Diagnosis of mTBI in an ER Setting Using Eye-Tracking and Virtual Reality Technology: An Exploratory Study
Abstract
1. Introduction
2. Patients and Methods
2.1. Patient Recruitment and Data Acquisition
2.2. Inclusion Criteria
- Age 18–65 years
- Admission within 24 h after trauma
- Accident mechanism compatible with mTBI (e.g., direct head impact)
2.3. Exclusion Criteria
- Strabism;
- Pre-existing or traumatic damage to cranial nerves III (oculomotor nerve), IV (trochlear nerve) and VI (abducens nerve);
- Alcohol consumption (if suspected, confirmed by breath alcohol test);
- Sedating medication and intoxication;
- Multi-system injury;
- Seizures;
- Major physiological perturbations (e.g., hypotension).
- Moderate to severe TBI
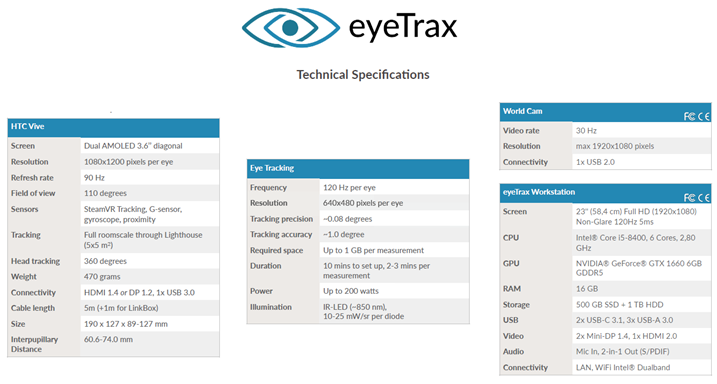
2.4. Index-Test (ET/VR Examination)
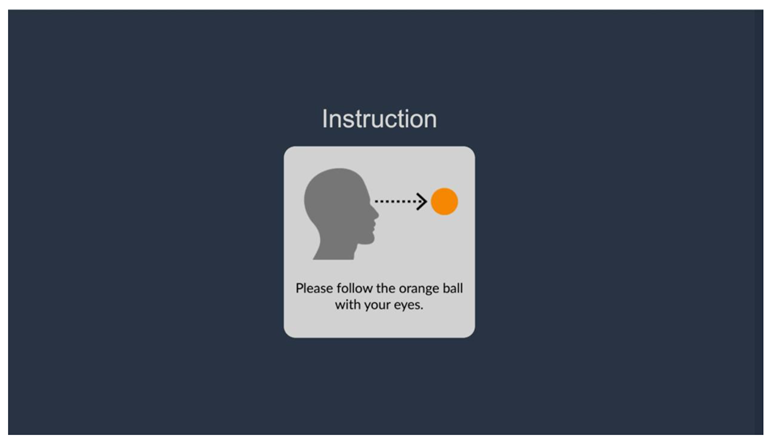
2.5. VR-Based Eye Tracking Protocols
2.6. Reference Test
2.7. Statistical Analysis
3. Results
3.1. SCAT3 Analysis
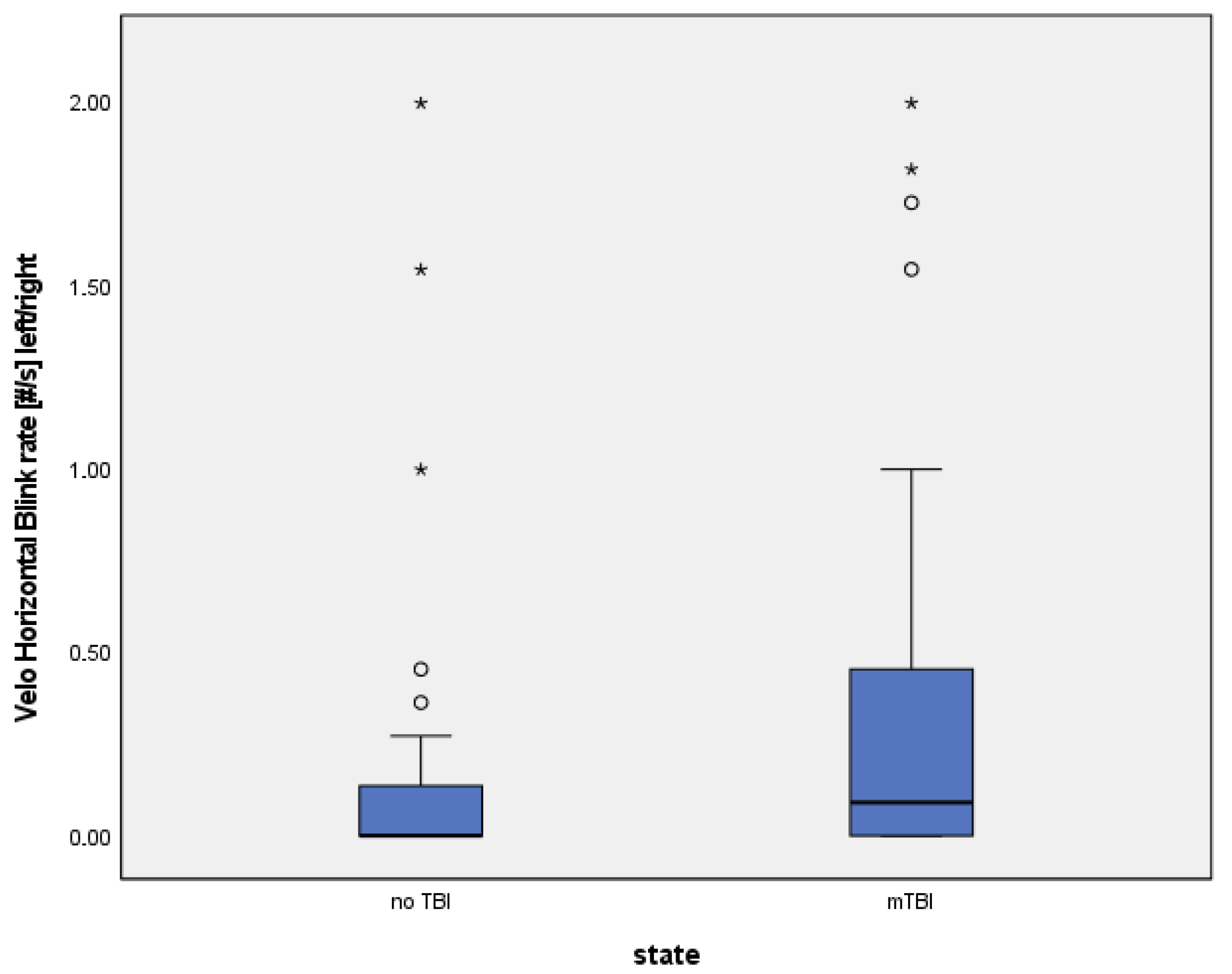
3.2. ET/VR Parameters
- 1.
- Velo Horizontal—number of eyelid closures (left/right merged)
- 2.
- Velo Horizontal—blink rate [#/s] (left/right merged)
3.3. Numerical Group Comparisons
3.4. Physiological Implications
3.5. β-Error Considerations
3.6. Figures
3.7. Side Effects and Practicability
3.8. Summary of Results
4. Discussion
4.1. Comparison with Current Diagnostic Methods
4.2. ET/VR Technology Therefore Offers Several Potential Advantages
4.3. Findings of the Present Study
5. Limitations
Strengths and Future Directions
6. Conclusions
7. Transparency, Rigor, and Reproducibility Summary
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
Appendix B
References
- Lefevre-Dognin, C.; Cogné, M.; Perdrieau, V.; Granger, A.; Heslot, C.; Azouvi, P. Definition and epidemiology of mild traumatic brain injury. Neurochirurgie 2021, 67, 218–221. [Google Scholar] [CrossRef]
- Rickels, E.; von Wild, K.; Wenzlaff, P. Head injury in Germany: A population-based prospective study on epidemiology, causes, treatment and outcome of all degrees of head-injury severity in two distinct areas. Brain Inj. 2010, 24, 1491–1504. [Google Scholar] [CrossRef]
- Michelson, E.A.; Huff, S.; Loparo, M.; Naunheim, R.S.; Perron, A.; Rahm, M.; Smith, D.W.; Stone, J.; Berger, A. Emergency Department Time Course for Mild Traumatic Brain Injury Workup. WestJEM 2018, 19, 635–640. [Google Scholar] [CrossRef]
- Rowe, B.H.; Eliyahu, L.; Lowes, J.; Gaudet, L.A.; Beach, J.; Mrazik, M.; Cummings, G.; Voaklander, D. Concussion diagnoses among adults presenting to three Canadian emergency departments: Missed opportunities. Am. J. Emerg. Med. 2018, 36, 2144–2151. [Google Scholar] [CrossRef]
- Powell, J.M.; Ferraro, J.V.; Dikmen, S.S.; Temkin, N.R.; Bell, K.R. Accuracy of Mild Traumatic Brain Injury Diagnosis. Arch. Phys. Med. Rehabil. 2008, 89, 1550–1555. [Google Scholar] [CrossRef]
- Alexander, M.P. Mild traumatic brain injury: Pathophysiology, natural history, and clinical management. Neurology 1995, 45, 1253–1260. [Google Scholar] [CrossRef]
- Patricios, J.S.; Schneider, K.J.; Dvorak, J.; Ahmed, O.H.; Blauwet, C.; Cantu, R.C.; A Davis, G.; Echemendia, R.J.; Makdissi, M.; McNamee, M.; et al. Consensus statement on concussion in sport: The 6th International Conference on Concussion in Sport–Amsterdam, October 2022. Br. J. Sports Med. 2023, 57, 695–711. [Google Scholar] [CrossRef]
- McAllister, T.W.; Arciniegas, D. Evaluation and treatment of postconcussive symptoms. NeuroRehabilitation. 2002, 17, 265–283. [Google Scholar] [CrossRef]
- Arneson, D.; Zhang, G.; Ying, Z.; Zhuang, Y.; Byun, H.R.; Ahn, I.S.; Gomez-Pinilla, F.; Yang, X. Single cell molecular alterations reveal target cells and pathways of concussive brain injury. Nat. Commun. 2018, 9, 1–18. [Google Scholar] [CrossRef]
- Hocke, L.M.; Duszynski, C.C.; Debert, C.T.; Dleikan, D.; Dunn, J.F. Reduced Functional Connectivity in Adults with Persistent Post-Concussion Symptoms: A Functional Near-Infrared Spectroscopy Study. J. Neurotrauma 2018, 35, 1224–1232. [Google Scholar] [CrossRef]
- Mckee, A.C.; Daneshvar, D.H. The neuropathology of traumatic brain injury. In Handbook of Clinical Neurology; Elsevier: Amsterdam, The Netherlands, 2015; pp. 45–66. Available online: https://linkinghub.elsevier.com/retrieve/pii/B9780444528926000040 (accessed on 21 September 2022).
- Fralick, M.; Thiruchelvam, D.; Tien, H.C.; Redelmeier, D.A. Risk of suicide after a concussion. Can. Med. Assoc. J. 2016, 188, 497–504. [Google Scholar] [CrossRef]
- Theadom, A.; Starkey, N.; Barker-Collo, S.; Jones, K.; Ameratunga, S.; Feigin, V.; on behalf of the BIONIC4you Research Group. Population-based cohort study of the impacts of mild traumatic brain injury in adults four years post-injury. PLoS ONE 2018, 13, e0191655. [Google Scholar] [CrossRef]
- Stein, M.B.; Jain, S.; Giacino, J.T.; Levin, H.; Dikmen, S.; Nelson, L.D.; Vassar, M.J.; Okonkwo, D.O.; Diaz-Arrastia, R.; Robertson, C.S.; et al. Risk of Posttraumatic Stress Disorder and Major Depression in Civilian Patients After Mild Traumatic Brain Injury: A TRACK-TBI Study. JAMA Psychiatry 2019, 76, 249–258. [Google Scholar] [CrossRef]
- Marin, J.R.; Weaver, M.D.; Yealy, D.M.; Mannix, R.C. Trends in Visits for Traumatic Brain Injury to Emergency Departments in the United States. JAMA 2014, 311, 1917–1919. [Google Scholar] [CrossRef]
- Gaw, C.E.; Zonfrillo, M.R. Emergency department visits for head trauma in the United States. BMC Emerg. Med. 2016, 16, 1–10. [Google Scholar] [CrossRef]
- Dougherty, A.L.; MacGregor, A.J.; Han, P.P.; Heltemes, K.J.; Galarneau, M.R. Visual dysfunction following blast-related traumatic brain injury from the battlefield. Brain Inj. 2011, 25, 8–13. [Google Scholar] [CrossRef]
- Ventura, R.E.; Jancuska, J.M.; Balcer, L.J.; Galetta, S.L. Diagnostic Tests for Concussion: Is Vision Part of the Puzzle? J. Neuro-Ophthalmol. 2015, 35, 73–81. [Google Scholar] [CrossRef]
- Sussman, E.S.; Ho, A.L.; Pendharkar, A.V.; Ghajar, J. Clinical evaluation of concussion: The evolving role of oculomotor assessments. Neurosurgical Focus 2016, 40, E7. [Google Scholar] [CrossRef]
- Capó-Aponte, J.E.; Beltran, T.A.; Walsh, D.V.; Cole, W.R.; Dumayas, J.Y. Validation of Visual Objective Biomarkers for Acute Concussion. Mil. Med. 2018, 183, 9–17. [Google Scholar] [CrossRef]
- Cochrane, G.D.; Christy, J.B.; Almutairi, A.; Busettini, C.; Swanson, M.W.; Weise, K.K. Visuo-oculomotor Function and Reaction Times in Athletes with and without Concussion. Optom. Vis. Sci. 2019, 96, 256–265. [Google Scholar] [CrossRef]
- DiCesare, C.A.; Kiefer, A.W.; Nalepka, P.; Myer, G.D. Quantification and analysis of saccadic and smooth pursuit eye movements and fixations to detect oculomotor deficits. Behav. Res. Methods 2017, 49, 258–266. [Google Scholar] [CrossRef]
- Howell, D.R.; Brilliant, A.N.; Storey, E.P.; Podolak, O.E.; Meehan, W.P.; Master, C.L. Objective Eye Tracking Deficits Following Concussion for Youth Seen in a Sports Medicine Setting. J. Child Neurol. 2018, 33, 794–800. [Google Scholar] [CrossRef]
- Kelly, K.M.; Kiderman, A.; Akhavan, S.; Quigley, M.R.; Snell, E.D.; Happ, E.; S Andrea, S.; Eric, M.; A Melissa, B.; P Liza, O.; et al. Oculomotor, Vestibular, and Reaction Time Effects of Sports-Related Concussion: Video-Oculography in Assessing Sports-Related Concussion. J. Head Trauma Rehabil. 2019, 34, 176–188. [Google Scholar] [CrossRef]
- Ciuffreda, K.J.; Kapoor, N.; Rutner, D.; Suchoff, I.B.; Han, M.E.; Craig, S. Occurrence of oculomotor dysfunctions in acquired brain injury: A retrospective analysis. Optom. -J. Am. Optom. Assoc. 2007, 78, 155–161. [Google Scholar] [CrossRef]
- Shinoda, Y.; Takahashi, M.; Sugiuchi, Y. Brainstem neural circuits for fixation and generation of saccadic eye movements. In Progress in Brain Research; Elsevier: Amsterdam, The Netherlands, 2019; pp. 95–104. Available online: https://linkinghub.elsevier.com/retrieve/pii/S0079612319300834 (accessed on 19 July 2023).
- Heitger, M.H.; Anderson, T.J.; Jones, R.D. Saccade sequences as markers for cerebral dysfunction following mild closed head injury. In Progress in Brain Research; Elsevier: Amsterdam, The Netherlands, 2002; pp. 433–448. Available online: https://linkinghub.elsevier.com/retrieve/pii/S0079612302400672 (accessed on 19 July 2023).
- Heitger, M.H. Eye movement and visuomotor arm movement deficits following mild closed head injury. Brain 2003, 127, 575–590. [Google Scholar] [CrossRef] [PubMed]
- Hoffer, M.E.; Balaban, C.; Szczupak, M.; Buskirk, J.; Snapp, H.; Crawford, J.; Wise, S.; Murphy, S.; Marshall, K.; Pelusso, C.; et al. The use of oculomotor, vestibular, and reaction time tests to assess mild traumatic brain injury (mTBI) over time: OVRT Test to Assess mTBI. Laryngoscope Investig. Otolaryngol. 2017, 2, 157–165. [Google Scholar] [CrossRef] [PubMed]
- Heitger, M.H.; Jones, R.D.; Macleod, A.D.; Snell, D.L.; Frampton, C.M.; Anderson, T.J. Impaired eye movements in post-concussion syndrome indicate suboptimal brain function beyond the influence of depression, malingering or intellectual ability. Brain 2009, 132, 2850–2870. [Google Scholar] [CrossRef]
- Mullen, S.J.; Yücel, Y.H.; Cusimano, M.; Schweizer, T.A.; Oentoro, A.; Gupta, N. Saccadic Eye Movements in Mild Traumatic Brain Injury: A Pilot Study. Can. J. Neurol. Sci. 2014, 41, 58–65. [Google Scholar] [CrossRef]
- Drew, A.S.; Langan, J.; Halterman, C.; Osternig, L.R.; Chou, L.S.; van Donkelaar, P. Attentional disengagement dysfunction following mTBI assessed with the gap saccade task. Neurosci. Lett. 2007, 417, 61–65. [Google Scholar] [CrossRef] [PubMed]
- Shenton, M.E.; Hamoda, H.M.; Schneiderman, J.S.; Bouix, S.; Pasternak, O.; Rathi, Y.; Vu, M.-A.; Purohit, M.P.; Helmer, K.; Koerte, I.; et al. A review of magnetic resonance imaging and diffusion tensor imaging findings in mild traumatic brain injury. Brain Imaging Behav. 2012, 6, 137–192. [Google Scholar] [CrossRef]
- Hunt, A.W.; Mah, K.; Reed, N.; Engel, L.; Keightley, M. Oculomotor-Based Vision Assessment in Mild Traumatic Brain Injury: A Systematic Review. J. Head Trauma Rehabil. 2016, 31, 252–261. [Google Scholar] [CrossRef] [PubMed]
- Flanagan, S. Traumatic brain injury: Future assessment tools and treatment prospects. NDT 2008, 877. [Google Scholar] [CrossRef] [PubMed]
- Slobounov, S.; Slobounov, E.; Newell, K. Application of Virtual Reality Graphics in Assessment of Concussion. CyberPsychology Behav. 2006, 9, 188–191. [Google Scholar] [CrossRef]
- Wright, W.G.; McDevitt, J.; Tierney, R.; Haran, F.J.; Appiah-Kubi, K.O.; Dumont, A. Assessing subacute mild traumatic brain injury with a portable virtual reality balance device. Disabil. Rehabil. 2017, 39, 1564–1572. [Google Scholar] [CrossRef] [PubMed]
- Silverberg, N.D.; Iverson, G.L.; Cogan, A.; Dams-O-Connor, K.; Delmonico, R.; Iaccarino, M.A.; Kajankova, M.; Kamins, J.; McCulloch, K.L.; McKinne, G.; et al. The American Congress of Rehabilitation Medicine Diagnostic Criteria for Mild Traumatic Brain Injury. Arch. Phys. Med. Rehabil. 2023, 104, 1343–1355. [Google Scholar] [CrossRef]
- Reneker, J.C.; Pruett, W.A.; Babl, R.; Brown, M.; Daniels, J.; Pannell, W.C.; Shirley, H.L. Developmental methods and results for a novel virtual reality concussion detection system. Virtual Real. 2025, 29, 72. [Google Scholar] [CrossRef]
- Pozzato, I.; Meares, S.; Kifley, A.; Craig, A.; Gillett, M.; Van Vu, K.; Liang, A.; Cameron, I.; Gopinath, B. Challenges in the acute identification of mild traumatic brain injuries: Results from an emergency department surveillance study. BMJ Open 2020, 10, e034494. [Google Scholar] [CrossRef]
- Mayer, A.R.; Quinn, D.K.; Master, C.L. The spectrum of mild traumatic brain injury: A review. Neurology 2017, 89, 623–632. [Google Scholar] [CrossRef]
- Stuart, S.; Hickey, A.; Vitorio, R.; Welman, K.E.; Foo, S.; Keen, D.; Godfrey, A. Eye-tracker algorithms to detect saccades during static and dynamic tasks: A structured review. Physiol. Meas. 2019, 40, 02TR01. [Google Scholar] [CrossRef]
- Maruta, J.; Spielman, L.A.; Rajashekar, U.; Ghajar, J. Association of Visual Tracking Metrics with Post-concussion Symptomatology. Front Neurol. 2018, 9, 611. [Google Scholar] [CrossRef]
- Yaribeygi, H.; Panahi, Y.; Sahraei, H.; Johnston, T.P.; Sahebkar, A. The Impact of Stress on Body Function: A Review. EXCLI J. 2017, 16, 1057. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Shi, Y.; Li, N. The role of selective attention in emergency wayfinding: An eye tracking-integrated virtual reality experiment. Saf. Sci. 2023, 168, 106320. [Google Scholar] [CrossRef]
- Zhang, W.; Hashemi, M.M.; Kaldewaij, R.; Koch, S.B.; Beckmann, C.; Klumpers, F.; Roelofs, K. Acute stress alters the ‘default’ brain processing. NeuroImage 2019, 189, 870–877. [Google Scholar] [CrossRef] [PubMed]



| TBI State | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| No TBI | mTBI | ||||||||
| Mean | Std. Dev. | No. | % | Mean | Std. Dev. | No. | % | ||
| Age (years) | 41 | 15 | 39 | 15 | |||||
| Sex | Male | 16 | 51.6% | 38 | 74.5% | ||||
| Female | 15 | 48.4% | 13 | 25.5% | |||||
| History of head injuries (SHT)? | No | 21 | 65.6% | 25 | 49.0% | ||||
| Yes | 11 | 34.4% | 26 | 51.0% | |||||
| Headaches (in general) | No | 18 | 56.3% | 25 | 49.0% | ||||
| Yes | 14 | 43.8% | 26 | 51.0% | |||||
| Migraine | No | 7 | 50.0% | 17 | 65.4% | ||||
| Yes | 7 | 50.0% | 9 | 34.6% | |||||
| Difficulty falling asleep | No | 29 | 90.6% | 45 | 88.2% | ||||
| Yes | 3 | 9.4% | 6 | 11.8% | |||||
| Difficulty sleeping through the night | No | 25 | 78.1% | 46 | 90.2% | ||||
| Yes | 7 | 21.9% | 5 | 9.8% | |||||
| Location of impact | Front | 11 | 36.7% | 17 | 40.5% | ||||
| Rear | 10 | 33.3% | 9 | 21.4% | |||||
| Right | 7 | 23.3% | 4 | 9.5% | |||||
| Left | 0 | 0.0% | 7 | 16.7% | |||||
| Top | 2 | 6.7% | 4 | 9.5% | |||||
| From below | 0 | 0.0% | 1 | 2.4% | |||||
| Retrograde amnesia: Missing memories of events shortly before the injury? | No | 30 | 93.8% | 30 | 58.8% | ||||
| Yes | 2 | 6.3% | 21 | 41.2% | |||||
| Anterograde amnesia: Missing memories of events shortly after the injury? | No | 28 | 87.5% | 27 | 54.0% | ||||
| Yes | 4 | 12.5% | 23 | 46.0% | |||||
| Unconsciousness: Did the person concerned lose consciousness? | No | 26 | 81.3% | 26 | 52.0% | ||||
| Yes | 6 | 18.8% | 24 | 48.0% | |||||
| Test Name | Brief Description | Main Measurements | Clinical Relevance/Pathologies Detected |
|---|---|---|---|
| Biflicker (horizontal/vertical/3D) | Tracking of a moving orange ball across axes and in 3D | Saccadic amplitude, duration, velocity, acceleration | Detects deficits in basic saccadic control |
| Smooth pursuit (Sinus) | Ball moving along sinusoidal trajectories | Pursuit gain, intersaccadic interval | Identifies pursuit deficits, often impaired in mTBI |
| Diverge | Object increasing/decreasing in size while moving across the field | Amplitude, duration, velocity | Detects convergence/vergence dysfunction |
| Velo (horizontal/vertical) | Rapid shifts between two static targets | Amplitude, duration, velocity | Measures peak saccadic velocity, attention shifting |
| Anti-saccades | Suppress response to distractor stimulus | Latency, directional errors, accuracy | Sensitive to executive/attentional dysfunction in mTBI |
| Dice | Visual search of rotating 3D dice with numbers | Iris adaptation, saccadic control | Higher-order visual integration, fatigue detection |
| Flash | Light flashes are presented in series | Iris adaptation, pupil velocity | Photophobia, pupillary reflex alterations |
| Vestibular (horizontal/vertical) | Head/eye coordination with central fixation | Saccadic amplitude, duration, velocity | Vestibulo-ocular reflex assessment |
| TBI State | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No TBI | mTBI | ||||||||||
| 25th Perc | md | 75th Perc | No | % | 25th Perc | md | 75th Perc | No | % | ||
| Headache | 0 | 2 | 3 | 1 | 2 | 3 | |||||
| “Pressure in head” | 0 | 1 | 2 | 0 | 2 | 3 | |||||
| Neck Pain | 0 | 1 | 3 | 0 | 2 | 3 | |||||
| Nausea or vomiting | 0 | 0 | 1 | 0 | 0 | 1 | |||||
| Dizziness | 0 | 0 | 2 | 0 | 1 | 2 | |||||
| Blurred vision | 0 | 0 | 0 | 0 | 0 | 1 | |||||
| Balance problems | 0 | 0 | 0 | 0 | 0 | 1 | |||||
| Sensitivity to light | 0 | 0 | 1 | 0 | 0 | 1 | |||||
| Sensitivity to noise | 0 | 0 | 0 | 0 | 0 | 0 | |||||
| Feeling slowed down | 0 | 0 | 1 | 0 | 0 | 2 | |||||
| Feeling like “in a fog” | 0 | 0 | 1 | 0 | 1 | 2 | |||||
| “Don’t feel right” | 0 | 0 | 1 | 0 | 1 | 2 | |||||
| Difficulty concentrating | 0 | 0 | 1 | 0 | 0 | 1 | |||||
| Difficulty remembering | 0 | 0 | 0 | 0 | 0 | 2 | |||||
| Fatigue or low energy | 0 | 1 | 3 | 1 | 2 | 3 | |||||
| Confusion | 0 | 0 | 0 | 0 | 0 | 0 | |||||
| Drowsiness | 0 | 0 | 1 | 0 | 0 | 2 | |||||
| Trouble falling asleep | 0 | 0 | 0 | 0 | 0 | 0 | |||||
| More emotional | 0 | 0 | 0 | 0 | 0 | 1 | |||||
| Irritability | 0 | 0 | 0 | 0 | 0 | 0 | |||||
| Sadness | 0 | 0 | 0 | 0 | 0 | 1 | |||||
| Nervous or Anxious | 0 | 0 | 0 | 0 | 0 | 0 | |||||
| Do the symptoms get worse with physical or mental activity? | No | 25 | 83.3% | 32 | 66.7% | ||||||
| Yes | 5 | 16.7% | 16 | 33.3% | |||||||
| AUC | Standard Error | p | Lower Limit with 95% CI | Upper Limit with 95% CI | |
|---|---|---|---|---|---|
| Velo Horizontal Number of eyelid closures left/right | 0.634 | 0.062 | 0.041 | 0.511 | 0.756 |
| Velo Horizontal Blink rate [#/s] left/right | 0.630 | 0.063 | 0.048 | 0.507 | 0.752 |
| Biflicker Main saccade amplitude [°] right/Biflicker Gain of main saccade [%] right | 0.612 | 0.064 | 0.089 | 0.486 | 0.737 |
| Velo vertical average peak velocity [°/s] left | 0.400 | 0.067 | 0.125 | 0.269 | 0.530 |
| Biflicker Vertical V_max of the main saccade [°/s] left | 0.404 | 0.065 | 0.142 | 0.277 | 0.531 |
| Biflicker Duration of the main acceleration [ms] left | 0.405 | 0.062 | 0.148 | 0.283 | 0.527 |
| Biflicker direction with respect to the X-axis in the UZS. [°] right | 0.589 | 0.065 | 0.172 | 0.462 | 0.717 |
| Velo vertical Number of saccades right | 0.585 | 0.064 | 0.197 | 0.459 | 0.710 |
| Velo vertical Number of saccades left | 0.584 | 0.064 | 0.202 | 0.458 | 0.710 |
| Velo Horizontal Average peak speed [°/s] left | 0.424 | 0.068 | 0.244 | 0.291 | 0.557 |
| Biflicker Vertical trigger direction with regard to the X-axis in the UZS. [°] | 0.571 | 0.065 | 0.278 | 0.444 | 0.698 |
| Biflicker V_max of the main saccade [°/s] left | 0.431 | 0.064 | 0.295 | 0.305 | 0.557 |
| Biflicker Vertical Blink rate [#/s] left/right | 0.567 | 0.063 | 0.303 | 0.444 | 0.691 |
| Velo Horizontal Duration of repetition [ms] | 0.566 | 0.066 | 0.310 | 0.438 | 0.695 |
| Biflicker Vertical Number of eyelid closures left/right | 0.564 | 0.063 | 0.331 | 0.440 | 0.687 |
| Biflicker Vertical Number of saccades left/right | 0.437 | 0.064 | 0.335 | 0.311 | 0.563 |
| Biflicker Duration of repetition [ms] | 0.561 | 0.065 | 0.352 | 0.433 | 0.689 |
| Velo Horizontal Average precision error [°] right | 0.444 | 0.063 | 0.392 | 0.320 | 0.568 |
| Velo Horizontal Average peak speed [°/s] right | 0.447 | 0.066 | 0.416 | 0.318 | 0.575 |
| Biflicker Vertical Duration of repetition [ms] | 0.451 | 0.066 | 0.454 | 0.322 | 0.580 |
| Biflicker Main saccade amplitude [°] left/Biflicker Gain of the main saccade [%] left | 0.547 | 0.065 | 0.471 | 0.420 | 0.674 |
| Velo Horizontal Average precision error [°] left | 0.454 | 0.064 | 0.486 | 0.329 | 0.580 |
| Velo Vertical Duration of repetition [ms] | 0.456 | 0.065 | 0.507 | 0.330 | 0.583 |
| Biflicker direction with respect to the X-axis in the UZS. [°] left | 0.538 | 0.066 | 0.562 | 0.409 | 0.67 |
| Biflicker Number of saccades left | 0.533 | 0.064 | 0.610 | 0.408 | 0.659 |
| Biflicker Vertical V_max of the main saccade [°/s] right | 0.467 | 0.069 | 0.617 | 0.332 | 0.603 |
| Biflicker vertical Duration of main saccade [ms] left/right | 0.470 | 0.067 | 0.650 | 0.339 | 0.602 |
| Biflicker vertical direction with respect to the X-axis in the UZS. [°] right | 0.527 | 0.065 | 0.677 | 0.399 | 0.655 |
| Biflicker Latency of the main saccade to the trigger [ms] left | 0.474 | 0.065 | 0.694 | 0.346 | 0.602 |
| Biflicker vertical gain of the main saccade [%] right | 0.475 | 0.067 | 0.698 | 0.343 | 0.606 |
| Biflicker Vertical gain of main saccade [%] left | 0.477 | 0.066 | 0.722 | 0.347 | 0.607 |
| Biflicker Number of saccades right | 0.522 | 0.064 | 0.733 | 0.397 | 0.648 |
| Biflicker vertical main saccade amplitude [°] left | 0.478 | 0.066 | 0.736 | 0.349 | 0.607 |
| Velo vertical blink rate [#/s] left | 0.521 | 0.065 | 0.747 | 0.394 | 0.649 |
| Velo vertical blink rate [#/s] right | 0.521 | 0.065 | 0.747 | 0.394 | 0.649 |
| Biflicker Vertical Main saccade amplitude [°] right | 0.479 | 0.068 | 0.754 | 0.347 | 0.612 |
| Velo Vertical Number of eyelid closures left/right | 0.521 | 0.065 | 0.754 | 0.393 | 0.648 |
| Biflicker Vertical Latency main saccade to trigger [ms] left/right | 0.519 | 0.065 | 0.775 | 0.390 | 0.647 |
| Biflicker directional error prosaccade [%] right | 0.517 | 0.067 | 0.793 | 0.386 | 0.649 |
| Biflicker Vertical Direction error prosaccade [%] left | 0.488 | 0.068 | 0.859 | 0.355 | 0.622 |
| Velo Vertical Average precision error [°] left | 0.490 | 0.064 | 0.881 | 0.364 | 0.616 |
| Biflicker Vertical Direction with respect to the X-axis in UZS. [°] left | 0.509 | 0.065 | 0.896 | 0.381 | 0.636 |
| Biflicker V_max of the main saccade [°/s] right | 0.508 | 0.069 | 0.899 | 0.373 | 0.644 |
| Biflicker trigger direction with respect to the X-axis in the UZS. [°] | 0.508 | 0.065 | 0.903 | 0.380 | 0.636 |
| Velo Horizontal Number of saccades left | 0.493 | 0.066 | 0.918 | 0.365 | 0.622 |
| Biflicker direction error prosaccade [%] left | 0.494 | 0.068 | 0.925 | 0.361 | 0.626 |
| Velo Horizontal Number of saccades right | 0.494 | 0.066 | 0.925 | 0.365 | 0.622 |
| Biflicker Number of left/right eyelid closures | 0.506 | 0.065 | 0.925 | 0.378 | 0.634 |
| Velo Vertical Average precision error [°] right | 0.505 | 0.069 | 0.944 | 0.369 | 0.640 |
| Biflicker Blink rate [#/s] left/right | 0.504 | 0.065 | 0.948 | 0.376 | 0.633 |
| Biflicker Vertical Directional error prosaccade [%] right | 0.498 | 0.067 | 0.978 | 0.366 | 0.630 |
| Velo Vertical Average top speed [°/s] right | 0.502 | 0.066 | 0.978 | 0.373 | 0.630 |
| Descriptives | |||||
|---|---|---|---|---|---|
| State | Statistic | Std. Error | |||
| Velo Horizontal Number of eyelid closures left/right | no TBI | Mean | 2.19 | 0.900 | |
| 95% Confidence Interval for Mean | Lower Bound | 0.35 | |||
| Upper Bound | 4.02 | ||||
| 5% Trimmed Mean | 1.31 | ||||
| Median | 0.00 | ||||
| Variance | 25.899 | ||||
| Std. Deviation | 5.089 | ||||
| Minimum | 0 | ||||
| Maximum | 22 | ||||
| Range | 22 | ||||
| Interquartile Range | 2 | ||||
| Skewness | 3.008 | 0.414 | |||
| Kurtosis | 8.874 | 0.809 | |||
| mTBI | Mean | 3.71 | 0.765 | ||
| 95% Confidence Interval for Mean | Lower Bound | 2.17 | |||
| Upper Bound | 5.24 | ||||
| 5% Trimmed Mean | 2.97 | ||||
| Median | 1.00 | ||||
| Variance | 29.812 | ||||
| Std. Deviation | 5.460 | ||||
| Minimum | 0 | ||||
| Maximum | 22 | ||||
| Range | 22 | ||||
| Interquartile Range | 5 | ||||
| Skewness | 2.040 | 0.333 | |||
| Kurtosis | 3.846 | 0.656 | |||
| Descriptives | |||||
|---|---|---|---|---|---|
| State | Statistic | Std. Error | |||
| Velo Horizontal Blink rate [#/s] left/right | no TBI | Mean | 0.1985 | 0.08162 | |
| 95% Confidence Interval for Mean | Lower Bound | 0.0320 | |||
| Upper Bound | 0.3650 | ||||
| 5% Trimmed Mean | 0.1191 | ||||
| Median | 0.0000 | ||||
| Variance | 0.213 | ||||
| Std. Deviation | 0.46171 | ||||
| Minimum | 0.00 | ||||
| Maximum | 2.00 | ||||
| Range | 2.00 | ||||
| Interquartile Range | 0.16 | ||||
| Skewness | 3.008 | 0.414 | |||
| Kurtosis | 8.872 | 0.809 | |||
| mTBI | Mean | 0.3364 | 0.06940 | ||
| 95% Confidence Interval for Mean | Lower Bound | 0.1970 | |||
| Upper Bound | 0.4758 | ||||
| 5% Trimmed Mean | 0.2701 | ||||
| Median | 0.0908 | ||||
| Variance | 0.246 | ||||
| Std. Deviation | 0.49563 | ||||
| Minimum | 0.00 | ||||
| Maximum | 2.00 | ||||
| Range | 2.00 | ||||
| Interquartile Range | 0.45 | ||||
| Skewness | 2.040 | 0.333 | |||
| Kurtosis | 3.843 | 0.656 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sikorski, F.; Güthoff, C.; Schmehl, I.; Rogge, W.; Frese, J.; Schulz, A.-P.; Gonschorek, A. Diagnosis of mTBI in an ER Setting Using Eye-Tracking and Virtual Reality Technology: An Exploratory Study. Brain Sci. 2025, 15, 1051. https://doi.org/10.3390/brainsci15101051
Sikorski F, Güthoff C, Schmehl I, Rogge W, Frese J, Schulz A-P, Gonschorek A. Diagnosis of mTBI in an ER Setting Using Eye-Tracking and Virtual Reality Technology: An Exploratory Study. Brain Sciences. 2025; 15(10):1051. https://doi.org/10.3390/brainsci15101051
Chicago/Turabian StyleSikorski, Felix, Claas Güthoff, Ingo Schmehl, Witold Rogge, Jasper Frese, Arndt-Peter Schulz, and Andreas Gonschorek. 2025. "Diagnosis of mTBI in an ER Setting Using Eye-Tracking and Virtual Reality Technology: An Exploratory Study" Brain Sciences 15, no. 10: 1051. https://doi.org/10.3390/brainsci15101051
APA StyleSikorski, F., Güthoff, C., Schmehl, I., Rogge, W., Frese, J., Schulz, A.-P., & Gonschorek, A. (2025). Diagnosis of mTBI in an ER Setting Using Eye-Tracking and Virtual Reality Technology: An Exploratory Study. Brain Sciences, 15(10), 1051. https://doi.org/10.3390/brainsci15101051





