Therapeutic Potential of Palmitoylethanolamide in Gastrointestinal Disorders
Abstract
1. Introduction
2. Therapeutic Effects of Palmitoylethanolamide (PEA)
2.1. The Endocannabinoid System
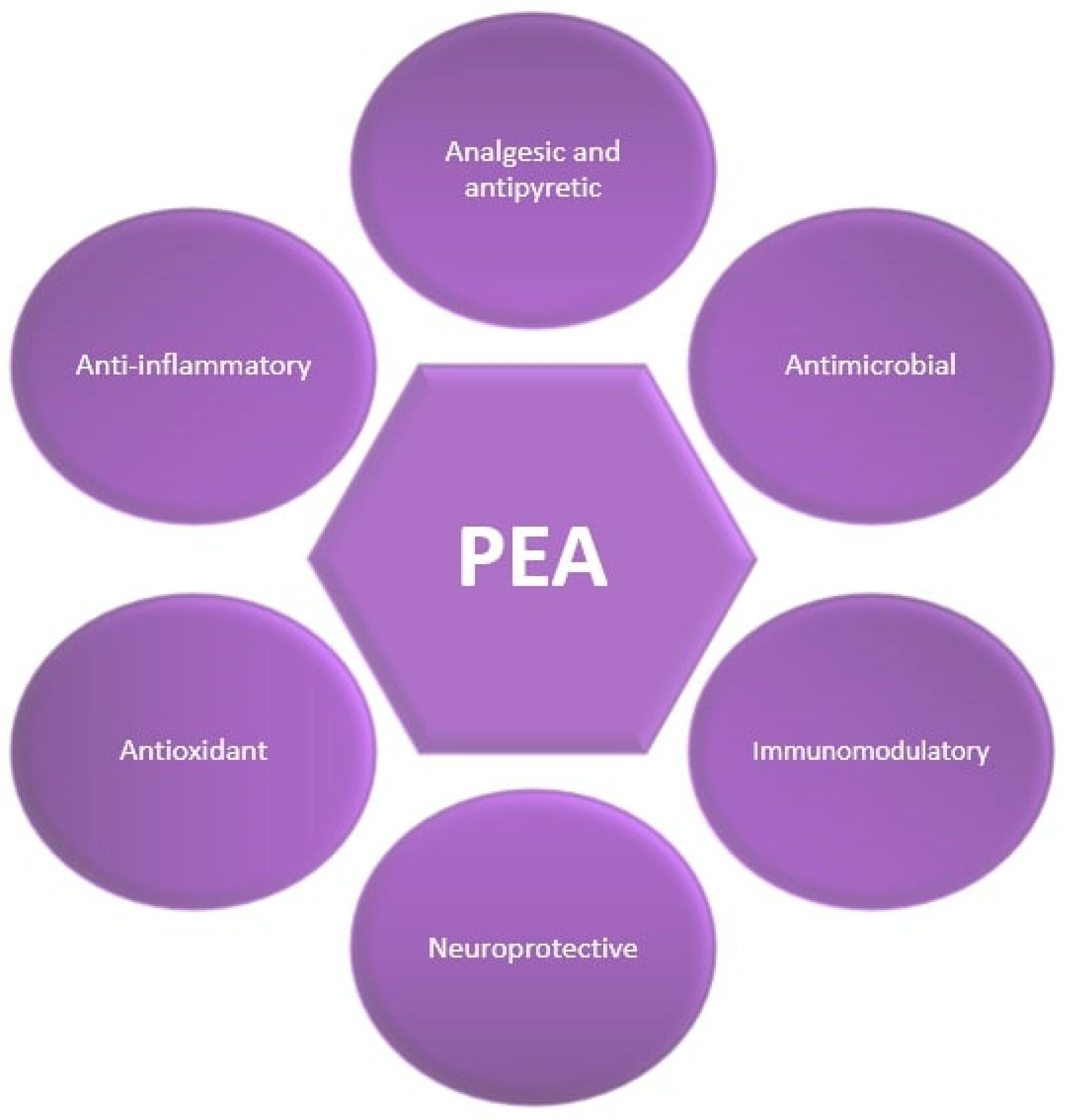
2.2. Palmitoylethanolamide’s (PEA’s) Pharmacological Profile
2.3. Palmitoylethanolamide’s (PEA’s) Mechanisms of Action
2.3.1. Pain Management
2.3.2. Anti-Inflammatory Effects
2.3.3. Antioxidant Effects
3. Therapeutic Potential of Palmitoylethanolamide (PEA) in Gastrointestinal Disorders
3.1. The Role of Palmitoylethanolamide (PEA) in Irritable Bowel Syndrome (IBS)
3.2. The Role of Palmitoylethanolamide (PEA) in Inflammatory Bowel Diseases (IBD)
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Clayton, P.; Hill, M.; Bogoda, N.; Subah, S.; Venkatesh, R. Palmitoylethanolamide: A Natural Compound for Health Management. Int. J. Mol. Sci. 2021, 22, 5305. [Google Scholar] [CrossRef] [PubMed]
- Rooks, M.G.; Garrett, W.S. Gut Microbiota, Metabolites and Host Immunity. Nat. Rev. Immunol. 2016, 16, 341–352. [Google Scholar] [CrossRef] [PubMed]
- Sharon, G.; Sampson, T.R.; Geschwind, D.H.; Mazmanian, S.K. The Central Nervous System and the Gut Microbiome. Cell 2016, 167, 915–932. [Google Scholar] [CrossRef] [PubMed]
- van der Flier, L.G.; Clevers, H. Stem Cells, Self-Renewal, and Differentiation in the Intestinal Epithelium. Annu. Rev. Physiol. 2009, 71, 241–260. [Google Scholar] [CrossRef] [PubMed]
- Peterson, L.W.; Artis, D. Intestinal Epithelial Cells: Regulators of Barrier Function and Immune Homeostasis. Nat. Rev. Immunol. 2014, 14, 141–153. [Google Scholar] [CrossRef] [PubMed]
- de Punder, K.; Pruimboom, L. Stress Induces Endotoxemia and Low-Grade Inflammation by Increasing Barrier Permeability. Front. Immunol. 2015, 6, 223. [Google Scholar] [CrossRef]
- Couch, D.G.; Tasker, C.; Theophilidou, E.; Lund, J.N.; O’Sullivan, S.E. Cannabidiol and Palmitoylethanolamide Are Anti-Inflammatory in the Acutely Inflamed Human Colon. Clin. Sci. 2017, 131, 2611–2626. [Google Scholar] [CrossRef] [PubMed]
- Raso, G.M.; Russo, R.; Calignano, A.; Meli, R. Palmitoylethanolamide in CNS Health and Disease. Pharmacol. Res. 2014, 86, 32–41. [Google Scholar] [CrossRef]
- Kiani, A.K.; Bonetti, G.; Donato, K.; Bertelli, M. Dietary Supplements for Intestinal Inflammation. J. Prev. Med. Hyg. 2022, 63 (Suppl. 3), E214–E220. [Google Scholar] [CrossRef]
- Iannotti, F.A.; Di Marzo, V.; Petrosino, S. Endocannabinoids and Endocannabinoid-Related Mediators: Targets, Metabolism and Role in Neurological Disorders. Prog. Lipid Res. 2016, 62, 107–128. [Google Scholar] [CrossRef]
- Zolese, G.; Bacchetti, T.; Masciangelo, S.; Ragni, L.; Ambrosi, S.; Ambrosini, A.; Marini, M.; Ferretti, G. Effect of Acylethanolamides on Lipid Peroxidation and Paraoxonase Activity. Biofactors 2008, 33, 201–209. [Google Scholar] [CrossRef] [PubMed]
- Rankin, L.; Fowler, C.J. The Basal Pharmacology of Palmitoylethanolamide. Int. J. Mol. Sci. 2020, 21, 7942. [Google Scholar] [CrossRef] [PubMed]
- Keppel Hesselink, J.M. The Terms “Autacoid”, “hormone” and “Chalone” and How They Have Shifted with Time. Aut. Autacoid Pharmacol. 2015, 35, 51–58. [Google Scholar] [CrossRef] [PubMed]
- Kuehl, F.A., Jr.; Jacob, T.A.; Ganley, O.H.; Ormond, R.E.; Meisinger, M.A.P. The Identification of N-(2-Hydroxyethyl)-Palmitamide as a Naturally Occurring Anti-Inflammatory Agent. J. Am. Chem. 1957, 79, 5577–5578. [Google Scholar] [CrossRef]
- Coburn, A.F.; Moore, L.V. Nutrition as a Conditioning Factor in the Rheumatic State. Am. J. Dis. Child. 1943, 65, 744–756. [Google Scholar] [CrossRef]
- Coburn, A.F.; Graham, C.E.; Haninger, J. The Effect of Egg Yolk in Diets on Anaphylactic Arthritis (Passive Arthus Phenomenon) in the Guinea Pig. J. Exp. Med. 1954, 100, 425–435. [Google Scholar] [CrossRef]
- Heidari, A.; Rostam-Abadi, Y.; Rezaei, N. The Immune System and Autism Spectrum Disorder: Association and Therapeutic Challenges. Acta Neurobiol. Exp. 2021, 81, 249–263. [Google Scholar] [CrossRef]
- Ochoa-Cortes, F.; Turco, F.; Linan-Rico, A.; Soghomonyan, S.; Whitaker, E.; Wehner, S.; Cuomo, R.; Christofi, F.L. Enteric Glial Cells: A New Frontier in Neurogastroenterology and Clinical Target for Inflammatory Bowel Diseases. Inflamm. Bowel Dis. 2016, 22, 433–449. [Google Scholar] [CrossRef] [PubMed]
- Darmani, N.A.; Izzo, A.A.; Degenhardt, B.; Valenti, M.; Scaglione, G.; Capasso, R.; Sorrentini, I.; Di Marzo, V. Involvement of the Cannabimimetic Compound, N-Palmitoyl-Ethanolamine, in Inflammatory and Neuropathic Conditions: Review of the Available Pre-Clinical Data, and First Human Studies. Neuropharmacology 2005, 48, 1154–1163. [Google Scholar] [CrossRef]
- Lombardi, G.; Miglio, G.; Varsaldi, F.; Minassi, A.; Appendino, G. Oxyhomologation of the Amide Bond Potentiates Neuroprotective Effects of the Endolipid N-Palmitoylethanolamine. J. Pharmacol. Exp. Ther. 2007, 320, 599–606. [Google Scholar] [CrossRef]
- Zolese, G.; Bacchetti, T.; Ambrosini, A.; Wozniak, M.; Bertoli, E.; Ferretti, G. Increased Plasma Concentrations of Palmitoylethanolamide, an Endogenous Fatty Acid Amide, Affect Oxidative Damage of Human Low-Density Lipoproteins: An in Vitro Study. Atherosclerosis 2005, 182, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Pirozzi, C.; Coretti, L.; Opallo, N.; Bove, M.; Annunziata, C.; Comella, F.; Turco, L.; Lama, A.; Trabace, L.; Meli, R.; et al. Palmitoylethanolamide Counteracts High-Fat Diet-Induced Gut Dysfunction by Reprogramming Microbiota Composition and Affecting Tryptophan Metabolism. Front. Nutr. 2023, 10, 1143004. [Google Scholar] [CrossRef] [PubMed]
- Esposito, G.; Pesce, M.; Seguella, L.; Lu, J.; Corpetti, C.; Del Re, A.; De Palma, F.D.E.; Esposito, G.; Sanseverino, W.; Sarnelli, G. Engineered Lactobacillus Paracasei Producing Palmitoylethanolamide (PEA) Prevents Colitis in Mice. Int. J. Mol. Sci. 2021, 22, 2945. [Google Scholar] [CrossRef] [PubMed]
- Esposito, G.; Capoccia, E.; Turco, F.; Palumbo, I.; Lu, J.; Steardo, A.; Cuomo, R.; Sarnelli, G.; Steardo, L. Palmitoylethanolamide Improves Colon Inflammation through an Enteric Glia/Toll like Receptor 4-Dependent PPAR-α Activation. Gut 2014, 63, 1300–1312. [Google Scholar] [CrossRef] [PubMed]
- Azuma, Y.-T.; Nishiyama, K.; Matsuo, Y.; Kuwamura, M.; Morioka, A.; Nakajima, H.; Takeuchi, T. PPARα Contributes to Colonic Protection in Mice with DSS-Induced Colitis. Int. Immunopharmacol. 2010, 10, 1261–1267. [Google Scholar] [CrossRef] [PubMed]
- D’Argenio, G.; Petrosino, S.; Gianfrani, C.; Valenti, M.; Scaglione, G.; Grandone, I.; Nigam, S.; Sorrentini, I.; Mazzarella, G.; Di Marzo, V. Overactivity of the Intestinal Endocannabinoid System in Celiac Disease and in Methotrexate-Treated Rats. J. Mol. Med. 2007, 85, 523–530. [Google Scholar] [CrossRef] [PubMed]
- Dömötör, A.; Peidl, Z.; Vincze, A.; Hunyady, B.; Szolcsányi, J.; Kereskay, L.; Szekeres, G.; Mózsik, G. Immunohistochemical Distribution of Vanilloid Receptor, Calcitonin-Gene Related Peptide and Substance P in Gastrointestinal Mucosa of Patients with Different Gastrointestinal Disorders. Inflammopharmacology 2005, 13, 161–177. [Google Scholar] [CrossRef]
- Cuzzocrea, S.; Di Paola, R.; Mazzon, E.; Genovese, T.; Muià, C.; Centorrino, T.; Caputi, A.P. Role of Endogenous and Exogenous Ligands for the Peroxisome Proliferators Activated Receptors Alpha (PPAR-Alpha) in the Development of Inflammatory Bowel Disease in Mice. Lab. Investig. 2004, 84, 1643–1654. [Google Scholar] [CrossRef]
- Kimball, E.S.; Wallace, N.H.; Schneider, C.R.; D’Andrea, M.R.; Hornby, P.J. Vanilloid Receptor 1 Antagonists Attenuate Disease Severity in Dextran Sulphate Sodium-Induced Colitis in Mice. Neurogastroenterol. Motil. 2004, 16, 811–818. [Google Scholar] [CrossRef]
- Capasso, R.; Izzo, A.A.; Fezza, F.; Pinto, A.; Capasso, F.; Mascolo, N.; Di Marzo, V. Inhibitory Effect of Palmitoylethanolamide on Gastrointestinal Motility in Mice. Br. J. Pharmacol. 2001, 134, 945–950. [Google Scholar] [CrossRef]
- Di Nardo, G.; Bernardo, L.; Cremon, C.; Barbara, G.; Felici, E.; Evangelisti, M.; Ferretti, A.; Furio, S.; Piccirillo, M.; Coluzzi, F.; et al. Palmitoylethanolamide and Polydatin in Pediatric Irritable Bowel Syndrome: A Multicentric Randomized Controlled Trial. Nutrition 2024, 122, 112397. [Google Scholar] [CrossRef] [PubMed]
- Couch, D.G.; Cook, H.; Ortori, C.; Barrett, D.; Lund, J.N.; O’Sullivan, S.E. Palmitoylethanolamide and Cannabidiol Prevent Inflammation-Induced Hyperpermeability of the Human Gut In Vitro and In Vivo-A Randomized, Placebo-Controlled, Double-Blind Controlled Trial. Inflamm. Bowel Dis. 2019, 25, 1006–1018. [Google Scholar] [CrossRef]
- Cremon, C.; Stanghellini, V.; Barbaro, M.R.; Cogliandro, R.F.; Bellacosa, L.; Santos, J.; Vicario, M.; Pigrau, M.; Alonso Cotoner, C.; Lobo, B.; et al. Randomised Clinical Trial: The Analgesic Properties of Dietary Supplementation with Palmitoylethanolamide and Polydatin in Irritable Bowel Syndrome. Aliment. Pharmacol. Ther. 2017, 45, 909–922. [Google Scholar] [CrossRef] [PubMed]
- Fichna, J.; Wood, J.T.; Papanastasiou, M.; Vadivel, S.K.; Oprocha, P.; Sałaga, M.; Sobczak, M.; Mokrowiecka, A.; Cygankiewicz, A.I.; Zakrzewski, P.K.; et al. Endocannabinoid and Cannabinoid-like Fatty Acid Amide Levels Correlate with Pain-Related Symptoms in Patients with IBS-D and IBS-C: A Pilot Study. PLoS ONE 2013, 8, e85073. [Google Scholar] [CrossRef] [PubMed]
- Mechoulam, R.; Fride, E.; Di Marzo, V. Endocannabinoids. Eur. J. Pharmacol. 1998, 359, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Matsuda, L.A.; Lolait, S.J.; Brownstein, M.J.; Young, A.C.; Bonner, T.I. Structure of a Cannabinoid Receptor and Functional Expression of the Cloned CDNA. Nature 1990, 346, 561–564. [Google Scholar] [CrossRef] [PubMed]
- Cascio, M.G. PUFA-Derived Endocannabinoids: An Overview. Proc. Nutr. Soc. 2013, 72, 451–459. [Google Scholar] [CrossRef] [PubMed]
- Di Marzo, V.; Bifulco, M.; De Petrocellis, L. The Endocannabinoid System and Its Therapeutic Exploitation. Nat. Rev. Drug Discov. 2004, 3, 771–784. [Google Scholar] [CrossRef] [PubMed]
- Yang, F.; Zheng, J. Understand Spiciness: Mechanism of TRPV1 Channel Activation by Capsaicin. Protein Cell 2017, 8, 169–177. [Google Scholar] [CrossRef]
- O’Sullivan, S.E. An Update on PPAR Activation by Cannabinoids. Br. J. Pharmacol. 2016, 173, 1899–1910. [Google Scholar] [CrossRef]
- Howlett, A.C.; Barth, F.; Bonner, T.I.; Cabral, G.; Casellas, P.; Devane, W.A.; Felder, C.C.; Herkenham, M.; Mackie, K.; Martin, B.R.; et al. International Union of Pharmacology. XXVII. Classification of Cannabinoid Receptors. Pharmacol. Rev. 2002, 54, 161–202. [Google Scholar] [CrossRef] [PubMed]
- de Sá, M.C.I.; Castor, M.G.M. Therapeutic Use of Palmitoylethanolamide as an Anti-Inflammatory and Immunomodulator. Future Pharmacol. 2023, 3, 951–977. [Google Scholar] [CrossRef]
- Montell, C. Physiology, Phylogeny, and Functions of the TRP Superfamily of Cation Channels. Sci. STKE 2001, 2001, re1. [Google Scholar] [CrossRef] [PubMed]
- Gunthorpe, M.J.; Benham, C.D.; Randall, A.; Davis, J.B. The Diversity in the Vanilloid (TRPV) Receptor Family of Ion Channels. Trends Pharmacol. Sci. 2002, 23, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Brown, A.J. Novel Cannabinoid Receptors. Br. J. Pharmacol. 2007, 152, 567–575. [Google Scholar] [CrossRef] [PubMed]
- Holzer, P. TRPV1 and the Gut: From a Tasty Receptor for a Painful Vanilloid to a Key Player in Hyperalgesia. Eur. J. Pharmacol. 2004, 500, 231–241. [Google Scholar] [CrossRef] [PubMed]
- Grygiel-Górniak, B. Peroxisome Proliferator-Activated Receptors and Their Ligands: Nutritional and Clinical Implications—A Review. Nutr. J. 2014, 13, 17. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, S.E.; Kendall, D.A. Cannabinoid Activation of Peroxisome Proliferator-Activated Receptors: Potential for Modulation of Inflammatory Disease. Immunobiology 2010, 215, 611–616. [Google Scholar] [CrossRef] [PubMed]
- Delerive, P.; Fruchart, J.C.; Staels, B. Peroxisome Proliferator-Activated Receptors in Inflammation Control. J. Endocrinol. 2001, 169, 453–459. [Google Scholar] [CrossRef]
- Devchand, P.R.; Keller, H.; Peters, J.M.; Vazquez, M.; Gonzalez, F.J.; Wahli, W. The PPARalpha-Leukotriene B4 Pathway to Inflammation Control. Nature 1996, 384, 39–43. [Google Scholar] [CrossRef]
- Grabacka, M.; Pierzchalska, M.; Płonka, P.M.; Pierzchalski, P. The Role of PPAR Alpha in the Modulation of Innate Immunity. Int. J. Mol. Sci. 2021, 22, 10545. [Google Scholar] [CrossRef] [PubMed]
- Delerive, P.; Gervois, P.; Fruchart, J.C.; Staels, B. Induction of IkappaBalpha Expression as a Mechanism Contributing to the Anti-Inflammatory Activities of Peroxisome Proliferator-Activated Receptor-Alpha Activators. J. Biol. Chem. 2000, 275, 36703–36707. [Google Scholar] [CrossRef] [PubMed]
- Calebiro, D.; Godbole, A. Internalization of G-Protein-Coupled Receptors: Implication in Receptor Function, Physiology and Diseases. Best Pr. Res. Clin. Endocrinol. Metab. 2018, 32, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Godlewski, G.; Offertáler, L.; Wagner, J.A.; Kunos, G. Receptors for Acylethanolamides-GPR55 and GPR119. Prostaglandins Other Lipid Mediat. 2009, 89, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Ryberg, E.; Sjögren, N.L.S.; Hjorth, S.; Hermansson, N.-O.; Leonova, J.; Elebring, T.; Nilsson, K.; Drmota, T.; Greasley, P.J. The Orphan Receptor GPR55 Is a Novel Cannabinoid Receptor. Br. J. Pharmacol. 2007, 152, 1092–1101. [Google Scholar] [CrossRef] [PubMed]
- Pertwee, R.G. Endocannabinoids and Their Pharmacological Actions. Handb. Exp. Pharmacol. 2015, 231, 1–37. [Google Scholar] [CrossRef]
- Okamoto, Y.; Morishita, J.; Tsuboi, K.; Tonai, T.; Ueda, N. Molecular Characterization of a Phospholipase D Generating Anandamide and Its Congeners. J. Biol. Chem. 2004, 279, 5298–5305. [Google Scholar] [CrossRef]
- Cravatt, B.F.; Giang, D.K.; Mayfield, S.P.; Boger, D.L.; Lerner, R.A.; Gilula, N.B. Molecular Characterization of an Enzyme That Degrades Neuromodulatory Fatty-Acid Amides. Nature 1996, 384, 83–87. [Google Scholar] [CrossRef]
- Lambert, D.M.; Vandevoorde, S.; Jonsson, K.-O.; Fowler, C.J. The Palmitoylethanolamide Family: A New Class of Anti-Inflammatory Agents? Curr. Med. Chem. 2002, 9, 663–674. [Google Scholar] [CrossRef]
- Borrelli, F.; Romano, B.; Petrosino, S.; Pagano, E.; Capasso, R.; Coppola, D.; Battista, G.; Orlando, P.; Di Marzo, V.; Izzo, A.A. Palmitoylethanolamide, a Naturally Occurring Lipid, Is an Orally Effective Intestinal Anti-Inflammatory Agent. Br. J. Pharmacol. 2015, 172, 142–158. [Google Scholar] [CrossRef]
- Clayton, P.; Subah, S.; Venkatesh, R.; Hill, M.; Bogoda, N. Palmitoylethanolamide: A Potential Alternative to Cannabidiol. J. Diet. Suppl. 2023, 20, 505–530. [Google Scholar] [CrossRef] [PubMed]
- Zhukov, O.D. Distribution of N-([1-14C]-Palmitoyl)Ethanolamine in Rat Tissues. Ukr. Biokhim Zh 1999, 71, 124–125. [Google Scholar]
- Costa, B.; Comelli, F.; Bettoni, I.; Colleoni, M.; Giagnoni, G. The Endogenous Fatty Acid Amide, Palmitoylethanolamide, Has Anti-Allodynic and Anti-Hyperalgesic Effects in a Murine Model of Neuropathic Pain: Involvement of CB(1), TRPV1 and PPARgamma Receptors and Neurotrophic Factors. Pain 2008, 139, 541–550. [Google Scholar] [CrossRef] [PubMed]
- Artukoglu, B.B.; Beyer, C.; Zuloff-Shani, A.; Brener, E.; Bloch, M.H. Efficacy of Palmitoylethanolamide for Pain: A Meta-Analysis. Pain Physician 2017, 20, 353–362. [Google Scholar] [PubMed]
- Lowin, T.; Apitz, M.; Anders, S.; Straub, R.H. Anti-Inflammatory Effects of N-Acylethanolamines in Rheumatoid Arthritis Synovial Cells Are Mediated by TRPV1 and TRPA1 in a COX-2 Dependent Manner. Arthritis Res. Ther. 2015, 17, 321. [Google Scholar] [CrossRef]
- Ghonghadze, M.; Pachkoria, K.; Okujava, M.; Antelava, N.; Gongadze, N. Endocannabinoids Receptors Mediated Central and Peripheral Effects (Review). Georg. Med. News 2020, 298, 137–143. [Google Scholar]
- Kramar, C.; Loureiro, M.; Renard, J.; Laviolette, S.R. Palmitoylethanolamide Modulates GPR55 Receptor Signaling in the Ventral Hippocampus to Regulate Mesolimbic Dopamine Activity, Social Interaction, and Memory Processing. Cannabis Cannabinoid Res. 2017, 2, 8–20. [Google Scholar] [CrossRef] [PubMed]
- D’Amico, R.; Impellizzeri, D.; Cuzzocrea, S.; Di Paola, R. ALIAmides Update: Palmitoylethanolamide and Its Formulations on Management of Peripheral Neuropathic Pain. Int. J. Mol. Sci. 2020, 21, 5330. [Google Scholar] [CrossRef]
- Lang-Illievich, K.; Klivinyi, C.; Lasser, C.; Brenna, C.T.A.; Szilagyi, I.S.; Bornemann-Cimenti, H. Palmitoylethanolamide in the Treatment of Chronic Pain: A Systematic Review and Meta-Analysis of Double-Blind Randomized Controlled Trials. Nutrients 2023, 15, 1350. [Google Scholar] [CrossRef]
- Briskey, D.; Skinner, R.; Smith, C.; Rao, A. Effectiveness of Palmitoylethanolamide (Levagen+) Compared to a Placebo for Reducing Pain, Duration, and Medication Use during Migraines in Otherwise Healthy Participants-A Double-Blind Randomised Controlled Study. Pharmaceuticals 2024, 17, 145. [Google Scholar] [CrossRef]
- de Oliveira, C.M.B.; Sakata, R.K.; Issy, A.M.; Gerola, L.R.; Salomão, R. Cytokines and Pain. Rev. Bras. Anestesiol. 2011, 61, 255–259, 260–265, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Voscopoulos, C.; Lema, M. When Does Acute Pain Become Chronic? Br. J. Anaesth. 2010, 105, i69–i85. [Google Scholar] [CrossRef] [PubMed]
- Woolf, C.J. Central Sensitization: Implications for the Diagnosis and Treatment of Pain. Pain 2011, 152 (Suppl. 3), S2–S15. [Google Scholar] [CrossRef] [PubMed]
- Magerl, W.; Fuchs, P.N.; Meyer, R.A.; Treede, R.D. Roles of Capsaicin-Insensitive Nociceptors in Cutaneous Pain and Secondary Hyperalgesia. Brain 2001, 124 Pt 9, 1754–1764. [Google Scholar] [CrossRef] [PubMed]
- Ji, R.-R.; Nackley, A.; Huh, Y.; Terrando, N.; Maixner, W. Neuroinflammation and Central Sensitization in Chronic and Widespread Pain. Anesthesiology 2018, 129, 343–366. [Google Scholar] [CrossRef] [PubMed]
- Luongo, L.; Guida, F.; Boccella, S.; Bellini, G.; Gatta, L.; Rossi, F.; de Novellis, V.; Maione, S. Palmitoylethanolamide Reduces Formalin-Induced Neuropathic-like Behaviour through Spinal Glial/Microglial Phenotypical Changes in Mice. CNS Neurol. Disord. Drug Targets 2013, 12, 45–54. [Google Scholar] [CrossRef] [PubMed]
- Ambrosino, P.; Soldovieri, M.V.; Russo, C.; Taglialatela, M. Activation and Desensitization of TRPV1 Channels in Sensory Neurons by the PPARα Agonist Palmitoylethanolamide. Br. J. Pharmacol. 2013, 168, 1430–1444. [Google Scholar] [CrossRef] [PubMed]
- Horn-Hofmann, C.; Kunz, M.; Madden, M.; Schnabel, E.-L.; Lautenbacher, S. Interactive Effects of Conditioned Pain Modulation and Temporal Summation of Pain-the Role of Stimulus Modality. Pain 2018, 159, 2641–2648. [Google Scholar] [CrossRef] [PubMed]
- Kucharczyk, M.W.; Valiente, D.; Bannister, K. Developments in Understanding Diffuse Noxious Inhibitory Controls: Pharmacological Evidence from Pre-Clinical Research. J. Pain Res. 2021, 14, 1083–1095. [Google Scholar] [CrossRef]
- Gutierrez, T.; Nackley, A.G.; Neely, M.H.; Freeman, K.G.; Edwards, G.L.; Hohmann, A.G. Effects of Neurotoxic Destruction of Descending Noradrenergic Pathways on Cannabinoid Antinociception in Models of Acute and Tonic Nociception. Brain Res. 2003, 987, 176–185. [Google Scholar] [CrossRef]
- González-Hernández, A.; Martínez-Lorenzana, G.; Rodríguez-Jiménez, J.; Rojas-Piloni, G.; Condés-Lara, M. Intracisternal Injection of Palmitoylethanolamide Inhibits the Peripheral Nociceptive Evoked Responses of Dorsal Horn Wide Dynamic Range Neurons. J. Neural Transm. 2015, 122, 369–374. [Google Scholar] [CrossRef] [PubMed]
- Déciga-Campos, M.; Jaramillo-Morales, O.A.; Espinosa-Juárez, J.V.; Aguilera-Martínez, M.E.; Ventura-Martínez, R.; López-Muñoz, F.J. N-Palmitoylethanolamide Synergizes the Antinociception of Morphine and Gabapentin in the Formalin Test in Mice. J. Pharm. Pharmacol. 2023, 75, 1154–1162. [Google Scholar] [CrossRef]
- Petrosino, S.; Cordaro, M.; Verde, R.; Moriello, A.S.; Marcolongo, G.; Schievano, C.; Siracusa, R.; Piscitelli, F.; Peritore, A.F.; Crupi, R.; et al. Oral Ultramicronized Palmitoylethanolamide: Plasma and Tissue Levels and Spinal Anti-Hyperalgesic Effect. Front. Pharmacol. 2018, 9, 249. [Google Scholar] [CrossRef]
- Avagliano, C.; Russo, R.; De Caro, C.; Cristiano, C.; La Rana, G.; Piegari, G.; Paciello, O.; Citraro, R.; Russo, E.; De Sarro, G.; et al. Palmitoylethanolamide Protects Mice against 6-OHDA-Induced Neurotoxicity and Endoplasmic Reticulum Stress: In Vivo and in Vitro Evidence. Pharmacol. Res. 2016, 113 Pt A, 276–289. [Google Scholar] [CrossRef]
- Cristiano, C.; Pirozzi, C.; Coretti, L.; Cavaliere, G.; Lama, A.; Russo, R.; Lembo, F.; Mollica, M.P.; Meli, R.; Calignano, A.; et al. Palmitoylethanolamide Counteracts Autistic-like Behaviours in BTBR T+tf/J Mice: Contribution of Central and Peripheral Mechanisms. Brain Behav. Immun. 2018, 74, 166–175. [Google Scholar] [CrossRef] [PubMed]
- Guida, F.; Luongo, L.; Boccella, S.; Giordano, M.E.; Romano, R.; Bellini, G.; Manzo, I.; Furiano, A.; Rizzo, A.; Imperatore, R.; et al. Palmitoylethanolamide Induces Microglia Changes Associated with Increased Migration and Phagocytic Activity: Involvement of the CB2 Receptor. Sci. Rep. 2017, 7, 375. [Google Scholar] [CrossRef]
- Wang, J.; Zheng, J.; Kulkarni, A.; Wang, W.; Garg, S.; Prather, P.L.; Hauer-Jensen, M. Palmitoylethanolamide Regulates Development of Intestinal Radiation Injury in a Mast Cell-Dependent Manner. Dig. Dis. Sci. 2014, 59, 2693–2703. [Google Scholar] [CrossRef]
- Hu, J.; Ying, H.; Yao, J.; Yang, L.; Jin, W.; Ma, H.; Li, L.; Zhao, Y. Micronized Palmitoylethanolamide Ameliorates Methionine- and Choline-Deficient Diet-Induced Nonalcoholic Steatohepatitis via Inhibiting Inflammation and Restoring Autophagy. Front. Pharmacol. 2021, 12, 744483. [Google Scholar] [CrossRef] [PubMed]
- D’Antongiovanni, V.; Pellegrini, C.; Antonioli, L.; Benvenuti, L.; Di Salvo, C.; Flori, L.; Piccarducci, R.; Daniele, S.; Martelli, A.; Calderone, V.; et al. Palmitoylethanolamide Counteracts Enteric Inflammation and Bowel Motor Dysfunctions in a Mouse Model of Alzheimer’s Disease. Front. Pharmacol. 2021, 12, 748021. [Google Scholar] [CrossRef]
- Lo Verme, J.; Fu, J.; Astarita, G.; La Rana, G.; Russo, R.; Calignano, A.; Piomelli, D. The Nuclear Receptor Peroxisome Proliferator-Activated Receptor-Alpha Mediates the Anti-Inflammatory Actions of Palmitoylethanolamide. Mol. Pharmacol. 2005, 67, 15–19. [Google Scholar] [CrossRef]
- Borrelli, F.; Izzo, A.A. Role of Acylethanolamides in the Gastrointestinal Tract with Special Reference to Food Intake and Energy Balance. Best. Pr. Res. Clin. Endocrinol. Metab. 2009, 23, 33–49. [Google Scholar] [CrossRef] [PubMed]
- de La Serre, C.B.; Ellis, C.L.; Lee, J.; Hartman, A.L.; Rutledge, J.C.; Raybould, H.E. Propensity to High-Fat Diet-Induced Obesity in Rats Is Associated with Changes in the Gut Microbiota and Gut Inflammation. Am. J. Physiol. Gastrointest. Liver Physiol. 2010, 299, G440-8. [Google Scholar] [CrossRef] [PubMed]
- Malesza, I.J.; Malesza, M.; Walkowiak, J.; Mussin, N.; Walkowiak, D.; Aringazina, R.; Bartkowiak-Wieczorek, J.; Mądry, E. High-Fat, Western-Style Diet, Systemic Inflammation, and Gut Microbiota: A Narrative Review. Cells 2021, 10, 3164. [Google Scholar] [CrossRef]
- Stojanov, S.; Berlec, A.; Štrukelj, B. The Influence of Probiotics on the Firmicutes/Bacteroidetes Ratio in the Treatment of Obesity and Inflammatory Bowel Disease. Microorganisms 2020, 8, 1715. [Google Scholar] [CrossRef] [PubMed]
- Zhuang, P.; Zhang, Y.; Shou, Q.; Li, H.; Zhu, Y.; He, L.; Chen, J.; Jiao, J. Eicosapentaenoic and Docosahexaenoic Acids Differentially Alter Gut Microbiome and Reverse High-Fat Diet-Induced Insulin Resistance. Mol. Nutr. Food Res. 2020, 64, e1900946. [Google Scholar] [CrossRef] [PubMed]
- Falony, G.; Vlachou, A.; Verbrugghe, K.; De Vuyst, L. Cross-Feeding between Bifidobacterium longum BB536 and Acetate-Converting, Butyrate-Producing Colon Bacteria during Growth on Oligofructose. Appl. Environ. Microbiol. 2006, 72, 7835–7841. [Google Scholar] [CrossRef] [PubMed]
- McNabney, S.M.; Henagan, T.M. Short Chain Fatty Acids in the Colon and Peripheral Tissues: A Focus on Butyrate, Colon Cancer, Obesity and Insulin Resistance. Nutrients 2017, 9, 1348. [Google Scholar] [CrossRef] [PubMed]
- Domingo, J.J.S. Irritable Bowel Syndrome. Med. Clin. 2022, 158, 76–81. [Google Scholar] [CrossRef] [PubMed]
- Barbara, G.; Cremon, C.; Stanghellini, V. Inflammatory Bowel Disease and Irritable Bowel Syndrome: Similarities and Differences. Curr. Opin. Gastroenterol. 2014, 30, 352–358. [Google Scholar] [CrossRef]
- Vaiopoulou, A.; Karamanolis, G.; Psaltopoulou, T.; Karatzias, G.; Gazouli, M. Molecular Basis of the Irritable Bowel Syndrome. World J. Gastroenterol. 2014, 20, 376–383. [Google Scholar] [CrossRef]
- Corsetti, M.; Tack, J. FDA and EMA End Points: Which Outcome End Points Should We Use in Clinical Trials in Patients with Irritable Bowel Syndrome? Neurogastroenterol. Motil. 2013, 25, 453–457. [Google Scholar] [CrossRef] [PubMed]
- Barbara, G.; Stanghellini, V.; De Giorgio, R.; Cremon, C.; Cottrell, G.S.; Santini, D.; Pasquinelli, G.; Morselli-Labate, A.M.; Grady, E.F.; Bunnett, N.W.; et al. Activated Mast Cells in Proximity to Colonic Nerves Correlate with Abdominal Pain in Irritable Bowel Syndrome. Gastroenterology 2004, 126, 693–702. [Google Scholar] [CrossRef] [PubMed]
- Klooker, T.K.; Braak, B.; Koopman, K.E.; Welting, O.; Wouters, M.M.; van der Heide, S.; Schemann, M.; Bischoff, S.C.; van den Wijngaard, R.M.; Boeckxstaens, G.E. The Mast Cell Stabiliser Ketotifen Decreases Visceral Hypersensitivity and Improves Intestinal Symptoms in Patients with Irritable Bowel Syndrome. Gut 2010, 59, 1213–1221. [Google Scholar] [CrossRef] [PubMed]
- Lam, C.; Tan, W.; Leighton, M.; Hastings, M.; Lingaya, M.; Falcone, Y.; Zhou, X.; Xu, L.; Whorwell, P.; Walls, A.F.; et al. A Mechanistic Multicentre, Parallel Group, Randomised Placebo-Controlled Trial of Mesalazine for the Treatment of IBS with Diarrhoea (IBS-D). Gut 2016, 65, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Wouters, M.M.; Balemans, D.; Van Wanrooy, S.; Dooley, J.; Cibert-Goton, V.; Alpizar, Y.A.; Valdez-Morales, E.E.; Nasser, Y.; Van Veldhoven, P.P.; Vanbrabant, W.; et al. Histamine Receptor H1-Mediated Sensitization of TRPV1 Mediates Visceral Hypersensitivity and Symptoms in Patients With Irritable Bowel Syndrome. Gastroenterology 2016, 150, 875–887.e9. [Google Scholar] [CrossRef] [PubMed]
- Bischoff, S.C. Mast Cells in Gastrointestinal Disorders. Eur. J. Pharmacol. 2016, 778, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Barbara, G.; Wang, B.; Stanghellini, V.; de Giorgio, R.; Cremon, C.; Di Nardo, G.; Trevisani, M.; Campi, B.; Geppetti, P.; Tonini, M.; et al. Mast Cell-Dependent Excitation of Visceral-Nociceptive Sensory Neurons in Irritable Bowel Syndrome. Gastroenterology 2007, 132, 26–37. [Google Scholar] [CrossRef]
- Vivinus-Nébot, M.; Dainese, R.; Anty, R.; Saint-Paul, M.C.; Nano, J.L.; Gonthier, N.; Marjoux, S.; Frin-Mathy, G.; Bernard, G.; Hébuterne, X.; et al. Combination of Allergic Factors Can Worsen Diarrheic Irritable Bowel Syndrome: Role of Barrier Defects and Mast Cells. Am. J. Gastroenterol. 2012, 107, 75–81. [Google Scholar] [CrossRef]
- Barbara, G.; Stanghellini, V.; Cremon, C.; De Giorgio, R.; Fronzoni, L.; Serra, M.; Corinaldesi, R. Aminosalicylates and Other Anti-Inflammatory Compounds for Irritable Bowel Syndrome. Dig. Dis. 2009, 27 (Suppl. 1), 115–121. [Google Scholar] [CrossRef]
- Izzo, A.A.; Sharkey, K.A. Cannabinoids and the Gut: New Developments and Emerging Concepts. Pharmacol. Ther. 2010, 126, 21–38. [Google Scholar] [CrossRef]
- Russo, E.B. Clinical Endocannabinoid Deficiency (CECD): Can This Concept Explain Therapeutic Benefits of Cannabis in Migraine, Fibromyalgia, Irritable Bowel Syndrome and Other Treatment-Resistant Conditions? Neuro Endocrinol. Lett. 2004, 25, 31–39. [Google Scholar] [PubMed]
- Parigi, T.L.; Iacucci, M.; Ghosh, S. Blockade of IL-23: What Is in the Pipeline? J. Crohns Colitis 2022, 16, ii64–ii72. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Li, Z.; Liu, S.; Zhang, D. Global, Regional and National Burden of Inflammatory Bowel Disease in 204 Countries and Territories from 1990 to 2019: A Systematic Analysis Based on the Global Burden of Disease Study 2019. BMJ Open 2023, 13, e065186. [Google Scholar] [CrossRef] [PubMed]
- Schreiner, P.; Martinho-Grueber, M.; Studerus, D.; Vavricka, S.R.; Tilg, H.; Biedermann, L.; on behalf of Swiss IBDnet an official working group of the Swiss Society of Gastroenterology. Nutrition in Inflammatory Bowel Disease. Digestion 2020, 101, 120–135. [Google Scholar] [CrossRef]
- Ng, S.C.; Shi, H.Y.; Hamidi, N.; Underwood, F.E.; Tang, W.; Benchimol, E.I.; Panaccione, R.; Ghosh, S.; Wu, J.C.Y.; Chan, F.K.L.; et al. Worldwide Incidence and Prevalence of Inflammatory Bowel Disease in the 21st Century: A Systematic Review of Population-Based Studies. Lancet 2017, 390, 2769–2778. [Google Scholar] [CrossRef] [PubMed]
- Ng, S.C.; Bernstein, C.N.; Vatn, M.H.; Lakatos, P.L.; Loftus, E.V., Jr.; Tysk, C.; O’Morain, C.; Moum, B.; Colombel, J.-F.; Epidemiology and Natural History Task Force of the International Organization of Inflammatory Bowel Disease (IOIBD). Geographical Variability and Environmental Risk Factors in Inflammatory Bowel Disease. Gut 2013, 62, 630–649. [Google Scholar] [CrossRef]
- Rogler, G.; Vavricka, S. Exposome in IBD: Recent Insights in Environmental Factors That Influence the Onset and Course of IBD. Inflamm. Bowel Dis. 2015, 21, 400–408. [Google Scholar] [CrossRef]
- Lee, J.C.; Biasci, D.; Roberts, R.; Gearry, R.B.; Mansfield, J.C.; Ahmad, T.; Prescott, N.J.; Satsangi, J.; Wilson, D.C.; Jostins, L.; et al. Genome-Wide Association Study Identifies Distinct Genetic Contributions to Prognosis and Susceptibility in Crohn’s Disease. Nat. Genet. 2017, 49, 262–268. [Google Scholar] [CrossRef] [PubMed]
- Ananthakrishnan, A.N.; Bernstein, C.N.; Iliopoulos, D.; Macpherson, A.; Neurath, M.F.; Ali, R.A.R.; Vavricka, S.R.; Fiocchi, C. Environmental Triggers in IBD: A Review of Progress and Evidence. Nat. Rev. Gastroenterol. Hepatol. 2018, 15, 39–49. [Google Scholar] [CrossRef]
- Impellizzeri, D.; Campolo, M.; Paola, R.; Bruschetta, G.; Stefano, D.D.; Esposito, E.; Cuzzocrea, S. Ultramicronized Palmitoylethanolamide Reduces Inflammation an a Th1-Mediated Model of Colitis. Eur. J. Inflamm. 2015, 13, 14–31. [Google Scholar] [CrossRef]
- Andersen, S.N.; Rognum, T.O.; Bakka, A.; Clausen, O.P. Ki-67: A Useful Marker for the Evaluation of Dysplasia in Ulcerative Colitis. Mol. Pathol. 1998, 51, 327–332. [Google Scholar] [CrossRef]
- Krawisz, J.E.; Sharon, P.; Stenson, W.F. Quantitative Assay for Acute Intestinal Inflammation Based on Myeloperoxidase Activity. Assessment of Inflammation in Rat and Hamster Models. Gastroenterology 1984, 87, 1344–1350. [Google Scholar] [CrossRef] [PubMed]
- Tsuboi, K.; Takezaki, N.; Ueda, N. The N-Acylethanolamine-Hydrolyzing Acid Amidase (NAAA). Chem. Biodivers. 2007, 4, 1914–1925. [Google Scholar] [CrossRef] [PubMed]
- Schicho, R.; Storr, M. A Potential Role for GPR55 in Gastrointestinal Functions. Curr. Opin. Pharmacol. 2012, 12, 653–658. [Google Scholar] [CrossRef] [PubMed]
- Capasso, R.; Orlando, P.; Pagano, E.; Aveta, T.; Buono, L.; Borrelli, F.; Di Marzo, V.; Izzo, A.A. Palmitoylethanolamide Normalizes Intestinal Motility in a Model of Post-Inflammatory Accelerated Transit: Involvement of CB1 Receptors and TRPV1 Channels. Br. J. Pharmacol. 2014, 171, 4026–4037. [Google Scholar] [CrossRef] [PubMed]
- Peritore, A.F.; D’Amico, R.; Cordaro, M.; Siracusa, R.; Fusco, R.; Gugliandolo, E.; Genovese, T.; Crupi, R.; Di Paola, R.; Cuzzocrea, S.; et al. PEA/Polydatin: Anti-Inflammatory and Antioxidant Approach to Counteract DNBS-Induced Colitis. Antioxidants 2021, 10, 464. [Google Scholar] [CrossRef] [PubMed]
- Araújo, D.F.S.; Guerra, G.C.B.; Pintado, M.M.E.; Sousa, Y.R.F.; Algieri, F.; Rodriguez-Nogales, A.; Araújo, R.F., Jr.; Gálvez, J.; de Queiroga, R.C.R.E.; Rodriguez-Cabezas, M.E. Intestinal Anti-Inflammatory Effects of Goat Whey on DNBS-Induced Colitis in Mice. PLoS ONE 2017, 12, e0185382. [Google Scholar] [CrossRef] [PubMed]
- Impellizzeri, D.; Peritore, A.F.; Cordaro, M.; Gugliandolo, E.; Siracusa, R.; Crupi, R.; D’Amico, R.; Fusco, R.; Evangelista, M.; Cuzzocrea, S.; et al. The Neuroprotective Effects of Micronized PEA (PEA-m) Formulation on Diabetic Peripheral Neuropathy in Mice. FASEB J. 2019, 33, 11364–11380. [Google Scholar] [CrossRef] [PubMed]
- Fang, Y.-Z.; Yang, S.; Wu, G. Free Radicals, Antioxidants, and Nutrition. Nutrition 2002, 18, 872–879. [Google Scholar] [CrossRef]
- Ali, T.; Hao, Q.; Ullah, N.; Rahman, S.U.; Shah, F.A.; He, K.; Zheng, C.; Li, W.; Murtaza, I.; Li, Y.; et al. Melatonin Act as an Antidepressant via Attenuation of Neuroinflammation by Targeting Sirt1/Nrf2/HO-1 Signaling. Front. Mol. Neurosci. 2020, 13, 96. [Google Scholar] [CrossRef]
- Fusco, R.; Scuto, M.; Cordaro, M.; D’Amico, R.; Gugliandolo, E.; Siracusa, R.; Peritore, A.F.; Crupi, R.; Impellizzeri, D.; Cuzzocrea, S.; et al. N-Palmitoylethanolamide-Oxazoline Protects against Middle Cerebral Artery Occlusion Injury in Diabetic Rats by Regulating the SIRT1 Pathway. Int. J. Mol. Sci. 2019, 20, 4845. [Google Scholar] [CrossRef]
- Fan, H.; Chen, W.; Zhu, J.; Zhang, J.; Peng, S. Toosendanin Alleviates Dextran Sulfate Sodium-Induced Colitis by Inhibiting M1 Macrophage Polarization and Regulating NLRP3 Inflammasome and Nrf2/HO-1 Signaling. Int. Immunopharmacol. 2019, 76, 105909. [Google Scholar] [CrossRef]
- Kim, H.-J.; Barajas, B.; Wang, M.; Nel, A.E. Nrf2 Activation by Sulforaphane Restores the Age-Related Decrease of T(H)1 Immunity: Role of Dendritic Cells. J. Allergy Clin. Immunol. 2008, 121, 1255–1261.e7. [Google Scholar] [CrossRef]
- Pan, H.; He, M.; Liu, R.; Brecha, N.C.; Yu, A.C.H.; Pu, M. Sulforaphane Protects Rodent Retinas against Ischemia-Reperfusion Injury through the Activation of the Nrf2/HO-1 Antioxidant Pathway. PLoS ONE 2014, 9, e114186. [Google Scholar] [CrossRef]
- Zheng, H.; Whitman, S.A.; Wu, W.; Wondrak, G.T.; Wong, P.K.; Fang, D.; Zhang, D.D. Therapeutic Potential of Nrf2 Activators in Streptozotocin-Induced Diabetic Nephropathy. Diabetes 2011, 60, 3055–3066. [Google Scholar] [CrossRef]
- Gugliandolo, E.; Fusco, R.; Biundo, F.; D’Amico, R.; Benedetto, F.; Di Paola, R.; Cuzzocrea, S. Palmitoylethanolamide and Polydatin Combination Reduces Inflammation and Oxidative Stress in Vascular Injury. Pharmacol. Res. 2017, 123, 83–92. [Google Scholar] [CrossRef]
- Di Paola, R.; Fusco, R.; Gugliandolo, E.; Crupi, R.; Evangelista, M.; Granese, R.; Cuzzocrea, S. Co-Micronized Palmitoylethanolamide/Polydatin Treatment Causes Endometriotic Lesion Regression in a Rodent Model of Surgically Induced Endometriosis. Front. Pharmacol. 2016, 7, 382. [Google Scholar] [CrossRef]
- Cordaro, M.; Impellizzeri, D.; Siracusa, R.; Gugliandolo, E.; Fusco, R.; Inferrera, A.; Esposito, E.; Di Paola, R.; Cuzzocrea, S. Effects of a Co-Micronized Composite Containing Palmitoylethanolamide and Polydatin in an Experimental Model of Benign Prostatic Hyperplasia. Toxicol. Appl. Pharmacol. 2017, 329, 231–240. [Google Scholar] [CrossRef]
- Gabrielsson, L.; Mattsson, S.; Fowler, C.J. Palmitoylethanolamide for the Treatment of Pain: Pharmacokinetics, Safety and Efficacy. Br. J. Clin. Pharmacol. 2016, 82, 932–942. [Google Scholar] [CrossRef]
| Article Type | Year | Authors | Title | Main Findings | Ref. No. |
|---|---|---|---|---|---|
| Reviews | 2022 | A. K. Kiani et al. | Dietary supplements for intestinal inflammation | The PEA treatment was reported to be noticeably effective in decreasing abdominal pain severity in IBS. PEA is a nutritional compound able to decrease the activation of mast cells. | [9] |
| 2021 | A. Heidari et al. | The immune system and autism spectrum disorder: association and therapeutic challenges | PEA, an endocannabinoid molecule, has potential anti-inflammatory effects. Consistently, it improved autistic-like behaviors by affecting intestinal microbial composition in mice. | [17] | |
| 2016 | F. Ochoa-Cortes et al. | Enteric Glial Cells: A New Frontier in Neurogastroenterology and Clinical Target for Inflammatory Bowel Diseases | PEA, by interacting with peroxisome proliferator-activated receptor–α expressed by glial cells, can counteract the increased expression of TLR4/S100B proteins, together with p38/p-ERK/pJNK-pathway signaling molecules, NF-κB expression, and NO release, in patients with ulcerative colitis. | [18] | |
| 2005 | N. A. Darmani et al. | Involvement of the cannabimimetic compound, N-palmitoyl-ethanolamine, in inflammatory and neuropathic conditions: review of the available pre-clinical data, and first human studies | Colonic PEA levels in biopsies from patients with ulcerative colitis were found to be 1.8-fold higher than those in healthy subjects. | [19] | |
| In vitro studies | 2008 | Zolese G. et al. | Effect of Acylethanolamides on Lipid Peroxidation and Paraoxonase Activity | N-acylethanolamides protect plasma lipids and PON1 activity against AAPH and/or copper-induced oxidation. | [11] |
| 2007 | Lombardi G. et al. | Oxyhomologation of the Amide Bond Potentiates Neuroprotective Effects of the Endolipid N-PEA | Oxyhomologation of the amide bond potentiates the neuroprotective effects of the endolipid N-PEA. Also proven is the antioxidant effect of PEA. | [20] | |
| 2005 | Zolese G. et al. | Increased Plasma Concentrations of Palmitoylethanolamide, an Endogenous Fatty Acid Amide, Affect Oxidative Damage of Human Low-Density Lipoproteins: An in Vitro Study | Indicate both anti-oxidative and slightly pro-oxidative effects of PEA. | [21] | |
| Murine models | 2023 | Pirozzi C. et al. | Palmitoylethanolamide Counteracts High-Fat Diet-Induced Gut Dysfunction by Reprogramming Microbiota Composition and Affecting Tryptophan Metabolism | PEA leads to a decrease in inflammatory factors in the gut. The administration of ultra micronized PEA reprograms gut microbial community assortment. | [22] |
| 2021 | Esposito G. et al. | Engineered Lactobacillus Paracasei Producing Palmitoylethanolamide (PEA) Prevents Colitis in Mice | They concluded that pNAPE-LP with ultra-low palmitate supply stands as a new method to increase the in situ intestinal delivery of PEA and as a new therapeutic able to control intestinal inflammation in inflammatory bowel disease. | [23] | |
| 2014 | Esposito G. et al. | Palmitoylethanolamide Improves Colon Inflammation through an Enteric Glia/Toll like Receptor 4-Dependent PPAR-α Activation | Because of its lack of toxicity, its ability to reduce inflammation, and its selective PPARα action, PEA might be an innovative molecule to broaden pharmacological strategies against UC. | [24] | |
| 2010 | Azuma Y-T. et al. | PPARα Contributes to Colonic Protection in Mice with DSS-Induced Colitis | They suggest that PPARα has a role in controlling colonic inflammation and mucosal tissue homeostasis. | [25] | |
| 2007 | D’Argenio G. et al. | Overactivity of the Intestinal Endocannabinoid System in Celiac Disease and in Methotrexate-Treated Rats | The levels of anandamide and PEA were significantly elevated (approx. 2 and 1.8-fold, respectively) in active celiac patients, as were those of CB1 receptors. The levels of anandamide, 2-AG, and PEA peaked 3 days after treatment with Methotrexate and returned to basal levels at remission 7 days after treatment. | [26] | |
| 2005 | Dömötör A. et al. | Immunohistochemical Distribution of Vanilloid Receptor, Calcitonin-Gene Related Peptide and Substance P in Gastrointestinal Mucosa of Patients with Different Gastrointestinal Disorders | The immunohistochemical distribution of TRPV1, CGRP, and SP differs in gastrointestinal diseases of the upper and lower tract, and the participation of TRPV1, CGRP, and SP differs significantly in these different gastrointestinal diseases. | [27] | |
| 2004 | Cuzzocrea S. et al. | Role of Endogenous and Exogenous Ligands for the Peroxisome Proliferators Activated Receptors Alpha (PPAR-Alpha) in the Development of Inflammatory Bowel Disease in Mice | The absence of the PPAR-alpha receptor significantly abolished the protective effect of the PPAR-alpha agonist against DNBS-induced colitis. Endogenous and exogenous PPAR-alpha ligands reduce the degree of colitis caused by DNBS, so PPAR-alpha ligands may be useful in the treatment of IBD. | [28] | |
| 2004 | Kimball E. et al. | Vanilloid Receptor 1 Antagonists Attenuate Disease Severity in Dextran Sulphate Sodium-Induced Colitis in Mice | The results suggest that pharmacological modulation of TRPV1 attenuates indices of experimental colitis in mice and that the development of orally active TRPV1 antagonists might have therapeutic potential for the treatment of IBD. | [29] | |
| 2001 | Capasso R. et al. | Inhibitory Effect of Palmitoylethanolamide on Gastrointestinal Motility in Mice | It is concluded that PEA inhibits intestinal motility through a peripheral mechanism independent from cannabinoid receptor activation. | [30] | |
| Clinical Trials | 2024 | G. Di Nardo et al. | Palmitoylethanolamide and polydatin in pediatric irritable bowel syndrome: A multicentric randomized controlled trial | Co-micronized PEA/polydatin (PEA/PD) demonstrated efficacy in pediatric irritable bowel syndrome, significantly increasing complete remission. Subgroup analysis highlighted benefits in the irritable bowel syndrome-diarrhea subtype. Treatment with PEA/PD resulted in a notable reduction in abdominal pain intensity and frequency compared with placebo. | [31] |
| 2019 | D. G. Couch et al. | Palmitoylethanolamide and Cannabidiol Prevent Inflammation-induced Hyperpermeability of the Human Gut In Vitro and In Vivo-A Randomized, Placebo-controlled, Double-blind Controlled Trial | In vitro, PEA decreased the inflammation-induced flux of dextran and prevented an inflammation-induced fall in TRPV1 and an increase in PPARα transcription. In conclusion. PEA reduces permeability in the human colon. | [32] | |
| 2017 | Cremon C. et al. | Randomized Clinical Trial: The Analgesic Properties of Dietary Supplementation with Palmitoylethanolamide and Polydatin in Irritable Bowel Syndrome | The marked effect of the dietary supplement PEA/polydatin on abdominal pain in patients with IBS suggests that this is a promising natural approach for pain management in this condition. | [33] | |
| 2013 | Fichna J. et al. | Endocannabinoid and Cannabinoid-like Fatty Acid Amide Levels Correlate with Pain-Related Symptoms in Patients with IBS-D and IBS-C: A Pilot Study | Patients with IBS-D had higher levels of 2AG and lower levels of OEA and PEA. In contrast, patients with IBS-C had higher levels of OEA. Multivariate analysis found that lower PEA levels are associated with cramping abdominal pain. FAAH mRNA levels were lower in patients with IBS-C. | [34] |
| Aminosalicylates | Corticosteroids | Advanced Therapy |
|---|---|---|
| mesalamine | methylprednisolone | infliximab |
| sulfasalazine | prednisone | adalimumab |
| olsalazine | hydrocortisone | golimumab |
| balsalazide | budesonide | vedolizumab |
| ustekinumab | ||
| tofacitinib | ||
| upadacitinib |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Branković, M.; Gmizić, T.; Dukić, M.; Zdravković, M.; Daskalović, B.; Mrda, D.; Nikolić, N.; Brajković, M.; Gojgić, M.; Lalatović, J.; et al. Therapeutic Potential of Palmitoylethanolamide in Gastrointestinal Disorders. Antioxidants 2024, 13, 600. https://doi.org/10.3390/antiox13050600
Branković M, Gmizić T, Dukić M, Zdravković M, Daskalović B, Mrda D, Nikolić N, Brajković M, Gojgić M, Lalatović J, et al. Therapeutic Potential of Palmitoylethanolamide in Gastrointestinal Disorders. Antioxidants. 2024; 13(5):600. https://doi.org/10.3390/antiox13050600
Chicago/Turabian StyleBranković, Marija, Tijana Gmizić, Marija Dukić, Marija Zdravković, Branislava Daskalović, Davor Mrda, Novica Nikolić, Milica Brajković, Milan Gojgić, Jovana Lalatović, and et al. 2024. "Therapeutic Potential of Palmitoylethanolamide in Gastrointestinal Disorders" Antioxidants 13, no. 5: 600. https://doi.org/10.3390/antiox13050600
APA StyleBranković, M., Gmizić, T., Dukić, M., Zdravković, M., Daskalović, B., Mrda, D., Nikolić, N., Brajković, M., Gojgić, M., Lalatović, J., Kralj, Đ., Pantić, I., Vojnović, M., Milovanović, T., Đurašević, S., & Todorović, Z. (2024). Therapeutic Potential of Palmitoylethanolamide in Gastrointestinal Disorders. Antioxidants, 13(5), 600. https://doi.org/10.3390/antiox13050600












