Abstract
Background/Objectives: Dual task (DT) training consists of practicing exercises while simultaneously performing a concurrent motor or cognitive task. This training modality seems to have beneficial effects on both domains. Various forms of DT training have been implemented for older adults in recent years, but no official guidelines currently exist. This review sought to analyze the studies published on this topic in the last ten years and provide a standard operating procedure (SOP) for healthy older adults in this context. Methods: The review collected articles from PubMed, Web of Science, and Scopus, adopting a designated set of keywords. Selected manuscripts and relevant information were selected, extrapolated, including information related to the training frequency, intensity, time, and type, and secondary tasks adopted. The secondary tasks were grouped according to previously published studies, and the SOP was created based on the frequency of the parameters collected from the included articles. Results: A total of 44 studies were included in the review. Based on the results, the SOP recommends postural balance or resistance training as primary tasks, combined with a mental tracking task as a secondary component. Two 60-min sessions per week for at least 12 weeks are required to achieve measurable results. Conclusions: Despite heterogeneity in the literature reviewed, the findings support the proposal of a SOP to guide future research on DT training in healthy older adults. Given its feasibility and positive effects on both motor and cognitive functions, this type of training can also be implemented in everyday settings.
1. Introduction
The dual task (DT) concept, introduced at the beginning of the 21st century, consists of performing a primary and a secondary task simultaneously [1]. The tasks, either primary or secondary, can be motor or cognitive [2]. The aim is to shift attention between the two tasks, and this can be modulated by controlling the difficulty of either the primary or secondary task [3]. The DT concept aims to create a more challenging condition. Indeed, a reduction in postural control (in static condition) has been observed in older adults during DT situations [4]. This concept has also been applied in dynamic situations, such as walking, and in falls among older adults [5]. In the literature, different secondary tasks exist, such as manual tasks, reaction time tasks, discrimination and decision-making tasks, mental tracking tasks, verbal fluency tasks, and working memory tasks [2,6], and they are widely adopted during testing and training. Two recent reviews helped the community to better standardize secondary tasks during static [2] and dynamic conditions [6], providing useful guidelines for the evaluation.
Dual task testing aims to reveal individual risks through the concurrent combination of a primary task (such as a postural balance test or a walking test) and a secondary task (such as a manual or a cognitive task). Examples include studies on postural balance [7] and gait ability [8], which are also adopted to predict possible future falls in healthy [9], and pathological populations [10]. This testing methodology is also adopted to assess cognitive performance [11], influence manual dexterity [12], and evaluate mobility [13,14]. Another example of DT testing is its use as a predictive tool for cognitive impairment [15,16]. Considering the various domains in which the DT concept is applied, it also shows strong potential as a training tool. Consequently, greater attention should be given to DT training.
Training in a DT context means that traditional training can be combined with cognitive training or with a concurrent motor task, or that two cognitive tasks can be combined [3]. This training methodology takes different forms and can be adapted to the participant’s level and context [11]. The advantage of DT training lies in its benefits for both motor and cognitive functions. Indeed, this methodology significantly engages with the left prefrontal cortex and the parietal area [17]. In young adults, DT situations have been shown to increase activity in the prefrontal cortex [18]. This brain region is considered as an executive hub, and is strongly associated with executive function [19]. Consequently, DT training improves executive function more effectively than single cognitive training [20,21]. Dual task training, proposed for healthy older adults, has a positive effect on postural balance [22,23] and also reduces the risk of falls [3]. It is also used for walking speed training [24]. Furthermore, it has shown positive results on cognition [11]. Cognitive and physical function can be improved with DT training not only in heathy individuals, but also in people with dementia or mild cognitive impairment [15,16], or in people with Parkinson’s disease [25], neurological impairment [26], in people suffering from chronic stroke [23], and in those with multiple sclerosis and Alzheimer’s disease [27]. Generally, it seems that this training methodology works in people with neurologic disorders to improve gait, postural balance, and cognition [28].
The American College of Sports Medicine (ACSM) periodically provides updated and clear guidelines for exercise testing and prescription [29]. Specific indications for training frequency, intensity, time, type, volume, and progression (FITT-VP) are provided for different training methodologies across various populations, both healthy and clinical [29]. Despite the DT concept with different testing and training protocols being proposed at the beginning of the 21st century, clear and standardized guidelines have not yet been created. Unfortunately, DT training includes diverse and inconsistent protocols, limiting comparisons between studies [28]. Therefore, a standardized DT training protocol does not exist [15], and there is considerable heterogeneity in this field [26]. The research gap that still exists in this training methodology lies in the variety of approaches, and at times, the impracticality of applying them in everyday contexts [11]. One review highlighted that gaps still exist on the optimal dose and the best approach to adopt [25], and there is also a lack of reporting on key implementation details [11]. Furthermore, it would be valuable to study the most effective training protocols tailored for specific diagnostic groups [28], but this is only possible if a common starting point is established. Standard operating procedures (SOPs) are present in the literature and are defined as detailed documents outlining each step of a procedure [30,31]. They are also used in the field of sports science, providing guidelines and ensuring that procedures are replicable and comparable [32]. Because it is essential to design feasible interventions and achieve positive outcomes, the objective of the present study was to investigate DT training in healthy older adults aimed at improving physical and cognitive function and to propose a SOP for DT training in this population.
2. Materials and Methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA-ScR) checklist and explanation for scoping reviews [33] was followed. For more details, the PRISMA checklist is included in the Supplementary Materials. The work has not been registered on a specific database, but the protocol was previously written and followed step by step.
2.1. Eligibility Criteria
The eligibility criteria of this review were, as suggested by the PRISMA checklist, for a Population, Intervention, Comparison, Outcomes, and Study design (PICO-S). The population investigated was composed of healthy older adults (65 years and above). Studies were excluded if any kind of physical (i.e., muscle or bone injuries or problems, inflammatory joint conditions, pathologies) or cognitive (i.e., dementia, cognitive deterioration) impairment had been investigated. Studies were also excluded if a specific population, such as people with Parkinson’s disease, multiple sclerosis, fibromyalgia, and similar conditions, had been investigated.
The intervention had to be characterized by training based on the DT principle. The training had to include a primary task performed with another task, called a secondary task [1]. The primary task had to be motor training, while the secondary task could be a motor or a cognitive task. Only interventions that did not require specific technologies (i.e., televisions, computers, tablets, consoles, or three-dimensional environments) were considered to make our findings replicable in any context with zero costs. Studies that adopted virtual reality, specific games and consoles, or specific settings were excluded. Specific dance programs not based on dual-tasking were also excluded. Acute interventions were excluded as we aimed to focus attention on something created to obtain effects in the long-term period.
Because a meta-analysis was not performed, our types of comparison and outcomes were all accepted. Our main goal was centered on the protocol adopted in the studies.
Studies included had to present a study design that could be cross-sectional, longitudinal, correlational (both randomized and non-randomized controlled trials, and quasi-randomized studies), or intervention studies. The included studies had to be original, peer-reviewed, published in international journals, and had to be written in English. Pre-print and protocol studies were excluded. Other kinds of study designs or those written in a different language were excluded. Considering the trend of published articles on PubMed, the studies were included if published from 2015 (in the last ten years).
2.2. Data Collection
Studies were collected from three different electronic databases (PubMed, Web of Science, and Scopus). All articles published until 25 March 2025 were included. Four groups of keywords were adopted and matched with the Boolean operators AND/OR to create the following string:
- Group 1: dual task, double task;
- Group 2: training, protocol, practice, exercise;
- Group 3: cognitive function, cognition;
- Group 4: older adults, elderly.
The string generated was composed of: (dual task OR double task) AND (training OR protocol OR practice OR exercise) AND (cognitive function OR cognition) AND (older adults OR elderly).
The string was adopted in the three databases in the current form. No filters were used.
2.3. Study Record
The software EndNote (EndNote version X8; Thompson Reuters, New York, NY, USA) was adopted to manage the studies. In the first step, duplicates were searched and eliminated. In the second step, two investigators independently performed the study selection by applying the eligibility criteria. The title, abstract, and full-length articles were screened in this order. The studies were included if both investigators agreed, otherwise, the coordinator made the final decision. The investigators were not blinded to the information related to the authors or associated institutions.
When all of the articles had been selected, data regarding the sample size and age of the population, intervention duration, frequency, intensity, time, and type, any adverse events, adherence and dropout rates, single task, and secondary tasks were collected. The information on the secondary task proposed was collected according to the macro-categories presented in previously published articles [2,6]. Furthermore, information about the objective and the DT efficacy was also detected. The SOP was created based on the frequency of the parameters considered (frequency, intensity, time, type, primary and secondary task typology) in the included studies. Data were presented through tables and discussed narratively.
3. Results
A total of 2915 articles (PubMed, 1624; Web of Science, 774; and Scopus, 517) were identified. After duplicate removal, 2098 studies were screened against the eligibility criteria. After title selection, 376 abstracts were screened, and a final number of 211 articles remained for the full-text review. After applying the full-text eligibility criteria, a final number of 44 original articles were included in the review. The selection process is presented in Figure 1.
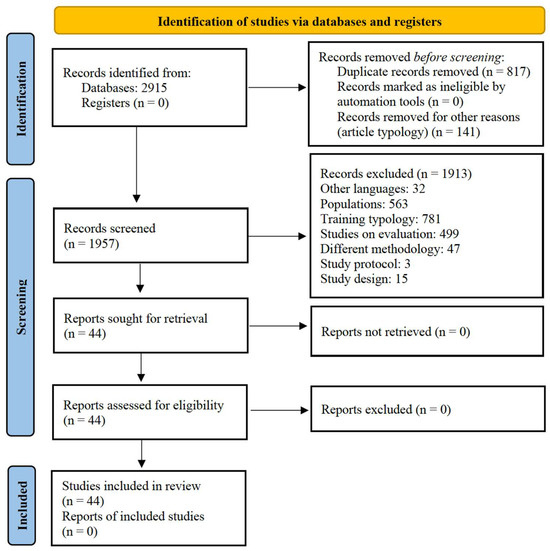
Figure 1.
PRISMA 2020 flow diagram for the scoping reviews, which only included searches of the databases and registers.
3.1. Characteristics of the Studies
A total of 2568 participants were included in the studies, with a sample size ranging from 11 [34] to 158 [35]. The mean age ranged from 62 [36] to 85 years [37,38,39,40]. Two studies [41,42] did not report the participants’ ages but only general demographic information. Two studies reported an age range [37,43]. Overall, the adherence to the training was above 70%, with only one article reporting an adherence below this percentage. The dropout rate was also low, with data showing around 10% of dropouts. Only one article reported a high dropout rate of 50%. Information related to the studies included is presented in Table 1.

Table 1.
Articles overview.
3.2. Description of the Intervention
The protocol duration ranged from three training sessions [43] to 26 weeks [77]. Most of the studies opted for a 12-week intervention. Some studies presented the data in terms of sessions: 12 [35], 16 [52], and 24 sessions were reported [85]. Four studies did not report the length of the intervention, but it appeared to be long-term. Most of the studies proposed two or three sessions per week; one study did not report this information, and one study adopted a previously published protocol [66]. A session duration of 60 min was mostly adopted. Ranges such as 54–60 and 60–75/80 min were also reported in the included studies.
Most of the studies adopted progressive intensity. Seven studies clearly reported how the intensity was monitored, two adopted the percentages (60–70% and 70–85%) of maximal heart rate, and three adopted the rate of perceived effort. Two studies adopted the 1 repetition maximal. Six studies did not provide information about the intensity or type of intervention. More details are presented in Table 2.

Table 2.
Number of studies for the parameters of protocol duration, session number, and duration.
To structure the training session, “warm-up, conditioning, and cool-down” phases were adopted in 18 studies. The detailed length of each phase can be found in Table 1 because most of the studies adopted different protocols. Only the warm-up or the cool-down phases were described in one study. Interesting, amusing, and social tasks were adopted in the cool-down by Blasco-Lafarga and colleagues [65], and beginning and finishing rituals were included in the study of Rosado and colleagues [97]. Fifteen minutes of mental gymnastics (finger motions) during the warm-up was adopted by Yokoyama and colleagues [108]. A useful addition was the 10-min communication time proposed by Sok and colleagues [104]. Regarding the content of the programs, some studies included activities of daily living or similar patterns within resistance, endurance, postural balance, or mobility training [67,71,85,106]. Specific and previously published protocols were adopted in 20 studies, most of which were used once [38,46,50,51,54,55,56,57,58,59,60,61,62,63,64,66,72,74,76,78,82,84,95,96,99,101,102,103,105,107]. The protocols of Halvarsson (2015) and Wollesen and colleagues [63,70] were each adopted in two studies [69,80] and the protocols of Arrieta and colleagues and Rodriguez-Larrad and colleagues [95,96] twice [38,100]. The ACSM guidelines were cited in four studies, but different citations were adopted [48,54,68]. The American Geriatrics Society Panel on Exercise and Osteoarthritis [49] guidelines were adopted in one study.
The most studied aspects were elements related to cognitive function. Postural balance, walking or gait characteristics, and physical fitness were also investigated multiple times. More details are provided in Table 3.

Table 3.
Number of studies for aspects evaluated in the included studies.
3.3. Characteristics of the Dual-Task Training
The primary tasks, secondary task interventions, the outcomes investigated, and their effects are presented in Table 4. The effects of the interventions were mostly positive, with two studies reporting a small effect, five studies reporting no differences with DT training, and the study of Rezola-Pardo and colleagues [39] showing a negative trend. Sequential and simultaneous cognitive and physical training was adopted by Chuang and colleagues [35].

Table 4.
Training characteristics, variables considered, and effects obtained.
The frequency of the primary and secondary tasks is presented in Table 5. In the included studies, motor tasks were mainly proposed as a primary tasks such as postural balance, resistance training exercises, gait and walking exercises, aerobic training, stepping, mobility exercise, and daily life activities. Less adopted training methodologies are presented in Table 5. Previously published protocols [63,72,82,95,96,99,101,102,103,105,111,122] were adopted in eight studies.

Table 5.
Number of studies for each parameter of the primary and secondary tasks.
The most adopted secondary tasks were mental tracking tasks. Among them, mathematical calculations, counting backward, or solving anagrams were widely adopted. These tasks were closely followed by working memory tasks such as short-term memory (i.e., evoking names, remembering words and how they are listed, items, shapes, colors, or numbers previously said, counting the days of the week), long-term memory (i.e., completing proverbs or traditional songs), and semantic memory. Verbal fluency tasks were also widely adopted including reading and talking, reverse spelling, and singing songs. Less frequently adopted tasks were reaction time tasks (e.g., simple and choice, using visual and auditory stimuli) and discrimination-decision making tasks (e.g., the ability to inhibit automated responses, problem-solving, task prioritization, and task switching). Ten studies adopted other types of tasks, such as tooth brushing, as in the study by Granacher and colleagues [75]. The Shiritori, a Japanese word chain game in which one player has to say a word starting with the last character of the word given by the previous player, was adopted by Yokoyama and colleagues [108]. Talking was adopted by Anandh and colleagues [43] and a visuospatial skills task by Chuang and colleagues [35], while visual tasks were used by de Maio Nascimento and colleagues [71]. Ansai and colleagues [47] adopted cards of different colors with a description of different activities, requiring the participants to say and execute the action based only on observing the card color. Singing unknown songs, memorizing, and learning the lyrics of songs played in previous sessions was adopted by Nieto-Guisado and colleagues [90]. The emotional prosody task was adopted by Jardim and colleagues [85]. No details were provided in the study by Ho and colleagues [81]. Examples of motor tasks adopted include holding half-filled glasses with both hands, carrying and/or manipulating objects, bimanual tapping, throwing or holding a ball or a bag, balancing a cup on the palm, and tossing a ball from one hand to the other hand. Seventeen studies adopted previously published protocols. The protocol by Halvarsson and colleagues [70] was adopted in two studies [79,80] as was the protocol by Rezola-Pardo and colleagues [103], which was also adopted by two studies [38,39]. Detailed information about the number of studies for each motor and cognitive task is provided in Table 4.
4. Discussion
The literature review highlighted heterogeneity and uncertainty in the protocol designs. Despite this, from the protocols of the included studies, a SOP as proposed for healthy older adults, as presented in Table 6, and is discussed in-depth below.

Table 6.
Standard operating procedure for a dual-task training in healthy older adults.
The ACSM guidelines for older adults were followed by different authors, and the primary task proposed in the DT training could follow the latest ACSM guidelines suggested [29] for the reference population. It seems that for the length of the intervention, if the participants were regular and attended the weekly sessions, 12 weeks or more were necessary to obtain positive results [27]. Our SOP, in line with the literature [123], suggests a progression in difficulty as well as task specificity to obtain better outcomes on cognitive functions. The most adopted primary task in the included studies was postural balance, both static and dynamic, such as gait exercises. In line with a recent article [124], postural balance training involves modifying the body position with movement and gesture. It should also change the nature of the ground surface or environment, or use sports equipment [124]. The optimal postural balance training should include various postural tasks that people encounter in physical practice [124]. Reviews [8,23] that examined DT during gait and balance training confirmed more positive outcomes than single task training. This supports the use and feasibility of postural balance training integrated with the DT concept. Consequently, as a practical guide, we strongly suggest including this component to prevent falls or to improve activities of daily living. Among the included studies, resistance training was also widely adopted. When resistance training is proposed, trainers or researchers should consider using machine-based strength training devices. According to the literature [125], this makes it easier to control the volume and intensity (to prevent cognitive components from interfering with strength training). Furthermore, resistance training should also include power training [125]. An example could be combining this training modality with a cognitive task such as a rapid reaction task [125]. From a practical point of view, resistance training must be properly monitored, and the participants provided with adequate instructions and technique to ensure safety [126]. In terms of dosage, 5–8 repetitions with 2–3 sets at 50–80% of 1 RM should be proposed. The trainer should offer 1–2 exercises for the major muscle groups, 2–3 times a week. These guidelines were drawn from both the included studies and the literature [29,126]. If well-planned, resistance training and power training should be included as they have positive effects on muscle mass, strength, and the risk of falls [127]. Additional benefits include musculoskeletal health, psychological well-being, sleep quality, and the management of chronic conditions [128]. Less adopted primary tasks in the included articles were aerobic exercises, mobility, and daily life activity-based exercises. From a practical point of view, high-intensity interval training or moderate-intensity continuous training should be proposed. These approaches yield positive outcomes on cardio-respiratory function, fat distribution, and cognitive function [129]. According to the literature, high-intensity interval training not only benefits the cardiometabolic system, but also improves quality of life [130], while mobility training enhances functional mobility [131]. Activities of daily life, when used as exercise, facilitate the transfer of training effects into daily living [24].
The most frequently adopted secondary tasks in the included studies were mental tracking tasks. These included counting backward, arithmetic tasks, and sequence tasks, three widely adopted categories [2]. From a practical standpoint, counting backward is easy to administer and modulate in terms of difficulty. Counting backward by one is the easiest, followed by three, with seven being the most challenging [2]. Arithmetic tasks (e.g., mathematical problems [2]) can be presented in a game-like format, as can sequence tasks. Mental tracking tasks significantly impact the motor system. A study on walking in young and older adults showed that these tasks, when proposed during walking, shortened stride length, increased stride time, and raised the stride length and variability [132]. This suggests that simple, easy-to-propose tasks can be used to create challenging practice conditions in everyday practice. Working memory tasks were also widely adopted. Common types included n-back tasks, backward digit recall, the Brooks’ spatial/nonspatial memory task, and digit or word memory tasks (e.g., memorizing the greatest number of numbers or words) [2]. According to the literature [133], a strong link exists between physical activity and working memory involving the capacity and efficiency of attentional resources. Working memory training improves memory performance, especially visual working memory [134], which may enhance overall cognitive functioning [135]. Verbal fluency tasks were the third most frequently adopted in the included studies. Examples included sentence completion and repeating numbers aloud [2]. A study on people with Alzheimer’s disease showed that walking speed decreased during a verbal fluency task, [136], which suggests that verbalization increases cognitive–motor interference [23], raising the attentional demand during post-lexical processing [137]. Overall, verbal fluency, discrimination and decision-making, and reaction time tasks appear less challenging than mental tracking and working memory tasks when combined with postural control [138]. The impact of cognitive tasks depends on the attentional resources each task requires, and limitations in central capacity to allocate an appropriate level of attention can influence performance [139].
Motor/manual secondary tasks were also adopted several times such as holding a glass of water or an object, finger tapping, and similar activities [2]. One study found that fallers were less accurate than non-fallers when placing an object during a postural stability task [140]. Unlike cognitive-motor combinations (which use different neuronal networks), motor-motor combinations use the same resources. According to the cross-talk model, similar domain tasks interfere with one another [141]. The bottleneck principle also suggests that two tasks relying on the same neural processors must be performed sequentially to avoid performance interference [142].
It is important that trainers modulate the intensity of the secondary task in both motor-cognitive and motor-motor combinations. According to the literature [24], task prioritization should be varied between primary and secondary tasks. When planning DT training, the personalization and adaptation of both primary and secondary tasks is essential. Training must be challenging but not discouraging, as motivational aspects are crucial to maintain adherence [125].
In terms of outcomes, DT training has positive effects on cognitive and executive function. The literature shows that DT activity leads to structural brain changes such as in the gray (visual motion complex area) and white matter volume [143]. Even in older adults, cognitive and exercise training can induce cognitive plasticity [144]. Moreover, older adults demonstrate the ability to increase neural resource allocation [145].
From the findings of this review, DT training also improves static and dynamic postural balance. The literature shows that adding a motor task to a balance task triggers brain network reorganization, increasing interregional connectivity and central resource expansion [146]. Given that DT relies on attentional resource allocation during postural control [147,148], DT postural training offers a high cognitive challenge. In the included studies, improvements in general physical fitness, falls prevention, mobility, and quality of life were observed. Another review confirmed that more than two sessions per week, each over 30 min, improved global cognition, executive and physical functions, working memory, and postural balance in both healthy and cognitively impaired older adults [16,149]. Dual tasking efficacy is particularly enhanced in individuals with declines in vision, proprioception, and vestibular function [150].
The study had several limitations. First, no risk of bias or article quality assessment was performed due to methodological heterogeneity. Second, the effect sizes were not reported. The SOP was based only on parameter frequency, without considering the study sample sizes. Narrative synthesis was used, as a meta-analysis was not feasible due to heterogeneity in the secondary tasks and outcomes measures, limiting the strength of the conclusions. Outcomes were considered in general, without categorization, to maintain focus on the training protocols. Training volume variability made statistical analysis unfeasible.
Future studies adopting common protocols could help in quantifying the real impact of DT training, and evaluate outcomes more rigorously. This review did not address the use of technology to ensure SOP applicability across settings. Even if studies exist on the use of exergames as cognitive training [151], this exercise methodology was also excluded due to its distinct mechanisms. However, technology-based DT interventions may be effective on global cognitive function, inhibitory control, and processing speed [123]. Future research should include original field studies and randomized controlled trials directly comparing different types of cognitive tasks (e.g., spatial memory vs. calculation) combined with the same motor tasks. It would be also interesting to study DT training as a tool for the performance of fine motor skills such as manual dexterity. Indeed, different populations suffer from hand tremors, and one recent study investigated the correlation between hand exercise and hand tremors [152], so its understanding in a DT contest could also provide more information. It would also be valuable to create population-specific SOPs, particularly for those with cognitive disorders, considering the DT training role in the prevention and deceleration of cognitive impairments [153]. Standardized trials should better assess the progression, modulation, and task difficulty, tailored to participant characteristics. Only then will true progress in SOP development be achieved. Our SOP aims to highlight the need for greater clarity in this emerging field.
5. Conclusions
The topic of DT training for older adults presents a diverse and heterogenous literature. Comparisons between protocols were limited by the variability of the articles, compromising the overall quality of the research. The SOP proposed for healthy older adults consists of two sessions per week, each lasting 60 min, with adapted and progressively intensified exercises. Postural balance, resistance, aerobic, and mobility training are included. The secondary tasks proposed are primarily mental tracking or working memory tasks. The SOP is intended as a starting point, with the hope that future studies will build upon and refine this direction.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/brainsci15080785/s1, Table S1: Preferred reporting items for systematic review and meta-analyses extension for scoping review (PRISMA-ScR) checklist.
Author Contributions
L.P. and A.A. worked equally on the manuscript in the conceptualization, methodology, analysis; data curation, writing—original draft preparation, and writing—review and editing. A.C. contributed in the writing—review and editing. G.M. contributed to the supervision, project administration, and funding acquisition. All authors have read and agreed to the published version of the manuscript.
Funding
This research was carried out as part of the PIACERI 2024–2026 project entitled “PreRoF4 OA” financed by BIOMETEC department, University of Catania.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| DT | Dual task |
| SOP | Standard operating procedure |
References
- Woollacott, M.; Shumway-Cook, A. Attention and the control of posture and gait: A review of an emerging area of research. Gait Posture 2002, 16, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Petrigna, L.; Gentile, A.; Mani, D.; Pajaujiene, S.; Zanotto, T.; Thomas, E.; Paoli, A.; Palma, A.; Bianco, A. Dual-task conditions on static postural control in older adults: A systematic review and meta-analysis. J. Aging Phys. Act. 2020, 29, 162–177. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.J.; Kannan, P.; Wong, T.W.; Fong, K.N.K.; Winser, S.J. A Systematic Review Exploring the Theories Underlying the Improvement of Balance and Reduction in Falls Following Dual-Task Training among Older Adults. Int. J. Environ. Res. Public Health 2022, 19, 16890. [Google Scholar] [CrossRef] [PubMed]
- Huxhold, O.; Li, S.-C.; Schmiedek, F.; Lindenberger, U. Dual-tasking postural control: Aging and the effects of cognitive demand in conjunction with focus of attention. Brain Res. Bull. 2006, 69, 294–305. [Google Scholar] [CrossRef] [PubMed]
- Beauchet, O.; Dubost, V.; Allali, G.; Gonthier, R.; Hermann, F.R.; Kressig, R.W. ‘Faster counting while walking’ as a predictor of falls in older adults. Age Ageing 2007, 36, 418–423. [Google Scholar] [CrossRef] [PubMed]
- Al-Yahya, E.; Dawes, H.; Smith, L.; Dennis, A.; Howells, K.; Cockburn, J. Cognitive motor interference while walking: A systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2011, 35, 715–728. [Google Scholar] [CrossRef] [PubMed]
- Omana, H.; Madou, E.; Montero-Odasso, M.; Payne, M.W.; Viana, R.; Hunter, S.W. The effect of dual-task testing on the balance and gait of people with lower limb amputations: A systematic review. PM R 2023, 15, 94–128. [Google Scholar] [CrossRef] [PubMed]
- De Freitas, T.B.; Leite, P.B.; Doná, F.; Pompeu, J.E.; Swarowsky, A.; Torriani-Pasin, C. The effects of dual task gait and balance training in Parkinson’s disease: A systematic review. Physiother. Theory Pract. 2020, 36, 1088–1096. [Google Scholar] [CrossRef] [PubMed]
- Muir-Hunter, S.W.; Wittwer, J.E. Dual-task testing to predict falls in community-dwelling older adults: A systematic review. Physiotherapy 2016, 102, 29–40. [Google Scholar] [CrossRef] [PubMed]
- Abou, L.; Peters, J.; Fritz, N.E.; Sosnoff, J.J.; Kratz, A.L. Motor Cognitive Dual-Task Testing to Predict Future Falls in Multiple Sclerosis: A Systematic Review. Neurorehabil Neural Repair 2022, 36, 757–769. [Google Scholar] [CrossRef] [PubMed]
- Versi, N.; Murphy, K.; Robinson, C.; Franklin, M. Simultaneous Dual-Task Interventions That Improve Cognition in Older Adults: A Scoping Review of Implementation-Relevant Details. J. Aging Res. 2022, 2022, 6686910. [Google Scholar] [CrossRef] [PubMed]
- Petrigna, L.; Pajaujiene, S.; Iacona, G.M.; Thomas, E.; Paoli, A.; Bianco, A.; Palma, A. The execution of the grooved pegboard test in a dual-task situation: A pilot study. Heliyon 2020, 6, e04678. [Google Scholar] [CrossRef] [PubMed]
- Cedervall, Y.; Stenberg, A.M.; Åhman, H.B.; Giedraitis, V.; Tinmark, F.; Berglund, L.; Halvorsen, K.; Ingelsson, M.; Rosendahl, E.; Åberg, A.C. Timed Up-and-Go Dual-Task Testing in the Assessment of Cognitive Function: A Mixed Methods Observational Study for Development of the UDDGait Protocol. Int. J. Environ. Res. Public Health 2020, 17, 1715. [Google Scholar] [CrossRef] [PubMed]
- Tamura, K.; Kocher, M.; Finer, L.; Murata, N.; Stickley, C. Reliability of clinically feasible dual-task tests: Expanded timed get up and go test as a motor task on young healthy individuals. Gait Posture 2018, 60, 22–27. [Google Scholar] [CrossRef] [PubMed]
- Yu, D.; Li, X.; He, S.T.; Zhu, H.A.; Lam, F.M.H.; Pang, M.Y.C. The effect of dual-task training on cognitive ability, physical function, and dual-task performance in people with dementia or mild cognitive impairment: A systematic review and meta-analysis. Clin. Rehabil. 2024, 38, 443–456. [Google Scholar] [CrossRef] [PubMed]
- Ali, N.; Tian, H.; Thabane, L.; Ma, J.; Wu, H.; Zhong, Q.; Gao, Y.; Sun, C.; Zhu, Y.; Wang, T. The Effects of Dual-Task Training on Cognitive and Physical Functions in Older Adults with Cognitive Impairment; A Systematic Review and Meta-Analysis. J. Prev. Alzheimer’s Dis. 2022, 9, 359–370. [Google Scholar] [CrossRef] [PubMed]
- Collette, F.; Olivier, L.; Van der Linden, M.; Laureys, S.; Delfiore, G.; Luxen, A.; Salmon, E. Involvement of both prefrontal and inferior parietal cortex in dual-task performance. Brain Res. Cogn. Brain Res. 2005, 24, 237–251. [Google Scholar] [CrossRef] [PubMed]
- Saraiva, M.; Castro, M.A.; Vilas-Boas, J.P. Muscular and Prefrontal Cortex Activity during Dual-Task Performing in Young Adults. Eur. J. Investig. Health Psychol. Educ. 2023, 13, 736–747. [Google Scholar] [CrossRef] [PubMed]
- Paik, E. Functions of the prefrontal cortex in the human brain. J. Korean Med. Sci. 1998, 13, 569–581. [Google Scholar] [CrossRef] [PubMed]
- Kirova, A.-M.; Bays, R.B.; Lagalwar, S. Working memory and executive function decline across normal aging, mild cognitive impairment, and Alzheimer’s disease. BioMed Res. Int. 2015, 2015, 748212. [Google Scholar] [CrossRef] [PubMed]
- Zhu, X.; Yin, S.; Lang, M.; He, R.; Li, J. The more the better? A meta-analysis on effects of combined cognitive and physical intervention on cognition in healthy older adults. Ageing Res. Rev. 2016, 31, 67–79. [Google Scholar] [CrossRef] [PubMed]
- Ercan Yildiz, S.; Fidan, O.; Gulsen, C.; Colak, E.; Genc, G.A. Effect of dual-task training on balance in older adults: A systematic review and meta-analysis. Arch. Gerontol. Geriatr. 2024, 121, 105368. [Google Scholar] [CrossRef] [PubMed]
- Ghai, S.; Ghai, I.; Effenberg, A.O. Effects of dual tasks and dual-task training on postural stability: A systematic review and meta-analysis. Clin. Interv. Aging 2017, 12, 557–577. [Google Scholar] [CrossRef] [PubMed]
- Varela-Vásquez, L.A.; Minobes-Molina, E.; Jerez-Roig, J. Dual-task exercises in older adults: A structured review of current literature. J. Frailty Sarcopenia Falls 2020, 5, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Johansson, H.; Folkerts, A.K.; Hammarström, I.; Kalbe, E.; Leavy, B. Effects of motor-cognitive training on dual-task performance in people with Parkinson’s disease: A systematic review and meta-analysis. J. Neurol. 2023, 270, 2890–2907. [Google Scholar] [CrossRef] [PubMed]
- Pichierri, G.; Wolf, P.; Murer, K.; de Bruin, E.D. Cognitive and cognitive-motor interventions affecting physical functioning: A systematic review. BMC Geriatr. 2011, 11, 29. [Google Scholar] [CrossRef] [PubMed]
- Oliva, H.N.P.; Machado, F.S.M.; Rodrigues, V.D.; Leao, L.L.; Monteiro, R.S. The effect of dual-task training on cognition of people with different clinical conditions: An overview of systematic reviews. IBRO Rep. 2020, 9, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Fritz, N.E.; Cheek, F.M.; Nichols-Larsen, D.S. Motor-Cognitive Dual-Task Training in Persons With Neurologic Disorders: A Systematic Review. J. Neurol. Phys. Ther. 2015, 39, 142–153. [Google Scholar] [CrossRef] [PubMed]
- Ozemek, C.; Bonikowske, A.; Christle, J.; Gallo, P. ACSM’s Guidelines for Exercise Testing and Prescription; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2025. [Google Scholar]
- Angiuoli, S.V.; Gussman, A.; Klimke, W.; Cochrane, G.; Field, D.; Garrity, G.M.; Kodira, C.D.; Kyrpides, N.; Madupu, R.; Markowitz, V. Toward an online repository of standard operating procedures (SOPs) for (meta) genomic annotation. OMICS J. Integr. Biol. 2008, 12, 137–141. [Google Scholar] [CrossRef] [PubMed]
- Tuck, M.K.; Chan, D.W.; Chia, D.; Godwin, A.K.; Grizzle, W.E.; Krueger, K.E.; Rom, W.; Sanda, M.; Sorbara, L.; Stass, S. Standard operating procedures for serum and plasma collection: Early detection research network consensus statement standard operating procedure integration working group. J. Proteome Res. 2009, 8, 113–117. [Google Scholar] [CrossRef] [PubMed]
- Petrigna, L.; Pajaujiene, S.; Delextrat, A.; Gómez-López, M.; Paoli, A.; Palma, A.; Bianco, A. The importance of standard operating procedures in physical fitness assessment: A brief review. Sport Sci. Health 2022, 18, 21–26. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Araújo, E.M.; Coelho, H.J., Jr.; Sousa, C.V.; Rosa, T.D.; Neto, I.V.S.; Marzetti, E.; Franco, O.L.; Aguiar, S.D. Improving serum redox balance, inflammatory status, physical function, and cognitive ability through dual-task resistance training and detraining in nursing home residents. Exp. Gerontol. 2025, 200, 112662. [Google Scholar] [CrossRef] [PubMed]
- Chuang, I.C.; Chen, I.C.; Wu, Y.R.; Li, K.Y. Prediction and mediation analysis for treatment responses to combined cognitive and physical training for older adults. Sci. Rep. 2024, 14, 10571. [Google Scholar] [CrossRef] [PubMed]
- Jabeen, H.; Mahmood, T.; Mahmood, W.; Ahmad, N. Effects of Physical Cognitive Dual Task Training versus Conventional Single Task Training for Balance and Quality of Life among Older Adults—A Quasi Experimental Study. Int. J. Gerontol. 2024, 18, 258–262. [Google Scholar] [CrossRef]
- Rajalaxmi, V.; Arthi, J.; Kumar, G.M.; Muthukumaran, N.; Balathandayutham, K.; Saraswathi, K.; Kavitha, E. Effects of Dual Task Training Versus PNF Pattern on Balance and Cognition in Geriatric Population. Int. J. Life Sci. Pharma Res. 2022, 12, L1–L7. [Google Scholar] [CrossRef]
- Rezola-Pardo, C.; Arrieta, H.; Gil, S.M.; Zarrazquin, I.; Yanguas, J.J.; López, M.A.; Irazusta, J.; Rodriguez-Larrad, A. Comparison between multicomponent and simultaneous dual-task exercise interventions in long-term nursing home residents: The Ageing-ONDUAL-TASK randomized controlled study. Age Ageing 2019, 48, 817–823. [Google Scholar] [CrossRef] [PubMed]
- Rezola-Pardo, C.; Irazusta, J.; Mugica-Errazquin, I.; Gamio, I.; Sarquis-Adamson, Y.; Gil, S.M.; Ugartemendia, M.; Montero-Odasso, M.; Rodriguez-Larrad, A. Effects of multicomponent and dual-task exercise on falls in nursing homes: The AgeingOn Dual-Task study. Maturitas 2022, 164, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Yuzlu, V.; Oguz, S.; Timurtas, E.; Aykutoglu, E.; Polat, M.G. The Effect of 2 Different Dual-Task Balance Training Methods on Balance and Gait in Older Adults: A Randomized Controlled Trial. Phys. Ther. 2022, 102, pzab298. [Google Scholar] [CrossRef] [PubMed]
- Nishiguchi, S.; Yamada, M.; Tanigawa, T.; Sekiyama, K.; Kawagoe, T.; Suzuki, M.; Yoshikawa, S.; Abe, N.; Otsuka, Y.; Nakai, R.; et al. A 12-Week Physical and Cognitive Exercise Program Can Improve Cognitive Function and Neural Efficiency in Community-Dwelling Older Adults: A Randomized Controlled Trial. J. Am. Geriatr. Soc. 2015, 63, 1355–1363. [Google Scholar] [CrossRef] [PubMed]
- Trombini-Souza, F.; de Moura, V.T.G.; da Silva, L.W.N.; dos Santos Leal, I.; Nascimento, C.A.; Silva, P.S.T.; Perracini, M.R.; Sacco, I.C.N.; de Araújo, R.C.; de Maio Nascimento, M. Effects of two different dual-task training protocols on gait, balance, and cognitive function in community-dwelling older adults: A 24-week randomized controlled trial. PeerJ 2023, 11, e15030. [Google Scholar] [CrossRef] [PubMed]
- Anandh, S.; Varadharajulu, G.; Alate, M.M.; Mane, D.A. Effect of dual task training on balance and gait over regular and diversified land surfaces in independent elderly. Int. J. Curr. Res. Rev. 2021, 13, 165–168. [Google Scholar] [CrossRef]
- Akin, H.; Senel, A.; Taskiran, H.; Kaya Mutlu, E. Do motor-cognitive and motor-motor dual task training effect differently balance performance in older adults? Eur. Geriatr. Med. 2021, 12, 371–378. [Google Scholar] [CrossRef] [PubMed]
- Amini, A.; Vaezmousavi, M.; Shirvani, H. The effectiveness of cognitive-motor training on reconstructing cognitive health components in older male adults, recovered from the COVID-19. Neurol. Sci. 2022, 43, 1395–1403. [Google Scholar] [CrossRef] [PubMed]
- Silsupadol, P.; Shumway-Cook, A.; Lugade, V.; van Donkelaar, P.; Chou, L.S.; Mayr, U.; Woollacott, M.H. Effects of single-task versus dual-task training on balance performance in older adults: A double-blind, randomized controlled trial. Arch. Phys. Med. Rehabil. 2009, 90, 381–387. [Google Scholar] [CrossRef] [PubMed]
- Ansai, J.H.; de Andrade, L.P.; Buto, M.S.D.; Barroso, V.D.; Farche, A.C.S.; Rossi, P.G.; Takahashi, A.C.D. Effects of the Addition of a Dual Task to a Supervised Physical Exercise Program on Older Adults’ Cognitive Performance. J. Aging Phys. Act. 2017, 25, 234–239. [Google Scholar] [CrossRef] [PubMed]
- Chodzko-Zajko, W.J.; Proctor, D.N.; Singh, M.A.F.; Minson, C.T.; Nigg, C.R.; Salem, G.J.; Skinner, J.S. Exercise and physical activity for older adults. Med. Sci. Sports Exerc. 2009, 41, 1510–1530. [Google Scholar] [CrossRef] [PubMed]
- American Geriatrics Society Panel on Exercise and Osteoarthritis (A.G.S.P.). Exercise prescription for older adults with osteoarthritis pain: Consensus practice recommendations. A supplement to the AGS Clinical Practice Guidelines on the management of chronic pain in older adults. J. Am. Geriatr. Soc. 2001, 49, 808–823. [Google Scholar] [CrossRef] [PubMed]
- Coelho-Júnior, H.J.; Araújo, E.M.; Uchida, M.C.; Marzetti, E.; Aguiar, S.D.S. Effects of resistance training associated with a verbal fluency task on physical performance and cognitive function in frail nursing home residents. Arch. Gerontol. Geriatr. 2024, 121, 105353. [Google Scholar] [CrossRef] [PubMed]
- Castaño, L.A.A.; Castillo de Lima, V.; Barbieri, J.F.; de Lucena, E.G.P.; Gáspari, A.F.; Arai, H.; Teixeira, C.V.L.; Coelho-Júnior, H.J.; Uchida, M.C. Resistance Training Combined With Cognitive Training Increases Brain Derived Neurotrophic Factor and Improves Cognitive Function in Healthy Older Adults. Front. Psychol. 2022, 13, 870561. [Google Scholar] [CrossRef] [PubMed]
- Bagheri, H.; Khanmohammadi, R.; Olyaei, G.; Talebian, S.; Hadian, M.R.; Najafi, M. Video game and motor-cognitive dual-task training could be suitable treatments to improve dual-task interference in older adults. Neurosci. Lett. 2021, 760, 136099. [Google Scholar] [CrossRef] [PubMed]
- Bischoff, L.L.; Cordes, T.; Meixner, C.; Schoene, D.; Voelcker-Rehage, C.; Wollesen, B. Can cognitive-motor training improve physical functioning and psychosocial wellbeing in nursing home residents? A randomized controlled feasibility study as part of the PROCARE project. Aging Clin. Exp. Res. 2021, 33, 943–956. [Google Scholar] [CrossRef] [PubMed]
- Garber, C.E.; Blissmer, B.; Deschenes, M.R.; Franklin, B.A.; Lamonte, M.J.; Lee, I.-M.; Nieman, D.C.; Swain, D.P. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med. Sci. Sports Exerc. 2011, 43, 1334–1359. [Google Scholar] [CrossRef] [PubMed]
- de Souto Barreto, P.; Morley, J.E.; Chodzko-Zajko, W.; Pitkala, K.H.; Weening-Djiksterhuis, E.; Rodriguez-Mañas, L.; Barbagallo, M.; Rosendahl, E.; Sinclair, A.; Landi, F. Recommendations on physical activity and exercise for older adults living in long-term care facilities: A taskforce report. J. Am. Med. Dir. Assoc. 2016, 17, 381–392. [Google Scholar] [CrossRef] [PubMed]
- Wollesen, B.; Mattes, K.; Schulz, S.; Bischoff, L.L.; Seydell, L.; Bell, J.W.; von Duvillard, S.P. Effects of Dual-Task Management and Resistance Training on Gait Performance in Older Individuals: A Randomized Controlled Trial. Front. Aging Neurosci. 2017, 9, 415. [Google Scholar] [CrossRef] [PubMed]
- Wollesen, B.; Voelcker-Rehage, C. Training effects on motor-cognitive dual-task performance in older adults: A systematic review. Eur. Rev. Aging Phys. Act. 2014, 11, 5–24. [Google Scholar] [CrossRef]
- Sherrington, C.; Whitney, J.C.; Lord, S.R.; Herbert, R.D.; Cumming, R.G.; Close, J.C. Effective exercise for the prevention of falls: A systematic review and meta-analysis. J. Am. Geriatr. Soc. 2008, 56, 2234–2243. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.J.; Latham, N.K. Progressive resistance strength training for improving physical function in older adults. Cochrane Database Syst. Rev. 2009, 2009, Cd002759. [Google Scholar] [CrossRef] [PubMed]
- Fiatarone, M.A.; Marks, E.C.; Ryan, N.D.; Meredith, C.N.; Lipsitz, L.A.; Evans, W.J. High-intensity strength training in nonagenarians: Effects on skeletal muscle. Jama 1990, 263, 3029–3034. [Google Scholar] [CrossRef] [PubMed]
- Thomas, S.; Mackintosh, S.; Halbert, J. Does the ‘Otago exercise programme’reduce mortality and falls in older adults?: A systematic review and meta-analysis. Age Ageing 2010, 39, 681–687. [Google Scholar] [CrossRef] [PubMed]
- Wollesen, B.; Schulz, S.; Seydell, L.; Delbaere, K. Does dual task training improve walking performance of older adults with concern of falling? BMC Geriatr. 2017, 17, 213. [Google Scholar] [CrossRef] [PubMed]
- Wollesen, B.; Voelcker-Rehage, C.; Willer, J.; Zech, A.; Mattes, K. Feasibility study of dual-task-managing training to improve gait performance of older adults. Aging Clin. Exp. Res. 2015, 27, 447–455. [Google Scholar] [CrossRef] [PubMed]
- Littbrand, H.; Carlsson, M.; Lundin-Olsson, L.; Lindelöf, N.; Håglin, L.; Gustafson, Y.; Rosendahl, E. Effect of a high-intensity functional exercise program on functional balance: Preplanned subgroup analyses of a randomized controlled trial in residential care facilities. J. Am. Geriatr. Soc. 2011, 59, 1274–1282. [Google Scholar] [CrossRef] [PubMed]
- Blasco-Lafarga, C.; Cordellat, A.; Forte, A.; Roldán, A.; Monteagudo, P. Short and Long-Term Trainability in Older Adults: Training and Detraining Following Two Years of Multicomponent Cognitive-Physical Exercise Training. Int. J. Environ. Res. Public Health 2020, 17, 5984. [Google Scholar] [CrossRef] [PubMed]
- Blasco-Lafarga, C.; Martinez-Navarro, I.; Cordellat, A.; Roldán, A.; Monteagudo, P.; Sanchis-Soler, G.; Sanchis-Sanchis, R. Método de Entrenamiento Funcional Cognitivo Neuromotor. España Pat. 2016, 156, 24. [Google Scholar]
- Chen, Y.L.; Tseng, C.H.; Lin, H.T.; Wu, P.Y.; Chao, H.C. Dual-task multicomponent exercise-cognitive intervention improved cognitive function and functional fitness in older adults. Aging Clin. Exp. Res. 2023, 35, 1855–1863. [Google Scholar] [CrossRef] [PubMed]
- Chodzko-Zajko, W.J. ACSM’s Exercise for Older Adults; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2014. [Google Scholar]
- Conradsson, D.; Halvarsson, A. The effects of dual-task balance training on gait in older women with osteoporosis: A randomized controlled trial. Gait Posture 2019, 68, 562–568. [Google Scholar] [CrossRef] [PubMed]
- Halvarsson, A.; Dohrn, I.-M.; Ståhle, A. Taking balance training for older adults one step further: The rationale for and a description of a proven balance training programme. Clin. Rehabil. 2015, 29, 417–425. [Google Scholar] [CrossRef] [PubMed]
- Nascimento, M.M.; Maduro, P.A.; Rios, P.M.B.; Nascimento, L.D.S.; Silva, C.N.; Kliegel, M.; Ihle, A. The Effects of 12-Week Dual-Task Physical-Cognitive Training on Gait, Balance, Lower Extremity Muscle Strength, and Cognition in Older Adult Women: A Randomized Study. Int. J. Environ. Res. Public Health 2023, 20, 5498. [Google Scholar] [CrossRef] [PubMed]
- Nascimento, M.D.; Maduro, P.A.; Rios, P.M.B.; Nascimento, L.D.; Silva, C.N.; Kliegel, M.; Ihle, A. Effects of 12 Weeks of Physical-Cognitive Dual-Task Training on Executive Functions, Depression, Sleep Quality, and Quality of Life in Older Adult Women: A Randomized Pilot Study. Sustainability 2023, 15, 97. [Google Scholar] [CrossRef]
- Falbo, S.; Condello, G.; Capranica, L.; Forte, R.; Pesce, C. Effects of Physical-Cognitive Dual Task Training on Executive Function and Gait Performance in Older Adults: A Randomized Controlled Trial. BioMed Res. Int. 2016, 2016, 5812092. [Google Scholar] [CrossRef] [PubMed]
- Voelcker-Rehage, C.; Niemann, C. Structural and functional brain changes related to different types of physical activity across the life span. Neurosci. Biobehav. Rev. 2013, 37, 2268–2295. [Google Scholar] [CrossRef] [PubMed]
- Granacher, U.; Muehlbauer, T.; Göstemeyer, G.; Gruber, S.; Gruber, M. The performance of balance exercises during daily tooth brushing is not sufficient to improve balance and muscle strength in healthy older adults. BMC Geriatr. 2021, 21, 257. [Google Scholar] [CrossRef] [PubMed]
- Muehlbauer, T.; Roth, R.; Bopp, M.; Granacher, U. An exercise sequence for progression in balance training. J. Strength Cond. Res. 2012, 26, 568–574. [Google Scholar] [CrossRef] [PubMed]
- Gregory, M.A.; Gill, D.P.; Zou, G.; Liu-Ambrose, T.; Shigematsu, R.; Fitzgerald, C.; Hachinski, V.; Shoemaker, K.; Petrella, R.J. Group-based exercise combined with dual-task training improves gait but not vascular health in active older adults without dementia. Arch. Gerontol. Geriatr. 2016, 63, 18–27. [Google Scholar] [CrossRef] [PubMed]
- Gill, D.P.; Gregory, M.A.; Zou, G.; Liu-Ambrose, T.; Shigematsu, R.; Hachinski, V.; Fitzgerald, C.; Petrella, R.J. The Healthy Mind, Healthy Mobility Trial: A Novel Exercise Program for Older Adults. Med. Sci. Sports Exerc. 2016, 48, 297–306. [Google Scholar] [CrossRef] [PubMed]
- Halvarsson, A.; Franzén, E.; Ståhle, A. Balance training with multi-task exercises improves fall-related self-efficacy, gait, balance performance and physical function in older adults with osteoporosis: A randomized controlled trial. Clin. Rehabil. 2015, 29, 365–375. [Google Scholar] [CrossRef] [PubMed]
- Halvarsson, A.; Oddsson, L.; Franzén, E.; Ståhle, A. Long-term effects of a progressive and specific balance-training programme with multi-task exercises for older adults with osteoporosis: A randomized controlled study. Clin. Rehabil. 2016, 30, 1049–1059. [Google Scholar] [CrossRef] [PubMed]
- Ho, V.; Chan, Y.H.; Merchant, R.A. Patterns of improvement in functional ability and predictors of responders to dual-task exercise: A latent class analysis. Front. Public Health 2022, 10, 1069970. [Google Scholar] [CrossRef] [PubMed]
- Merchant, R.A.; Tsoi, C.; Tan, W.; Lau, W.; Sandrasageran, S.; Arai, H. Community-based peer-led intervention for healthy ageing and evaluation of the ‘HAPPY’program. J. Nutr. Health Aging 2021, 25, 520–527. [Google Scholar] [CrossRef] [PubMed]
- Tasvuran Horata, E.; Cetin, S.Y.; Erel, S. Effects of individual progressive single- and dual-task training on gait and cognition among older healthy adults: A randomized-controlled comparison study. Eur. Geriatr. Med. 2021, 12, 363–370. [Google Scholar] [CrossRef] [PubMed]
- Brustio, P.R.; Rabaglietti, E.; Formica, S.; Liubicich, M.E. Dual-task training in older adults: The effect of additional motor tasks on mobility performance. Arch. Gerontol. Geriatr. 2018, 75, 119–124. [Google Scholar] [CrossRef] [PubMed]
- Jardim, N.Y.V.; Bento-Torres, N.V.O.; Costa, V.O.; Carvalho, J.P.R.; Pontes, H.T.S.; Tomás, A.M.; Sosthenes, M.C.K.; Erickson, K.I.; Bento-Torres, J.; Diniz, C.W.P. Dual-Task Exercise to Improve Cognition and Functional Capacity of Healthy Older Adults. Front. Aging Neurosci. 2021, 13, 589299. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.J.; Yoo, G.E. Rhythm-Motor Dual Task Intervention for Fall Prevention in Healthy Older Adults. Front. Psychol. 2019, 10, 3027. [Google Scholar] [CrossRef] [PubMed]
- Kitazawa, K.; Showa, S.; Hiraoka, A.; Fushiki, Y.; Sakauchi, H.; Mori, M. Effect of a dual-task net-step exercise on cognitive and gait function in older adults. J. Geriatr. Phys. Ther. 2015, 38, 133–140. [Google Scholar] [CrossRef] [PubMed]
- Konak, H.E.; Kibar, S.; Ergin, E.S. The effect of single-task and dual-task balance exercise programs on balance performance in adults with osteoporosis: A randomized controlled preliminary trial. Osteoporos. Int. 2016, 27, 3271–3278. [Google Scholar] [CrossRef] [PubMed]
- Mundada, P.H.; Dadgal, R.M. Comparison of Dual Task Training Versus Aerobics Training in Improving Cognition in Healthy Elderly Population. Cureus 2022, 14, e29027. [Google Scholar] [CrossRef] [PubMed]
- Nieto-Guisado, A.; Solana-Tramunt, M.; Cabrejas, C.; Morales, J. The Effects of an 8-Week Cognitive-Motor Training Program on Proprioception and Postural Control Under Single and Dual Task in Older Adults: A Randomized Clinical Trial. Healthcare 2024, 12, 2297. [Google Scholar] [CrossRef] [PubMed]
- Me, N. Physical activity and public health in older adults: Recommendation from the American College of Sports Medicine and the American Heart Association. Med. Sci. Sports Exerc. 2007, 39, 1435–1445. [Google Scholar]
- Norouzi, E.; Vaezmosavi, M.; Gerber, M.; Pühse, U.; Brand, S. Dual-task training on cognition and resistance training improved both balance and working memory in older people. Phys. Sportsmed. 2019, 47, 471–478. [Google Scholar] [CrossRef] [PubMed]
- Pantoja-Cardoso, A.; Aragao-Santos, J.C.; Santos, P.D.; Dos-Santos, A.C.; Silva, S.R.; Lima, N.B.C.; Vasconcelos, A.B.S.; Fortes, L.D.; Da Silva-Grigoletto, M.E. Functional Training and Dual-Task Training Improve the Executive Function of Older Women. Geriatrics 2023, 8, 83. [Google Scholar] [CrossRef] [PubMed]
- Párraga-Montilla, J.A.; Aibar-Almazán, A.; Cabrera-Linares, J.C.; Lozano-Aguilera, E.; Huete, V.S.; Arrieta, M.D.E.; Latorre-Román, P.A. A Randomized Controlled Trial Protocol to Test the Efficacy of a Dual-Task Multicomponent Exercise Program vs. a Simple Program on Cognitive and Fitness Performance in Elderly People. Int. J. Environ. Res. Public Health 2021, 18, 6507. [Google Scholar] [CrossRef] [PubMed]
- Arrieta, H.; Rezola-Pardo, C.; Zarrazquin, I.; Echeverria, I.; Yanguas, J.J.; Iturburu, M.; Gil, S.M.; Rodriguez-Larrad, A.; Irazusta, J. A multicomponent exercise program improves physical function in long-term nursing home residents: A randomized controlled trial. Exp. Gerontol. 2018, 103, 94–100. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Larrad, A.; Arrieta, H.; Rezola, C.; Kortajarena, M.; Yanguas, J.J.; Iturburu, M.; Susana, M.G.; Irazusta, J. Effectiveness of a multicomponent exercise program in the attenuation of frailty in long-term nursing home residents: Study protocol for a randomized clinical controlled trial. BMC Geriatr. 2017, 17, 60. [Google Scholar] [CrossRef] [PubMed]
- Rosado, H.; Bravo, J.; Raimundo, A.; Carvalho, J.; Marmeleira, J.; Pereira, C. Effects of two 24-week multimodal exercise programs on reaction time, mobility, and dual-task performance in community-dwelling older adults at risk of falling: A randomized controlled trial. BMC Public Health 2021, 21, 408. [Google Scholar] [CrossRef] [PubMed]
- Santos, P.C.; Machado, D.R.L.; Abdalla, P.P.; Santos, C.V.; Lopes, S.; Martins, A.C.; Mota, J.; Mesquita, C. Otago Exercise Program Plus Cognitive Dual-task can Reduce Fall Risk, Improve Cognition and Functioning in Older Adults. Curr. Aging Sci. 2023, 16, 65–74. [Google Scholar] [CrossRef] [PubMed]
- Martins, A.C.; Santos, C.; Silva, C.; Baltazar, D.; Moreira, J.; Tavares, N. Does modified Otago Exercise Program improves balance in older people? A systematic review. Prev. Med. Rep. 2018, 11, 231–239. [Google Scholar] [CrossRef] [PubMed]
- Sedaghati, P.; Goudarzian, M.; Ahmadabadi, S.; Tabatabai-Asl, S.M. The impact of a multicomponent-functional training with postural correction on functional balance in the elderly with a history of falling. J. Exp. Orthop. 2022, 9, 23. [Google Scholar] [CrossRef] [PubMed]
- Agmon, M.; Belza, B.; Nguyen, H.Q.; Logsdon, R.G.; Kelly, V.E. A systematic review of interventions conducted in clinical or community settings to improve dual-task postural control in older adults. Clin. Interv. Aging 2014, 9, 477–492. [Google Scholar] [CrossRef] [PubMed]
- Pereira, C.; Rosado, H.; Cruz-Ferreira, A.; Marmeleira, J. Effects of a 10-week multimodal exercise program on physical and cognitive function of nursing home residents: A psychomotor intervention pilot study. Aging Clin. Exp. Res. 2018, 30, 471–479. [Google Scholar] [CrossRef] [PubMed]
- Rezola-Pardo, C.; Arrieta, H.; Gil, S.M.; Yanguas, J.J.; Iturburu, M.; Irazusta, J.; Sanz, B.; Rodriguez-Larrad, A. A randomized controlled trial protocol to test the efficacy of a dual-task multicomponent exercise program in the attenuation of frailty in long-term nursing home residents: Aging-ON(DUAL-TASK) study. BMC Geriatr. 2019, 19, 6. [Google Scholar] [CrossRef] [PubMed]
- Sok, S.; Shin, E.; Kim, S.; Kim, M. Effects of Cognitive/Exercise Dual-Task Program on the Cognitive Function, Health Status, Depression, and Life Satisfaction of the Elderly Living in the Community. Int. J. Environ. Res. Public Health 2021, 18, 7848. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.M.; Joung, J.; Shin, S.H. Effects of Fumanet exercise on Korean older adults with mild dementia. Jpn. J. Nurs. Sci. 2020, 17, e12286. [Google Scholar] [CrossRef] [PubMed]
- Tait, J.L.; Duckham, R.L.; Rantalainen, T.; Milte, C.M.; Main, L.C.; Nowson, C.A.; Sanders, K.M.; Taaffe, D.R.; Hill, K.D.; Abbott, G.; et al. Effects of a 6-month dual-task, power-based exercise program on cognitive function, neurological and inflammatory markers in older adults: Secondary analysis of a cluster randomised controlled trial. Geroscience 2025, 47, 1251–1268. [Google Scholar] [CrossRef] [PubMed]
- Trombini-Souza, F.; de Maio Nascimento, M.; da Silva, T.F.A.; de Araújo, R.C.; Perracini, M.R.; Sacco, I.C.N. Dual-task training with progression from variable- to fixed-priority instructions versus dual-task training with variable-priority on gait speed in community-dwelling older adults: A protocol for a randomized controlled trial: Variable- and fixed-priority dual-task for older adults. BMC Geriatr. 2020, 20, 76. [Google Scholar] [CrossRef]
- Yokoyama, H.; Okazaki, K.; Imai, D.; Yamashina, Y.; Takeda, R.; Naghavi, N.; Ota, A.; Hirasawa, Y.; Miyagawa, T. The effect of cognitive-motor dual-task training on cognitive function and plasma amyloid β peptide 42/40 ratio in healthy elderly persons: A randomized controlled trial. BMC Geriatr. 2015, 15, 60. [Google Scholar] [CrossRef] [PubMed]
- Sergeant, J.A.; Geurts, H.; Oosterlaan, J. How specific is a deficit of executive functioning for attention-deficit/hyperactivity disorder? Behav. Brain Res. 2002, 130, 3–28. [Google Scholar] [CrossRef] [PubMed]
- Strauss, E.; Sherman, E.; Spreen, O. Trail making test. In A Compendium of Neuropsychological Tests: Administration, Norms, and Commentary, 3rd ed.; Oxford University Press: Oxford, UK, 2006; pp. 655–677. [Google Scholar]
- Shigematsu, R.; Okura, T. A novel exercise for improving lower-extremity functional fitness in the elderly. Aging Clin. Exp. Res. 2006, 18, 242–248. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira, T.C.G.; Soares, F.C.; De Macedo, L.D.E.D.; Diniz, D.L.W.P.; Bento-Torres, N.V.O.; Picanço-Diniz, C.W. Beneficial effects of multisensory and cognitive stimulation on age-related cognitive decline in long-term-care institutions. Clin. Interv. Aging 2014, 9, 309–321. [Google Scholar] [PubMed]
- Kim, S.J.; Cho, S.-R.; Yoo, G.E. Age-related changes in bimanual instrument playing with rhythmic cueing. Front. Psychol. 2017, 8, 1569. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.J.; Cho, S.R.; Yoo, G.E. The Applicability of Rhythm-Motor Tasks to a New Dual Task Paradigm for Older Adults. Front. Neurol. 2017, 8, 671. [Google Scholar] [CrossRef] [PubMed]
- Yamada, M.; Aoyama, T.; Tanaka, B.; Nagai, K.; Ichihashi, N. Seated stepping exercise in a dual-task condition improves ambulatory function with a secondary task: A randomized controlled trial. Aging Clin. Exp. Res. 2011, 23, 386–392. [Google Scholar] [CrossRef] [PubMed]
- Yamada, M.; Tanaka, B.; Nagai, K.; Aoyama, T.; Ichihashi, N. Rhythmic stepping exercise under cognitive conditions improves fall risk factors in community-dwelling older adults: Preliminary results of a cluster-randomized controlled trial. Aging Ment. Health 2011, 15, 647–653. [Google Scholar] [CrossRef] [PubMed]
- Dorfman, M.; Herman, T.; Brozgol, M.; Shema, S.; Weiss, A.; Hausdorff, J.M.; Mirelman, A. Dual-task training on a treadmill to improve gait and cognitive function in elderly idiopathic fallers. J. Neurol. Phys. Ther. 2014, 38, 246–253. [Google Scholar] [CrossRef] [PubMed]
- Halvarsson, A.; Olsson, E.; Farén, E.; Pettersson, A.; Ståhle, A. Effects of new, individually adjusted, progressive balance group training for elderly people with fear of falling and tend to fall: A randomized controlled trial. Clin. Rehabil. 2011, 25, 1021–1031. [Google Scholar] [CrossRef] [PubMed]
- Silsupadol, P.; Siu, K.-C.; Shumway-Cook, A.; Woollacott, M.H. Training of balance under single-and dual-task conditions in older adults with balance impairment. Phys. Ther. 2006, 86, 269–281. [Google Scholar] [CrossRef] [PubMed]
- Jung, J.-H.; Kim, M.-J.; Woo, H.-J.; Kim, Y.-S.; Kim, M.-H.; Song, S.-R.; Kang, S.-M.; Choi, Y.-W.; Kim, J.-H. Effect of CLX training combined with PNF pattern on balance ability. J. Korean Phys. Ther. Sci. 2019, 26, 1–8. [Google Scholar] [CrossRef]
- Weeks, D.L.; Forget, R.; Mouchnino, L.; Gravel, D.; Bourbonnais, D. Interaction between attention demanding motor and cognitive tasks and static postural stability. Gerontology 2003, 49, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Hollman, J.H.; Kovash, F.M.; Kubik, J.J.; Linbo, R.A. Age-related differences in spatiotemporal markers of gait stability during dual task walking. Gait Posture 2007, 26, 113–119. [Google Scholar] [CrossRef] [PubMed]
- Wollesen, B.; Wildbredt, A.; van Schooten, K.S.; Lim, M.L.; Delbaere, K. The effects of cognitive-motor training interventions on executive functions in older people: A systematic review and meta-analysis. Eur. Rev. Aging Phys. Act. 2020, 17, 9. [Google Scholar] [CrossRef] [PubMed]
- Paillard, T. The optimal method for improving postural balance in healthy young and older people: Specific training for postural tasks encountered in personal physical practice. Front. Physiol. 2023, 14, 1188496. [Google Scholar] [CrossRef] [PubMed]
- Esmaeilzadeh, S.; Kumpulainen, S.; Pesola, A.J. Strength-Cognitive Training: A Systemic Review in Adults and Older Adults, and Guidelines to Promote “Strength Exergaming” Innovations. Front. Psychol. 2022, 13, 855703. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, F.; Domingos, C.; Monteiro, D.; Morouco, P. A Review on Aging, Sarcopenia, Falls, and Resistance Training in Community-Dwelling Older Adults. Int. J. Environ. Res. Public Health 2022, 19, 874. [Google Scholar] [CrossRef] [PubMed]
- Jiménez-Lupión, D.; Chirosa-Ríos, L.; Martínez-García, D.; Rodríguez-Pérez, M.; Jerez-Mayorga, D. Effects of Power Training on Functional Capacity Related to Fall Risk in Older Adults: A Systematic Review and Meta-analysis. Arch. Phys. Med. Rehabil. 2023, 104, 1514–1525. [Google Scholar] [CrossRef] [PubMed]
- Syed-Abdul, M.M. Benefits of Resistance Training in Older Adults. Curr. Aging Sci. 2021, 14, 5–9. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, A.; Fidalgo, A.; Farinatti, P.; Monteiro, W. Effects of high-intensity interval and continuous moderate aerobic training on fitness and health markers of older adults: A systematic review and meta-analysis. Arch. Gerontol. Geriatr. 2024, 124, 105451. [Google Scholar] [CrossRef] [PubMed]
- Sert, H.; Gulbahar Eren, M.; Gurcay, B.; Koc, F. The effectiveness of a high-intensity interval exercise on cardiometabolic health and quality of life in older adults: A systematic review and meta-analysis. BMC Sports Sci. Med. Rehabil. 2025, 17, 128. [Google Scholar] [CrossRef] [PubMed]
- Treacy, D.; Hassett, L.; Schurr, K.; Fairhall, N.J.; Cameron, I.D.; Sherrington, C. Mobility training for increasing mobility and functioning in older people with frailty. Cochrane Database Syst. Rev. 2022, 6, Cd010494. [Google Scholar] [CrossRef] [PubMed]
- Bonetti, L.V.; Hassan, S.A.; Kasawara, K.T.; Reid, W.D. The effect of mental tracking task on spatiotemporal gait parameters in healthy younger and middle-and older aged participants during dual tasking. Exp. Brain Res. 2019, 237, 3123–3132. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.K.; Huang, C.J.; Chen, K.F.; Hung, T.M. Physical activity and working memory in healthy older adults: An ERP study. Psychophysiol. 2013, 50, 1174–1182. [Google Scholar] [CrossRef] [PubMed]
- Buschkuehl, M.; Jaeggi, S.M.; Hutchison, S.; Perrig-Chiello, P.; Däpp, C.; Müller, M.; Breil, F.; Hoppeler, H.; Perrig, W.J. Impact of working memory training on memory performance in old-old adults. Psychol. Aging 2008, 23, 743. [Google Scholar] [CrossRef] [PubMed]
- Heinzel, S.; Schulte, S.; Onken, J.; Duong, Q.-L.; Riemer, T.G.; Heinz, A.; Kathmann, N.; Rapp, M.A. Working memory training improvements and gains in non-trained cognitive tasks in young and older adults. Aging Neuropsychol. Cogn. 2014, 21, 146–173. [Google Scholar] [CrossRef] [PubMed]
- Camicioli, R.; Howieson, D.; Lehman, S.; Kaye, J. Talking while walking: The effect of a dual task in aging and Alzheimer’s disease. Neurology 1997, 48, 955–958. [Google Scholar] [CrossRef] [PubMed]
- Fournet, M.; Pernon, M.; Catalano Chiuvé, S.; Lopez, U.; Laganaro, M. Attention in post-lexical processes of utterance production: Dual-task cost in younger and older adults. Q. J. Exp. Psychol. 2021, 74, 1852–1872. [Google Scholar] [CrossRef] [PubMed]
- Rafiee Manesh, V.; Inanlu, M.; Yekaninejad, M.S.; Khanmohammadi, R. The effect of different types of cognitive tasks on postural sway fluctuations in older and younger adults: A nonlinear study. J. Bodyw. Mov. Ther. 2024, 37, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Friedman, A.; Polson, M.C.; Dafoe, C.G.; Gaskill, S.J. Dividing attention within and between hemispheres: Testing a multiple resources approach to limited-capacity information processing. J. Exp. Psychol. Hum. Percept. Perform. 1982, 8, 625. [Google Scholar] [CrossRef] [PubMed]
- Santos, L.O.d.; Carvalho de Abreu, D.C.; Moraes, R. Performance of faller and nonfaller older adults on a motor–motor interference task. J. Mot. Behav. 2018, 50, 293–306. [Google Scholar] [CrossRef] [PubMed]
- Navon, D.; Miller, J. Role of outcome conflict in dual-task interference. J. Exp. Psychol. Hum. Percept. Perform. 1987, 13, 435. [Google Scholar] [CrossRef] [PubMed]
- Pashler, H. Dual-task interference in simple tasks: Data and theory. Psychol. Bull. 1994, 116, 220. [Google Scholar] [CrossRef] [PubMed]
- Malik, J.; Stemplewski, R.; Maciaszek, J. The Effect of Juggling as Dual-Task Activity on Human Neuroplasticity: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 7102. [Google Scholar] [CrossRef] [PubMed]
- Bherer, L. Cognitive plasticity in older adults: Effects of cognitive training and physical exercise. Ann. N. Y. Acad. Sci. 2015, 1337, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.Y.; Lin, L.L.; Hwang, I.S. Age-Related Differences in Reorganization of Functional Connectivity for a Dual Task with Increasing Postural Destabilization. Front. Aging Neurosci. 2017, 9, 96. [Google Scholar] [CrossRef] [PubMed]
- Hwang, I.S.; Huang, C.Y. Neural Correlates of Task Cost for Stance Control with an Additional Motor Task: Phase-Locked Electroencephalogram Responses. PLoS ONE 2016, 11, e0151906. [Google Scholar] [CrossRef] [PubMed]
- Shumway-Cook, A.; Woollacott, M. Attentional demands and postural control: The effect of sensory context. J. Gerontol. A Biol. Sci. Med. Sci. 2000, 55, M10–M16. [Google Scholar] [CrossRef] [PubMed]
- Rankin, J.K.; Woollacott, M.H.; Shumway-Cook, A.; Brown, L.A. Cognitive influence on postural stability: A neuromuscular analysis in young and older adults. J. Gerontol. A Biol. Sci. Med. Sci. 2000, 55, M112–M119. [Google Scholar] [CrossRef] [PubMed]
- Law, L.L.; Barnett, F.; Yau, M.K.; Gray, M.A. Effects of combined cognitive and exercise interventions on cognition in older adults with and without cognitive impairment: A systematic review. Ageing Res. Rev. 2014, 15, 61–75. [Google Scholar] [CrossRef] [PubMed]
- Papegaaij, S.; Taube, W.; Baudry, S.; Otten, E.; Hortobágyi, T. Aging causes a reorganization of cortical and spinal control of posture. Front. Aging Neurosci. 2014, 6, 28. [Google Scholar] [CrossRef] [PubMed]
- Gallou-Guyot, M.; Mandigout, S.; Bherer, L.; Perrochon, A. Effects of exergames and cognitive-motor dual-task training on cognitive, physical and dual-task functions in cognitively healthy older adults: An overview. Ageing Res. Rev. 2020, 63, 101135. [Google Scholar] [CrossRef] [PubMed]
- Papale, O.; Di Rocco, F.; Festino, E.; Gammino, V.; Cortis, C.; Fusco, A. Do Hand Exercises Influence Physiological Hand Tremor? An Observational Cohort Study on Healthy Young Adults. Appl. Sci. 2024, 14, 4467. [Google Scholar] [CrossRef]
- Hong, X.L.; Cheng, L.J.; Feng, R.C.; Goh, J.; Gyanwali, B.; Itoh, S.; Tam, W.S.W.; Wu, X.V. Effect of physio-cognitive dual-task training on cognition in pre-ageing and older adults with neurocognitive disorders: A meta-analysis and meta-regression of randomized controlled trial. Arch. Gerontol. Geriatr. 2024, 116, 105161. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).