1 | 500 | 378 | 6 | 0 | 4 | ND | ND |
| 591IRDKRFHYDRNNIAVGADES610 | DR4, DQ8 | - | 25 | 1 | 0.2 | 4 | 4 | 25 | 2 | 1132 | 0.5 |
| 601NNIAVGADESVVKEAHREVI620 | DR4, DQ8 | - | 4989 | 10 | 1183 | 750 | 732 | 16 | 122 | 2191 | 6 |
| 621NSSTEGLLLNIDKDIRKILS640 | - | Infected | 2236 | 1 | 414 | 80 | 53 | 3 | 77 | ND | ND |
| 631IDKDIRKILSGYIVEIEDTE650 | DR1 | Infected | 5 | 775 | 510 | 1 | 72 | 1026 | 0.3 | ND | ND |
| 641GYIVEIEDTEGLKEVINDRY660 | DR4 | - | 3162 | 82 | 21 | 65 | 433 | 1333 | 0.1 | ND | ND |
| 651GLKEVINDRYDMLNISSLRQ670 | DQ8 | Infected | 7 | 10 | 6 | 22 | 46 | 15 | 6 | >3054 | 1 |
| 661DMLNISSLRQDGKTFIDFKK680 | - | Infected | 200 | 2 | 30 | 27 | 33 | 4 | 27 | ND | ND |
| 671DGKTFIDFKKYNDKLPLYIS690 | - | Vaccinee, Infected | 2494 | 100 | >1788 | 138 | 14 | 25 | 4 | ND | ND |
| 681YNDKLPLYISNPNYKVNVYA700 | DR1, DR4 | Infected | 1 | 4 | 1 | 2 | 2 | 30 | 1 | ND | ND |
| 691NPNYKVNVYAVTKENTIINP710 | - | Infected | 50 | 3 | 75 | 0.3 | 13 | 6 | 10 | ND | ND |
| 711SENGDTSTNGIKKILIFSKK730 | DR4, DQ8 | - | >6667 | >667 | >1788 | 133 | 3 | 217 | 3 | >3054 | >166 |
| 716TSTNGIKKILIFSKKGYEIG735 | DQ8 | - | 183 | 1 | 849 | 35 | 0.4 | 0.4 | 1 | >3054 | >166 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ascough, S.; Ingram, R.J.; Chu, K.K.Y.; Moore, S.J.; Gallagher, T.; Dyson, H.; Doganay, M.; Metan, G.; Ozkul, Y.; Baillie, L.; et al. Impact of HLA Polymorphism on the Immune Response to Bacillus Anthracis Protective Antigen in Vaccination versus Natural Infection. Vaccines 2022, 10, 1571. https://doi.org/10.3390/vaccines10101571
Ascough S, Ingram RJ, Chu KKY, Moore SJ, Gallagher T, Dyson H, Doganay M, Metan G, Ozkul Y, Baillie L, et al. Impact of HLA Polymorphism on the Immune Response to Bacillus Anthracis Protective Antigen in Vaccination versus Natural Infection. Vaccines. 2022; 10(10):1571. https://doi.org/10.3390/vaccines10101571
Chicago/Turabian StyleAscough, Stephanie, Rebecca J. Ingram, Karen K. Y. Chu, Stephen J. Moore, Theresa Gallagher, Hugh Dyson, Mehmet Doganay, Gökhan Metan, Yusuf Ozkul, Les Baillie, and et al. 2022. "Impact of HLA Polymorphism on the Immune Response to Bacillus Anthracis Protective Antigen in Vaccination versus Natural Infection" Vaccines 10, no. 10: 1571. https://doi.org/10.3390/vaccines10101571
APA StyleAscough, S., Ingram, R. J., Chu, K. K. Y., Moore, S. J., Gallagher, T., Dyson, H., Doganay, M., Metan, G., Ozkul, Y., Baillie, L., Williamson, E. D., Robinson, J. H., Maillere, B., Boyton, R. J., & Altmann, D. M. (2022). Impact of HLA Polymorphism on the Immune Response to Bacillus Anthracis Protective Antigen in Vaccination versus Natural Infection. Vaccines, 10(10), 1571. https://doi.org/10.3390/vaccines10101571





