Accurate Identification of ADHD among Adults Using Real-Time Activity Data
Abstract
:1. Introduction
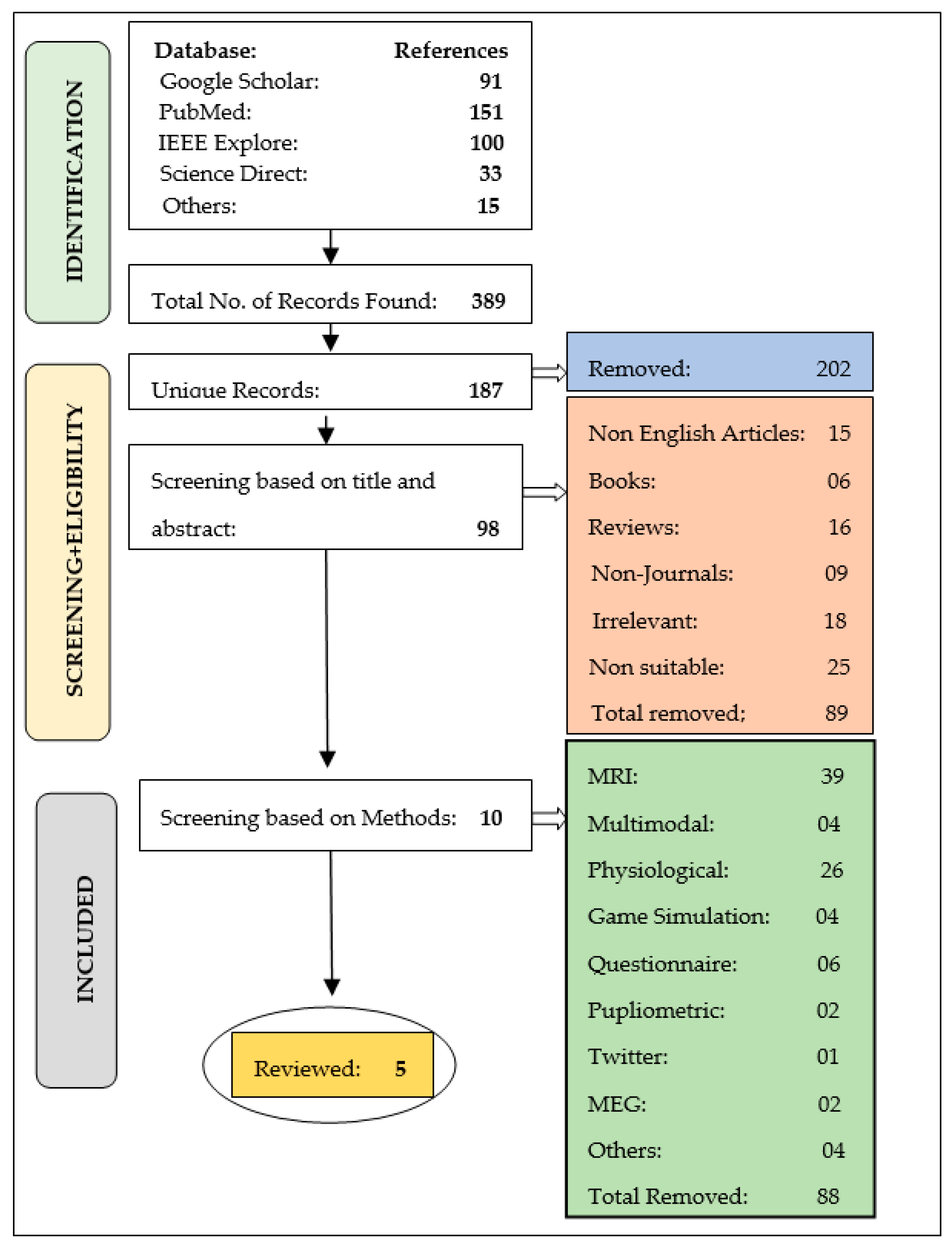
2. Literature Survey
- Only one study out of five has utilized an adult dataset to diagnose ADHD.
- The majority of the studies relied on private datasets, which necessitated a significant amount of effort and time for data gathering and processing.
- On the activity datasets, only five studies have used machine learning approaches.
- The machine learning models applied to the activity dataset even did not provide many reliable and precise results.
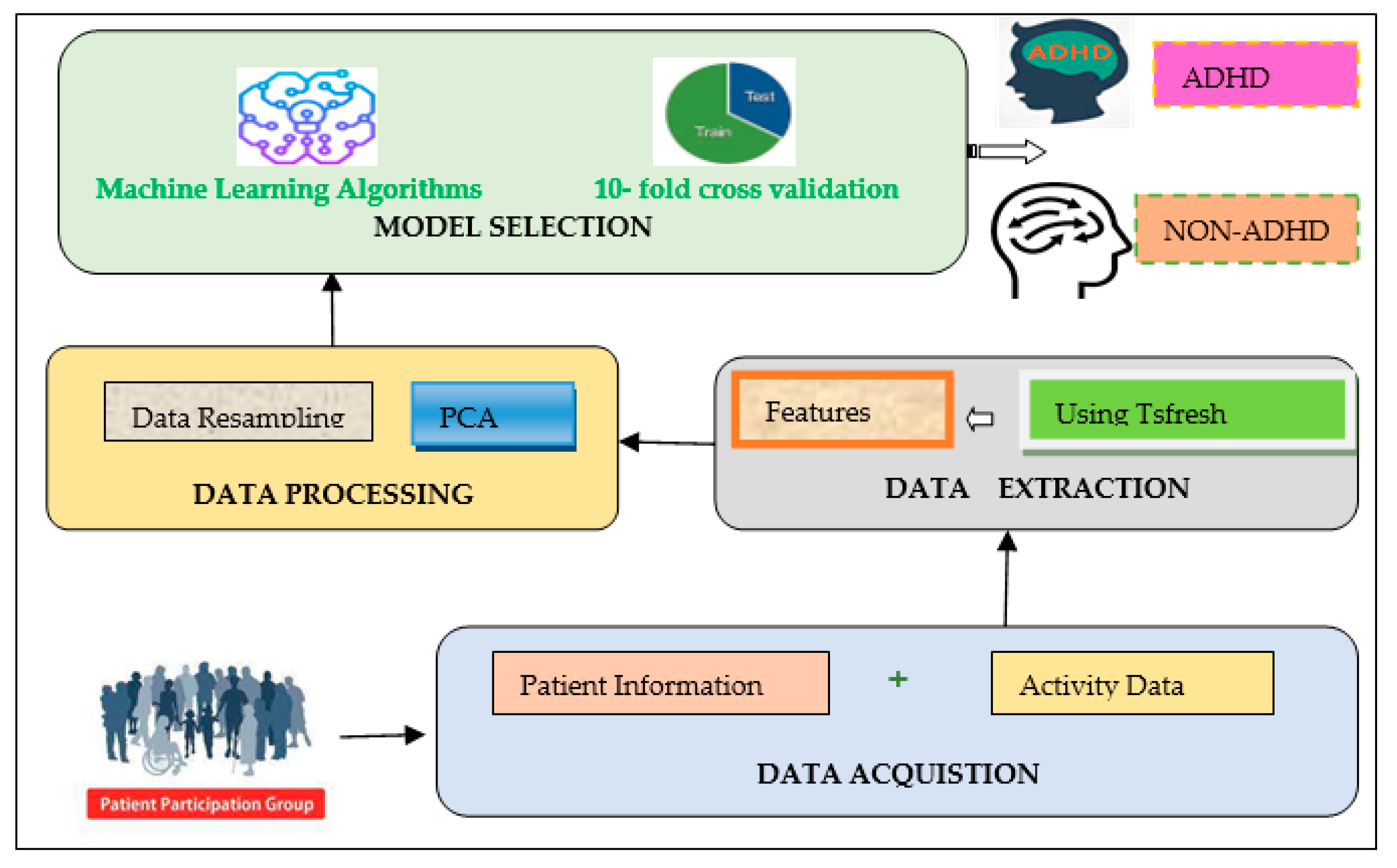
3. Methods and Materials
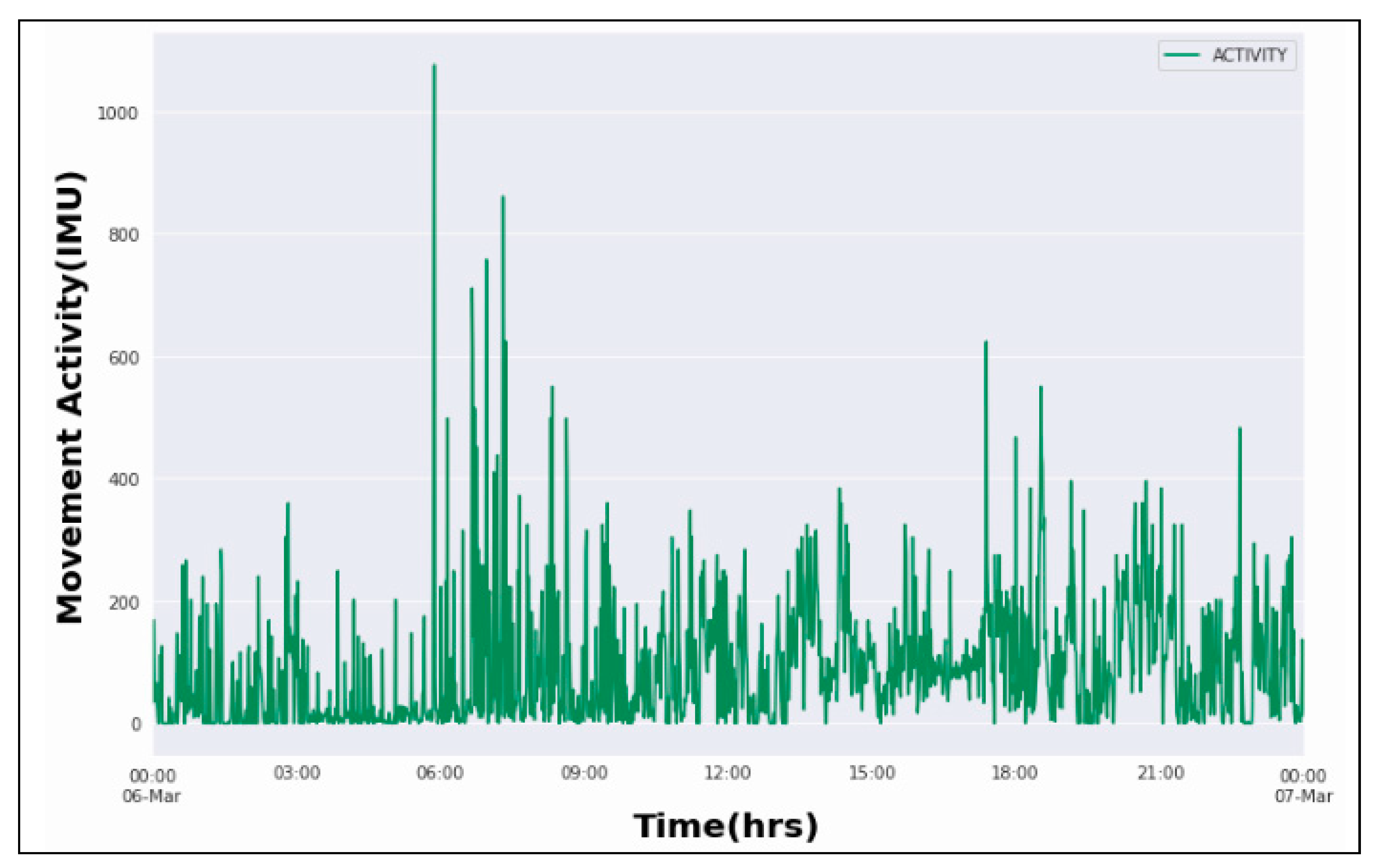
3.1. Data Acquisition
3.2. Feature Extraction
3.3. Feature Processing
4. Model Selection
4.1. Machine Learning Techniques and Hyperparameter Tuning
4.1.1. Support Vector Machine (SVM)
4.1.2. Naive Bayes (NB)
4.1.3. C 4.5 Decision Tree
4.1.4. Random Forest (RF)
4.1.5. k-Nearest Neighbor (kNN)
4.1.6. Logit Boost (LBoost)
4.2. Performance Evaluation
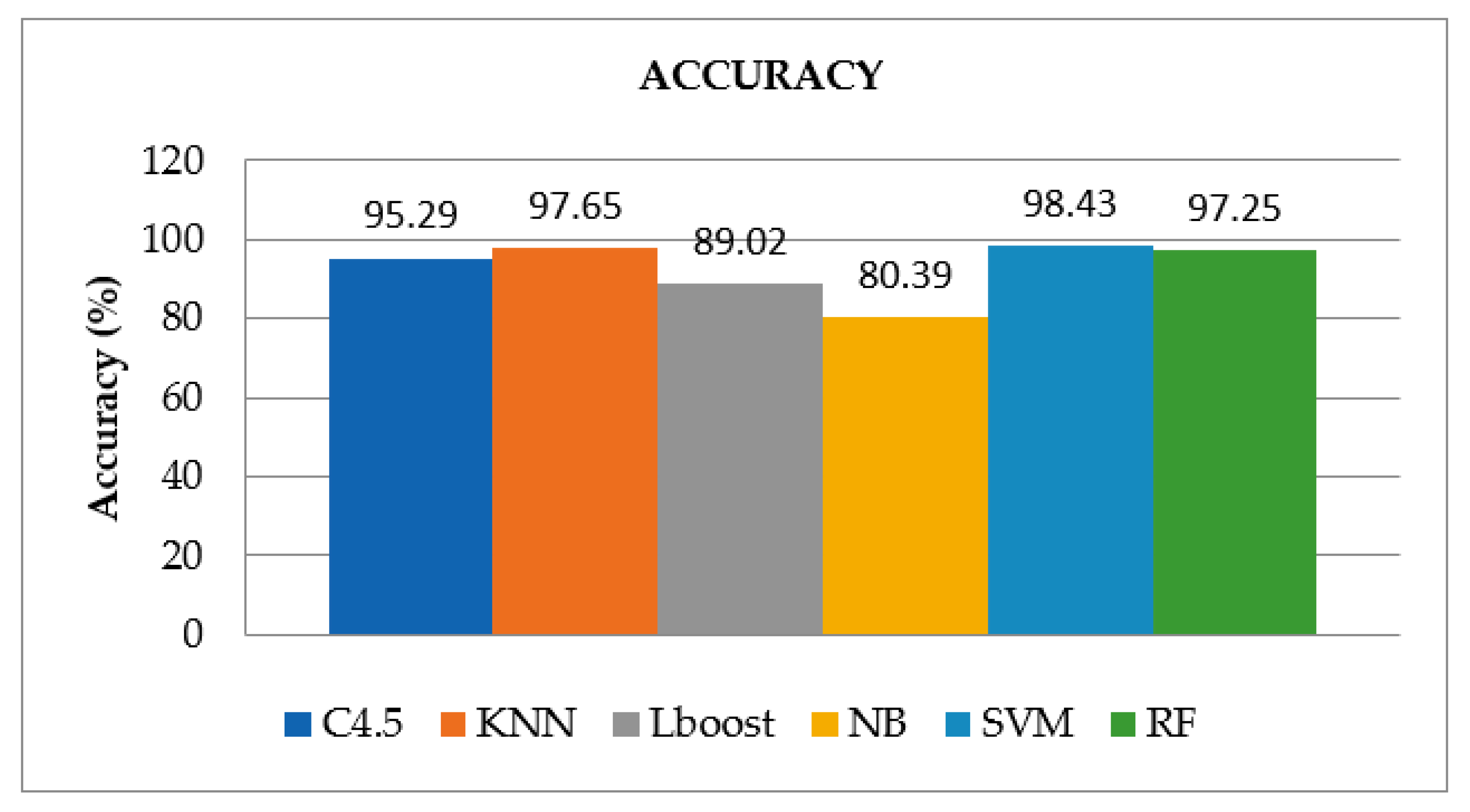
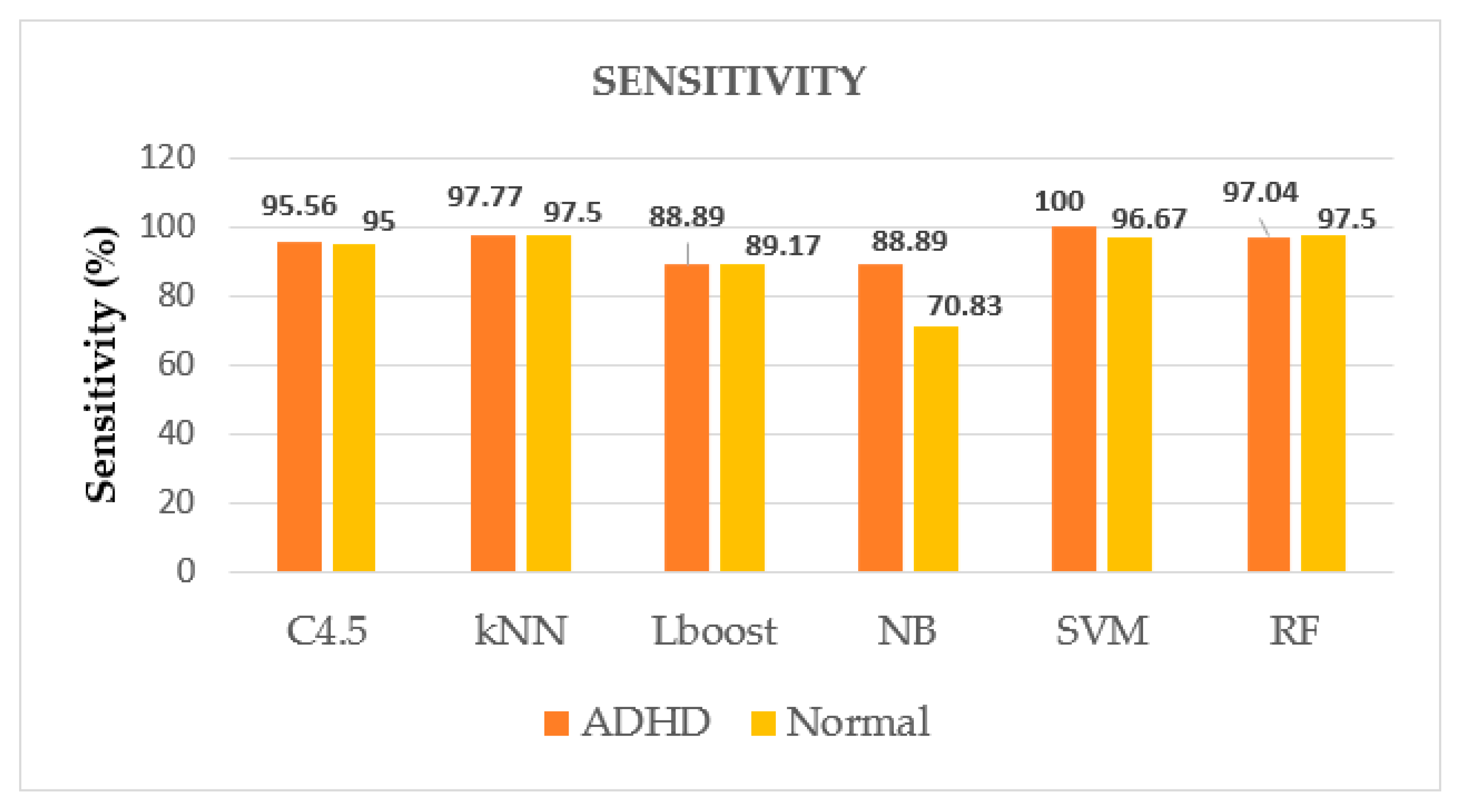
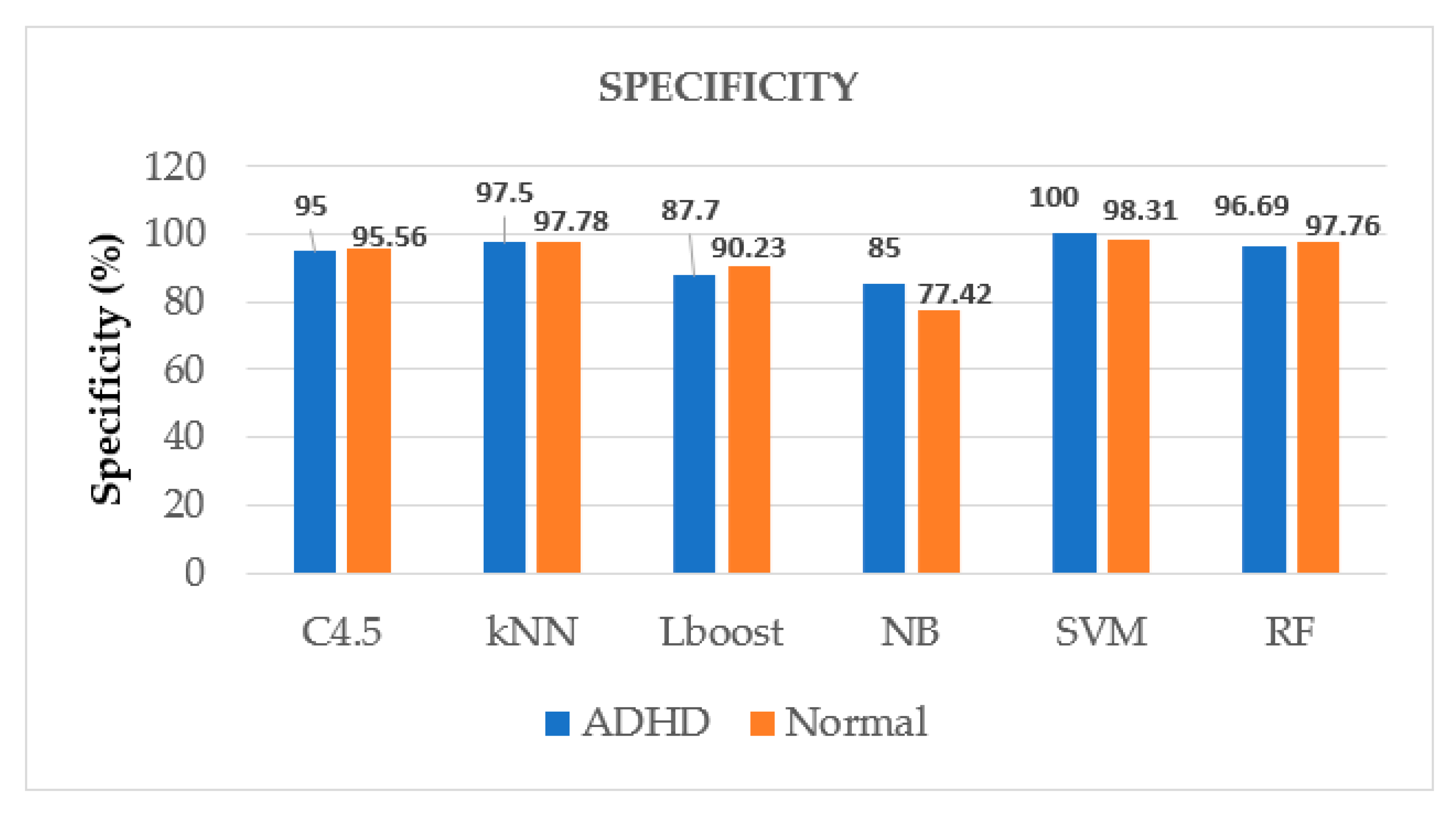
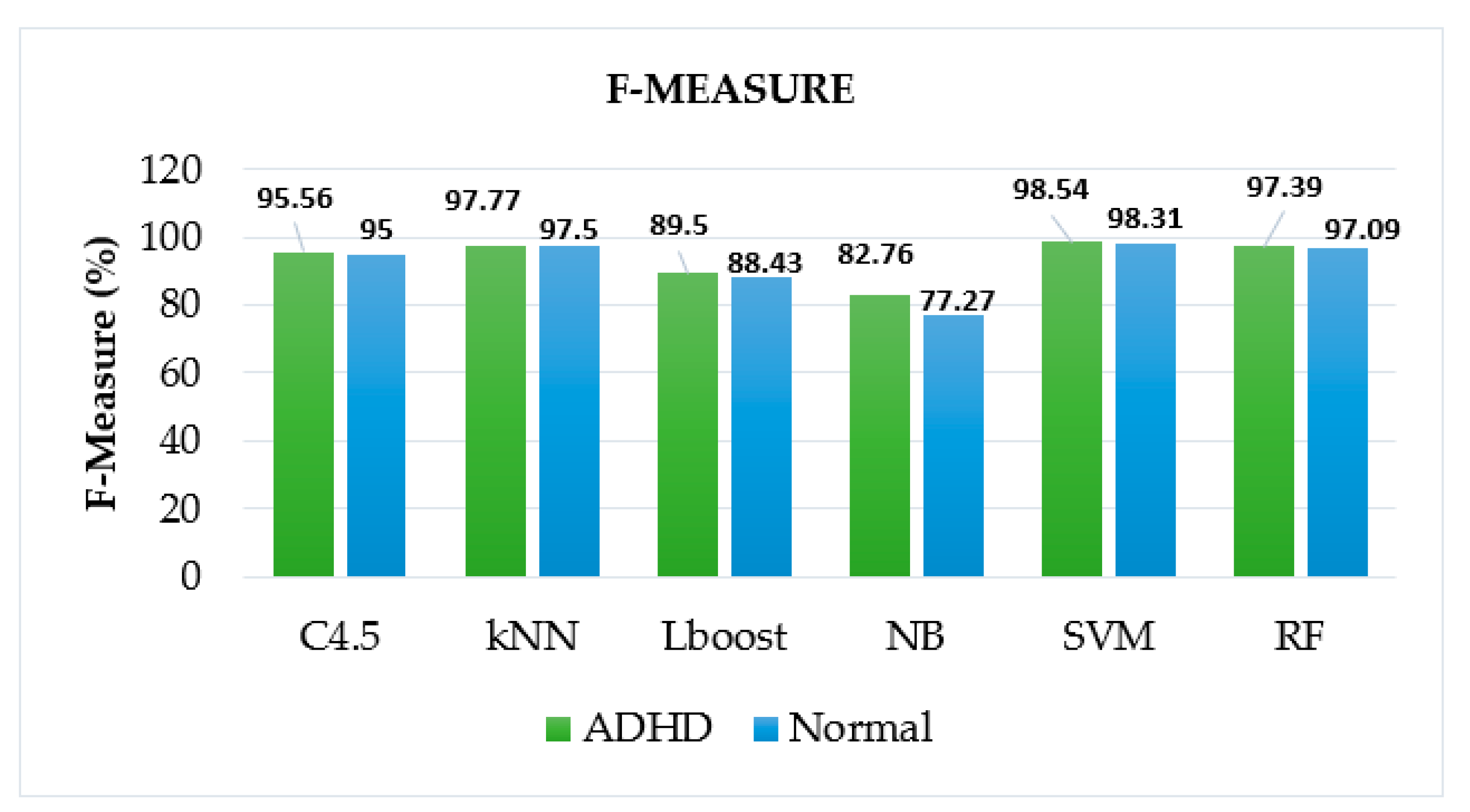
5. Results
6. Discussion
6.1. This Work
6.2. Contributions and Limitations
6.3. Future Scope
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ADHD | Attention Deficit Hyperactivity Disorder |
| ADD | Attention Deficit Disorder |
| AUC | Area Under the ROC Curve |
| HRV | Heart Rate Variability |
| IGR | Information Gain Ratio |
| IMU | Inertial Measurement Unit |
| kNN | k-Nearest Neighbor |
| LBoost | Logit Boost |
| ML | Machine Learning |
| NB | Naïve Bayes |
| PCA | Principal Component Analysis |
| RF | Random Forest |
| SVM | Support Vector Machine |
| WURS | Wender Utah Rating Scale |
| MADRS | Montgomery and Asberg Depression Rating Scale |
References
- Hicks, S.A.; Stautland, A.; Fasmer, O.B.; Forland, W.; Hammer, H.L.; Halvorsen, P.; Mjeldheim, K.; Oedegaard, K.J.; Osnes, B.; Syrstad, V.E.G.; et al. Hyperaktiv: An Activity Dataset from Adult Patients with Attention-Deficit/Hyperactivity Disorder (ADHD). In Proceedings of the 12th ACM Multimedia Systems Conference (MMSys ’21), Istanbul, Turkey, 28 September–1 October 2021; Volume 1, pp. 314–319. [Google Scholar]
- Brahmbhatt, K.; Hity, D.M.; Hah, M.; Han, J.; Angkustsiri, K.; Schweitzer, J. Diagnosis and Treatment of Adhd During Adolescence in the Primary Care Setting: Review and Future Directions. J. Adolesc. Health 2016, 59, 135–143. [Google Scholar] [CrossRef] [Green Version]
- Seidman, L.J.; Valera, E.M.; Makris, N. Structural brain imaging of attention-deficit/hyperactivity disorder. Biol. Psychiatry 2005, 57, 1263–1272. [Google Scholar] [CrossRef] [PubMed]
- Bassett, D.S.; Meyer-Lindenberg, A.; Achard, S.; Duke, T.; Bullmore, E. Adaptive reconfiguration of fractal small-world human brain functional networks. Proc. Natl. Acad. Sci. USA 2006, 103, 19518–19523. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shaw, P.; Stringaris, A.; Nigg, J.; Leibenluft, E. Emotion dysregulation in attention deficit hyperactivity disorder. American J. Psychiatry 2014, 171, 276–293. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ellison, A.T.; Johnson, B.B.; Harrell, M.N. Attention-Deficit/Hyperactivity Disorders (ADHD); Elsevier: Amsterdam, The Netherlands, 2016. [Google Scholar]
- Sayal, K.; Prasad, V.; Daley, D.; Ford, T.; Coghill, D. ADHD in children and young people: Prevalence, care pathways, and service provision. Lancet Psychiatry 2018, 5, 175–186. [Google Scholar] [CrossRef]
- Syrstad, V.E.G.; Oedagaard, K.J.; Fasmer, O.B.; Halmay, A.; Haavik, J.; Dilsaver, S.; Gjestad, R. Cyclothymic temperament: Associations with ADHD, other psychopathology, and medical morbidity in the general population. J. Affect. Disord. 2019, 260, 440–447. [Google Scholar] [CrossRef]
- Tistarelli, N.; Fagnani, C.; Troianiello, M.; Stazi, M.A.; Adriani, W. The nature and nurture of ADHD and its comorbidities: A narrative review on twin studies. Neurosci. Biobehav. Rev. 2020, 109, 63–77. [Google Scholar] [CrossRef]
- Barkley, A.R. Attention Deficit Hyperactivity Disorder: A Handbook for Diagnosis and Treatment; Guilford Press: New York, NY, USA, 2015; Volume 20. [Google Scholar]
- Swanson, J.M.; Kinsbourne, M.; Nigg, J.; Lamphear, B.; Stefanatos, G.A.; Volkow, N.; Taylor, E.; Casey, B.J.; Castellanos, F.X.; Wadhwa, P.D. Etiologic Subtypes of Attention-Deficit/Hyperactivity Disorder: Brain Imaging, Molecular Genetic and Environmental Factors and the Dopamine Hypothesis. Neuropsychol. Rev. 2007, 17, 39–59. [Google Scholar] [CrossRef]
- Rantekkar, U.P.; Reirsen, A.M.; Todoron, A.A.; Todd, R.D. Sex and age differences in Attention-Deficit/Hyperactivity Disorder symptoms and diagnoses: Implications for DSM-V and ICD-11. J. Am. Acad. Child Adolesc. Psychiatry 2011, 49, 217–228. [Google Scholar]
- Hinshaw, S.P.; Owens, E.B.; Zalecki, C.; Huggins, S.P.; Nevado, A.J.M.; Schrodek, E.; Swanson, E.N. Prospective follow-up of girls with attention-deficit/ hyperactivity disorder into early adulthood: Continuing impairment includes elevated risk for suicide attempts and self-injury. J. Consult. Clin. Psychol. 2012, 80, 1041–1051. [Google Scholar] [CrossRef] [Green Version]
- Hinshaw, S.P.; Arnold, L.E. ADHD, Multimodal Treatment, and Longitudinal Outcome: Evidence, Paradox, and Challenge. Wiley Interdiscip. Rev. Cogn. Sci. 2015, 6, 39–52. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Volkow, N.; Swanson, J. Adult attention deficit–hyperactivity disorder. New Engl. J. Med. 2013, 369, 1935–1944. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Das, W.; Khanna, S. A Robust Machine Learning Based Framework for the Automated Detection of ADHD Using Pupillometric Biomarkers and Time Series Analysis. Sci. Rep. 2021, 11, 16370. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Ceja, E.; Riegler, M.; Nordgreen, T.; Jakobsen, P.; Oedgaard, K.J.; Tørresen, J. Mental health monitoring with multimodal sensing and machine learning: A survey. Pervasive Mob. Comput. 2018, 51, 1–26. [Google Scholar] [CrossRef]
- Koh, J.E.W.; Ooi, C.P.; Vicnesh, J.; Oh, S.L. Automated classification of attention deficit hyperactivity disorder and conduct disorder using entropy features with ECG signals. Comput. Biol. Med. 2022, 140, 105–120. [Google Scholar] [CrossRef]
- Ahmadi, A.; Kashefi, M.; Shahrokhi, S.; Nazari, M.A. Computer aided diagnosis system using deep convolutional neural networks for ADHD subtypes. Biomed. Signal Processing Control 2021, 63, 102–227. [Google Scholar] [CrossRef]
- Öztoprak, H.; Toucan, M.; Alp, Y.K.; Arıkan, O.; Doğutepe, E.; Karakaş, S. Machine-based classification of ADHD and non-ADHD participants using time/frequency features of event-related neuroelectric activity. Clin. Neurophysiol. 2017, 128, 2400–2410. [Google Scholar] [CrossRef]
- Bohland, J.W.; Saperstein, S.; Pereira, F.; Rapin, J.; Grady, L. Network, anatomical, and non-imaging measures for the prediction of ADHD diagnosis in individual subjects. Front. Syst. Neurosci. 2012, 6, 1–36. [Google Scholar] [CrossRef] [Green Version]
- Tang, Y.; Sun, J.; Wang, C.; Zhong, Y.; Jiang, A.; Liu, G.; Liu, X. ADHD classification using auto-encoding neural network and binary hypothesis testing. Artif. Intell. Med. 2022, 123, 102–109. [Google Scholar] [CrossRef]
- Heller, M.D.; Roots, K.; Srivastava, S.; Schumann, J.; Srivastava, J.; Hale, T.S. A Machine Learning-Based Analysis of Game Data for Attention Deficit Hyperactivity Disorder Assessment. Games Health J. 2013, 2, 291–298. [Google Scholar] [CrossRef]
- O’Mahony, N.; Florentino-Liano, B.; Carballo, J.J.; Baca-García, E.; Rodríguez, A.A. Objective diagnosis of ADHD using IMUs. Med. Eng. Phys. 2014, 36, 922–926. [Google Scholar] [CrossRef] [PubMed]
- Zolubak, M.; Paszkiel, S. EEG Analysis and Neurofeedback Therapy Concentration Problems in Mother and Child. In Advances in Intelligent Systems and Computing (AISC); Springer: Charm, Switzerland, 2021; Volume 362, pp. 79–93. [Google Scholar]
- Martin, J.L.; Hakim, A.D. Wrist actigraphy. Chest 2011, 139, 1514–1527. [Google Scholar] [CrossRef] [PubMed]
- Muñoz-Organero, M.; Powell, L.; Heller, B.; Harpin, V.; Parker, J. Automatic extraction and detection of characteristic movement patterns in children with ADHD based on a convolutional neural network (CNN) and acceleration images. Sensors 2018, 18, 3924. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Faedda, G.L.; Ohashi, K.; Hernandez, N.; McGreenery, C.E.; Grant, M.C.; Baroni, A.; Polcari, A.; Teicher, M.H. Actigraph measures discriminate pediatric bipolar disorder from attention-deficit/hyperactivity disorder and typically developing controls. J. Child Psychol. Psychiatry Allied Discip. 2016, 57, 706–716. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Amado-Caballero, P.; Casaseca-da-la-Higuera, P.; Alberola-Lopez, S.; Andres-de-Llano, J.M.; Villalobos, J.A.L.; Garmendia-Leiza, J.R.; Alberola-Lopez, C. Objective ADHD Diagnosis Using Convolutional Neural Networks over Daily-Life Activity Records. IEEE J. Biomed. Health Inform. 2020, 24, 2690–2700. [Google Scholar] [CrossRef] [Green Version]
- Fasmer, O.B.; Fasmer, E.E.; Mjeldheim, K.; Forland, W.; Syrstad, V.E.G.; Jakobsen, P.; Berle, J.Ø.; Henriksen, T.E.G.; Sepasdar, Z.; Hauge, E.R.; et al. Diurnal variation of motor activity in adult ADHD patients analyzed with methods from graph theory. PLoS ONE 2020, 15, e0241991. [Google Scholar] [CrossRef]
- Usami, M.; Okada, T.; Sasayama, D.; Iwadare, Y.; Watanable, K.; Ushijima, H.; Kodaira, M.; Sugiyama, N.; Sawa, T.; Saito, K. What time periods of the day are concerning for parents of children with attention deficit hyperactivity disorder? PLoS ONE 2013, 8, e79806. [Google Scholar] [CrossRef] [Green Version]
- Álvarez, R.F.P.; Batra, C.; Carpentier, P.J.; Carrithers, S.; Crunelle, C.L.; Demetrovics, Z.; Dom, G.; Faraone, S.V.; Franck, J.; Johnson, B.; et al. Validity of the ADHD module of the Mini International Neuropsychiatric Interview PLUS for screening of adult ADHD in treatment seeking substance use disorder patients: ADHD screening with MINI-Plus. Rev. Psiquiatr. Y Salud Ment. 2020; in press. [Google Scholar] [CrossRef]
- Conners, C.K.; Sitarenios, G. Conners’ Continuous Performance Test (CPT), Encyclopedia of Clinical Neuropsychology; Springer: New York, NY, USA, 2011. [Google Scholar]
- Brage, S.; Brage, N.; Franks, P.W.; Ekelund, U.; Wareham, N.J. Reliability and validity of the combined heart rate and movement sensor Actiheart. Eur. J. Clin. Nutr. 2005, 59, 561–570. [Google Scholar] [CrossRef] [Green Version]
- Google Colaboratory, Welcome to Colaboratory. Available online: https://colab.research.google.com (accessed on 20 May 2022).
- Hawley, C.J.; Gale, T.M.; Sivakumaran, T. Defining remission by cut-off score on the MADRS: Selecting the optimal value. J. Affect. Disord. 2002, 72, 177–184. [Google Scholar] [CrossRef]
- Brevik, E.J.; Lundervold, A.J.; Haavik, J.; Posserud, M.B. Validity and accuracy of the Adult Attention-Deficit/Hyperactivity Disorder (ADHD) Self-Report Scale (ASRS) and the Wender Utah Rating Scale (WURS) symptom checklists in discriminating between adults with and without ADHD. Brain Behav. 2020, 10, e01605. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Christ, M.; Braun, N.; Neuffer, J.; Kempa-Liehr, A.W. Time Series Feature Extraction on basis of Scalable Hypothesis tests (tsfresh—A Python package). Neurocomputing 2018, 307, 72–77. [Google Scholar] [CrossRef]
- Heaton, J. An empirical analysis of feature engineering for predictive modeling. In Proceedings of the SoutheastCon2016, Norfolk, VA, USA, 30 March–3 April 2016; pp. 1–6. [Google Scholar]
- Jolliffe, I.T.; Cadima, J. Principal component analysis: A review and recent developments. Philos. Trans. R. Soc. A 2016, 374, 20150202. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Castelló, A. Principal components analysis in clinical studies. Ann. Transl. Med. 2017, 5, 3–9. [Google Scholar] [CrossRef] [Green Version]
- Cervantes, J.; Garcia-Lamont, F.; Rodriguez-Mazahua, L.; Lopez, A. A comprehensive survey on support vector machine classification: Applications, challenges and trends. Neurocomputing 2020, 408, 189–215. [Google Scholar] [CrossRef]
- Kaviani, P.; Dhotre, S. Short Survey on Naïve Bayes Algorithm. Int. J. Adv. Res. Comput. Sci. Manag. 2017, 4, 607–611. [Google Scholar]
- Patel, H.; Prajapati, P. Study and Analysis of Decision Tree based classification algorithms. Int. J. Comput. Sci. Eng. 2018, 6, 74–78. [Google Scholar] [CrossRef]
- Breiman, L. Random Forests. Mach. Learn. 2001, 45, 5–32. [Google Scholar] [CrossRef] [Green Version]
- Gou, G.; Wang, H.; Bell, D.A.; Bi, Y.; Greer, K. kNN Model Based Approach in Classification. In On the Move to Meaningful Internet Systems, 2003: CoopIS, DOA and ODBASE.OTM 2003. Lecture Notes in Computer Science; Springer: Berlin/Heidelberg, Germany, 2003; Volume 2888. [Google Scholar]
- Sun, P.; Reid, M.; Zhou, J. An improved multiclass LogitBoost using adaptive one-vs-one. Mach. Learn. 2014, 97, 295–326. [Google Scholar] [CrossRef]
- Baratloo, A.; Hosseini, M.; Negida, A.; Ashal, G.A.I. Part 1: Simple Definition and Calculation of Accuracy, Sensitivity and Specificity. 2015. Available online: https://www.jemerg.com (accessed on 21 April 2022).
- Sasaki, Y. The truth of the F-measure. Teach Tutor Mater 2007, 1, 1–5. [Google Scholar]
- Hajian-Tilaki, K. Receiver operating characteristic (ROC) curve analysis for medical diagnostic test evaluation. Casp. J. Intern. Med. 2013, 4, 627–635. [Google Scholar]
- Lin, J.; Chang, Y.; Chang, C.; Ko, L. Applications of Transfer Learning in Field verification for children in Attention Deficit Hyperactivity Disorder. In Proceedings of the International Conference in Fuzzy Theory and its Applications, Taitung, Taiwan, 5–8 October 2021. [Google Scholar]
- Vahid, A.; Bluschke, A.; Roessner, V.; Stober, S.; Bete, C. Deep Learning based on Event-Related EEG differentiates children with ADHD from Healthy Controls. J. Clin. Med. 2021, 8, 1055. [Google Scholar] [CrossRef] [PubMed] [Green Version]



| S.No | Reference | Year | Dataset | Age Group | Public/Private | Method | Features | Model | Validation Approach | Highest Accuracy |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Munoz-Organero et al. [27] | 2018 | 22 school children with ADHD = 11, Paired Controls = 11 | 6–15 years | Private | Two trial axial accelerometers: one on the wrist of the dominant arm and the other on the axle of the dominant leg | 2D acceleration images | Deep learning | 4-fold cross-validation | CNN 87.5% with wrist sensor and 93.8% with axle sensor |
| 2 | Faedda et al. [28] | 2016 | 155 children with ADHD = 44 ADHD + Depression = 21 Bipolar = 48 Controls = 42 | 5–18 years | Private | Belt worn actigraphs | 28 metrics | Machine Learning | 4-Fold cross validation | SVM 83.1% |
| 3 | Amado-Caballeroat et al. [29] | 2020 | 148 children with ADHD = 73 Normal = 75 | 6–15 years | Private | Wrist Worn ActiGraph GT3x | End-to-End | Deep Learning | 10 fold cross validation | CNN 98.6% |
| 4 | O’Mahony et al. [24] | 2014 | 43 children with ADHD = 24 Normal = 19 | 6–11 years | Private | Two IMU one at the waist and the other at the ankle of the dominant leg | Inertial measurement Units | Machine Learning | Leave one out cross-validation | SVM 95.1% |
| 5 | Hicks et al. [1] | 2021 | 103 patients with ADHD = 51 Normal = 52 | 17–67 years | Public | Wrist-worn Actigraph device | Feature extraction with tsfresh | Machine Learning | 10 fold cross-validation | Random Forest gives 72% |
| S.No | Model | Accuracy (%) | Sensitivity (%) | Specificity (%) | F-Measure (%) | AUC |
|---|---|---|---|---|---|---|
| 1 | C4.5 | 95.29 | 95.28 | 95.28 | 95.28 | 0.973 |
| 2 | kNN | 97.65 | 97.64 | 97.64 | 97.64 | 0.975 |
| 3 | LBoost | 89.02 | 89.03 | 88.96 | 88.99 | 0.941 |
| 4 | NB | 80.39 | 79.86 | 81.21 | 80.02 | 0.889 |
| 5 | SVM | 98.43 | 98.33 | 98.56 | 98.42 | 0.983 |
| 6 | RF | 97.25 | 97.27 | 97.23 | 97.25 | 0.999 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kaur, A.; Kahlon, K.S. Accurate Identification of ADHD among Adults Using Real-Time Activity Data. Brain Sci. 2022, 12, 831. https://doi.org/10.3390/brainsci12070831
Kaur A, Kahlon KS. Accurate Identification of ADHD among Adults Using Real-Time Activity Data. Brain Sciences. 2022; 12(7):831. https://doi.org/10.3390/brainsci12070831
Chicago/Turabian StyleKaur, Amandeep, and Karanjeet Singh Kahlon. 2022. "Accurate Identification of ADHD among Adults Using Real-Time Activity Data" Brain Sciences 12, no. 7: 831. https://doi.org/10.3390/brainsci12070831
APA StyleKaur, A., & Kahlon, K. S. (2022). Accurate Identification of ADHD among Adults Using Real-Time Activity Data. Brain Sciences, 12(7), 831. https://doi.org/10.3390/brainsci12070831






