Potential Neuroprotective Role of Melatonin in Sepsis-Associated Encephalopathy Due to Its Scavenging and Anti-Oxidative Properties
Abstract
1. Introduction—Sepsis and Sepsis-Associated Encephalopathy
1.1. Sepsis
1.2. Sepsis-Associated Encephalopathy
1.3. Clinical Picture of SAE
1.4. Epidemiology of SAE
1.5. Melatonin
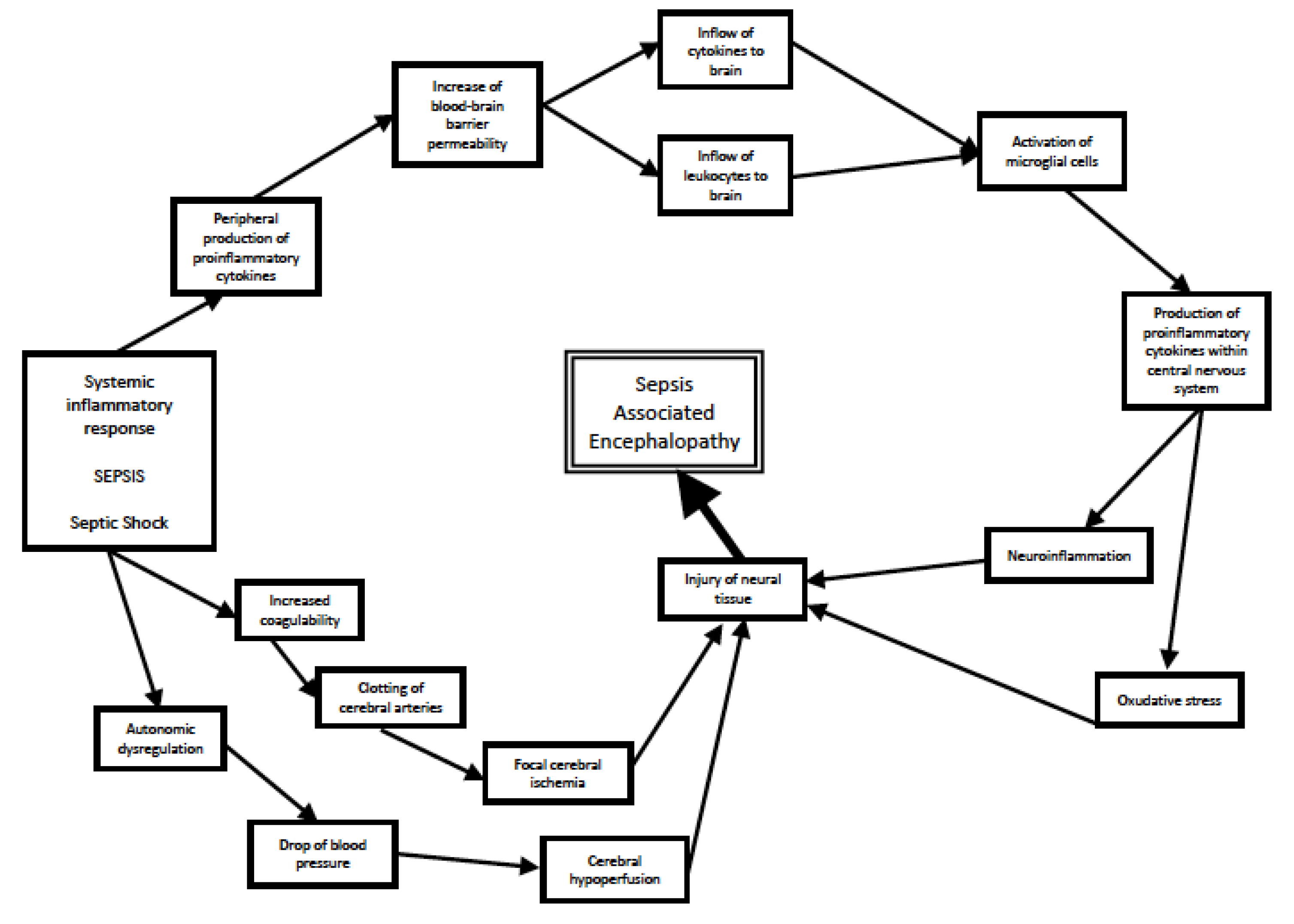
2. Mechanisms of Sepsis-Associated Encephalopathy
2.1. Pathomechanisms of SAE
2.2. The Role of Oxidative Stress and Free Radicals in Sepsis-Associated Encephalopathy
3. Clinical Role of Melatonin
3.1. Melatonin
3.2. Main Clinical Roles of Melatonin
3.3. Scavenging and Antioxidant Potential of Melatonin
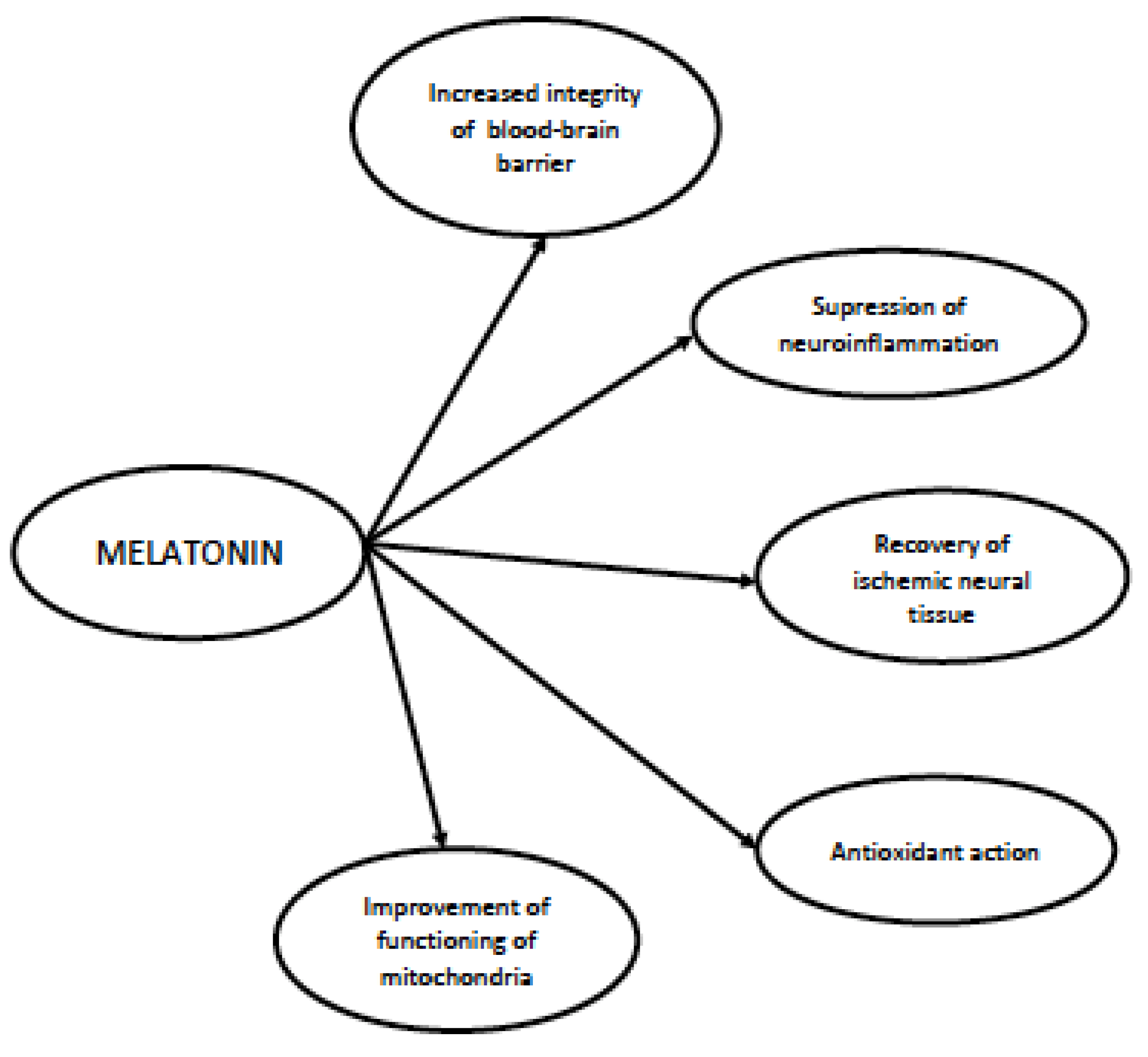
4. Role of Melatonin in Sepsis and in Sepsis-Associated Encephalopathy
4.1. Therapeutic Potential of Melatonin in Sepsis
4.2. Neuroprotective Potential of Melatonin in Sepsis-Associated Encephalopathy
5. Conclusions and Future Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.-D.; Coopersmith, C.M.; et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef] [PubMed]
- Seymour, C.W.; Liu, V.X.; Iwashyna, T.J.; Brunkhorst, F.M.; Rea, T.D.; Scherag, A.; Rubenfeld, G.; Kahn, J.M.; Shankar-Hari, M.; Singer, M.; et al. Assessment of Clinical Criteria for Sepsis: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 762–774. [Google Scholar] [CrossRef] [PubMed]
- Fleischmann-Struzek, C.; Mellhammar, L.; Rose, N.; Cassini, A.; Rudd, K.E.; Schlattmann, P.; Allegranzi, B.; Reinhart, K. Incidence and Mortality of Hospital- and ICU-Treated Sepsis: Results from an Updated and Expanded Systematic Review and Meta-Analysis. Intensive Care Med. 2020, 46, 1552–1562. [Google Scholar] [CrossRef] [PubMed]
- Rhee, C.; Dantes, R.; Epstein, L.; Murphy, D.J.; Seymour, C.W.; Iwashyna, T.J.; Kadri, S.S.; Angus, D.C.; Danner, R.L.; Fiore, A.E.; et al. Incidence and Trends of Sepsis in US Hospitals Using Clinical vs Claims Data, 2009–2014. JAMA 2017, 318, 1241–1249. [Google Scholar] [CrossRef]
- Fleischmann-Struzek, C.; Rose, N.; Freytag, A.; Spoden, M.; Prescott, H.C.; Schettler, A.; Wedekind, L.; Ditscheid, B.; Storch, J.; Born, S.; et al. Epidemiology and Costs of Postsepsis Morbidity, Nursing Care Dependency, and Mortality in Germany, 2013 to 2017. JAMA Netw. Open 2021, 4, e2134290. [Google Scholar] [CrossRef]
- Chung, H.-Y.; Wickel, J.; Brunkhorst, F.M.; Geis, C. Sepsis-Associated Encephalopathy: From Delirium to Dementia? J. Clin. Med. 2020, 9, 703. [Google Scholar] [CrossRef]
- Dantzer, R. Evolutionary Aspects of Infections: Inflammation and Sickness Behaviors. Curr. Top. Behav. Neurosci. 2022, 61, 1–14. [Google Scholar] [CrossRef]
- Heming, N.; Mazeraud, A.; Verdonk, F.; Bozza, F.A.; Chrétien, F.; Sharshar, T. Neuroanatomy of Sepsis-Associated Encephalopathy. Crit. Care 2017, 21, 65. [Google Scholar] [CrossRef]
- Wasyluk, W.; Wasyluk, M.; Zwolak, A. Sepsis as a Pan-Endocrine Illness-Endocrine Disorders in Septic Patients. J. Clin. Med. 2021, 10, 2075. [Google Scholar] [CrossRef]
- Hosokawa, K.; Gaspard, N.; Su, F.; Oddo, M.; Vincent, J.-L.; Taccone, F.S. Clinical Neurophysiological Assessment of Sepsis-Associated Brain Dysfunction: A Systematic Review. Crit. Care 2014, 18, 674. [Google Scholar] [CrossRef]
- Catarina, A.V.; Branchini, G.; Bettoni, L.; De Oliveira, J.R.; Nunes, F.B. Sepsis-Associated Encephalopathy: From Pathophysiology to Progress in Experimental Studies. Mol. Neurobiol. 2021, 58, 2770–2779. [Google Scholar] [CrossRef]
- Bowman, E.M.L.; Cunningham, E.L.; Page, V.J.; McAuley, D.F. Phenotypes and Subphenotypes of Delirium: A Review of Current Categorisations and Suggestions for Progression. Crit. Care 2021, 25, 334. [Google Scholar] [CrossRef]
- Mazeraud, A.; Righy, C.; Bouchereau, E.; Benghanem, S.; Bozza, F.A.; Sharshar, T. Septic-Associated Encephalopathy: A Comprehensive Review. Neurother. J. Am. Soc. Exp. Neurother. 2020, 17, 392–403. [Google Scholar] [CrossRef] [PubMed]
- Polito, A.; Eischwald, F.; Maho, A.-L.; Polito, A.; Azabou, E.; Annane, D.; Chrétien, F.; Stevens, R.D.; Carlier, R.; Sharshar, T. Pattern of Brain Injury in the Acute Setting of Human Septic Shock. Crit. Care 2013, 17, R204. [Google Scholar] [CrossRef] [PubMed]
- Young, G.B.; Bolton, C.F.; Archibald, Y.M.; Austin, T.W.; Wells, G.A. The Electroencephalogram in Sepsis-Associated Encephalopathy. J. Clin. Neurophysiol. 1992, 9, 145–152. [Google Scholar] [CrossRef] [PubMed]
- Pantzaris, N.-D.; Platanaki, C.; Tsiotsios, K.; Koniari, I.; Velissaris, D. The Use of Electroencephalography in Patients with Sepsis: A Review of The Literature. J. Transl. Intern. Med. 2021, 9, 12–16. [Google Scholar] [CrossRef] [PubMed]
- Foreman, B.; Mahulikar, A.; Tadi, P.; Claassen, J.; Szaflarski, J.; Halford, J.J.; Dean, B.C.; Kaplan, P.W.; Hirsch, L.J.; LaRoche, S.; et al. Generalized Periodic Discharges and “Triphasic Waves”: A Blinded Evaluation of Inter-Rater Agreement and Clinical Significance. Clin. Neurophysiol. 2016, 127, 1073–1080. [Google Scholar] [CrossRef]
- Orhun, G.; Tüzün, E.; Bilgiç, B.; Ergin Özcan, P.; Sencer, S.; Barburoğlu, M.; Esen, F. Brain Volume Changes in Patients with Acute Brain Dysfunction Due to Sepsis. Neurocrit. Care 2020, 32, 459–468. [Google Scholar] [CrossRef]
- Masse, M.-H.; Richard, M.A.; D’Aragon, F.; St-Arnaud, C.; Mayette, M.; Adhikari, N.K.J.; Fraser, W.; Carpentier, A.; Palanchuck, S.; Gauthier, D.; et al. Early Evidence of Sepsis-Associated Hyperperfusion-A Study of Cerebral Blood Flow Measured With MRI Arterial Spin Labeling in Critically Ill Septic Patients and Control Subjects. Crit. Care Med. 2018, 46, e663–e669. [Google Scholar] [CrossRef]
- Orhun, G.; Sencer, S.; Tüzün, E.; Bebek, N.; Ergin Özcan, P.; Barburoğlu, M.; Günver, M.G.; Esen, F. Posterior Reversible Encephalopathy in Sepsis-Associated Encephalopathy: Experience from a Single Center. Neurocrit. Care 2022, 36, 372–386. [Google Scholar] [CrossRef]
- Young, G.B.; Bolton, C.F.; Austin, T.W.; Archibald, Y.M.; Gonder, J.; Wells, G.A. The Encephalopathy Associated with Septic Illness. Clin. Investig. Med. Med. Clin. Exp. 1990, 13, 297–304. [Google Scholar]
- Chen, J.; Shi, X.; Diao, M.; Jin, G.; Zhu, Y.; Hu, W.; Xi, S. A Retrospective Study of Sepsis-Associated Encephalopathy: Epidemiology, Clinical Features and Adverse Outcomes. BMC Emerg. Med. 2020, 20, 77. [Google Scholar] [CrossRef]
- Feng, Q.; Ai, Y.-H.; Gong, H.; Wu, L.; Ai, M.-L.; Deng, S.-Y.; Huang, L.; Peng, Q.-Y.; Zhang, L.-N. Characterization of Sepsis and Sepsis-Associated Encephalopathy. J. Intensive Care Med. 2019, 34, 938–945. [Google Scholar] [CrossRef] [PubMed]
- Sonneville, R.; de Montmollin, E.; Poujade, J.; Garrouste-Orgeas, M.; Souweine, B.; Darmon, M.; Mariotte, E.; Argaud, L.; Barbier, F.; Goldgran-Toledano, D.; et al. Potentially Modifiable Factors Contributing to Sepsis-Associated Encephalopathy. Intensive Care Med. 2017, 43, 1075–1084. [Google Scholar] [CrossRef] [PubMed]
- Iwashyna, T.J.; Ely, E.W.; Smith, D.M.; Langa, K.M. Long-Term Cognitive Impairment and Functional Disability among Survivors of Severe Sepsis. JAMA 2010, 304, 1787–1794. [Google Scholar] [CrossRef]
- Iwashyna, T.J.; Cooke, C.R.; Wunsch, H.; Kahn, J.M. Population Burden of Long-Term Survivorship after Severe Sepsis in Older Americans. J. Am. Geriatr. Soc. 2012, 60, 1070–1077. [Google Scholar] [CrossRef] [PubMed]
- Stallmach, A.; Kesselmeier, M.; Bauer, M.; Gramlich, J.; Finke, K.; Fischer, A.; Fleischmann-Struzek, C.; Heutelbeck, A.; Katzer, K.; Mutschke, S.; et al. Comparison of Fatigue, Cognitive Dysfunction and Psychological Disorders in Post-COVID Patients and Patients after Sepsis: Is There a Specific Constellation? Infection 2022, 50, 661–669. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.E.; Kabeto, M.M.; Gray, M.; Wadley, V.G.; Muntner, P.; Judd, S.E.; Safford, M.M.; Kempker, J.; Levine, D.A. Trajectory of Cognitive Decline After Sepsis. Crit. Care Med. 2021, 49, 1083–1094. [Google Scholar] [CrossRef] [PubMed]
- Iuvone, P.M.; Tosini, G.; Pozdeyev, N.; Haque, R.; Klein, D.C.; Chaurasia, S.S. Circadian Clocks, Clock Networks, Arylalkylamine N-Acetyltransferase, and Melatonin in the Retina. Prog. Retin. Eye Res. 2005, 24, 433–456. [Google Scholar] [CrossRef]
- Carrillo-Vico, A.; Calvo, J.R.; Abreu, P.; Lardone, P.J.; García-Mauriño, S.; Reiter, R.J.; Guerrero, J.M. Evidence of Melatonin Synthesis by Human Lymphocytes and Its Physiological Significance: Possible Role as Intracrine, Autocrine, and/or Paracrine Substance. FASEB J. 2004, 18, 537–539. [Google Scholar] [CrossRef]
- Slominski, A.T.; Zmijewski, M.A.; Semak, I.; Kim, T.-K.; Janjetovic, Z.; Slominski, R.M.; Zmijewski, J.W. Melatonin, Mitochondria, and the Skin. Cell. Mol. Life Sci. CMLS 2017, 74, 3913–3925. [Google Scholar] [CrossRef]
- Bertrand, P.P.; Polglaze, K.E.; Bertrand, R.L.; Sandow, S.L.; Pozo, M.J. Detection of Melatonin Production from the Intestinal Epithelium Using Electrochemical Methods. Curr. Pharm. Des. 2014, 20, 4802–4806. [Google Scholar] [CrossRef]
- Shukla, M.; Vincent, B. Melatonin as a Harmonizing Factor of Circadian Rhythms, Neuronal Cell Cycle and Neurogenesis: Additional Arguments for Its Therapeutic Use in Alzheimer’s Disease. Curr. Neuropharmacol. 2023, 21, 1273–1298. [Google Scholar] [CrossRef] [PubMed]
- Tan, D.-X.; Reiter, R.J.; Zimmerman, S.; Hardeland, R. Melatonin: Both a Messenger of Darkness and a Participant in the Cellular Actions of Non-Visible Solar Radiation of Near Infrared Light. Biology 2023, 12, 89. [Google Scholar] [CrossRef]
- Ramos, E.; Gil-Martín, E.; De Los Ríos, C.; Egea, J.; López-Muñoz, F.; Pita, R.; Juberías, A.; Torrado, J.J.; Serrano, D.R.; Reiter, R.J.; et al. Melatonin as Modulator for Sulfur and Nitrogen Mustard-Induced Inflammation, Oxidative Stress and DNA Damage: Molecular Therapeutics. Antioxidants 2023, 12, 397. [Google Scholar] [CrossRef] [PubMed]
- Piekarska, K.; Bonowicz, K.; Grzanka, A.; Jaworski, Ł.M.; Reiter, R.J.; Slominski, A.T.; Steinbrink, K.; Kleszczyński, K.; Gagat, M. Melatonin and TGF-β-Mediated Release of Extracellular Vesicles. Metabolites 2023, 13, 575. [Google Scholar] [CrossRef] [PubMed]
- Guan, Q.; Wang, Z.; Cao, J.; Dong, Y.; Chen, Y. Mechanisms of Melatonin in Obesity: A Review. Int. J. Mol. Sci. 2021, 23, 218. [Google Scholar] [CrossRef] [PubMed]
- Cvikova, D.; Sutovska, H.; Babarikova, K.; Molcan, L. Hypotensive Effects of Melatonin in Rats: Focus on the Model, Measurement, Application, and Main Mechanisms. Hypertens. Res. 2022, 45, 1929–1944. [Google Scholar] [CrossRef]
- Gao, Q.; Hernandes, M.S. Sepsis-Associated Encephalopathy and Blood-Brain Barrier Dysfunction. Inflammation 2021, 44, 2143–2150. [Google Scholar] [CrossRef]
- Erikson, K.; Tuominen, H.; Vakkala, M.; Liisanantti, J.H.; Karttunen, T.; Syrjälä, H.; Ala-Kokko, T.I. Brain Tight Junction Protein Expression in Sepsis in an Autopsy Series. Crit. Care 2020, 24, 385. [Google Scholar] [CrossRef]
- Torii, K.; Takagi, S.; Yoshimura, R.; Miyata, S. Microglial Proliferation Attenuates Sickness Responses in Adult Mice during Endotoxin-Induced Inflammation. J. Neuroimmunol. 2022, 365, 577832. [Google Scholar] [CrossRef] [PubMed]
- van Munster, B.C.; Aronica, E.; Zwinderman, A.H.; Eikelenboom, P.; Cunningham, C.; Rooij, S.E.J.A. de Neuroinflammation in Delirium: A Postmortem Case-Control Study. Rejuven. Res. 2011, 14, 615–622. [Google Scholar] [CrossRef] [PubMed]
- Zrzavy, T.; Höftberger, R.; Berger, T.; Rauschka, H.; Butovsky, O.; Weiner, H.; Lassmann, H. Pro-Inflammatory Activation of Microglia in the Brain of Patients with Sepsis. Neuropathol. Appl. Neurobiol. 2019, 45, 278–290. [Google Scholar] [CrossRef] [PubMed]
- Sharshar, T.; Chevret, S.; Bourdain, F.; Raphaël, J.-C. Early Predictors of Mechanical Ventilation in Guillain-Barré Syndrome. Crit. Care Med. 2003, 31, 278–283. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Z.; Wang, Y.; Zhou, R.; Li, Y.; Gao, Y.; Tu, D.; Wilson, B.; Song, S.; Feng, J.; Hong, J.-S.; et al. A Novel Role of NLRP3-Generated IL-1β in the Acute-Chronic Transition of Peripheral Lipopolysaccharide-Elicited Neuroinflammation: Implications for Sepsis-Associated Neurodegeneration. J. Neuroinflamm. 2020, 17, 64. [Google Scholar] [CrossRef]
- Ammar, M.A.; Ammar, A.A.; Wieruszewski, P.M.; Bissell, B.D.; Long, M.T.; Albert, L.; Khanna, A.K.; Sacha, G.L. Timing of Vasoactive Agents and Corticosteroid Initiation in Septic Shock. Ann. Intensive Care 2022, 12, 47. [Google Scholar] [CrossRef]
- Smith, S.M.; Padayachee, S.; Modaresi, K.B.; Smithies, M.N.; Bihari, D.J. Cerebral Blood Flow Is Proportional to Cardiac Index in Patients with Septic Shock. J. Crit. Care 1998, 13, 104–109. [Google Scholar] [CrossRef]
- Pfister, D.; Siegemund, M.; Dell-Kuster, S.; Smielewski, P.; Rüegg, S.; Strebel, S.P.; Marsch, S.C.U.; Pargger, H.; Steiner, L.A. Cerebral Perfusion in Sepsis-Associated Delirium. Crit. Care 2008, 12, R63. [Google Scholar] [CrossRef]
- Caldas, J.; Quispe-Cornejo, A.A.; Crippa, I.A.; Subira, C.; Creteur, J.; Panerai, R.; Taccone, F.S. Cerebral Autoregulation Indices Are Not Interchangeable in Patients With Sepsis. Front. Neurol. 2022, 13, 760293. [Google Scholar] [CrossRef]
- Okazaki, N.; Lankadeva, Y.R.; Peiris, R.M.; Birchall, I.E.; May, C.N. Rapid and Persistent Decrease in Brain Tissue Oxygenation in Ovine Gram-Negative Sepsis. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2021, 321, R990–R996. [Google Scholar] [CrossRef]
- Sharshar, T.; Annane, D.; de la Grandmaison, G.L.; Brouland, J.P.; Hopkinson, N.S.; Françoise, G. The Neuropathology of Septic Shock. Brain Pathol. 2004, 14, 21–33. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Xu, H.; Lin, H.; Molnar, M.; Ren, H. The Role of the Cholinergic Anti-Inflammatory Pathway in Septic Cardiomyopathy. Int. Immunopharmacol. 2021, 90, 107160. [Google Scholar] [CrossRef] [PubMed]
- Erbaş, O.; Taşkıran, D. Sepsis-Induced Changes in Behavioral Stereotypy in Rats; Involvement of Tumor Necrosis Factor-Alpha, Oxidative Stress, and Dopamine Turnover. J. Surg. Res. 2014, 186, 262–268. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Zhang, B.; Duan, S.; Qing, W.; Tan, L.; Chen, S.; Wang, Y.; Li, D.; Yang, J.; Tong, J.; et al. Small Dose of L-Dopa/Benserazide Hydrochloride Improved Sepsis-Induced Neuroinflammation and Long-Term Cognitive Dysfunction in Sepsis Mice. Brain Res. 2020, 1737, 146780. [Google Scholar] [CrossRef]
- Serantes, R.; Arnalich, F.; Figueroa, M.; Salinas, M.; Andrés-Mateos, E.; Codoceo, R.; Renart, J.; Matute, C.; Cavada, C.; Cuadrado, A.; et al. Interleukin-1beta Enhances GABAA Receptor Cell-Surface Expression by a Phosphatidylinositol 3-Kinase/Akt Pathway: Relevance to Sepsis-Associated Encephalopathy. J. Biol. Chem. 2006, 281, 14632–14643. [Google Scholar] [CrossRef] [PubMed]
- Gu, M.; Mei, X.-L.; Zhao, Y.-N. Sepsis and Cerebral Dysfunction: BBB Damage, Neuroinflammation, Oxidative Stress, Apoptosis and Autophagy as Key Mediators and the Potential Therapeutic Approaches. Neurotox. Res. 2021, 39, 489–503. [Google Scholar] [CrossRef]
- Haileselassie, B.; Joshi, A.U.; Minhas, P.S.; Mukherjee, R.; Andreasson, K.I.; Mochly-Rosen, D. Mitochondrial Dysfunction Mediated through Dynamin-Related Protein 1 (Drp1) Propagates Impairment in Blood Brain Barrier in Septic Encephalopathy. J. Neuroinflamm. 2020, 17, 36. [Google Scholar] [CrossRef]
- Huang, Z.-S.; Xie, D.-Q.; Xu, L.-J.; Huang, C.-S.; Zheng, M.; Chen, Y.-J.; Cao, Y. Tetramethylpyrazine Ameliorates Lipopolysaccharide-Induced Sepsis in Rats via Protecting Blood-Brain Barrier, Impairing Inflammation and Nitrous Oxide Systems. Front. Pharmacol. 2020, 11, 562084. [Google Scholar] [CrossRef]
- Kawakami, M.; Hattori, M.; Ohashi, W.; Fujimori, T.; Hattori, K.; Takebe, M.; Tomita, K.; Yokoo, H.; Matsuda, N.; Yamazaki, M.; et al. Role of G Protein-Coupled Receptor Kinase 2 in Oxidative and Nitrosative Stress-Related Neurohistopathological Changes in a Mouse Model of Sepsis-Associated Encephalopathy. J. Neurochem. 2018, 145, 474–488. [Google Scholar] [CrossRef]
- Wang, P.; Hu, Y.; Yao, D.; Li, Y. Omi/HtrA2 Regulates a Mitochondria-Dependent Apoptotic Pathway in a Murine Model of Septic Encephalopathy. Cell. Physiol. Biochem. 2018, 49, 2163–2173. [Google Scholar] [CrossRef]
- Jiang, Y.; Zhang, K.; Yu, Y.; Wang, Y.; Lian, N.; Xie, K.; Yu, Y. Molecular Hydrogen Alleviates Brain Injury and Cognitive Impairment in a Chronic Sequelae Model of Murine Polymicrobial Sepsis. Exp. Brain Res. 2020, 238, 2897–2908. [Google Scholar] [CrossRef] [PubMed]
- Boutin, J.A.; Jockers, R. Melatonin Controversies, an Update. J. Pineal Res. 2021, 70, e12702. [Google Scholar] [CrossRef] [PubMed]
- Kennaway, D.J. Measuring Melatonin by Immunoassay. J. Pineal Res. 2020, 69, e12657. [Google Scholar] [CrossRef] [PubMed]
- Maldonado, M.D.; Mora-Santos, M.; Naji, L.; Carrascosa-Salmoral, M.P.; Naranjo, M.C.; Calvo, J.R. Evidence of Melatonin Synthesis and Release by Mast Cells. Possible Modulatory Role on Inflammation. Pharmacol. Res. 2010, 62, 282–287. [Google Scholar] [CrossRef]
- Cecon, E.; Oishi, A.; Jockers, R. Melatonin Receptors: Molecular Pharmacology and Signalling in the Context of System Bias. Br. J. Pharmacol. 2018, 175, 3263–3280. [Google Scholar] [CrossRef] [PubMed]
- Janjetovic, Z.; Jarrett, S.G.; Lee, E.F.; Duprey, C.; Reiter, R.J.; Slominski, A.T. Melatonin and Its Metabolites Protect Human Melanocytes against UVB-Induced Damage: Involvement of NRF2-Mediated Pathways. Sci. Rep. 2017, 7, 1274. [Google Scholar] [CrossRef]
- Tordjman, S.; Chokron, S.; Delorme, R.; Charrier, A.; Bellissant, E.; Jaafari, N.; Fougerou, C. Melatonin: Pharmacology, Functions and Therapeutic Benefits. Curr. Neuropharmacol. 2017, 15, 434–443. [Google Scholar] [CrossRef]
- Lalanne, S.; Fougerou-Leurent, C.; Anderson, G.M.; Schroder, C.M.; Nir, T.; Chokron, S.; Delorme, R.; Claustrat, B.; Bellissant, E.; Kermarrec, S.; et al. Melatonin: From Pharmacokinetics to Clinical Use in Autism Spectrum Disorder. Int. J. Mol. Sci. 2021, 22, 1490. [Google Scholar] [CrossRef]
- Erren, T.C.; Reiter, R.J. Melatonin: A Universal Time Messenger. Neuro Endocrinol. Lett. 2015, 36, 187–192. [Google Scholar]
- Truong, K.K.; Lam, M.T.; Grandner, M.A.; Sassoon, C.S.; Malhotra, A. Timing Matters: Circadian Rhythm in Sepsis, Obstructive Lung Disease, Obstructive Sleep Apnea, and Cancer. Ann. Am. Thorac. Soc. 2016, 13, 1144–1154. [Google Scholar] [CrossRef]
- Li, J.; Cai, S.; Liu, X.; Mei, J.; Pan, W.; Zhong, M.; Zhang, Y. Circadian Rhythm Disturbance and Delirium in ICU Patients: A Prospective Cohort Study. BMC Anesthesiol. 2023, 23, 203. [Google Scholar] [CrossRef] [PubMed]
- Melone, M.-A.; Becker, T.C.; Wendt, L.H.; Ten Eyck, P.; Patel, S.B.; Poston, J.; Pohlman, A.S.; Pohlman, M.; Miller, A.; Nedeltcheva, A.; et al. Disruption of the Circadian Rhythm of Melatonin: A Biomarker of Critical Illness Severity. Sleep Med. 2023, 110, 60–67. [Google Scholar] [CrossRef] [PubMed]
- Sørensen, K.M.; Olesen, C.; Meyhoff, C.S.; Andersen, L.P.K. The Use of Melatonin in Danish Intensive Care Departments-A Nationwide Observational Study. Acta Anaesthesiol. 2022, 66, 833–837. [Google Scholar] [CrossRef]
- Juszczak, K.; Ziomber, A.; Machowska, A.; Furgała, A.; Dobrek, Ł.; Wyczółkowski, M.; Thor, P.J. The Ameliorating Effect of Exogenous Melatonin on Urinary Bladder Function in Hyperosmolar Bladder Overactivity and Its Influence on the Autonomic Nervous System Activity. Acta Med. 2011, 54, 63–68. [Google Scholar] [CrossRef]
- Campos, L.A.; Bueno, C.; Barcelos, I.P.; Halpern, B.; Brito, L.C.; Amaral, F.G.; Baltatu, O.C.; Cipolla-Neto, J. Melatonin Therapy Improves Cardiac Autonomic Modulation in Pinealectomized Patients. Front. Endocrinol. 2020, 11, 239. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.-T.; Tai, H.C.-H.; Chung, J.-Y.; Chen, J.-H.; Chen, W.-L. Depressed Sympathovagal Modulation Indicates Sepsis in Patients with Suspected Infection. Medicine 2020, 99, e18961. [Google Scholar] [CrossRef]
- Kohoutova, M.; Horak, J.; Jarkovska, D.; Martinkova, V.; Tegl, V.; Nalos, L.; Vistejnova, L.; Benes, J.; Sviglerova, J.; Kuncova, J.; et al. Vagus Nerve Stimulation Attenuates Multiple Organ Dysfunction in Resuscitated Porcine Progressive Sepsis. Crit. Care Med. 2019, 47, e461–e469. [Google Scholar] [CrossRef]
- Baker, J.; Kimpinski, K. Role of Melatonin in Blood Pressure Regulation: An Adjunct Anti-Hypertensive Agent. Clin. Exp. Pharmacol. Physiol. 2018, 45, 755–766. [Google Scholar] [CrossRef]
- Cipolla-Neto, J.; Amaral, F.G.; Afeche, S.C.; Tan, D.X.; Reiter, R.J. Melatonin, Energy Metabolism, and Obesity: A Review. J. Pineal Res. 2014, 56, 371–381. [Google Scholar] [CrossRef]
- Karamitri, A.; Jockers, R. Melatonin in Type 2 Diabetes Mellitus and Obesity. Nat. Rev. Endocrinol. 2019, 15, 105–125. [Google Scholar] [CrossRef]
- Mannino, G.; Caradonna, F.; Cruciata, I.; Lauria, A.; Perrone, A.; Gentile, C. Melatonin Reduces Inflammatory Response in Human Intestinal Epithelial Cells Stimulated by Interleukin-1β. J. Pineal Res. 2019, 67, e12598. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Gan, L.; Xu, Y.; Luo, D.; Ren, Q.; Wu, S.; Sun, C. Melatonin Alleviates Inflammasome-Induced Pyroptosis through Inhibiting NF-ΚB/GSDMD Signal in Mice Adipose Tissue. J. Pineal Res. 2017, 63, e12414. [Google Scholar] [CrossRef] [PubMed]
- Galano, A.; Tan, D.-X.; Reiter, R.J. Melatonin: A Versatile Protector against Oxidative DNA Damage. Molecules 2018, 23, 530. [Google Scholar] [CrossRef]
- Purushothaman, A.; Sheeja, A.A.; Janardanan, D. Hydroxyl Radical Scavenging Activity of Melatonin and Its Related Indolamines. Free Radic. Res. 2020, 54, 373–383. [Google Scholar] [CrossRef] [PubMed]
- Matuszak, Z.; Reszka, K.; Chignell, C.F. Reaction of Melatonin and Related Indoles with Hydroxyl Radicals: EPR and Spin Trapping Investigations. Free Radic. Biol. Med. 1997, 23, 367–372. [Google Scholar] [CrossRef]
- Galano, A. On the Direct Scavenging Activity of Melatonin towards Hydroxyl and a Series of Peroxyl Radicals. Phys. Chem. Chem. Phys. PCCP 2011, 13, 7178–7188. [Google Scholar] [CrossRef]
- Chang, C.-C.; Huang, T.-Y.; Chen, H.-Y.; Huang, T.-C.; Lin, L.-C.; Chang, Y.-J.; Hsia, S.-M. Protective Effect of Melatonin against Oxidative Stress-Induced Apoptosis and Enhanced Autophagy in Human Retinal Pigment Epithelium Cells. Oxid. Med. Cell. Longev. 2018, 2018, 9015765. [Google Scholar] [CrossRef]
- Aydogan, S.; Yerer, M.B.; Goktas, A. Melatonin and Nitric Oxide. J. Endocrinol. Investig. 2006, 29, 281–287. [Google Scholar] [CrossRef]
- Limson, J.; Nyokong, T.; Daya, S. The Interaction of Melatonin and Its Precursors with Aluminium, Cadmium, Copper, Iron, Lead, and Zinc: An Adsorptive Voltammetric Study. J. Pineal Res. 1998, 24, 15–21. [Google Scholar] [CrossRef]
- Romero, A.; Ramos, E.; de Los Ríos, C.; Egea, J.; Del Pino, J.; Reiter, R.J. A Review of Metal-Catalyzed Molecular Damage: Protection by Melatonin. J. Pineal Res. 2014, 56, 343–370. [Google Scholar] [CrossRef]
- Gancitano, G.; Reiter, R.J. The Multiple Functions of Melatonin: Applications in the Military Setting. Biomedicines 2022, 11, 5. [Google Scholar] [CrossRef] [PubMed]
- Colares, J.R.; Hartmann, R.M.; Schemitt, E.G.; Fonseca, S.R.B.; Brasil, M.S.; Picada, J.N.; Dias, A.S.; Bueno, A.F.; Marroni, C.A.; Marroni, N.P. Melatonin Prevents Oxidative Stress, Inflammatory Activity, and DNA Damage in Cirrhotic Rats. World J. Gastroenterol. 2022, 28, 348–364. [Google Scholar] [CrossRef] [PubMed]
- Rehman, S.U.; Ikram, M.; Ullah, N.; Alam, S.I.; Park, H.Y.; Badshah, H.; Choe, K.; Kim, M.O. Neurological Enhancement Effects of Melatonin against Brain Injury-Induced Oxidative Stress, Neuroinflammation, and Neurodegeneration via AMPK/CREB Signaling. Cells 2019, 8, 760. [Google Scholar] [CrossRef] [PubMed]
- Blanco, S.; Hernández, R.; Franchelli, G.; Ramos-Álvarez, M.M.; Peinado, M.Á. Melatonin Influences NO/NOS Pathway and Reduces Oxidative and Nitrosative Stress in a Model of Hypoxic-Ischemic Brain Damage. Nitric Oxide Biol. Chem. 2017, 62, 32–43. [Google Scholar] [CrossRef] [PubMed]
- Gou, Z.; Su, X.; Hu, X.; Zhou, Y.; Huang, L.; Fan, Y.; Li, J.; Lu, L. Melatonin Improves Hypoxic-Ischemic Brain Damage through the Akt/Nrf2/Gpx4 Signaling Pathway. Brain Res. Bull. 2020, 163, 40–48. [Google Scholar] [CrossRef]
- Barlow-Walden, L.R.; Reiter, R.J.; Abe, M.; Pablos, M.; Menendez-Pelaez, A.; Chen, L.D.; Poeggeler, B. Melatonin Stimulates Brain Glutathione Peroxidase Activity. Neurochem. Int. 1995, 26, 497–502. [Google Scholar] [CrossRef]
- Slominski, A.T.; Semak, I.; Fischer, T.W.; Kim, T.-K.; Kleszczyński, K.; Hardeland, R.; Reiter, R.J. Metabolism of Melatonin in the Skin: Why Is It Important? Exp. Dermatol. 2017, 26, 563–568. [Google Scholar] [CrossRef]
- Galano, A.; Reiter, R.J. Melatonin and Its Metabolites vs Oxidative Stress: From Individual Actions to Collective Protection. J. Pineal Res. 2018, 65, e12514. [Google Scholar] [CrossRef]
- Zhen, G.; Liang, W.; Jia, H.; Zheng, X. Melatonin Relieves Sepsis-Induced Myocardial Injury via Regulating JAK2/STAT3 Signaling Pathway. Minerva Med. 2022, 113, 983–989. [Google Scholar] [CrossRef]
- Rahim, I.; Sayed, R.K.; Fernández-Ortiz, M.; Aranda-Martínez, P.; Guerra-Librero, A.; Fernández-Martínez, J.; Rusanova, I.; Escames, G.; Djerdjouri, B.; Acuña-Castroviejo, D. Melatonin Alleviates Sepsis-Induced Heart Injury through Activating the Nrf2 Pathway and Inhibiting the NLRP3 Inflammasome. Naunyn. Schmiedebergs Arch. Pharmacol. 2021, 394, 261–277. [Google Scholar] [CrossRef]
- Kang, J.-Y.; Xu, M.-M.; Sun, Y.; Ding, Z.-X.; Wei, Y.-Y.; Zhang, D.-W.; Wang, Y.-G.; Shen, J.-L.; Wu, H.-M.; Fei, G.-H. Melatonin Attenuates LPS-Induced Pyroptosis in Acute Lung Injury by Inhibiting NLRP3-GSDMD Pathway via Activating Nrf2/HO-1 Signaling Axis. Int. Immunopharmacol. 2022, 109, 108782. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.A.; Khan, M.; Jo, M.-H.; Jo, M.G.; Amin, F.U.; Kim, M.O. Melatonin Stimulates the SIRT1/Nrf2 Signaling Pathway Counteracting Lipopolysaccharide (LPS)-Induced Oxidative Stress to Rescue Postnatal Rat Brain. CNS Neurosci. Ther. 2017, 23, 33–44. [Google Scholar] [CrossRef] [PubMed]
- Xu, S.; Li, L.; Wu, J.; An, S.; Fang, H.; Han, Y.; Huang, Q.; Chen, Z.; Zeng, Z. Melatonin Attenuates Sepsis-Induced Small-Intestine Injury by Upregulating SIRT3-Mediated Oxidative-Stress Inhibition, Mitochondrial Protection, and Autophagy Induction. Front. Immunol. 2021, 12, 625627. [Google Scholar] [CrossRef] [PubMed]
- Colunga Biancatelli, R.M.L.; Berrill, M.; Mohammed, Y.H.; Marik, P.E. Melatonin for the Treatment of Sepsis: The Scientific Rationale. J. Thorac. Dis. 2020, 12, S54–S65. [Google Scholar] [CrossRef] [PubMed]
- Lowes, D.A.; Webster, N.R.; Murphy, M.P.; Galley, H.F. Antioxidants That Protect Mitochondria Reduce Interleukin-6 and Oxidative Stress, Improve Mitochondrial Function, and Reduce Biochemical Markers of Organ Dysfunction in a Rat Model of Acute Sepsis. Br. J. Anaesth. 2013, 110, 472–480. [Google Scholar] [CrossRef]
- Escames, G.; López, L.C.; Ortiz, F.; López, A.; García, J.A.; Ros, E.; Acuña-Castroviejo, D. Attenuation of Cardiac Mitochondrial Dysfunction by Melatonin in Septic Mice. FEBS J. 2007, 274, 2135–2147. [Google Scholar] [CrossRef]
- Carrillo-Vico, A.; Lardone, P.J.; Naji, L.; Fernández-Santos, J.M.; Martín-Lacave, I.; Guerrero, J.M.; Calvo, J.R. Beneficial Pleiotropic Actions of Melatonin in an Experimental Model of Septic Shock in Mice: Regulation of pro-/Anti-Inflammatory Cytokine Network, Protection against Oxidative Damage and Anti-Apoptotic Effects. J. Pineal Res. 2005, 39, 400–408. [Google Scholar] [CrossRef]
- Arioz, B.I.; Tarakcioglu, E.; Olcum, M.; Genc, S. The Role of Melatonin on NLRP3 Inflammasome Activation in Diseases. Antioxidants 2021, 10, 1020. [Google Scholar] [CrossRef]
- Lorente, L.; Martín, M.M.; Abreu-González, P.; de la Cruz, T.; Ferreres, J.; Solé-Violán, J.; Labarta, L.; Díaz, C.; Jiménez, A.; Borreguero-León, J.M. Serum Melatonin Levels Are Associated with Mortality in Severe Septic Patients. J. Crit. Care 2015, 30, 860. [Google Scholar] [CrossRef]
- Alamili, M.; Bendtzen, K.; Lykkesfeldt, J.; Rosenberg, J.; Gögenur, I. Effect of Melatonin on Human Nighttime Endotoxaemia: Randomized, Double-Blinded, Cross-over Study. Vivo Athens Greece 2014, 28, 1057–1063. [Google Scholar]
- Alamili, M.; Bendtzen, K.; Lykkesfeldt, J.; Rosenberg, J.; Gögenur, I. Melatonin Suppresses Markers of Inflammation and Oxidative Damage in a Human Daytime Endotoxemia Model. J. Crit. Care 2014, 29, e9–e184. [Google Scholar] [CrossRef] [PubMed]
- Galley, H.F.; Lowes, D.A.; Allen, L.; Cameron, G.; Aucott, L.S.; Webster, N.R. Melatonin as a Potential Therapy for Sepsis: A Phase I Dose Escalation Study and an Ex Vivo Whole Blood Model under Conditions of Sepsis. J. Pineal Res. 2014, 56, 427–438. [Google Scholar] [CrossRef] [PubMed]
- Aisa-Alvarez, A.; Soto, M.E.; Guarner-Lans, V.; Camarena-Alejo, G.; Franco-Granillo, J.; Martínez-Rodríguez, E.A.; Gamboa Ávila, R.; Manzano Pech, L.; Pérez-Torres, I. Usefulness of Antioxidants as Adjuvant Therapy for Septic Shock: A Randomized Clinical Trial. Med. Kaunas Lith. 2020, 56, 619. [Google Scholar] [CrossRef]
- Taher, A.; Shokoohmand, F.; Abdoli, E.; Mohammadi, Y.; Mehrpooya, M. A Pilot Study on the Melatonin Treatment in Patients with Early Septic Shock: Results of a Single-Center Randomized Controlled Trial. Ir. J. Med. Sci. 2022, 191, 1913–1924. [Google Scholar] [CrossRef]
- Mansilla-Roselló, A.; Hernández-Magdalena, J.; Domínguez-Bastante, M.; Olmedo-Martín, C.; Comino-Pardo, A.; Escames, G.; Acuña-Castroviejo, D. A Phase II, Single-Center, Double-Blind, Randomized Placebo-Controlled Trial to Explore the Efficacy and Safety of Intravenous Melatonin in Surgical Patients with Severe Sepsis Admitted to the Intensive Care Unit. J. Pineal Res. 2023, 74, e12845. [Google Scholar] [CrossRef]
- Aisa-Álvarez, A.; Pérez-Torres, I.; Guarner-Lans, V.; Manzano-Pech, L.; Cruz-Soto, R.; Márquez-Velasco, R.; Casarez-Alvarado, S.; Franco-Granillo, J.; Núñez-Martínez, M.E.; Soto, M.E. Randomized Clinical Trial of Antioxidant Therapy Patients with Septic Shock and Organ Dysfunction in the ICU: SOFA Score Reduction by Improvement of the Enzymatic and Non-Enzymatic Antioxidant System. Cells 2023, 12, 1330. [Google Scholar] [CrossRef] [PubMed]
- Galley, H.F.; Allen, L.; Colin, P.J.; Galt, S.P.; Webster, N.R. Dose Assessment of Melatonin in Sepsis (DAMSEL2) Study: Pharmacokinetics of Two Doses of Oral Melatonin in Patients with Sepsis. J. Pineal Res. 2022, 73, e12830. [Google Scholar] [CrossRef] [PubMed]
- Ji, M.-H.; Xia, D.-G.; Zhu, L.-Y.; Zhu, X.; Zhou, X.-Y.; Xia, J.-Y.; Yang, J.-J. Short- and Long-Term Protective Effects of Melatonin in a Mouse Model of Sepsis-Associated Encephalopathy. Inflammation 2018, 41, 515–529. [Google Scholar] [CrossRef]
- Wang, X.; Xue, G.-X.; Liu, W.-C.; Shu, H.; Wang, M.; Sun, Y.; Liu, X.; Sun, Y.E.; Liu, C.-F.; Liu, J.; et al. Melatonin Alleviates Lipopolysaccharide-Compromised Integrity of Blood-Brain Barrier through Activating AMP-Activated Protein Kinase in Old Mice. Aging Cell 2017, 16, 414–421. [Google Scholar] [CrossRef]
- Liu, W.-C.; Wang, X.; Zhang, X.; Chen, X.; Jin, X. Melatonin Supplementation, a Strategy to Prevent Neurological Diseases through Maintaining Integrity of Blood Brain Barrier in Old People. Front. Aging Neurosci. 2017, 9, 165. [Google Scholar] [CrossRef]
- Zhou, Q.; Lin, L.; Li, H.; Wang, H.; Jiang, S.; Huang, P.; Lin, Q.; Chen, X.; Deng, Y. Melatonin Reduces Neuroinflammation and Improves Axonal Hypomyelination by Modulating M1/M2 Microglia Polarization via JAK2-STAT3-Telomerase Pathway in Postnatal Rats Exposed to Lipopolysaccharide. Mol. Neurobiol. 2021, 58, 6552–6576. [Google Scholar] [CrossRef]
- Ali, T.; Rahman, S.U.; Hao, Q.; Li, W.; Liu, Z.; Ali Shah, F.; Murtaza, I.; Zhang, Z.; Yang, X.; Liu, G.; et al. Melatonin Prevents Neuroinflammation and Relieves Depression by Attenuating Autophagy Impairment through FOXO3a Regulation. J. Pineal Res. 2020, 69, e12667. [Google Scholar] [CrossRef]
- Zhao, L.; An, R.; Yang, Y.; Yang, X.; Liu, H.; Yue, L.; Li, X.; Lin, Y.; Reiter, R.J.; Qu, Y. Melatonin Alleviates Brain Injury in Mice Subjected to Cecal Ligation and Puncture via Attenuating Inflammation, Apoptosis, and Oxidative Stress: The Role of SIRT1 Signaling. J. Pineal Res. 2015, 59, 230–239. [Google Scholar] [CrossRef] [PubMed]
- Mehrpooya, M.; Mazdeh, M.; Rahmani, E.; Khazaie, M.; Ahmadimoghaddam, D. Melatonin Supplementation May Benefit Patients with Acute Ischemic Stroke Not Eligible for Reperfusion Therapies: Results of a Pilot Study. J. Clin. Neurosci. 2022, 106, 66–75. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.W.; Chen, T.Y.; Hung, C.Y.; Tai, S.H.; Huang, S.Y.; Chang, C.C.; Hung, H.Y.; Lee, E.J. Melatonin Protects Brain against Ischemia/Reperfusion Injury by Attenuating Endoplasmic Reticulum Stress. Int. J. Mol. Med. 2018, 42, 182–192. [Google Scholar] [CrossRef]
- Liu, Z.-J.; Ran, Y.-Y.; Qie, S.-Y.; Gong, W.-J.; Gao, F.-H.; Ding, Z.-T.; Xi, J.-N. Melatonin Protects against Ischemic Stroke by Modulating Microglia/Macrophage Polarization toward Anti-Inflammatory Phenotype through STAT3 Pathway. CNS Neurosci. Ther. 2019, 25, 1353–1362. [Google Scholar] [CrossRef]
- Zhao, Y.; Wang, H.; Chen, W.; Chen, L.; Liu, D.; Wang, X.; Wang, X. Melatonin Attenuates White Matter Damage after Focal Brain Ischemia in Rats by Regulating the TLR4/NF-ΚB Pathway. Brain Res. Bull. 2019, 150, 168–178. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Sun, Y.; Li, F.; Zhang, X.; Hu, X.; Zhao, X.; Li, Y.; Li, H.; Zhang, J.; Liu, W.; et al. Modulation of A7nAchR by Melatonin Alleviates Ischemia and Reperfusion-Compromised Integrity of Blood-Brain Barrier Through Inhibiting HMGB1-Mediated Microglia Activation and CRTC1-Mediated Neuronal Loss. Cell. Mol. Neurobiol. 2022, 42, 2407–2422. [Google Scholar] [CrossRef] [PubMed]
- Krzyzaniak, K.; Krion, R.; Szymczyk, A.; Stepniewska, E.; Sieminski, M. Exploring Neuroprotective Agents for Sepsis-Associated Encephalopathy: A Comprehensive Review. Int. J. Mol. Sci. 2023, 24, 10780. [Google Scholar] [CrossRef]
| Author of the Study (Year of Publication) | Number of Participants | Study Design, Dose of Melatonin Assessed | Assessed Outcome | Conclusions |
|---|---|---|---|---|
| Alamili et al. (2014) [110] | 12 healthy volunteers with experimentally evoked endotoxaemia | Randomized, placebo-controlled, double-blinded cross-over trial, comparing infusion of 100 mg i.v. melatonin with placebo | Concentrations of pro- and anti-inflammatory markers in plasma of participants during night | Melatonin had no effect on concentratons of markers during the night |
| Alamili et al. (2014) [111] | 12 healthy volunteers with experimentally evoked endotoxaemia | Randomized, placebo-controlled, double-blinded cross-over trial, comparing infusion of 100 mg i.v. melatonin with placebo | Concentrations of pro- and anti-inflammatory markers in plasma of participants during day | Melatonin reduced concentrations of pro-inflammatory biomarkers during the day |
| Aisa-Álvarez et. al. (2020) [113] | 97 subjects divided into 5 subgroups | Randomized, controlled, triple-masked, and with parallel assignment clinical trial with a control group without treatment. Comparison of 4 molecules (vitamin C, vitamin E, n-acetylcysteine, melatonin—50 mg p.o. daily) and no antioxidant treatment | Concentrations of inflammation and oxidative stress markers in plasma | Reduction in procalcitonine and lipid peroxidation in subjects treated with melatonin, paralleled with reduction in sepsis severity measured with SOFA score |
| Taher et al. (2022) [114] | 40 patients with septic shock | Prospective, two-arm, double-blind, randomized clinical trial; 50 mg melatonin given p.o. through 5 days was compared with placebo. | Change in SOFA score, need for mechanical ventilation, required dosage of vasopressor | Insignificant reduction in SOFA score, percentage of patients requiring ventilation and usage of vasopressors in melatonin-treated group |
| Mansilla-Roseló et al. (2023) [115] | 29 patients (14 in placebo group, 15 in melatonin group) | Unicenter, randomized, placebo-controlled, double-blind trial; 60 mg of i.v. given melatonin was compared to placebo therapy | Change in SOFA score, concentrations of inflammatory markers, oxidative stress status | Treatment with melatonin led to decrease in SOFA score and in concentrations of inflammatory markers and improvement in oxidative stress status |
| Aisa-Álvarez et al. (2023) [116] | 131 subjects divided into 5 subgroups | Randomized, controlled, triple-masked, and with parallel assignment clinical trial with a control group without treatment. Comparison of 4 molecules (vitamin C, vitamin E, n-acetylcysteine, melatonin—50 mg p.o. daily) and no antioxidant treatment | Change in SOFA score, change in concentrations of inflammatory markers and antioxidant activity | Therapy with melatonin was related to decrease in SOFA score, decrease in inflammatory markers and improvement in antioxidant activity |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sieminski, M.; Szaruta-Raflesz, K.; Szypenbejl, J.; Krzyzaniak, K. Potential Neuroprotective Role of Melatonin in Sepsis-Associated Encephalopathy Due to Its Scavenging and Anti-Oxidative Properties. Antioxidants 2023, 12, 1786. https://doi.org/10.3390/antiox12091786
Sieminski M, Szaruta-Raflesz K, Szypenbejl J, Krzyzaniak K. Potential Neuroprotective Role of Melatonin in Sepsis-Associated Encephalopathy Due to Its Scavenging and Anti-Oxidative Properties. Antioxidants. 2023; 12(9):1786. https://doi.org/10.3390/antiox12091786
Chicago/Turabian StyleSieminski, Mariusz, Karolina Szaruta-Raflesz, Jacek Szypenbejl, and Klaudia Krzyzaniak. 2023. "Potential Neuroprotective Role of Melatonin in Sepsis-Associated Encephalopathy Due to Its Scavenging and Anti-Oxidative Properties" Antioxidants 12, no. 9: 1786. https://doi.org/10.3390/antiox12091786
APA StyleSieminski, M., Szaruta-Raflesz, K., Szypenbejl, J., & Krzyzaniak, K. (2023). Potential Neuroprotective Role of Melatonin in Sepsis-Associated Encephalopathy Due to Its Scavenging and Anti-Oxidative Properties. Antioxidants, 12(9), 1786. https://doi.org/10.3390/antiox12091786








