Factors Influencing Decision Making Regarding the Acceptance of the COVID-19 Vaccination in Egypt: A Cross-Sectional Study in an Urban, Well-Educated Sample
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Setting and Population
2.2. Ethical Considerations
2.3. Study Tool
2.4. Sample Size and Sampling
2.5. Statistical Analysis
3. Results
3.1. Population Characteristics
3.2. Beliefs about the Vaccination among Study Participants
3.3. Predictors for Vaccine Acceptance among Population Characteristics
3.4. Correlation between Beliefs about the Vaccine and Acceptance towards Vaccination
3.5. Correlation between Population Characteristics and Acceptance towards Vaccination
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO Coronavirus (COVID-19) Dashboard, WHO Coronavirus (COVID-19) Dashboard with Vaccination Data. Available online: https://covid19.who.int/ (accessed on 24 September 2021).
- Helmy, Y.A.; Fawzy, M.; Elaswad, A.; Sobieh, A.; Kenney, S.P.; Shehata, A.A. The COVID-19 Pandemic: A Comprehensive Review of Taxonomy, Genetics, Epidemiology, Diagnosis, Treatment, and Control. J. Clin. Med. 2020, 9, 1225. [Google Scholar] [CrossRef] [PubMed]
- Wu, F.; Zhao, S.; Yu, B.; Chen, Y.M.; Wang, W.; Song, Z.G.; Hu, Y.; Tao, Z.W.; Tian, J.H.; Pei, Y.Y.; et al. A new coronavirus associated with human respiratory disease in China. Nature 2020, 579, 265–269. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cucinotta, D.; Vanelli, M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020, 91, 157–160. [Google Scholar] [CrossRef]
- COVID Live Update: 230,529,939 Cases and 4,725,868 Deaths from the Coronavirus—Worldometer. Available online: https://www.worldometers.info/coronavirus/ (accessed on 24 September 2021).
- Vakili, K.; Fathi, M.; Pezeshgi, A.; Mohamadkhani, A.; Hajiesmaeili, M.; Rezaei-Tavirani, M.; Sayehmiri, F. Critical complications of COVID-19: A descriptive meta-analysis study. Rev. Cardiovasc. Med. 2020, 21, 433–442. [Google Scholar] [CrossRef]
- Alvarado-Socarras, J.; Vesga-Varela, A.; Quintero-Lesmes, D.; Fama-Pereira, M.; Serrano-Diaz, N.; Vasco, M.; Carballo-Zarate, V.; Zambrano, L.; Paniz-Mondolfi, A.; Rodriguez-Morales, A. Perception of COVID-19 Vaccination Amongst Physicians in Colombia. Vaccines 2021, 9, 287. [Google Scholar] [CrossRef]
- Sheikh, N.S.; Touseef, M.; Sultan, R.; Cheema, K.H.; Cheema, S.S.; Sarwar, A.; Siddique, H.Z. Understanding COVID-19 vaccine hesitancy in Pakistan: The paradigm of Confidence, Convenience, and Complacency; A Cross-sectional study. medRxiv 2021. [Google Scholar] [CrossRef]
- Nicola, M.; Alsafi, Z.; Sohrabi, C.; Kerwan, A.; Al-Jabir, A.; Iosifidis, C.; Agha, M.; Agha, R. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. Int. J. Surg. 2020, 78, 185–193. [Google Scholar] [CrossRef] [PubMed]
- Kaddoura, M.; AlIbrahim, M.; Hijazi, G.; Soudani, N.; Audi, A.; Alkalamouni, H.; Haddad, S.; Eid, A.; Zaraket, H. COVID-19 Therapeutic Options Under Investigation. Front. Pharmacol. 2020, 11, 1196. [Google Scholar] [CrossRef]
- Hussein, I.E.; Echams, N.; Echams, S.; Sayegh, S.E.; Badran, R.; Eraad, M.; Egerges-Geagea, A.; Eleone, A.; Ejurjus, A. Vaccines Through Centuries: Major Cornerstones of Global Health. Front. Public Health 2015, 3, 269. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, C.; Plotkin, S.A. Impact of Vaccines; Health, Economic and Social Perspectives. Front. Microbiol. 2020, 11, 1526. [Google Scholar] [CrossRef] [PubMed]
- Ehreth, J. The value of vaccination: A global perspective. Vaccine 2003, 21, 4105–4117. [Google Scholar] [CrossRef]
- Omer, S.B.; Yildirim, I.; Forman, H.P. Herd Immunity and Implications for SARS-CoV-2 Control. JAMA 2020, 324, 2095. [Google Scholar] [CrossRef]
- Gong, W.; Aspatwar, A.; Wang, S.; Parkkila, S.; Wu, X. COVID-19 pandemic: SARS-CoV-2 specific vaccines and challenges, protection via BCG trained immunity, and clinical trials. Expert Rev. Vaccines 2021, 20, 857–880. [Google Scholar] [CrossRef] [PubMed]
- Fine, P.; Eames, K.; Heymann, D.L. “Herd Immunity”: A Rough Guide. Clin. Infect. Dis. 2011, 52, 911–916. [Google Scholar] [CrossRef] [PubMed]
- Neumann-Böhme, S.; Varghese, N.E.; Sabat, I.; Barros, P.P.; Brouwer, W.; Van Exel, J.; Schreyögg, J.; Stargardt, T. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur. J. Health Econ. 2020, 21, 977–982. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, N.E.; Sage Working Group on Vaccine Hesitancy. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- Schoch-Spana, M.; Brunson, E.K.; Long, R.; Ruth, A.; Ravi, S.J.; Trotochaud, M.; Borio, L.; Brewer, J.; Buccina, J.; Connell, N.; et al. The public’s role in COVID-19 vaccination: Human-centered recommendations to enhance pandemic vaccine awareness, access, and acceptance in the United States. Vaccine 2021, 39, 6004–6012. [Google Scholar] [CrossRef]
- French, J.; Deshpande, S.; Evans, W.; Obregon, R. Key Guidelines in Developing a Pre-Emptive COVID-19 Vaccination Uptake Promotion Strategy. Int. J. Environ. Res. Public Health 2020, 17, 5893. [Google Scholar] [CrossRef] [PubMed]
- Egypt: WHO Coronavirus Disease (COVID-19) Dashboard with Vaccination Data | WHO Coronavirus (COVID-19) Dashboard With Vaccination Data. Available online: https://covid19.who.int/region/emro/country/eg (accessed on 24 September 2021).
- Egypt: The Latest Coronavirus COUNTS, Charts and Maps. Available online: https://graphics.reuters.com/world-coronavirus-tracker-and-maps/countries-and-territories/egypt/ (accessed on 24 September 2021).
- Gallè, F.; Sabella, E.A.; Roma, P.; De Giglio, O.; Caggiano, G.; Tafuri, S.; Da Molin, G.; Ferracuti, S.; Montagna, M.T.; Liguori, G.; et al. Knowledge and Acceptance of COVID-19 Vaccination among Undergraduate Students from Central and Southern Italy. Vaccines 2021, 9, 638. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Jing, R.; Lai, X.; Zhang, H.; Lyu, Y.; Knoll, M.D.; Fang, H. Acceptance of COVID-19 Vaccination during the COVID-19 Pandemic in China. Vaccines 2020, 8, 482. [Google Scholar] [CrossRef] [PubMed]
- El-Sokkary, R.H.; El Seifi, O.S.; Hassan, H.M.; Mortada, E.M.; Hashem, M.K.; Gadelrab, M.R.M.A.; Tash, R.M.E. Predictors of COVID-19 vaccine hesitancy among Egyptian healthcare workers: A cross-sectional study. BMC Infect. Dis. 2021, 21, 762. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Ten Threats to Global Health in 2019. 2019. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 26 September 2021).
- Egypt Population (2021) Live—Countrymeters. Available online: https://countrymeters.info/en/Egypt (accessed on 27 October 2021).
- Egypt: Total Urban Population by Governorate 2021 | Statista. Available online: https://www.statista.com/statistics/1229861/urban-population-of-egypt-by-governorate/ (accessed on 27 October 2021).
- CAPMAS: Household Annual Income Increased to EGP 69000. Available online: https://see.news/capmas-household-annual-income-increased-to-egp-69000ll/ (accessed on 27 October 2021).
- Otu, A.; Osifo-Dawodu, E.; Atuhebwe, P.; Agogo, E.; Ebenso, B. Beyond vaccine hesitancy: Time for Africa to expand vaccine manufacturing capacity amidst growing COVID-19 vaccine nationalism. Lancet Microbe 2021, 2, e347–e348. [Google Scholar] [CrossRef]
- Omar, D.I.; Hani, B.M. Attitudes and intentions towards COVID-19 vaccines and associated factors among Egyptian adults. J. Infect. Public Health 2021, 14, 1481–1488. [Google Scholar] [CrossRef]
- Saied, S.M.; Saied, E.M.; Kabbash, I.A.; Abdo, S.A.E. Vaccine hesitancy: Beliefs and barriers associated with COVID-19 vaccination among Egyptian medical students. J. Med. Virol. 2021, 93, 4280–4291. [Google Scholar] [CrossRef] [PubMed]
- Fares, S.; Elmnyer, M.M.; Mohamed, S.S.; Elsayed, R. COVID-19 Vaccination Perception and Attitude among Healthcare Workers in Egypt. J. Prim. Care Community Health 2021, 12, 21501327211013303. [Google Scholar] [CrossRef]
- Malik, A.A.; McFadden, S.M.; Elharake, J.; Omer, S.B. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine 2020, 26, 100495. [Google Scholar] [CrossRef]
- Holzmann-Littig, C.; Braunisch, M.; Kranke, P.; Popp, M.; Seeber, C.; Fichtner, F.; Littig, B.; Carbajo-Lozoya, J.; Allwang, C.; Frank, T.; et al. COVID-19 Vaccination Acceptance and Hesitancy among Healthcare Workers in Germany. Vaccines 2021, 9, 777. [Google Scholar] [CrossRef] [PubMed]
- Elgendy, M.O.; Abdelrahim, M.E.A. Public awareness about coronavirus vaccine, vaccine acceptance, and hesitancy. J. Med. Virol. 2021, 93, 6535–6543. [Google Scholar] [CrossRef] [PubMed]
- Mohamed-Hussein, A.A.; Makhlouf, H.; Abd El Aal, H.; Kholief, K.; Saad, M.M.; Abdellal, D.A. A national survey of potential acceptance of COVID-19 vaccines in healthcare workers in Egypt. medRxiv 2021. [Google Scholar] [CrossRef]
- Qunaibi, E.; Basheti, I.; Soudy, M.; Sultan, I. Hesitancy of Arab Healthcare Workers towards COVID-19 Vaccination: A Large-Scale Multinational Study. Vaccines 2021, 9, 446. [Google Scholar] [CrossRef]
| Characteristic | No. | % |
|---|---|---|
| Age | 968 | |
| Mean ± SD | 29.11 ± 8.2 | |
| Age Groups | 968 | |
| Below 30 | 675 | 69.73 |
| 30–59 | 281 | 29.03 |
| Over 60 | 12 | 1.24 |
| Gender | 968 | |
| Male | 371 | 38.33 |
| Female | 597 | 61.67 |
| Residency | 968 | |
| Urban | 758 | 78.31 |
| Rural | 210 | 21.69 |
| Race | 968 | |
| Egyptian | 921 | 95.14 |
| Non Egyptian | 47 | 4.86 |
| Education | 968 | |
| Secondary or below | 31 | 3.20 |
| Post-Secondary | 494 | 51.03 |
| Tertiary | 443 | 45.76 |
| Occupation | 968 | |
| Unemployed | 94 | 9.71 |
| Part-time | 82 | 8.47 |
| Full time | 605 | 62.50 |
| Student | 187 | 19.32 |
| Marital status | 968 | |
| Single | 607 | 62.71 |
| With partner | 361 | 37.29 |
| Monthly Income | 968 | |
| Less than 5 k | 122 | 12.60 |
| 5–10 k | 332 | 34.30 |
| More than 10 k | 514 | 53.10 |
| Vaccine acceptance | ||
| I will accept the vaccine as soon as it becomes available | 318 | 32.8 |
| Delay vaccination until I have confirmed the safety of the vaccine | 650 | 67.2 |
| Question Item | No | Yes | ||
|---|---|---|---|---|
| No. | % | No. | % | |
| COVID-19 vaccination is an effective way to prevent and control COVID-19. | 302 | 31.20 | 666 | 68.80 |
| I would like to accept vaccination if the COVID-19 vaccine is successfully developed and approved for listing in the future. | 182 | 18.80 | 786 | 81.20 |
| Vaccine convenience (vaccination method, frequency, and distance to vaccination sites) is an important factor in vaccination decision making. | 140 | 14.46 | 828 | 85.54 |
| Doctor’s recommendation is an important factor in vaccination decision making. | 125 | 12.91 | 843 | 87.09 |
| Vaccine price is an important factor in vaccination decision making. | 245 | 25.31 | 723 | 74.69 |
| Characteristics | Hesitant | Accept | Unadjusted Analysis | Adjusted Analysis * | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | p | ORs | 95 | CI | p | ORs | 95 | CI | |
| Age Groups | 650 | 318 | ||||||||||
| Below 30 | 456 | 67.6 | 219 | 32.4 | Ref | |||||||
| 30–59 | 186 | 66.2 | 95 | 33.8 | 0.683 | 1.063 | 0.792 | 1.428 | 0.746 | 0.944 | 0.665 | 1.339 |
| Over 60 | 8 | 66.7 | 4 | 33.3 | 0.948 | 1.041 | 0.310 | 3.495 | 0.965 | 1.030 | 0.272 | 3.904 |
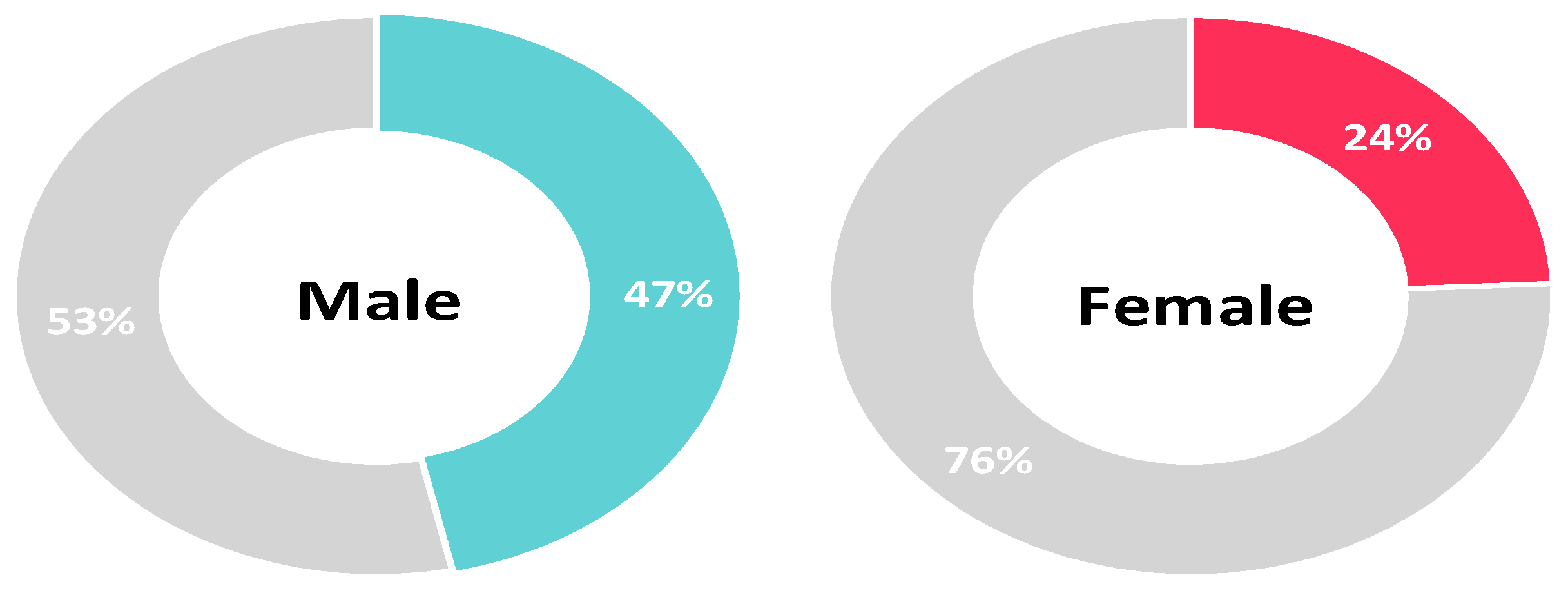
| Gender | 650 | 318 | ||||||||||
| Male | 198 | 53.4 | 173 | 46.6 | Ref | |||||||
| Female | 452 | 75.7 | 145 | 24.3 | <0.001 | 0.367 | 0.278 | 0.484 | <0.001 | 0.360 | 0.270 | 0.481 |
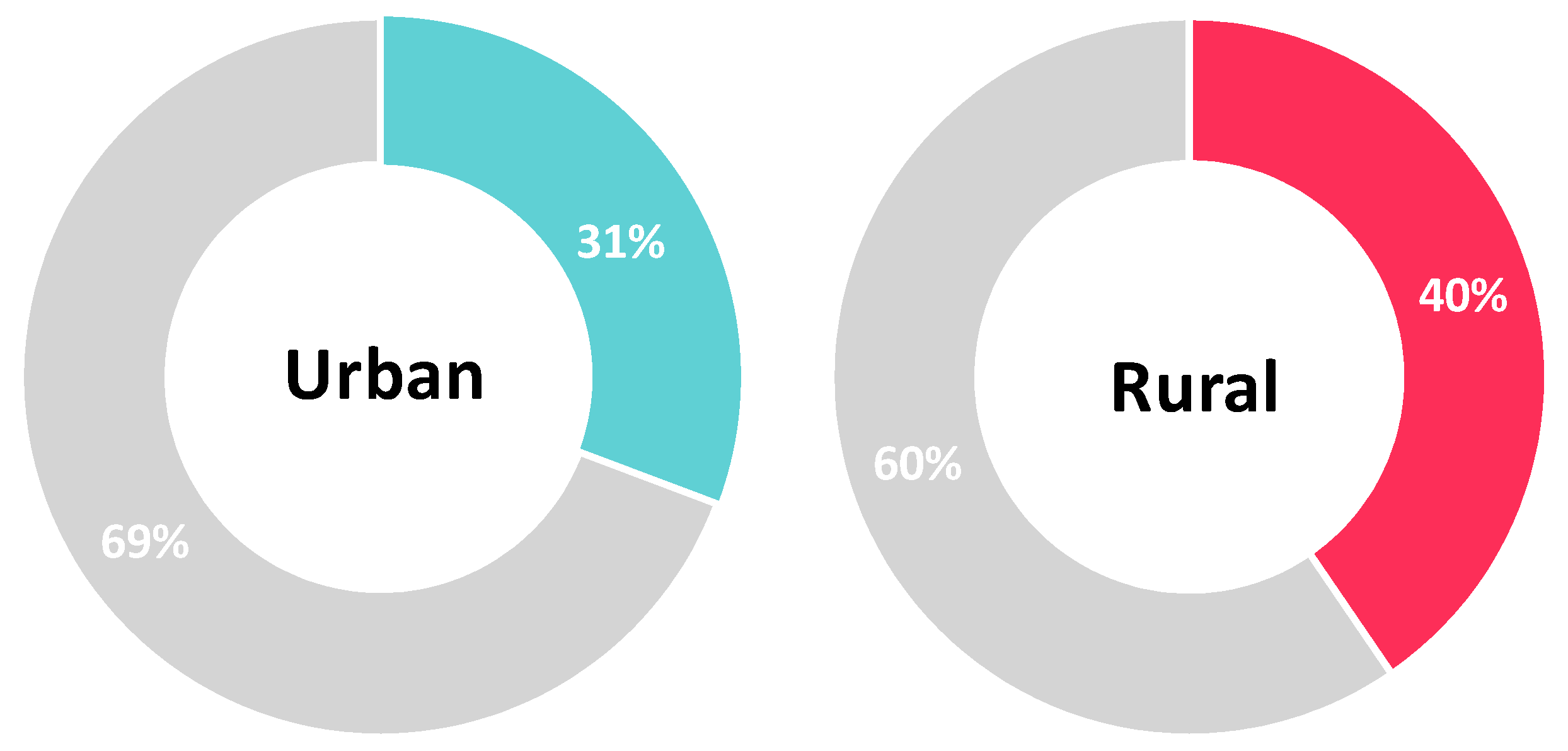
| Residency | 650 | 318 | ||||||||||
| Urban | 525 | 69.3 | 233 | 30.7 | Ref | |||||||
| Rural | 125 | 59.5 | 85 | 40.5 | 0.008 | 1.532 | 1.117 | 2.101 | 0.001 | 1.783 | 1.256 | 2.531 |
| Nationality | 650 | 318 | ||||||||||
| Egyptian | 621 | 67.4 | 300 | 32.6 | Ref | |||||||
| Non-Egyptian | 29 | 61.7 | 18 | 38.3 | 0.416 | 1.285 | 0.702 | 2.351 | 0.766 | 1.104 | 0.576 | 2.114 |
| Education | 650 | 318 | ||||||||||
| Secondary or below | 22 | 71 | 9 | 29.0 | Ref | |||||||
| Post-Secondary | 336 | 68 | 158 | 32.0 | 0.732 | 1.149 | 0.517 | 2.554 | 0.656 | 1.222 | 0.505 | 2.958 |
| Tertiary | 292 | 65.9 | 151 | 34.1 | 0.566 | 1.264 | 0.568 | 2.813 | 0.414 | 1.466 | 0.586 | 3.666 |
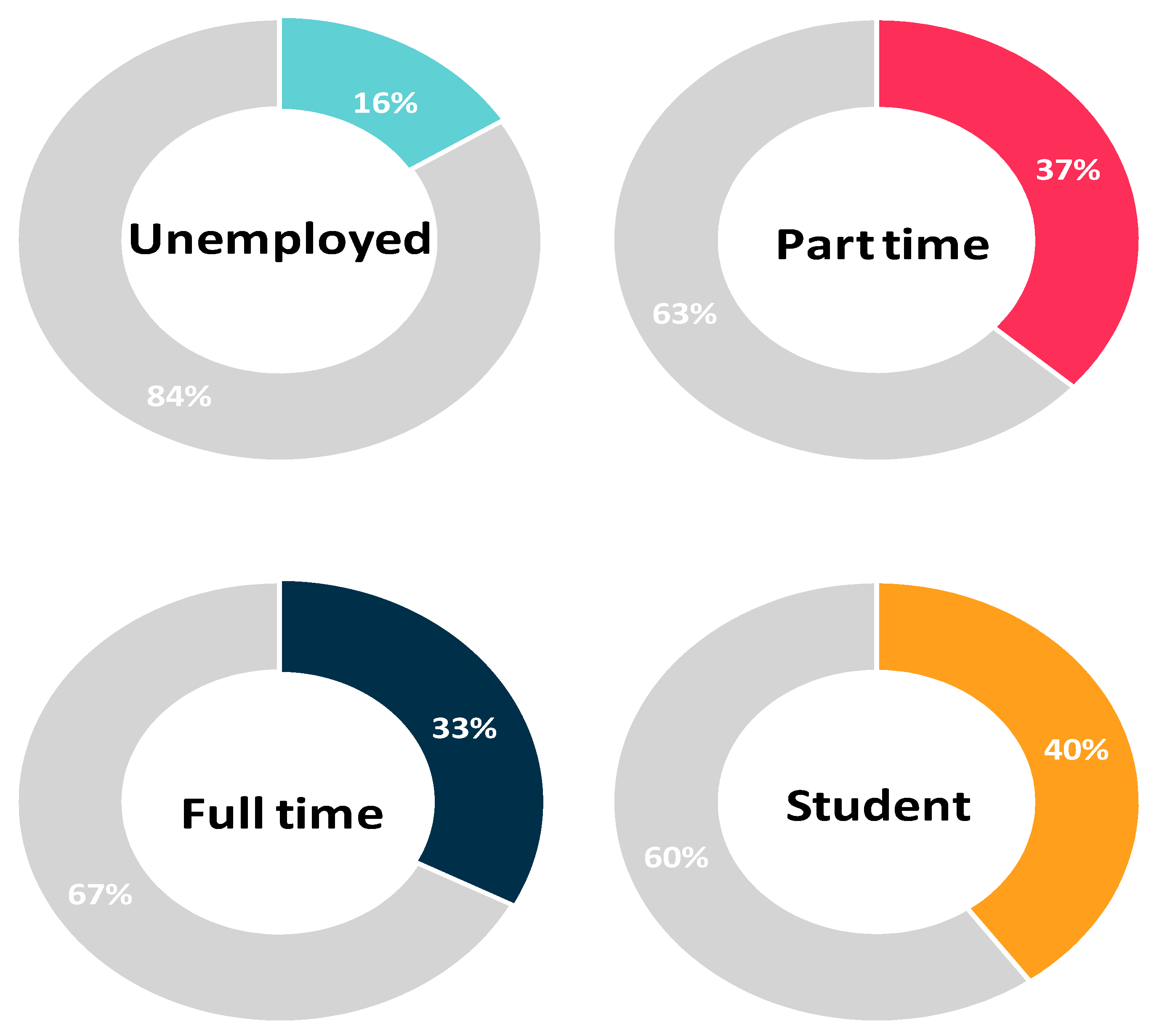
| Occupation | 650 | 318 | ||||||||||
| Unemployed | 79 | 84 | 15 | 16.0 | Ref | |||||||
| Part time | 52 | 63.4 | 30 | 36.6 | 0.002 | 3.038 | 1.491 | 6.191 | 0.015 | 2.535 | 1.202 | 5.343 |
| Full time | 407 | 67.3 | 198 | 32.7 | 0.001 | 2.562 | 1.438 | 4.565 | 0.033 | 1.951 | 1.056 | 3.604 |
| Student | 112 | 59.9 | 75 | 40.1 | <0.001 | 3.527 | 1.888 | 6.587 | <0.001 | 3.516 | 1.805 | 6.852 |
| Marital status | 650 | 318 | ||||||||||
| Single | 414 | 68.2 | 193 | 31.8 | Ref | |||||||
| With partner | 236 | 65.4 | 125 | 34.6 | 0.365 | 1.136 | 0.862 | 1.497 | 0.020 | 1.457 | 1.062 | 2.000 |
| Monthly Income | 650 | 318 | ||||||||||
| Less than 5k | 87 | 71.3 | 35 | 28.7 | Ref | |||||||
| 5k–10k | 222 | 66.9 | 110 | 33.1 | 0.368 | 1.232 | 0.782 | 1.939 | 0.130 | 1.466 | 0.894 | 2.404 |
| More than 10k | 341 | 67.6 | 173 | 33.7 | 0.294 | 1.261 | 0.818 | 1.944 | 0.075 | 1.553 | 0.956 | 2.522 |
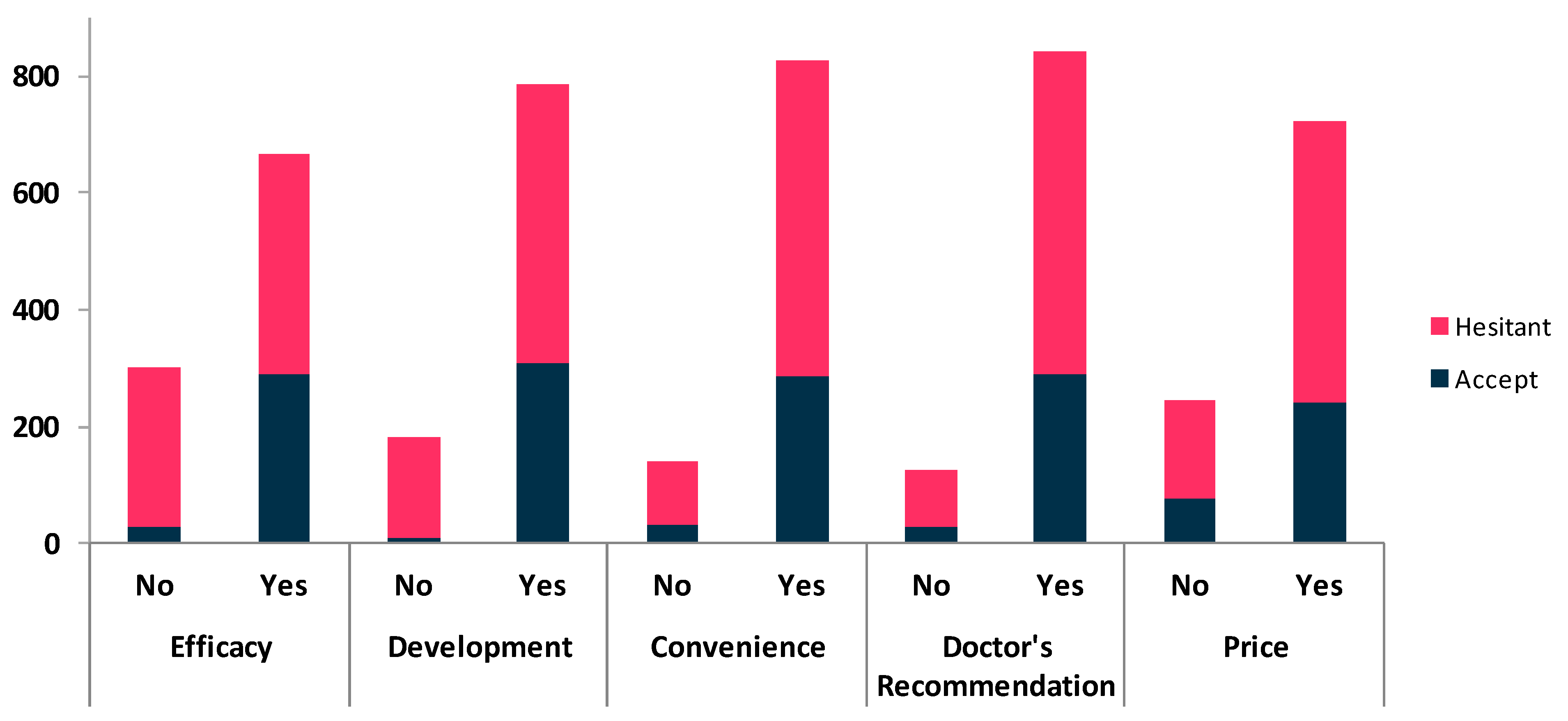
| Belief about Vaccine | Hesitant | Accept | Chi2 | p | Spearman’s r | p | ||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | |||||
| Efficacy | 650 | 318 | ||||||
| No | 272 | 90.1 | 30 | 9.9 | 104.508 | <0.001 | 0.309 | <0.001 |
| Yes | 378 | 56.8 | 288 | 43.2 | ||||
| Development | 650 | 318 | ||||||
| No | 171 | 94.0 | 11 | 6.0 | 73.02 | <0.001 | 0.277 | <0.001 |
| Yes | 479 | 60.9 | 307 | 39.1 | ||||
| Convenience | 650 | 318 | ||||||
| No | 107 | 76.4 | 33 | 23.6 | 6.389 | 0.011 | 0.078 | 0.016 |
| Yes | 543 | 65.6 | 285 | 34.4 | ||||
| Doctor’s Recommendation | 650 | 318 | ||||||
| No | 95 | 76.0 | 30 | 24.0 | 5.098 | 0.024 | 0.061 | 0.058 |
| Yes | 555 | 65.8 | 288 | 34.2 | ||||
| Price | 650 | 318 | ||||||
| No | 169 | 69.0 | 76 | 31.0 | 0.498 | 0.480 | 0.021 | 0.518 |
| Yes | 481 | 66.5 | 242 | 33.5 | ||||
| Characteristics | Hesitant | Accept | Chi2 | p | Spearman’s r | p | ||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | |||||
| Age Groups | 650 | 318 | ||||||
| Below 30 | 456 | 67.6 | 219 | 32.4 | 0.168 | 0.919 | 0.013 | 0.685 |
| 30–59 | 186 | 66.2 | 95 | 33.8 | ||||
| Over 60 | 8 | 66.7 | 4 | 33.3 | ||||
| Gender | 650 | 318 | ||||||
| Male | 198 | 53.4 | 173 | 46.6 | 51.779 | 0.000 | -0.231 | <0.001 |
| Female | 452 | 75.7 | 145 | 24.3 | ||||
| Residency | 650 | 318 | ||||||
| Urban | 525 | 69.3 | 233 | 30.7 | 7.068 | 0.008 | 0.085 | 0.008 |
| Rural | 125 | 59.5 | 85 | 40.5 | ||||
| Nationality | 650 | 318 | ||||||
| Egyptian | 621 | 67.4 | 300 | 32.6 | 0.664 | 0.415 | 0.026 | 0.416 |
| Non-Egyptian | 29 | 61.7 | 18 | 38.3 | ||||
| Education | 650 | 318 | ||||||
| Secondary or below | 22 | 71 | 9 | 29 | 0.68 | 0.712 | 0.026 | 0.424 |
| Post-Secondary | 336 | 68 | 158 | 32 | ||||
| Tertiary | 292 | 65.9 | 151 | 34.1 | ||||
| Occupation | 650 | 318 | ||||||
| Unemployed | 79 | 84 | 15 | 16 | 17.147 | 0.001 | 0.102 | 0.002 |
| Part time | 52 | 63.4 | 30 | 36.6 | ||||
| Full time | 407 | 67.3 | 198 | 32.7 | ||||
| Student | 112 | 59.9 | 75 | 40.1 | ||||
| Marital status | 650 | 318 | ||||||
| Single | 414 | 68.2 | 193 | 31.8 | 0.822 | 0.365 | 0.029 | 0.365 |
| With partner | 236 | 65.4 | 125 | 34.6 | ||||
| Monthly Income | 650 | 318 | ||||||
| Less than 5k | 87 | 71.3 | 35 | 28.7 | 1.122 | 0.571 | 0.025 | 0.429 |
| 5k–10k | 222 | 66.9 | 110 | 33.1 | ||||
| More than 10k | 341 | 67.6 | 173 | 33.7 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Elsayed, M.; El-Abasiri, R.A.; Dardeer, K.T.; Kamal, M.A.; Htay, M.N.N.; Abler, B.; Marzo, R.R. Factors Influencing Decision Making Regarding the Acceptance of the COVID-19 Vaccination in Egypt: A Cross-Sectional Study in an Urban, Well-Educated Sample. Vaccines 2022, 10, 20. https://doi.org/10.3390/vaccines10010020
Elsayed M, El-Abasiri RA, Dardeer KT, Kamal MA, Htay MNN, Abler B, Marzo RR. Factors Influencing Decision Making Regarding the Acceptance of the COVID-19 Vaccination in Egypt: A Cross-Sectional Study in an Urban, Well-Educated Sample. Vaccines. 2022; 10(1):20. https://doi.org/10.3390/vaccines10010020
Chicago/Turabian StyleElsayed, Mohamed, Radwa Abdullah El-Abasiri, Khaled T. Dardeer, Manar Ahmed Kamal, Mila Nu Nu Htay, Birgit Abler, and Roy Rillera Marzo. 2022. "Factors Influencing Decision Making Regarding the Acceptance of the COVID-19 Vaccination in Egypt: A Cross-Sectional Study in an Urban, Well-Educated Sample" Vaccines 10, no. 1: 20. https://doi.org/10.3390/vaccines10010020
APA StyleElsayed, M., El-Abasiri, R. A., Dardeer, K. T., Kamal, M. A., Htay, M. N. N., Abler, B., & Marzo, R. R. (2022). Factors Influencing Decision Making Regarding the Acceptance of the COVID-19 Vaccination in Egypt: A Cross-Sectional Study in an Urban, Well-Educated Sample. Vaccines, 10(1), 20. https://doi.org/10.3390/vaccines10010020








